
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 12 February 2019
Sec. Pediatric Nephrology
Volume 7 - 2019 | https://doi.org/10.3389/fped.2019.00025
 Fatma Zehra Oztek-Celebi1
Fatma Zehra Oztek-Celebi1 Marion Herle2
Marion Herle2 Valentin Ritschl3
Valentin Ritschl3 Lukas Kaltenegger2
Lukas Kaltenegger2 Tanja Stamm3
Tanja Stamm3 Christoph Aufricht2
Christoph Aufricht2 Michael Boehm2*
Michael Boehm2*Background: Kidney transplantation is the preferred treatment modality for children with end-stage renal disease. In the adult population, migration-related modifiable factors were associated with low living donation rates; no such data are available on the pediatric population. This pilot study therefore compares donation modality, communication, knowledge, and attitudes/beliefs between families of immigrant and non-immigrant descent.
Methods: Demographic and clinical characteristics of a cohort of children from 77 families of immigrant (32; 42%) and non-immigrant (45; 58%) descent who had undergone renal transplantation were assessed and related to donation modality at the Medical University of Vienna. In a representative subset, modifiable migration-related factors were assessed in a questionnaire-based study.
Results: In immigrant families, information delay, limited communication, low knowledge levels, and self-reported conflicting beliefs were significantly more prevalent than in non-immigrants. The living kidney donation rate to children was high in both populations (immigrants: 63%, non-immigrants: 44%; p = 0.12). Living donation to children on dialysis was even significantly higher in immigrant families (immigrants: 13 out of 20; 57%, non-immigrants: 9 out of 33; 27%; p = 0.03).
Conclusion: Contrary to expectations, migration-related disparities did not translate into decreased living donation rates in immigrant families, in particular to children on dialysis. Certain factors might therefore be less important for the living donation process in pediatric care structures and/or might be overcome by yet undefined protective factors. Larger pediatric studies including qualitative and quantitative methods are required to validate and refine current conceptual frameworks integrating the perspective of affected families.
Kidney transplantation (KTx) is the treatment modality of choice in end-stage renal disease (1–3). Previously, racial and ethnic disparities in KTx have been reported in the pediatric setting (4). Children from minority groups in the US, particularly African-Americans, wait longer for a deceased donor (DD) KTx, and undergo less living donor (LD) and preemptive KTx compared to children of Caucasians (5–10). In Europe, a large ESPN/ERA-EDTA Registry report recently confirmed racial disparities in access to KTx (11), only few single center studies investigated the role of migration-associated disparities in pediatric KTx despite the increasing role of migration in Europe (12–15). Data from US immigrants are likely not transferable, as European immigrants are less likely to demonstrate racial differences, less likely to represent recent immigrants and mostly exposed to a less restrictive health care system (4, 11, 14, 15).
Recent research in the adult setting demonstrated that modifiable factors in the dimensions of communication, knowledge, and attitudes/beliefs are important in the living donation process (16). Based on that theoretical framework, two randomized trials successfully tested multicomponent interventions and resulted in increased referral of potential donors and actual LD KTx rates with stratified measures (17, 18). The same modifiable factors are also likely to differ between immigrant and non-immigrant families, and might therefore represent attractive targets to increase LD (and preemptive) KTx in that setting, thereby reducing disparities for children in immigrant families (4). To the best of our knowledge, however, neither disparities in modifiable factors (used to build the “adult” psychosocial concept of LD) nor their actual clinical relevance in immigrant and non-immigrant families on donation modality have been assessed in the pediatric setting of KTx to date.
The main objective of this pilot study was, therefore, to explore KTx donation modalities and modifiable factors in the dimensions of communication, knowledge, and attitudes/beliefs in parents of children with KTx in an Austrian cohort of families of immigrant or non-immigrant descent.
