- 1College of Nursing, The Ohio State University, Columbus, OH, United States
- 2Department of Emergency Medicine, The Ohio State University College of Medicine, Columbus, OH, United States
- 3Department of Psychological Sciences, Purdue University, West Lafayette, IN, United States
- 4College of Nursing, University of Cincinnati, Cincinnati, OH, United States
- 5College of Pharmacy, University of Cincinnati, Cincinnati, OH, United States
Introduction: Patients are stakeholders in their own pain management. Factors motivating individuals to seek or use opioids therapeutically for treatment of acute pain are not well characterized but could be targeted to reduce incident iatrogenic opioid use disorder (OUD). Emergency departments (EDs) commonly encounter patients in acute pain for whom decisions regarding opioid therapy are required. Decision-making is necessarily challenged in episodic, unscheduled care settings given time pressure, limited information, and lack of pre-existing patient provider relationship. Patients may decline to take prescribed opioids or conversely seek opioids from other providers or non-medical sources.
Methods: Using a framework analysis approach, we qualitatively analyzed transcripts from 29 patients after discharge from an ED visit for acute pain at a large, urban, academic hospital in the midwestern United States to describe motivating factors influencing patient decisions regarding opioid use for acute pain. A semi-structured interview guide framed participant discussion in either a focus group or interview transcribed and analyzed with conventional content analysis.
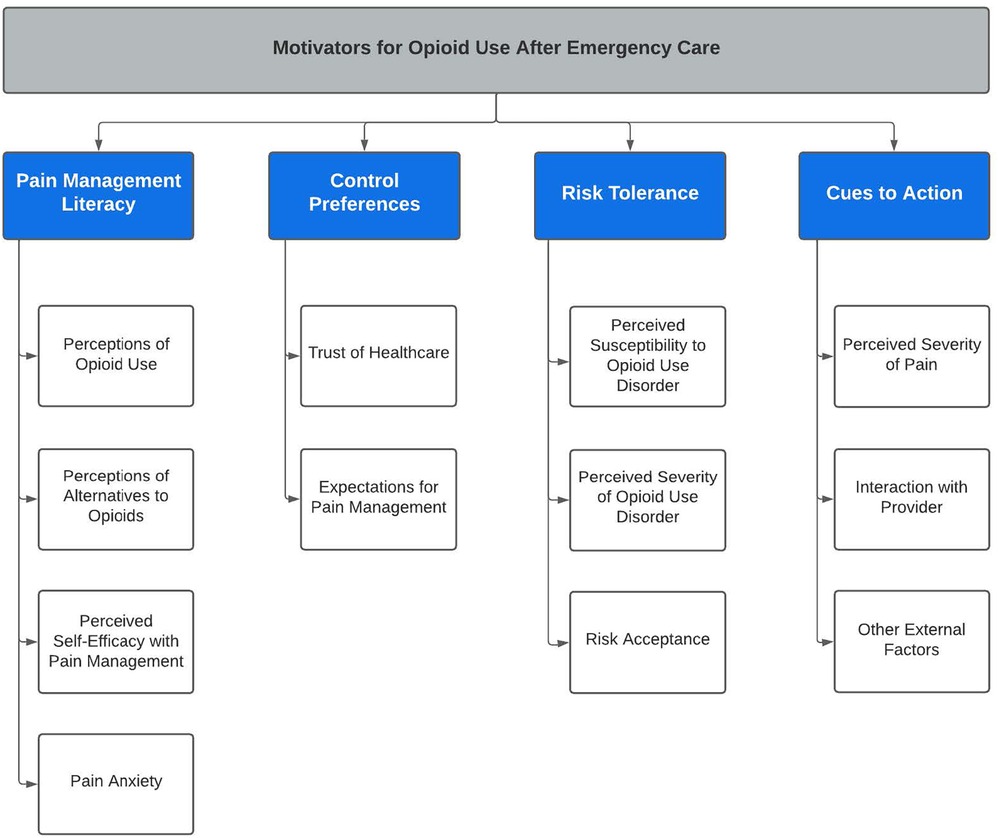
Results: Four major themes emerged from our analysis including a) pain management literacy, b) control preferences, c) risk tolerance, and d) cues to action.
Discussion: Our findings suggest targets for future intervention development and a framework to guide the engagement of patients as stakeholders in their own acute pain management.
1. Introduction
Opioid use disorder (OUD) incurs tremendous individual and societal costs (1–7). Healthcare costs associated with response to overdose emergencies as well as injuries and complications of OUD are also exorbitant (8). Increasing evidence indicates the development of OUD is frequently iatrogenic at least in part, whereby OUD is could be a consequence of opioid use that began as therapeutic (9–15).
