
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 10 January 2020
Sec. Pediatric Urology
Volume 7 - 2019 | https://doi.org/10.3389/fped.2019.00530
 Nader Shaikh1,2*
Nader Shaikh1,2* Vinod Rajakumar1
Vinod Rajakumar1 Caitlin G. Peterson3
Caitlin G. Peterson3 Jillian Gorski4
Jillian Gorski4 Anastasia Ivanova5
Anastasia Ivanova5 Lisa Gravens Muller5
Lisa Gravens Muller5 Yosuke Miyashita2
Yosuke Miyashita2 Kenneth J. Smith6
Kenneth J. Smith6 Tej Mattoo7
Tej Mattoo7 Hans G. Pohl8
Hans G. Pohl8 Ranjiv Mathews9
Ranjiv Mathews9 Saul P. Greenfield10
Saul P. Greenfield10 Steven G. Docimo1,2
Steven G. Docimo1,2 Alejandro Hoberman1,2
Alejandro Hoberman1,2Objective: Antimicrobial prophylaxis for children with vesicoureteral reflux (VUR) reduces recurrences of urinary tract infection (UTI) but requires daily antimicrobials for extended periods. We used a cost-utility model to evaluate whether the benefits of antimicrobial prophylaxis outweigh its risks and, if so, to investigate whether the benefits and risks vary according to grade of VUR.
Methods: We compared the cost per quality-adjusted life-year (QALY) gained in four treatment strategies in children aged <6 years diagnosed with VUR after a first UTI, considering these treatment strategies: (1) prophylaxis for all children with VUR, (2) prophylaxis for children with Grade III or Grade IV VUR, (3) prophylaxis for children with Grade IV VUR, and (4) no prophylaxis. Costs and effectiveness were estimated over the patient's lifetime. We used $100,000/QALY gained as the threshold for considering a treatment strategy cost effective.
Results: Based on current data and plausible ranges to account for data uncertainty, prophylaxis of children with Grades IV VUR costs $37,903 per QALY gained. Treating children with Grade III and IV VUR costs an additional $302,024 per QALY gained. Treating children with all grades of VUR costs an additional $339,740 per QALY gained.
Conclusions: Treating children with Grades I, II, and III VUR with long-term antimicrobial prophylaxis costs substantially more than interventions typically considered economically reasonable. Prophylaxis in children with Grade IV VUR is cost effective.
Although long-term antimicrobial prophylaxis for children with VUR has been shown to substantially reduce recurrences of UTI (from 27.4 to 14.8% during a 2-year follow-up period) (1), its use in children with VUR remains contentious. Proponents argue that, by preventing recurrent febrile UTIs, antimicrobial prophylaxis has the potential to reduce subsequent hypertension (HTN), preeclampsia, chronic kidney disease (CKD), and end-stage renal disease (ESRD). Opponents argue that the risk of prophylaxis outweighs its benefits, because, using the aforementioned data, only 27.4% of children with untreated VUR developed a reinfection during the 2-year follow-up period. Others argue that the benefits of treatment may differ in children according to the grade of VUR.
A cost-utility analysis is particularly well-suited to address this controversy, because both risks and benefits can be combined into a single metric, cost per quality-adjusted life year (QALY) gained and compared across treatment strategies.
We conducted a cost-utility analysis to evaluate whether the benefits of antimicrobial prophylaxis outweigh its risks in children with known VUR and, if not, for which subgroups of children could prophylaxis be considered cost-effective.
We compared clinical and economic outcomes of four treatment strategies in a hypothetical cohort of symptomatic children younger than 6 years of age diagnosed with VUR after a first UTI. Children were assigned to 1 of the following 4 strategies. These strategies include treating all children, leaving all children untreated, and treating only children with high-grade VUR. Some experts consider grades III and IV VUR as being high-grade, others consider only grade IV as high grade. As such we analyzed the data both ways (treat only children grade IV vs. treat both grade III and IV). Although other combinations are possible (e.g., treat grade I and IV), these are not logical because risk or reinfection, and thus renal scarring, increases steadily with increasing grade of VUR. Thus, in our modeling, we considered all logical combinations of VUR grade. Each strategy is described in more detail below. As recommended by the Panel on Cost-Effectiveness in Health and Medicine (2), we adopted a societal perspective and included both direct and indirect medical costs in our model. We constructed and analyzed our decision tree using TreeAge Pro software (TreeAge Software, Williamstown, Massachusetts).