The study cohort consists of all families who were treated at the Medical University of Vienna between 2008 and 2013. The full cohort was used to establish baseline demographic and clinical characteristics; a random sample (the first 50 families who came to our transplant clinic during the study period) were asked to participate in the questionnaire-based modifiable factors study.
Demographic and clinical characteristics were taken from the patients' medical charts: age at KTx, sex, migration status, primary renal disease, first referral to pediatric nephrologist (FR), prior renal replacement therapy (RRT), preemptive vs. non-preemptive KTx, and organ donor source. A family's descent was classified as immigrant if the parents of the patient were first-generation immigrants (mother tongue of at least one parent was not German). In Austria, all patients have full insurance that cover all health-related costs, resulting in no disparities in listing and waiting times for KTx (14, 15). Patients who had already undergone transplantation were excluded.
Modifiable factors were evaluated in a questionnaire testing knowledge and assessing beliefs about LD KTx with support of one of the authors (FO-C; MB). If responding family members were uncertain about the meaning of a question, they were assisted and could ask for clarification. Out of 11 original belief statements published by Stothers (19), only six were used, since the remaining questions did not apply to a parent donor (“Donating a kidney to someone requires an extremely close personal relationship”; “It is acceptable for a parent to receive a kidney from his/her child (over 18 years old)”; “Approaching a potential donor who then says no will change the relationship between the two people”; “Asking someone to donate makes the recipient seem selfish or greedy”; “Decisions about donation should be made by the donor alone. The recipient should not ask for a kidney”).
Questionnaires were prepared in Turkish, Serbian/Croatian and German, and validated using back-translation by native speakers of the target languages. After the back-translation had been completed, an extensive debriefing took place and the wording of the questionnaires was adapted.
A “knowledge score” was calculated by adding the number of correct answers for each individual on the seven items that focused on knowledge. If all statements were answered correctly, a maximum score of seven could be achieved. Responses to attitude/belief statements and donating experience were analyzed by assigning a score of 1 (for the least positive attitude toward donation) to 5 (for the most positive attitude toward donation); The scores for each statement were then added up to obtain a so-called “belief score” for each individual.
Variables were compared between groups using Wilcoxon Signed Ranks, Mann-Whitney-U, ANOVA and chi-square tests, as appropriate. A P-value of ≤ 0.05 was considered to be statistically significant. All analyses were performed with SPSS version 24. No power calculation was made. Bonferroni correction was not applied to the statistical tests as this study is of an exploratory nature and each test considered to be led by a separate, cross-sectional hypothesis.
The Medical University Vienna approved the study protocol [EK number 190/2008] and the study was carried out in line with the declaration of Helsinki. All participants were informed in detail about the study procedures and had to give oral and written informed consent.
Out of 77 children who received a kidney transplant and who were treated at the Medical University of Vienna from 2008 to 2013, 32 were from immigrant families (42%). Twenty-two families originated from ex-Yugoslavia (n = 12) or Turkey (n = 10), the rest (n = 10) from Romania, Bulgaria, Spain, Hungary, Jordan, Nigeria, Sudan, and Thailand. The baseline characteristics are shown in Table 1. There was no difference in the time from first referral to the start of RRT, the waiting time from listing at Eurotransplant to KTx, or age at KTx (Table 1).
Children from immigrant families tended to receive a LD transplant more frequently than non-immigrant ones (immigrant: 20 out of 32; 63%, non-immigrant: 20/45; 44%; p = 0.12). There were no differences in the overall rate of preemptive donation (immigrant: 9/32; 28%, non-immigrant: 12/45; 27%) (Table 1). In preemptive KTx, the proportions of LD were comparable (immigrant: 7/9; 78%, non-immigrant: 11/12; 92%; p = 0.37) (Figure 1). In non-preemptive KTx, the proportion of LD was significantly higher in immigrant families (immigrant: 13/20; 57%, non-immigrant: 9/33; 27%; p = 0.03) (Figure 1).