This evidence surrounding opioid use and various policy initiatives have led to significant reductions in opioid prescribing with uncertain effects (9, 16–19). Presumably, there are still patients who receive therapeutic opioids that might be avoided, patients for whom therapeutic opioids cannot be avoided, and others denied opioids unnecessarily (20). Amidst ambiguity in balancing individualized OUD risk versus pain severity, shared-decision making in which patients are primary stakeholders in pain management decisions is likely to continue. At a minimum, patients are primary agents in the decision to seek or use opioids non-medically when pain is unmanaged through medical sources (20, 21). Emergency medicine prescribers are especially challenged. Patient-provider interactions in the emergency department (ED) are necessarily brief, often with limited information and no pre-existing or longitudinal patient relationship, all presenting barriers to risk assessment and shared decision-making (20, 22). Moreover, the risk of short-term, low-potency opioid therapy is even less well characterized than is opioid therapy for chronic pain management (10, 11, 23, 24).
Patients are stakeholders in their own pain management. Not only may they influence provider prescribing decisions, but they may also decline to take prescribed opioids or conversely seek opioids from other providers or non-medical sources. It follows that patients’ individual motivations to take or avoid opioids could be targeted for development of future interventions to reduce OUD or improve pain management. We sought to qualitatively describe motivating factors influencing ED patient decisions for opioid use when presenting for care in an acute pain.
2. Materials and methods
2.1. Design
This study is grounded in theoretical underpinnings of the Health Belief Model (25) and followed COREQ standards for qualitative research (26). A framework analysis method of qualitative analysis was used to explore motivating factors that influence patient decisions to use opioids after emergency care (27). This method was chosen for its ability to allow the data to emerge directly from the words of the participants but also place minimal interpretation on their thoughts. The study was approved by the local Institutional Review Board.
2.2. Setting and sample
Purposive sampling was used to recruit patients between August and December 2021 from an urban, academic, adult trauma center emergency department with approximately 75,000 visits annually.
Potential participants were screened for preliminary eligibility via the electronic health record during the ED visit, and were subsequently consented and enrolled by trained study staff. Participants were required to be at least 18 years of age, English-speaking, and having an ED visit related to acute pain (i.e., due to recent illness or injury). Participants were excluded if they were prisoners/in custody, previously enrolled, suicidal, lacked capacity to consent and participate, or pregnant/trying to conceive, but were not excluded for pre-existing opioid use disorder, chronic pain, or chronic opioid use. Participants completed baseline surveys and were scheduled for follow-up interview/focus group at approximately 7 days (±4 days) after ED discharge. Study staff scheduled focus groups (n = 5) with 2–3 participants based on similar histories of opioid exposure (e.g., opioid naïve, sporadic use, and consistent use) since prior exposure is intuitively associated with current perceptions of opioids. Individuals with similar histories of opioid use were brought together in focus groups. When an eligible participants prior opioid history was not consistent with a pending focus group, they were scheduled for individual interviews.
Participants completed a baseline questionnaire assessing sociodemographic characteristics, basic health information, and current substance use based on Diagnostic and Statistical Manual of Mental Disorders, 5th revision (DSM-5) criteria (28). All baseline data were collected and managed in a secure Research Electronic Data Capture (REDCap) system database (29). Participants received a $20 gift card for completing the survey in the ED.
2.3. Qualitative assessment
We used a semi-structured interview guide, informed by the Health Belief Model and previous literature (20) to assure that all participants received the same core questions during the interview. Interviews were conducted by two members of the study team, one of whom is a licensed social worker (NT) and the other a PhD prepared emergency nurse (BP). Conversations occurred via Microsoft Teams and were digitally recorded and subsequently transcribed and verified for accuracy. Focus group discussion lasted between 42 and 64 min and individual interviews ranged from 25 to 76 min. Although full study consent was obtained in the ED, the qualitative follow-up visit began with reiteration of study purpose and verbal consent for recording. In order to avoid stigma and response bias, question prompts asked participants to reflect on peer behaviors in the community generally, allowing participants to avoid self-report of their own behaviors. However, we allowed participants to describe their own thoughts, perceptions, and behaviors if desired. Participants received a $25 gift card for completing a focus group or interview.
2.4. Data analysis
Sample characteristics were descriptively analyzed. Using the framework analysis approach, two members of the research team coded categories with a predetermined code list (30, 31), allowing new concepts to emerge from the voice of the participants. In phase 1 (familiarization), the analysis team worked first independently and then together using an iterative content analysis approach (31), eventually achieving consensus in regard to important themes and ideas. Next, the team met to develop our thematic hierarchy (Figure 2). In phase 3 of analysis (indexing), the qualitative data were coded according to the developed thematic framework. During phase 4 (charting), we compiled direct quotes from the participants with their corresponding headings and definitions. Finally, in phase 5 (mapping and interpretation), the analysis team established supporting literature of the concepts in our thematic framework. We enrolled participants until we achieved redundancy in content, achieving thematic saturation (32). Any disagreements were brought to the other members of the research team and discussed until consensus was achieved. Credibility was upheld by minimizing investigator bias through adhering to inclusion criteria and maintaining an audit trail. Reliability was accounted for through standardized procedures, and confirmability was supported by triangulation of investigators and audit trail (32). The qualitative software NVIVO (QSR International, Burlington, MA) was used for the data analysis procedures.
