- 1Division of Restorative Dentistry, Faculty of Dentistry, The University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 2Department of Special Care Dentistry, The Dental School, Universidad Católica de Córdoba, Córdoba, Argentina
- 3Special Care Dentistry, Dublin Dental Hospital, Trinity College, Dublin, Ireland
- 4Applied Oral Sciences and Biomaterials, Faculty of Dentistry, Hong Kong University, Sai Ying Pun, Hong Kong SAR, China
The aim of this systematic review was to update an existing review on the management of dental caries lesions in patients with disabilities so as to provide an up-to-date summary of the evidence. Randomized clinical trials and cohort studies related to preventive and restorative programmes for dental caries among people requiring special care, published in English, Spanish, Portuguese, French and German languages from February 1st 2011 to April 1st 2022, were retrieved from three databases (“updated review”). From the 1,105 titles identified using the search topic “Caries AND Disability”, 17 papers informed in the analyses: 6 referring to caries preventive strategies and 11 related to restorative care strategies. Most of these studies targeted children and adults with intellectual/physical disability, although preventive and therapeutic strategies were also reported for frail older adults and onchohematological patients. Fluorides in tablets, gels or varnishes forms and the use of xylitol as a sugar substitute were reported as effective approach to prevent the onset of caries in high-risk groups. Minimally intervention treatment options such as the Hall technique, the ART approach and the use of SDF for arresting caries, were deemed suitable and effective strategies for treating existing lesions in-office. In conclusion, in the past decade (2011–2022) an increased number of articles reported strategies to prevent and manage caries among people requiring special care. Although an array of preventive and therapeutic strategies for dental caries exists, more and better-quality clinical evidence is needed to offer guidance to inform policy and practice for special care dentistry.
Introduction
In 2011, a systematic review regarding strategies to prevent and/or treat caries lesions in patients with disability concluded that more studies, and specifically more high-quality research was required to provide stronger scientific evidence to inform feasible and effective approaches to safeguard and improve the oral health of people requiring special care dentistry (1). The publication was a call for action to clinicians, researchers, and international oral health associations to spearhead the promotion of oral health, based on scientific evidence, for people with disability and medically compromised patients. Although the prevalence of caries is not necessarily higher among people with disabilities compared to the general population, it has been repeatedly described that people with disabilities have a higher number of untreated lesions, thus a higher unmet caries treatment needs as well as poorer oral hygiene and poorer periodontal status conditions than people without disabilities (2, 3).
In the last decade, in dentistry, major technical advances have led to improved quality of dental treatment and improved ability to maintain oral function and aesthetics over the life span. However, there are still gross and unfair inequalities in term of the quantity and the quality of dental treatment provided to people with disabilities. Special Care Dentistry is often perceived as the discipline of compromise—where “better than nothing” is the bottom line (4).
There is evidence that most but not all dental needs could be met in primary dental care settings (5). The problem for oral health care providers and governments is how to identify and select those who are best manged in the primary dental care setting and to decipher who needs additional specialist skills and adjuncts to receive and tolerate dental care. Furthermore, there is a need to ensure that such dental care is optimized and personalized to the patient's specific dental needs, considering that the scope of disability extends to a wide range of medical conditions that may compromise a “one-fits-all” approach of guidelines. Notwithstanding these considerations, references of best practices -targeting groups with similar characteristics- may help clinicians to offer their people with disabilities a variety of strategies that may suit them best to safeguard and improve their oral health.
The aim of this review was to update an existing review (1) on the management of dental caries lesions in patients with disabilities so as to provide an up-to-date summary of the evidence.
Materials and methods
PICO principle (Population, Intervention, Comparator, Outcome) was used to define the research question: What is the suitability and effectiveness of available strategies for preventing and/or treating caries lesions in people with disability?
Three electronic databases, the Cochrane Library database for Clinical Trials, PubMed and LILACS (Latin American and Caribbean Health Science Literature) were searched, and all publications listed in the databases from February 1st 2011 to April 1st 2022 were included. Different combinations of MeSH terms, limits and Boolean operators were tested to identify those that could include the highest number of relevant publications. The search strategy repeated the one that had been used in 2011 with a change in the dates for the search instead. Details of the search strategy for each database are described in Appendix 3.
Reference-linkage of review articles were used to identify additional relevant publications. In addition, hand searches of key publications were undertaken to identify other studies that had not been retrieved from the electronic databases search.
The inclusion criteria were with respect to three aspects:
1) Types of studies. Randomized controlled (clinical) trials and cohort studies on preventive and restorative intervention programmes published in English, Portuguese, Spanish, French and German languages were included. If only a relevant title without a listed abstract was available, a full copy of the article was obtained and assessed.
