
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Pediatr. , 08 October 2018
Sec. General Pediatrics and Pediatric Emergency Care
Volume 6 - 2018 | https://doi.org/10.3389/fped.2018.00260
This article is part of the Research Topic Highlights in General Pediatrics and Pediatric Emergency Care: 2021 View all 10 articles
Introduction: While fever is the main complaint among pediatric emergency services and high antibiotic prescription are observed, only a few studies have been published addressing this subject. Therefore this systematic review aims to summarize antibiotic prescriptions in febrile children at the ED and assess its determinants.
Methods: We extracted studies published from 2000 to 2017 on antibiotic use in febrile children at the ED from different databases. Author, year, and country of publishing, study design, inclusion criteria, primary outcome, age, and number of children included in the study was extracted. To compare the risk-of-bias all articles were assessed using the MINORS criteria. For the final quality assessment we additionally used the sample size and the primary outcome.
Results: We included 26 studies reporting on antibiotic prescription and 28 intervention studies on the effect on antibiotic prescription. In all 54 studies antibiotic prescriptions in the ED varied from 15 to 90.5%, pending on study populations and diagnosis. Respiratory tract infections were mostly studied. Pediatric emergency physicians prescribed significantly less antibiotics then general emergency physicians. Most frequent reported interventions to reduce antibiotics are delayed antibiotic prescription in acute otitis media, viral testing and guidelines.
Conclusion: Evidence on antibiotic prescriptions in children with fever presenting to the ED remains inconclusive. Delayed antibiotic prescription in acute otitis media and guidelines for fever and respiratory infections can effectively reduce antibiotic prescription in the ED. The large heterogeneity of type of studies and included populations limits strict conclusions, such a gap in knowledge on the determining factors that influence antibiotic prescription in febrile children presenting to the ED remains.
Fever is the main complaint among pediatric emergency services (1). In only 15% (IQR 8·0–23·2%) a serious bacterial infection (SBI) is diagnosed with pneumonia and urinary tract infection (UTI) being the most prevalent (2, 3).
In contrast to the above, high antibiotic prescriptions are observed in febrile children (4, 5). Guidelines, or new diagnostic approaches have shown to effectively reduce antibiotic prescriptions in primary care (6–9). This is important because unnecessary antibiotic use increases antibiotic resistance (10, 11). In contrast to hospital based studies or primary care settings (11–15), few studies have been published in emergency department (ED) settings nor do we have valid estimates of potential benefits of antibiotic reducing interventions. Therefore our primary study aim is to assess antibiotic prescriptions for febrile children visiting the emergency department and their determinants. Secondary, we aim to investigate potential interventions that have been proven to be effective in the ED.
All descriptive and interventional studies published in 2000–2017 reporting on antibiotic use in children (age under 18) with fever in the emergency department were eligible for this review.
We searched Embase, Medline (OvidSP), Web-of-science, Scopus, Cinahl, Cochrane, PubMed publisher, and Google scholar for the (analogs of) keywords: fever, antibiotics, emergency department, children and antibiotic prescription. Initially search was performed in 2015 and updated in October 2017 (Supplementary Material 1). References were checked for additional articles to be included.
A screening by title/abstract resulted in potential eligible articles that underwent full text review. Two authors reviewed all articles; any discrepancies were solved by oral agreement between authors.
– Setting: Emergency department; if mixed settings, at least 30% (50 patients minimum) of the population needed to be admitted to the ED.
– Design: observational studies and randomized controlled trials with a minimum of 50 participants.
– Outcome: the studies had to report the number or percentage of antibiotics prescribed.
– Population: participants under the age of 18; if mixed ages, at least 20% of the population needed to be <18 years (with a minimum of 50) or age specific antibiotic prescriptions had to be presented. Studies on children with specific comorbidities only were excluded.
– Fever: at least 30% of all included children needed to have fever or the reason of visit was (reported) fever.
To compare the risk-of-bias of all these different study designs all articles were assessed using the MINORS criteria (16). Zero points were given for the item if not reported, one point if reported but insufficient and two points if reported and sufficient. As loss to follow-up was not applicable, due to emergency setting, we have let this particular item out of consideration; the maximum score for studies is 14 or 22 for respectively non-comparative and comparative studies. A maximum score on the MINORS criteria was needed to receive the status of a low risk of bias study (A) (17). For the final quality assessment we additionally used the sample size and the primary outcome. A high quality study was defined by status low risk of bias (A) on the MINORS, antibiotic prescription being the primary outcome and a sample size of at least 500 children. Two reviewers (EV and RO) have independently assessed all included studies. Supplementary Material 2 contains the complete quality assessment.
Extracted data included: Author, year, and country of publishing, study design, inclusion criteria, primary outcome, median (or mean when median not available) age, number of included children. Aiming to invest determinants of antibiotic prescription, we additionally extracted (if available): diagnosis, type of antibiotics, type of physicians, and type of intervention.
Due to heterogeneity in participants, outcome measures, interventions and study designs, no statistical pooling but a qualitative analysis was performed (18). Results are presented for the 5 main diagnosis, i.e., fever, AOM, pneumonia, other respiratory tract infections (RTI other) and UTI, with a minimum of 50 cases per diagnostic group required.
We obtained 837 articles by literature search. Screening the full text articles excluded 97 out of 151, which leaves 52 articles for data extraction. Two additional studies were included by reference check of included studies (Figure 1).
The study characteristics are presented in Table 1 for the included 54 studies. Most studies come from the US (n = 32, 59%), 16 others came from Europe, and 6 others from Canada (n = 3) (33, 36, 49), Australia (n = 2) (3), and Israel (n = 1) (26). The size of the studied population varied between 72 and 266.000 participants (median = 391). Most studies included children up to 36 months (n = 14, 25%) or all ages < 18 year (n = 18, 32%). Antibiotic prescription was the primary outcome in 33 studies (59%). Quality and feasibility assessment of the included studies (Supplementary Material 2).
