- 1Centre for Pain Research, Leeds Beckett University, Leeds, United Kingdom
- 2Academic Unit of Palliative Care, University of Leeds, Leeds, United Kingdom
In this article, we provide a unique perspective on the use of mindfulness interventions in a whole health framework embedded within the theory of salutogenesis and the concept of painogenic environments. We argue that mindfulness is a valuable tool to bridge exploration of inner experiences of bodily pain with socio-ecological influences on thoughts and emotions. We outline research from neuroimaging studies that mindfulness techniques mediate neural processing and neuroplastic changes that alleviate pain and related symptoms. We also review evidence examining behavioural changes associated with mindfulness meditation providing evidence that it promotes self-regulatory activity, including the regulation and control of emotion and catalysation of health behaviour changes; both of which are important in chronic illness. Our viewpoint is that mindfulness could be a core element of salutogenic approaches to promote health and well-being for people living with pain because it rebuilds a fractured sense of cohesion. Mindfulness empowers people in pain to embrace their existence; shifting the focus away from pain and giving their lives meaning. We propose that integrating mindfulness into activities of daily living and individual or community-based activities will promote living well in the modern world, with or without pain; thus, promoting individual potential for fulfilment. Future research should consider the effects of mindfulness on people with pain in real-life settings, considering social, environmental, and economic factors using a broader set of outcomes, including self-efficacy, sense of coherence and quality of life.
Introduction
Painogenicity, described as the tendency of socio-ecological environments to promote persistent pain (1), and salutogenesis, a concept that considers the origins of health as opposed to the origins of disease, have proved useful ways of exploring a healthy settings approach to the challenge of persistent pain in society (2–5). Salutogenesis is premised on the concept of a sense of coherence—the way people make sense of the interaction of their body in the world—and is fundamental to understand why some people develop persistent pain whilst others do not (6, 7). Sense of coherence operates at individual, group (family), organization and societal levels and includes meaningfulness of one's life, comprehensibility of stimuli arising from the internal and external environments, and manageability of these stimuli using resources at a person's disposal, such as health care services and treatments, social networks and peer support, and self-coping strategies to promote mental and physical well-being (8).
Mindfulness involves paying non-judgemental attention to experiences inside and outside of “oneself” on a moment-by-moment basis to aid reconnection of sensations, thoughts and feelings with the outside world in a positive way (9). Our viewpoint proposed here is that mindfulness is a valuable tool to bridge exploration of inner experiences of bodily pain with socio-ecological influences on thoughts and emotions. In this article, we discuss mindfulness interventions within the framework of the theory of salutogenesis and the concept of painogenic environments.
Shortcomings of the biopsychosocial model
The biomedical model, which associates pain with potential or actual tissue damage, has, at least in part, fostered a reductionist and materialist approach to alleviating pain by analysing and diagnosing the status of tissue, rather than synthesising factors affecting a whole-person's lived experience of pain in the complex socio-ecological milieu of the modern era (10–12). In recent decades, the shift towards a broader biopsychosocial model of pain has acknowledged the importance of psychosocial risk factors—employment conditions and socioeconomic status as two examples—which potentially promote pain and hinder recovery resulting in pain management strategies utilising multimodal interventions and multidisciplinary teams. Often, biopsychosocial interventions are delivered as discrete entities targeting specific elements of a person's psychophysiology in a disconnected manner (e.g., surgery, medication, exercise, diet therapy, cognitive behavioural therapy (CBT), acceptance and commitment therapy (ACT), etc.) Thus, some people experience fragmented care to the detriment of their health and well-being. Moreover, there is a treatment-prevalence paradox in which an ever-increasing variety of interventions have not reduced the burden of persistent pain. Calls to shift emphasis towards holistic models of pain supported by integrated health care service delivery are growing (13, 14).
The whole health model
Gaudet advocates a cultural transformation of the purpose of healthcare, and other systems impacting on health and well-being, underpinned by the concept of “whole person health” (15). Gaudet argues for a change in the focus of health care by discovering what gives people a sense of meaning and purpose in their lives and building systems that support this. Advocates of Whole Health view a person's life as a journey of “push and pull” within a continuum of health and disease. Thus, Whole Health focuses on factors that create health not just factors that prevent disease.
The concept of wholeness has been discussed by academics for decades; mostly emanating from the “Whole Person Medicine” movement during the 1970's which had its roots in complementary and alternative medicine (CAM) (16). Viewpoints from different CAM protagonists have recently been discussed (17), providing a summary of current thinking from academics endorsing a variety of approaches. Interestingly, it is acknowledged that this model is still falling short of providing effective, integrated care, even after decades of research because “… in order to successfully transform the existing biomedical model, the Whole Health model must demonstrate validated research outcomes …” (17) (p. 3). This, according to Langevin, needs to be achieved by moving away from the reductionist approach to biomedical research (18) and there is still much debate on how this can be achieved.
In 2020, Agarwal published a postmodernist, social constructionist treatise on an “ecology of wholeness” which describes the relationship between the biomedical understanding of the body in pain and its relationship with a person's awareness of themselves and their interaction with micro and macro level aspects of material existence with the natural world (19). Agarwal's ecological model of wholeness comprises The Self (i.e., reflexive and embodied) and The Body [i.e., material and discursive (conversational)], in relationship with The Context (i.e., time, change, Illness intrusion, traditional health system, food, nature, body/self-integration) (19). Agarwal's model emphasises the need to consider not only the person within a diagnostic framework, but also the wider ecological (salutogenic) setting (19, 20). Within this framework, patient involvement, education and empowerment are central tenets.
