
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 31 July 2019
Sec. Pediatric Cardiology
Volume 7 - 2019 | https://doi.org/10.3389/fped.2019.00308
Background: The aim of this study was to investigate the prognostic role of the neutrophil to lymphocyte ratio (NLR) in pediatric patients undergoing open-heart surgery with cardiopulmonary bypass (CPB).
Methods: A retrospective cohort study of 61 pediatric patients who underwent CPB in the First Affiliated Hospital of Nanjing Medical University from January 2017 to October 2018 was conducted. All perioperative clinical data, including neutrophil count, lymphocyte count, and C-reactive protein (CRP), were collected retrospectively. The prognostic value of NLR and its association with extubation time, duration of intensive care unit (ICU) stay and in-hospital stay were analyzed.
Results: Neutrophil count, NLR, and CRP were significantly increased post-operative compared with pre-operative (p < 0.05). The increased post-operative levels of NLR were significantly associated with longer extubation time, as well as prolonged post-operative cardiac ICU stay (p < 0.05). Multivariate linear regression analysis revealed that elevated NLR displayed a significant independent association with extubation time and the duration of an ICU stay.
Conclusion: Increased post-operative NLR followed by cardiac surgery with CPB in pediatric patients was associated with longer extubation time and a longer duration of an ICU stay.
Previous studies have demonstrated that a systemic inflammatory response is activated in patients undergoing cardiothoracic surgery with cardiopulmonary bypass (CBP) (1, 2). Multiple studies have demonstrated a relationship between altered production of inflammatory mediators and clinical outcome in pediatric patients after CPB (3, 4). However, few inflammatory biomarkers have been used for outcome evaluation in the clinical practice. Therefore, the identification and quantification of clinical factors in the early post-operative period could be predictive of increased risk of post-operative morbidity and poor outcomes is imperative.
Neutrophil activation can trigger systemic inflammation and has been recognized to play a pivotal role in the inflammatory response induced by CPB (5, 6). Moreover, the neutrophil to lymphocyte ratio (NLR) is a novel inflammatory marker which has been found to be associated with the severity and prognosis of many cardiovascular diseases (7). Importantly, increased perioperative NLR was shown to be associated with poor cardiac surgery patient outcomes in adult patients (8, 9). Despite this, NLR has not been well-studied in exclusively pediatric patients undergoing cardiac surgery requiring CPB. Therefore, the objective of the present study is to examine the association between NLR levels and clinical outcomes in pediatric patients undergoing cardiac surgery with CPB.
This is a retrospective observational study. From January 2017 to October 2018, a total of 61 pediatric patients undergoing cardiac surgery requiring CPB were included. This study was approved by the hospital's institutional review board (IRB). Since no intervention was performed and no personally identifiable information was used in the study, our local IRB waived the requirement for informed consent. The inclusion criteria of this study were: patients were to be aged between 3 and 72 months and underwent pediatric cardiac surgery requiring CPB. Exclusion criteria for this study included a birth weight of <2.3 kg, associated extracardiac abnormalities, and a history of cardiac surgery.
Anesthesia and management of CPB were performed using standard techniques depending on the age, weight, and hematocrit (HCT) level of the pediatric patients. Briefly, anesthesia was induced with 8% sevoflurane, followed by the placing of a peripheral venous catheter. After an intravenous injection of fentanyl (5 μg/kg), cisatracurium (0.15 mg/kg), propofol (3 mg/kg), and midazolam (0.05 mg/kg), endotracheal intubation was performed. Pressure-controlled ventilation was performed, and the frequency of respiration was adjusted based on the patient's age as well as partial pressure of arterial carbon dioxide. Propofol (8 mg/kg/h), cisatracurium (2 μg/kg/min), and sevoflurane (1–3%) were used for the maintenance of anesthesia. Fentanyl (20–30 μg/kg) and midazolam (0.1 mg/kg) were added for the maintenance of anesthesia. All subjects received methylprednisolone (30 mg/kg) and cefazolin sodium (50 mg/kg) before skin incision. None received intraoperative steroids.