Sixteen studies (29%) were considered as high quality and 17 (30%) were considered low quality. In general, observational studies did not describe sufficiently how sample size was approximated. Almost all high quality studies, except one (3), used antibiotic prescriptions as a primary outcome.
Table 2 presents the antibiotic prescriptions among the five diagnostic groups we distinguished. Sixteen out of 26 descriptive studies focused on febrile children in general, one paper specifically addressed acute otitis media (AOM) (30), two pneumonia (45, 63), four other respiratory infections (RTI other)(19, 23, 43, 57), and one urinary tract infections (UTI)(32). One paper on febrile children also provide separate numbers for pneumonia and UTI (3) and one for AOM (61). Two additional papers focused on respiratory infections and provided separate numbers for pneumonia, AOM and RTI other (44, 56).
Sixteen out of 26 studies focused on febrile children in general, seven of them selected children based on fever without source; five included febrile children based on additional testing (Table 2). In studies of general febrile populations only, antibiotic prescriptions ranged from 15 to 71% (3, 31, 35, 36, 39, 42, 50, 61, 71). The lowest prescriptions (15%) came from a study on parenteral empirical antibiotics only (50). Study quality did not influence antibiotic prescription rate.
Three high quality, six moderate quality and two low quality studies reported on SBI rate, which ranged from 7 to 41% (Figure 2) (3, 26, 35–38, 42, 44, 50, 60, 71). As the SBI rate in Khine et al. (42) is similar to antibiotic prescriptions, one may question how SBI is defined. Massin et al. (50) reports on parenteral antibiotics only and may not represent antibiotic prescription in total. Focusing on the remaining eight studies, we observe a trend toward higher antibiotic prescriptions with higher rates of SBI, although not significant.
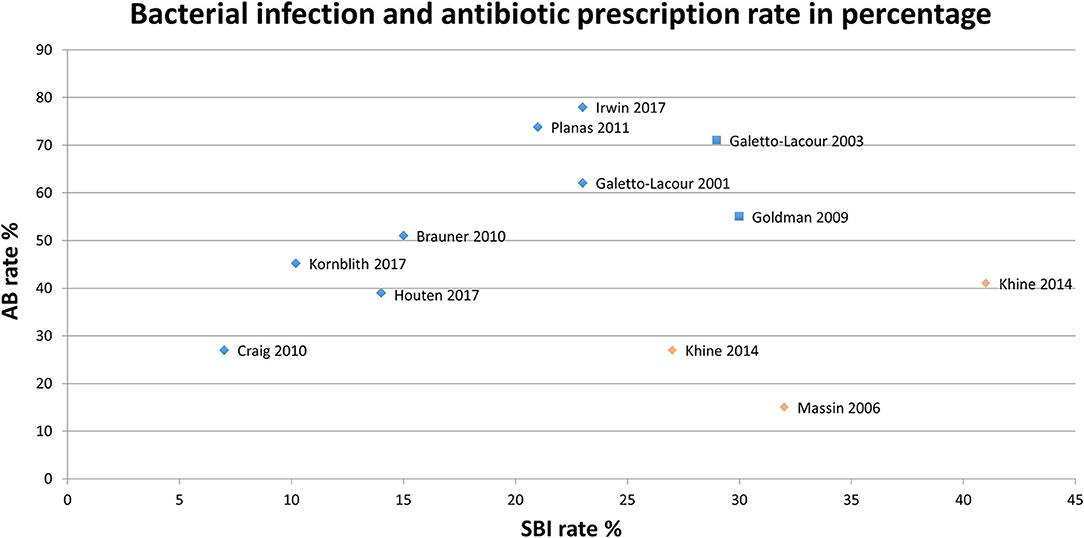
Figure 2. Serious bacterial infection rate and antibiotic prescriptions per study.  High/Moderate quality,
High/Moderate quality,  High/Moderate quality, outlier,
High/Moderate quality, outlier,  Low quality,
Low quality,  Low quality, outlie.
Low quality, outlie.
In the studies on fever in general, we observed a higher prescriptions in children under the age of one (45 to 71%; weighted mean 58%), compared to older ones (prescriptions of 17 to 44%; weighted mean 28%), independent of study quality (Figure 3) (3, 28, 31, 35–37, 39, 42, 50, 71).
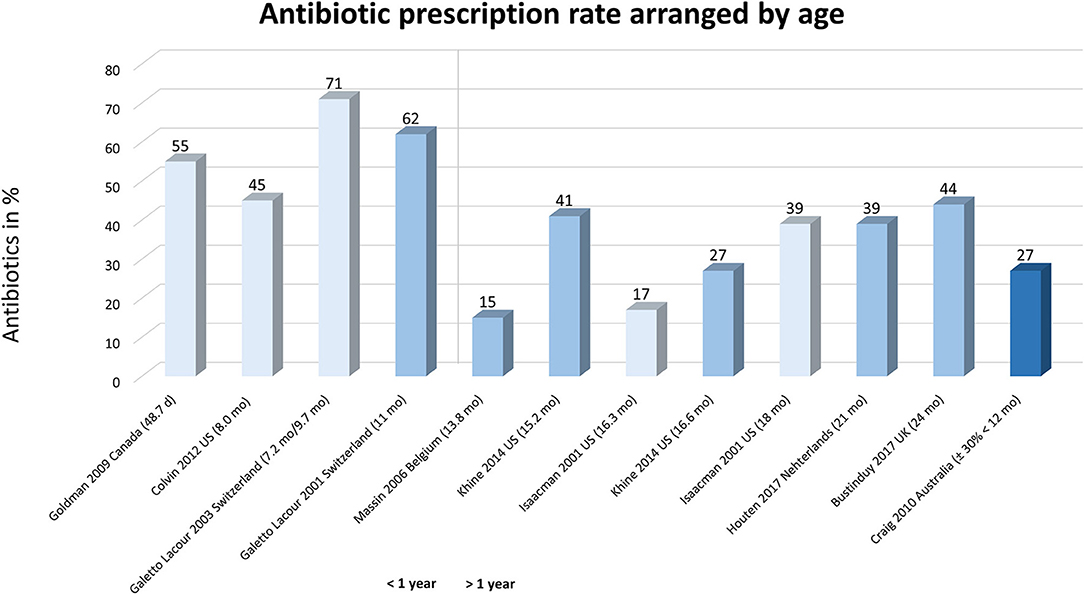
Figure 3. Antibiotic prescriptions arranged on age in children with fever. Studies are arranged by age, i.e., left represents younger children to right (older ages). Light bars represent studies with a low quality.