We advocate reconfiguring the health care mindset away from a reductionist and materialist viewpoint towards a whole-person (societal) health lens that focuses on factors that support and empower people to create their own health and wellbeing, i.e., salutogenesis (2, 5).
Pain and salutogenesis
In 1979, Antonovsky introduced the term “salutogenesis”, meaning, “the origins of health” (21). It considers the origins of health as opposed to the origins of disease (22). The key to understanding persistent pain within a salutogenic framework is to consider how people can develop meaning from their suffering and translate pain into something positive and meaningful for them through their internal sense of coherence, either as an individual or as part of a group (7). Salutogenesis is influenced by surroundings, socio-economic and environmental factors that can promote or hinder recovery from pain. Its premise is that people can be healthy despite pain. Environments which promote the persistence, severity, or impact of pain, including hindering recovery from pain, have been described as “painogenic” (1). The relationships between the salutogenic framework and Agarwal's “ecology of wholeness” in a context of persistent pain and whole health are illustrated in Figure 1.

Figure 1. A whole-health model of mindful awareness within a salutogenic framework for individuals with persistent pain (19).
Painogenicity
The term “painogencity” was introduced to reflect parallels between persistent pain and Boyd Swinburn's concept of obesogenicity (1). Swinburn defined obesogenicity as the sum of influences that the surroundings, opportunities or conditions of life have on promoting obesity in people or populations (23). It moved away from an individualistic understanding that obesity was “caused” through individual choice or action towards a wider recognition that social, environmental, and commercial conditions may promote conditions that made obesity more likely. Johnson (1) appraised persistent pain from an evolutionary mismatch-perspective and argued that, like obesity, socio-ecological conditions may promote the persistence of pain i.e., that aspects of modern-day living were painogenic. Thus, painogencity was defined as the tendency of socio-ecological environments (or “settings”) to promote persistent pain.
Settings-based approaches and health promotion
Rather than focusing on the manifestation of a behaviour or condition (i.e., pain), academic debate on alternative ways to approach the problem of persistent pain, using interventions embedded within the theory of salutogenesis and a settings approach to health and wellbeing has become more accepted in the discourse (7, 24, 25). It is grounded in the World Health Organisation's (WHO) Ottawa Charter, which prioritised empowering people and communities to increase control over, and to improve, their own health by providing the conditions and resources to do this (26).
Settings-based approaches to health are “upstream” and maximize disease prevention and its impact on health (e.g., pain) by attending to the settings where people actively use and shape their environment and create or solve problems relating to their health. Settings comprise physical boundaries and organisational structures. They include homes, workplaces, schools, villages, towns, cities, hospitals, prisons etc. The goal of a settings-based approach is to maximise health promotion and disease prevention through a “whole system” model of public health via community participation, partnership, empowerment and equity (26, 27). Empowering people to understand and make sense of their lives by increasing their sense of coherence has been shown to decrease the risk of non-communicable diseases for which there are currently programmes acting solely on “downstream” risk factors (e.g., hypercholesterolaemia, hypertension and type 2 diabetes) (28).
Campaigns to enable people to explore their emotional relationship with pain and to offer strategies to foster living better lives with their pain have arisen; e.g., Live Well with Pain (https://livewellwithpain.co.uk/), Pain Café (https://pain.cafe/), Flippin' Pain (https://www.flippinpain.co.uk/), Pain revolution (https://www.painrevolution.org/), and others. These strategies include, amongst other things, mind-body techniques that increase a person's sense of coherence, such as mindfulness meditation, yoga, tai chi, relaxation techniques and hypnosis. Of these techniques, mindfulness has risen in popularity since the end of the 20th century with healthcare providers (29). Integrating mindfulness practice into activities of daily living can improve a person's sense of coherence.
Mindfulness
Context
The historical roots of mindfulness date back to the 5th century BC. Mindfulness has been defined as: “…the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment” (30). Mindfulness involves people being aware of their situation, without being reactive, judgemental, or overwhelmed by what is happening to them or around them. Mindfulness interventions in various guises have been used to prevent or alleviate maladaptive perceptions of pain, such as catastrophising and associated psychological manifestations such as anxiety and depression (31).
The principles of mindfulness can be readily incorporated into creative activities (e.g., music, drawing, writing, painting, clay making, dance), daily activities (e.g., shopping, washing dishes, gardening, walking) and sport, recreation and exercise activities (e.g., swimming, fishing and yoga), both individually and as a group. The optimal state of mindfulness is of “relaxed alertness”, which is associated with better mental health (32). Interestingly, it is likely that people who are able to withstand extreme physical discomfort, such as ultra-endurance athletes (33) or those engaging in extreme sports (34) are able to enter some sort of mindful, or self-hypnotic state to divert their attention away from the physical (and psychological) pain.
