- 1Johns Hopkins School of Nursing, Baltimore, MD, United States
- 2Johns Hopkins School of Nursing Center for Innovative Care in Aging, Baltimore, MD, United States
- 3Xiangya School of Nursing, Central South University, Changsha, China
- 4Department of Orthopaedic Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, United States
Background: Nearly 50% of Americans aged 65 and above have been diagnosed with arthritis and an estimated 80% of adults experience low back pain (LBP). Little is known about the experience of LBP in older adults with arthritis and its relationships with mental and physical health.
Objective: In this study, we examined the relationships between LBP and four physical and mental health conditions (psychological distress, insomnia, mobility limitations, and self-rated health) in older adults with arthritis in the National Health and Aging Trends Study (NHATS). We also examined whether vigorous exercise mediated the relationships between LBP and these four conditions.
Materials and Methods: The data from this study comes from waves five through nine of the NHATS. The sample size ranged from 3,490 to 2,026 across these waves. All variables in this study are based on self-report. We used descriptive analyses including means and standard deviations for continuous variables or frequencies and proportions for demographic data. We used structural equation modeling (SEM) to examine if vigorous activity mediated the relationship between LBP with the four conditions.
Results: The age range of the sample was 65 years of age and older. Among those with back pain 78.53% had no mobility limitations. There was a significant relationship between LBP with insomnia (B = 0.48, p < 0.001), perceived health status (B = −0.38, p < 0.0010), and psychological distress (0.67, p < 0.001). Activity mediated the relationship between LBP and insomnia, psychological distress and physical health in adjusted models.
Discussion: The presence of low back pain in older adults with arthritis increases the risk of insomnia, psychological distress, mobility limitations, and poorer self-rated health. Consequently, targeting comorbid LBP may be an important component of the treatment plans of older adults with arthritis. In addition, providers of patients with arthritis and LBP should conduct routine assessments of mental and physical health to ensure the LBP is being adequately addressed.
Introduction
Low back pain (LBP) is the single leading cause of disability worldwide, affecting ~540 million people at any given time (1). In the United States, back pain is the most common type of musculoskeletal pain reported by older adults and an estimated 80% of adults experience low back pain (LBP) at some point in their lives (2). In addition to disability, it is well-documented that pain, especially musculoskeletal-related pain, is associated with limitations in mobility, worsened mental health, insomnia, and poorer self-rated health (3–7).
LBP, chronic or otherwise, is commonly associated with musculoskeletal comorbidities such as osteoarthritis (OA), rheumatoid arthritis, and osteoporosis, and various factors exacerbate LBP irrespective of the associated musculoskeletal comorbidity (8–11). The interaction of OA (e.g., of the hip, knee, and spine) with chronic LBP contributes to increased disability, possibly due to exacerbation of pain (12–19).
Among the common suggested treatments for LBP is vigorous activity; however, little is known about overall effectiveness of vigorous activity for treating pain and related symptoms. Findings are mixed regarding exercise and outcomes typically associated with LBP (20–25). In young- and- middle-aged adults, vigorous activity moderate to high levels of exercise/activity has been shown to buffer insomnia related to back pain (25). In one study, researchers reported that cycling reduced the risk of LBP over time (20, 24). Researchers have examined whether exercise is related to mental health outcomes, sleep and disability in individuals with LBP (22–24); however, few researchers have looked at exercise as the potential mediator between LBP and these associated conditions. Further understanding the effects of vigorous activity on common LBP and related conditions in older adults may help identify if similar buffering effects occur in older populations. In addition, the benefits of physical activity in older adults with LBP may have positive spillover effects onto mental and physical health conditions related to back pain.
The present study is grounded in the biopsychosocial model of pain (26). This model asserts that, although there is a physiological response to pain, the way in which a person experiences or perceives pain is based on multiple factors including biological or genetic composition, prior learning, and sociocultural and psychological influences (26). Per Wachholtz et al. (27), “This model facilitates an approach to the treatment of medical illness and pain that recognizes the complex interactions between individuals and their environment, as well as the potential bidirectional pathways between psychological and biological factors with regard to disease.” Regarding physical factors, LBP is known to be a key contributor to the global burden of disability. Vigorous activity has been shown to counteract pain catastrophizing, strengthen muscles and bones, help people with pain return to adaptive activity, and ultimately reduce pain in some circumstances (28–30). Hence, we conceptualized physical activity as a potential mediator in our analyses. Specifically, we examine vigorous activity as a hypothesized mediator, which may be related to psychological and psychosocial outcomes. Regarding variables we identified variables from the physiological, psychosocial, and biological domains that are related to LBP. Insomnia has been identified as a CNS pain generator in persons with chronic low back pain (31), and as an it is classified as a psychophysiological disorder, and we also felt it fit within the psychological component of the biopsychosocial framework as an evidence-based outcome variable in our model. Mobility limitations are often the body's response to various conditions and has been linked to LBP. We classify this as a physiological response to pain (32). Self-rated health has been identified as a psychosocial factor related to LBP and the prognosis of LBP in previous work (33, 34). We categorized self-rated health as a psychosocial factor associated with LBP for this study.
Identifying conditions related to LBP in older adults may elucidate how they are experiencing or living with their pain. A better understanding of consequences specific to LBP in older adults can assist with intervention development that will address not just LBP but potentially associated conditions as well.
