- 1Department of Psychosomatic Dentistry, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University (TMDU), Tokyo, Japan
- 2Division of Disease Control and Molecular Epidemiology, Department of Oral Growth and Development, School of Dentistry, Health Sciences University of Hokkaido, Ishikari-Tobetsu, Japan
- 3Division of Oral Medicine and Pathology, School of Dentistry, Health Sciences University of Hokkaido, Ishikari-Tobetsu, Japan
As burning mouth syndrome (BMS) and atypical odontalgia (AO) continue to remain complex in terms of pathophysiology and lack explicit treatment protocol, clinicians are left searching for appropriate solutions. Oversimplification solves nothing about what bothers us in clinical situations with BMS or AO. It is important to treat a complicated phenomenon as complex. We should keep careful observations and fact-finding based on a pragmatic approach toward drug selection and prescription with regular follow-up. We also need to assess the long-term prognosis of treatment with a meticulous selection of sample size and characteristics. Further investigation of BMS and AO from a psychosomatic perspective has the potential to provide new insight into the interface between brain function and “chronic orofacial pain.”
1 Introduction
“Chronic orofacial pain (COFP)” is an umbrella term used to describe painful regional syndromes with a chronic, unremitting pattern (1). This term is very convenient; however, the author does not prefer the term “chronic orofacial pain” due to its lack of therapeutic indications and potential for confusion (2). In fact, the study of COFP now seems to be losing focus because of its ambiguity.
For example, studies on burning mouth syndrome (BMS) have seen remarkable growth in the last two decades. These study data have many limitations and do not apply to many clinical cases. Management of BMS has been seen as a “jumble of wheat and tares,” with little evidence to support or refute interventions. The existence of “too many reviews and too few trials” leads to difficulty in choosing an appropriate therapy for each patient with BMS (3).
Consequently, BMS often persists for many years, and patients may undergo several unproductive tests without any improvement in oral symptoms despite many treatment attempts (4). Dentists obviously feel the urgent need to offer some treatments for these BMS patients, developing a feeling of helplessness and frustration.
Atypical odontalgia (AO) is included as another COFP condition that presents challenges for many dentists (5). This pain condition has been given more attention by many dentists because conventional dental procedures seldom provide relief for these patients; on the contrary, there is a risk of legal troubles. AO “pain” differs significantly from ordinary dental conditions like caries or pulpitis; however, patients’ complaints are sometimes very confusing to distinguish from such ordinary dental pain that can be treated successfully. Dentists have become more cautious and nervous in diagnosing “toothache” and more careful when performing invasive dental procedures these days.
Moreover, confusing terminology is impeding progress in the research for the treatment and pathophysiology of both conditions. It might be accurate to say that there is no perfect treatment that can be effective for all BMS or AO patients with various underlying backgrounds. In my opinion, the lack of “psychosocial interventions” is probably the most critical factor contributing to this confusing situation.
In this brief opinion article, BMS and AO are mainly argued as “psychosomatic oral pain”; on the other hand, temporo-mandibular disorders (TMDs) and trigeminal neuralgia (TN) are distinguished from them.
2 What type of “pain” are patients complaining about in cases of BMS or AO?
Many studies have indicated the important role of psychological factors such as depression and anxiety in BMS and AO. Nonetheless, most of them have remained superficial, failing to suggest any hopeful solutions for these chronic oral pain conditions. It seems nonsensical to argue the efficacies of antidepressants or other neuromodulations for BMS or AO without accompanying “psychosocial interventions.” Like other chronic pain, treatment outcomes of BMS were affected easily by placebo and nocebo effects (6). Therefore, every treatment outcome of BMS and AO is probably affected by the patient–physician relationship. Moreover, the patient–physician relationship is crucial for patient’s adherence to any pain medications.
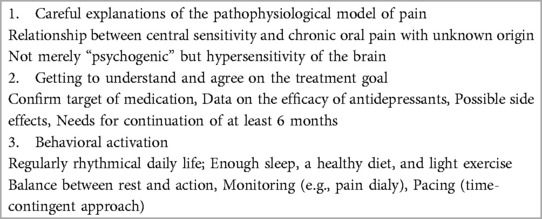
Mere administration without a convincing reason and a full understanding of patients would easily result in their non-adherence. The patient–physician relationship is one of the biggest watersheds between adherence and non-adherence. It should be prioritized to be aware of this psychological background underlying every prescription. Pain medication for BMS and AO requires this psychosomatic perspective. “Psychoeducational treatment” (Table 1) would be necessary for successful pain medication. This is one of the very basic cognitive behavioral therapies (7).