Because long-term sequelae of VUR extend throughout life, we used a time horizon of 78 years, the current average US life expectancy at birth in the United States. We assumed that ESRD would start at age 17 (median age of ESRD in children with reflux nephropathy in the US) (3), and would continue for the patient's lifetime. We assumed that patients with ESRD would have a 7-year period with CKD (4). We also assumed that the life span of an individual with HTN would be 73 years (5).
Figure 1s shows the structure of the decision tree. Short term outcomes (outcomes within the first 4 years) included recurrences of UTI and surgery for VUR. Long term outcomes included HTN, preeclampsia, CKD, and ESRD. We chose a decision tree model (rather than a Markov model) because pertinent events occurred over a relatively short time frame (4 years) and these events during this period, albeit recurrent, could be compactly modeled in a decision tree structure. Once pertinent events occur, the remaining costs and QALYs were assigned based on the presence or absence of renal scarring (which had its onset within the relevant time frame).
Prophylaxis for all children with VUR—all children were started on antimicrobial prophylaxis and continued on prophylaxis for 2 years (in all strategies involving prophylaxis, we assumed that trimethoprim sulfamethoxazole at 2 mg/kg/day would be used for prophylaxis), at which time a VCUG was repeated. If VUR of any grade was still present on the follow-up VCUG, 2 more years of prophylaxis were prescribed, otherwise, children were observed for an additional 2 years without prophylaxis.
Prophylaxis for children with Grade III or Grade IV VUR—only children with grades III or IV VUR were started on antimicrobial prophylaxis. These children received prophylaxis for 2 years at which time a VCUG was repeated (a repeat VCUG was not performed on children with Grade I or II VUR). If grades III or IV VUR was still present on the follow-up VCUG, 2 more years of prophylaxis were prescribed; children with no VUR or grades I, or II VUR at the time of follow-up VCUG were observed for an additional 2 years without prophylaxis.
Prophylaxis for children with Grade IV VUR—only children with grades IV VUR were started on antimicrobial prophylaxis. These children received prophylaxis for 2 years at which time a VCUG was repeated (a repeat VCUG was not performed on children with grade I or II or III VUR). If grade IV VUR was still present on the follow-up VCUG, 2 more years of prophylaxis were prescribed; children with no VUR or grades I, or II or III VUR at the time of follow-up VCUG were observed for an additional 2 years without prophylaxis.
No prophylaxis—all children were observed without antimicrobial prophylaxis for 4 years. No follow-up VCUGs were performed.
Regardless of the initial strategy, children with 2 febrile reinfections who were not on prophylactic antibiotics were started on prophylactic antibiotics. Ureteral reimplantation during the follow-up period was at the discretion of the treating urologist. For the latter, we used individual patient data from the Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) trial (Table 1s).
The primary short-term outcome of interest was the development of renal scars during the first 4 years after diagnosis of VUR. The likelihood of renal scarring was estimated from the number of febrile UTIs observed during this period (6). We chose this strategy because the RIVUR trial was not powered to detect small differences in rates of renal scarring. We chose a 4-year time period because significant VUR would have resolved or would have been repaired for most children. Accordingly, after year 4, we assumed that rates of recurrent UTI would be equivalent across all strategies. The number of febrile UTIs in each strategy was obtained from individual-patient data from the RIVUR study, which compared the efficacy of trimethoprim-sulfamethoxazole prophylaxis to placebo in preventing recurrent UTIs (1). That study was well-suited for the present purpose because it included a placebo arm, and short-term outcomes were carefully monitored during the 2-year follow-up period. To allow us to focus this paper on children with a first UTI, in whom antimicrobial treatment remains controversial, children with a history of previous UTIs before enrollment into the RIVUR study were excluded. Because the incidence of UTI decreased by 50% from year 1 to 2 in the RIVUR study, we estimated that in years 3 and 4 we would observe half as many UTIs as we observed in year 2 of the RIVUR study.
The primary long-term outcomes of interest were HTN, preeclampsia, CKD, and ESRD. We used the estimated rate of renal scarring in the first 4 years in each strategy (which was largely determined using individual patient data) to estimate the probability of long-term outcomes. For the latter we used data from published studies that reported incidences of these outcomes in children with renal scarring; children without renal scarring were assumed not to have long-term sequelae attributable to UTIs. All children with ESRD were assumed to have had CKD for an average of 7.4 years before the need for dialysis (7).
Values used in the model for costs and quality-of-life utilities associated with individual clinical states are summarized in Table 1.