This study examines the relationship of LBP with mobility limitations, psychological distress, insomnia, and self-rated health status in order to more clearly define the burden experienced by older adults with arthritis over a 6-year period. We specifically examine if vigorous activities are mediating factors within the biopsychosocial model of pain. We hypothesize that (1) LBP will be independently associated with more mobility limitations, insomnia, psychological distress, and poor self-rated health, and (2) vigorous activity will mediate the relationship between LBP with mobility limitations, insomnia, psychological distress, and poor self-rated health.
Methods
Procedures and data collection
Data for this study were collected as part of the National Health and Aging Trends Study (NHATS), a nationally representative sample of Medicare beneficiaries ages 65 and older. The sampling frame included all persons enrolled in Medicare, representing 96% of U.S. Medicare beneficiaries, and excluded 4% of older adults ineligible for Medicare for various reasons (27). A stratified, three-stage design was implemented for participant selection, first drawing from counties/groups of counties, then ZIP codes, and lastly from Medicare beneficiaries enrolled as of September 30, 2010 (35). The NHATS is an ongoing study with data collection occurring on an annual basis beginning in 2011. Measures collected include information on participants' physical capabilities, economic status, cognition, living arrangements, wellbeing, and activity engagement, among other variables. More detailed information related to the NHATS design and recruitment procedures is available elsewhere (35, 36). We included NHATS participants from waves 5–9 (2015–2019) who were living in the community and reported having arthritis at the time of data collection. The inclusion criteria were: (1) age 65 and above, (2) community-dwelling, and (3) comorbid diagnoses of arthritis and low back pain.
Instruments
Pain
Back, knee, and hip pain were measured by a yes/no question asking if respondents had been bothered by pain in the last month, and a follow-up question asking participants to specify the site(s) of pain.
Mobility limitations
Participants were asked if they had difficulties or needed help with going outside, getting around outside, or getting in and/or out of bed. For the demographics we examined the number of mobility limitations. For the mediation analysis a binary mobility limitation variable was created that indicated difficulties or no difficulties with mobility. Each mobility item was binary coded and a total number was calculated to represent the number of mobility limitations a participant had.
Psychological distress
Participants were asked “over the last month, have you ever felt down/depressed/anxious?” The scores of these two items were averaged to represent the severity of depression (range from 0 to 6). In accordance with the PHQ-2 criteria, participants were classified as having depressive symptoms if the cumulative score for both items was 3 or more (37).
Insomnia
Difficulty initiating sleep and difficulty maintaining sleep were determined by asking the questions “How often does it take you more than 30 min to fall asleep at night?” and “How often do you have trouble falling back to sleep on nights after waking up from sleep?” Responses to these questions included 0 (never), 1 (rarely), 2 (some nights), 3(most nights), and 4 (every night). The total score ranged from 0 to 8, with a higher total score stands for more insomnia.
Health status
Participants' self-rated health was measured by a single question asking them to rate their general health using a Likert scale where 4 indicates “excellent health” and 0 indicates “poor health”. Higher scores indicate worse self-rated health.
Vigorous activity
Participants' self-report of participation in physical activities was a dichotomous (yes/no) variable assessed by a single question asking, “In the last month, did you ever spend time on vigorous activities that increased your heart rate and made you breathe harder?” Sample activities included working out, swimming, running, biking, or playing a sport.
Potential covariates
We sought to understand the association of LBP with mobility limitations, psychological distress, and insomnia in older adults with arthritis and to determine whether vigorous activity would mediate those associations. Potential covariates were identified by consulting the literature. Fehrmann et al. (38) examined age and gender as moderators on the influence of chronic LBP on activities, participation, and environmental factors. We also adjusted for age, gender, highest level of education, and marital status.
Statistical analyses
Descriptive analyses, including means and standard deviations for continuous variables or frequencies and proportions for categorical variables, were used to summarize the demographic and functional characteristics of the samples from 2015 to 2019. Independent t-tests for continuous variables and chi-square tests for categorical variables were used to compare demographic characteristics and health-related variables for persons with and without self-reported back pain.
This study applied structural equation modeling (SEM) to examine the association of back pain (distinct from other pain) with psychological distress, insomnia, and self-rated health status and random effect logit models to examine the association of back pain with mobility limitations. These models adjusted for potential confounding covariates as previously defined. The main constructs in this study (e.g.., back pain, vigorous activities, and health outcomes) were measured at each point of time. For example, the latent variable pain was measured by back pain status from the fifth to ninth waves. By using latent variables in SEMs, we could also see the impact of each measurement over time.
Across all models, the latent pain variable served as the independent variable, vigorous activities were applied as the mediating variable, and health outcomes were integrated into the SEM model as the dependent variable. In the models, the direct effects from pain to vigorous activities are marked as a, the direct effects from vigorous activities to health outcomes are marked as b, the direct effects from pain to health outcomes are marked as c. The indirect effects are calculated by multiplying a and b (a*b). Missing values in the data set were handled using maximum likelihood estimation. Data management and analyses were all performed using R (ver.4.1.2) and the Laveran package (ver.0.6-9).