3. Results
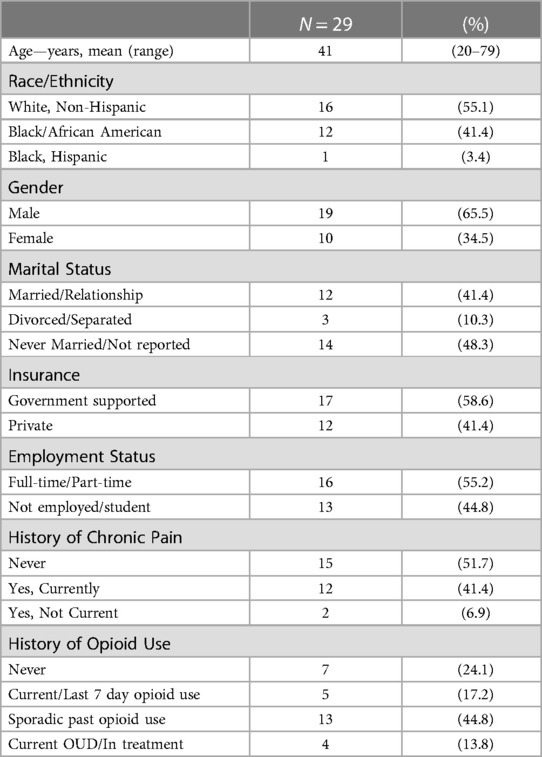
We approached 217 patients for eligibility, of which 62 (28.6%) were eligible and consented to procedures. Of the 29 participants who completed either a focus group (n = 11) or interview (n = 18), the majority were white (16, 55.1%) and male (19, 65.5%). Seven (24.1%) of the sample had never used opioids, and four (13.8%) had current OUD (Table 1). Four major themes emerged from the analysis (Figure 1), which represent motivating factors influencing patient decisions to use opioids for pain management. These themes include (a) pain management literacy, (b) control preferences, (c) risk tolerance, and (d) cues to action. There were no differences in themes across varying histories of opioid use.
3.1. Theme 1: pain management literacy
All participants described aspects of knowledge, attitudes, and beliefs about pain management including using opioids for pain and alternative therapies for pain management. Grounded in the Health Belief Model theoretical constructs of perceived susceptibility, severity, benefits, and barriers (25), we found that an individual’s pain management literacy combines their personal experiences and information gained from providers, family, and peers. There was also mention of other aspects of knowledge such as internet sources and schooling. Finally, perceptions of pain included pain management self-efficacy and pain anxieties for the ability to apply knowledge to manage their own pain.
3.1.1. Sub-theme: perceptions of opioid use
Participants frequently discussed beliefs and knowledge of opioids including their beliefs on why individuals would or would not take opioids for pain. This included benefits of opioids such as relieving pain, euphoric/pleasant feelings from the opioids, as well as being able to escape problems. Some stated sentiments of not being able to be in pain due to their commitments as a caregiver or needing to be able to work.
One participant stated, “(Opioid medication) helps. You know it doesn't take it totally away, but it makes it a point to where I can do everything that I need to do… You know to take care of my daughters effectively. Play with them, you know, to just have a normal life” (45 y/o black female).
There were also unique perspectives of use, “people tell me their sex drive, (that) they can last longer (when they take opioids). So some people take it just for that. Some people don't even take it for the pain” (40 y/o black male).
Reasons that would prevent opioid use for pain management included potential side effects such as nausea, grogginess, and not being able to think clearly. A participant described her side effects with opioids, “took one and then of course by that time I was getting nauseous. ‘cause that’s what they do, to me they make me sick at my stomach… Like I've had after surgery, I'll throw up. So they're not good for me to take anyway” (79 y/o white female).
Additionally, some brought up thoughts that some people may not take their opioid prescription medications due to the potential for diversion of opioids for financial reasons: “just getting pills just to sell them, and they might not necessarily take them but they know how to get money off them. I definitely say they’d do it” (53 y/o black male).
3.1.2. Sub-theme: access, awareness, and acceptance of alternatives to opioids
Individuals in the focus groups and interviews expressed varying knowledge and beliefs about alternatives to opioids. Participants generally expressed a lack of knowledge of and access to alternative therapies to opioids including confusion on types of pain medications that were non-opioids and available over the counter. When discussing awareness of alternative therapies for pain management, individuals mentioned learning from family members as well as a lack of knowledge about pain management outside of healthcare. Finally, individuals expressed sentiments that alternatives to opioids either do not work or take too long to work and requiring an immediate solution to the pain. The majority of the responses indicated financial factors playing into reasons for their use of alternatives to opioids.
3.1.2.1. Access
“And it tends to be with people who had just have more access (to alternatives to opioids), more money, and can afford it” (31 y/o white male).
3.1.2.2. Awareness
“I mean, I'm just being honest. In a daily family like, in a low (income) poverty family, they're not going to talk about something like (alternative methods for pain). Maybe in an upper-class neighborhood, but no, not in a low (income) poverty neighborhood, no” (47 y/o black female).