BMS and AO share common trigeminal nerve input, yet they are highly distinct disorders (8). Somatotopic segregation may occur at the level of the trigeminal nucleus, thalamus, and somatosensory cortex, and distinct ionic or neurochemical signaling pathways may be involved (9). This structural basis probably has a strong connection with instinctual emotional function, easily affected by various psychosocial factors.
BMS and AO might be seen as models of a psychosomatic disorder, in which the biological environment interacts with psychosocial factors. This approach does not mean that the mechanisms underlying BMS and AO are purely psychological, but that the role of psychological (or psychopathological) factors is more substantial than in most diseases (4).
In Japanese dentistry, BMS and AO have been regarded as oral psychosomatic disorders for more than half a century, requiring a multidisciplinary (medical and psychosocial) approach. Amitriptyline, a classic tricyclic antidepressant (TCA), has been used for both BMS and AO, with the need for accompanying psychotherapies since then. Nevertheless, difficulties in time-consuming psychosomatic treatments and poor reimbursement (healthcare fee) have prevented many dentists from diligent practice for such patients. However, we have kept searching for BMS and AO as “psychosomatic oral pain” in the hope of finding treatments for them.
3 Problems pile up in researching BMS and AO
3.1 Heterogeneity
The heterogeneity of BMS or AO is the biggest barrier preventing us from reaching the best treatment (3). Moreover, BMS symptoms may change fluidly over time. Sometimes, burning pain goes successfully; however, relapse of oral discomforts such as xerostomia or taste disturbances might quickly become a new problem instead of pain.
The nature of BMS is precisely that of a syndrome, which has several causative factors, including the psychosomatic nature of chronic pain. Hence, treatment response might differ depending on the predominance of individual confounding pathological factors such as neuropathic component, central sensitization, or psychiatric comorbidities. The problems are intertwined in so complex a way that they cannot be solved completely by a single therapy (3).
In particular, psychiatric comorbidities might be significant for any treatments of both BMS and AO. Specifically, when planning pharmacotherapy, one should always consider the psychiatric condition and involve a complete psychologic/psychiatric assessment (10).
Recently, we have had to pay more attention to neurodevelopmental disorders hidden behind intractable AO or BMS (11, 12). Their hypersensitivity might make the pain treatments more difficult; however, treatment response for a dopaminergic medication suggests some common pathophysiology underlying both conditions (13). Regarding these clinical phenomena, confirming pharmacological response (e.g., TCA-responsive BMS/AO vs. non-responders) is one of the challenging issues in understanding the pathophysiology of this pain (14).
On the other hand, neurovascular compression of the trigeminal nerve might also be valuable to distinguish possible peripheral pathophysiology of AO (15).
3.2 Oral cenesthopathy superimposed on BMS or AO
The complaint of “burning” is often regarded as neuropathic pain; however, it also has a very similar nature to oral cenesthopathy (16). Oral cenesthopathy is characterized by bizarre and abnormal oral sensations without medical and dental evidence. In fact, oral cenesthopathy is sometimes comorbid with BMS (26.24%) or AO (5.78%) (17).
The diagnosis of oral cenesthopathy is still controversial, and contemporary psychiatry does not provide independently defined diagnostic criteria (18). Oral sensory disturbances fall within a continuum in patients with or without diagnosed somatoform disorders. Careful consideration of the patient's dopaminergic state and the possible contribution of psychiatric comorbidities can help guide therapeutic choices, but the management may still involve some trial and error since symptoms evolve and overlap (19).
3.3 Assessment of improvement
In chronic pain research like BMS or AO, the biggest problem remains in how to assess subjective oral symptoms that cannot be quantitated. Next, what should be set as the treatment goal or target? How can we say a patient with BMS or AO has been saved?
A satisfactory assessment tool for BMS remission is not yet available. The suffering of BMS or AO could hardly be assessed in visual analog scale (VAS) scores only. BMS involves not only a burning sensation but also discomfort such as dryness or dysgeusia (20), as mentioned above. Therefore, the clinicians should reconsider what a patient claims as “pain.” We need more effective qualitative assessment tools for insight into the patient’s experience of “pain” instead of using VAS only.
