
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Pain Res. , 15 June 2023
Sec. Musculoskeletal Pain
Volume 4 - 2023 | https://doi.org/10.3389/fpain.2023.1185280
This article is part of the Research Topic Yoga for Pain Relief View all 5 articles
 Pradeep M. K. Nair1*
Pradeep M. K. Nair1* Sucheta Kriplani2
Sucheta Kriplani2 Prakash Babu Kodali3
Prakash Babu Kodali3 Ayush Maheshwari2
Ayush Maheshwari2 Kinjal Dilipsinh Bhalavat4
Kinjal Dilipsinh Bhalavat4 Deepika Singh2
Deepika Singh2 Sanjeev Saini2
Sanjeev Saini2 Dinesh Yadav2
Dinesh Yadav2 Jyoti Keswani5
Jyoti Keswani5 Karishma Silwal2
Karishma Silwal2 Hemanshu Sharma6
Hemanshu Sharma6 Gulab Rai Tewani2
Gulab Rai Tewani2
Objectives: The aim of this study is to identify the characteristics of patients who underwent yoga therapy for pain in yoga and naturopathy clinical settings in India.
Methods: Electronic medical records of patients who received yoga therapy for pain in three inpatient yoga and naturopathy hospitals were reviewed retrospectively from January 2021 to September 2022. Demographic characteristics and details on pain condition, socioeconomic status, comorbidities, ancillary therapies received, and insurance status were collected. In addition, we prospectively collected data on adherence to yoga practice through a telephonic interview.
Results: A total of 984 patients were identified from a pool of 3,164 patients who received yoga therapy for pain for an average of 9.48 (1.13) days. Patients aged between 8 and 80 underwent therapy for varying pain conditions and diseases that include pain in the extremities, pain due to infection, trauma, degenerative diseases, autoimmune diseases, and spine and neurological diseases. The majority of the patients were females (66.3%), from middle class families (74.8%), and who did not have any insurance coverage (93.8%). Most of the patients were under naturopathy treatment (99.8%), followed by ayurveda (56%), and physiotherapy (49.3%), along with yoga therapy. All patients reported a significant reduction in pain post-integrated yoga therapy (p < 0.001). Adherence to yoga was significantly associated with underlying pain conditions, the presence of comorbidities, the types of therapies used, and socioeconomic status (p < 0.001).
Conclusion: This study highlights the real-time application of yoga in pain management in Indian yoga and naturopathy settings, as well as implications for future research.
The popularity of yoga across the globe has grown over the years. This surge in the acceptability of yoga has made it one of the most prominently used complementary medicine therapies for various medical conditions (1). Evidence also supports the use of yoga for various medical conditions. However, little is known about the characteristics and socioeconomic background of patients who use yoga as a treatment modality, especially those of the Indian population. A recent cross-sectional study from India reported a prevalence rate of 11.8% for yogic practice among Indians(2). However, the primary focus of this survey is to understand the usefulness of yoga in diabetes mellitus. Barring this survey, no other reports are available on the characteristics of patients from India who use yoga for different medical conditions.
Understanding the characteristics, socioeconomic background, and duration of illness of patients who use yoga as a therapy will provide useful insights that may aid in devising public health policies. While the beneficial effect of yoga in managing psychological and metabolic conditions is well known, there is a growing interest in using yoga for pain management as well (3, 4). However, a recent review indicates that the majority of the studies reporting the efficacy of yoga in pain are related to backache, migraine, and fibromyalgia (3). Presently, there is no literature available regarding the use of yoga in pain conditions based on socioeconomic status, clinical condition, associated comorbidities, or the concomitant therapies used alongside yoga therapy.
In India, yoga and naturopathy are regarded among the official indigenous systems of medicine under the Ministry of Ayurveda, Yoga and Naturopathy, Unani, Siddha, Sowa-Rigpa, and Homoeopathy (AYUSH), Government of India (5). In Indian yoga and naturopathy hospitals, yoga therapy prescription is made by yoga and naturopathy physicians who have a Bachelors' degree in Yoga and Naturopathy (BNYS—Bachelor of Naturopathy and Yogic Sciences) and an “A” class medical registration in their respective state medical councils (6). A typical yoga and naturopathy inpatient setting offers therapies like diet therapy, heliotherapy, acupressure, acupuncture, hydrotherapy, massage therapy, and yoga therapy (6).