None of the studies on febrile children in general compared antibiotic prescriptions between countries. In the eleven studies (3, 28, 31, 35–37, 39, 42, 50, 61, 71) on children with fever in general (without additional testing), the highest prescriptions were reported in a Swiss study (71%) (35) and the lowest in a study originating from the US (17%) (39). The three studies originating from the US reported antibiotic prescription between 39–45% (31, 39, 42); for the two Swiss studies this varied from 62 to 71%, although originating from the same hospital (35, 71).
Four studies provided data for antibiotic prescription in AOM, ranging from 88–93%. We could not determine influences of age on prescriptions. Five studies reported on antibiotic prescription in pneumonia, ranging from 69 to 93%. The study with the lowest prescription (3) included children <6 years only compared to the other four (including children in the range of 1-18 years). Antibiotic prescription in RTI other (6 studies) varied on a broader range from 17 to 51%, but could not be related to age. Only two studies provided information on antibiotic prescription in UTI, ranging from 66 to 70%.
Nine out of 26 (35%) studies [two high quality (30, 56)] reported on antibiotic type (Figure 4). Six studies addressed respiratory tract infections (19, 30, 43, 56, 57, 63) and five were conducted in the US (19, 30, 32, 57, 63). We did not observe a predominance for one antibiotic type for a specific diagnosis or country; amoxicillin was always reported. Studies describing cephalosporin use (n = 7) included both second or third generations.
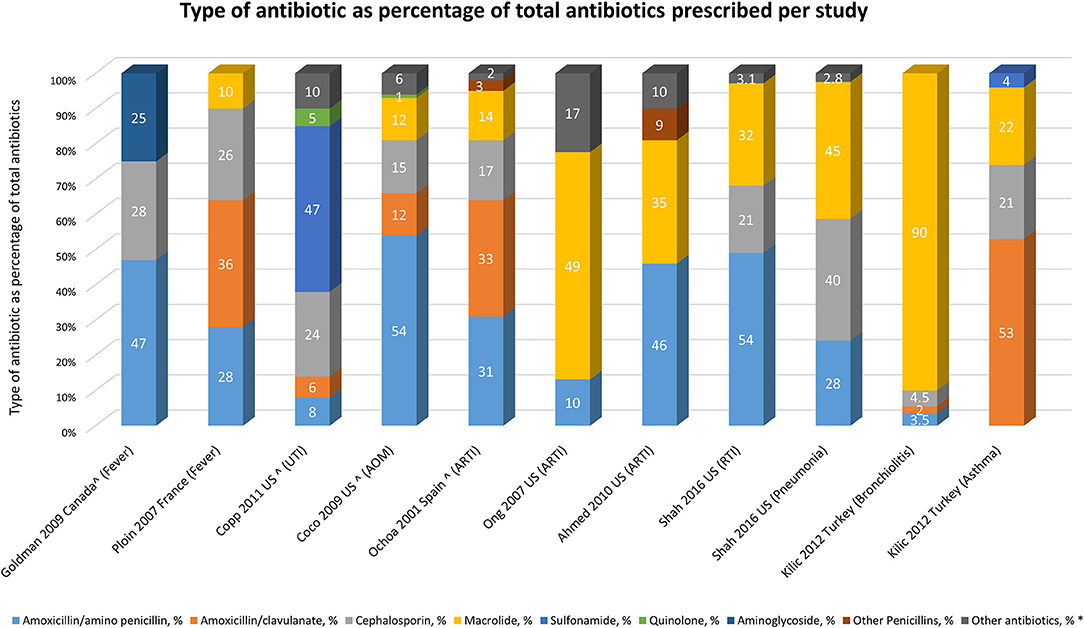
Figure 4. Type of antibiotic as percentage of total antibiotics prescribed per study. *As defined in article. Ahmed et al. (19): not specified; Copp et al. (32): nitrofurantoin and others are not specified antibiotics. Coco et al. (30): not specified. Ochoa et al. (56): trimethoprim/sulfamethoxazole, clindamycin, fosfomycin, rifampin, trimethoprim, topical use and others are not specified. Ong et al. (57): trimethoprim/sulfamethoxazole; Shah et al. (63): not specified. ∧Calculated from article as percentage of total antibiotics, in article given as percentage of cases.
Five (39, 42, 47, 63, 72) out of seven studies [three high quality studies (44, 47, 66)], reported significant lower antibiotic prescriptions by pediatric emergency physicians compared to general emergency physicians (Table 3). Two addressed young children with fever without source (39, 42), and five addressed older children with respiratory tract infections (19, 44, 47, 63, 65).
Nine out of 27 studies on interventions for antibiotic prescription (32%) reported about rapid viral testing (22, 24, 25, 27, 33, 40, 58, 62, 64), four about delayed antibiotic prescription in acute otitis media (29, 34, 52, 66), six about guideline/management strategies (20, 21, 41, 53, 59, 68), four about laboratory tests (22, 46, 47, 49) and five using other interventions (Table 4). In fourteen studies (50%) a significant reduction in antibiotic use was found.