The CPB circuit was primed with acetated Ringer's solution, red blood cells (RBCs), plasma, 20% mannitol, 5% sodium bicarbonate, and heparin. HCT was maintained at 24–28% during CPB. Heparin was given at a dose of 3 mg/kg to achieve a target activated clotting time of 480 s. After the initiation of CPB, moderate hypothermia was started with a target rectal temperature of 28 to 32°C. The pump flow rates ranged from 2 to 3 L/min/m2. The mean arterial blood pressure during CPB was maintained between 35 and 60 mmHg according to the patient's age. Dopamine (5 μg/kg/min) and milrinone (0.5 μg/kg/min) were routinely used to facilitate weaning off from CPB. Ultrafiltration was used during and/or after termination of CPB. Platelets and cryoprecipitate were regularly used after CPB. RBCs and fresh frozen plasma were given at the anesthesiologist's discretion. The reversal of heparin after termination of bypass was achieved with the administration of protamine (3 mg/kg).
All data was collected retrospectively in November 2018. Pre-operative and post-operative levels (first post-operative day) of neutrophils, lymphocytes, and CRP were obtained through the electronic database of the hospital. NLR was calculated on the basis of data. Clinical patient data were collected through medical and nursing patient record review.
Categorical and numerical data are expressed as n and mean ± SD, respectively. Post-operative neutrophil counts, NLR and CRP were compared with pre-operative counts by using the paired t-test. Spearman rank correlation coefficients were used to assess the association between neutrophil counts, NLR, and CRP and continuous clinical outcomes. Multivariable linear regression was used to further examine the relationship between post-operative neutrophil counts, NLR, and CRP and clinical outcome variables, including extubation time, the duration of an ICU stay, and length of hospital stay. The significance level was defined as a p < 0.05. All statistical analyses were performed using the statistical software SPSS 21.0 (SPSS Inc., Chicago, IL).
During study period (January 2017 to October 2018), 61 children (n = 39 male, n = 22 female) were included in the final analysis. Diagnoses of 61 patients included congenital heart defect ventricular septal defect (n = 28), atrial septal defect (n = 2), ventricular septal defect with atrial septal defect (n = 7), tetralogy of Fallot (n = 5), tetralogy of Fallot with atrial septal defect (n = 4), complete endocardial cushion defect (n = 3), pulmonary atresia (n = 4), and complex congenital heart disease (n = 9).
The median age was 20.4 ± 19.2 months (ranging from 3 to 69.5 months). The mean duration of ICU and in-hospital stay were 1.705 ± 0.955 days (ranging from 1 to 5 days) and 10.393±2.795 days (ranging from 7 to 17 days), respectively. The mean time of extubation was 16.346 ± 19.539 h (ranging from 1.2 to 92.8 h). A detailed table of the subjects' baseline and operative characteristics in comparison with the entire cohort is presented in Table 1.
The data showed that post-operative neutrophil counts, as well as CRP and NLR levels were significantly higher compared to their respective pre-operative levels in pediatric patients requiring CPB (Figure 1, p < 0.05). Using a univariate analysis of clinical outcomes (Table 2), it was revealed that the post-operative NLR was significantly associated with the duration of surgery, extubation time, and length of ICU stay (p < 0.05). However, both pre-operative and post-operative neutrophil levels were significantly associated with length of ICU stay and extubation time (p < 0.05). In addition, the post-operative CRP levels were associated with CPB duration, circulatory arrest duration and length of ICU stay (p < 0.05).