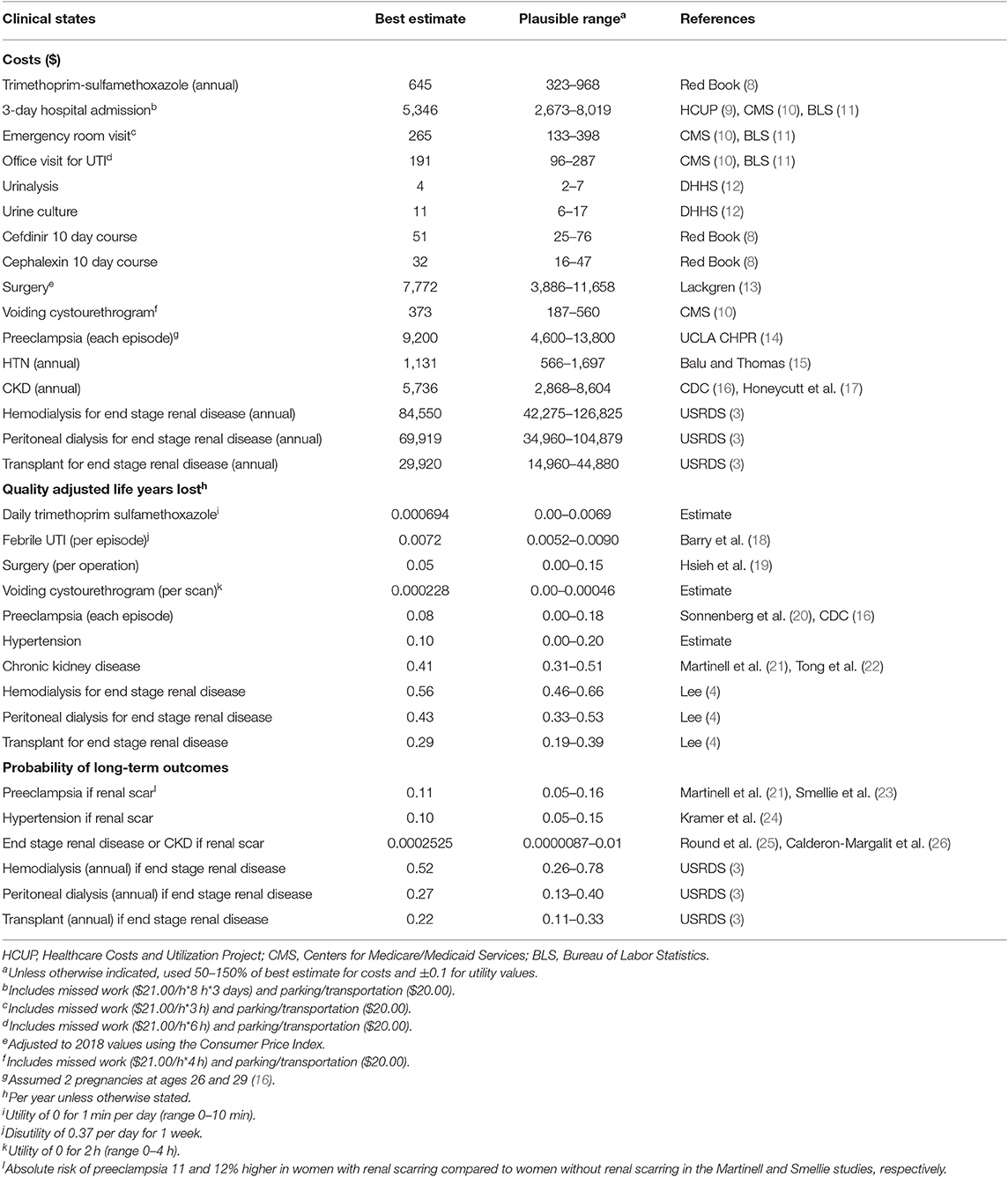
Table 1. Costs (before discounting), quality adjusted years lost (before discounting), and probabilities associated with specific clinical states, as used in the decision model.
Healthcare costs included costs of visits, medications, and laboratory tests. Accordingly, for each recurrent UTI, we included costs of the physician visit, antibiotics (cefdinir for 10 days in children on prophylaxis and cephalexin for 10 days for children not on prophylaxis), urine culture, and urinalysis.
Because HTN, preeclampsia, CKD, and ESRD occur years after the index UTI, future costs associated with these states were discounted at a rate of 3% per year, in accordance with US recommendations (2).
For each visit, we included non-medical costs. These included cost of work lost by parents, cost of childcare if needed, and cost of parking. We estimated the cost of work lost by multiplying estimated hours of work missed (27) by average wage as reported by the U.S. Bureau of Labor Statistics (11).
