
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Pain Res. , 05 February 2025
Sec. Non-Pharmacological Treatment of Pain
Volume 6 - 2025 | https://doi.org/10.3389/fpain.2025.1463321
This article is part of the Research Topic Non-biomedical Perspectives on Pain and its Prevention and Management – Volume II View all 3 articles
 Justyna Świdrak1,2*
Justyna Świdrak1,2*
Fibromyalgia is called a pathology of misconnection at the neurophysiological, psychological, and social levels, and is characterised by widespread musculoskeletal pain, which is accompanied by a series of symptoms, such as chronic fatigue, depression, anxiety, body perception disturbances, and cognitive deficits. In this article, I argue that interventions that in various ways enhance interpersonal neural synchronisation (INS) may bring long-term benefits to people with fibromyalgia (PwF). In the first part, I briefly introduce studies on INS in the general population. In the second part, I hypothesise that interpersonal synchrony may contribute to symptom reduction for individuals with fibromyalgia, in the sense that repeated experience of being in sync with others may play a role in restoring both the brain-body and self-others connection in this population and consequently result in simultaneous lasting improvement of wellbeing. In the final part, I discuss potential future research directions.
With one in ten adults diagnosed each year (1), chronic pain is one of the major health challenges in the world. It has a detrimental effect not only on the wellbeing of those who suffer from it (2), but also on their social and family environment (3, 4). These consequences are evident in fibromyalgia, the most common central sensitivity syndrome, characterised by a combination of symptoms known as FIBRO: Fatigue and Fog (cognitive dysfunction), Blues (depression, anxiety) Rigidity (stiffness), and “Ow!” (chronic pain, tenderness) (5). It is “a pathology of misconnection” at the neurophysiological, psychological, and social levels. Perrot (6) observed that due to its invisibility and lack of a specific biomarker, people with fibromyalgia (PwF) are disconnected from society. They are also disconnected internally due to the complex pathophysiology that leads to a desynchronisation of the brain and body. Consequently, the recommended treatments aim to restore good connections (6). Essential pain symptoms are related to augmented sensory processing (central sensitisation) and an inability to modulate pain effectively (7). I argue that interventions that in various ways enhance interpersonal neural synchronisation (INS) may facilitate a simultaneous body-brain and self-other reconnection and bring long-term benefits to PwF. In this paper, I will briefly introduce studies on INS in the general population and explain its potential role in the treatment of widespread chronic musculoskeletal pain in the context of existing evidence.
After studying human cognition in isolated individuals (single-brain studies), in the last two decades the interest of social neuroscientists has been shifting towards second-person neuroscience thanks to advances in hyperscanning. This is a simultaneous measurement of more than one person's neural activity (dual-brain studies) (8). Hyperscanning studies led to a discovery of INS which can be defined as a phenomenon “that promotes social interactions by enabling functional integration of multiple brains” (9, 354). Despite its short history, second-person neuroscience has already provided sophisticated theoretical frameworks which attempt to explain the interplay of inter- and intrabrain networks, for example, the hypothesis of hyperbrain cell assembly (10), the plasticity of the interbrain (11), the two-body joint forward model for interpersonal action coordination (12). Another interesting approach is the embodied mutual prediction theory which states that the coherence of neural signals between two brains can arise during a social interaction between two people as their brains simultaneously control own actions and mutually predict each other's actions (13). Importantly, interbrain coherence should not be investigated in isolation from the body, but as a process simultaneously happening on behavioural, psychophysiological, and neural level. These levels need to be analysed jointly, as visual, auditory, and motor processes mediate any coordination between two brains (Figure 1) (14).
Syncing with others leads to an increased predictability of incoming signals which offers many benefits ranging from basic information processing at the individual level to the bonding of dyads and larger groups (15, 16). Furthermore, synchrony increases cooperation (17), social connection, and improves affect (18). It is associated with self-other overlap (19), which also reduces sensitivity to own bodily pain (20) and increases empathy for the pain of others (21). Interpersonal synchrony during touch can potentially reduce acute pain (22). Thus, synchrony tends to feel good and creates a sense of connection (23). I argue that looking at complex chronic pain conditions such as fibromyalgia through a lens of embodied INS offers an exciting opportunity to reinterpret existing evidence and open new research pathways. I hypothesise that interpersonal synchrony can be healing for PwF, in the sense that repeated experience of being in sync with others may play a role in restoring both the brain-body and self-others connection in this population and consequently result in simultaneous lasting improvement of several key symptoms, such as pain, depression, anxiety, and attention deficits (Figure 2).