Interventions with a significant effect on antibiotic reduction were guidelines and the wait-and-see prescription in acute otitis media (AOM). For this latter a significant reduction was found in four articles (three of them with moderate to high quality) (29, 34, 52, 66).
Most studies on interventions for reduction of antibiotic prescription addressed rapid viral testing for influenza (RVT, n = 9). Fewer antibiotics were prescribed when the RVT is positive (24, 25, 27, 64), although not confirmed by studies on the impact of RVT use vs. not using RVT in the ED (27, 40, 58, 62). Only one low quality study reported a significant difference for this topic (58). The use of point-of-care testing above testing on indication had only significant benefit in children with proven influenza (33, 48). One study reported reduced length of stay, but no effect on antibiotic prescription (48).
Three high quality studies showed a significant reduction in antibiotic prescription by a guideline for lower respiratory infections or infants with fever (20, 21, 41). Among two articles on streptococcal A testing, the article with the highest quality didn't find a significant reduction (22, 47). Introduction of a clinical pathway for young febrile infants showed reduced time to first antibiotic dose, but did not evaluate the effect on antibiotic prescription itself (53). The use of chest radiographs in particular reduces antibiotics in children with low clinical suspicion of pneumonia (54). For all other interventions no significant reduction was found on antibiotic prescription (46, 49, 65, 69, 70).
We observed a highly variable reported antibiotic prescriptions in children presenting to a general or pediatric ED in the five major groups of diagnosis. Studies on a specific diagnosis, such as AOM, pneumonia, or UTI report higher antibiotic prescriptions. However, studies are too heterogeneous to study true effects of determinants. Strong evidence was found for watchful waiting in AOM and implementation of guidelines for fever or respiratory infections to reduce antibiotic use in the ED. Intervention studies report mostly on rapid viral testing for influenzae (RVT) to reduce antibiotic prescription, but its effect is controversial.
It is important to note that the high variability in antibiotic prescription observed in our systematic review differ from reported antibiotic prescriptions from literature, or websites (12, 73). However, these numbers are based on national or local registries and include in-hospital patients, not reflecting our interest on use of antibiotics in ED settings. Next, not all countries are represented in our systematic review and only Switzerland, USA are represented by more than one study. For the latter two, however we observed high variability in antibiotic prescription within studies of the same country. Even within studies focusing on similar group of diagnoses, we observed a large heterogeneity in their way of patient selection and their type of febrile illness. Therefore, we think these antibiotic prescriptions cannot be considered to be representative for the general population of febrile children in a country.
Limited evidence was found for age effects on antibiotic prescriptions, potentially due to age distribution among study populations. Infants below 2 months are underrepresented in our review. From community studies, we know that pre-school children are more frequently exposed to antibiotic therapy (13).
After exclusion of two outlier studies given their patient selection and outcome definition (42, 50), we observed in studies on children with fever a trend toward higher antibiotic prescriptions in studies with higher SBI rates is noticeable. This, however, only explains some variation in antibiotic prescription.
Similar to studies in primary care, watchful waiting intervention seems highly effective for reducing antibiotic use in AOM at the ED (74). Results however are limited to patients above the age of 6 months that did not appear toxic and it is questionable if the study populations were large enough to detect serious adverse outcomes such as meningitis. Although the most frequently studied intervention, rapid viral testing for influenza has no additional effect above testing on indication and controversial evidence was found for its effect. Effects of guidelines are seen in two well-defined groups (respiratory infections or young febrile infants) and including a well-defined implementation plan. Implementation of a clinical decision model to reduce antibiotic prescriptions was only tested in a tertiary pediatric university ED and antibiotic reduction was not a primary outcome of this study (17). All other interventions are not (yet) proven to be effective for reducing the antibiotic prescriptions in children on the ED. Overall the evidence to reduce antibiotic prescription in the emergency department remains limited. We observed a general association between antibiotic prescription and the type of prescriber, i.e., pediatricians prescribe less antibiotics than general physicians may suggest that guideline implementation could be most effective in hospitals with general physicians treating children in the ED.
The quality of the studies that reported about fever in general was low to moderate, with only one high quality study (3). Specific drawbacks of study design are included in the MINOR assessment as a measure of quality. The use of MINORS in combination with the study population and study aim helps to increase the reproducibility of this review and made it possible to compare the different levels of evidence (16). Most studies did not reported on missing values regarding antibiotic prescription, which could lead to an underestimation of antibiotic prescriptions. In a substantial part of the included papers, antibiotic prescription was not the primary outcome. This may explain some diversity in antibiotic prescriptions, although this was partially corrected for in the quality assessment.
This systematic review focuses on prescription of antibiotics in the ED setting. In many European countries, antibiotics are available as over the counter drugs as well (75). This issue is not accounted for by any of the articles, which may lead to a general underestimation of the antibiotic use.
Unfortunately, we observed a large heterogeneity of the studies or had only 1 study per diagnosis group, hampering meta-analysis. Most heterogeneity is caused by specific patient selection (age, setting), by study design (intervention vs. observational cohort study). This also applies to the population of febrile children <36 months that constitute the majority of ED attendances.
To validly estimate baseline antibiotic prescriptions in children with fever presenting to the emergency department we need observational studies including the general spectrum of febrile children. Being able to determine influences of antibiotic prescription, we should address geographical and cultural influences, differences in setting, adherence area, general patient characteristics, and descriptors of illness severity. Insight in these determinants may help to define targets for intervention to reduce antibiotic prescriptions. Next, this information will contribute to valid power calculations for intervention studies and to generalize effects to other settings.
