- Department of Epidemiology and Biostatistics, University of South Carolina, Columbia, SC, United States
We are what we eat
Research linking diet and health outcomes, and oral and systemic health has proliferated in the last two decades. The notion that poor oral health leads to poor diet is intuitive, and is supported by studies showing that individuals with missing or decayed teeth or oral soft tissue lesions are more likely to replace foods that are hard to chew, such as fresh fruits and vegetables, with less healthy alternatives such as processed foods [1]. Studying the effects of diet on health outcomes, including oral health, is more complicated. James Lind published a study in 1783 showing that vitamin C deficiency caused scurvy [2], but it took two more centuries for substantial progress to occur in the field of nutritional epidemiology. The recent explosion of studies relating nutrition, disease, and oral health is likely due to a combination of advances in designing and analyzing population health studies [3] including oral health measures [4], methods to measure diet [5, 6], and fast data processing. Recent studies leveraging advances in gene sequencing show that the human microbiome is much more diverse and complex than previously thought, and that its composition is correlated with the metabolic state, health, and disease [7]. Importantly, the human microbiome is affected by diet, and the oral microbiome and gut and human microbiome are connected [8–10]. These findings have opened a new window for future research.
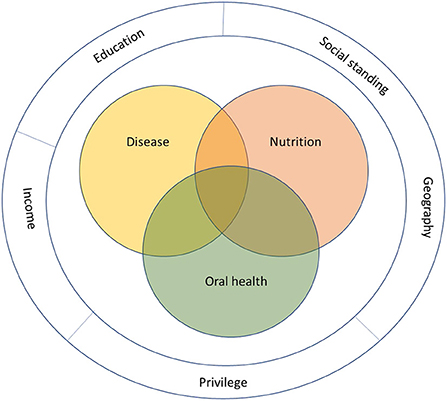
At a population level, social and economic factors such as education, social standing, privilege, geography, and income affect both health outcomes and access to food, causing disparities in disease burden [11]. Globally, undernutrition continues to affect primarily mothers and children living in poor communities, while rates of obesity, diabetes, and chronic disease are rising [12–14]. On the other hand, the growing aging population has a unique set of circumstance—including multimorbidity, frailty, mobility, cognition, and loneliness—that potentially affect health and access to food [15]. This is the context within which nutrition researchers work (Figure 1).
The goal is to answer questions at the intersection of nutrition, oral health, disease, and their determinants that would inform clinical practice and policy. A substantial body of observational and mechanistic data exist relating various aspects of the relationships between diet, disease, and oral health. Poor oral health is associated with increased mortality [16, 17], heart disease [18], cancer [19], diabetes [20, 21], Alzheimer's disease [22], adverse birth outcomes [23], and other health conditions.
Diet is associated with oral and general health and affects the human microbiome. Changes in oral health are associated with changes in the oral and gut microbiome [8, 12], and dental treatment affects the oral microbiome [24]. Based on these data organizations including the American Diabetes Association [25], and American College of Obstetrics and Gynecology acknowledge that poor oral health is related to poor health outcomes [26], but neither of these organizations recommend dental treatment as a strategy to improve general health outcomes. The reason is that the effect of dental treatment in the prevention of general health outcomes is understudied.
Randomized controlled trials (RCT) are the gold standard to evaluate causality, but such studies are difficult to conduct in this area. For example, in an RCT designed to evaluate the effectiveness of dental treatment to prevent cardiovascular disease, dental treatment would need to be withheld from individuals in the control group for the time it would take for cardiovascular disease to develop. Restricting effective treatment for any length of time but particularly for the several years it takes for the outcome to develop would be ethically unacceptable [27]. Angrist showed that it was possible to leverage natural experiments using observational data to evaluate cause and effect [28]. The method is widely used in economics to evaluate the effect of policies, and Angrist and Imbens (a co-author on the seminal paper on the topic) received the 2021 Nobel Prize in economics for this contribution. McClellan et al. demonstrated the feasibility of using this approach in the medical field by comparing different treatments of myocardial infarction in relation to mortality using observational data [29]. More recently, Rigdon et al. used this method to assess the effect of the Supplemental Nutrition Assistance Program (SNAP) on body mass index (BMI) [30]. Robins proposed alternative approaches to evaluate the effect of treatment on health outcomes using observational data [31]. Hernan et al. reproduced the results of an RCT by applying these methods to observational data [32]. The Target Trial approach is exactly this—analyzing observational data to emulate a clinical trial [33, 34]. Given the difficulties in conducting RCTs in this field, we need to rely on good observational studies combined with these promising but underused alternative approaches understand the relationships between nutrition, disease, and oral health.