There are approximately 5,000 yoga and naturopathy hospitals in India (7) that use yoga therapy as an integral part of their treatment plan for all conditions, including pain. However, little is known about the pattern of clinical practice in these hospitals. Mapping the clinical patterns of yoga usage among patients will provide information on the current prescription practices of yoga, factors associated with its adherence, commonly used conditions, and so on, which will help in policy formulation and research. Therefore, in this study, we focus on the use of yoga for pain management and aim to provide information on the characteristics of patients who sought yoga as a therapy for their pain conditions in three yoga- and naturopathy-based inpatient hospitals from three different parts of India.
This study used a cross-sectional study design. The medical records of patients treated with yoga alone or in combination with other complementary medicine therapies for pain were retrospectively reviewed between January 2021 and September 2022 at three in-patient yoga and naturopathy settings in the north, south, and central parts of India . These hospitals were purposefully selected as they had an average bed occupancy rate of over 60% throughout the year.
The electronic medical records were reviewed to collect data on the patients' sociodemographic characteristics such as age, gender, economic status [computed using the Kuppuswamy scale (8)], insurance coverage, pain condition for which the patient underwent yoga therapy (refer Supplementary File), duration of the pain condition, additional treatments received along with yoga therapy, and visual analog scores for pain. Further, we prospectively collected data on adherence to yoga practice through a telephonic interview. An individual was considered adhering to practice if they reported that they continued to practice yoga at least once a week post discharge.
All patients who were treated as inpatients for pain (see Supplementary File) exclusively with yoga or yoga integrated with other complementary medicine therapies (CAM) such as naturopathy, ayurveda, and physiotherapy at the three study settings were included in the study. Patients who were treated with other CAM modalities, excluding yoga, outpatients, patients whose electronic medical records were incomplete, and those who were treated for conditions other than pain were excluded from the study.
We analyzed the data of 984 patients who were treated for pain using yoga or yoga with other complementary medicine therapies in the three selected study sites. Prior to analysis, we cleaned the data to address issues relating to any missing data, data entry errors, and inconsistencies. The missing data were found to be minimal (n = 6) and were observed only under the category of variable age. We employed the item mean substitution method (9) to replace these missing data. The variable age was classified into three categories using class intervals. The categories in the variables such as non-communicable disease (NCD) status, socioeconomic status, and use of complementary/multiple therapies were collapsed into fewer categories to facilitate the analysis. Frequency tables were constructed to study the characteristics of patients and the characteristics of the therapy received.
The pain scores captured using the Visual Analog Scale (VAS) were descriptively analyzed using mean and standard deviation. Normality of the pain scores was assessed using the skewness of the scores and Q–Q plots. The pretherapy pain scores had a near normal distribution with a skewness of 0.239. We compared the differences in pre- and post-therapy VAS pain scores across the patient characteristics using linear mixed models (LMMs). The effect size was calculated using Glass delta (10) to measure the magnitude and direction of difference between pain scores before and after treatment with yoga or yoga integrated with other complementary medicine therapies.
The patients were followed up to determine their levels of adherence to yogic practice after discharge. A binary logistic regression analysis was conducted to assess the factors associated with adherence to yoga among the participants. The Hosmer–Lemeshow test was conducted to identify the model fit. Adjusted odds ratios (AORs) and 95% CI for the AORs were computed.
The study was approved by the Institutional Ethics Committee of Sant Hirdaram Medical College of Naturopathy and Yogic Sciences for Women (F.No:12/SHMCNYS-IEC/P27/2022-23), Prakriti Shakti Clinic of Natural Medicine (CGH-PS/IRB/2022/2), and Morarji Desai Institute of Naturopathy and Yogic Sciences (MDINYS/IEC/2022/P7). All participants signed an informed consent (obtained during their in-patient stay for using their de-identified data for research purposes) form to participate in the study.
The three study sites in total had 3,764 inpatient admissions, with the average stay of patients being 9.48 ± 1.13 days. Of these 3,764, 26.14% (n = 984) were found to have undergone a yoga therapy session for a pain condition. These 984 patients accounted for the study sample. The study participants included 66.3% (n = 652) females and were primarily in the age group of 34–58 years (55.1%, n = 542). All participants enrolled reported suffering from some form of pain, with pain due to spine and neurological conditions being the most prominent (36.2%). Most of the participants (93.8%) who sought yoga therapy were not covered by any insurance policies (see Table 1).