2) Type of participants. People of any age and gender, presenting any medical condition related to disability. The intention was to include publications having a control group, either with or without disability. Definition of a person with disability was adopted from the WHO-ICF (International Classification of Functioning, Disability and Health) (6) referring to people who experience the negative aspects of the interaction between their environmental and personal context and any functional impairments, activity limitations and participation restrictions that they may present (6).
3) Type of interventions. Preventive and/or restorative intervention programmes for managing dental caries including but not limited to the use of chemical products to control cariogenic bacteria, remineralizing agents, restorative and non-restorative options for caries treatment. Case reports, narrative reviews and epidemiological studies were excluded for their analysis.
Titles and abstracts were initially retrieved in duplicate by 2 reviewers (GFM and MZ) to identify potentially included studies, discussing eligibility until agreement was achieved by consensus. Data regarding authorship, study design, type of intervention and outcomes of the interventions were extracted from the articles independently and in duplicate and recorded into an excel spreadsheet.
Studies were assessed by two reviewers (GFM, MZ) and double-checked by the other two review authors (AD, CM). Disagreements among the reviewers were resolved through discussion until agreement was reached. Two reviewers (MZ, GFM) independently assessed the risk of bias of included RCTs using the Cochrane Collaboration's tool (7) and disagreements were resolved by consensus. Each study was judged and categorized as being of low, moderate, high or unclear risk of bias. Unclear risk of bias was assigned to indicate lack of information or uncertainty about the potential for bias.
GRADE criteria (Grading of Recommendations Assessment, Development, and Evaluation—GRADE approach) (8) was used to rate the certainty of the evidence, based on the assessment of the study design, risk of bias, imprecision, inconsistency, indirectness, and magnitude of effect of the articles.
Finally, included articles were categorized regarding the hierarchy of the level of evidence (9) (Appendix 2), a tool that had been used in the systematic review that is being updated in this article, to analyze whether the findings of this review have improved the quality of the publications compared to those articles retrieved in the previous review (1).
To report the outcomes of this systematic review the guidance from the PRISMA Checklist (10) (Appendix 1) was followed.
Analyses of data
Data were grouped in tables with a synoptic description of type of study, type of intervention and main outcomes to assess the relative effectiveness of each intervention. If studies reported dissimilar follow-up times or lacked a common comparator or if pairwise meta-analysis was not possible or failed to obtain measures of association, these data were reported as described by the primary study authors.
Quantitative analysis had been proposed by using Review Manager 5.3 software to compare studies using the same interventions and assessing the same outcomes by the same measurements. Meta-analysis were considered unfeasible for most of the outcomes due to the heterogeneity of the type of studies, participants and interventions, with a low number of strategies suitable for comparisons. A graphic showing the level of bias associated with each domain was obtained using this Cochrane software (Appendix 4).
Fixed effect model was applied if the total number of studies included in meta analysis was less than six studies (11). Due to lack of correlation in change from available studies, anticipated correlation of 0.5 was used to estimate the standard deviation of change (12). Continuity correction of 0.5 was applied if standard error cannot be computed due to estimated proportion is at 0 or 1 (13).
Finally, one-way ANOVA was used to analyze 5-year survival percentages among different restorative treatments.
Results
A flow diagram of the systematic search is presented in Appendix 5. After reaching an agreement on potential suitable titles/abstracts, 52 full articles regarding preventive and/or therapeutical caries management strategies were retrieved for analysis of which 35 were finally excluded. Reasons for exclusion were: (1) articles describing epidemiological studies (n = 8); (2) narrative articles (n = 10); (3) case reports (n = 7); (4) articles not related to the topic of this review (n = 8) and (5) systematic reviews (n = 2).
A total of 17 publications were suitable for final analyses: 6 related to caries-preventive programmes and 11 to restorative treatment programmes.
Caries-preventive strategies
Table 1 provides a summary of key information obtained from the included studies on caries preventive and therapeutic strategies. The level of the evidence of the included studies was rated between grades II and III-2, having included four RCTs (14–17), one cluster RCT (18) and one longitudinal field trial (19). The sample size of these six studies presented a significant variation among them with an impact on to the quality of the evidence. A total number of 532 participants was followed up in 6 clinical trials, in most cases recruiting primarily children and adolescents with intellectual disability (ID), with the exception of one study that was conducted in a population with visual/hearing impairment.