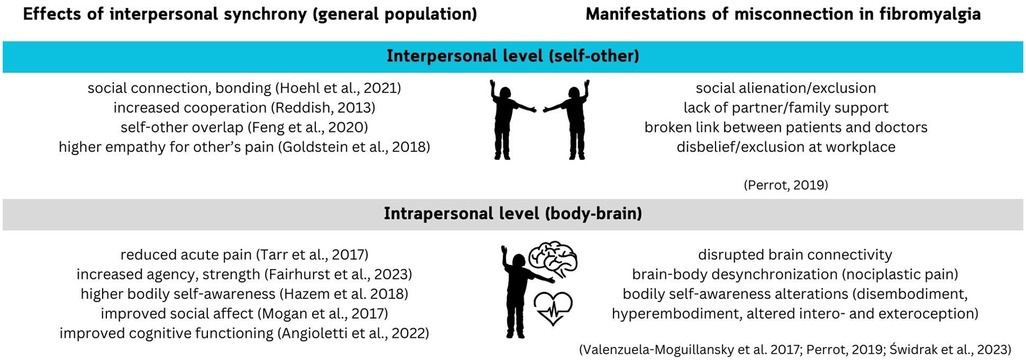
Figure 2. Effects of interpersonal synchrony on typical adults (left) compared to misconnection observed in fibromyalgia (right).
Similarly to the second-person social neuroscience, a recent shift from the first- to the second-person perspective of the bodily self can be observed (24, 25). The bodily self originates from the multisensory integration of bodily-related signals, with the motor systems playing a key role (26). The social self links the bodily self with that of others (27). It plays a fundamental role in the constitution of the other as another self. It seems that this connection is bidirectional, as there is evidence that social contact enhances bodily self-awareness (28, 29). At the same time, interpersonal synchrony is also known to blur self-other boundaries (30), which may lead to the weakening of affective self-regulation (23). This perspective helps to understand the relationships between a broken brain-body connection, as observed in PwF (31) and the social alienation of this population (3).
According to the sensorimotor theory of pain, changes in sensorimotor processing, especially motor deficits, sensory changes, and body representation distortions, may be a reason for persistent pain (32). Chronic pain often includes not only continuous nociceptive stimulation, but also multiple sensorimotor distortions that lead to a disrupted body experience (33), including distortions in body image (perceiving own body as a physical object with its size and shape) and body schema (representation of a body for action planning and control) (34). Pain is a fundamentally social experience, because it challenges basic human needs, such as the need for autonomy, the need to belong, and the need for justice/fairness (35). People diagnosed with fibromyalgia indeed often struggle with fulfilling these needs as they are commonly alienated, discriminated, and disbelieved by others when discussing their symptoms. This experience of a broken social bodily self manifests in perceiving their bodies as a barrier to the social world, leading to a disruption of a basic sense of being with others (36).
Simple social contact, such as direct gaze, improves bodily self-awareness (28, 29). Furthermore, focussing on its one's own physiological processes during a socially framed task that requires motor synchronisation “boosts” the hemodynamic correlates in the regions of the brain that support sustained attention, reorientation of attention, social responsiveness, and synchronisation (37), cognitive functions often disturbed in fibromyalgia (38, 39). One of the best examples of a recurring embodied social interaction aimed at improving the broken body-mind and social connections is psychotherapy. Therapeutic alliance – the bond between the therapist and the patient/client built throughout the therapeutic process – is one of the main drivers of therapy success (40). There is a growing body of evidence that this success positively correlates with movement synchrony between therapists and patients (41). Furthermore, a review by Sened, Zilcha-Mano, and Shamay-Tsoory (42) indicates that high interbrain coherence is associated with better relationships in both therapy and in daily life, while deficits in the ability to achieve interbrain synchrony are associated with a variety of psychological and developmental disorders. Affective symptoms, such as depression and anxiety, are extremely common in fibromyalgia, and psychotherapy is a central element of many interdisciplinary treatment programs (43). Indeed, evidence indicates that various psychotherapeutic treatments obtain positive effects in short-, mid-, and even long-term (44–48). Interestingly, a comparison of group therapy alone and multidisciplinary programs which contained group therapy demonstrated that the latter are only slightly more effective in reducing primary and secondary symptoms of fibromyalgia (49).