Utility reflects the health-related quality of life of an individual at a particular point in time. Utility values are scaled from 0 to 1, where 0 denotes death and 1 denotes perfect health. Disutility values are one minus the utility values. For each undesirable state, we determined the QALYs lost by multiplying the time spent in that state by its associated disutility value. Similar to costs, we discounted QALYs at a rate of 3% annually. Of note, because VUR is an asymptomatic condition, no disutility value was assigned to it in our models. Rather, to arrive at the disutility values in each strategy, we relied on the number of symptomatic events each child with VUR experienced (e.g., UTIs, VCUGs).
For the main analysis, we assumed, as per current standard practice (28), that management after the initial 2-year period, would be largely driven by the grade of VUR at the time of repeat VCUG. Recently, some have proposed that, rather than using VUR grade, occurrence of febrile UTI after diagnosis of VUR (29), should guide subsequent management (i.e., no repeat VCUG performed if no breakthrough UTIs). Accordingly, to test the robustness of our model, we constructed a model in which, after 2 years of the initial treatment strategy, antimicrobial prophylaxis was continued for another 2 years only in children receiving antimicrobial prophylaxis who had at least 1 febrile recurrence in the first 2 years after diagnosis.
We compared strategies using their incremental cost-utility ratios (ICERs), defined as the extra cost of a more expensive strategy compared to the cost of the nearest less expensive strategy, divided by the added QALYs conferred by the more expensive strategy. We used a $100,000 per QALY gained, a commonly cited US benchmark (30), as our cost-effectiveness willingness-to-pay threshold. We conducted one-way sensitivity analyses for variables by varying baseline estimates within clinically plausible ranges. Whenever individual patient data were available, we based ranges on 95% confidence intervals calculated using the Clopper-Pearson formula. We also conducted probabilistic sensitivity analyses in which we varied all parameters simultaneously over distributions, using beta distributions for probabilities and utilities and gamma distributions for costs, with distributions fitted to approximate ranges in Table 1. In these analyses, values from each probability distribution are randomly selected during each of 10,000 iterations, and the percentage of iterations for which a given strategy was favored was tracked.
Table 2 shows cost-effectiveness analysis results for each of the four treatment options. The total cost of each treatment strategy, listed in order from most to least costly, was as follows: prophylaxis for all children, prophylaxis for children with Grade III or IV VUR, prophylaxis for children with Grade IV VUR, and no prophylaxis for any child. The high cost of non-cost-effective strategies was mainly driven by the higher proportion of children requiring prophylaxis in these strategies (Table 2).
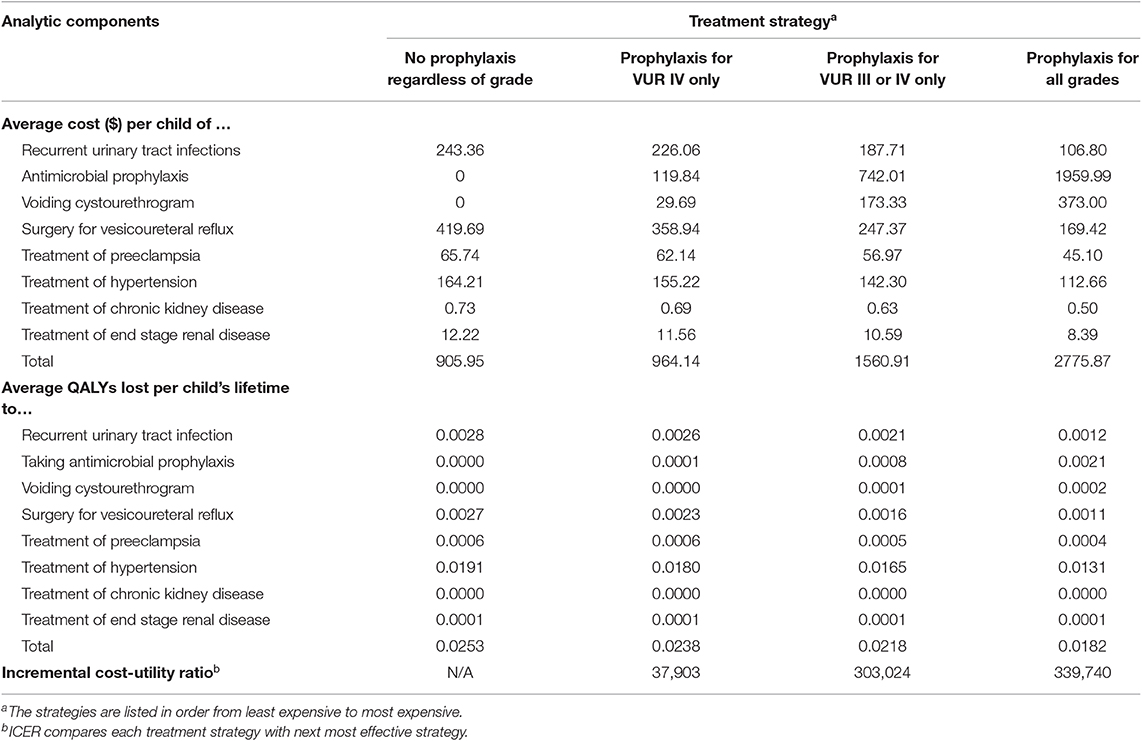
Table 2. Comparative cost-utility of 4 treatment strategies for treatment of vesicoureteral reflux in children <6 years of age.