We noted that most of the participants received more than one type of therapy in addition to their yoga therapy. Among the participants who were receiving naturopathy, a substantial proportion also received ayurveda and physiotherapy (see Figure 1). Differentials in the use of various forms of therapy across demographic and health status were noted among the study participants (see Table 2).
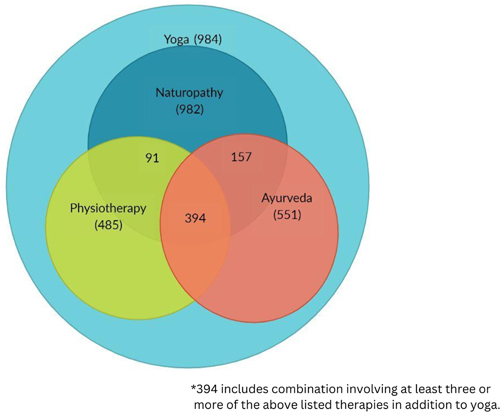
Figure 1. Schematic representation outlining the use of multiple therapies among the study participants.
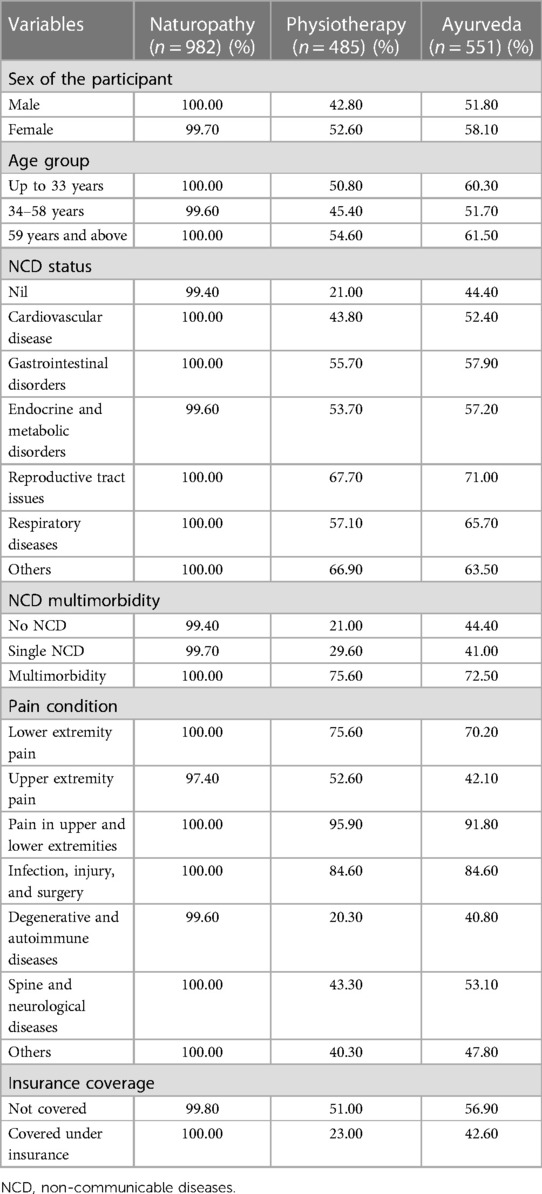
Table 2. Characteristics of the study participants in terms of the use of naturopathy and other complementary therapies along with yoga (n = 984).
The VAS pain scores were captured prior to the therapy and after the therapy among study participants during their inpatient stay. The LMMs were used to assess the changes in VAS scores before and after therapy across the patient characteristics. The findings indicate that yoga therapy resulted in a significant pain reduction (see Table 3).