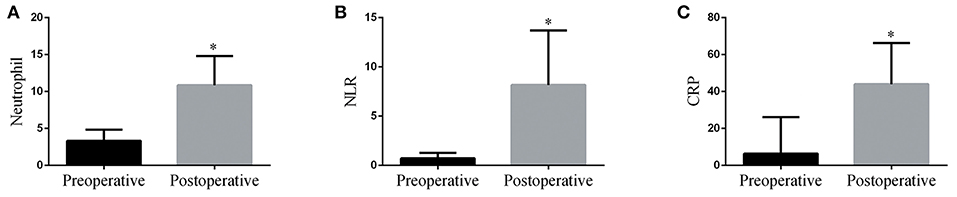
Figure 1. Post-operative neutrophil counts (A), NLR (B), and CRP (C) levels were significantly increased compared with their respective pre-operative values in pediatric patients following CPB. *p < 0.05 vs. pre-operative.
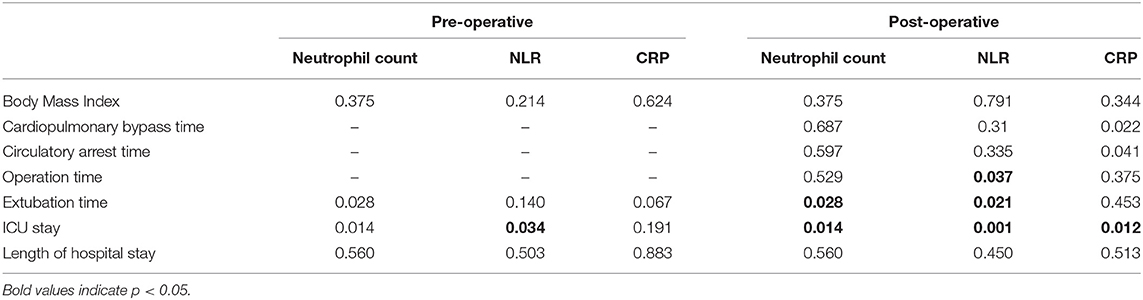
Table 2. Spearman rank correlation coefficients of neutrophil count, NLR, and CRP levels measured before and after operation with clinical outcome.
We then set out to determine whether post-operative NLR maintained an independent association with extubation time, duration of ICU stay, and length of hospital stay when controlling for key operative factors, as well as post-operative neutrophil counts and CRP levels. Multivariable modeling results showed that post-operative NLR demonstrated an independent association with extubation time and length of ICU stay (Table 3, p < 0.05).
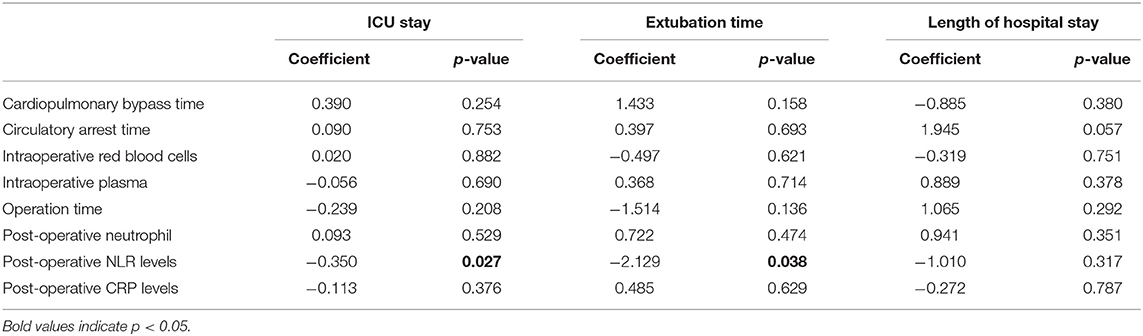
Table 3. Multivariate analysis for duration of ICU stay, extubation time and length of hospital stay.
The main findings of this study were that CRP, NLR, and neutrophil counts were significantly increased post-operatively compared with pre-operatively. In addition, the post-operative neutrophil counts and NLR on the first post-operative day after surgery were significantly correlated with extubation time and duration of ICU stay. However, the post-operative CRP was only associated with ICU stay. After adjustment for key operative factors, post-operative neutrophil counts, and CRP levels, the elevated NLR on the first post-operative day was independently associated with extubation time and length of ICU stay. Our data suggests that the NLR could be an adjunct indicator for post-operative outcome in pediatric patients who had undergone CPB.