Racial disparities in relation to disease prevalence, oral health and diet are well-documented, but few studies have examined possible factors contributing to racial disparities in health outcomes. Kovesdy et al. found that Black individuals did not have a higher risk of death than White individuals in a large cohort of US veterans, but had a higher mortality risk in a similar sample representative of the general US population [35]. The US veterans had similar access to care irrespective of race, but Black persons have less access to care compared to their White peers in the general US population. Race was probably a proxy for access to care, which was unmeasured in the cohort of the general US population. Duggan and colleagues recently published a comprehensive update on this issue highlighting the limitations of using race in biomedical research and provided possible alternative approaches. There is growing recognition for the need to study health disparities in relation to their underlying determinants, such as access to care, discrimination, and social class for which race often serves as a crude proxy [36].
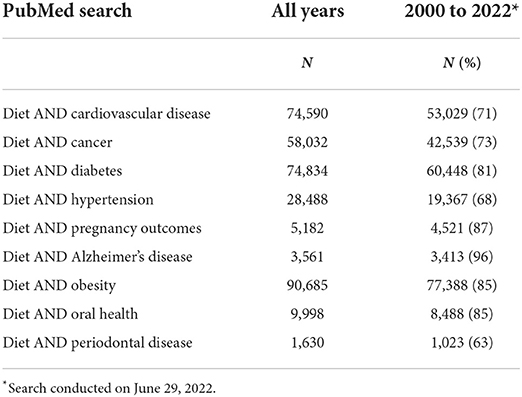
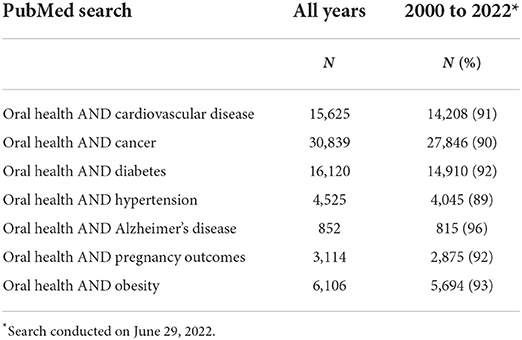
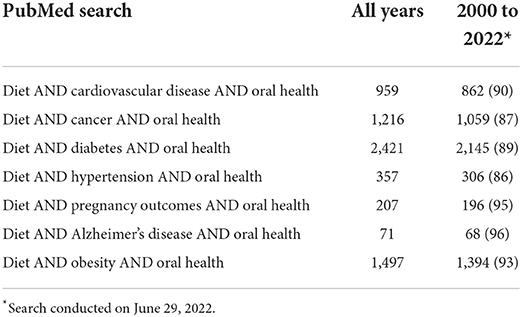
This is a particularly opportune time to study connections between nutrition, oral health, and disease because there are many unanswered questions. When we conducted a PubMed search with the terms “diet AND cardiovascular disease”, there were 74,590 results overall, of which 71% were from studies conducted from the year 2000 onwards (Table 1). A PubMed search with the terms “oral health AND cardiovascular disease” returned 15,625 results, 91% of which were after 2000 (Table 2). A PubMed search with the terms “diet AND cardiovascular disease AND oral health” returned 959 results overall, with a far larger percent (90%) after 2000 (Table 3). Studying the interrelatedness of nutrition, oral health, general health and their context is important because the results can be used in developing interventions and policies to improve oral and general health.
There are also a growing number of resources to address these questions. The complexity and cost of collecting primary data to answer these questions could have blocked this line of research, but increased availability of datasets for secondary analysis now make this possible. For example, Berkowitz et al. combined data from the 2011 National Health Interview Survey (NHIS) and Medical Expenditure Panel Survey (MEPS) to evaluate the relationship between SNAP program participation and health care costs [37]. The National Center for Health Statistics collects NHIS and MEPS data from a nationally representative sample and makes these data available for research. The National Health and Nutrition Examination Survey (NHANES) are publicly available data representative of the US population that several researchers have used [38]. Online resources such as a catalog of potential sources of datasets for secondary analyses are also available [39]. There have been substantial advances in methods to collect and analyze nutritional data, use observational data to emulate clinical trials, and evaluate mediators of causal effect.
Diet affects health including the health of teeth, gums, and tissues of the mouth, and is correlated with other lifestyle choices such as physical activity, and consumption of sugar sweetened beverages, alcohol, and betel nut chewing, which could be related to both oral and general health. The Oral Health and Nutrition section of Frontiers in Oral Health will consider studies evaluating:
• the impact of oral health and tooth loss on diet
• the impact of nutrition on health including bone, teeth and soft tissues in the mouth and on overall health
• common nutritional risk and preventive factors of oral disease and health
• taste and nutrition
• socioeconomic disparities and food insecurity in relation to oral and systemic health
• promotion of healthy diet and referral to dietitians
• lifestyle and its impact on oral and general health.