A summary of studies on antibiotic prescription in the 5 main diagnostic groups at the ED did not yield uniform outcomes. There seems to be a trend toward higher antibiotic prescriptions in younger children and for diagnoses that are more often related to bacterial infections. Delayed antibiotic prescription in children with acute otitis media and guidelines for fever/LRTI seem useful to reduce antibiotic prescriptions at the ED. However no strict conclusions can be drawn on the basis of this review because of the large heterogeneity of type of studies and included populations. This means that there is still a gap in knowledge on the determining factors that influence antibiotic prescription in febrile children presenting to the ED. A multicentre study including a wide range of countries on a general population of febrile children would be recommended to provide a valid baseline of antibiotic prescriptions in general, and influencing factors that identify targets for future interventions.
EvdV was responsible for search, dataextraction and writing of the manuscript. HM, SM, and AG contributed to datainterpretation and writing of the manuscript. RO concepted the idea of the paper, supervised search, dataextraction, and writing of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2018.00260/full#supplementary-material
AB, antibiotic(s); AOM, acute otitis media; ARS, acute respiratory symptoms; ARTI, acute respiratory tract infection; BC, blood culture; CAP, community acquired pneumonia; CC, case control study; CI, confidence interval; CP, cohort study, prospective; CR, cohort study, retrospective; CS, cross sectional study; CSF, cerebrospinal fluid; d, days; ED, emergency department; EL, extreme leukocytosis; FWS, fever without source; GED, general emergency department; GEMP, general emergency medicine physician; ILI, influenza-like illness; ML, moderate leukocytosis; mo, months; NR, not reported; NS, not specified; PED, pediatric emergency department; PEMP, pediatric emergency medicine physician; qRCT, quasi-randomized controlled trial; RCT, randomized controlled trial; reg, registration; RIDT, rapid influenza diagnostic tests; RST, rapid streptococcal test; RVT, rapid viral testing; SBI, serious bacterial infection; SD, standard deviation; T, temperature; URTI, upper respiratory tract infection; UTI, urinary tract infection; y, years.
1. Fields E, Chard J, Murphy MS, Richardson M, Guideline Development G, Technical T. Assessment and initial management of feverish illness in children younger than 5 years: summary of updated NICE guidance. BMJ (2013) 346:f2866. doi: 10.1136/bmj.f2866
2. Nijman RG, Vergouwe Y, Thompson M, van Veen M, van Meurs AH, van der Lei J, et al. Clinical prediction model to aid emergency doctors managing febrile children at risk of serious bacterial infections: diagnostic study. BMJ (2013) 346:f1706. doi: 10.1136/bmj.f1706
3. Craig JC, Williams GJ, Jones M, Codarini M, Macaskill P, Hayen A, et al. The accuracy of clinical symptoms and signs for the diagnosis of serious bacterial infection in young febrile children: Prospective cohort study of 15 781 febrile illnesses. BMJ (2010) 340:1015. doi: 10.1136/bmj.c1594
4. Brett A, Bielicki J, Newland JG, Rodrigues F, Schaad UB, Sharland M. Neonatal and pediatric antimicrobial stewardship programs in europe - defining the research agenda. Pediatr Infect Dis J. (2013) 32:e456–65. doi: 10.1097/INF.0b013e31829f0460
5. Otters HB, van der Wouden JC, Schellevis FG, van Suijlekom-Smit LW, Koes BW. Trends in prescribing antibiotics for children in Dutch general practice. J Antimicrob Chemother. (2004) 53:361–6. doi: 10.1093/jac/dkh062
6. Blair PS, Turnbull S, Ingram J, Redmond N, Lucas PJ, Cabral C, et al. Feasibility cluster randomised controlled trial of a within-consultation intervention to reduce antibiotic prescribing for children presenting to primary care with acute respiratory tract infection and cough. BMJ Open. (2017) 7:e014506. doi: 10.1136/bmjopen-2016-014506
7. Stille CJ, Rifas-Shiman SL, Kleinman K, Kotch JB, Finkelstein JA. Physician responses to a community-level trial promoting judicious antibiotic use. Ann Fam Med. (2008) 6:206–12. doi: 10.1370/afm.839
8. Meeker D, Linder JA, Fox CR, Friedberg MW, Persell SD, Goldstein NJ, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: a randomized clinical trial. JAMA (2016) 315:562–70. doi: 10.1001/jama.2016.0275
9. Davey P, Brown E, Charani E, Fenelon L, Gould IM, Holmes A, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev. (2013) 2:CD003543. doi: 10.1002/14651858.CD003543.pub4
10. Lieberman JM. Appropriate antibiotic use and why it is important: the challenges of bacterial resistance. Pediatr Infect Dis J. (2003) 22:1143–51. doi: 10.1097/01.inf.0000101851.57263.63
11. Versporten A, Sharland M, Bielicki J, Drapier N, Vankerckhoven V, Goossens H, et al. The antibiotic resistance and prescribing in European Children project: a neonatal and pediatric antimicrobial web-based point prevalence survey in 73 hospitals worldwide. Pediatr Infect Dis J. (2013) 32:e242–53. doi: 10.1097/INF.0b013e318286c612
12. Molstad S, Lundborg CS, Karlsson AK, Cars O. Antibiotic prescription rates vary markedly between 13 European countries. Scand J Infect Dis. (2002) 34:366–71. doi: 10.1080/00365540110080034
