
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr., 04 February 2020
Sec. Pediatric Otolaryngology
Volume 8 - 2020 | https://doi.org/10.3389/fped.2020.00022
 Ken Fukuda1
Ken Fukuda1 Hiroki Yasudo1*
Hiroki Yasudo1* Naoki Ohta1
Naoki Ohta1 Hiroko Narumi1
Hiroko Narumi1 Nozomi Abe1
Nozomi Abe1 Shunsuke Tarumoto2
Shunsuke Tarumoto2 Hiroshi Yamashita2
Hiroshi Yamashita2 Kiyoshi Ichihara3
Kiyoshi Ichihara3 Shouichi Ohga1,4
Shouichi Ohga1,4 Shunji Hasegawa1
Shunji Hasegawa1Delayed physical growth is a common complication of pediatric obstructive sleep apnea syndrome (OSAS). Adenotonsillectomy (AT) is the first-line treatment for pediatric OSAS. Only a few studies have performed time-course BMI evaluation in pediatric OSAS patients post-operatively. Thus, we aimed to evaluate the time-course changes in pediatric OSAS patients after AT. Thirty-three children with OSAS who underwent AT were included and divided into two groups on the basis of their BMI z-scores (delayed physical growth group, n = 15; non-delayed physical growth group, n = 18). Clinical records of height and weight were collected before AT and at 6, 12, 24, and 36 months after AT. Changes in the mean BMI z-scores of the two groups were assessed up to 36 months. The mean BMI z-score was significantly increased in the delayed physical growth group at 6 months after AT. In contrast, the increase in mean BMI z-score was not observed in the non-delayed physical growth group. Growth improvement was noted in pediatric OSAS patients with delayed physical growth after AT. Our results suggest that AT is a promising therapy for improving the physical growth of pediatric OSAS patients with such problems.
Obstructive sleep apnea syndrome (OSAS) in children is defined as a breathing disorder that occurs during sleep, characterized by sustained partial upper airway obstruction and/or intermittent complete obstruction (obstructive apnea), that inhibits normal breathing during sleep (1). It can occur in children of all ages from neonates to adolescents, and its prevalence is at least 1–3% (1–3). The clinical characteristics are snoring, difficulty in breathing during sleep, and repeated obstructive apnea (1, 4). Adenotonsillar hypertrophy (ATH) is the primary cause of OSAS in children, resulting in intermittent pharyngeal airway collapse intervened by airflow, hypoxemia, hypercapnia, and brief arousals from sleep (4). Complications of OSAS in children may include nocturnal enuresis, sweating during sleep, reduced neurocognition, behavioral problems, and school performance decline (5–7). Among the complications of OSAS, delayed physical growth is one of the most common concerns (5, 8, 9). Bonuck et al. (9) estimated that the prevalence of delayed physical growth due to OSAS in children younger than 6 years was 21%. ATH and sleep-disordered breathing are risk factors in the etiology of growth failure.
The first-line treatment of pediatric OSAS is adenotonsillectomy (AT). Polysomnographic resolution after AT is associated with symptom resolution (5, 10–13). Many studies have shown increases in height, weight, and BMI in OSAS patients after AT (5, 13–23), suggesting physical growth improvement. However, most of the studies measured patients' BMI only at a certain time point after the operation or lacked full records of time-course evaluation of BMI after the operation, indicating that the evaluations in these studies might be insufficient owing to the limited measurements of BMI for the time-course analysis of physical growth improvement after the operation. Additionally, the effect of AT should be compared between OSAS patients with and without delayed physical growth, as there are no studies investigating the effects of AT in OSAS patients according to the presence or absence of delayed physical growth.
The aim of our study was to evaluate physical growth changes in pediatric OSAS patients by consistently measuring BMI z-scores at 6, 12, 24, and 36 months after AT and to investigate how AT could affect physical growth changes in pediatric OSAS patients with or without delayed physical growth.