Studying these connections can help to translate research findings into clinical practice and policy to improve oral and overall health.
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ritchie CS, Joshipura K, Hung HC, Douglass CW. Nutrition as a mediator in the relation between oral and systemic disease: associations between specific measures of adult oral health and nutrition outcomes. Crit Rev Oral Biol Med. (2002) 13:291–300. doi: 10.1177/154411130201300306
2. Lind J. Nutrition classics. A treatise of the scurvy by James Lind, MDCCLIII. Nutr Rev. (1983) 41:155–7. doi: 10.1111/j.1753-4887.1983.tb07177.x
3. Advances in Epidemiology. Using 21st Century Science to Improve Risk-Related Evaluations. Washington DC: National Academies Press (2017). 71 p.
4. Dye BA, Afful J, Thornton-Evans G, Iafolla T. Overview and quality assurance for the oral health component of the National Health and Nutrition Examination Survey (NHANES), 2011-2014. BMC Oral Health. (2019) 19:95. doi: 10.1186/s12903-019-0777-6
5. Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. (1992) 135:1114–26; discussion 1127-1136. doi: 10.1093/oxfordjournals.aje.a116211
6. Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, et al. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. (2010) 29:2857–68. doi: 10.1002/sim.4063
7. Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature. (2007) 449:804–10. doi: 10.1038/nature06244
8. Maier TV, Lucio M, Lee LH, VerBerkmoes NC, Brislawn CJ, Bernhardt J, et al. Impact of dietary resistant starch on the human gut microbiome, metaproteome, and metabolome. mBio. (2017) 8. doi: 10.1128/mBio.01343-17
9. Ursell LK, Haiser HJ, Van Treuren W, Garg N, Reddivari L, Vanamala J, et al. The intestinal metabolome: an intersection between microbiota and host. Gastroenterology. (2014) 146:1470–6. doi: 10.1053/j.gastro.2014.03.001
10. Goh CE, Bohn B, Marotz C, Molinsky R, Roy S, Paster BJ, et al. Nitrite generating and depleting capacity of the oral microbiome and cardiometabolic risk: results from ORIGINS. J Am Heart Assoc. (2022) 11:e023038. doi: 10.1161/JAHA.121.023038
11. Chattopadhyay A. Oral health disparities in the United States. Dent Clin North Am. (2008) 52:297–318, vi. doi: 10.1016/j.cden.2007.11.001
12. Collaborators GBDD. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
13. Collaborators GBDRF. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
14. Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
15. Leroux J, Cox J, Rosenberg M. Food insecurity and aging: a scoping study of the literature. Can J Aging. (2020) 39:662–96. doi: 10.1017/S071498081900059X
16. Ansai T, Takata Y, Yoshida A, Soh I, Awano S, Hamasaki T, et al. Association between tooth loss and orodigestive cancer mortality in an 80-year-old community-dwelling Japanese population: a 12-year prospective study. BMC Public Health. (2013) 13:814. doi: 10.1186/1471-2458-13-814
17. Garcia RI, Krall EA, Vokonas PS. Periodontal disease and mortality from all causes in the VA dental longitudinal study. Ann Periodontol. (1998) 3:339–49. doi: 10.1902/annals.1998.3.1.339
18. Humphrey LL, Fu R, Buckley DI, Freeman M, Helfand M. Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J Gen Intern Med. (2008) 23:2079–86. doi: 10.1007/s11606-008-0787-6
19. Abnet CC, Qiao YL, Dawsey SM, Dong ZW, Taylor PR, Mark SD. Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int J Epidemiol. (2005) 34:467–74. doi: 10.1093/ije/dyh375
20. Stohr J, Barbaresko J, Neuenschwander M, Schlesinger S. Bidirectional association between periodontal disease and diabetes mellitus: a systematic review and meta-analysis of cohort studies. Sci Rep. (2021) 11:13686. doi: 10.1038/s41598-021-93062-6
21. Zheng M, Wang C, Ali A, Shih YA, Xie Q, Guo C. Prevalence of periodontitis in people clinically diagnosed with diabetes mellitus: a meta-analysis of epidemiologic studies. Acta Diabetol. (2021) 58:1307–27. doi: 10.1007/s00592-021-01738-2
22. Borsa L, Dubois M, Sacco G, Lupi L. Analysis the link between periodontal diseases and Alzheimer's disease: a systematic review. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18179312