Results
Sample demographic characteristics
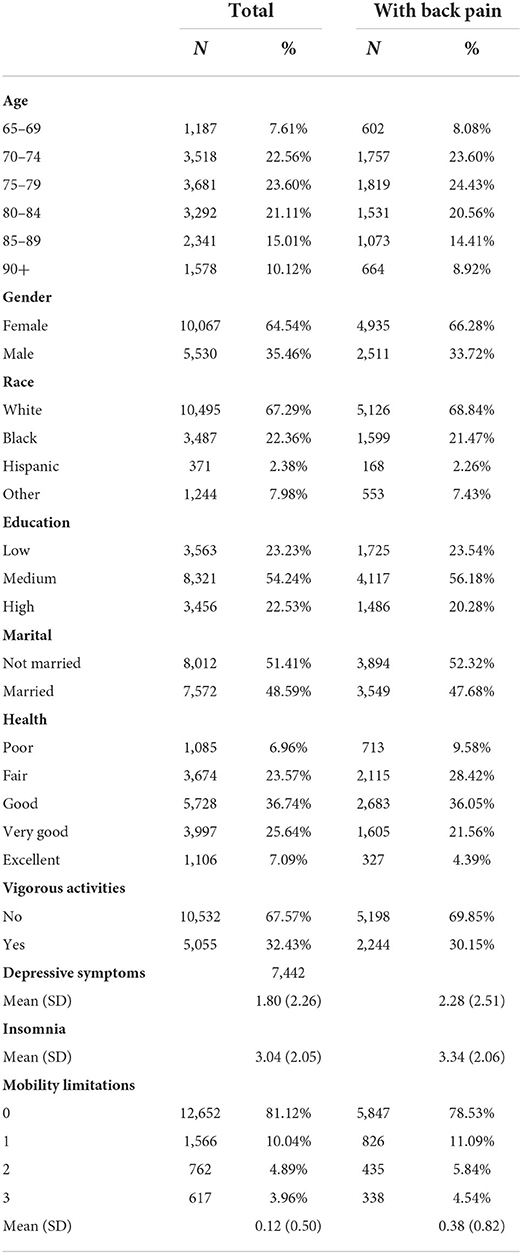
Table 1 provides descriptive characteristics for the total sample of older adults with arthritis and by the presence of LBP. At the baseline wave in 2015, respondents were primarily female (64.54%), White (67.29%), and 48.59% lived with a spouse, partner, or others. Most of the participants engaged in little-to-no vigorous activity on a regular basis (67.57%). White older adults were significantly more likely to report back pain (p = 0.021) than non-Whites. Among older adults with LBP, psychological stress scores were higher (p < 0.001), insomnia levels were higher (p < 0.001), poorer health was reported (p < 0.001), and more mobility limitations were reported (p < 0.001), compared to older adults without LBP conditions.