This is a retrospective observational study. We consecutively accumulated 176 OSAS children who underwent AT between January 2004 and May 2016 at the Department of Pediatrics and Otolaryngology in Yamaguchi University Hospital (24). OSAS was diagnosed on the basis of the International Classification of Sleep Disorders (third edition). Eight children were excluded because of comorbidity of chromosomal disorders, preterm birth, other cardiovascular diseases, and tumorous diseases. Of the remaining 168 patients, 135 were excluded because of incomplete body height and weight data within the required observation period of 36 months. As a result, 33 pediatric patients were enrolled in this study as shown in the flow chart of the case selection process (Figure 1).
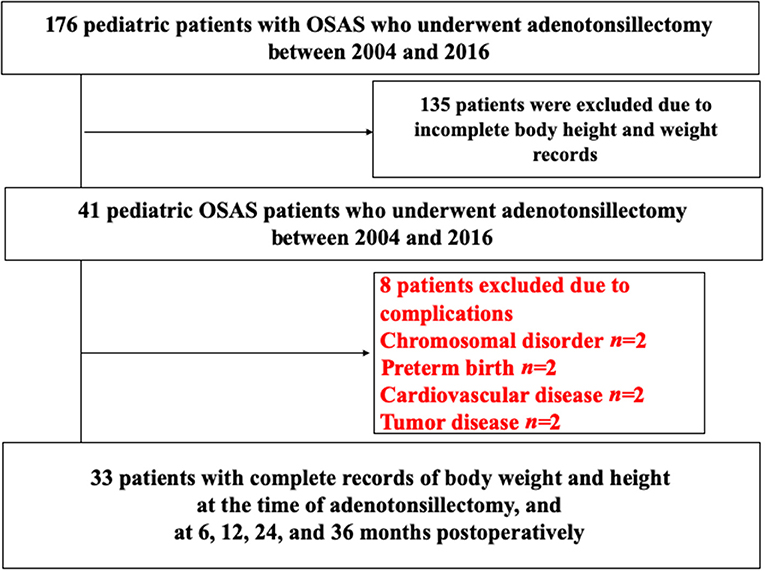
Figure 1. Flow chart for selecting the OSAS patients in this study. OSAS, obstructive sleep apnea syndrome.
Before the start of the operation, informed consent was obtained from patients and patients' parents. The study design was approved by the institutional ethics committee of Yamaguchi University Hospital (No. H30-150). For safety reasons, eight patients were excluded from the study if they had craniofacial anomalies, obesity, Down syndrome, neuromuscular disorders, sickle cell disease, mucopolysaccharidoses, cardiac complications, current respiratory infections, and a history of prior upper airway surgery. As a result, 33 pediatric OSAS patients with completely body weight and height records at the time of AT and at 6, 12, 24, 36 months post-operatively were enrolled for the study.
The enrolled patients were divided into two groups according to the values of the BMI z-scores: the delayed physical growth group (BMI z-scores <0, n = 18) and the non-delayed physical growth group (BMI z-scores ≥0, n = 15) to determine if there is any difference in the changes of the BMI z-score values after the operation.
We retrospectively analyzed the hospital records of OSAS patients who underwent AT at the Department of Otolaryngology and were followed up for 3 years post-operatively. All subjects were measured height and weight preoperatively and at 6, 12, 24, and 36 months post-operatively. All measurements were conducted by trained nurses. Height was measured by using a stadiometer to the nearest 1.0 mm. Weight was measured by using an electronic scale to the nearest 0.1 kg. For each child, z-scores for height and weight values were calculated by using the file produced by the Japanese 2,000 references (25). BMI z-scores were calculated according to Inokuchi et al. (26).
All statistical analyses were performed using JMP®13.1 (SAS Institute Inc., Cary, NC, USA). Data were analyzed for normal distributions using the Kolmogorov–Smirnov test and were presented as mean ± standard deviation. Pre-operative and post-operative (up to 24 months) SDS values for height and weight were compared using the paired t-test. To determine the significance of time-dependent changes between the pre-operative and post-operative (up to 36 months) BMI z-scores, the paired t-test was used with Bonferroni correction for multiple testing.