Previous research has demonstrated that CPB-induced systemic inflammatory response is a major cause of mortality (10, 11). Neutrophils are the common type of leukocytes, and arrive rapidly to sites of acute inflammation, where they are responsible for phagocytosis and killing of invading pathogens (12). Neutrophil activation is known to trigger systemic inflammation and has been demonstrated to play a pivotal role in the inflammatory response induced by CPB (6, 13, 14). CPB triggers the activation of neutrophils in the complement cascade, inducing the secretion of polymorphonuclear elastase (PMN-E). Overactivation of PMN-E on one hand can directly induce cell injury and, on the other hand, indirectly enhances the inflammatory response by promoting the synthesis and release of IL-8 through the IL-1 signaling (15). Previous research has demonstrated a positive correlation between plasma concentrations of IL-8 at the end of CPB with duration of CPB and circulatory arrest, as well as with aortic cross-clamp time, and a negative correlation with lowest temperature on CPB (3). The pre-treatment with the neutrophil elastase inhibitor sivelestat could suppress the perioperative inflammatory response following pediatric cardiac surgery with CPB (15, 16). Our current data demonstrate that a significant increase of neutrophil levels is associated with increased post-operative extubation time and increased length of ICU stay. Taken together with findings from previous research studies, our results demonstrate the need for targeted anti-inflammatory therapy in the pediatric population, with a specific focus on the neutrophil cells.
In adult patients, an augmentation in perioperative NLR was shown to be associated with increased mortality and morbidity in patients undergoing cardiac surgery (8). In comparison with adult patients, the inflammatory response is increased in pediatric patients undergoing CPB (1). Many potential prognostic and predictive molecular inflammatory biomarkers have now been identified in the evaluation of poor outcomes following CPB; however, none have yet entered into clinical practice. Accumulating evidence demonstrated that NLR could reflect a systemic inflammatory response (17, 18); however, there is only one study evaluating the prognosis associations of NLR in pediatric patients with CPB (19). According to the results of the study, the NLR measured before extubation displayed significantly more variation in pediatric patients with failed extubation; less variation in NLR was found in children in whom extubation was successful (20). In addition, pre-extubation NLR was indicative of successful extubation (20). In the current study, we also found that post-operative NLR was significantly increased in pediatric patients compared to pre-operative NLR. In addition, there was a significant and positive correlation between the duration of ventilation and serum NLR in pediatric patients after cardiac surgery with CPB. Lastly, our data showed that post-operative NLR was also associated with a longer duration of post-operative ICU stay. These findings suggest that monitoring of the NLR has the potential to make predictions about probable outcomes in pediatric patients undergoing cardiac surgery with CPB.
C-reactive protein (CRP) is an acute-phase pentameric protein secreted in response to inflammation (20). Previous data showed that serum CRP levels significantly increased after CPB compared with pre-operative levels (21). The current data presents both NLR and CRP levels in the same pediatric patients requiring CPB. Despite significantly increased post-operative CRP levels compared with pre-operative levels, there was no significant association between post-operative CRP levels, extubation time, and length of ICU stay after adjusting for post-operative neutrophil counts, NLR, and key operative factors. These results suggest that NLR would be more effective than CRP to monitor patients with delayed tracheal extubation and predict length of ICU stay in pediatric patients requiring CPB.
The present study has some limitations. Firstly, the study was conducted in only one hospital. Therefore, a multicenter study needs to be carried out in order to further contribute to our findings. Secondly, due to the retrospective design of our study, it is potentially susceptible to systematic error and bias. However, the numerical data used in our study were collected prospectively and analyzed independently. Thirdly, our data examination was limited to the period which ended upon patients' discharge from the hospital, and further research is needed to examine the long-term impact of NLR on patient outcomes. Finally, the current study examined a fairly wide age group which covers a diverse group of underlying congenital heart defects, and future research will further develop and confirm these initial findings by narrowing the age range for each type of heart disease.