The effectiveness of each strategy, listed from most effective to least effective, was as follows: prophylaxis for all children with VUR, prophylaxis for children with Grade III or IV VUR, prophylaxis for children with Grade IV VUR, and no prophylaxis for any child. The low effectiveness of no prophylaxis was largely driven by the higher rates of surgery relative to the other strategies (Table 2). No prophylaxis for any child was the least costly and also the least effective treatment strategy. Prophylaxis for all Grades of VUR was the most costly and most effective treatment strategy. Prophylaxis only for children with Grade IV VUR compared to not using prophylaxis on any child cost $37,903 per QALY gained (Table 2), while prescribing prophylaxis for Grades III and IV compared with prescribing prophylaxis only for children with Grade IV VUR cost an additional $302,024 per QALY gained. Results of the probabilistic sensitivity analysis were consistent with the base case analysis, showing that prophylaxis of Grade IV VUR was the strategy most likely to be favored if willingness-to-pay thresholds are $40,000/QALY gained or more, with no prophylaxis favored at lower thresholds and other strategies unlikely to be favored at any threshold considered (Figure 2s).
Table 3 shows the number of children with HTN, preeclampsia, and ESRD in each treatment strategy for 1,000,000 children entered into the model. In more effective strategies, fewer children developed long term sequelae; for example, all prophylaxis (the most effective strategy) had the lowest number of cases of HTN, preeclampsia, and ESRD.
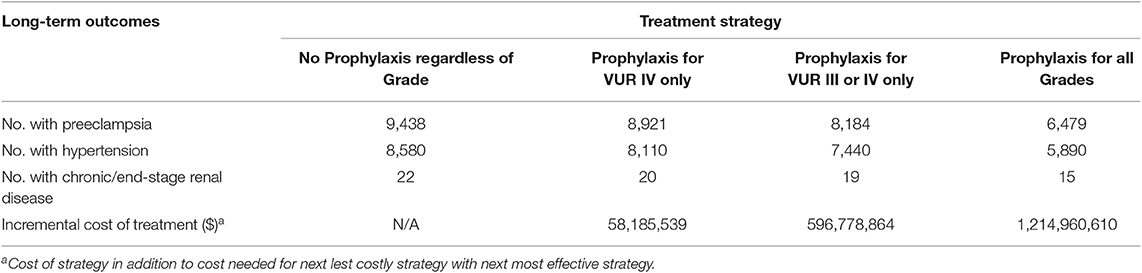
Table 3. Number of children with each long-term sequela according to treatment strategy in a population of 1,000,000 children with known vesicoureteral reflux.
We conducted one-way sensitivity analyses to identify variables that would change the preferred strategy, using the $100,000/QALY gained criterion, from prophylaxis for only children with VUR IV to any of the other strategies. Only one parameter did so (disutility of prophylaxis, Table 2s). In no case did strategies that included treatment of children with lower grades of VUR become preferred.
Results were similar when using the alternate treatment strategy mentioned above: treatment of grade IV VUR was the most cost-effective strategy and its ICER was ($43,798/QALY gained) similar to what we found in our initially considered strategy.
We sought to determine whether immediate antimicrobial therapy, given its benefits, adverse effects, and costs, is cost-effective in children younger than 6 years of age with VUR and, if so, for which subgroup of children antimicrobial therapy is most cost-effective.