We evaluated the characteristics of the pediatric patients to determine any presence of delayed physical growth (Table 1). The mean height z-score, weight z-score, and BMI z-score at the operation were −0.42 SD (±1.45), −0.45 SD (±1.31), and −0.12 SD (±1.99), respectively, indicating that OSAS patients who underwent AT tend to have overall delayed growth.
There were no differences in the ratio of male to female and age between the two groups (Table 1). Moreover, we compared the mean BMI z-scores preoperatively and at 6, 12, 24, and 36 months after AT between the two groups (Figure 2). The mean BMI z-score had significantly increased by 6 months after AT in the delayed physical growth group, although there were no significant differences between 6 and 36 months after AT. Conversely, the mean BMI z-score had not increased in the non-delayed physical growth group during the study period. These results suggest that physical growth recovery was observed in the delayed physical growth group but not in the non-delayed physical growth group.
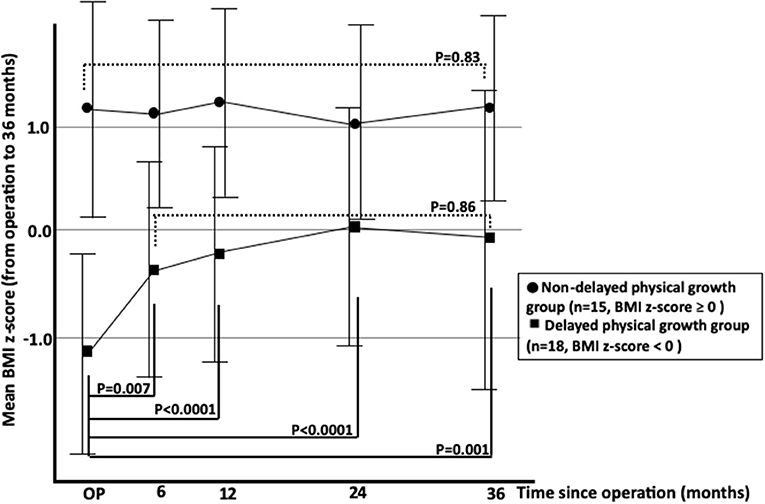
Figure 2. Changes in mean BMI z-scores of OSAS patients with delayed and non-delayed physical growth after adenotonsillectomy. OSAS, obstructive sleep apnea syndrome; BMI, body mass index.
We further divided the delayed physical growth group into two subgroups based on the values of BMI z-score [non-severe subgroup (n = 9): BMI z-score 0≥ and −1.0<; severe subgroup (n = 9): BMI z-score ≦ −1.0] (Figure 3). BMI z-scores had increased in both subgroups at 6 months after AT (Figure 3). However, changes in BMI z-score were more drastic in the severe subgroup than in the non-severe subgroup, suggesting that physical growth recovery was more prominently observed in patients with severe delayed physical growth at 6 months after AT than in those without severe delayed physical growth.

Figure 3. Changes in mean BMI z-scores of OSAS patients with severe and non-severe delayed physical growth after adenotonsillectomy. OSAS, obstructive sleep apnea syndrome; BMI, body mass index.
In this study, we compared the physical growth after AT between pediatric OSAS patients with and those without delayed physical growth. We found that the mean BMI z-score in patients with delayed physical growth was significantly increased after the operation and returned to the normal levels, whereas in patients without delayed physical growth, the mean BMI z-score did not increase. Additionally, the mean BMI z-score was more drastically increased in patients with severe delayed physical growth than in those without severe delayed physical growth. These results suggest that growth recovery can be expected in OSAS patients with delayed physical growth. Additionally, more dramatic physical growth recovery can be expected within 6 months in subjects with severe delayed physical growth after the AT operation.