A standardized symptom assessment tool is necessary to facilitate scientific discussion among researchers for improving diagnosis and treatment modalities. We developed the Oral Dysesthesia Rating Scale (Oral DRS) and evaluated its validity as an assessment tool (18). Since patients often develop impairments in oral functions such as eating and speaking and in the performance of daily activities, this new tool is designed to also assess these dysfunctions.
We believe that the treatment goal or target for BMS or AO should not be set in “complete remission” nor “symptom-free” but good enough satisfaction for both patients and physicians. It must be hastened to develop better “clinically meaningful outcomes.”
3.4 Safety of pharmacotherapy
Despite no strong evidence of the efficacy of specific medications or agreement between the authors, it is worth noting that the absence of evidence is not evidence of absence. Neuromodulators such as benzodiazepines (e.g., clonazepam) or antidepressants (e.g., amitriptyline) have been used for the treatment of BMS (21) or AO (14). We have anecdotal evidence in many patients that these drugs work well.
These medication therapies can be continued as long as the patient's benefits outweigh the harm. Tricyclic antidepressants are not always safe (22), and there is the risk of abuse with benzodiazepines (23). However, in Japan, we seldom experience big problems such as dependence or misuse in prescribing benzodiazepines for BMS patients (24). It might be due to the different prescription “refill” service systems in each country. However, benzodiazepine therapy should only ever be initiated when the patient is aware of the risks and benefits of these drugs, understands what physiologic dependence is, and has a clear understanding that the drug will be discontinued after a short time (25). Physicians should weigh the risks versus benefits when prescribing benzodiazepines to patients with BMS. A low-dose strategy in these medications is probably appropriate in most cases.
3.5 Lack of long-term prognosis
Then, another important problem arises in the assessment of duration and follow-up of medications. BMS and AO have continuous, long-lasting symptoms, often with fluctuations. Despite the importance of studies evaluating the long-term prognosis, there is little data on longitudinal outcomes or recurrence in treating BMS or AO.
We cannot ignore the systemic problem in university hospitals, where many staff members transfer their positions frequently. It becomes challenging for a patient to be followed up by one physician. This unstable treatment situation must be affected by the treatment effect and the dropout ratio.
Patients with BMS or AO tend to easily drop out from any treatment. We believe evaluating the differences between dropout cases and the cases in good clinical courses would help resolve this (26). We suggest that real-world data may be more essential than short-term RCTs to know the best benefits and limitations of the treatment.
Retrospective long-term treatment outcomes may be a more critical option (27, 28). Complete remission of BMS or AO is not so frequent in these medication therapies; however, it is not always impossible if adequate psychosocial intervention is available.
3.6 What should we do next?
It might also be helpful to clarify the factors contributing to patient satisfaction with long-term observations. Goal attainment scaling (GAS) (29), a flexible and responsive technique for assessing outcomes in complex interventions, assimilates the achievement of individual goals into a single standardized “goal attainment scale.” GAS has been proposed as a patient-centered, semi-quantitative measure. Each patient's problems are identified through agreement between the physician and the patient. Treatment goals are set for each problem using the specific, measurable, attainable, realistic, and timed (SMART) methodology. Such an assessment method could shed light on a new treatment strategy that reinforces the previous treatments for BMS and AO.
4 Summary
As BMS and AO continue to remain complex in terms of pathophysiology and lack explicit treatment protocols, clinicians are left searching for appropriate solutions.
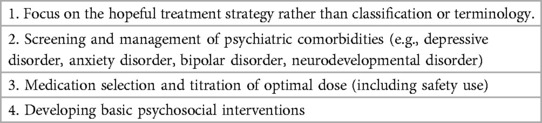
Oversimplification solves nothing about what bothers us in clinical situations with BMS or AO. It is important to treat a complicated phenomenon as complex. We should keep careful observations and fact-finding based on a pragmatic approach for drug selection and prescription with regular follow-up. We also need to assess long-term prognosis of treatment with a meticulous selection of sample size and characteristics (Table 2). Further investigation of BMS and AO with a psychosomatic perspective can provide new insight into the interface between brain function and “COFP.”