Of the four strategies we considered, we found that prophylaxis for only Grade IV VUR was the most cost-effective with an ICER of $37,903 per QALY gained compared to the “no prophylaxis” strategy, which is < $100,000 per QALY gained that is generally considered cost-effective (30). Of note, our main findings would have been the same even if we had chosen another frequently used threshold (i.e., $50,000 or $200,000) (31–33). The results of sensitivity analyses indicated that the findings were robust; only one variable (disutility of taking daily prophylactic medications) flipped the preferred strategy (from “prophylaxis for Grade IV VUR” to “no prophylaxis”). In contrast, the two strategies which involved treatment of children with low-grade VUR (prophylaxis for all children with VUR, or prophylaxis for children with Grades III or IV VUR) never approached the cost-effectiveness threshold in sensitivity analyses. Our results suggest that use of long-term antimicrobial prophylaxis for children with Grades I–III VUR is unlikely to be considered economically reasonable given the data used and the assumptions made. Reduction of antibiotic use for children with VUR, most of whom have low-grade VUR, constitutes an important contribution to public health.
A strength of our study was our use of individual patient data to obtain values for most parameters. Our study had several limitations. We did not consider children with Grade V VUR because such children were not included in the RIVUR study. Nor did we consider the potential impact of antimicrobial-induced bacterial resistance; however, considering it would likely further strengthen our conclusion that treating children with low-grade VUR is not cost-effective. Because most of our data came from the RIVUR study, the conclusions are only readily applicable to patients in the United States. Furthermore, we chose to use the definitions of “treatment failure” used in the RIVUR study (no change in treatment strategy unless two febrile reinfections). There are countless other ways of defining “treatment failure” in current practice; however, modeling these strategies would require making assumptions regarding the number of reinfections occurring in each of these hypothetical scenarios. In order to limit the number of assumptions made, we used the definition that the RIVUR study investigators agreed upon at the time as a clinically reasonable strategy for managing children with VUR. Accordingly, our results need to be interpreted in this context. To check the robustness of our analysis we chose to examine the results if we had chosen an alternate (and very different) strategy for the management of children after the initial 2-year period; that the results were largely similar is reassuring.
As with any modeling study, conclusions are limited by the available data. Long-term risks of HTN and ESRD failure resulting from UTI-related renal scarring are highly uncertain. However, in sensitivity analyses, we found that variation of ESRD risk within the reported range did not affect strategy favorability, while lower HTN risk could shift favorability to the no prophylaxis strategy; the analysis was insensitive to higher levels of hypertension risk from scarring. From among a long list of possible variables, we chose to stratify our analyses based on grade of VUR. We did so because VUR is a known risk factor for renal scarring and because it was available for all children included. Furthermore, the relationship between grade of VUR, febrile reinfections, and renal scarring had not been explored in detail in previous manuscripts on the RIVUR study. Although presence of bowel and bladder dysfunction in toilet trained children has also been linked to higher rates of UTI recurrence, most of the children included were not toilet trained: BBD could only be assessed in a minority (18%) of the included children. Accordingly, we did not feel that the available data lent itself readily to a detailed exploration of the role of BBD. Similarly, the proportion of males in RIVUR was very small (9% of the sample were males). Thus, neither sex nor circumcision status could be meaningfully explored using available data. It is important to note that our choice of stratification variable does not mean that the effect of other variables is being ignored in the analyses. On the contrary, because we used individual patient data, the rates of renal scarring within each stratum continues to reflect all the other known and unknown risk factors of recurrent UTIs and renal scarring. We did not assess the cost-effectiveness of endoscopic treatment because the RIVUR trial did not evaluate this intervention and thus no individual patient data were available. Because we used individual patient data from the RIVUR trial the conclusions are most applicable to the types of children enrolled in the RIVUR trial. However, because patients in RIVUR were enrolled from 19 sites and from both primary care and subspecialty clinics, the included data is likely a reasonable representation of the general population with VUR.
In summary, for children <6 years of age with VUR, use of long-term antimicrobial prophylaxis for children with low-grade VUR does not appear to be cost-effective.
The datasets generated for this study can be found in https://repository.niddk.nih.gov/studies/rivur/?query=RIVUR; https://repository.niddk.nih.gov/studies/cutie/?query=CUTIE.
The studies involving human participants were reviewed and approved by the participating IRBs (University of Pittsburgh IRB, University of Pennsylvania IRB, University of Buffalo IRB, Children's National Human Research Protection Program/IRB, Wayne State University IRB). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
NS conceptualized and designed the study, assisted with the analysis, drafted the initial manuscript, and approved the final manuscript as submitted. VR, JG, and CP carried out the analyses, reviewed, and revised the manuscript and approved the final manuscript as submitted. LG and AI performed statistical analyses that were used as inputs for the model and approved the final manuscript as submitted. KS helped to develop the decision tree and approved the final manuscript as submitted. RM assisted with data collection, interpretation of the findings, and approval of the final manuscript. HP, TM, SG, SD, YM, and AH assisted with the interpretation of the findings and approved the final manuscript. All authors contributed substantially to the content of the article, critically revised the article for important intellectual content, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work.
