- 1Weill Cornell Medicine-Qatar, Ar-Rayyan, Qatar
- 2Sidra Medical and Research Center, Doha, Qatar
- 3College of Medicine, Qatar University, Doha, Qatar
Although more than 300 different techniques for hypospadias repair do exist, successful outcome depends mainly on the surgeon's skills, availability of adequate tissue for urethral reconstruction and choice of the best suitable technique in each case. Significant advancements in the management of hypospadias occurred over the last few decades but there remains great controversy on how to select the best technical options (1). The general principle for hypospadias repair consists in the tubularization of ventral urethral plate, bringing the meatus all the way to the tip of the glans, depending on the presence of associated ventral penile curvature. Such accomplishment can be achieved with a single or staged procedure. In the most common scenario, distal hypospadias without curvature, tubularization of the urethral plate is the currently most frequently utilized approach (2). However simple tubularization is not always suitable, especially in narrow plates that could result in stenosis. Aiming to augment the plate dimensions Snodgrass, in 1998, popularized to simply deeply incise and tubularize the urethral plate, relying on epithelization/granulation of the raw dorsal urethra (3, 4). This procedure has been successful in a great number of cases, reason why it was quickly adopted worldwide. The mechanism of healing the incised plate is still open for discussion (5). Some authors believe there is complete re-epithelization with urothelium while others think that there is formation of granulation tissue that later is followed by gradual fibrosis of the area. This could be reason why some authors reported worse outcomes in narrow urethral plates, theorizing that most of the neourethra would be reconstructed based on a raw, current dorsal urethrotomy that gradually heals narrowing the segment (4, 6). Moreover, healing of a larger incised raw area of neourethra is unpredictable; it seems that this process may exert tension on the ventral suture line affecting its primary healing (7). In an attempt to improve healing of the neourethra after the TIP urethroplasty, grafting of the dorsal incised (GTIP) area using the inner prepuce has been described by several authors (8–10). It was shown, in a series of 1,095 hypospadias, that there were 0 and 18% complication rate with GTIP in primary and repeat surgeries in contrast to about 5, 23% consecutively (11). Although the GTIP is an attractive and well-accepted procedure by adult reconstructive urologists repairing urethral strictures, its acceptance for primary hypospadias in children is still unclear. GTIP is more technically demanding than regular TIP therefore its indication should be tailored appropriately. Unfortunately, it has been difficult to prove the advantages of the GTIP over the TIP repair as both have low complication rates, demanding a large number of subjects for a randomized study aiming to answer this question. Therefore, at this point in time, we are faced with a procedure that makes sense but still not proved by evidence and most surgeons adopt it based on expert opinion. We have been trying to delineate which patients with hypospadias need to have GTIP, considering those with unfavorable plates (narrow and poor spongiosum) as the ideal candidates. However, based on visual inspection, it is not easy to agree upon urologists what is a favorable or unfavorable plate (12). Considering these difficulties, we would like to propose an objective simple formula, measuring the ratio of the urethra before and after incision, to help deciding to graft or not the incised plate. The urethral plate should be maximally stretched and measured in its widest point. It is then deeply incised all the way to the corpora and the same measurements are repeated, therefore producing a urethral plate ratio before and after incision. If the ratio is less than 0.5 we consider that a significant component of the neourethra will be composed by raw tissue, therefore vulnerable to stenosis and such cases should be grafted (Figure 1).
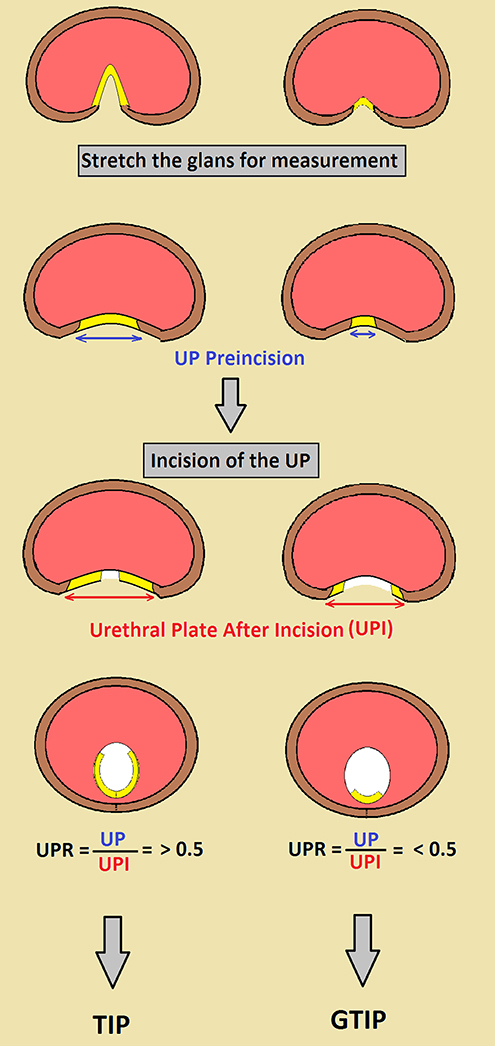
Figure 1. Schematic representation of a cross section at the level of the glans in distal hypospadias repair demonstrating the utilization of the Urethral Plate Ratio.