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
Author contributions
AT: Conceptualization, Writing – original draft. HM: Conceptualization, Supervision, Writing – review & editing. YA: Conceptualization, Supervision, Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This work was supported by JSPS KAKENHI under Grant Number 22K10141.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor YU declared a past co-authorship with the author AT.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Benoliel R, Sharav Y. Chronic orofacial pain. Curr Pain Headache Rep. (2010) 14(1):33–40. doi: 10.1007/s11916-009-0085-y
2. Ananthan S, Benoliel R. Chronic orofacial pain. J Neural Transm (Vienna). (2020) 127(4):575–88. doi: 10.1007/s00702-020-02157-3
3. Tu TTH, Takenoshita M, Matsuoka H, Watanabe T, Suga T, Aota Y, et al. Current management strategies for the pain of elderly patients with burning mouth syndrome: a critical review. Biopsychosoc Med. (2019) 13:1. doi: 10.1186/s13030-019-0142-7
4. Galli F, Pravettoni G. Burning mouth syndrome-opening the door to a psychosomatic approach in the era of patient-centered medicine. JAMA Otolaryngol Head Neck Surg. (2020) 146(6):569–70. doi: 10.1001/jamaoto.2020.0524
5. Abiko Y, Matsuoka H, Chiba I, Toyofuku A. Current evidence on atypical odontalgia: diagnosis and clinical management. Int J Dent. (2012) 2012:518548. doi: 10.1155/2012/518548
6. Colloca L, Barsky AJ. Placebo and nocebo effects. N Engl J Med. (2020) 382(6):554–61. doi: 10.1056/NEJMra1907805
7. Matsuoka H, Chiba I, Sakano Y, Toyofuku A, Abiko Y. Cognitive behavioral therapy for psychosomatic problems in dental settings. Biopsychosoc Med. (2017) 11:18. doi: 10.1186/s13030-017-0102-z
8. Takenoshita M, Sato T, Kato Y, Katagiri A, Yoshikawa T, Sato Y, et al. Psychiatric diagnoses in patients with burning mouth syndrome and atypical odontalgia referred from psychiatric to dental facilities. Neuropsychiatr Dis Treat. (2010) 6:699–705. doi: 10.2147/NDT.S12605
9. Sharav Y, Katsarava Z, Charles A. Facial presentations of primary headache disorders. Cephalalgia. (2017) 37(7):714–9. doi: 10.1177/0333102417705374
10. Galli F, Gambini O. Psychopharmacology of headache and its psychiatric comorbidities. Handb Clin Neurol. (2019) 165:339–44. doi: 10.1016/B978-0-444-64012-3.00020-4
11. Kasahara S, Kato Y, Takahashi K, Matsudaira K, Sato N, Fukuda KI, et al. Improvement in persistent idiopathic facial pain with comorbid ADHD using the combination of a dopamine system stabilizer and psychostimulant: a case report. Clin Case Rep. (2023) 11(6):e7552. doi: 10.1002/ccr3.7552
12. Kasahara S, Takao C, Matsudaira K, Sato N, Tu TTH, Niwa SI, et al. Case report: treatment of persistent atypical odontalgia with attention deficit hyperactivity disorder and autism spectrum disorder with risperidone and atomoxetine. Front Pain Res (Lausanne). (2022) 3:926946. doi: 10.3389/fpain.2022.926946
13. Kasahara S, Takahashi K, Matsudaira K, Sato N, Fukuda KI, Toyofuku A, et al. Diagnosis and treatment of intractable idiopathic orofacial pain with attention-deficit/hyperactivity disorder. Sci Rep. (2023) 13(1):1678. doi: 10.1038/s41598-023-28931-3
14. Tu TTH, Miura A, Shinohara Y, Mikuzuki L, Kawasaki K, Sugawara S, et al. Pharmacotherapeutic outcomes in atypical odontalgia: determinants of pain relief. J Pain Res. (2019) 12:831–9. doi: 10.2147/JPR.S188362
15. Kawasaki K, Sugawara S, Watanabe K, Hong C, Tu TTH, Watanabe T, et al. Differences in the clinical characteristics of persistent idiopathic facial pain (atypical odontalgia) patients with or without neurovascular compression of the trigeminal nerve. Pain Med. (2020) 21(4):814–21. doi: 10.1093/pm/pnz300