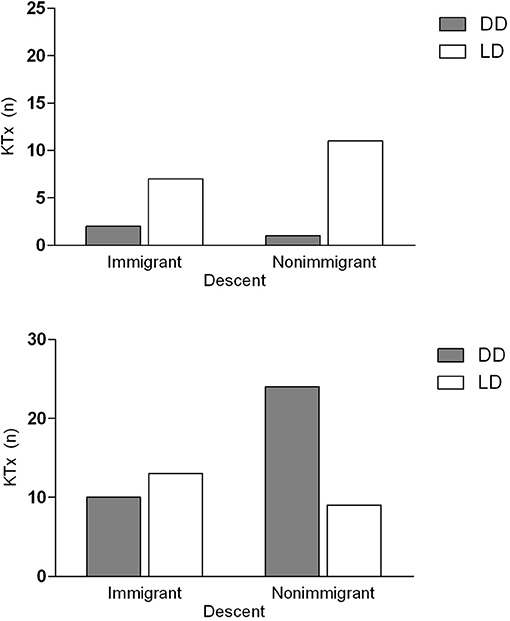
Figure 1. Kidney transplantation in families of immigrant and non-immigrant descent in Austria. Patients are stratified by donation modality of KTx (upper panel: preemptive, lower panel: non-preemptive) and by descent (left bars: immigrant and right bars: non-immigrant) and by donor source. The dark bars show the number of DD KTx, the light bars indicate the amount of LD transplantations. In non-preemptive KTx, the proportion of living donations was significantly higher in immigrant families than in non-immigrant ones (p = 0.03). KTx, Kidney transplantation; DD, deceased donor; LD, living donor.
Forty-four families (88% of those invited) agreed to participate in the questionnaire-based study, fourteen immigrant families and 30 non-immigrant ones (35 mothers, 9 fathers); out of these 23 children received a LD and 21 children a DD transplant. In 39 families, at least one parent was screened for feasibility of LD KTx. Twenty-three out of these 39 parents donated their kidney, significantly more from immigrant families (11/12) than from non-immigrant ones (12/27), (immigrant: 92%, non-immigrant: 44%; p = 0.009). As shown in Table 1, the questionnaire sub-population was representative of the total cohort regarding demographic and clinical characteristics.
KTx-related communication is demonstrated in Table 2. Both groups felt that they had enough time and sufficient information to consider organ donation (immigrant: 93%, non-immigrant: 90%; p = 0.8). However, significantly fewer immigrant families stated that the first communication on organ donation with the medical staff was 2 years or more before KTx (immigrant: 3 out of 14; 21%, non-immigrant: 16/30; 55%; p = 0.04). The medical staff were the main source of information on LD in both populations, but use of other sources of information, such as the mass media, to obtain information about organ donation was significantly lower in immigrant families (immigrant: 3/14; 23%, non-immigrant: 17/30; 57%; p = 0.04).
The knowledge results are shown in Table 3. The percentage of correct answers was significantly higher in the non-immigrant group (immigrant: 56%, non-immigrant: 70%; p = 0.045). A significantly higher percentage of immigrants than non-immigrants answered, “I don't know” to many of the knowledge statements (immigrants: 28%, non-immigrants: 12%; p = 0.03).
The belief results are presented in Table 4. The total score for the belief statements did not differ between both groups, but two conflicting statements were more often chosen by immigrant families, “since there is a life after death, people should enter the next life with a complete body” and “donating a kidney is a rewarding experience for donors” (immigrant: 3/14; 21% and 11/13; 84%, non-immigrant: 1/28; 4% and 14/30; 48%; p = 0.04 and p = 0.03, respectively).
This study found disparities in communication and knowledge, and some significant differences in beliefs about LD KTx in immigrant families in Austria with children who had received a transplant. Surprisingly, these disparities were not associated with reduced access to LD KTx, but rather with a tendency toward a higher rate of living donation to children in immigrant families. Whereas, the preemptive donating rate was similar for both groups, significantly more LD KTx were performed in immigrant families than in non-immigrant ones, once dialysis had been initiated.