Beneficial effects of mindfulness
Comprehensive reviews of evidence suggest that mindfulness alters processing of multiple brain regions leading to a variety of beneficial effects for people with persistent pain (35–37). Briefly, mindfulness practices involving focussed attention (e.g., slow, rhythmic breathing or body scanning techniques), promote calmness and relaxation that increase parasympathetic activity (vagal tone) which ameliorates the hypothalamic-pituitary-adrenal (HPA) axis response to stressors such as pain. This improves physiological status including blood pressure, respiration, heart rate reactivity, fatigue and pain and other bodily sensations (38–41). Mindfulness decouples thalamus–precuneus and ventromedial prefrontal deactivation, effectively inhibiting onward transmission of nociceptive input (42). Mindfulness improves emotional and cognitive well-being in people with persistent pain mediated in part by functional alterations in the insula, amygdala, and hippocampus (35–38, 42–50). Neuroplastic changes occur in the insula associated with interoception and a reduction in negative emotional responses to unpleasant sensations such as pain (40, 51). For some people, patterns of neural activity experienced during mindfulness practise can be replicated at will (52). Thus, better acceptance of painful or unpleasant sensations are achieved through modulation of negative appraisals of interoceptive stimuli and by promoting coping strategies (40, 53, 54).
A review of evidence examining behaviour changes associated with mindfulness meditation provided evidence that the intervention promotes self-regulatory activity, including the regulation and control of emotion and catalysation of health behaviour changes; both of which are important in chronic illness (55). Other behavioural changes such as self-compassion are also thought to occur; encouraging behaviours associated with self-compassion and a reduction in overidentification with painful experiences (56). A meta-analysis also showed beneficial effects on negative self-related rumination, suggesting that it might reduce repetitive focus on symptoms (57).
Clinical research evidence for beneficial effects of mindfulness interventions for people with persistent pain is growing, but based on small, under-powered studies which show statistical significance but fail to demonstrate favourable effect sizes (35, 58, 59).
A systematic review published in 2016 indicated that mindfulness produced small improvements in pain symptoms based on a meta-analysis of 24 RCTs of low quality (60). systematic review of 30 RCTs published in 2017 found that mindfulness produced small improvements in the severity of persistent (chronic) pain compared with various control groups (61), yet a systematic review of 13 RCTs published in the same year found that mindfulness did not improve the severity of persistent pain but did improve psychological aspects of pain, such as depression (62). The methodological quality of RCTs included in both reviews was judged to be low. In 2021, Pei et al., conducted a systematic review of eight RCTs that did not find any statistically significant differences between mindfulness and control groups on the severity of persistent pain, although there were improvements in mindfulness and depression in the short-term (63). Pei et al., suggested a need for evaluations of dose–response to optimise mindfulness technique. We suggest that these systematic review findings are promising and might provide impetus for further research.
Since the COVID-19 pandemic, online and smartphone self-help interventions for pain, including mindfulness techniques have become popular (64), but research findings on the efficacy and effectiveness of these self-help interventions are inconclusive (65). However, these applications potentially represent a cost-effective way of implementing mindfulness interventions.
Reviews and evidence syntheses of mindfulness studies for persistent pain conditions using qualitative methodologies were not found but several small individual studies of varying methodological quality reveal several recurring themes following mindfulness-based interventions. A small analysis of four groups of older adults with persistent low back pain, following an eight-week mindfulness programme revealed benefits such as overcoming fear of pain, a reduction in negative emotions and a reduction in focus on the pain (66). Another demonstrated an improvement in pain-related strategies following group mindfulness and problem-solving (67), and a feasibility study found patients more empowered to look after themselves, and were more self-aware and in the moment following an eight-week Mindfulness-Based Stress Reduction (MBSR) programme (68).
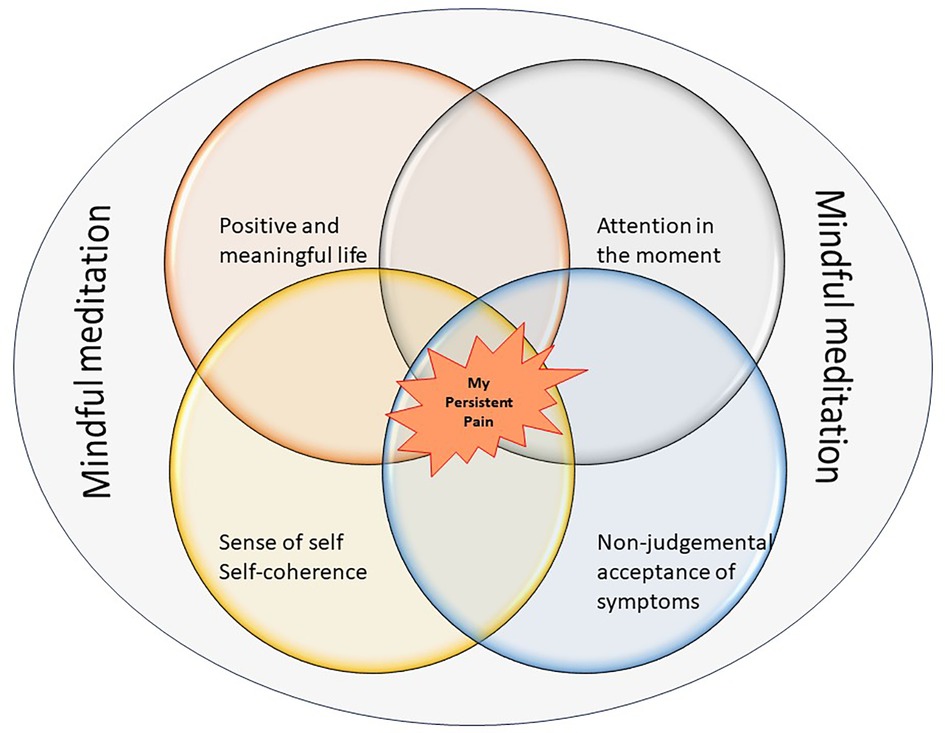
A simplified diagrammatic illustration of the overlap between the key elements of mindfulness meditation in the context of persistent pain is shown in Figure 2.