3.1.2.3. Acceptance
“At times (opioids are) the cheapest available…Like right now I'm struggling with this pain. I need to be at work (and) I don't have enough time to pursue my own healing and so you end up maybe giving into a pill that you can pop and feel better. A few hours pop another pill, as opposed to maybe getting sessions of physical therapy and extensive imaging to find out what’s really is the problem and therefore manage it appropriately” (53 y/o black male).
3.1.3. Sub-theme: perceived self-efficacy with pain management
In this subtheme, participants describe confidence and beliefs about their abilities to manage pain with or without opioids. This subtheme combines their application of knowledge and beliefs of opioids and alternatives to opioids in pain management. Some participants also noted generational acceptance of pain, “We get soft and we're not willing to deal with some pain, and like I can deal with some” (78 y/o White male), and a need for immediate pain relief, “we’re living in a microwave world so much that ‘I don't care. I just want this pain gone’” (28 y/o black male). Finally, participants described personal abilities to manage pain due to previous pain experiences:
“I'm not a big med taker in general, so I can endure some pain. I mean, as a side note, I have (…), so I am pretty much constantly in some type of discomfort. I am on medication for it, but it doesn't work” (51 y/o white female).
3.1.4. Sub-theme: pain anxiety
This refers to a person’s subjective perception of chances of and reactions to pain. This may include a fear of pain, “When it comes to (pain) I'm a baby, I have to get something for it” (27 y/o white female). Additionally, we found that some people confused the concept of pain and physiologic drug tolerance, stating they believed they had a high pain tolerance and therefore required very strong opioid medications:
“I have a very high tolerance for pain… they wanted me to take ibuprofen where ibuprofen don't do anything for me …They gave me hydrocodone and they didn't do anything …So I guess my pain level is more intense to other people to where I really need something really strong” (57 y/o black female).
3.2. Theme 2: control preferences
This domain describes individuals’ beliefs and trust surrounding healthcare as well as specific expectations surrounding pain management. Subthemes included in this domain are trust of health care and expectations for pain management. We found that individuals were explicit whether they were going to follow provider instructions versus display a distrust and skepticism for aligning with provider recommendations.
3.2.1. Sub-theme: trust of health care
The theme of trust in healthcare describes both the confidence and reliance in their healthcare provider’s decisions surrounding pain management and opioid use for the individual patient. Within this theme, participants described power dynamics and willingness to put faith in the medical provider’s decision as well as personal philosophies to approaching healthcare and medications. Participants described instances where they just went along with what the healthcare provider said, following instructions:
“I felt like I honestly at that point when they did the hydromorphone, I didn't really have an option or an ability to say, hey, let’s try something lower because I was feeling pain from my hand… I think I was trusting the situation more than advocating for myself” (51 y/o white female).
Additionally, some participants described skepticism and lack of trust related to the healthcare system:
“Just there’s a lack of trust. I think, uh, going on with medical community in general right now … and so it’s sort of seen as, a money, money and a prize and not actually healthcare enterprise” (31 y/o white male).
Finally, some participants stated that they didn’t like taking medication because it went against their personal beliefs:
“I'm not gonna take a bunch of medicine that makes me painless, because pain in our body is an alarm system that says there’s something wrong… I wouldn't take a pain medicine if I thought it was just gonna mask my problem and the problem wasn't going to go away” (78 y/o white male).
3.2.2. Sub-theme: expectations for pain management
The theme of expectations for pain management portrays beliefs and ideologies when approaching pain management. Within this theme, participants describe whether a diagnosis and pain were validated by the healthcare provider. Also embedded in this theme, participants stated that receiving a prescription pain medication that was not available over the counter was a method of validation of their individual concerns surrounding pain, “'cause they feel like the opioid is stronger and it’s gonna work better than like that regular medicine” (32 y/o black male). Another participant described the lack of validation of her symptoms, “I'm in terrific pain… for her not to give me any pain medicine … she didn’t take a x-ray or anything … I'm ready for a second opinion”. One participant discussed dissatisfaction when receiving an opioid prescription against his wishes:
“they prescribed an opioid. And when I specifically said I didn't want that, they still did not give me a different prescription or even want to have a conversation… but that still left a really bad taste in my mouth and especially because I made them aware of the reasons why I didn't want that prescription” (22 y/o white male).
3.3. Theme 3: risk tolerance
Participants describe aspects of risk tolerance including subthemes of risk acceptance, perceived severity of OUD, and perceived susceptibility to OUD. One participant said: “But I do not want to deal (with) the opioid at all. I was prescribed that one time and I felt… I didn’t feel comfortable…I mean the pain was subsided, but I was not feeling confident taking it, with a chance of me getting too addicted to it and everything else” (53 y/o black male). Notably, most of the participants agreed that opioid use disorder was a serious disease and many stated they knew of individuals who transitioned from opioid prescriptions to injection drug use.