Our data describe clear differences in communication, knowledge, and beliefs in immigrant families in Austria, confirming findings regarding migration-related disparities in the adult setting of KTx (16). A delay in information on LD KTx from the medical staff, together with less use of the media, books, and other important sources of information on LD, might have resulted in a lower level of health literacy, exacerbated by limited access to reliable information in their mother tongues (20). Health literacy has previously been reported to be lower in immigrant families in other pediatric settings and associated with reduced access to LD KTx in the adult setting (21–23). However, health literacy was not directly assessed in our study, and alternate interpretations, such as positive effects on LD due to decreased exposure to misleading information from media might also be valid. Whether the lower knowledge levels concerning LD KTx in the immigrant families in our study, manifesting themselves in the form of more “I don't know” answers and more factually wrong answers such as “Women may have difficulty with future pregnancies, if they donate a kidney,” are attributable to reduced health literacy therefore needs clarification in future studies. In addition, higher prevalence of conflicting beliefs that might preclude or dissuade an individual from participating in LD such as “since there is a life after death, people should enter the next life with a complete body,” might pose a potential obstacle for LD in the immigrant families. Taken together, limitations in information/communication/knowledge about LD, combined with ambiguous attitudes/beliefs, are likely to increase decision-making conflicts regarding the living donation process (24).
However, our study found—in contrast to the expectations from the literature (25, 26)—no disparities in actual LD KTx rates in children of immigrant families in Austria. Why did migration-related factors that determined a low likelihood of LD in the adult setting (thus forming the current theoretical framework for LD) not result in reduced LD KTx rates in our pediatric population? The extent of the disparities in these modifiable factors, were almost identical in our immigrant group to those found in non-donors in the adult KTx population (19). In a previous study, we also found comparable disparities in measures of socioeconomic status, such as education levels and job quality, as was reported in the adult KTx populations (14, 19). We suggest as one possible explanation that adult and pediatric nephrology care settings are distinctly different in the context of the LD communication process. In the patient-centered adult setting, the patient with ESRD is expected to actively recruit potential donors. Consequently, deficits in communication with potential donors are directly linked to low rates of LD KTx (16). As a result, targeting this deficit with home-based education and communication by the transplant team was proven to be effective interventions (17, 18). In contrast, it is standard procedure in the family-focused pediatric setting for the interdisciplinary transplant team to repeatedly discuss all LD options with the parents, who inherently represent the most likely donors. In our study, this setting resulted in a high recruitment level, with about 90% of parents undergoing donor evaluation, compared to the adult setting with rates of <20% prior to intervention, and of about 60% post intervention (17, 18). Our results therefore suggest that certain migration-related disparities defined in the adult setting, such as limited communication and knowledge, might be less dominant in the case of the living donation process in pediatric care structures.
The surprisingly high rate of LD KTx in the immigrant families suggests that the disparities observed might have been more than overcome by yet undefined protective factors (16). The phenomenon of immigrant groups demonstrating equal or even better health outcomes than non-immigrants, despite the presence of obvious disparities, has previously been described as an “epidemiological paradox” (27). In the context of US-based KTx outcome studies, the “Hispanic Paradox” is used to summarize complex social and cultural “protective” factors such as strong ethnic identity and intense family relationships (9). Indeed, “donating a kidney is a rewarding experience for donors” was a significantly more frequently stated belief in the immigrant group, and medically adequate donors from immigrant families were twice as likely to ultimately donate a kidney than parents from non-immigrant families. Interestingly, the LD rate in immigrant families in Austria was selectively increased in non-preemptive KTx. Non-immigrant families appeared to be motivated to donate when it enabled a preemptive transplantation to be made but tended not to donate once the patient was on dialysis. In contrast, immigrant families were much more likely to donate when their child was on dialysis. The potential role of sociocultural factors for this apparently paradoxical donation pattern is supported by comparably high LD (with low preemptive donation) rates in Serbia and Turkey, the main countries of origin of immigrant families in Austria (26, 27). Unfortunately, our questionnaire was not designed to detect alternate explanations for the epidemiological paradox, such as concerns among the immigrant community that DD KTx may be less accessible to their group. To understand these findings better and to define as yet unknown factors, innovative study designs will be required which integrate qualitative methods in order to explore the perspective of the families affected of both immigrant and non-immigrant descent (28, 29).