Adverse effects of mindfulness meditation
As with any intervention, an awareness of possible adverse effects is essential but frequently overlooked. The British Psychological Society guidelines on mindfulness-based approaches warns that these interventions should not be expected to confer benefit on everyone (69), although the prevalence of adverse events is thought to be no more likely than it is using other psychotherapeutic techniques (70).
Inducing body-awareness and introspection through mindfulness can vary within and between people and may produce detrimental effects such as autonomic hyperarousal, perceptual disturbances, flashbacks, and even psychosis in those with particularly disturbing past experiences, e.g., childhood trauma or abuse (71, 72). A systematic review by Farias et al. (70), found that adverse events in meditation-based practices included psychosis, delusional events, fear and traumatic flashbacks and a population based survey of 434 people in the US suggested that approximately one third of people had experienced a meditation-related adverse effect such as re-experiencing of trauma, anxiety, emotional sensitivity and functional impairments (73). Surprisingly, approximately 80% of those experiencing adverse effects reported they were still “glad” to have meditated.
It is clear that a “one size fits all” approach to mindfulness meditation carries risks, particularly to people who already suffer from psychiatric illnesses or those who have had previous negative life-experiences (71). The British Psychological Society refers to guidance for monitoring and reporting of harm or side-effects in patients with psychosis (74), and this might also be applicable to people with persistent pain, with or without mental illness.
Discussion
Mindfulness to promote the “healing journey”
A salutogenic view of the benefits of mindfulness to promote living well with persistent pain could encompass an ecology of wholeness and the context of a person's “healing journey” (19, 75). Toye et al., (76) conducted a meta-ethnography that synthesized the findings of 195 qualitative studies exploring the experience of people living with persistent, non-malignant musculoskeletal pain that identified key elements of a health intervention to assist people on their “healing journey”:
1. Validating pain through meaningful and acceptable explanations.
2. Validating patients by listening to and valuing their stories.
3. Encouraging patients to connect with a meaningful sense of self, to be kind to themselves, and to explore new possibilities for the future.
4. Facilitating safe reconnection with the social world.
Toye et al. concluded that people in pain should be encouraged to move forward alongside their pain, rather than focusing on expectations of a cure; a model in which self-value, acceptance and recognition are central. Mindfulness is already being embedded in a variety of biopsychosocial interventions used to alleviate pain, thus promoting re-connection with a meaningful sense of self. This would enable people to explore new possibilities for the future.
Mindfulness within a whole health delivery system
We advocate placing mindfulness at the core of interventions to aid recovery by improving a sense of coherence and empowering people to embrace their existence as a whole, giving their lives meaning and potential for fulfilment. In health care, mindfulness is seen as a psychological tool to aid self-management and is disconnected from many biomedical approaches (e.g., surgery and medication). Mindfulness is often at the core of community support activities e.g., yoga, that are rarely integrated with standard health care service delivery. Mindfulness has potential to develop health and well-being across core theoretical components underpinning interventions to promote the health of individuals, communities and nature (i.e., Whole Health perspective), such as those described by Kemp and Fisher (77); balanced mind, healthy body, connecting with people, connecting with nature, socio-structural factors, and sustaining behaviour change. Thus, we believe that encouraging mindfulness as an integrated lifestyle practice offers opportunities for people to use these techniques as adjuncts for many biopsychosocial interventions. Mindfulness skills could be developed through social prescribing of community-based support services for healthy living, and this could confer benefits in all aspects of life from activities of daily living to life enriching activities such as gardening, arts and crafts, walking, swimming, etc. Locating mindfulness as a lifestyle practice sits more comfortably within a whole-systems approach where people move forward in their journey towards better health through validation, acceptance, empowerment and, ultimately, fulfilment.
Future research
Presently, there is tentative, low quality evidence that mindfulness is beneficial for pain (78). Recently, Moore et al., (79) have raised serious concern about methodological shortcomings of RCTs in the broader field of pain research resulting in low confidence in evidence for many analgesic treatments. The Medical Research Council's guidance suggests that attention be given to how interventions are used in the real world (i.e., their utility) including mediating factors, implementability, acceptability, feasibility of delivery and cost-effectiveness (80, 81). Thus, research evaluating baseline level of mindfulness skills, optimal “dose” and moderating influences of environmental factors may prove informative (31, 82). Attention also needs to be given to how best to capture holistic outcomes within the ecology of wholeness model without fragmenting this “wholeness” into a collection of discrete outcomes that are viewed as disconnected entities.