3.3.1. Sub-theme: risk acceptance
This is when a participant describes being knowledgeable about the risks of opioid use and would choose to take an opioid for pain despite the known risks. This would include aspects of not caring about the risk, just wanting the pain gone, or believing that there would be a way to prevent or treat opioid use disorder. One participant stated, “if I'm in like 9 out of 10 out of pain and …a doctor prescribes me a … strong medicine that … could be addictive … I might take that risk just to get rid of that pain. … you're obviously going to take that step or take that risk“ (20 y/o white male). Another participant response described some of the thoughts that are considered when weighing benefits and risks of an opioid:
“Some people actually like the feeling of being high off the pain medicines or just feeling real relaxed. And they ain't gotta deal with the pain. And then you got some people that it’s like, ‘alright, I will on … how just pain medicine and you got me feeling good little bit from my pain’. But it’s like I don't wanna be like this all the time ‘cause now you interfering with other things in your life. It ain't just dealing with that right now, you interfering with other things. You might be too sleepy and miss something or you might be too drowsy to do something” (32 y/o black male).
3.3.2. Sub-theme: perceived severity of opioid use disorder (OUD)
This refers to a person’s feelings on the seriousness of developing OUD. The theme of perceived severity of OUD can include personal beliefs about OUD and the complications it has on individuals’ lives, violence and crime surrounding OUD, and their specific fears of developing OUD. An individual discussing both fear of addiction and awareness of severity stated:
“A lot of them just might not want to take (opioid prescription) because they see other people struggling. You know with (addiction), and they're like… I don't wanna do that to myself. I see these people out here, homeless, struggling, bumming for money. You know, don't know when they're going to get their next fix. So they're like hell I might as well throw them (pills) away because I don't want to be like that person” (27 y/o white female).
3.3.3. Sub-theme: perceived susceptibility to opioid use disorder
This refers to a person’s subjective perception of the risk of acquiring OUD. This theme combines traits and beliefs participants describe as affecting an individual’s vulnerability to OUD. Characteristics believed to increase susceptibility include personality, genetics/family history, friends, not having a ’strong mind’, not taking opioids as medically prescribed, and varying other beliefs such as ‘it won’t be me’. One participant stated, “a lot of people have pride to the extent that they think well other people, but not me” (25 y/o white male). Another person indicating that she was not at risk stated: “I won't worry about getting addicted because I know how strong my mind is” (57 y/o black female).
3.4. Theme 4: cues to action
This final theme describes an internal or external stimulus that can trigger the decision-making process in order to take an opioid for pain. Specific cues to action include subthemes of (1) perceived severity of pain, (2) interactions with providers, and (3) other external factors that influence their decision.
3.4.1. Sub-theme: perceived severity of pain
In this subtheme, participants detail components of pain severity that may motivate them to take an opioid for pain relief. During the discussions, aspects of interferences with sleep, daily activities, and work were prominent. Additionally, discussions of physical responses to pain such as crying or screaming were mentioned when relating the severity of pain to motivation to take an opioid. Several participants discussed that high levels of pain would motivate an individual to take a medication even if they initially did not intend to, as one participant stated, “there’s only so much pain your body can take and that’s why they have torture chambers to make you talk” (78 y/o white male). Another agreed, “people, if they're in enough pain, will cave to it, which can obviously create a pretty slippery slope” (25 y/o white male).
3.4.2. Sub-theme: interaction with provider
Participants reported mixed reactions when discussing pain management with their emergency care provider and their choices to use opioid after discharge. Of the participants interviewed, 31% (n = 9) stated that emergency care providers are prescribing fewer opioids now due to the opioid crisis and legislative changes. One participant stated:
“But if the pending on what type of pain there in… they may get a Vicodin or Percocet, but they're not gonna get a big quantity of it. ‘cause I mean, with the laws nowadays they don't prescribe pain meds like that anymore” (47 black female).
Notably, many participants thought that emergency care providers would be more likely to give opioid medications for pain management due to the hurried nature of emergency care: “because they wanna get them out (of) the emergency room. Quick, fast and in a hurry, so that’s a quick fix” (47 y/o black female) and with little information, “a lot of time (there) are options to find out what’s exactly wrong, and so just easier to treat the pain than it is necessary to treat whatever is underlying it. Not having a complete medical record” (31 y/o white male).
3.4.3. Sub-theme: other external factors
Participants also described other external motivators that cued them to take or not take an opioid for pain management. These external factors included friends and family members, “I had refused to (take the opioid), it took a lot of convincing from family as well as my doctors to do something, because it had came to the point to where I was in so much pain” (45 y/o black female). Additional external factors include stigma, societal acceptability, and fear of being labeled as a drug user, “I do believe that pain medication now has a stigma, because of everything you hear on social media, the news and any kind of reporting” (35 y/o white female).
4. Discussion
This study identified discrete categories of information, perceptions, and ultimately motivations that influence patient decisions to use opioids. Our qualitative analysis found four categories of patient motivators to use opioids including: pain management literacy, control preferences, risk tolerance, and cues to action. These results suggest potential targets to engage the patient as a stakeholder in their own acute pain management, either reducing or increasing opioid use depending on the desired outcome. Knowing key patient motivators for decisions to use opioids for acute pain after an emergency care visit may be foundational to the development of personalized, patient-centered interventions for acute pain after an emergency department (ED) visit.