This study has several limitations. Due to the rarity of pediatric KTx, the single center design precluded the use of complex statistical analysis and might have introduced bias of center specific experiences and attitudes of the pediatric nephrologists. For example, higher promotion of the advantages of LD could be a reason for the higher percentage of donor evaluation in our population. Our observations thus need independent validation to be generalizable to other populations or health care systems. However, it should be stated that the overall LD KTx rate in this study was comparable to the average European rate (26), suggesting that our results do not merely reflect an “Austrian-approach” effect. Small numbers of responders may underestimate difference in the complex psychosocial setting of LD in chronic renal failure, therefor a multicenter study should be envisaged. However, this was an exploratory study that yielded unexpected new findings in a representative pediatric cohort. Parents who participated in the questionnaire subgroup might have differed from those who did not. However, no significant differences were noted in terms of demographic or clinical variables. As the study was performed in families with children who had already undergone KTx, data on beliefs and knowledge were subject to several biases, including post-hoc justification and recall bias. However, their responses best reflect their current perception of the situation having had time to reflect. Despite these shortcomings, our pilot study delineated—in addition to the novel observation of an apparently paradoxical donation pattern in immigrant families—important differences to current adult concepts of the LD process.
In conclusion, our study describes high rates of pediatric LD KTx in immigrant families in Austria, despite confirmation of significant disparities, such as information delay, limited communication, lower knowledge levels, and more conflicting belief systems regarding LD. Therefore, certain migration-related disparities defined in the adult setting might be less important/dominant in the case of the living donation process in pediatric care structures and did not translate into reduced willingness to donate. The observation that immigrant families were much more likely to donate once they saw the challenges of dialysis (for patient and/or family) additionally suggests yet undefined migration-related protective factors (“epidemiological paradox”). These new and unexpected findings of our pilot study indicate the need for future quantitative and qualitative research to validate this donation pattern in independent populations and to explore yet unknown perspectives of immigrant and non-immigrant families to build a robust theoretical framework for pediatric KTx.
All authors have significantly contributed to conception (FO-C, CA, MB), design (FO-C, CA, MH, MB), analysis (FO-C, LK, CA, MB) and interpretation of data (FO-C, CA, MH, VR, TS, LK, MB). The questionnaires were filled out during a questionnaire-based study with FO-C and MB. All authors gave final approval of the submitted version. The results presented in this paper have not been published previously in whole or part, except in abstract form.