Treating children with Grades I, II, and III VUR with long-term antimicrobial prophylaxis costs substantially more than interventions typically considered economically reasonable. Prophylaxis in children with Grade IV VUR could be cost effective.
Long-term antimicrobial prophylaxis reduces the incidence of febrile urinary tract infections in children with vesicoureteral reflux (VUR). However, whether risks and costs of antimicrobial therapy outweigh its benefits has not been adequately studied.
Use of antimicrobial prophylaxis appears to be cost effective for children with Grade IV VUR but not for children lower grades of VUR (grades I–III).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2019.00530/full#supplementary-material
VUR, vesicoureteral reflux; QALY, quality-adjusted life-year; UTI, urinary tract infection; CKD, chronic kidney disease; ESRD, end-stage renal disease; ICER, incremental cost-utility ratio.
1. Hoberman A, Greenfield SP, Mattoo TK, Keren R, Mathews R, Pohl HG, et al. Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med. (2014) 370:2367–76. doi: 10.1056/NEJMoa1401811
2. Sanders GD, Neumann PJ, Basu A, Brock DW, Feeny D, Krahn M, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. (2016) 316:1093–103. doi: 10.1001/jama.2016.12195
3. United States Renal Data System. Medicare Expenditures for Persons With ESRD. (2015). Available online at: https://www.usrds.org/2015/view/v2_11.aspx (accessed October 04, 2017).
4. Lee AJ, Morgan CL, Conway P, Currie CJ. Characterisation and comparison of health-related quality of life for patients with renal failure. Curr Med Res Opin. (2005) 21:1777–83. doi: 10.1185/030079905X65277
5. Franco OH, de Laet C, Peeters A, Jonker J, Mackenbach J, Nusselder W. Effects of physical activity on life expectancy with cardiovascular disease. Arch Intern Med. (2005) 165:2355–60. doi: 10.1001/archinte.165.20.2355
6. Shaikh N, Haralam M, Kurs-Lasky M, Hoberman A. Association of renal scarring with number of febrile urinary tract infections in children. JAMA Pediatr. (2019) 173:949–52. doi: 10.1001/jamapediatrics.2019.2504
7. Staples AO, Greenbaum LA, Smith JM, Gipson DS, Filler G, Warady BA, et al. Association between clinical risk factors and progression of chronic kidney disease in children. Clin J Am Soc Nephrol. (2010) 5:2172–9. doi: 10.2215/CJN.07851109
8. Red Book: Pharmacy's Fundamental Reference. 114th ed. Armonk, NY: PDR Network (2015). Available online at: https://www.ibm.com/us-en/marketplace/micromedex-red-book
9. Healthcare Cost & Utilization Project (HCUP). Agency for Healthcare Research and Quality. Available online at: https://hcupnet.ahrq.gov/#setup (accessed October 04, 2017).
10. Centers for Medicare and Medicaid Services. (2016). Available online at: https://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx (accessed October 04, 2017).
11. Beureau of Labor and Statistics. Total Private Average Hourly Earnings of Prod. and Nonsup. Employees - Seasonally Adjusted. (2015). Available online at: http://data.bls.gov/cgi-bin/surveymost?bls (accessed November 14, 2015).
12. Department of Health and Human Services. Comparing Lab test Payment Rates. (2013). Available online at: https://oig.hhs.gov/oei/reports/oei-07-11–00010.pdf (accessed October 04, 2017).
13. Lackgren G. Endoscopic treatment of vesicoureteral reflux: current status. Indian J Urol. (2009) 25:34–9. doi: 10.4103/0970-1591.45534
14. UCLA Center for Health Research Policy. Costs of Gestational Hypertensive Disorders in California: Hypertension, Preeclampsia, and Eclampsia. (2013). Available online at: http://healthpolicy.ucla.edu/publications/Documents/PDF/gestationaldisordersreport-oct2013.pdf (accessed October 04, 2017).
15. Balu S, Thomas J III. Incremental expenditure of treating hypertension in the United States. Am J Hypertens. (2006) 19:810–6; discussion 817. doi: 10.1016/j.amjhyper.2005.12.013
16. Centers for Disease Control and Prevention. Births: Final Data for 2014. (2014). Available online at: https://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_12.pdf (accessed October 04, 2017).