Following this pathway, we can speculate that social interactions that simultaneously promote spontaneous synchronisation with others and a concentration on own bodily signals, such as psychotherapy, yoga and other mind-body activities, may facilitate reconnecting brain-body processing, particularly in the motor and prefrontal areas (50).
The broken connection between PwF and their social networks often leads to loneliness and depression, and therefore more social and family-orientated research initiatives are recommended (4). Regular physical activity is one of the pillars of the treatment of fibromyalgia, due to its multiple positive influences, including improved mood and sleep quality, raising pain thresholds, breaking the vicious cycle of pain-inactivity-pain, and reducing physical deconditioning (51, 52). Thus, the only “strong” EULAR1 recommendation for PwF is exercise (53). Adherence to exercise programmes in chronic pain treatment is the key to their efficiency, but it varies significantly (54), and can be improved by implementing a social component in the programme (55).
One of the most beneficial types of physical activity for PwF is dance. Dance reduces musculoskeletal pain and dance therapy is recommended as an effective addition to the treatment of chronic pain (56), including fibromyalgia, with PwF who dance report lower depression, anxiety and kinesiophobia (fear of movement), and dance-based interventions effects described as large (57, 58). Zumba dance, compared to treadmill walking and control groups, also improves cognitive functioning (59). According to the Synchronicity Hypothesis of Dance, humans dance to enhance both intra- and interbrain synchrony (60). Dance engages both interoceptive and exteroceptive processes, in addition to the haptic, visual, and auditory processing, which influence group synchrony, with haptic coupling having the most general effect on synchrony during group dancing (61). Exertive and synchronised movement modulates pain and may be an effective group bonding activity (20). For example, in a nine-month group exercise programme, participants reported that the social connections created within the group helped them reduce isolation, frustration, and depression (55). These results are in line with the literature on movement synchrony, as moving in sync with others makes us happier and more connected. For example, in a study in which participants were walking together, greater coordination resulted in greater feelings of agency, strength, and happiness (15). Such synchronisation also occurs implicitly, since humans tend to sync their movements with others (15, 62).
Interpersonal synchrony occurs in many contexts, and not everyone finds group dance or yoga attractive. Paying more attention to personal factors in pain management interventions by including activities that, for example, offer enjoyable and meaningful connections within one's social networks, could lead to improvements in physical and psychological well-being (63). Thus, it may be useful to study INS in people with chronic pain also during other types of social learning, such as learning to play music together with others or playing collaborative games (64).
To the best knowledge of the author, there have been no studies on INS in people with widespread chronic pain. Therefore, this paper aims to spark interest in the pain research community in the role of interpersonal synchrony in chronic pain treatment. Importantly, the field of INS research is still relatively young and thus, faces the challenges of defining INS and forming a uniform theoretical framework which would explain the effects described in the literature (9). Therefore, one may only speculate on the precise role of INS in the alleviation of fibromyalgia symptoms and the restoration of the social bodily self. There are various types of interpersonal synchrony, and thus, the mechanisms underlying its health benefits in each case may vary. Nonetheless, one may suspect that recurringly switching attention from internal, painful to external, social stimuli could play a role in reducing the attentional bias towards painful stimuli, typical for PwF (65). Additionally, the health benefits may come from improved interoception, as social contact improves bodily self-awareness (29, 37). At last, may INS-enhancing activities feel good and make people bond (20, 23), which may improve psychological symptoms in PwF, who often suffer from social alienation and loneliness (66).