The broad concept of health literacy includes the ability to understand, interpret, and apply health information and services to make informed decisions (33). Our findings on the importance of pain management literacy in patient decision-making aligns with other studies in which individuals with lower health literacy were more likely to misuse opioids, have higher levels of pain severity, and have increased catastrophizing (34, 35). Participants in our study had many misconceptions and knowledge gaps about pain, opioids, and alternatives to opioids. Preferences for uptake of pain management literacy included generational transfer of knowledge of pain management strategies andability to access health and pain management information online.
Control preferences refers to patient preferences for the degree of control in healthcare decision making. Participants vocalized preferences for control in pain management, combining their trust in healthcare as well as expectations for pain management as key to whether or not they would adhere to recommendations or seek opioids from alternative sources. Several participants varied in the source of their discontent in pain management, with some even upset they received opioids when they did not wish them. Our findings are consistent with previous studies describing discontent with pain management as a trigger to seek opioids from non-medical sources (20), as well as studies linking control preferences to clinical outcomes and satisfaction with care (36–38).
Participants were aware of potential risks of opioid use, though some focused on factors such as personality traits and family history rather than the opioids themselves. Having a “strong mind” and taking opioids as medically intended was thought to be protective. This finding is consistent with beliefs that OUD is a moral failing and stigmas against individuals who have developed OUD as having a “weaker mind” (39, 40). It was generally unclear how individuals translated their views of the role of risk factors into their own personal risk perception. This raises the critical importance of research to scientifically quantify individualized risk. It will not be useful to emphasize overall risks or safety of opioids in counseling sessions if individuals are prone to viewing their own risk as different from the general population.
Cues to action are considered either internal or external influences to trigger a decision to accept an action, such as taking an opioid medication (41). Participants stated that interactions with providers and advice from others such as family members influenced their actions and decisions to take opioids for pain. This finding is consistent with other literature where patient experience and interactions with providers have implications for healthcare outcomes beyond the ED encounter (20, 42–45). Moreover, it is important to consider that external influences beyond the ED encounter may influence opioid use for acute pain management. Risk counseling and shared decision-making strategies are important in opioid use mitigation; however, other influences outside of the provider’s control may trigger later opioid use.
Our findings should be considered in context with several limitations. We did achieve thematic saturation using a semi-structured interview guide, but qualitative research is an in-depth analysis of a sample that may not be generalizable to the larger population. The description of our setting and sample characteristics should inform transferability. Similarly, we are not able quantify prevalence of these patient-reported cognitive factors or to investigate strength of associations or mediating effects. Our findings may have been influenced by our thematic framework guided by the Health Belief Model and previous literature. Finally, while this study was focused on the patient perspective of opioid use, the authors note that external influences such as provider training, system-level factors, and societal views of pain care may inform patient experiences.
5. Conclusion
Our study provides a framework for understanding patient motivations to take or avoid opioids. This warrants future investigation to determine the prevalence of these factors, their associations and predictive capacity, and the degree to which these cognitive factors and behaviors are modifiable. This demonstrates potential targets for the development of future interventions to reduce OUD or improve pain management after emergency care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Cincinnati. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors have contributed sufficiently to the project to be included as authors. All authors contributed to the article and approved the submitted version.
Funding
Research reported in this paper was generously supported by the NIH/National Institute on Drug Abuse (K08DA049948, PI: B.P.; K24DA037109, PI: E.B.; R01DA047236, PI: E.B.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpain.2023.1151704/full#supplementary-material
References
1. Murphy SM, Polsky D, Lee JD, Friedmann PD, Kinlock TW, Nunes EV, et al. Cost-effectiveness of extended release naltrexone to prevent relapse among criminal justice-involved individuals with a history of opioid use disorder. Addiction. (2017) 112(8):1440–50. doi: 10.1111/add.13807
2. Krebs E, Urada D, Evans E, Huang D, Hser Y-I, Nosyk B. The costs of crime during and after publicly funded treatment for opioid use disorders: a population-level study for the state of California. Addiction. (2017) 112(5):838–51. doi: 10.1111/add.13729