We acknowledge that such proposal lacks evidence support but it is an objective and consistent measurement that may be useful to surgeons deciding to graft or not the incised plate.
Author Contributions
TA has come up with the suggested UPR ratio. JP has validated the point and both wrote this manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The publication of the article was funded by Qatar National library.
References
1. Keays MA, Dave S. Current hypospadias management: diagnosis, surgical management, and long-term patient-centred outcomes. Can Urol Assoc J. (2017) 11(1–2 Suppl. 1):S48–53. doi: 10.5489/cuaj.4386
2. Snodgrass WT, Bush N, Cost N. Tubularized incised plate hypospadias repair for distal hypospadias. J Pediatr Urol. (2010) 6:408–13. doi: 10.1016/j.jpurol.2009.09.010
3. Mousavi SA, Aarabi M. Tubularized incised plate urethroplasty for hypospadias reoperation: a review and meta-analysis. Int Braz J Urol. (2014) 40:588–95. doi: 10.1590/S1677-5538.IBJU.2014.05.02
4. Holland AJ, Smith GH, Cass DT. Clinical review of the “Snodgrass” hypospadias repair. Aust N Z J Surg. (2000) 70:597–600. doi: 10.1046/j.1440-1622.2000.01906.x
5. Eassa W, He X, El-Sherbiny M. How much does the midline incision add to urethral diameter after tubularized incised plate urethroplasty? An experimental animal study. J Urol. (2011) 186:1625–30. doi: 10.1016/j.juro.2011.03.073
6. Sarhan O, Saad M, Helmy T, Hafez A. Effect of suturing technique and urethral plate characteristics on complication rate following hypospadias repair: a prospective randomized study. J Urol. (2009) 182:682–6. doi: 10.1016/j.juro.2009.04.034
7. Elbakry A, Hegazy M, Matar A, Zakaria A. Tubularised incised-plate versus tubularisation of an intact and laterally augmented plate for hypospadias repair: a prospective randomised study. Arab J Urol. (2016) 14:163–70. doi: 10.1016/j.aju.2016.03.004
8. Mouravas V, Filippopoulos A, Sfoungaris D. Urethral plate grafting improves the results of tubularized incised plate urethroplasty in primary hypospadias. J Pediatr Urol. (2014) 10:463–8. doi: 10.1016/j.jpurol.2013.11.012
9. Silay MS, Sirin H, Tepeler A, Karatag T, Armagan A, Horasanli K, et al. “Snodgraft” technique for the treatment of primary distal hypospadias: pushing the envelope. J Urol. (2012) 188:938–42. doi: 10.1016/j.juro.2012.04.126
10. Gundeti M, Queteishat A, Desai D, Cuckow P. Use of an inner preputial free graft to extend the indications of Snodgrass hypospadias repair (Snodgraft). J Pediatr Urol. (2005) 1:395–6. doi: 10.1016/j.jpurol.2005.03.010
11. Ferro F, Vallasciani S, Borsellino A, Atzori P, Martini L. Snodgrass urethroplasty: grafting the incised plate –10 years later. J Urol. (2009) 182:1730–5. doi: 10.1016/j.juro.2009.03.066
12. El-Hout Y, Braga LHP, Pippi Salle JL, Moore K, Bägli DJ, Lorenzo AJ. Assessment of urethral plate appearance through digital photography: do pediatric urologists agree in their visual impressions of the urethral plate in children with hypospadias? J Pediatr Urol. (2010) 6:294–300. doi: 10.1016/j.jpurol.2009.09.003
Keywords: hypospadias, grafted tubularized incised plate, dorsal inlay graft, urethral plate, Ratio
Citation: Abbas TO and Pippi Salle JL (2018) When to Graft the Incised Plate During TIP Repair? A Suggested Algorithm That may Help in the Decision-Making Process. Front. Pediatr. 6:326. doi: 10.3389/fped.2018.00326
Received: 18 June 2018; Accepted: 11 October 2018;
Published: 14 November 2018.
Edited by:
Alexander Springer, Medizinische Universität Wien, AustriaReviewed by:
Grzegorz Kudela, Medical University of Silesia, PolandOnur Telli, Dr Lütfi Kirdar Kartal Egitim ve Araştirma Hastanesi, Turkey
Copyright © 2018 Abbas and Pippi Salle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tariq O. Abbas, dGFyaXEyY0Bob3RtYWlsLmNvbQ==
 Tariq O. Abbas
Tariq O. Abbas Joao L. Pippi Salle2
Joao L. Pippi Salle2