Conclusion
Pain, especially when persistent, catalyses a loss of identity, a diminished sense of self, retreat from the world outside of the painful body and alienation and detachment from a meaningful life (83). Bullington (83) argues that rehabilitation must open up new possibilities of a life beyond or alongside pain through an enhanced sense of self.
By developing skills to attend, on a moment-to-moment basis, to happenings inside and outside of oneself mindfulness can rebuild a sense of cohesion and “wholeness”. In doing so, mindfulness can be used to instil a positive, proactive, approach to promote health through learning of a new sense of self and shifting focus away from the dominant biomedical narrative of deficit and opening new opportunities for a fulfilling life beyond, or alongside pain.
Our viewpoint is that mindfulness could be a core element of salutogenic approaches to promote health and well-being for people living with pain because mindfulness rebuilds the sense of cohesion fractured when pain threatens the future self. Mindfulness underpins an “ecology of wholeness” and could be a strategy used by people to mitigate the detrimental consequences of painogenicity. Greater credence should be given to the findings of research investigating the effects of mindfulness on people with pain in real-life settings that considers the influence of social, environmental, and economic factors using a broader set of outcomes including self-efficacy, sense of coherence and quality of life. This will shift the focus of evidence-gathering and expectations of rehabilitation from efficacy and pain to utility and outcomes associated with valuable and fulfilling lives.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
CP and MJ contributed to conception of the article. CP wrote the first draft of the manuscript. CP and MJ wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version. All authors contributed to the article and approved the submitted version.
Conflict of interest
In the previous 5 years, MJ has received income for expert consultancy activities from GlaxoSmithKline, TENSCare, and LifeCare Ltd. that lie outside of the submitted work. MJ declares book royalties from Oxford University Press.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Johnson MI. Opinions on paleolithic physiology living in painogenic environments: changing the perspective through which we view chronic pain. Pain Manag. (2019) 9(3):219–24. doi: 10.2217/pmt-2018-0095
2. Johnson MI, Bonacaro A, Georgiadis E, Woodall J. Reconfiguring the biomedical dominance of pain: time for alternative perspectives from health promotion? Health Promot Int. (2022) 37(4):daac128. doi: 10.1093/heapro/daac128
3. Johnson MI, Briggs M, Dixey R. Should health promotion be on the pain agenda? Pain Manag. (2014) 4(6):385–8. doi: 10.2217/pmt.14.31
4. Johnson MI, Dixey R. Should pain be on the health promotion agenda? Glob Health Promot. (2012) 19(4):41–4. doi: 10.1177/1757975912464251
5. Johnson MI, Woodall J. A healthy settings approach to addressing painogenic environments: new perspectives from health promotion. Front Pain Res. (2022) 3. doi: 10.3389/fpain.2022.1000170
6. Eriksson M, Lindstrom B. A salutogenic interpretation of the Ottawa charter. Health Promot Int. (2008) 23(2):190–9. doi: 10.1093/heapro/dan014
7. Oliveira CC. Suffering and salutogenesis. Health Promot Int. (2015) 30(2):222–7. doi: 10.1093/heapro/dau061
8. Eriksson M, Mittelmark MB. The sense of coherence and its measurement. In: Mittelmark MB, Sagy S, Eriksson M, Bauer GF, Pelikan JM, Lindström B, et al., editors. The handbook of salutogenesis. Cham (CH): Springer (2017). p. 97–106.
9. Khoo EL, Small R, Cheng W, Hatchard T, Glynn B, Rice DB, et al. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network meta-analysis. Evid Based Ment Health. (2019) 22(1):26–35. doi: 10.1136/ebmental-2018-300062
10. Kusnanto H, Agustian D, Hilmanto D. Biopsychosocial model of illnesses in primary care: a hermeneutic literature review. J Family Med Prim Care. (2018) 7(3):497–500. doi: 10.4103/jfmpc.jfmpc_145_17
11. Roberts A. The biopsychosocial model: its use and abuse. Med Health Care Philos. (2023) 26(3):367–84. doi: 10.1007/s11019-023-10150-2
12. Xiao X, Song H, Sang T, Wu Z, Xie Y, Yang Q. Analysis of real-world implementation of the biopsychosocial approach to healthcare: evidence from a combination of qualitative and quantitative methods. Front Psychiatry. (2021) 12. doi: 10.3389/fpsyt.2021.725596
13. Dunn V. The holistic assessment of the patient in pain. Prof Nurse. (2000) 15(12):791–3. PMID: 1202642812026428
14. Kress HG, Aldington D, Alon E, Coaccioli S, Collett B, Coluzzi F, et al. A holistic approach to chronic pain management that involves all stakeholders: change is needed. Curr Med Res Opin. (2015) 31(9):1743–54. doi: 10.1185/03007995.2015.1072088
15. Gaudet T. Cultural transformation to a whole health system: lessons learned. Glob Adv Health Med. (2022) 11:2164957X221091452. doi: 10.1177/2164957X221091452
16. Jonas WB, Eisenberg D, Hufford D, Crawford C. The evolution of complementary and alternative medicine (cam) in the USA over the last 20 years. Forsch Komplementmed. (2013) 20(1):65–72. doi: 10.1159/000348284
17. Mills PJ, Bushell WC. Returning wholeness to health. Glob Adv Health Med. (2022) 11:2164957X221092358. doi: 10.1177/2164957X221092358
18. Langevin HM. Making connections to improve health outcomes. Glob Adv Health Med. (2022) 11:2164957X221079792. doi: 10.1177/2164957X221079792
19. Agarwal V. Medical humanism, chronic illness, and the body in pain: An ecology of wholeness. Maryland, US: Lexington Books (2020). 328 p.