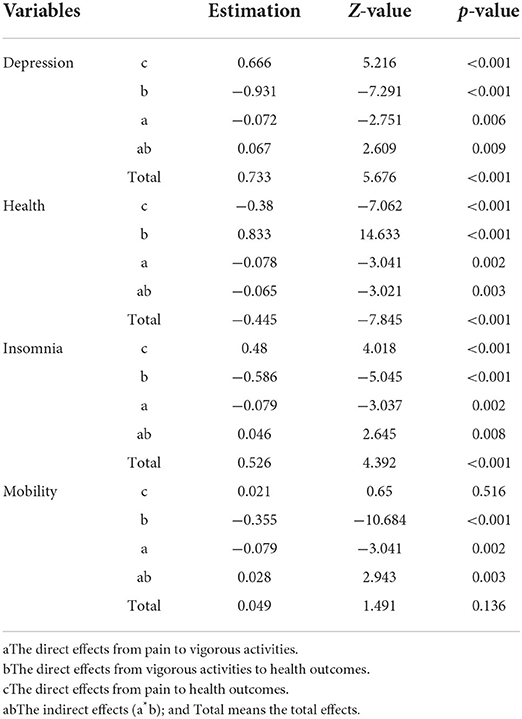
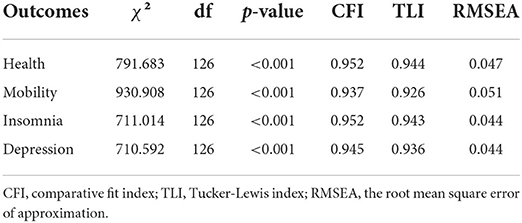
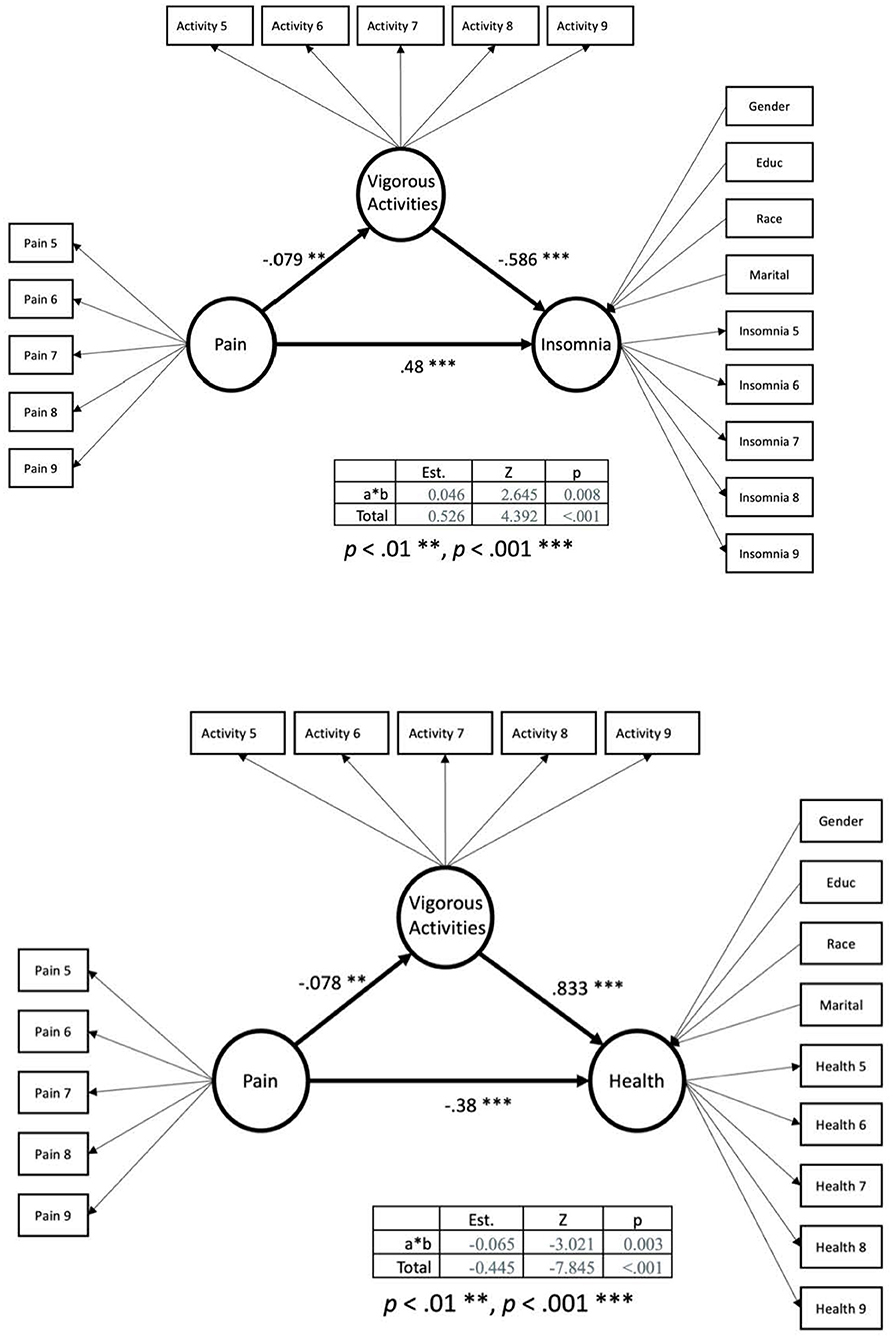
Mediation of the relationship between back pain and outcome variables
Table 2 summarizes the results from the mediating models. Table 3 summarizes the model fit for the four mediating models. In Figure 1 the SEM models of the mediation modeling are presented looking at vigorous activities mediating the relationship between pain and depression and pain and mobility. In Figure 2 the SEM models of the mediation modeling are presented looking at vigorous activities mediating the relationship between pain and insomnia and pain and health.
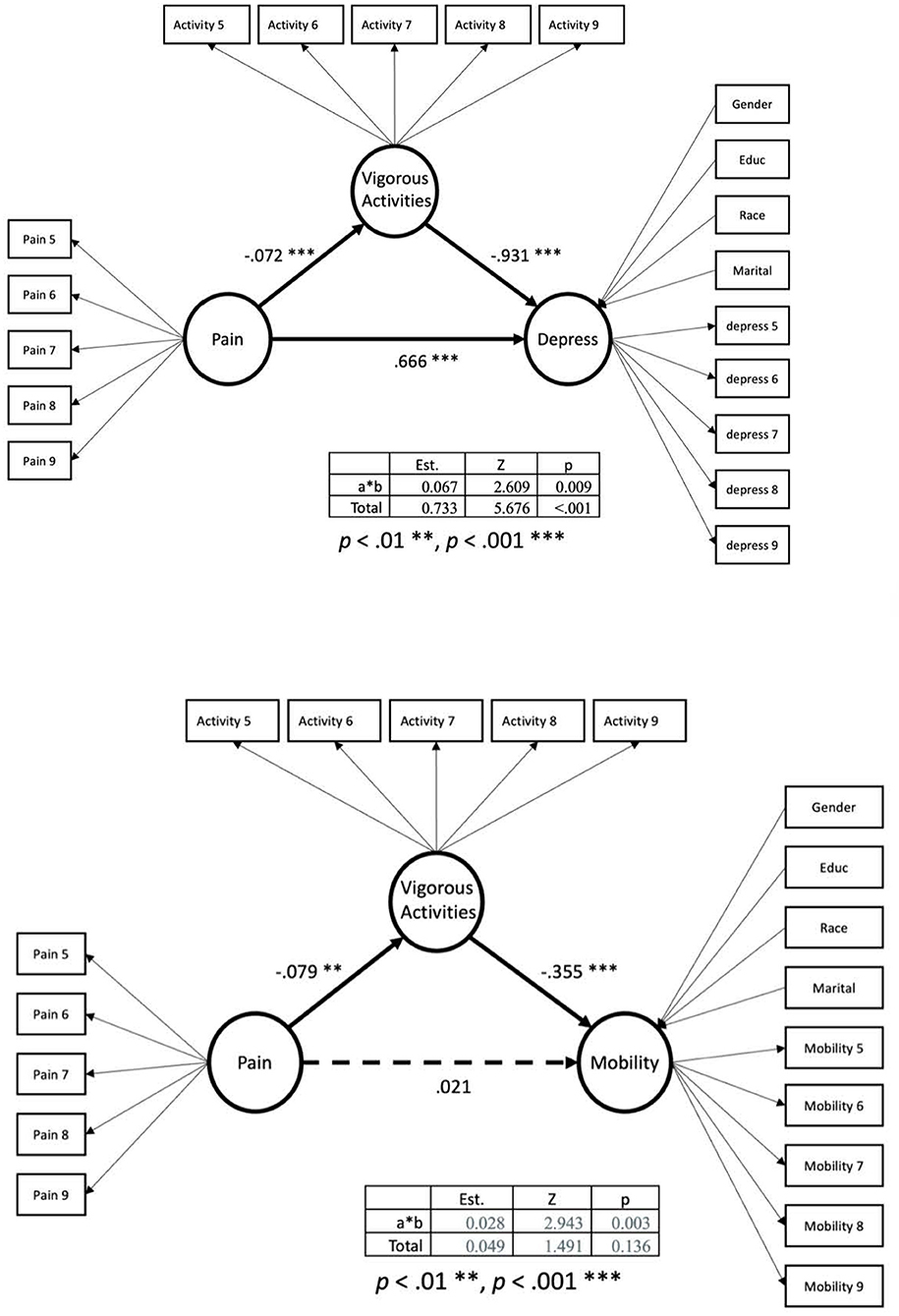
Figure 1. Mediation model with vigorous activities mediating relationship between pain and mobility.