23. Iheozor-Ejiofor Z, Middleton P, Esposito M, Glenny AM. Treating periodontal disease for preventing adverse birth outcomes in pregnant women. Cochrane Database Syst Rev. (2017) 6:CD005297. doi: 10.1002/14651858.CD005297.pub3
24. Di Stefano M, Polizzi A, Santonocito S, Romano A, Lombardi T, Isola G. Impact of oral microbiome in periodontal health and periodontitis: a critical review on prevention and treatment. Int J Mol Sci. (2022) 23. doi: 10.3390/ijms23095142
25. Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, Freeman R, et al. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes-2022. Diabetes Care. (2022) 45(Suppl. 1):S46–59. doi: 10.2337/dc22-S004
26. American College of Obstetricians and Gynecologists. Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol. (2012) 120:964–73. doi: 10.1097/AOG.0b013e3182723b1b
27. Merchant AT, Virani SS. Evaluating periodontal treatment to prevent cardiovascular disease: challenges and possible solutions. Curr Atheroscler Rep. (2017) 19:4. doi: 10.1007/s11883-017-0640-7
28. Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables - Reply. J Am Stat Assoc. (1996) 91:468–72. doi: 10.1080/01621459.1996.10476907
29. McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. JAMA. (1994) 272:859–66. doi: 10.1001/jama.1994.03520110039026
30. Rigdon J, Berkowitz SA, Seligman HK, Basu S. Re-evaluating associations between the Supplemental Nutrition Assistance Program participation and body mass index in the context of unmeasured confounders. Soc Sci Med (1982). (2017) 192:112–24. doi: 10.1016/j.socscimed.2017.09.020
31. Robins J. A new approach to causal inference in mortality studies with a sustained exposure period - application to control of the healthy worker survivor effect. Math Modelling. (1986) 7:1393–512. doi: 10.1016/0270-0255(86)90088-6
32. Hernan MA, Alonso A, Logan R, Grodstein F, Michels KB, Stampfer MJ et al. Observational studies analyzed like randomized experiments: an application to postmenopausal hormone therapy and coronary heart disease. Epidemiology. (2008) 19:766–79. doi: 10.1097/EDE.0b013e3181875e61
33. Dickerman BA, Gerlovin H, Madenci AL, Kurgansky KE, Ferolito BR, Figueroa Muñiz MJ, et al. Comparative effectiveness of BNT162b2 and mRNA-1273 vaccines in U.S. Veterans N Engl J Med. (2022) 386:105–15. doi: 10.1056/NEJMoa2115463
34. Hernan MA. Methods of public health research - strengthening causal inference from observational data. N Engl J Med. (2021) 385:1345–8. doi: 10.1056/NEJMp2113319
35. Kovesdy CP, Norris KC, Boulware LE, Lu JL, Ma JZ, Streja E, et al. Association of race with mortality and cardiovascular events in a large cohort of US veterans. Circulation. (2015) 132:1538–48. doi: 10.1161/CIRCULATIONAHA.114.015124
36. Duggan CP, Kurpad A, Stanford FC, Sunguya B, Wells JC. Race, ethnicity, and racism in the nutrition literature: an update for 2020. Am J Clin Nutr. (2020) 112:1409–14. doi: 10.1093/ajcn/nqaa341
37. Berkowitz SA, Seligman HK, Rigdon J, Meigs JB, Basu S. Supplemental Nutrition Assistance Program (SNAP) participation and health care expenditures among low-income adults. JAMA Intern Med. (2017) 177:1642–9. doi: 10.1001/jamainternmed.2017.4841
38. National Health and Nutrition Examination Survey (2022). Available online at: https://www.cdc.gov/nchs/nhanes/index.htm (accessed June 7, 2022).
39. Finding Datasets for Secondary Analysis. (2022). Available online at: https://browse.welch.jhmi.edu/datasets (accessed June 7, 2022).
Keywords: oral health, nutrition, diet, health outcomes, socioeconomic disparities, food insecurity
Citation: Merchant AT (2022) Grand challenges in oral health and nutrition: We are what we eat. Front. Oral. Health 3:999817. doi: 10.3389/froh.2022.999817
Received: 21 July 2022; Accepted: 08 August 2022;
Published: 24 August 2022.
Edited and reviewed by:
Mohammad Altamimi, An-Najah National University, PalestineCopyright © 2022 Merchant. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anwar T. Merchant, bWVyY2hhbnRAbWFpbGJveC5zYy5lZHU=
 Anwar T. Merchant
Anwar T. Merchant