This study was supported by the Medical-Scientific Fund of the Mayor of Vienna (Nr. 2581; CA) and the Anniversary Fund of the Oesterreichische Nationalbank (Nr. 17194; MB).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Vats AN, Donaldson L, Fine RN, Chavers BM. Pretransplant dialysis status and outcome of renal transplantation in North American children: a NAPRTCS Study. North american pediatric renal transplant cooperative study. Transplantation (2000) 69:1414–9. doi: 10.1097/00007890-200004150-00035
2. Amaral S, Sayed BA, Kutner N, Patzer RE. Preemptive kidney transplantation is associated with survival benefits among pediatric patients with end-stage renal disease. Kidney Int. (2016) 90:1100–8. doi: 10.1016/j.kint.2016.07.028
3. Boehm M, Winkelmayer WC, Arbeiter K, Mueller T, Aufricht C. Late referral to paediatric renal failure service impairs access to pre-emptive kidney transplantation in children. Arch Dis Child. (2010) 95:634–8. doi: 10.1136/adc.2009.174581
4. Freeman MA, Myaskovsky L. An overview of disparities and interventions in pediatric kidney transplantation worldwide. Pediatr Nephrol. (2015) 30:1077–86. doi: 10.1007/s00467-014-2879-3
5. Furth SL, Garg PP, Neu AM, Hwang W, Fivush BA, Powe NR. Racial differences in access to the kidney transplant waiting list for children and adolescents with end-stage renal disease. Pediatrics (2000) 106:756–61. doi: 10.1542/peds.106.4.756
6. Omoloja A, Mitsnefes M, Talley L, Benfield M, Neu A. Racial differences in graft survival: a report from the north american pediatric renal trials and collaborative studies (NAPRTCS). Clin J Am Soc Nephrol. (2007) 2:524–8. doi: 10.2215/CJN.03100906
7. Gore JL, Danovitch GM, Litwin MS, Pham PT, Singer JS. Disparities in the utilization of live donor renal transplantation. Am J Transplant. (2009) 9:1124–33. doi: 10.1111/j.1600-6143.2009.02620.x
8. Patzer RE, Sayed BA, Kutner N, McClellan WM, Amaral S. Racial and ethnic differences in pediatric access to preemptive kidney transplantation in the United States. Am J Transplant. (2013) 13:1769–81. doi: 10.1111/ajt.12299
9. Patzer RE, Mohan S, Kutner N, McClellan WM, Amaral S. Racial and ethnic disparities in pediatric renal allograft survival in the United States. Kidney Int. (2015) 87:584–92. doi: 10.1038/ki.2014.345
10. Ku E, McCulloch CE, Grimes BA, Johansen KL. Racial and ethnic disparities in survival of children with ESRD. J Am Soc Nephrol. (2017) 28:1584–91. doi: 10.1681/ASN.2016060706
11. Tjaden LA, Noordzij M, van Stralen KJ, Kuehni CE, Raes A, Cornelissen EA , et al. Racial disparities in access to and outcomes of kidney transplantation in children, adolescents, and young adults: results from the ESPN/ERA-EDTA (European Society of Pediatric Nephrology/European Renal Association-European Dialysis and Transplant Association) Registry. Am J Kidney Dis. (2016) 67:293–301. doi: 10.1053/j.ajkd.2015.09.023
12. Rudge C, Johnson RJ, Fuggle SV, Forsythe JL. Kidney, and Pancreas Advisory Group, U.K.T.N.H.S.B.T. Renal transplantation in the United Kingdom for patients from ethnic minorities. Transplantation (2007) 83:1169–73. doi: 10.1097/01.tp.0000259934.06233.ba
13. Tromp WF, Cransberg K, van der Lee JH, Bouts AH, Collard L, Van Damme-Lombaerts R , et al. Fewer pre-emptive renal transplantations and more rejections in immigrant children compared to native Dutch and Belgian children. Nephrol Dial Transplant. (2012) 27:2588–93. doi: 10.1093/ndt/gfr628
14. Oztek FZ, Ipsiroglu O, Mueller T, Aufricht C. Outcome after renal transplantation in children from native and immigrant families in Austria. Eur J Pediatr. (2009) 168:11–6. doi: 10.1007/s00431-008-0698-x
15. Oztek FZ, Tekin P, Herle M, Mueller T, Arbeiter K, Aufricht C. Does immigration background influence outcomes after renal transplantation? Pediatr Nephrol. (2011) 26:309–15. doi: 10.1007/s00467-010-1685-9