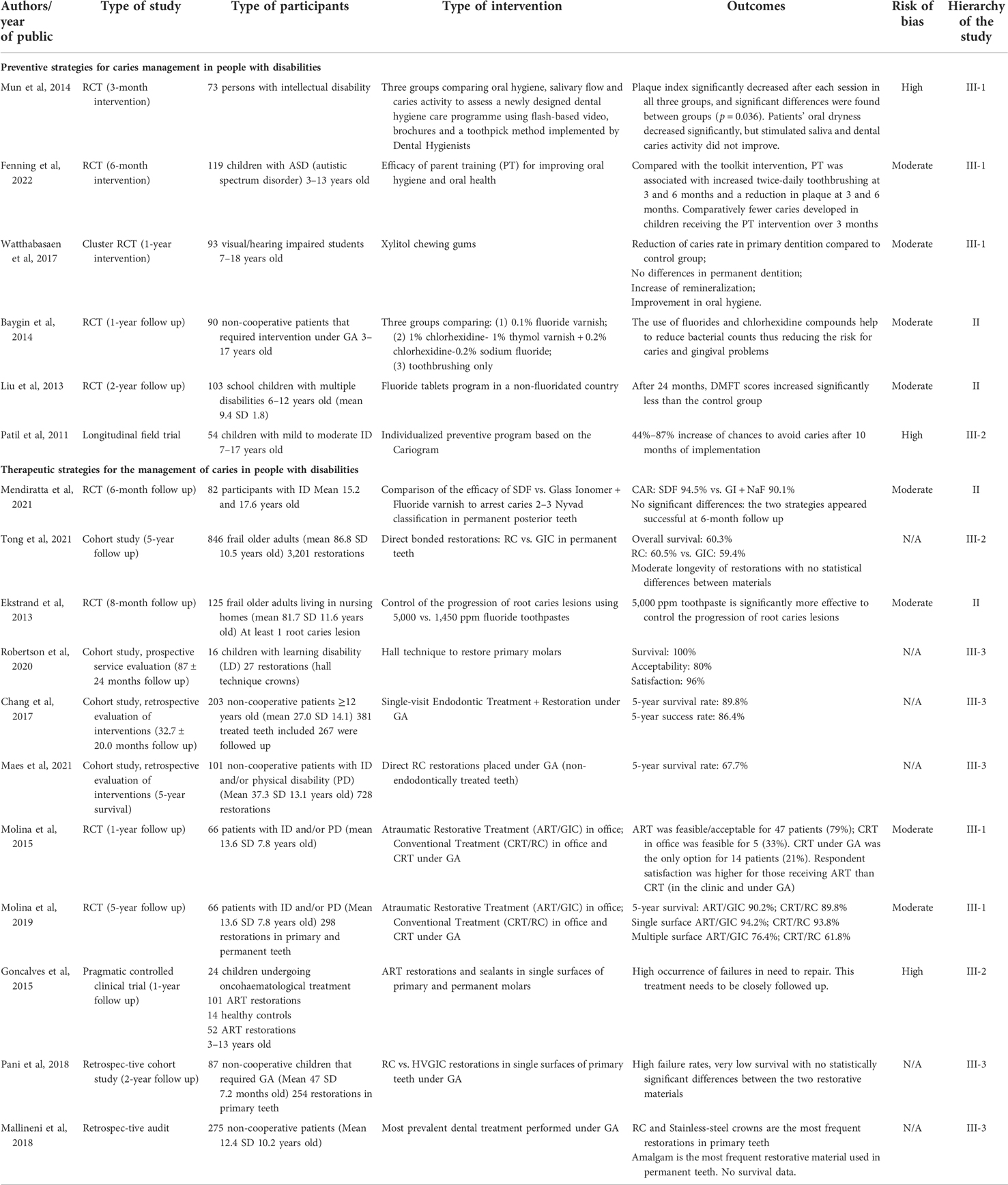
Table 1. A summary of key information obtained from the included studies regarding preventive and therapeutic strategies for caries management in people with disabilities.
There was a significant heterogeneity in the type of interventions and conclusive results were of low certainty in most of studies.
Three studies introduced strategies that focused on how to effectively produce changes in attitudes and behavior towards oral health care, implemented in people with intellectual disability and autistic disorder spectrum. The study by Mun et al. (14) assessed the effectiveness of a dental hygiene care programme implemented by Dental Hygienists in a population with intellectual disability whereas the study by Fenning et al. (15) emphasized the importance of training the parents to improve oral hygiene standards in children with autistic spectrum disorders. Oral health variables such as plaque index or caries activity measured the impact of these strategies, reporting promising results for targeting special groups with individualized and creative methods (14, 15).
The third of these types of studies, followed the line of assessing caries risk to target individualized strategies to prevent the onset of the disease. The Cariogram assessment model (20) was adopted to follow up customized preventive programs in a population of 54 children with ID, adjusting different risk factors according to each child's situation to avoid the development of new lesions (19). Despite promising results of this aiding tool, details of specific strategies to modify the individuals’ caries risk were not provided in this study.