3. Kozhimannil KB, Chantarat T, Ecklund AM, Henning-Smith C, Jones C. Maternal opioid use disorder and neonatal abstinence syndrome among rural US residents, 2007–2014. J Rural Health. (2019) 35(1):122–32. doi: 10.1111/jrh.12329
4. Dooley J, Ryan G, Finn LG, Bollinger M, Matsumoto C, Hopman WM, et al. Maternal opioid use disorder and neonatal abstinence syndrome in northwest Ontario: a 7-year retrospective analysis. Can J Rural Med. (2018) 23(2):39–45. PMID: 29547380
5. Schiff DM, Patrick SW. Treatment of opioid use disorder during pregnancy and cases of neonatal abstinence syndrome. JAMA Pediatr. (2017) 171(7):707–707. doi: 10.1001/jamapediatrics.2017.0854
6. Ko JY, Wolicki S, Barfield WD, Patrick SW, Broussard CS, Yonkers KA, et al. CDC grand rounds: public health strategies to prevent neonatal abstinence syndrome. MMWR Morb Mortal Wkly Rep. (2017) 66(9):242. doi: 10.15585/mmwr.mm6609a2
7. Faryar KA, Ancona RM, Reau Z, Lyss SB, Braun RS, Rademaker T, et al. HIV detection by an emergency department HIV screening program during a regional outbreak among people who inject drugs. PLoS One. (2021) 16(5):e0251756. doi: 10.1371/journal.pone.0251756
8. Peterson C, Li M, Xu L, Mikosz CA, Luo F. Assessment of annual cost of substance use disorder in US hospitals. JAMA Netw Open. (2021) 4(3):e210242–e210242. doi: 10.1001/jamanetworkopen.2021.0242
9. Butler MM, Ancona RM, Beauchamp GA, Yamin CK, Winstanley EL, Hart KW, et al. Emergency department prescription opioids as an initial exposure preceding addiction. Ann Emerg Med. (2016) 68(2):202–8. doi: 10.1016/j.annemergmed.2015.11.033
10. Punches BE, Ancona RM, Freiermuth CE, Brown JL, Lyons MS. Incidence of opioid use disorder in the year after discharge from an emergency department encounter. J Am Coll Emerg Physicians Open. (2021) 2(3):e12476. doi: 10.1002/emp2.12476
11. Punches BE, Stolz U, Freiermuth CE, Ancona RM, McLean SA, House SL, et al. Predicting at-risk opioid use three months after ed visit for trauma: results from the AURORA study. PLoS One. (2022) 17(9):e0273378. doi: 10.1371/journal.pone.0273378
12. Hayden JA, Ellis J, Asbridge M, Ogilvie R, Merdad R, Grant DG, et al. Prolonged opioid use among opioid-naive individuals after prescription for nonspecific low back pain in the emergency department. Pain. (2021) 162(3):740–8. doi: 10.1097/j.pain.0000000000002075
13. Hoppe JA, Kim H, Heard K. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med. (2015) 65(5):493–9. doi: 10.1016/j.annemergmed.2014.11.015
14. Barnett ML, Olenski AR, Jena AB. Opioid-prescribing patterns of emergency physicians and risk of long-term use. N Engl J Med. (2017) 376(7):663–73. doi: 10.1056/NEJMsa1610524
15. Daoust R, Paquet J, Gosselin S, Lavigne G, Cournoyer A, Piette E, et al. Opioid use and misuse three months after emergency department visit for acute pain. Acad Emerg Med. (2019) 26(8):847–55. doi: 10.1111/acem.13628
16. Administration UF and D. FDA Announces enhanced warnings for immediate-release opioid pain medications related to risks of misuse, abuse, addiction, overdose and death. FDA News Release. (2016). https://www.fda.gov/news-events/press-announcements/fda-announces-enhanced-warnings-immediate-release-opioid-pain-medications-related-risks-misuse-abuse
17. Bohnert AS, Guy Jr GP, Losby JL. Opioid prescribing in the United States before and after the centers for disease control and prevention’s 2016 opioid guideline. Ann Intern Med. (2018) 169(6):367–75. doi: 10.7326/M18-1243
18. Chou R, Turner J A, Devine E B, Hansen R N, Sullivan S D, Blazina I, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a national institutes of health pathways to prevention workshop. Ann Intern Med. (2015) 162(4):276–86. doi: 10.7326/M14-2559
19. Prevention CDC C for DC and. Vital signs: overdoses of prescription opioid pain relievers—united States, 1999–2008. MMWR Morb Mortal Wkly Rep (2011) 60(43):1487–92. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm22048730
20. Punches BE, Brown JL, Soliman S, Johnson KD, Freiermuth CE, Walker Q, et al. Patient pain experiences and the emergency department encounter: a qualitative analysis. Pain Manag Nurs. (2022) 23(4):391–6. doi: 10.1016/j.pmn.2022.03.012
21. Elphinston RA, Connor JP, de Andrade D, Hipper L, Freeman C, Chan G, et al. Impact of a policy change restricting access to codeine on prescription opioid-related emergency department presentations: an interrupted time series analysis. Pain. (2021) 162(4):1095–103. doi: 10.1097/j.pain.0000000000002115
22. Punches BE, Berger KM, Freiermuth CE, Soliman SA, Walker QT, Lyons MS. Emergency nurse perceptions of pain and opioids in the emergency department. Pain Manag Nurs. (2021) 22(5):586–91. doi: 10.1016/j.pmn.2021.05.003
23. Beauchamp GA, Nelson LS, Perrone J, Lyons MS. A theoretical framework and nomenclature to characterize the iatrogenic contribution of therapeutic opioid exposure to opioid induced hyperalgesia, physical dependence, and opioid use disorder. Am J Drug Alcohol Abuse. (2020) 46(6):671–83. doi: 10.1080/00952990.2020.1778713
24. Jeffery MM, Hooten WM, Hess EP, Meara ER, Ross JS, Henk HJ, et al. Opioid prescribing for opioid-naive patients in emergency departments and other settings: characteristics of prescriptions and association with long-term use. Ann Emerg Med. (2018) 71(3):326–36. doi: 10.1016/j.annemergmed.2017.08.042