Several lines of evidence have revealed that there are some factors associated with delayed physical growth in OSAS. OSAS patients are reported to be insensitive to growth hormone (GH) releasing hormone-induced GH response and a delayed insulin-like growth factor type 1 (IGF-1) synthesis after GH injection in untreated disease (27). AT may restore the GH axis activity resulting in growth recovery. Moreover, hypertrophied tonsil is a mechanical barrier for food intake, thus reducing caloric intake (28). Bar et al. (19) showed that 83% of parents reported an increase in their children's appetite following AT. Nachalon et al. (28) indicated a significant change in diet composition in children with OSAS after surgery. Sleep energy expenditure reduction and weight gain improvement by surgery suggest that the increased energy expenditure could have been caused by increased respiratory work during sleep in OSAS children (14). The reasons for physical growth recovery after AT in OSAS patients were not fully understood. However, the imbalance between caloric intake, energy expenditure, and insufficient growth hormone secretion could be associated with physical growth changes after AT. It is reported that IGF-1 and IGF binding protein-3 levels increase 3–6 months after AT (19, 24, 29). These results are consistent with the timing of physical growth recovery observed in our study.
There are some studies reporting obesity resulting from AT in OSAS patients (17, 20–22). In our study, the mean BMI z-score increased and returned to normal levels in OSAS patients with delayed physical growth, whereas the BMI z-score was not increased in those without delayed physical growth up to 36 months after AT. These results suggest that obesity is unlikely to be caused by AT in OSAS participants, regardless of the presence of delayed physical growth. The prevalence of obesity in Japanese 5 years-old is 2.73% for boys and 2.58% for girls (30). Asian children are more susceptible to metabolic disorders caused by obesity of even mild degree than the Caucasian. For this reason, more attention is generally paid to obesity at an early stage. Therefore, obese children may have already been restricted of food intake at home or school prior to the surgery, which may have suppressed the increase in post-operative food intake. As a matter of fact, a Korean report (31), which enrolled OSAS children similar to those of our study, had the same trend as our results. Hence, the peculiar phenomenon may be caused by racial difference. This study focused on delayed physical growth subgroup, but we would like to increase the number of cases so that the subgroup of obesity could be evaluated in the future.
Although there are many reports mentioning delayed physical growth as a common complication of OSAS, it is difficult to tell whether it is directly caused by OSAS or other factors. Our results showed that the mean BMI z-score returned to normal levels in participants with delayed physical growth after AT and that the mean BMI z-score was more drastically increased in patients with severe delayed physical growth within 6 months after AT. These results suggest that delayed physical growth in OSAS patients could be directly caused by OSAS, not by other reasons, and that AT can be a promising therapy to improve delayed physical growth in OSAS patients.
There are some limitations to this study. This study is a pilot study conducted in a single center. Further multi-center or prospective studies involving different regions, races, and populations are warranted to confirm whether AT is a promising therapy for growth improvement in OSAS patients with such problems.
Physical growth improvement was observed within 6 months after AT in OSAS patients with delayed physical growth but not in those without delayed physical growth. Thus, AT is a promising therapy for improving the physical growth of OSAS patients with such problems.
All datasets generated for this study are included in the article/supplementary material.
The studies involving human participants were reviewed and approved by the Institutional Ethics Committee of Yamaguchi University Hospital. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
HYas, SO, and SH were the principal investigators taking primary responsibility for the manuscript. KF, HYas, KI, HYam, SO, and SH performed the clinical management with helpful discussion for the completion of the study. KF, NO, HN, NA, ST, and HYam took responsibility for the diagnosis and data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank all the staff members who helped treat patients at Yamaguchi University Hospital for their assistance with patient care during our study.