16. Karakuş İH, Bulut NS. Oral cenesthopathy superimposed on burning mouth syndrome treated with aripiprazole: a case report with a phenomenological overview. Gerodontology. (2021) 38(1):113–6. doi: 10.1111/ger.12516
17. Umezaki Y, Miura A, Shinohara Y, Mikuzuki L, Sugawara S, Kawasaki K, et al. Clinical characteristics and course of oral somatic delusions: a retrospective chart review of 606 cases in 5 years. Neuropsychiatr Dis Treat. (2018) 14:2057–65. doi: 10.2147/NDT.S167527
18. Uezato A, Toyofuku A, Umezaki Y, Watanabe M, Toriihara A, Tomita M, et al. Oral dysesthesia rating scale: a tool for assessing psychosomatic symptoms in oral regions. BMC Psychiatry. (2014) 14:1696. doi: 10.1186/s12888-014-0359-8
19. Yu JRT, Yu XX, Rajaram R, Fernandez HH, Siddiqui J. Burning mouth syndrome to oral cenesthopathy: a spectrum of neuropsychiatric and sensory complications in neurodegenerative parkinsonism? Parkinsonism Relat Disord. (2022) 104:1–2. doi: 10.1016/j.parkreldis.2022.09.010
20. Shin HI, Bang JI, Kim GJ, Kim MR, Sun DI, Kim SY. Therapeutic effects of clonazepam in patients with burning mouth syndrome and various symptoms or psychological conditions. Sci Rep. (2023) 13(1):7257. doi: 10.1038/s41598-023-33983-6
21. Kim MJ, Choi JH, Kho HS. Long-term prognosis of burning mouth syndrome following treatment. Int J Oral Maxillofac Surg. (2022) 51(12):1538–44. doi: 10.1016/j.ijom.2022.08.011
22. Watanabe M, Nakabayashi T, Nayanar G, Takao C, Maeda C, Tu TTH, et al. Case report: auditory hallucination induced by amitriptyline for the treatment of atypical odontalgia. Front Psychiatry. (2022) 13:863485. doi: 10.3389/fpsyt.2022.863485
23. Suga T, Tu TTH, Nagamine T, Toyofuku A. Careful use of clonazepam and alpha lipoid acid in burning mouth syndrome treatment. Oral Dis. (2022) 28(3):846–7. doi: 10.1111/odi.13776
24. Paudel D, Utsunomiya M, Yoshida K, Giri S, Uehara O, Matsuoka H, et al. Pharmacotherapy in relieving the symptoms of burning mouth syndrome: a 1-year follow-up study. Oral Dis. (2020) 26(1):193–9. doi: 10.1111/odi.13226
25. Pergolizzi JV, LeQuang JA. Reappraising the use of benzodiazepines in chronic pain patients. Postgrad Med. (2020) 132(sup3):10–2. doi: 10.1080/00325481.2020.1725352
26. Nayanar GK, Tu TTH, Nagamine T, Toyofuku A. Comment on: the assessment of the long-term prognosis of burning mouth syndrome following treatment necessitates a reappraisal. Int J Oral Maxillofac Surg. (2023) 52(9):1013–4. doi: 10.1016/j.ijom.2023.01.011
27. Watanabe M, Takenoshita M, Tu TTH, Toyofuku A. Real-world discontinuation of antidepressant treatment in patients with burning mouth syndrome: a chart review. Pain Med. (2020) 21(9):2009–10. doi: 10.1093/pm/pnz324
28. Watanabe M, Takao C, Liu Z, Nayanar G, Suga T, Hong C, et al. The effectiveness and adverse events of amitriptyline and aripiprazole in very elderly patients with BMS. Front Pain Res (Lausanne). (2022) 3:809207. doi: 10.3389/fpain.2022.809207
Keywords: burning mouth syndrome, atypical odontalgia, psychosomatic oral pain, chronic orofacial pain, treatment strategy
Citation: Toyofuku A, Matsuoka H and Abiko Y (2024) Reappraising the psychosomatic approach in the study of “chronic orofacial pain”: looking for the essential nature of these intractable conditions. Front. Pain Res. 5:1349847. doi: 10.3389/fpain.2024.1349847
Received: 5 December 2023; Accepted: 17 April 2024;
Published: 10 May 2024.
Edited by:
Yojiro Umezaki, Fukuoka Dental College, JapanReviewed by:
Xiaoxiang Xu, Peking University Hospital of Stomatology, China© 2024 Toyofuku, Matsuoka and Abiko. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akira Toyofuku, dG95b29tcG1AdG1kLmFjLmpw
 Akira Toyofuku
Akira Toyofuku Hirofumi Matsuoka
Hirofumi Matsuoka Yoshihiro Abiko
Yoshihiro Abiko