Among multiple ways forward, two main research pathways are emerging, related to (1) describing the mechanisms of INS in people diagnosed with fibromyalgia (and chronic pain in general), and (2) its potential role of modulating symptoms.
The first pathway to validate the proposed hypothesis would be to investigate whether such synchrony occurs similarly to the general population, and if not, what are the differences. For example, do higher pain levels impede INS, as one becomes too overwhelmed with their own bodily signals to direct their attention toward others? What types of activity evoke INS in PwF?
The second pathway is related to the modulating effect of interpersonal synchrony. In what circumstances can being with others distract someone from their own pain and other symptoms? Could such INS-inducing interventions help modulate fibromyalgia symptoms and which symptoms should be targeted? What frequency and duration are needed to observe the alleged benefits? These are just a few of multiple questions that need to be answered to establish what role INS can play in fibromyalgia treatment and, more broadly, chronic pain management.
There are also several important challenges that need to be addressed. First, although significant progress has been made in the last decade (51), the underlying mechanisms of fibromyalgia itself are very complex and not fully understood, leading to a large heterogeneity of the population due to diagnostical difficulties (67). Other challenges are related to the character of symptoms, which hinder adherence to treatments, as the burden of commuting to regularly participate in treatment sessions is very high (68), which could potentially be reduced by designing interventions using virtual or extended reality (69, 70).
This article briefly introduced the concept of interpersonal neural synchrony and linked it for the first time to studies on fibromyalgia and its treatment. Various types of interventions that can involve interpersonal synchrony, such as group dance or exercise, have been shown to be effective in lasting symptoms reduction in people diagnosed with fibromyalgia. Future research is necessary to describe the INS mechanisms in fibromyalgia and reveal their potential health benefits, to verify whether they can eventually contribute to the reconnection on both intra- and interpersonal levels for people living with this severe condition.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
JŚ: Conceptualization, Visualization, Writing – original draft, Writing – review & editing.
The author declares financial support was received for the research, authorship, and/or publication of this article. My work is supported by (1) XR-PAIN (GA No 101070533), funded by the European Media and Immersion Lab project financial support to third parties, which is funded by the European Union, (2) META-TOO (GA No 101160266) funded by the European Union, and (3) Departament de Recerca i Universitats de la Generalitat de Catalunya (AGAUR 2021-SGR-01165 - NEUROVIRTUAL).
I want to thank Prof. Maria Sanchez-Vives and Prof. Antonia Hamilton for their invaluable comments on the manuscript.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. ^The European Alliance of Associations for Rheumatology, https://www.eular.org/
1. Andrews P, Steultjens M, Riskowski J. Chronic widespread pain prevalence in the general population: a systematic review. Eur J Pain. (2018) 22(1):5–18. doi: 10.1002/ejp.1090
2. Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. (2021) 397(10289):2082–97. doi: 10.1016/S0140-6736(21)00393-7
3. Ben-Yosef M, Tanai G, Buskila D, Amital D, Amital H. Fibromyalgia and its consequent disability. Israel Med Assoc J. (2020) 22(7):446–50.