According to Hu and Bentler (39), a good model fit is characterized as having a value close to 0.95 for TLI and CFI and a value smaller than 0.06 for RMSEA. The values of model fit for the mediating model for health were, χ2 = 791.683, df = 126, p < 0.001, CFI = 0.952, TLI = 0.944, and RMSEA = 0.047, indicating that the model is well fit. All loadings from observations to latent variables were statistically significant. Back pain was negatively associated with the perceived health status of community-dwelling older adults with arthritis, B = −0.38, z = −7.06, p < 0.001, indicating that having back pain was related to poorer perceived health status. In addition, back pain was also negatively associated with older adults' level of vigorous activities, B = −0.078, z = −3.04, p = 0.002. Vigorous activities were positively associated with the health status, B = 0.833, z = 14.63, p < 0.001. The total effect from back pain to health status was −0.445 and the indirect effect was −0.065, indicating that about 15% of the effect from back pain to the health status of community-dwelling older adults with arthritis was mediated by their levels of vigorous activities.
The model fit of the mediating model for depressive symptoms was a strong model, χ2 = 710.592, df = 126, p < 0.001, CFI = 0.945, TLI = 0.936, and RMSEA = 0.044. Back pain correlated with higher levels of depressive symptoms by 0.67, z = 5.22, p < 0.001, demonstrating that back pain may increase the depressive symptoms. Additionally, back pain was negatively correlated to the level of vigorous activities, B = −0.072, z = −2.75, p = 0.006. The total effects from back pain to depressive symptoms were 0.733, p< 0.001, and the mediating effect was 0.049, p = 0.067. The proportion of mediated effects was 9.14%.
The third model tested the level of insomnia as the outcome variable and demonstrated a strong model fit, χ2 = 711.014, df = 126, p < 0.001, CFI = 0.952, TLI = 0.943, and RMSEA = 0.044. Back pain was still statistically and significantly predictive of the levels of insomnia and vigorous activities, with B = 0.48, z = 4.02, p < 0.001, and B = −0.078, z = −3.04, p = 0.002, respectively. Vigorous activities were related to lower levels of insomnia, B = −0.586, z = −5.05, p < 0.001. The indirect effect from back pain to insomnia was 0.046 while the total effects were 0.526, showing a 9% mediating effects.
The model fit was acceptable, χ2 = 930.908, df = 126, p < 0.001, CFI = 0.937, TLI = 0.926, and RMSEA = 0.051. Back pain was not associated with changes in mobility whereas vigorous activities were negatively related to mobility. The total effects from back pain to mobility were not statistically significant.
Discussion
Vigorous activity may improve back pain (40); hence, we hypothesized that vigorous activity would mediate the relationship between LBP and four health outcomes, i.e., mobility, psychological distress, insomnia, and self-rated health. Our findings did support that vigorous activities mediated the relationship between LBP with psychological distress, insomnia and self-rated health. Our findings did not support vigorous activity as a mediator between LBP and mobility.
As it was documented in the literature vigorous activity may be beneficial for LBP, however, we have identified that it may also benefit other aspects of health related to back pain such as sleep, mental health and self-rated health. The findings from this study support that there are likely secondary benefits to engaging in vigorous activity among older adults with osteoarthritis and LBP. It is important to consider that the benefits of activity may take time to manifest in older adult populations (32). For example, an older adult may not feel pain relief or see weight loss changes or improved muscle strength until after participating in vigorous exercises long term.
Future directions for research include examining other sociocultural and psychological influences that are related to LBP and health outcomes. Factors such as pain catastrophizing, stigma, access to health care and biases and stereotypes may be related to LBP and mental health or physiological conditions. Information about these factors may lead to understanding of other treatment strategies that could be paired with vigorous exercise to better treat LBP and associated conditions. Utilizing vigorous exercise with a mental health treatment may be an effective way to address the disabling effects of LBP and related physical and mental outcomes. Researchers can further test interventions that include physical, psychological, social, and health-related quality-of-life domains in addition to vigorous activity treatments of pain given that all of these domains shape a person's pain experience based on the biopsychosocial model of pain.
Clinical implications
This study showed further support for the relationships between LBP and co-occurring conditions. The results suggest that vigorous exercise may contribute to improved outcomes in the areas of mobility, psychological distress, insomnia, and self-rated health for persons with arthritis and LBP. Findings also highlight the burden of health conditions related to LBP, which may have implications for designing intervention studies for LBP. While prior studies have targeted back pain in isolation (42), it is important to treat the associated conditions as well including mobility limitations, psychological distress, and insomnia. Concomitant treatment of LBP and its comorbidities in older adults may better alleviate pain and improve quality of life and self-rated health. Unfortunately, to date, very few studies have examined interventions that treat both back pain and its associated conditions (43). Multidisciplinary-based rehabilitation should also be considered when treating LBP, given the psychological and physical factors associated with LBP (44).