1. Farber JM. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. (2002) 110:1255–7. doi: 10.1542/peds.110.6.1255-a
2. Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. (2012) 130:e714–55. doi: 10.1542/peds.2012-1672
3. Brunetti L, Rana S, Lospalluti ML, Pietrafesa A, Francavilla R, Fanelli M, et al. Prevalence of obstructive sleep apnea syndrome in a cohort of 1,207 children of southern Italy. Chest. (2001) 120:1930–5. doi: 10.1378/chest.120.6.1930
4. Martin J, Hiscock H, Hardy P, Davey D, Wake M. Adverse associations of infant and child sleep problems and parent health: an Australian population study. Pediatrics. (2007) 119:947–55. doi: 10.1542/peds.2006-2569
5. Ahlqvist-Rastad J, Hultcrantz E, Melander H, Svanholm H. Body growth in relation to tonsillar enlargement and tonsillectomy. Int J Pediatr Otorhinolaryngol. (1992) 24:55–61. doi: 10.1016/0165-5876(92)90066-X
6. Schwengel DA, Dalesio NM, Stierer TL. Pediatric obstructive sleep apnea. Anesthesiol Clin. (2014) 32:237–61. doi: 10.1016/j.anclin.2013.10.012
7. Tan HL, Alonso Alvarez ML, Tsaoussoglou M, Weber S, Kaditis AG. When and why to treat the child who snores? Pediatr Pulmonol. (2017) 52:399–412. doi: 10.1002/ppul.23658
8. Esteller E, Villatoro JC, Agüero A, Lopez R, Matiñó E, Argemi J, et al. Obstructive sleep apnea syndrome and growth failure. Int J Pediatr Otorhinolaryngol. (2018) 108:214–8. doi: 10.1016/j.ijporl.2018.03.011
9. Bonuck K, Parikh S, Bassila M. Growth failure and sleep disordered breathing: a review of the literature. Int J Pediatr Otorhinolaryngol. (2006) 70:769–78. doi: 10.1016/j.ijporl.2005.11.012
10. Fernandes AA, Alcantara TA, D'Avila DV, D'Avila JS. Study of weight and height development in children after adenotonsillectomy. Braz J Otorhinolaryngol. (2008) 74:391–4. doi: 10.1016/S1808-8694(15)30573-5
11. Leiberman A, Stiller-Timor L, Tarasiuk A, Tal A. The effect of adenotonsillectomy on children suffering from obstructive sleep apnea syndrome (OSAS): the Negev perspective. Int J Pediatr Otorhinolaryngol. (2006) 70:1675–82. doi: 10.1016/j.ijporl.2006.06.002
12. Tatlipinar A, Atalay S, Esen E, Yilmaz G, Koksal S, Gokceer T. The effect of adenotonsillectomy on serum insulin like growth factors and the adenoid/nasopharynx ratio in pediatric patients: a blind, prospective clinical study. Int J Pediatr Otorhinolaryngol. (2012) 76:248–52. doi: 10.1016/j.ijporl.2011.11.014
13. Williams EF III, Woo P, Miller R, Kellman RM. The effects of adenotonsillectomy on growth in young children. Otolaryngol Head Neck Surg. (1991) 104:509–16. doi: 10.1177/019459989110400415
14. Marcus CL, Carroll JL, Koerner CB, Hamer A, Lutz J, Loughlin GM. Determinants of growth in children with the obstructive sleep apnea syndrome. J Pediatr. (1994) 125:556–62. doi: 10.1016/S0022-3476(94)70007-9
15. Freezer NJ, Bucens IK, Robertson CF. Obstructive sleep apnoea presenting as failure to thrive in infancy. J Paediatr Child Health. (1995) 31:172–5. doi: 10.1111/j.1440-1754.1995.tb00779.x
16. Conlon BJ, Donnelly MJ, McShane DP. Tonsillitis, tonsillectomy and weight disturbance. Int J Pediatr Otorhinolaryngol. (1997) 42:17–23. doi: 10.1016/S0165-5876(97)00105-5
17. Soultan Z, Wadowski S, Rao M, Kravath RE. Effect of treating obstructive sleep apnea by tonsillectomy and/or adenoidectomy on obesity in children. Arch Pediatr Adolesc Med. (1999) 153:33–7. doi: 10.1001/archpedi.153.1.33
18. Ersoy B, Yuceturk AV, Taneli F, Urk V, Uyanik BS. Changes in growth pattern, body composition and biochemical markers of growth after adenotonsillectomy in prepubertal children. Int J Pediatr Otorhinolaryngol. (2005) 69:1175–81. doi: 10.1016/j.ijporl.2005.02.020