4. Dueñas M, Ojeda B, Salazar A, Mico JA, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. (2016) 9:457–67. doi: 10.2147/JPR.S105892
5. Boomershine CS. Fibromyalgia: the prototypical central sensitivity syndrome. Curr Rheumatol Rev. (2015) 11(2):131–45. doi: 10.2174/1573397111666150619095007
6. Perrot S. Fibromyalgia: a misconnection in a multiconnected world? Eur J Pain. (2019) 23(5):866–73. doi: 10.1002/ejp.1367
7. Ellingson LD, Shields MR, Stegner AJ, Cook DB. Physical activity, sustained sedentary behavior and pain modulation in women with fibromyalgia. J Pain. (2012) 13(2):195–206. doi: 10.1016/j.jpain.2011.11.001
8. Carollo A, Esposito G. Hyperscanning literature after two decades of neuroscientific research: a scientometric review. Neuroscience. (2024) 551:345–54. doi: 10.1016/j.neuroscience.2024.05.045
9. Holroyd CB. Interbrain synchrony: on wavy ground. Trends Neurosci. (2022) 45(5):346–57. doi: 10.1016/j.tins.2022.02.002
10. Müller V. Neural synchrony and network dynamics in social interaction: a hyper-brain cell assembly hypothesis. Front Hum Neurosci. (2022) 16:848026. doi: 10.3389/fnhum.2022.848026
11. Shamay-Tsoory SG. Brains that fire together wire together: interbrain plasticity underlies learning in social interactions. Neuroscientist. (2022) 28(6):543–51. doi: 10.1177/1073858421996682
12. Müller V, Fairhurst MT, Van Vugt FT, Keller PE, Müller MF. Editorial: interpersonal synchrony and network dynamics in social interaction. Front Hum Neurosci. (2022) 16:1095735. doi: 10.3389/fnhum.2022.1095735
13. Hamilton AFC. Hyperscanning: beyond the hype. Neuron. (2021) 109(3):404–7. doi: 10.1016/j.neuron.2020.11.008
14. Hakim U, De Felice S, Pinti P, Zhang X, Noah JA, Ono Y, et al. Quantification of inter-brain coupling: a review of current methods used in haemodynamic and electrophysiological hyperscanning studies. NeuroImage. (2023) 280:120354. doi: 10.1016/j.neuroimage.2023.120354
15. Fairhurst MT, Tajadura-Jiménez A, Keller PE, Deroy O. You, me, and US: maintaining self-other distinction enhances coordination, agency, and affect. iScience. (2023) 26(12):108253. doi: 10.1016/j.isci.2023.108253
16. Hoehl S, Fairhurst M, Schirmer A. Interactional synchrony: signals, mechanisms and benefits. Soc Cogn Affect Neurosci. (2021) 16(1–2):5–18. doi: 10.1093/scan/nsaa024
17. Reddish P, Fischer R, Bulbulia J. ‘Let’s dance together: synchrony, shared intentionality and cooperation’. PLoS One. (2013) 8(8):e71182. doi: 10.1371/journal.pone.0071182
18. Mogan R, Fischer R, Bulbulia JA. To be in synchrony or not? A meta-analysis of synchrony’s effects on behavior, perception, cognition and affect. J Exp Soc Psychol. (2017) 72:13–20. doi: 10.1016/j.jesp.2017.03.009
19. Feng X, Sun B, Chen C, Li W, Wang Y, Zhang W, et al. Self–other overlap and interpersonal neural synchronization serially mediate the effect of behavioral synchronization on prosociality. Soc Cogn Affect Neurosci. (2020) 15(2):203–14. doi: 10.1093/scan/nsaa017
20. Tarr B, Launay J, Cohen E, Dunbar R. Synchrony and exertion during dance independently raise pain threshold and encourage social bonding. Biol Lett. (2015) 11(10):20150767. doi: 10.1098/rsbl.2015.0767
21. Goldstein P, Weissman-Fogel I, Shamay-Tsoory SG. The role of touch in regulating inter-partner physiological coupling during empathy for pain. Sci Rep. (2017) 7(1):3252. doi: 10.1038/s41598-017-03627-7
22. Reddan MC, Young H, Falkner J, López-Solà M, Wager TD. Touch and social support influence interpersonal synchrony and pain. Soc Cogn Affect Neurosci. (2020) 15(10):1064–75. doi: 10.1093/scan/nsaa048