20. Agarwal V. Patient assessment and chronic pain self-management in ethnomedicine: seasonal and ecosystemic embodiment in ayurvedic patient-centered care. Int J Environ Res Public Health. (2020) 17(8). doi: 10.3390/ijerph17082842
21. Antonovsky A. Health stress and coping. 1st (5th printing) ed. San Francisco, US: Jossey-Bass inc (1979).
22. Mittelmark M, Bauer G. The meanings of salutogenesis. In: Mittelmark M, Sagy S, Eriksson M, Bauer G, Pelikan J, Lindström B, et al.,, editors. The handbook of salutogenesis [internet] 2017. Cham (CH): Springer (2016).
23. Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med. (1999) 29(6 Pt 1):563–70. doi: 10.1006/pmed.1999.0585
24. Dooris M, Poland B, Kolbe L, Leeuw ED, Mccall D, Wharf-Higgins J. Healthy settings: Building evidence for the effectiveness of whole system health promotion—challenges and future directions. In: Mcqueen DV, Jones CM, editors. Global perspectives on health promotion effectiveness. New York: Springer (2007).
25. Lindström B, Eriksson M. Contextualizing salutogenesis and antonovsky in public health development. Health Promot Int. (2006) 21(3):238–44. doi: 10.1093/heapro/dal016
26. World Health Organisation (WHO). Ottowa charter for health promotion. Health Promotion. (1986) 1(4):iii–v. doi: 10.1093/heapro/1.4.405
27. Stansfield J, South J, Mapplethorpe T. What are the elements of a whole system approach to community-centred public health? A qualitative study with public health leaders in England’s local authority areas. BMJ Open. (2020) 10(8):e036044. doi: 10.1136/bmjopen-2019-036044
28. Suominen S, Lindstrom B. Salutogenesis. Scand J Public Health. (2008) 36(4):337–9. doi: 10.1177/1403494808093268
29. Blanck P, Perleth S, Heidenreich T, Kröger P, Ditzen B, Bents H, et al. Effects of mindfulness exercises as stand-alone intervention on symptoms of anxiety and depression: systematic review and meta-analysis. Behav Res Ther. (2018) 102:25–35. doi: 10.1016/j.brat.2017.12.002
30. Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol: Sci Pract. (2003) 10(2): 144–56. doi: 10.1093/clipsy.bpg016
31. Day MA, Jensen MP, Ehde DM, Thorn BE. Toward a theoretical model for mindfulness-based pain management. J Pain. (2014) 15(7):691–703. doi: 10.1016/j.jpain.2014.03.003
32. Lomas T, Ivtzan I, Fu CH. A systematic review of the neurophysiology of mindfulness on eeg oscillations. Neurosci Biobehav Rev. (2015) 57:401–10. doi: 10.1016/j.neubiorev.2015.09.018
33. Brace AW, George K, Lovell GP. Mental toughness and self-efficacy of elite ultra-marathon runners. PLoS One. (2020) 15(11):e0241284. doi: 10.1371/journal.pone.0241284
34. Tofler IR, Hyatt BM, Tofler DS. Psychiatric aspects of extreme sports: three case studies. Perm J. (2018) 22:17–071. doi: 10.7812/TPP/17-071
35. Carlson LE. Mindfulness-based interventions for physical conditions: a narrative review evaluating levels of evidence. ISRN Psychiatry. (2012) 2012:651583. doi: 10.5402/2012/651583
36. Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. (2008) 31(1):23–33. doi: 10.1007/s10865-007-9130-7
37. Howarth A, Smith JG, Perkins-Porras L, Ussher M. Effects of brief mindfulness-based interventions on health-related outcomes: a systematic review. Mindfulness. (2019) 10:1957–68. doi: 10.1007/s12671-019-01163-1
38. Sovik R. The science of breathing–the yogic view. Prog Brain Res. (2000) 122:491–505. doi: 10.1016/s0079-6123(08)62159-7
39. Chui PL, Wai S, Lai LL, See MH, Tan SB. Mindful breathing: effects of a five-minute practice on perceived stress and mindfulness among patients with cancer. Clin J Oncol Nurs. (2021) 25(2):174–80. doi: 10.1188/21.Cjon.174-180
40. Gibson J. Mindfulness, interoception, and the body: a contemporary perspective. Front Psychol. (2019) 10. doi: 10.3389/fpsyg.2019.02012
41. Warth M, Stoffel M, Koehler F, Bardenheuer HJ, Kessler J, Ditzen B. Characteristics of salivary cortisol and alpha-amylase as psychobiological study outcomes in palliative care research. BMC Palliat Care. (2022) 21(1):226. doi: 10.1186/s12904-022-01085-1