17. Honeycutt AA, Segel JE, Zhuo X, Hoerger TJ, Imai K, Williams D. Medical costs of CKD in the medicare population. J Am Soc Nephrol. (2013) 24:1478–83. doi: 10.1681/ASN.2012040392
18. Barry HC, Ebell MH, Hickner J. Evaluation of suspected urinary tract infection in ambulatory women: a cost-utility analysis of office-based strategies. J Fam Pract. (1997) 44:49–60.
19. Hsieh MH, Swana HS, Baskin LS, Meng MV. Cost-utility analysis of treatment algorithms for moderate grade vesicoureteral reflux using Markov models. J Urol. (2007) 177:703–9; discussion 709. doi: 10.1016/j.juro.2006.10.002
20. Sonnenberg FA, Burkman RT, Hagerty CG, Speroff L, Speroff T. Costs and net health effects of contraceptive methods. Contraception. (2004) 69:447–59. doi: 10.1016/j.contraception.2004.03.008
21. Martinell J, Jodal U, Lidin-Janson G. Pregnancies in women with and without renal scarring after urinary infections in childhood. BMJ. (1990) 300:840–4. doi: 10.1136/bmj.300.6728.840
22. Tong A, Wong G, McTaggart S, Henning P, Mackie F, Carroll RP, et al. Quality of life of young adults and adolescents with chronic kidney disease. J Pediatr. (2013) 163:1179–85.e5. doi: 10.1016/j.jpeds.2013.04.066
23. Smellie JM, Prescod NP, Shaw PJ, Risdon RA, Bryant TN. Childhood reflux and urinary infection: a follow-up of 10-41 years in 226 adults. Pediatr Nephrol. (1998) 12:727–36. doi: 10.1007/s004670050535
24. Kramer MS, Tange SM, Drummond KN, Mills EL. Urine testing in young febrile children: a risk-benefit analysis. J Pediatr. (1994) 125:6–13. doi: 10.1016/S0022-3476(94)70114-8
25. Round J, Fitzgerald AC, Hulme C, Lakhanpaul M, Tullus K. Urinary tract infections in children and the risk of ESRF. Acta Paediatr. (2012) 101:278–82. doi: 10.1111/j.1651-2227.2011.02542.x
26. Calderon-Margalit R, Golan E, Twig G, Leiba A, Tzur D, Afek A, et al. History of childhood kidney disease and risk of adult end-stage renal disease. N Engl J Med. (2018) 378:428–38. doi: 10.1056/NEJMoa1700993
27. Smith KJ, Cook RL, Ness RB. Cost comparisons between home- and clinic-based testing for sexually transmitted diseases in high-risk young women. Infect Dis Obstet Gynecol. (2007) 2007:62467. doi: 10.1155/2007/62467
28. Mattoo T, Greenfield S. Management of Vesicoureteral Reflux. UpToDate Web site. (2018) (accessed October 01, 2018).
29. Bandari J, Docimo SG. Vesicoureteral reflux is a phenotype, not a disease: a population-centered approach to pediatric urinary tract infection. J Pediatr Urol. (2017) 13:378–82. doi: 10.1016/j.jpurol.2017.03.037
30. Laupacis A, Feeny D, Detsky AS, Tugwell PX. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. (1992) 146:473–81.
31. Braithwaite RS, Meltzer DO, King JT Jr, Leslie D, Roberts MS. What does the value of modern medicine say about the $50,000 per quality-adjusted life-year decision rule? Med Care. (2008) 46:349–56. doi: 10.1097/MLR.0b013e31815c31a7
32. Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness–the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. (2014) 371:796–7. doi: 10.1056/NEJMp1405158
Keywords: cost-effectiveness, cost utility, urinary tract infection (UTI), pediatric, pediatric infectious disease
Citation: Shaikh N, Rajakumar V, Peterson CG, Gorski J, Ivanova A, Gravens Muller L, Miyashita Y, Smith KJ, Mattoo T, Pohl HG, Mathews R, Greenfield SP, Docimo SG and Hoberman A (2020) Cost-Utility of Antimicrobial Prophylaxis for Treatment of Children With Vesicoureteral Reflux. Front. Pediatr. 7:530. doi: 10.3389/fped.2019.00530
Received: 28 July 2019; Accepted: 05 December 2019;
Published: 10 January 2020.
Edited by:
Raimund Stein, University Medical Center Mannheim, GermanyReviewed by:
Berk Burgu, Ankara University, TurkeyCopyright © 2020 Shaikh, Rajakumar, Peterson, Gorski, Ivanova, Gravens Muller, Miyashita, Smith, Mattoo, Pohl, Mathews, Greenfield, Docimo and Hoberman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nader Shaikh, bmFkZXIuc2hhaWtoQGNocC5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.