19. Bar A, Tarasiuk A, Segev Y, Phillip M, Tal A. The effect of adenotonsillectomy on serum insulin-like growth factor-I and growth in children with obstructive sleep apnea syndrome. J Pediatr. (1999) 135:76–80. doi: 10.1016/S0022-3476(99)70331-8
20. Roemmich JN, Barkley JE, D'Andrea L, Nikova M, Rogol AD, Carskadon MA, et al. Increases in overweight after adenotonsillectomy in overweight children with obstructive sleep-disordered breathing are associated with decreases in motor activity and hyperactivity. Pediatrics. (2006) 117:e200–8. doi: 10.1542/peds.2005-1007
21. Wijga AH, Scholtens S, Wieringa MH, Kerkhof M, Gerritsen J, Brunekreef B, et al. Adenotonsillectomy and the development of overweight. Pediatrics. (2009) 123:1095–101. doi: 10.1542/peds.2008-1502
22. Katz ES, Moore RH, Rosen CL, Mitchell RB, Amin R, Arens R, et al. Growth after adenotonsillectomy for obstructive sleep apnea: an RCT. Pediatrics. (2014) 134:282–9. doi: 10.1542/peds.2014-0591
23. Tahara S, Hara H, Yamashita H. Evaluation of body growth in prepubertal Japanese children with obstructive sleep apnea after adenotonsillectomy over a long postoperative period. Int J Pediatr Otorhinolaryngol. (2015) 79:1806–9. doi: 10.1016/j.ijporl.2015.08.005
24. Selimoglu E, Selimoglu MA, Orbak Z. Does adenotonsillectomy improve growth in children with obstructive adenotonsillar hypertrophy? J Int Med Res. (2003) 31:84–7. doi: 10.1177/147323000303100204
25. Ministry of Health, Labour and Welfare in Japan. Charts of Standard Growth in Japanese Infants in 2000. (2002). Available online at: https://www.mhlw.go.jp/houdou/0110/h1024-4.html (accessed January 25, 2020).
26. Inokuchi M, Matsuo N, Anzo M, Hasegawa T. Body mass index reference values (mean and SD) for Japanese children. Acta Paediatr. (2007) 96:1674–6. doi: 10.1111/j.1651-2227.2007.00490.x
27. Munzer T, Hegglin A, Stannek T, Schoch OD, Korte K, Buche D, et al. Effects of long-term continuous positive airway pressure on body composition and IGF1. Eur J Endocrinol. (2010) 162:695–704. doi: 10.1530/EJE-09-0919
28. Nachalon Y, Lowenthal N, Greenberg-Dotan S, Goldbart AD. Inflammation and growth in young children with obstructive sleep apnea syndrome before and after adenotonsillectomy. Mediators Inflamm. (2014) 2014:146893. doi: 10.1155/2014/146893
29. Zhang XM, Shi J, Meng GZ, Chen HS, Zhang LN, Wang ZY, et al. The effect of obstructive sleep apnea syndrome on growth and development in nonobese children: a parallel study of twins. J Pediatr. (2015) 166:646–50.e641. doi: 10.1016/j.jpeds.2014.11.060
30. The Ministry of Education, Culture Sport Science and Technology in Japan. Survey on School Health Statistics. (2018). Available online at: https://www.mext.go.jp/b_menu/toukei/chousa05/hoken/1268826.htm (accessed January 25, 2020).
Keywords: body mass index, pediatrics, obstructive sleep apnea syndrome, adenotonsillectomy, growth improvement
Citation: Fukuda K, Yasudo H, Ohta N, Narumi H, Abe N, Tarumoto S, Yamashita H, Ichihara K, Ohga S and Hasegawa S (2020) Time-Course Evaluation of Body Mass Index in Japanese Children With Obstructive Sleep Apnea Syndrome After Adenotonsillectomy: A Three-Years Follow-Up Study. Front. Pediatr. 8:22. doi: 10.3389/fped.2020.00022
Received: 05 November 2019; Accepted: 16 January 2020;
Published: 04 February 2020.
Edited by:
Lokesh Guglani, Emory University, United StatesReviewed by:
Ajay Kasi, Emory University, United StatesCopyright © 2020 Fukuda, Yasudo, Ohta, Narumi, Abe, Tarumoto, Yamashita, Ichihara, Ohga and Hasegawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hiroki Yasudo, eWFzdWRvQHlhbWFndWNoaS11LmFjLmpw
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.