42. Riegner G, Posey G, Oliva V, Jung Y, Mobley W, Zeidan F. Disentangling self from pain: mindfulness meditation–induced pain relief is driven by thalamic–default mode network decoupling. Pain. (2023) 164(2):280–91. doi: 10.1097/j.pain.0000000000002731
43. Adler-Neal AL, Waugh CE, Garland EL, Shaltout HA, Diz DI, Zeidan F. The role of heart rate variability in mindfulness-based pain relief. J Pain. (2020) 21(3–4):306–23. doi: 10.1016/j.jpain.2019.07.003
44. Chayadi E, Baes N, Kiropoulos L. The effects of mindfulness-based interventions on symptoms of depression, anxiety, and cancer-related fatigue in oncology patients: a systematic review and meta-analysis. PLoS One. (2022) 17(7):e0269519. doi: 10.1371/journal.pone.0269519
45. Ng D-L-C, Gan G-G, Anuar NA, Tung Y-Z, Lai N-Z, Tan Y-W, et al. The effect of a single session of 30-min mindful breathing in reducing fatigue among patients with haematological cancer—a randomised controlled trial. BMC Palliat Care. (2021) 20(1):160. doi: 10.1186/s12904-021-00855-7
46. Kerr C, Sacchet M, Lazar S, Moore C, Jones S. Mindfulness starts with the body: somatosensory attention and top-down modulation of cortical alpha rhythms in mindfulness meditation. Front Hum Neurosci. (2013) 7. doi: 10.3389/fnhum.2013.00012
47. Russell TA, Arcuri SM. A neurophysiological and neuropsychological consideration of mindful movement: clinical and research implications. Front Hum Neurosci. (2015) 9. doi: 10.3389/fnhum.2015.00282
48. Lardone A, Liparoti M, Sorrentino P, Rucco R, Jacini F, Polverino A, et al. Mindfulness meditation is related to long-lasting changes in hippocampal functional topology during resting state: a magnetoencephalography study. Neural Plast. (2018) 2018:5340717. doi: 10.1155/2018/5340717
49. Sharma M. Yoga as an alternative and complementary approach for stress management: a systematic review. J Evid Based Complementary Altern Med. (2014) 19(1):59–67. doi: 10.1177/2156587213503344
50. Tang Y-Y, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. (2015) 16(4):213–25. doi: 10.1038/nrn3916
51. Eller-Smith OC, Nicol AL, Christianson JA. Potential mechanisms underlying centralized pain and emerging therapeutic interventions. Front Cell Neurosci. (2018) 12. doi: 10.3389/fncel.2018.00035
52. Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin Psychol Sci Pract. (2003) 10(2):125. doi: 10.1093/clipsy.bpg015
53. Schmalzl L, Powers C, Henje Blom E. Neurophysiological and neurocognitive mechanisms underlying the effects of yoga-based practices: towards a comprehensive theoretical framework. Front Hum Neurosci. (2015) 9:235. doi: 10.3389/fnhum.2015.00235
54. Haase L, Thom NJ, Shukla A, Davenport PW, Simmons AN, Stanley EA, et al. Mindfulness-based training attenuates Insula response to an aversive interoceptive challenge. Soc Cogn Affect Neurosci. (2016) 11(1):182–90. doi: 10.1093/scan/nsu042
55. Schuman-Olivier Z, Trombka M, Lovas DA, Brewer JA, Vago DR, Gawande R, et al. Mindfulness and behavior change. Harv Rev Psychiatry. (2020) 28(6):371–94. doi: 10.1097/hrp.0000000000000277
56. Germer CK, Neff KD. Self-compassion in clinical practice. J Clin Psychol. (2013) 69(8):856–67. doi: 10.1002/jclp.22021
57. Britton W, Loucks E, King J, Schuman-Olivier Z, Lazar SW, Brewer JA, et al. Meta-analytic review of self-regulation processes in mindfulness-based cognitive therapy and mindfulness-based stress reduction. PROSPERO. (2016):CRD42016051765.
58. Guan NC, Beng TS, Sue-Yin L, Kanagasundram S. The effect of 5-min mindful breathing on pain in palliative care cancer patients: a randomized controlled study. Indian J Palliat Care. (2021) 27(1):83–8. doi: 10.4103/ijpc.Ijpc_122_20
59. Ngamkham S, Holden JE, Smith EL. A systematic review: mindfulness intervention for cancer-related pain. Asia Pac J Oncol Nurs. (2019) 6(2):161–9. doi: 10.4103/apjon.apjon_67_18
60. Maglione MA, Hempel S, Ruelaz Maher A, Apaydin E, Ewing B, Hilton L, et al. Mindfulness meditation for chronic pain: A systematic review. Santa Monica, CA: RAND Corporation (2016).
61. Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med. (2017) 51(2):199–213. doi: 10.1007/s12160-016-9844-2
62. Ball EF, Nur Shafina Muhammad Sharizan E, Franklin G, Rogozińska E. Does mindfulness meditation improve chronic pain? A systematic review. Curr Opin Obstet Gynecol. (2017) 29(6):359–66. doi: 10.1097/gco.0000000000000417
63. Pei J-H, Ma T, Nan R-L, Chen H-X, Zhang Y-B, Gou L, et al. Mindfulness-based cognitive therapy for treating chronic pain a systematic review and meta-analysis. Psychol Health Med. (2021) 26(3):333–46. doi: 10.1080/13548506.2020.1849746
64. Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, Lynch ME, et al. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (ehealth) pain management services. Pain. (2020) 161(5):889–93. doi: 10.1097/j.pain.0000000000001885
65. MacPherson M, Bakker AM, Anderson K, Holtzman S. Do pain management apps use evidence-based psychological components? A systematic review of app content and quality. Can J Pain. (2022) 6(1):33–44. doi: 10.1080/24740527.2022.2030212
66. Luiggi-Hernandez JG, Woo J, Hamm M, Greco CM, Weiner DK, Morone NE. Mindfulness for chronic low back pain: a qualitative analysis. Pain Med. (2018) 19(11):2138–45. doi: 10.1093/pm/pnx197
67. Smith C, Skaer T, Orr M, Barbosa-Leiker C, Howell D, Dyck D. Development of multi-family group and mindfulness treatment for chronic pain: preliminary outcomes. J Musculoskelet Disord Treat. (2017) 3. doi: 10.23937/2572-3243.1510042
68. Bawa F M, Sutton J, Mercer S, Bond C. “I’m empowered to Look after myself”—mindfulness as a way to manage chronic pain: an interpretative phenomenological analysis of participant experiences in Scotland. Soc Sci Med. (2021) 281:114073. doi: 10.1016/j.socscimed.2021.114073
69. Whomsley S, Russell TA. Mindfulness-based approaches: A guide for psychologists. Leicester, UK: The British Pscyhology Society (2022). doi: 10.53841/bpsrep.2022.rep166
70. Farias M, Maraldi E, Wallenkampf KC, Lucchetti G. Adverse events in meditation practices and meditation-based therapies: a systematic review. Acta Psychiatr Scand. (2020) 142(5):374–93. doi: 10.1111/acps.13225
71. Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, et al. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect Psychol Sci. (2018) 13(1):36–61. doi: 10.1177/1745691617709589
72. Farias M, Wikholm C. Has the science of mindfulness lost its mind? BJPsych Bull. (2016) 40(6):329–32. doi: 10.1192/pb.bp.116.053686
73. Goldberg SB, Lam SU, Britton WB, Davidson RJ. Prevalence of meditation-related adverse effects in a population-based sample in the United States. Psychother Res. (2022) 32(3):291–305. doi: 10.1080/10503307.2021.1933646
74. Ellett L, Chadwick P. Recommendations for monitoring and reporting harm in mindfulness for psychosis research. Br J Psychiatry. (2021) 219(6):629–31. doi: 10.1192/bjp.2021.98
75. Toye F, Seers K, Allcock N, Briggs M, Carr E, Andrews J, et al. A meta-ethnography of patients’ experience of chronic non-malignant musculoskeletal pain. Health Serv Deliv Res. (2013) 1(12). doi: 10.3310/hsdr01120
76. Toye F, Belton J, Hannink E, Seers K, Barker K. A healing journey with chronic pain: a meta-ethnography synthesizing 195 qualitative studies. Pain Med. (2021) 22(6):1333–44. doi: 10.1093/pm/pnaa373
77. Kemp AH, Fisher Z. Wellbeing, whole health and societal transformation: theoretical insights and practical applications. Glob Adv Health Med. (2022) 11:21649561211073077. doi: 10.1177/21649561211073077
78. Malinowski P. Neural mechanisms of attentional control in mindfulness meditation. Front Neurosci. (2013) 7:8. doi: 10.3389/fnins.2013.00008
79. Moore A, Fisher E, Eccleston C. Flawed, futile, and fabricated-features that limit confidence in clinical research in pain and anaesthesia: a narrative review. Br J Anaesth. (2023) 130(3):287–95. doi: 10.1016/j.bja.2022.09.030
80. Wolfenden L, Foy R, Presseau J, Grimshaw JM, Ivers NM, Powell BJ, et al. Designing and undertaking randomised implementation trials: guide for researchers. Br Med J. (2021) 372:m3721. doi: 10.1136/bmj.m3721
81. Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of medical research council guidance. Br Med J. (2021) 374:n2061. doi: 10.1136/bmj.n2061
82. Day MA, Thorn BE, Ward LC, Rubin N, Hickman SD, Scogin F, et al. Mindfulness-based cognitive therapy for the treatment of headache pain: a pilot study. Clin J Pain. (2014) 30(2):152–61. doi: 10.1097/AJP.0b013e318287a1dc
Keywords: mindfulness and chronic pain, salutogenesis and persistent pain, painogenicity, mindful approaches to pain, whole health, ecology of wholeness
Citation: Paley CA and Johnson MI (2023) Perspective on salutogenic approaches to persistent pain with a focus on mindfulness interventions. Front. Pain Res. 4:1188758. doi: 10.3389/fpain.2023.1188758
Received: 17 March 2023; Accepted: 15 August 2023;
Published: 29 August 2023.
Edited by:
Mark Henry Pitcher, National Center for Complementary and Integrative Health (NIH), United StatesReviewed by:
Ramajayam Govindaraj, National Institute of Mental Health and Neurosciences, India© 2023 Paley and Johnson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark I. Johnson bS5qb2huc29uQGxlZWRzYmVja2V0dC5hYy51aw==
 Carole A. Paley
Carole A. Paley Mark I. Johnson
Mark I. Johnson