23. Galbusera L, Finn MTM, Tschacher W, Kyselo M. Interpersonal synchrony feels good but impedes self-regulation of affect. Sci Rep. (2019) 9(1):14691. doi: 10.1038/s41598-019-50960-0
24. Brugger P, Lenggenhager B. The bodily self and its disorders: neurological, psychological and social aspects. Curr Opin Neurol. (2014) 27(6):644. doi: 10.1097/WCO.0000000000000151
25. Decety J, Chaminade T. When the self represents the other: a new cognitive neuroscience view on psychological identification. Conscious Cogn. (2003) 12(4):577–96. doi: 10.1016/S1053-8100(03)00076-X
26. Shimada S. Multisensory and sensorimotor integration in the embodied self: relationship between self-body recognition and the mirror neuron system. Sensors. (2022) 22(13):5059. doi: 10.3390/s22135059
27. Ferroni F, Gallese V. The routledge handbook of bodily awareness. In: Alsmith AJT, Longo MR, editors. Social Bodily Self. Conceptual and Psychopathological Considerations. The Routledge Handbook of Bodily Awareness. 1st ed. London: Routledge (2022). p. 522–41. doi: 10.4324/9780429321542
28. Baltazar M, Hazem N, Vilarem E, Beaucousin V, Picq J-L, Conty L. Eye contact elicits bodily self-awareness in human adults. Cognition. (2014) 133(1):120–7. doi: 10.1016/j.cognition.2014.06.009
29. Hazem N, Beaurenaut M, George N, Conty L. Social contact enhances bodily self-awareness. Sci Rep. (2018) 8(1):4195. doi: 10.1038/s41598-018-22497-1
30. Riečanský I, Lengersdorff LL, Pfabigan DM, Lamm C. Increasing self-other bodily overlap increases sensorimotor resonance to others’ pain. Cogn Affect Behav Neurosci. (2020) 20(1):19–33. doi: 10.3758/s13415-019-00724-0
31. Valenzuela-Moguillansky C, Reyes-Reyes A, Gaete MI. Exteroceptive and interoceptive body-self awareness in fibromyalgia patients. Front Hum Neurosci. (2017) 11:117. doi: 10.3389/fnhum.2017.00117
32. Vittersø AD, Halicka M, Buckingham G, Proulx MJ, Bultitude JH. The sensorimotor theory of pathological pain revisited. Neurosci Biobehav Rev. (2022) 139:104735. doi: 10.1016/j.neubiorev.2022.104735
33. Valenzuela-Moguillansky C. An exploration of the bodily experience of persons suffering from fibromyalgia. Constr Found. (2013) 8(3):339–50.
34. Raoul L, Grosbras M-H. Relating different dimensions of bodily experiences: review and proposition of an integrative model relying on phenomenology, predictive brain and neuroscience of the self. Neurosci Biobehav Rev. (2023) 148:105141. doi: 10.1016/j.neubiorev.2023.105141
35. Karos K, Williams ACC, Meulders A, Vlaeyen JWS. Pain as a threat to the social self: a motivational account. Pain. (2018) 159(9):1690–5. doi: 10.1097/j.pain.0000000000001257
36. Calsius J, Courtois I, Stiers J, De Bie J. How do fibromyalgia patients with alexithymia experience their body? A qualitative approach. SAGE Open. (2015) 5(1):2158244015574631. doi: 10.1177/2158244015574631
37. Angioletti L, Balconi M. The increasing effect of interoception on brain frontal responsiveness during a socially framed motor synchronization task. Front Hum Neurosci. (2022) 16:834619. doi: 10.3389/fnhum.2022.834619
38. Kratz AL, Whibley D, Kim S, Sliwinski M, Clauw D, Williams DA. Fibrofog in daily life: an examination of ambulatory subjective and objective cognitive function in fibromyalgia. Arthritis Care Res (Hoboken). (2020) 72(12):1669–77. doi: 10.1002/acr.24089
39. Walitt B, Čeko M, Khatiwada M, Gracely JL, Rayhan R, VanMeter JW, et al. Characterizing “fibrofog”: subjective appraisal, objective performance, and task-related brain activity during a working memory task. Neuroimage Clin. (2016) 11:173–80. doi: 10.1016/j.nicl.2016.01.021
40. Koole SL, Tschacher W. Synchrony in psychotherapy: a review and an integrative framework for the therapeutic alliance. Front Psychol. (2016) 7:862. doi: 10.3389/fpsyg.2016.00862