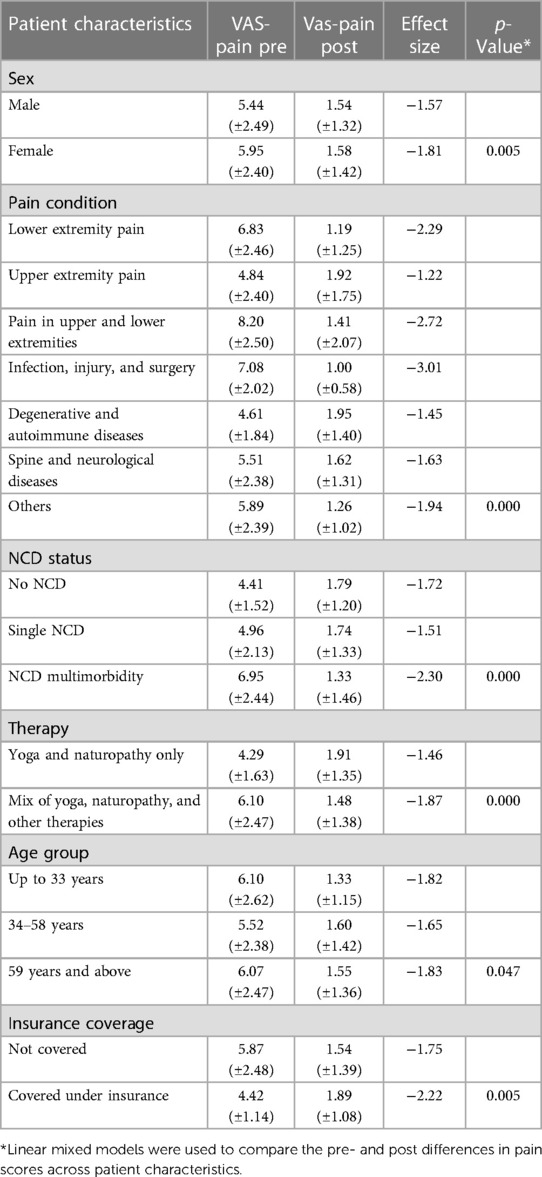
Table 3. Changes in the VAS pain score pre- and post therapy among the study participants (n = 984).
It was found that 75.3% (n = 741) reported continuing yoga after being discharged from the facility. Specifically, 39.8% (n = 392) practiced yoga every day of the week, 10.7% (n = 105) practiced yoga thrice a week, and 24.8% (n = 244) practiced yoga up to twice a week. Patients who were suffering from lower extremity pain (AOR = 2.05; 95% CI = 1.05–3.99), those who had NCD multimorbidity (AOR = 3.93; 95% CI = 2.47–6.25), and those who belonged to the middle (AOR = 2.27; 95% CI = 1.44–3.58) and upper (AOR = 2.02; 95% CI = 1.06–3.85) socioeconomic strata had greater odds of adhering to yoga therapy post discharge (see Table 4).
The present study is the first of its kind that showcases the characteristics of patients who use yoga for treating their pain conditions, from three yoga and naturopathy clinical settings in India. Our findings indicate that females and patients over the age of 34 are more likely to use yoga for pain management. This may be largely attributed to the gender predisposition of pain, wherein females suffer more from pain than their male counterparts (10). Similarly, the increased prevalence of the use of yoga for pain management among older adults can be attributed to the increased prevalence of chronic pain among older adults compared with their younger counterparts (10).
Our data suggest socioeconomic status to be a significant predictor for the use of yoga therapy for pain. Most of the patients who underwent yoga therapy for pain were from either the middle class or the upper class. This indicates the need for formulating policies that enhance the availability of yoga among the lower socioeconomic strata of society, as a lower socioeconomic status or financial instability is reported to increase the vulnerability to pain (11, 12).
Barring 16% of the patients, nearly one-third of the patients who underwent yoga therapy for pain had at least one NCD. Endocrine and metabolic disorders accounted for 50% of NCDs among the patients, and more than 46% of them had more than one NCD. This indicates the coexistence of NCDs and pain conditions. The need for providing palliative care among NCD patients is seldom suggested and is often considered as a secondary goal (13, 14). Our study population presenting with an NCD comorbidity along with pain indicates the need for introducing palliative care among NCD patients. The potential for integration of yoga as part of palliative care for patients suffering from NCDs should be further explored.
An earlier review reported that, most of the studies describing the efficacy of yoga in pain were related to chronic back pain (3). Underreporting, limited expertise, lack of experience, and/or lack of awareness on the importance of research among complementary and alternative medicine practitioners (15) may be a primary reason for the research reports to be confined to backache. Our case chart review suggests that yoga is being used for an array of pain conditions that are not limited to backache. This indicates that research on the area of yoga and pain should be expanded beyond backache by including patients from yoga- and naturopathy-based hospitals. Further, adequate exposure to research and journal communications are warranted for yoga and naturopathy physicians to unveil the magnitude of yoga in pain management.