Two studies referenced the effectiveness of chemical agents for controlling cariogenic biofilm, confirming the evidence that fluorides in different concentrations and presentations (tablets, gels, varnishes and pastes) may be useful resources for preventing caries lesions (16, 17). Although chlorhexidine has been mentioned in one of these studies (17), the evidence of its effectiveness has of low quality and uncertain.
The use of xylitol chewing gums in a visual/hearing impaired school population was a successful strategy to relent DMFT scores after 1 year (18). More studies are needed to confirm of reject these findings in order to promote a generalized use of these sugar substitutes to prevent the onset of caries in people with disability.
Restorative/non-restorative treatment strategies
Table 1 provides a summary of key information obtained from the included studies on restorative treatment programmes. The quality of the included studies rated between level II and lV. Three RCT (one of them has two entrances for different types of outcomes) (21–24), one pragmatic controlled clinical trial (25), one prospective cohort study (26), one retrospective audit (27), and four retrospective cohort studies (28–31) reported the outcomes of different interventions that aimed to restore teeth affected by caries disease in patients with disability in time interval 2011–2022.
The use of minimally invasive strategies had a double purpose in this population: (1) maximal preservation of tooth structures and (2) to avoid interventions under GA as much as possible.
Following a gradient of complexity of the interventions, two studies reported that fluorides in high concentrations have shown to be effective products to arrest root caries lesions (22) as well as to prevent the progression of occlusal lesions in permanent molars, either using SDF or a combination of fluoride varnish sealed with a glass ionomer restorative cement (21). Although the two studies evaluated the ability to arrest the progression of caries lesions, they used different criteria to report caries arrestment rates, allowing no comparison between the outcomes obtained for each study.
The ART approach, employing high-viscosity glass ionomer cement as a restorative material, was tested in two of the included studies, seeking for alternatives to conventional restorative treatment that comprises the use of rotary instruments for caries removal. One of these clinical trials reported 76% acceptance and 100% satisfaction with this treatment modality in one article (23) and overall survival of 90.2% after 5 years in a separate paper (24). The other article on ART targeted a population of children undergoing oncohaematologic treatment and, although it was stated that this approach is suitable for this group of patients, a high number of restorations in need for repair was detected in a short period (1-year follow up) suggesting that these restorations needed a close and frequent follow up (25).
The decision of using either resin composite (RC) or glass ionomer (GI) as the restorative material of choice was also analyzed in a cohort study that evaluated survival of direct bonded restorations in frail older adults (30). Results showed no statistically significant differences between these two materials and overall survival rates of 60.5% after 5 years (30).
To overcome low survival rates of large restorations, another minimally invasive resource in this review was the Hall technique to arrest caries lesions in primary teeth of 16 children with learning disability. This prospective cohort study reported 100% survival, 80% acceptance and 96% satisfaction respectively (26).
A retrospective audit of interventions undertaken aided by GA revealed that resin composite restorations and stainless-steel crowns are the most frequently used resources to restore teeth affected by caries in the primary dentition whereas dental amalgam is the preferred restorative material chosen for the permanent dentition (27).
As regards to restorative treatment carried out under GA, high failure rates were observed in single surface restorations performed in primary molars under GA in one study (29). Another retrospective study carried out in the permanent dentition of patients with intellectual and/or physical disability reported 67.7% survival after 5 years of follow up (31). These results were obtained in non-endodontically treated teeth, whereas 89.8% survival and 86.4% success were reported for single-visit endodontic treatment and restoration in permanent teeth that received treatment under GA (28).
Finally, irrespective of the heterogeneity of the reports, a comparison of outcomes regarding survival of different types of restoration at different follow-up periods, determined that the Hall technique was 100% effective at an average of a 2-year period. No significant difference after 5 years was observed for ART/HVGIC, resin composite (RC) and root canal treatment followed by single-visit RC restoration in permanent teeth (90.2%, 89.8% and 89.8% respectively; p ≥ 0.05). Results obtained after 5 years were significantly different for resin composite restorations in two studies, being 89.8% (21) and 67.7% (28) respectively, the latter placed under GA exclusively.
With respect to multiple-surface restorations, similar results were obtained in two studies (24, 30) for glass ionomer cement (GIC) and RC after 5 years, ranging from 59.4% to 76.4% (p = 0.06). Standard deviations of these percentages explain there were no statistical differences among these outcomes.
The lowest percentages of survival were observed for restorations in primary teeth, either using GIC or RC.
Certainty of the evidence
The analyzes of the certainty of the evidence using GRADE criteria for outcomes across studies is summarized in Table 2. Five different outcomes were identified for the prevention of caries and two outcomes for therapeutic strategies in the studies that had been included. The number of studies per outcome and the heterogeneity of these studies allowed few statistical analyses, leading to weak recommendations based on the power of this evidence.