41. Mende MA, Schmidt H. Psychotherapy in the framework of embodied cognition—does interpersonal synchrony influence therapy success? Front Psychiatry. (2021) 12:562490. doi: 10.3389/fpsyt.2021.562490
42. Sened H, Zilcha-Mano S, Shamay-Tsoory S. Inter-Brain plasticity as a biological mechanism of change in psychotherapy: a review and integrative model. Front Hum Neurosci. (2022) 16:955238. doi: 10.3389/fnhum.2022.955238
43. Lladser A-N, Monteso-Curto P, Lopez C, Rossello L, Lear S, Toussaint L, et al. Multidisciplinary rehabilitation treatments for patients with fibromyalgia: a systematic review. Eur J Phys Rehabil Med. (2021) 5(1):76–84. doi: 10.23736/S1973-9087.21.06432-7
44. Anderson FJ, Winkler AE. An integrated model of group psychotherapy for patients with fibromyalgia. Int J Group Psychother. (2007) 57(4):451–74. doi: 10.1521/ijgp.2007.57.4.451
45. Scheidt CE, Waller E, Endorf K, Schmidt S, König R, Zeeck A, et al. Is brief psychodynamic psychotherapy in primary fibromyalgia syndrome with concurrent depression an effective treatment? A randomized controlled trial. Gen Hosp Psychiatry. (2013) 35(2):160–7. doi: 10.1016/j.genhosppsych.2012.10.013
46. Farzadkia M, Farhangi A, Abolghasemi S. Comparison of effectiveness of intensive short-term dynamic psychotherapy and mindfulness-based stress reduction in depression and severity of symptoms in women with fibromyalgia. Jundishapur J Chronic Dis Care. (2023) 12(3):e133803. doi: 10.5812/jjcdc-133803
47. Jacobs H, Bockaert M, Bonte J, D’Haese M, Degrande J, Descamps L, et al. The impact of a group-based multidisciplinary rehabilitation program on the quality of life in patients with fibromyalgia: results from the QUALIFIBRO study. J Clin Rheumatol. (2020) 26(8):313. doi: 10.1097/RHU.0000000000001120
48. Gómez-de-Regil L, Estrella-Castillo DF. Psychotherapy for physical pain in patients with fibromyalgia: a systematic review. Pain Res Manag. (2020) 2020(1):3408052. doi: 10.1155/2020/3408052
49. Şen E, Hocaoğlu A, Berk Ö. Group psychotherapy with fibromyalgia patients: a systematic review. Arch Rheumatol. (2019) 34(4):476–91. doi: 10.5606/ArchRheumatol.2019.6801
50. de Oliveira Franco Á, da Silveira Alves CF, Vicuña P, Bandeira J, de Aratanha MA, Torres ILS, et al. Hyper-connectivity between the left motor cortex and prefrontal cortex is associated with the severity of dysfunction of the descending pain modulatory system in fibromyalgia. PLoS One. (2022) 17(5):e0247629. doi: 10.1371/journal.pone.0247629
51. Sarzi-Puttini P, Giorgi V, Atzeni F, Gorla R, Kosek E, Choy EH, et al. Fibromyalgia position paper. Clin Exp Rheumatol. (2021) 39(3):186–93. doi: 10.55563/clinexprheumatol/i19pig
52. Sullivan AB, Scheman J, Venesy D, Davin S. The role of exercise and types of exercise in the rehabilitation of chronic pain: specific or nonspecific benefits. Curr Pain Headache Rep. (2012) 16(2):153–61. doi: 10.1007/s11916-012-0245-3
53. Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Fluß E, et al. EULAR Revised recommendations for the management of fibromyalgia. Ann Rheum Dis. (2017) 76(2):318–28. doi: 10.1136/annrheumdis-2016-209724
54. Busch AJ, Schachter CL, Overend TJ, Peloso PM, Barber KAR. Exercise for fibromyalgia: a systematic review. J Rheumatol. (2008) 35(6):1130–44.18464301
55. Beltrán-Carrillo VJ, Tortosa-Martínez J, Jennings G, Sánchez ES. Contributions of a group-based exercise program for coping with fibromyalgia: a qualitative study giving voice to female patients. Women Health. (2013) 53(6):612–29. doi: 10.1080/03630242.2013.819399