In this study, it was found that a majority of the patients who availed yoga therapy for pain had no insurance coverage, reflecting out-of-pocket spending for accessing yoga services. This is perplexing, because, on the one hand, yoga is being immensely popularized by policymakers, and on the other hand, there exists shortcomings in policies that limit its accessibility. Numerous commentaries and reviews have opined that the non-availability of insurance coverage for yoga may restrict its use only among the upper strata of the society (3, 16, 17). Moreover, the limited focus of health insurance for yoga and complementary medical systems also comes in the way of the integration of yoga services with universal healthcare.
In this study, it was found that almost all patients who used yoga for pain management have also used another complementary and alternative therapy (CAM). This pattern was consistent across the three study settings, and naturopathy was reported as the mostly used therapy, followed by ayurveda. This may be attributed to prescription practice followed at the respective clinical settings. Further, the patients may have co-opted to undergo these therapies because of their comorbid conditions, as an integrated approach is reported to reduce the burden of NCDs (18–20). The report on the use of CAM therapies in our patients reiterates the integrative potential of yoga therapy with other therapies.
All patients reported a significant reduction in their pain irrespective of their age, clinical condition, NCD status, concomitant therapies used, and insurance status. This observation is consistent with that of other experimental studies reporting yoga to alleviate pain in various conditions (21–24). We also prospectively explored the adherence/continuity to yogic practice among the patients and found that 75% of them continued the practice after their initial exposure in the clinical setting. Adherence to yogic practice was associated with the pain condition of the patient, the presence of NCD, and the socioeconomic status. Furthermore, we did not gather any information about the time between the patient's discharge and the time of data collection. This could also play a part in adhering to yoga, and the lack of information on this could be regarded as a limitation of this study.
Patients with multiple NCD conditions were found to adhere more to yogic practice compared with those with a single NCD or no NCD. NCD multimorbidity is associated with significant burden and stress. Yoga integrated with naturopathy is recommended to reduce the burden and associated complications of NCD (18). An earlier community-based observational study from India also reported increased utilization of yoga therapy along with naturopathy among NCD patients (25). The heightened adherence to yoga among patients with multimorbid NCDs, which was found in the present study, may be viewed as an increasing acceptance of yoga therapy among patients.
Socioeconomic status has emerged as another important factor determining the adherence to yoga after the initial exposure. Confirming the results from earlier studies, our study also found a higher adherence of yoga among patients with a higher socioeconomic status (26, 27). Correlating the non-availability of insurance, reduced use and adherence of yoga among the lower socioeconomic group of patients in this study indicates the need for framing revised policies that improve the accessibility to yoga for this group.
To our knowledge, this is the first study to report the characteristics of patients using yoga for pain management in Indian clinical settings. However, there are notable limitations in the present study. First, barring one variable on adherence to yoga, the rest of our analyses were based on retrospective medical records from three yoga and naturopathy hospitals from India. Therefore, the results of this study have limited generalizability and may not fully reflect the present scenario. All the three clinical settings studied offers yoga and naturopathy as an integrated therapy; therefore, it is difficult to determine whether the patients enrolled for the program exclusively for yoga or to avail both interventions together.
Further, we could not extract any data regarding the type of yoga interventions provided, duration of practice, or the detailed use of other supportive therapies, because a manual extraction of such data was not attempted on the ground that it would be extremely exhaustive to do a manual search owing to the individualistic nature of prescription practice in these settings. This remains one of the significant limitations of this present study. We could not collect any data regarding the characteristics of pain and its impact on patient activities of daily living. Such data may have added more value to the findings of this study.
Our study indicates that yoga was used along with other multiple therapies. These insights suggest that future yoga research should use pragmatic designs that can include the common ancillary treatments with yoga therapy, which can offer meaningful results. Nevertheless, such research should at least enquire about the use of additional therapies with yoga, which can strengthen prescription practices. Large-scale observational studies are warranted in the future that can include the factors influencing patients to avail yoga therapy and its diverse prescription practices.
Yoga therapy is used by patients for managing diverse pain conditions, of which a majority of patients receive yoga therapy for degenerative and autoimmune diseases. Yoga is commonly used as an integrative therapy along with naturopathy, physiotherapy, and ayurveda in clinical settings. The inferences from the present study will help in designing future pragmatic trials in yoga.