In conclusion, elevated post-operative NLR was associated with increased extubation time and an increased length of ICU stay for pediatric patients after CPB surgery. As NLR can be easily calculated using the complete blood count, it can potentially provide a simple and cost-effective test in the management of pediatric cardiac surgery patients.
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
This study was approved by the institutional review board (IRB) of The First Affiliated Hospital With Nanjing Medical University. Since no personally identifiable information was used in the study, our local IRB waived the requirement for informed consent.
HX and SZ designed the study, interpreted results, and wrote the manuscript. YS collected data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors gratefully acknowledge the cardiac surgeons, anesthesiologists, and nurses at the Department of Cardiothoracic Surgery, the First Affiliated Hospital of Nanjing Medical University for their help with this study.
1. Boehne M, Sasse M, Karch A, Dziuba F, Horke A, Kaussen T, et al. Systemic inflammatory response syndrome after pediatric congenital heart surgery: incidence, risk factors, and clinical outcome. J cardiac surg. (2017) 32:116–25. doi: 10.1111/jocs.12879
2. Kim DS, Lee SI, Lee SB, Hyun MC, Cho JY, Lee YO. Outcome of inflammatory response after normothermia during cardiopulmonary bypass surgery in infants with isolated ventricular septal defect. Korean J pediatrics. (2014) 57:222–5. doi: 10.3345/kjp.2014.57.5.222
3. Allan CK, Newburger JW, McGrath E, Elder J, Psoinos C, Laussen PC, et al. The relationship between inflammatory activation and clinical outcome after infant cardiopulmonary bypass. Anesth analg. (2010) 111:1244–51. doi: 10.1213/ANE.0b013e3181f333aa
4. Ashraf SS, Tian Y, Zacharrias S, Cowan D, Martin P, Watterson K. Effects of cardiopulmonary bypass on neonatal and paediatric inflammatory profiles. Euro j cardio-thorac surg. (1997) 12:862–8.
5. Huber JN, Hilkin BM, Hook JS, Brophy PD, Davenport TL, Davis JE, et al. Neutrophil phenotype correlates with post-operative inflammatory outcomes in infants undergoing cardiopulmonary bypass. Pediatr crit care med. (2017) 18:1145–52. doi: 10.1097/pcc.0000000000001361
6. Reiter K, Balling G, Bonelli V, Pabst von Ohain J, Braun SL, Ewert P, et al. Neutrophil gelatinase-associated lipocalin reflects inflammation and is not a reliable renal biomarker in neonates and infants after cardiopulmonary bypass: a prospective case-control study. Cardiol young. (2018) 28:243–51. doi: 10.1017/s1047951117001767
7. Sari I, Sunbul M, Mammadov C, Durmus E, Bozbay M, Kivrak T, et al. Relation of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio with coronary artery disease severity in patients undergoing coronary angiography. Kardiol polska. (2015) 73:1310–6. doi: 10.5603/KP.a2015.0098
8. Giakoumidakis K, Fotos NV, Patelarou A, Theologou S, Argiriou M, Chatziefstratiou AA, et al. Perioperative neutrophil to lymphocyte ratio as a predictor of poor cardiac surgery patient outcomes. Pragmat obs res. (2017) 8:9–14. doi: 10.2147/por.s130560
9. Choi JE, Villarreal J, Lasala J, Gottumukkala V, Mehran RJ, Rice D, et al. Perioperative neutrophil:lymphocyte ratio and post-operative NSAID use as predictors of survival after lung cancer surgery: a retrospective study. Cancer med. (2015) 4:825–33. doi: 10.1002/cam4.428