Table 2. Analysis of the certainty of the evidence by outcomes across studies based on GRADE criteria.
Discussion
Diversity is a distinctive feature that relates to the population of people with disability. The broad spectrum of medical conditions that are included within the scope of disability (32) creates a context of heterogeneity that makes it difficult to provide clear recommendations that might be suitable for the whole spectrum. However, if we addressed that the etiology of caries disease is universal, meaning that it may affect any person that ticks the necessary boxes of risks factors, we may assume that preventing caries would be a matter of avoiding such risks irrespective of any medical condition. The type of disability itself may comprise specific risks that must be disclosed and taken into consideration when planning a preventive programme (33). That seems to have been acknowledged in some of the studies retrieved for this review.
Recent systematic reviews that analyzed strategies for oral care in people with disabilities show that the introduction of different strategies to reduce the risk for the development of caries disease had been reported in clinical studies comparing their efficacy, such as the use of special/modified manual vs. electric or powered toothbrushes, oral hygiene training of carers and of people with disability and the frequency of supervised toothbrushing, as well as the impact of regularly scheduled visits plus supervised toothbrushing and the discussion of photographs as motivators for oral care (34, 35). Beyond the use of universal strategies that have proved to be effective for the general public, like the use of mechanical and chemical resources to control the cariogenic biofilm, insights of contextual (training of carers) and personal (training of patients, discussion of photographs as motivators) factors have been brought to the table to tackle the problem in daily actions that may successfully and sustainably prevent the onset of caries in this at-risk population.
Although the number of publications regarding preventive strategies for managing caries in people with disability included in the present review is somewhat low, noticeable is the trend of interdisciplinary approach in comparison to the updated review. The evaluation of these resources is highlighted as a new perspective for the prevention of the disease as such, irrespective of the use of specific products, focusing on a more up to date concept of caries and the factors that trigger the onset of the disease instead of the mere avoidance of cavities. In this regard, there seems to be a shift from -for instance- “using fluorides” to “how we introduce an effective and sustainable use of fluorides according to the characteristics of each group of patients within the spectrum”. Far from being a semantic discussion, authors believe this is a key innovative approach for an old situation of unmet needs. Therefore, interdisciplinary studies involving social sciences may provide the frame for supporting strategies that may effectively reach these patients.
Unfortunately, when the disease has been activated in the oral environment, efforts must be taken to reverse the situation while treating the lesions that develop in such a condition. For that purpose, cooperation of the patient to undertake either restorative or non-restorative interventions is essential to achieve sustainable outcomes. Probably due to the barriers to provide restorative care to this population, most of the participants included in the studies on therapeutic strategies were some types of “non-cooperative” patients, including intellectual and/or physically to medically compromised patients, ranging in age from children to frail older adults. This means that a broad scope of situations was covered by the umbrella of the designs of these studies. However, the type of intervention evaluated in each study was mainly focused on the most prevalent dental treatment needs for each stage of their lifespan and therefore, generalized strategies for all stages were difficult to retrieve due to this heterogeneity.
The tooth restorative cycle speed seems to be increase exponentially in high-risk patients and, at the same time, risk factors may be too difficult to approach in certain medical conditions or in people with behavior problems. Non or minimally invasive techniques may help to introduce more patient-friendly techniques without compromising the quality of the interventions as it has been shown in clinical studies using SDF or the ART approach (36, 37). However, longevity of the restorations, regardless of using resin composite or glass ionomer, may not achieve minimum standards and therefore, need to seek for better alternatives. Interestingly, failures occur equally for restorations either performed in-office or under sedation or GA, meaning that a different type of restoration which may withstand worse challenges in the oral cavity must be sought. The use of indirect restorations may be one option, including CAD-CAM resources, should be explored as a part of the arsenal of strategies that might be offered to people with disability if quality treatment becomes an irrefutable aim.
Although a higher number of suitable articles have been included for analysis in comparison to the previous review, the present study presents almost the same limitations, as there is still a lack of well-designed randomized clinical trials regarding both preventive and restorative approaches appropriate for use in patients with disabilities. RCTs are the most appropriate type of studies for the evaluation of clinical treatments and the introduction of new or modified dental materials prior to marketing (38). The control of bias and the equal distribution of known confounding factors between groups are among many advantages that this kind of study provides. However, some of its obvious disadvantages are related to the fact that it might take a long time to obtain outcomes and possibly a long time to enroll patients (9). Moreover, obtaining approval in Ethics Committees may discourage researchers for these endeavors or extend the times for developing the proposals extensively, leading to incomplete or low-quality protocols usually abandoned halfway.