Publicly available datasets were analyzed in this study. Further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Institutional Ethics Committee of Sant Hirdaram Medical College of Naturopathy and Yogic Sciences for Women (F.No:12/SHMCNYS-IEC/P27/2022-23), Prakriti Shakti Clinic of Natural Medicine (CGH-PS/IRB/2022/2), and Morarji Desai Institute of Naturopathy and Yogic Sciences (MDINYS/IEC/2022/P7). The patients/participants provided their written informed consent to participate in this study.
PN was involved in the conceptualization, supervision, and writing of the manuscript. SK, AM, KB, DS, SS, DY, JK, KS, HS, and GT were involved in conceptualization, protocol development, and data collection. PK performed the formal analysis and was involved in writing the manuscript. All authors contributed to the article and approved the submitted version.
The authors would like to thank Cijith Sreedhar, Chief Medical Officer, and Suvith Vishnu Das, Medical officer of Prakriti Shakti Clinic of Natural Medicine, Kerala, for their support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpain.2023.1185280/full#supplementary-material
1. Cramer H, Ward L, Steel A, Lauche R, Dobos G, Zhang Y. Prevalence, patterns, and predictors of yoga use: results of a U.S. Nationally representative survey. Am J Prev Med. (2016) 50(2):230–5. doi: 10.1016/j.amepre.2015.07.037
2. Mishra AS, Sk R, Hs V, Nagarathna R, Anand A, Bhutani H, et al. Knowledge, attitude, and practice of yoga in rural and urban India, KAPY 2017: a nationwide cluster sample survey. Medicines. (2020) 7(2):8. doi: 10.3390/medicines7020008
3. Wren AA, Wright MA, Carson JW, Keefe FJ. Yoga for persistent pain: new findings and directions for an ancient practice. Pain. (2011) 152(3):477. doi: 10.1016/j.pain.2010.11.017
4. Gupta S, Gautam S, Kumar U, Arora T, Dada R. Potential role of yoga intervention in the management of chronic non-malignant pain. Evid Based Complement Alternat Med. (2022) 2022:5448671. doi: 10.1155/2022/5448671
5. Ministry of AYUSH. AYUSH Systems. Available at: https://main.ayush.gov.in/ayush-systems/.
6. Nair PMK, Nanda A. Naturopathic medicine in India. Focus Altern Complement Ther. (2014) 19(3):140–7. doi: 10.1111/fct.12125
7. Tewani GR, Sharma H, Nathani VV, Silwal K, Nair PMK. Adverse events reporting at naturopathy clinical settings: importance of accreditation systems in improving quality of care and patient safety. BMJ Open Qual. (2022) 11(4):2088. doi: 10.1136/bmjoq-2022-002088
8. Saleem SM. Modified Kuppuswamy socioeconomic scale updated for the year 2021. Indian J Foransic Community Med. (2021) 8(1):1–3. doi: 10.18231/j.ijfcm.2021.001
9. Downey RG, King CV. Missing data in Likert ratings: a comparison of replacement methods. J Gen Psychol. (1998) 125(2):175–91. doi: 10.1080/00221309809595542
10. Glass GV, McGaw B, Smith ML. Meta-analysis in social research. New Delhi: Sage (1981). Available at: https://www.jameslindlibrary.org/glass-gv-mcgaw-b-smith-ml-1981/
11. Rios R, Zautra AJ. Socioeconomic disparities in pain: the role of economic hardship and daily financial worry. Health Psychol. (2011) 30(1):58. doi: 10.1037/a0022025
12. Ikeda T, Sugiyama K, Aida J, Tsuboya T, Watabiki N, Kondo K, et al. Socioeconomic inequalities in low back pain among older people: the JAGES cross-sectional study. Int J Equity Health. (2019) 18(1):1–11. doi: 10.1186/s12939-019-0918-1
13. Effendy C, Silva JFDS, Padmawati RS. Identifying palliative care needs of patients with non-communicable diseases in Indonesia using the SPICT tool: a descriptive cross-sectional study. BMC Palliat Care. (2022) 21(1):1–8. doi: 10.1186/s12904-021-00896-y
14. Latour JM, Fulbrook P, Albarran JW. EfCCNa survey: European intensive care nurses’ attitudes and beliefs towards end-of-life care. Nurs Crit Care. (2009) 14(3):110–21. doi: 10.1111/j.1478-5153.2008.00328.x