16. Ismail SY, Luchtenburg AE, Kal VGJA, Zuidema WC, Weimar W, Busschbach JJ , et al. Modifiable factors in access to living-donor kidney transplantation among diverse populations. Transplantation (2013) 96:586–90. doi: 10.1097/TP.0b013e31829b754c
17. Ismail SY, Luchtenburg AE, Timman R, Zuidema WC, Boonstra C, Weimar W , et al. Home-based family intervention increases knowledge, communication and living donation rates: a randomized controlled trial. Am J Transplant. (2014) 14:1862–9. doi: 10.1111/ajt.12751
18. Patzer RE, Paul S, Plantinga L, Gander J, Sauls L, Krisher J , et al. A randomized trial to reduce disparities in referral for transplant evaluation. J Am Soc Nephrol. (2017) 28:935–42. doi: 10.1681/ASN.2016030320
19. Stothers L, Gourlay WA, Liu L. Attitudes and predictive factors for live kidney donation: a comparison of live kidney donors versus nondonors. Kidney Int. (2005) 67:1105–11. doi: 10.1111/j.1523-1755.2005.00176.x
20. Mazaris EM, Warrens AN, Smith G, Tekkis P, Papalois VE. Live kidney donation: attitudes towards donor approach, motives and factors promoting donation. Nephrol Dial Transplant. (2012) 27:2517–25. doi: 10.1093/ndt/gfr642
21. Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. (2004) 19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x
22. Sanders LM, Thompson VT, Wilkinson JD. Caregiver health literacy and the use of child health services. Pediatrics (2007) 119:e86–92. doi: 10.1542/peds.2005-1738
23. Dageforde LA, Petersen AW, Feurer ID, Cavanaugh KL, Harms KA, Ehrenfeld JM , et al. Health literacy of living kidney donors and kidney transplant recipients. Transplantation (2014) 98:88–93. doi: 10.1097/TP.0000000000000027
24. McPherson L, Basu M, Gander J, Pastan SO, Mohan S, Wolf MS , et al. Decisional conflict between treatment options among end-stage renal disease patients evaluated for kidney transplantation. Clin Transplant. (2017) 31:e12991. doi: 10.1111/ctr.12991
25. Roodnat JI, van de Wetering J, Zuidema W, van Noord MA, Kal-van Gestel JA, Ijzermans JN , et al. Ethnically diverse populations and their participation in living kidney donation programs. Transplantation (2010) 89:1263–9. doi: 10.1097/TP.0b013e3181d84ca7
26. Harambat J, van Stralen KJ, Schaefer F, Grenda R, Jankauskiene A, Kostic M , et al. Disparities in policies, practices and rates of pediatric kidney transplantation in Europe. Am J Transplant. (2013) 13:2066–74. doi: 10.1111/ajt.12288
27. Khlat M, Darmon N. Is there a mediterranean migrants mortality paradox in Europe? Int J Epidemiol. (2003) 32:1115–8. doi: 10.1093/ije/dyg308
28. Hanson CS, Ralph AF, Manera KE, Gill JS, Kanellis J, Wong G , et al. The lived experience of “being evaluated” for organ donation: focus groups with living kidney donors. Clin J Am Soc Nephrol. (2017) 12:1852–61. doi: 10.2215/CJN.03550417
Keywords: pediatric renal replacement therapy, racial and ethnic disparities, preemptive transplantation, donor source, immigration
Citation: Oztek-Celebi FZ, Herle M, Ritschl V, Kaltenegger L, Stamm T, Aufricht C and Boehm M (2019) High Rate of Living Kidney Donation to Immigrant Children Despite Disparities—An Epidemiological Paradox? Front. Pediatr. 7:25. doi: 10.3389/fped.2019.00025
Received: 08 October 2018; Accepted: 22 January 2019;
Published: 12 February 2019.
Edited by:
Robert P. Woroniecki, Stony Brook Children's Hospital, United StatesReviewed by:
Michael Aloysius Freeman, Penn State Milton S. Hershey Medical Center, United StatesCopyright © 2019 Oztek-Celebi, Herle, Ritschl, Kaltenegger, Stamm, Aufricht and Boehm. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael Boehm, bWljaGFlbC5ib2VobUBtZWR1bml3aWVuLmFjLmF0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.