In Disability and Oral Health, reports of clinical interventions are commonly restricted to isolated cases or case series that represent a lower level of evidence for their inclusion in a systematic review. This is a limiting aspect that has a significant impact on the construction of evidence-based guidelines for best practices in Special Care Dentistry. This issue has been discussed in the search of evidence for the use of dental implants among people with disabilities, but such controversies may also apply to Operative Dentistry as is the case of this review (39). Once again, these facts call for action. International organizations such as the International Association for Disability and Oral Health (IADH), the Special Care in Dentistry (SCD), the IADR, FDI and WHO, should give greater priority to the oral health of people with disabilities and measure core outcomes that are meaningful to them. Research methodology should be included or made mandatory in specialization courses for special needs dentists. Importantly, guidance should be provided regarding the development of an international agenda of relevant research topics and inclusive exclusion criteria should be scrutinized within ethics applications of ALL research studies to ensure that people with disabilities are only excluded with good reason in research studies which should reflect the diversity of the community (40). Furthermore, in view of the significant numbers of people with disabilities worldwide -over 1 billion people live with some form of disability; the number of people with disability are dramatically increasing due to demographic trends and increases in chronic health conditions, among other causes- (41), epidemiological data should always include those with disabilities and other hard to reach groups within their data collection. It is with great pleasure to notice that guidelines for carrying out research and for treating people with disability have been placed on the agenda of the forthcoming congresses of the IADH and SCD.
Conclusion
In the past decade (2011–2022) new evidence regarding the suitability and effectiveness of preventive and therapeutic strategies for managing caries lesions in people with disabilities has been published. There seems to be a shift in the focus of preventive strategies by introducing resources to effectively target special groups depending on their characteristics. For the restorative approach, minimally invasive strategies such as the use of SDF, ART and the Hall technique have demonstrated to be suitable and effective for the treatment of caries lesions both in primary and permanent teeth in office, thus reducing the need for interventions under general anesthesia. This review offers guidance to inform policy and practice for special care dentistry.
Author contributions
GM and CM contributed to the conception and design of the study; GM, CM, AD and MZ retrieved and selected the articles and analyzed the data. GM and MZ drafted the manuscript. All authors participated in the discussion of the manuscript until its last version and final approval was agreed to be accountable for all aspects of the work. All authors contributed to the article and approved the submitted version.
Funding
The processing charges of this journal will be covered using funds form the following grant: PRESTAMO BID-PROYECTO PICT 2020 SERIE A 00539 - FONCYT - AGENCIA NACIONAL DE PROMOCIÓN DE LA INVESTIGACIÓN, EL DESARROLLO TECNOLÓGICO Y LA INNOVACIÓN (ARGENTINA).
Acknowledgments
Authors are grateful to C.H. Chu and Duangporn Duganthip for encouraging the realization of this systematic review and to the International Association of Disability and Oral Health for its support and to Alejandra Bono, for their specialized advice regarding the methodology of systematic reviews.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/froh.2022.980048/full#supplementary-material.
References
1. Molina GF, Leal S, Frencken JE. Strategies for managing carious lesions in patients with disabilities: a systematic review. J Disabil Oral Health. (2011) 12(4):159–67.
2. Anders PL, Davis EL. Oral health of patients with intellectual disabilities: a systematic review. Spec Care Dentist. (2010) 30(3):110–7. doi: 10.1111/j.1754-4505.2010.00136.x
3. Petrovic BB, Peric TO, Markovic DLJ, Bajkin BB, Petrovic D, Blagojevic DB, et al. Unmet oral health needs among persons with intellectual disability. Res Dev Disabil. (2016) 59:370–7. doi: 10.1016/j.ridd.2016.09.020
4. da Rosa SV, Moysés SJ, Theis LC, Soares RC, Moysés ST, Werneck RI, et al. Barriers in access to dental services hindering the treatment of people with disabilities: a systematic review. Int J Dent. (2020) 2020:9074618. doi: 10.1155/2020/9074618
5. Duane BG, Freeman R, Richards D, Crosbie S, Patel P, White S, et al. Using the simplified case mix tool (sCMT) to identify cost in special care dental services to support commissioning. Community Dent Health. (2017) 34(1):56–9. doi: 10.1922/CDH_4012Duane04
6. Faulks D, Hennequin M. Defining the population requiring special care dentistry using the international classification of functioning, disability and health: a personal view. J Disabil Oral Health. (2006) 7:143–52.
7. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. Cochrane bias methods group; cochrane statistical methods group. The cochrane collaboration's tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343:d5928. doi: 10.1136/bmj.d5928
8. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. (2011) 64(4):383–94. doi: 10.1016/j.jclinepi.2010.04.026
9. Jacob RF, Carr AB. Hierarchy of research design used to categorize the “strength of evidence” in answering clinical dental questions. J Prosthet Dent. (2000) 83(2):137–52. doi: 10.1053/pr.2000.v83.apr832137
10. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
11. Tufanaru C, Munn Z, Stephenson M, Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Based Healthc. (2015) 13(3):196–207. doi: 10.1097/XEB.0000000000000065
12. Higgins JP. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (2011). The Cochrane Collaboration. Available at: https://handbook-5-1.cochrane.org/chapter_16/16_1_3_2_imputing_standard_deviations_for_changes_from_baseline.htm (Accessed March 2011).
13. Higgins JP. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (2011). The Cochrane Collaboration Available at: https://handbook-5-1.cochrane.org/chapter_16/16_9_2_studies_with_zero_cell_counts.htm (Accessed March 2011).
14. Mun SJ, Chung WG, Min SH, Park JK, Kim CB, Kim NH, et al. Reduction in dental plaque in patients with mental disorders through the dental hygiene care programme. Int J Dent Hyg. (2014) 12(2):133–40. doi: 10.1111/idh.12053
15. Fenning RM, Butter EM, Macklin EA, Norris M, Hammersmith KJ, McKinnon-Bermingham K, et al. Parent training for dental care in underserved children with autism: a randomized controlled trial. Pediatrics. (2022) 149(5):e2021050691. doi: 10.1542/peds.2021-050691
16. Liu HY, Hung HC, Hsiao SY, Chen HS, Yen YY, Huang ST, et al. Impact of 24-month fluoride tablet program on children with disabilities in a non-fluoridated country. Res Dev Disabil. (2013) 34(9):2598–605. doi: 10.1016/j.ridd.2013.05.006
17. Baygin O, Tuzuner T, Kusgoz A, Senel AC, Tanriver M, Arslan I. Antibacterial effects of fluoride varnish compared with chlorhexidine plus fluoride in disabled children. Oral Health Prev Dent. (2014) 12(4):373–82. doi: 10.3290/j.ohpd.a32129
18. Watthanasaen S, Merchant AT, Luengpailin S, Chansamak N, Pisek A, Pitiphat W. Xylitol-containing chewing gum for caries prevention in students with disabilities: a randomised trial. Oral Health Prev Dent. (2017) 15(6):519–27. doi: 10.3290/j.ohpd.a39668
19. Patil YB, Hegde-Shetiya S, Kakodkar PV, Shirahatti R. Evaluation of a preventive program based on caries risk among mentally challenged children using the cariogram model. Community Dent Health. (2011) 28(4):286–91.22320067
20. Bratthall D, Hänsel Petersson G. Cariogram–a multifactorial risk assessment model for a multifactorial disease. Community Dent Oral Epidemiol. (2005) 33(4):256–64. doi: 10.1111/j.1600-0528.2005.00233.x
21. Mendiratta M, BC M, Kumar A, Yadav V, Shyam R, Wig M. Effectiveness of silver diamine fluoride and glass ionomer cement combined with fluoride varnish in arresting dental caries among intellectually disabled individuals: a randomized controlled trial. Spec Care Dentist. (2021) 41(5):544–52. doi: 10.1111/scd.12607
22. Ekstrand KR, Poulsen JE, Hede B, Twetman S, Qvist V, Ellwood RP. A randomized clinical trial of the anti-caries efficacy of 5,000 compared to 1,450 ppm fluoridated toothpaste on root caries lesions in elderly disabled nursing home residents. Caries Res. (2013) 47(5):391–8. doi: 10.1159/000348581
23. Molina GF, Faulks D, Frencken J. Acceptability, feasibility and perceived satisfaction of the use of the atraumatic restorative treatment approach for people with disability. Braz Oral Res. (2015) 29:S1806–83242015000100292. doi: 10.1590/1807-3107BOR-2015.vol29.0097
24. Molina GF, Faulks D, Mulder J, Frencken JE. High-viscosity glass-ionomer vs. composite resin restorations in persons with disability: five-year follow-up of clinical trial. Clinical Trial Braz Oral Res. (2019) 33:e099. doi: 10.1590/1807-3107bor-2019.vol33.0099
25. Gonçalves CF, Silva MV E, Costa LR, de Toledo OA. One-year follow-up of atraumatic restorative treatment (ART) for dental caries in children undergoing oncohematological treatment: a pragmatic trial. BMC Oral Health. (2015) 15(1):127. doi: 10.1186/s12903-015-0110-y