It is unlikely that any one intervention will be uniformly beneficial for all older adults with LBP and associated conditions. Consequently, future research should focus on tailored interventions that may include individualized plans for each participant (41). These tailored intervention studies for adults with LBP should also have large sample sizes and target depression, fatigue/sleep, and mobility (45, 46). Future research is needed to identify effective ways to treat back pain and related conditions during times, such as the COVID-19 pandemic, when in-person visits and in-person physical therapies are less accessible for older adults with LBP (47). Self- management interventions that incorporate goal setting and tailored physical activities may be appropriate and sustainable for older adults living with back pain (48).
Clinicians play a key role in assisting patients with LBP in managing their pain and associated conditions. Understanding mechanisms that cause LBP may also be integral to determining the best treatment decisions for each patient. Translating current and future evidence into practice will allow clinicians to prescribe evidenced-based tailored interventions. Clinicians treating LBP should also check for the presence of associated conditions, including depression, insomnia, and mobility limitations, in order to develop a comprehensive treatment plan that will maximize the patient's quality of life. Due to the relationships that LBP has with psychological and psychosocial outcomes, incorporating a biopsychosocial approach into clinical practice may be an essential component for managing low back pain (49).
Limitations and strengths
Several potential limitations were identified. First, the pain measure included in our study only assessed for the presence of pain over the preceding month. This measure does not capture chronic pain or provide in-depth description of the pain (e.g., dull and sharp). The measures for exercise and mobility limitations were coded as dichotomous variables, which is a potential limitation as well. Use of dichotomous coding for these two variables does not provide detail on the frequency or type of exercise or the severity of the mobility limitations. The findings should be interpreted with caution given the limitations of the outcome variables in the study. Furthermore, osteoarthritis in other joints such as the hip can contribute to or co-occur with back pain, and this mechanism should be further explored in older adults (50). It is possible that those with LBP were unable to engage in vigorous activity, in which case it would have no bearing on associated outcomes examined in this study. We did not account for medications the participants may have been taking, which is also a limitation. If the participants were taking medications for pain, insomnia, or to treat mental health conditions this may have influenced their outcomes in the study. Despite these potential limitations, the study has several strengths of note. The large, nationally representative sample of Medicare beneficiaries provides the ability to compare back pain to other common sites of musculoskeletal pain in older adults with arthritis. This nationally representative sample also enables generalization of findings to the U.S. older adult population.
Lastly, this study demonstrated that LBP over time is related to increased mobility limitations, psychological distress, insomnia, and poorer self-rated health. This highlights the important implications that LBP can have on quality of life and disability outcomes in aging adults (35).
Conclusions
Pain, particularly in older adults, is a complex condition to treat, and not all pain can and/or should be treated with the same approach. Given the high prevalence of arthritis in older adults, the increased risk of disability if low back pain is simultaneously present, and the difficulty pinpointing the root cause of LBP, it is essential that researchers continue to examine what conditions are comorbid with LBP in this population as this may elucidate underlying pain mechanisms and suggest targets for intervention.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://nhats.org/researcher/data-access.
Ethics statement
The studies involving human participants were reviewed and approved by Johns Hopkins Internal Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
JT and RS contributed to conception and design of the study. QL and ML conducted statistical analysis. JT and NR wrote the first draft of the manuscript. JT, NR, and QL wrote sections of the manuscript. SS assisted with edits and development of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
JT was supported by the Robert Wood Johnson Harold. Amos Medical Faculty Program; NR was supported by the National Institute on Aging (K23AG058809); RS was supported by the NIH National Institute on Aging under Award (P01AG066603). QL was supported from the National Institute on Disability, Independent Living, and Rehabilitation Research (90RTGE0003). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this publication do not necessarily represent the policy of NIDILRR, ACL, or HHS, and you should not assume endorsement by the Federal Government.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388:1545–602. doi: 10.1016/S0140-6736(16)31678-6
2. Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from US national surveys 2002. Spine. (2006) 31:2724–7. doi: 10.1097/01.brs.0000244618.06877.cd
3. McKillop AB, Carroll LJ, Jones CA, Battié MC. The relation of social support and depression in patients with chronic low back pain. Disabil Rehabil. (2017) 39:1482–8. doi: 10.1080/09638288.2016.1202335
4. Park S, Kim H, Jang S, Kim H, Chang BS, Lee CK, et al. Depression is closely associated with chronic low back pain in patients over 50 years of age: a cross-sectional study using the sixth Korea national health and nutrition examination survey (KNHANES VI-2). Spine. (2018) 43:1281–8. doi: 10.1097/BRS.0000000000002595
5. Patel KV, Phelan EA, Leveille SG, Lamb SE, Missikpode C, Wallace RB, et al. High prevalence of falls, fear of falling, and impaired balance in older adults with pain in the United States: findings from the 2011. National health and aging trends study. J A Geriatr Soc. (2014) 62:1844–52. doi: 10.1111/jgs.13072
6. Weiner DK, Rudy TE, Morrow L, Slaboda J, Lieber S. The Relationship Between Pain, Neuropsychological Performance, and Physical Function in Community-Dwelling Older Adults with Chronic Low Back Pain. Pain medicine (2006) 7, pp.60–70.