15. Veziari Y, Kumar S, Leach M. Barriers to the conduct and application of research among complementary and alternative medicine professions in Australia and New Zealand: a cross-sectional survey. Complement Ther Med. (2021) 60:102752. doi: 10.1016/j.ctim.2021.102752
16. Patwardhan AR. Aligning yoga with its evolving role in health care: comments on yoga practice, policy, research. J Prim Care Community Health. (2017) 8(3):176–9. doi: 10.1177/2150131917690092
17. Elgelid S. Insurance reimbursement: what it might mean for the profession of yoga therapy. Int J Yoga Therap. (2001) 11(1):99–102. doi: 10.17761/ijyt.11.1.g87026671347x2v5
18. Salwa H, Nair PMK. Raising burden of non-communicable diseases: importance of integrating yoga and naturopathy at primary care level. J Complement Integr Med. (2020) 18(2):271–8. doi: 10.1515/jcim-2017-0019
19. Thomas A, Kirschbaum L, Crowe BM, Van Puymbroeck M, Schmid AA. The integration of yoga in physical therapy clinical practice. Complement Ther Med. (2021) 59:102712. doi: 10.1016/j.ctim.2021.102712
20. Datey P, Hankey A, Nagendra HR. Combined ayurveda and yoga practices for newly diagnosed type 2 diabetes mellitus: a controlled trial. Complement Med Res. (2018) 25(1):16–23. doi: 10.1159/000464441
21. Tilbrook HE, Cox H, Hewitt CE, Kang’ombe AR, Chuang LH, Jayakody S, et al. Yoga for chronic low back pain: a randomized trial. Ann Intern Med. (2011) 155(9):569–78. doi: 10.7326/0003-4819-155-9-201111010-00003
22. Sherman KJ, Cherkin DC, Wellman RD, Cook AJ, Hawkes RJ, Delaney K, et al. A randomized trial comparing yoga, Stretching, and a self-Care book for chronic low back pain. Arch Intern Med. (2011) 171(22):2019–26. doi: 10.1001/archinternmed.2011.524
23. Schmid AA, Fruhauf CA, Sharp JL, Van Puymbroeck M, Bair MJ, Portz JD. Yoga for people with chronic pain in a community-based setting: a feasibility and pilot RCT. J Evid Based Integr Med. (2019) 24. doi: 10.1177/2515690X19863763
24. Seguin-Fowler R, Graham M, Ward J, Eldridge G, Sriram U, Fine D. Feasibility of a yoga intervention to decrease pain in older women: a randomized controlled pilot study. BMC Geriatr. (2020) 20(1):1–12. doi: 10.1186/s12877-020-01818-y
25. Maheshkumar K, Venugopal V, Poonguzhali S, Mangaiarkarasi N, Venkateswaran ST, Manavalan N. Trends in the use of yoga and naturopathy based lifestyle clinics for the management of non-communicable diseases (NCDs) in Tamilnadu, South India. Clin Epidemiol Glob Heal. (2020) 8(2):647–51. doi: 10.1016/j.cegh.2019.09.013
26. Park CL, Braun T, Siegel T. Who practices yoga? A systematic review of demographic, health-related, and psychosocial factors associated with yoga practice. J Behav Med. (2015) 38(3):460–71. doi: 10.1007/s10865-015-9618-5
Keywords: yoga, pain, integrative medicine, palliative care, patient demographics, yoga adherence
Citation: Nair PMK, Kriplani S, Kodali PB, Maheshwari A, Bhalavat KD, Singh D, Saini S, Yadav D, Keswani J, Silwal K, Sharma H and Tewani GR (2023) Characteristics of patients who use yoga for pain management in Indian yoga and naturopathy settings: a retrospective review of electronic medical records. Front. Pain Res. 4:1185280. doi: 10.3389/fpain.2023.1185280
Received: 13 March 2023; Accepted: 19 May 2023;
Published: 15 June 2023.
Edited by:
Apar Avinash Saoji, Swami Vivekananda Yoga Anusandhana Samsthana, IndiaReviewed by:
Shijun Zhu, University of Maryland, United States© 2023 Nair, Kriplani, Kodali, Maheshwari, Bhalavat, Singh, Saini, Yadav, Keswani, Silwal, Sharma and Tewani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pradeep M. K. Nair ZHJwcmFkZWVwMThibnlzQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.