10. Madhok AB, Ojamaa K, Haridas V, Parnell VA, Pahwa S, Chowdhury D. Cytokine response in children undergoing surgery for congenital heart disease. Pediatric cardiol. (2006) 27:408–13. doi: 10.1007/s00246-006-0934-y
11. Gessler P, Schmitt B, Pretre R, Latal B. Inflammatory response and neurodevelopmental outcome after open-heart surgery in children. Pediatric cardiol. (2009) 30:301–5. doi: 10.1007/s00246-008-9354-5
12. Leliefeld PH, Wessels CM, Leenen LP, Koenderman L, Pillay J. The role of neutrophils in immune dysfunction during severe inflammation. Crit care. (2016) 20:73. doi: 10.1186/s13054-016-1250-4
13. Herbert C, Patel M, Nugent A, Dimas VV, Guleserian KJ, Quigley R, et al. Serum cystatin C as an early marker of neutrophil gelatinase-associated lipocalin-positive acute kidney injury resulting from cardiopulmonary bypass in infants with congenital heart disease. Congenit heart dis. (2015) 10:E180–8. doi: 10.1111/chd.12253
14. Prabhu A, Sujatha DI, Ninan B, Vijayalakshmi MA. Neutrophil gelatinase associated lipocalin as a biomarker for acute kidney injury in patients undergoing coronary artery bypass grafting with cardiopulmonary bypass. Ann vasc surg. (2010) 24:525–31. doi: 10.1016/j.avsg.2010.01.001
15. Kohira S, Oka N, Inoue N, Itatani K, Hanayama N, Kitamura T, et al. Effect of the neutrophil elastase inhibitor sivelestat on perioperative inflammatory response after pediatric heart surgery with cardiopulmonary bypass: a prospective randomized study. Artif organs. (2013) 37:1027–33. doi: 10.1111/aor.12103
16. Inoue N, Oka N, Kitamura T, Shibata K, Itatani K, Tomoyasu T, et al. Neutrophil elastase inhibitor sivelestat attenuates perioperative inflammatory response in pediatric heart surgery with cardiopulmonary bypass. Inter heart j. (2013) 54:149–53. doi: 10.1536/ihj.54.149
17. Imtiaz F, Shafique K, Mirza SS, Ayoob Z, Vart P, Rao S. neutrophil lymphocyte ratio as a measure of systemic inflammation in prevalent chronic diseases in Asian population. Inter arch med. (2012) 5:2. doi: 10.1186/1755-7682-5-2
18. Uslu AU, Kucuk A, Sahin A, Ugan Y, Yilmaz R, Gungor T, et al. Two new inflammatory markers associated with disease activity score-28 in patients with rheumatoid arthritis: neutrophil-lymphocyte ratio and platelet-lymphocyte ratio. Inter j rheum dis. (2015) 18:731–5. doi: 10.1111/1756-185x.12582
19. Savluk OF, Guzelmeric F, Yavuz Y, Akyuz M, Cevirme D, Tongut A, et al. The neutrophil lymphocyte ratio as a successful extubation predictor of prolonged intubation in pediatric heart surgery. Iran J Pediatrics. (2017) 27:e9416. doi: 10.5812/ijp.9416
20. Thiele JR, Zeller J, Bannasch H, Stark GB, Peter K, Eisenhardt SU. Targeting C-reactive protein in inflammatory disease by preventing conformational changes. Mediators inflamm. (2015) 2015:372432. doi: 10.1155/2015/372432
Keywords: pediatric patients, cardiopulmonary bypass, neutrophil lymphocyte ratio, C reactive protein, prognostic
Citation: Xu H, Sun Y and Zhang S (2019) The Relationship Between Neutrophil to Lymphocyte Ratio and Clinical Outcome in Pediatric Patients After Cardiopulmonary Bypass Surgery: A Retrospective Study. Front. Pediatr. 7:308. doi: 10.3389/fped.2019.00308
Received: 11 February 2019; Accepted: 09 July 2019;
Published: 31 July 2019.
Edited by:
Oswin Grollmuss, Université Paris-Sud, FranceReviewed by:
Elumalai Appachi, Baylor College of Medicine, United StatesCopyright © 2019 Xu, Sun and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sibi Zhang, ZHIuemhhbmdzaWJpQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.