7. Bahouq H, Allali F, Rkain H, Hmamouchi I, Hajjaj-Hassouni N. Prevalence and severity of insomnia in chronic low back pain patients. Rheumatol Int. (2013) 33:1277. doi: 10.1007/s00296-012-2550-x
8. Weiner DK, Fang M, Gentili A, Kochersberger G, Marcum ZA, Rossi MI, et al. Deconstructing chronic low back pain in the older adult—step by step evidence and expert-based recommendations for evaluation and treatment: Part I: Hip osteoarthritis. Pain Med. (2015) 16:886–97. doi: 10.1111/pme.12757
9. Laplante BL, DePalma MJ. Spine osteoarthritis. PM&R. (2012) 4:S28–36. doi: 10.1016/j.pmrj.2012.03.005
10. Abraham I, Killackey-Jones B. Lack of evidence-based research for idiopathic low back pain: the importance of a specific diagnosis. Arch Intern Med. (2002) 162:1442–4. doi: 10.1001/archinte.162.13.1442
11. VanderWeele TJ, Vansteelandt S. Odds ratios for mediation analysis for a dichotomous outcome. Am J Epidemiol. (2010) 172:1339–48. doi: 10.1093/aje/kwq332
12. Chou R, Huffman LH. Medications for acute and chronic low back pain: a review of the evidence for an American pain society/American college of physicians clinical practice guideline. Ann Intern Med. (2007) 147:505–14. doi: 10.7326/0003-4819-147-7-200710020-00008
13. Goode AP, Nelson AE, Kraus VB, Renner JB, Jordan JM. Biomarkers reflect differences in osteoarthritis phenotypes of the lumbar spine: the Johnston county osteoarthritis project. Osteoarthr Cartil. (2017) 25:1672–9. doi: 10.1016/j.joca.2017.07.007
14. Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. (2002) 27:E109–20. doi: 10.1097/00007632-200203010-00017
15. Weiner DK, Sakamoto S, Perera S, Breuer P. Chronic low back pain in older adults: prevalence, reliability, and validity of physical examination findings. J Am Geriatr Soc. (2006) 54:11–20. doi: 10.1111/j.1532-5415.2005.00534.x
16. Schneider S, Mohnen SM, Schiltenwolf M, Rau C. Comorbidity of low back pain: representative outcomes of a national health study in the Federal Republic of Germany. Eur J Pain. (2007) 11:387–97. doi: 10.1016/j.ejpain.2006.05.005
17. Iijima H, Suzuki Y, Aoyama T, Takahashi M. Interaction between low back pain and knee pain contributes to disability level in individuals with knee osteoarthritis: a cross-sectional study. Osteoarth Cartil. (2018) 26:1319–25. doi: 10.1016/j.joca.2018.06.012
18. Stupar M, Cote P, French MR, Hawker GA. The association between low back pain and osteoarthritis of the hip and knee: a population-based cohort study. J Manipulative Physiol Ther. (2010) 33:349–54. doi: 10.1016/j.jmpt.2010.05.008
19. Goode AP, Carey TS, Jordan JM. Low back pain and lumbar spine osteoarthritis: how are they related? Curr Rheumatol Rep. (2013) 15:305. doi: 10.1007/s11926-012-0305-z
20. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane reviews. Cochrane Datab Syst Rev. (2017) 4:CD011279. doi: 10.1002/14651858.CD011279.pub2
21. Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Noninvasive Treatments for Low Back Pain. Rockville, MD: Agency for Healthcare Research and Quality (2016).
22. Warburton DE, Bredin SS. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. (2017) 32:541–56. doi: 10.1097/HCO.0000000000000437
23. Pardo GB, Girbés EL, Roussel NA, Izquierdo TG, Penick VJ, Martín DP. Pain neurophysiology education and therapeutic exercise for patients with chronic low back pain: a single-blind randomized controlled trial. Arch Phys Med Rehabil. (2018) 99:338–47. doi: 10.1016/j.apmr.2017.10.016
24. Owen PJ, Miller CT, Mundell NL, Verswijveren SJ, Tagliaferri SD, Brisby H, et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. (2020) 54:1279–87. doi: 10.1136/bjsports-2019-100886
25. Axén I, Kwak L, Hagberg J, Jensen I. Does physical activity buffer insomnia due to back and neck pain? PLoS ONE. (2017) 12:e0184288. doi: 10.1371/journal.pone.0184288
26. Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain. Psychol Bull. (2007) 133:581–624. doi: 10.1037/0033-2909.133.4.581
27. Wachholtz AB, Pearce MJ, Koenig H. Exploring the relationship between spirituality, coping, and pain. J Behav Med. (2007) 30:311–8. doi: 10.1007/s10865-007-9114-7
28. Asmundson GJ, Fetzner MG, DeBoer LB, Powers MB, Otto MW, Smits JA. Letts get physical: a contemporary review of the anxiolytic effects of exercise for anxiety and its disorders. Depress Anxiety. (2013) 30:362–73. doi: 10.1002/da.22043
29. Centers for Disease Control Prevention. Physical Activityand Health. The Benefits of Physical Activity. Available online at: http://www.cdc.gov/physicalactivity/everyone/health/ (accessed July 11, 2022).
30. Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain: what works? Pain. (2004) 107:176–90. doi: 10.1016/j.pain.2003.10.017
31. Weiner DK, Gentili A, Coffey-Vega K, Morone N, Rossi M, Perera S. Biopsychosocial profiles and functional correlates in older adults with chronic low back pain: a preliminary study. Pain Med. (2019) 20:1300–10. doi: 10.1093/pm/pny065
32. Cedraschi C, Luthy C, Allaz AF, Herrmann FR, Ludwig C. Low back pain and health-related quality of life in community-dwelling older adults. Eur Spine J. (2016) 25.9:2822–32. doi: 10.1007/s00586-016-4483-7
33. Basiński K, Zdun-Ryzewska A, Majkowicz M. Psychosocial predictors of persistent low back pain in patients presenting to the emergency department. Am J Emerg Med. (2022) 51:85–91. doi: 10.1016/j.ajem.2021.10.018
34. Nordstoga AL, Nilsen TI, Vasseljen O, Unsgaard-Tøndel M, Mork PJ. The influence of multisite pain and psychological comorbidity on prognosis of chronic low back pain: longitudinal data from the Norwegian HUNT Study. BMJ Open. (2017) 7:e015312. doi: 10.1136/bmjopen-2016-015312
35. Kasper JD, Freedman VA. Findings from the 1st round of the National Health and Aging Trends Study (NHATS): Introduction to a special issue. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, (2014) 69(Suppl_1), pp.S1–S7.
36. Montaquila J, Freedman VA, Spillman B, Kasper JD. National health and aging trends study development of round 1 survey weights. NHATS Technical Paper. (2012) 2, 1–20.
37. Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. (2005) 58:163–71. doi: 10.1016/j.jpsychores.2004.09.006
38. Fehrmann E, Kotulla S, Fischer L, Kienbacher T, Tuechler K, Mair P, et al. The impact of age and gender on the ICF-based assessment of chronic low back pain. Disabil Rehabil. (2019) 41:1190–9. doi: 10.1080/09638288.2018.1424950
39. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Eq Model Multidiscip J. (1999) 6:1–55. doi: 10.1080/10705519909540118
40. Vadalà G, Russo F, De Salvatore S, Cortina G, Albo E, Papalia R, et al. Physical activity for the treatment of chronic low back pain in elderly patients: a systematic review. J Clin Med. (2020) 9:1023. doi: 10.3390/jcm9041023
41. Cancela JM, Perez CA, Rodrigues LP, Bezerra P. The long-term benefits of a multicomponent physical activity program to body composition, muscle strength, cardiorespiratory capacity, and bone mineral density in a group of nonagenarians. Rejuvenation Res. (2020) 23:217–23. doi: 10.1089/rej.2019.2195
42. Weiner DK, Gentili A, Rossi M, Coffey-Vega K, Rodriguez KL, Hruska KL, et al. Aging back clinics—A geriatric syndrome approach to treating chronic low back pain in older adults: results of a preliminary randomized controlled trial. Pain Med. (2020) 21:274–90. doi: 10.1093/pm/pnz179
43. Gannon J, Atkinson JH, Chircop-Rollick T, D'Andrea J, Garfin S, Patel S, et al. Telehealth therapy effects of nurses and mental health professionals from 2 randomized controlled trials for chronic back pain. Clin J Pain. (2019) 35:295–303. doi: 10.1097/AJP.0000000000000678
44. Casey M, Smart KM, Segurado R, Doody C. Multidisciplinary-based rehabilitation (MBR) compared with active physical interventions for pain and disability in adults with chronic pain: a systematic review and meta-analysis. Clin J Pain. (2020) 36:874–86. doi: 10.1097/AJP.0000000000000871
45. Szanton SL, Walker RK, Roberts L, Thorpe RJ Jr., Wolff J, Agree E, et al. Older adults' favorite activities are resoundingly active: findings from the NHATS study. Geriatr Nurs. (2015) 36:131–5. doi: 10.1016/j.gerinurse.2014.12.008
46. Skolasky RL, Wegener ST, Aaron RV, Ephraim P, Brennan G, Greene T, et al. The OPTIMIZE study: protocol of a pragmatic sequential multiple assessment randomized trial of nonpharmacologic treatment for chronic, nonspecific low back pain. BMC Musculoskeletal Disord. (2020) 21:1–14. doi: 10.1186/s12891-020-03324-z
47. Bantham A, Ross SET, Sebastião E, Hall G. Overcoming barriers to physical activity in underserved populations. Prog Cardiovasc Dis. (2021) 64:64–71. doi: 10.1016/j.pcad.2020.11.002
48. Taylor JL, Roberts L, Hladek MD, Liu M, Nkimbeng M, Boyd CM, et al. Achieving self-management goals among low income older adults with functional limitations. Geriatr Nurs. (2019) 40:424–30.49. doi: 10.1016/j.gerinurse.2019.01.003
49. Reid MC, Eccleston C, Pillemer K. Management of chronic pain in older adults. BMJ. (2015) 350:h532. doi: 10.1136/bmj.h532
Keywords: low back pain, disability, physical activity, older adults, depressive symptoms
Citation: Taylor JL, Regier NG, Li Q, Liu M, Szanton SL and Skolasky RL (2022) The impact of low back pain and vigorous activity on mental and physical health outcomes in older adults with arthritis. Front. Pain Res. 3:886985. doi: 10.3389/fpain.2022.886985
Received: 01 March 2022; Accepted: 01 July 2022;
Published: 22 July 2022.
Edited by:
Ann Horgas, University of Florida, United StatesReviewed by:
Sudeshna Aloke Chatterjee, University of Florida, United StatesEmily J. Bartley, University of Florida, United States
Copyright © 2022 Taylor, Regier, Li, Liu, Szanton and Skolasky. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Janiece L. Taylor, andhbGtlOTBAamh1LmVkdQ==
 Janiece L. Taylor
Janiece L. Taylor Natalie G. Regier1,2
Natalie G. Regier1,2 Minhui Liu
Minhui Liu Richard L. Skolasky
Richard L. Skolasky