56. Hickman B, Pourkazemi F, Pebdani RN, Hiller CE, Yan AF. Dance for chronic pain conditions: a systematic review. Pain Med. (2022) 23(12):2022–41. doi: 10.1093/pm/pnac092
57. Batista ASA, da Silva Maia JB, de-Souza CG, de Almeida Lins CA, de-Souza MC. Depression, anxiety and kinesiophobia in women with fibromyalgia practitioners or not of dance. Bras J Pain. (2021) 3:318–21. doi: 10.5935/2595-0118.20200184
58. Murillo-García Á, Villafaina S, Adsuar JC, Gusi N, Collado-Mateo D. Effects of dance on pain in patients with fibromyalgia: a systematic review and meta-analysis. Evid Based Complement Alternat Med. (2018) 2018:e8709748. doi: 10.1155/2018/8709748
59. Norouzi E, Hosseini F, Vaezmosavi M, Gerber M, Pühse U, Brand S. Zumba dancing and aerobic exercise can improve working memory, motor function, and depressive symptoms in female patients with fibromyalgia. Eur J Sport Sci. (2020) 20(7):981–91. doi: 10.1080/17461391.2019.1683610
60. Basso JC, Satyal MK, Rugh R. Dance on the brain: enhancing intra- and inter-brain synchrony. Front Hum Neurosci. (2021) 14:584312. doi: 10.3389/fnhum.2020.584312
61. Chauvigné LAS, Walton A, Richardson MJ, Brown S. Multi-person and multisensory synchronization during group dancing. Hum Mov Sci. (2019) 63:199–208. doi: 10.1016/j.humov.2018.12.005
62. Yun K, Watanabe K, Shimojo S. Interpersonal body and neural synchronization as a marker of implicit social interaction. Sci Rep. (2012) 2(1):959. doi: 10.1038/srep00959
63. Sturgeon JA, Zautra AJ. Social pain and physical pain: shared paths to resilience. Pain Manag. (2016) 6(1):63–74. doi: 10.2217/pmt.15.56
64. Zhao H, Li Y, Wang X, Kan Y, Xu S, Duan H. Inter-brain neural mechanism underlying turn-based interaction under acute stress in women: a hyperscanning study using functional near-infrared spectroscopy. Soc Cogn Affect Neurosci. (2022) 17(9):850–63. doi: 10.1093/scan/nsac005
65. Schoth DE, Nunes VD, Liossi C. Attentional bias towards pain-related information in chronic pain; a meta-analysis of visual-probe investigations. Clin Psychol Rev. (2012) 32(1):13–25. doi: 10.1016/j.cpr.2011.09.004
66. Montoya Navarro A, Sánchez Salazar CA, Krikorian A, Cortina CC, Marin ML. Suffering in patients with fibromyalgia and its relationship with impact on quality of life, loneliness, emotional state, and vital stress. Rev Colomb Reumatol. (2024) 31(2):193–204. doi: 10.1016/j.rcreue.2023.03.006
67. Kumbhare D, Ahmed S, Watter S. A narrative review on the difficulties associated with fibromyalgia diagnosis. Ther Adv Musculoskelet Dis. (2018) 10(1):13–26. doi: 10.1177/1759720X17740076
68. Oliveira Júnior JOd, Villegas Campos Ramos J. Adherence to fibromyalgia treatment: challenges and impact on the quality of life. Bras J Pain. (2019) 2:81–7. doi: 10.5935/2595-0118.20190015
69. Arlati S, Colombo V, Spoladore D, Greci L, Pedroli E, Serino S, et al. A social virtual reality-based application for the physical and cognitive training of the elderly at home. Sensors. (2019) 19(2):261. doi: 10.3390/s19020261
Keywords: fibromyalgia, bodily self, chronic pain management, interpersonal neural synchrony, interbrain coherence
Citation: Świdrak J (2025) Healing synchrony? potential benefits of interpersonal synchrony for chronic pain management. Front. Pain Res. 6:1463321. doi: 10.3389/fpain.2025.1463321
Received: 11 July 2024; Accepted: 14 January 2025;
Published: 5 February 2025.
Edited by:
Antonio Bonacaro, University of Parma, ItalyReviewed by:
Massimo Guasconi, University of Parma, ItalyCopyright: © 2025 Świdrak. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Justyna Świdrak, anVzdHluYS5zd2lkcmFrQGdtYWlsLmNvbQ==; c3dpZHJha0ByZWNlcmNhLmNsaW5pYy5jYXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.