26. Robertson MD, Harris JC, Radford JR, Innes NPT. Clinical and patient-reported outcomes in children with learning disabilities treated using the hall technique: a cohort study. Br Dent J. (2020) 228(2):93–7. doi: 10.1038/s41415-019-1166-x
27. Mallineni SK, Yiu CKY. A retrospective audit of dental treatment provided to special needs patients under general anesthesia during a ten-year period. J Clin Pediatr Dent. (2018) 42(2):155–60. doi: 10.17796/1053-4628-42.2.13
28. Chang J, Kim HY. Prognostic factors of single-visit endodontic and restorative treatment under general anaesthesia for special needs patients. J Oral Rehabil. (2017) 44(2):96–104. doi: 10.1111/joor.12458
29. Pani SC. Comparison of high viscosity glass ionomer cement to composite restorations placed in primary teeth under general anesthesia. Pediatr Dent J. (2018) 28:154–9. doi: 10.1016/j.pdj.2018.08.001
30. Tong N, Wyatt CCL. Five-year survival rate of bonded dental restorations in frail older adults. JDR Clin Trans Res. (2021) 6(1):77–86. doi: 10.1177/2380084420905785
31. Maes MS, Kanzow P, Hrasky V, Wiegand A. Survival of direct composite restorations placed under general anesthesia in adult patients with intellectual and/or physical disabilities. Clin Oral Investig. (2021) 25(7):4563–9. doi: 10.1007/s00784-020-03770-y
32. Dougall A, Martinez Pereira F, Molina G, Eschevins C, Daly B, Faulks D. Identifying common factors of functioning, participation and environment amongst adults requiring specialist oral health care using the international classification of functioning, disability and health. PLoS One. (2018) 13(7):e0199781. doi: 10.1371/journal.pone.0199781
33. Dougall A, Molina GF, Eschevins C, Faulks D. A global oral health survey of professional opinion using the international classification of functioning, disability and health. J Dent. (2015) 43(6):683–94. doi: 10.1016/j.jdent.2015.04.001
34. Waldron C, Nunn J, Mac Giolla Phadraig C, Comiskey C, Guerin S, van Harten MT, et al. Oral hygiene interventions for people with intellectual disabilities. Cochrane Database Syst Rev. (2019) 5(5):CD012628. doi: 10.1002/14651858.CD012628.pub2
35. Zhou N, Wong HM, Wen YF, McGrath C. Efficacy of caries and gingivitis prevention strategies among children and adolescents with intellectual disabilities: a systematic review and meta-analysis. J Intellect Disabil Res. (2019) 63(6):507–18. doi: 10.1111/jir.12576
36. Seifo N, Cassie H, Radford JR, Innes NPT. Silver diamine fluoride for managing carious lesions: an umbrella review. BMC Oral Health. (2019) 19(1):145. doi: 10.1186/s12903-019-0830-5
37. Frencken JE, Leal SC, Navarro MF. Twenty-five-year atraumatic restorative treatment (ART) approach: a comprehensive overview. Clin Oral Investig. (2012) 16(5):1337–46. doi: 10.1007/s00784-012-0783-4
38. Mjör IA. Controlled clinical trials and practice-based research in dentistry. J Dent Res. (2008) 87(7):605. doi: 10.1177/154405910808700702
39. Bergendal B. Evidence and clinical improvement: current experiences with dental implants in individuals with rare disorders. Int J Prosthodont. (2006) 19(2):132–4.16602359
40. Alwadi MA, Baker SR, Owens J. The inclusion of children with disabilities in oral health research: a systematic review. Community Dent Oral Epidemiol. (2018) 46(3):238–44. doi: 10.1111/cdoe.12374
41. Disability and health. Available at: https://www.who.int/news-room/fact-sheets/detail/disability-and-health#:∼:text=Over%201%20billion%20people%20are,often%20requiring%20health%20care%20services (Accessed June 12, 2022).
Keywords: disabled persons, dental care for disabled, systematic review, caries prevention, restorative care
Citation: Molina G, Zar M, Dougall A and McGrath C (2022) Management of dental caries lesions in patients with disabilities: Update of a systematic review. Front. Oral. Health 3:980048. doi: 10.3389/froh.2022.980048
Received: 28 June 2022; Accepted: 7 October 2022;
Published: 28 October 2022.
Edited by:
Yasmi O. Crystal, New York University, United StatesReviewed by:
Lucy OMalley, The University of Manchester, United Kingdom© 2022 Molina, Zar, Dougall and McGrath. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gustavo Molina bW9saW5hZ2ZAaGt1Lmhr
Specialty Section: This article was submitted to Preventive Dentistry, a section of the journal Frontiers in Oral Health
 Gustavo Molina
Gustavo Molina Mariana Zar2
Mariana Zar2 Colman McGrath
Colman McGrath