13. Rossignoli A, Clavenna A, Bonati M. Antibiotic prescription and prevalence rate in the outpatient paediatric population: analysis of surveys published during 2000–2005. Eur J Clin Pharmacol. (2007) 63:1099–106. doi: 10.1007/s00228-007-0376-3
14. Ryan J, Greene SK, Kleinma KP, Lakoma MD. Trends in antibiotic use in massachusetts children, 2000-2009. J Emerg Med. (2012) 43:e381. doi: 10.1016/j.jemermed.2012.09.009
15. Van Boeckel TP, Gandra S, Ashok A, Caudron Q, Grenfell BT, Levin SA, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis. (2014) 14:742–50. doi: 10.1016/S1473-3099(14)70780-7
16. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. (2003) 73:712–6. doi: 10.1046/j.1445-2197.2003.02748.x
17. de Vos-Kerkhof E, Geurts DH, Wiggers M, Moll HA, Oostenbrink R. Tools for 'safety netting' in common paediatric illnesses: a systematic review in emergency care. Arch Dis Child. (2016) 101:131–9. doi: 10.1136/archdischild-2014-306953
18. van Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review G. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (2003) 28:1290–9. doi: 10.1097/01.BRS.0000065484.95996.AF
19. Ahmed MN, Muyot MM, Begum S, Smith P. Antibiotic prescription pattern for viral respiratory illness in emergency room and ambulatory care settings. Clin Pediatr. (2010). 49:452–7. doi: 10.1177/0009922809357786
20. Angoulvant F, Skurnik D, Bellanger H, Abdoul H. Impact of implementing French antibiotic guidelines for acute respiratory-tract infections in a paediatric emergency department, 2005–2009. Eur J Ofin Microbiol Infect Dis. (2011) 31:1295–303. doi: 10.1007/s10096-011-1442-4
21. Aronson PL, Thurm C, Williams DJ, Nigrovic LE, Alpern ER, Tieder JS, et al. Association of clinical practice guidelines with emergency department management of febrile infants ≤ 56 days of age. J Hosp Med. (2015) 10:358–65. doi: 10.1002/jhm.2329
22. Ayanruoh S, Waseem M, Quee F. Impact of rapid streptococcal test on antibiotic use in a pediatric emergency department. Ped Emerg Care (2009) 25:748–50. doi: 10.1097/PEC.0b013e3181bec88c
23. Benin AL, Vitkauskas G, Thornquist E, Shiffman RN, Concato J, Krumholz HM, et al. Improving diagnostic testing and reducing overuse of antibiotics for children with pharyngitis: a useful role for the electronic medical record. Pediatric Infect Dis J. (2003) 22:1043–7. doi: 10.1097/01.inf.0000100577.76542.af
24. Benito-Fernandez J, Vazquez-Ronco MA, Morteruel-Aizkuren E, Mintegui-Raso S, Sanchez-Etxaniz J, Fernandez-Landaluce A. Impact of rapid viral testing for influenza A and B viruses on management of febrile infants without signs of focal infection. Pediatr Infect Dis J. (2006) 25:1153–7. doi: 10.1097/01.inf.0000246826.93142.b0
25. Blaschke AJ, Shapiro DJ, Pavia AT, Byington CL, Ampofo K, Stockmann C, et al. A national study of the impact of rapid influenza testing on clinical care in the emergency department. J Pediatric Infect Dis Soc. (2014) 3:112–8. doi: 10.1093/jpids/pit071
26. Brauner M, Goldman M, Kozer E. Extreme leucocytosis and the risk of serious bacterial infections in febrile children. Arch Dis Childhood. (2010) 95:209–12. doi: 10.1136/adc.2009.170969
27. Bonner AB, Monroe KW, Talley LI, Klasner AE, Kimberlin DW. Impact of the rapid diagnosis of influenza on physician decision-making and patient management in the pediatric emergency department: results of a randomized, prospective, controlled trial. Pediatrics (2003) 112:363–7. doi: 10.1542/peds.112.2.363
28. Bustinduy AL, Chis Ster I, Shaw R, Irwin A, Thiagarajan J, Beynon R, et al. Predictors of fever-related admissions to a paediatric assessment unit, ward and reattendances in a South London emergency department: the CABIN 2 study. Arch Dis Child. (2017) 102:22–8. doi: 10.1136/archdischild-2016-310494
29. Chao JH, Kunkov S, Reyes LB, Lichten S, Crain EF. Comparison of two approaches to observation therapy for acute otitis media in the emergency department. Pediatrics (2008) 121:1352–6. doi: 10.1542/peds.2007-2278
30. Coco AS, Horst MA, Gambler AS. Trends in broad-spectrum antibiotic prescribing for children with acute otitis media in the United States, 1998-2004. BMC Pediatr. (2009) 9:41. doi: 10.1186/1471-2431-9-41
31. Colvin JM, Muenzer JT, Jaffe DM, Smason A, Deych E, Shannon WD, et al. Detection of viruses in young children with fever without an apparent source. Pediatrics (2012) 130:e1455–e62. doi: 10.1542/peds.2012-1391
32. Copp HL, Shapiro DJ, Hersh AL. National ambulatory antibiotic prescribing patterns for pediatric urinary tract infection, 1998-2007. Pediatrics (2011) 127:1027–33. doi: 10.1542/peds.2010-3465
33. Doan QH, Kissoon N, Dobson S, Whitehouse S, Cochrane D, Schmidt B, et al. A randomized, controlled trial of the impact of early and rapid diagnosis of viral infections in children brought to an emergency department with febrile respiratory tract illnesses. J Pediatr. (2009) 154:91–5. doi: 10.1016/j.jpeds.2008.07.043
34. Fischer T, Singer AJ, Chale S. Observation option for acute otitis media in the emergency department. Pediatr Emerg Care (2009) 25:575–8. doi: 10.1097/PEC.0b013e3181b91ff0