25. Champion VL, Skinner CS. The health belief model. Health Behav Health Educ Theory Res Pract. (2008) 4:45–65.
26. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19(6):349–57. doi: 10.1093/intqhc/mzm042
27. Ritchie J, Spencer L. Qualitative data analysis for applied policy research. Analyzing qualitative data. Routledge, London: Routledge (2002):187–208.
28. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th edn. Arlington, VA: American Psychiatric Association (2013).
29. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42(2):377–81. doi: 10.1016/j.jbi.2008.08.010
30. Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. Los Angeles, CA: Sage (1994).
31. Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. (2013) 13(1):1–8. doi: 10.1186/1471-2288-13-1
33. Kindig DA, Panzer AM, Nielsen-Bohlman L. Health Literacy: a Prescription to end Confusion. Washington DC: National Academy of Sciences (2004). p. 4–16.
34. Gopinath B, Jagnoor J, Kifley A, Pozzato I, Craig A, Cameron ID. Health literacy and recovery following a non-catastrophic road traffic injury. BMC Public Health. (2022) 22(1):1–11. doi: 10.1186/s12889-022-13707-7
35. Rogers AH, Bakhshaie J, Orr MF, Ditre JW, Zvolensky MJ. Health literacy, opioid misuse, and pain experience among adults with chronic pain. Pain Med. (2020) 21(4):670–6. doi: 10.1093/pm/pnz062
36. Tarabochia M, Menendez ME, Ring D. Health literacy and decisional preferences in hand surgery. J Hand Surg. (2021) 46(1):70.e1–8. doi: 10.1016/j.jhsa.2020.08.008
37. Filardo G, Roffi A, Merli G, Marcacci T, Berti Ceroni F, Raboni D, et al. Patients control preferences and results in knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2017) 25(2):552–8. doi: 10.1007/s00167-016-4405-6
38. Matthias MS, Miech EJ, Myers LJ, Sargent C, Bair MJ. An expanded view of self-management: patients’ perceptions of education and support in an intervention for chronic musculoskeletal pain. Pain Med. (2012) 13(8):1018–28. doi: 10.1111/j.1526-4637.2012.01433.x
39. Adams JM, Volkow ND. Ethical imperatives to overcome stigma against people with substance use disorders. AMA J Ethics. (2020) 22(1):E702–708. doi: 10.1001/amajethics.2020.702
40. McCarthy M. US Must address addiction as an illness, not as a moral failing, surgeon general says. Br Med J. (2016) 355:i6265. doi: 10.1136/bmj.i6265
41. Strecher VJ, Rosenstock IM. The health belief model. Camb Handb Psychol Health Med. (1997) 113:117.
42. Edmondson D, Shimbo D, Ye S, Wyer P, Davidson KW. The association of emergency department crowding during treatment for acute coronary syndrome with subsequent posttraumatic stress disorder symptoms. JAMA Intern Med. (2013) 173(6):472–5. doi: 10.1001/jamainternmed.2013.2536
43. Konrad B, Hiti D, Chang BP, Retuerto J, Julian J, Edmondson D. Cardiac patients’ perceptions of neighboring patients’ risk: influence on psychological stress in the ED and subsequent posttraumatic stress. BMC Emerg Med. (2017) 17(1):1–7. doi: 10.1186/s12873-017-0144-3
44. Punches BE, Johnson KD, Acquavita SP, Felblinger DM, Gillespie GL. Patient perspectives of pregnancy loss in the emergency department. Int Emerg Nurs. (2019) 43:61–6. doi: 10.1016/j.ienj.2018.10.002
Keywords: opioid, acute pain, decision-making, emergency care, patient preferences
Citation: Punches BE, Brown JL, Taul NK, Sall HA, Bakas T, Gillespie GL, Martin-Boone JE, Boyer EW and Lyons MS (2023) Patient motivators to use opioids for acute pain after emergency care. Front. Pain Res. 4:1151704. doi: 10.3389/fpain.2023.1151704
Received: 26 January 2023; Accepted: 11 September 2023;
Published: 25 September 2023.
Edited by:
Paul Geha, University of Rochester, United StatesReviewed by:
Calia A. Morais, University of Alabama at Birmingham, United StatesTony L. Yaksh, University of California, United States
© 2023 Punches, Brown, Taul, Sall, Bakas, Gillespie, Martin-Boone, Boyer and Lyons. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brittany E. Punches UHVuY2hlcy41QG9zdS5lZHU=
 Brittany E. Punches
Brittany E. Punches Jennifer L. Brown3
Jennifer L. Brown3 Natalie K. Taul
Natalie K. Taul