35. Galetto-Lacour A, Zamora SA, Gervaix A. Bedside procalcitonin and C-reactive protein tests in children with fever without localizing signs of infection seen in a referral center. Pediatrics (2003) 112:1054–60 doi: 10.1542/peds.112.5.1054
36. Goldman RD, Scolnik D, Chauvin-Kimoff L, Farion KJ, Ali S, Lynch T, et al. Practice variations in the treatment of febrile infants among pediatric emergency physicians. Pediatrics (2009) 124:439–45. doi: 10.1542/peds.2007-3736
37. van Houten CB, de Groot JAH, Klein A, Srugo I, Chistyakov I, de Waal W, et al. A host-protein based assay to differentiate between bacterial and viral infections in preschool children (OPPORTUNITY): a double-blind, multicentre, validation study. Lancet Infect Dis. (2017) 17:431–40. doi: 10.1016/S1473-3099(16)30519-9
38. Irwin AD, Grant A, Williams R, Kolamunnage-Dona R, Drew RJ, Paulus S, et al. Predicting risk of serious bacterial infections in febrile children in the emergency department. Pediatrics (2017) 140:e20162853. doi: 10.1542/peds.2016-2853
39. Isaacman DJ, Kaminer K, Veligeti H, Jones M, Davis P, Mason JD. Comparative practice patterns of emergency medicine physicians and pediatric emergency medicine physicians managing fever in young children. Pediatrics (2001) 108:354–8. doi: 10.1542/peds.108.2.354
40. Iyer SB, Gerber MA, Pomerantz WJ, Mortensen JE, Ruddy RM. Effect of point-of-care influenza testing on management of febrile children. Acad Emerg Med. (2006) 13:1259–68. doi: 10.1197/j.aem.2006.07.026
41. Jain S, Frank G, McCormick K, Wu B, Johnson BA. Impact of physician scorecards on emergency department resource use, quality, and efficiency. Pediatrics (2015) 136:e670–e9. doi: 10.1542/peds.2014-2363
42. Khine H, Goldman DL, Avner JR. Management of fever in postpneumococcal vaccine era: comparison of management practices by pediatric emergency medicine and general emergency medicine physicians. Emerg Med Int. (2014) 2014:702053. doi: 10.1155/2014/702053
43. Kilic A, Unuvar E, Sutcu M, Suleyman A, Tamay Z, Yildiz I, et al. Acute obstructive respiratory tract diseases in a pediatric emergency unit: Evidence-based evaluation. Pediatr Emerg Care (2012) 28:1321–7. doi: 10.1097/PEC.0b013e3182768d17
44. Kornblith AE, Fahimi J, Kanzaria HK, Wang RC. Predictors for under-prescribing antibiotics in children with respiratory infections requiring antibiotics. Am J Emerg Med. (2018) 36:218–25. doi: 10.1016/j.ajem.2017.07.081
45. Kronman MP, Hersh AL, Feng R, Huang YS. Ambulatory visit rates and antibiotic prescribing for children with pneumonia, 1994–2007. Pediatrics (2011) 127:411–18. doi: 10.1542/peds.2010-2008
46. Lacroix L, Manzano S, Vandertuin L, Hugon F, Galetto-Lacour A, Gervaix A. Impact of the lab-score on antibiotic prescription rate in children with fever without source: a randomized controlled trial. PLoS ONE (2014) 9:e0115061. doi: 10.1371/journal.pone.0115061
47. Linder JA, Bates DW, Lee GM, Finkelstein JA. Antibiotic treatment of children with sore throat. JAMA (2005) 294:2315–22. doi: 10.1001/jama.294.18.2315
48. Li-Kim-Moy J, Dastouri F, Rashid H, Khandaker G, Kesson A, McCaskill M, et al. Utility of early influenza diagnosis through point-of-care testing in children presenting to an emergency department. J Paediatr Child Health (2016) 52:422–9. doi: 10.1111/jpc.13092
49. Manzano S, Bailey B, Girodias JB, Galetto-Lacour A, Cousineau J, Delvin E. Impact of procalcitonin on the management of children aged 1 to 36 months presenting with fever without source: a randomized controlled trial. Am J Emerg Med. (2010) 28: 647–53. doi: 10.1016/j.ajem.2009.02.022
50. Massin MM, Montesanti J, Lepage P. Management of fever without source in young children presenting to an emergency room. Acta Paediatr Int J Paediatr. (2006) 95:1446–50. doi: 10.1080/08035250600669751
51. McCaig LF, McDonald LC, Cohen AL, Kuehnert MJ. Increasing blood culture use at US Hospital Emergency Department visits, 2001 to 2004. Ann Emerg Med. (2007) 50:42–48.e2 doi: 10.1016/j.annemergmed.2006.12.002
52. McCormick DP, Chonmaitree T, Pittman C, Saeed K. Nonsevere acute otitis media: a clinical trial comparing outcomes of watchful waiting versus immediate antibiotic treatment. Am Acad Pediatrics (2005) 115:1455–65. doi: 10.1542/peds.2004-1665
53. Murray AL, Alpern E, Lavelle J, Mollen C. Clinical pathway effectiveness: febrile young infant clinical pathway in a pediatric emergency department. Pediatr Emerg Care (2017) 33:e33–e7. doi: 10.1097/PEC.0000000000000960
54. Nelson KA, Morrow C, Wingerter SL, Bachur RG, Neuman MI. Impact of chest radiography on antibiotic treatment for children with suspected pneumonia. Pediatr Emerg Care (2016) 32:514–9. doi: 10.1097/PEC.0000000000000868
55. Nibhanipudi KV, Hassan GW, Jain A. The utility of peripheral white blood cell count in cases of acute otitis media in children between 2 years and 17 years of age. Int J Otorhinolaryngol. (2016) 18. doi: 10.5580/IJORL.38086
56. Ochoa C, Inglada L, Eiros JM, Solis G, Vallano A, Guerra L, et al. Appropriateness of antibiotic prescriptions in community-acquired acute pediatric respiratory infections in Spanish emergency rooms. Pediatr Infect Dis J. (2001) 20:751–8. doi: 10.1097/00006454-200108000-00007
57. Ong S, Nakase J, Moran GJ, Karras DJ. Antibiotic use for emergency department patients with upper respiratory infections: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med. (2007) 50:213–20. doi: 10.1016/j.annemergmed.2007.03.026
58. Ozkaya E, Cambaz N, Coskun Y, Mete F, Geyik M, Samanci N. The effect of rapid diagnostic testing for influenza on the reduction of antibiotic use in paediatric emergency department. Acta Paediatr Int J Paediatr. (2009) 98:1589–92. doi: 10.1111/j.1651-2227.2009.01384.x
59. Ouldali N, Bellettre X, Milcent K, Guedj R, de Pontual L, Cojocaru B, et al. Impact of implementing national guidelines on antibiotic prescriptions for acute respiratory tract infections in pediatric emergency departments: an interrupted time series analysis. Clin Infect Dis. (2017) 65:1469–76. doi: 10.1093/cid/cix590
60. Planas AM, Almagro CM, Cubells CL, Julian AN, Selva L, Fernandez JP, et al. Low prevalence of invasive bacterial infection in febrile infants under 3 months of age with enterovirus infection. Clin Microbiol Infect. (2012) 18:856–61. doi: 10.1111/j.1469-0691.2011.03671.x
61. Ploin D, Gillet Y, Morfin F, Fouilhoux A, Billaud G, Liberas S, et al. Influenza burden in febrile infants and young children in a pediatric emergency department. Pediatr Infect Dis J. (2007) 26:142–7. doi: 10.1097/01.inf.0000253062.41648.60
62. Poehling KA, Zhu Y, Tang YW, Edwards K. Accuracy and impact of a point-of-care rapid influenza test in young children with respiratory illnesses. Arch Pediatr Adolesc Med. (2006) 160:713–8. doi: 10.1001/archpedi.160.7.713
63. Shah S, Bourgeois F, Mannix R, Nelson K, Bachur R, Neuman MI. Emergency department management of febrile respiratory illness in children. Pediatr Emerg Care (2016) 32:429–34. doi: 10.1097/PEC.0000000000000721
64. Sharma V, Denise Dowd M, Slaughter AJ, Simon SD. Effect of rapid diagnosis of influenza virus type A on the emergency department management of febrile infants and toddlers. Arch Pediatr Adolesc Med. (2002) 156:41–3. doi: 10.1001/archpedi.156.1.41
65. Spiro DM, King WD, Arnold DH, Johnston C, Baldwin S. A randomized clinical trial to assess the effects of tympanometry on the diagnosis and treatment of acute otitis media. Pediatrics (2004) 114:177–81. doi: 10.1542/peds.114.1.177
66. Spiro DM, Tay KY, Arnold DH, Dziura JD, Baker MD, Shapiro ED. Wait-and-see prescription for the treatment of acute otitis media: a randomized controlled trial. J Am Med Assoc. (2006) 296:1235–41. doi: 10.1001/jama.296.10.1235
67. Trautner BW, Caviness AC, Gerlacher GR. Prospective evaluation of the risk of serious bacterial infection in children who present to the emergency department with hyperpyrexia (temperature of 106 F or higher). Pediatrics (2006) 118:34–40. doi: 10.1542/peds.2005-2823
68. de Vos-Kerkhof E, Nijman RG, Vergouwe Y, Polinder S, Steyerberg EW, van der Lei J, et al. Impact of a clinical decision model for febrile children at risk for serious bacterial infections at the emergency department: a randomized controlled trial. PLoS ONE (2015) 10:e0127620. doi: 10.1371/journal.pone.0127620
69. Waddle E, Jhaveri R. Outcomes of febrile children without localising signs after pneumococcal conjugate vaccine. Arch Dis Child. (2008) 94:144–7. doi: 10.1136/adc.2007.130583
70. Wheeler JG, Fair M, Simpson PM, Rowlands LA. Impact of a waiting room videotape message on parent attitudes toward pediatric antibiotic use. Pediatrics (2001) 108:591–6. doi: 10.1542/peds.108.3.591
71. Lacour AG, Zamora SA, Vadas L, Lombard PR, Dayer JM, et al. Procalcitonin, IL-6, IL-8, IL-1 receptor antagonist and C-reactive protein as identificators of serious bacterial infections in children with fever without localising signs. Eur J Pediatr. (2001) 160:95–100.
72. Ahmed A, Brito F, Goto C, Hickey SM, Olsen KD, Trujillo M, et al. Clinical utility of the polymerase chain reaction for diagnosis of enteroviral meningitis in infancy. J Pediatr. (1997) 131:393–7. doi: 10.1016/S0022-3476(97)80064-9
73. The Center for Disease DynamicsEconomy and Policy. Antibiotic Prescribing Rates by Country. Available online at: www.cddep.org (Accessed July 20, 2018).
74. Tyrstrup M, Beckman A, Molstad S, Engstrom S, Lannering C, Melander E, et al. Reduction in antibiotic prescribing for respiratory tract infections in Swedish primary care-a retrospective study of electronic patient records. BMC Infect Dis. (2016) 16:709. doi: 10.1186/s12879-016-2018-9
Keywords: pediatric emergency care, fever, children, antibiotic prescription, management
Citation: van de Voort EMF, Mintegi S, Gervaix A, Moll HA and Oostenbrink R (2018) Antibiotic Use in Febrile Children Presenting to the Emergency Department: A Systematic Review. Front. Pediatr. 6:260. doi: 10.3389/fped.2018.00260
Received: 28 June 2018; Accepted: 31 August 2018;
Published: 08 October 2018.
Edited by:
Cristiana Nascimento-Carvalho, Universidade Federal da Bahia, BrazilReviewed by:
Adriana Yock-Corrales, Dr. Carlos Sáenz Herrera National Children's Hospital, Costa RicaCopyright © 2018 van de Voort, Mintegi, Gervaix, Moll and Oostenbrink. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rianne Oostenbrink, ci5vb3N0ZW5icmlua0BlcmFzbXVzbWMubmw=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.