- 1ACE Dental Clinic, Bellmead, TX, United States
- 2Family Health Centers of Southwest Florida, Port Charlotte, FL, United States
- 3St. Christopher's Hospital for Children, Philadelphia, PA, United States
- 4Mount Vernon Modern Dentistry, Alexandria, VA, United States
- 5Philadelphia V.A. Medical Center, Wynnewood, PA, United States
- 6A1 Dental Clinic, Philadelphia, PA, United States
- 7Section of Public and Population Health, University of California at Los Angeles School of Dentistry, Los Angeles, CA, United States
Introduction: Advocacy involves promoting a noble cause or voicing on behalf of a program, policy, or population group. Previous literature shows that dentists who provide services to Medicaid-enrolled, underserved, and vulnerable children are more compassionate than those who do not.
Aim: To explore the association between pediatric dentists' (PDs) participation in various advocacy-related activities (ARAs) and their monthly acceptance of new Medicaid-enrolled children in their clinical practice to provide dental care services.
Methods: A 14-item pilot-tested survey was created on the SurveyMonkey® online platform and emailed to 5591 PDs, active American Academy of Pediatric Dentistry members. Data from 789 PD respondents were analyzed. Frequencies, percentages, means, and standard deviations were used to describe the sample. Independent t-tests and chi-square tests assessed the differences between PDs accepting new Medicaid-enrolled children in their clinical practice every month vs. PDs who did not. A multivariable adjusted logistic regression model determined if there was an association between PDs' participation in ARAs and their acceptance of new Medicaid-enrolled children in their clinical practice, controlling for other independent variables.
Results: The mean number of different ARAs performed by PDs was 2.2 ± 1.8. Approximately 65% reported that they accepted new Medicaid-enrolled children every month in their dental clinic to provide dental care services. The multivariable logistic regression model showed that the odds of a PD accepting new Medicaid-enrolled children every month increased by 13% for each additional unit increase in ARA completed, with other variables being held constant (Odds ratio: 1.13, 95% CI: 1.03–1.25, p = 0.01).
Conclusion: PDs who performed more ARAs had greater odds of accepting new Medicaid-enrolled children into their dental practice every month. Education and training in oral health advocacy during dental education for dental students may promote performing ARAs and providing dental care services to Medicaid patients after graduation.
Introduction
Medicaid is one of the most extensive health insurance programs in the U.S., funded by federal and state governments to provide free or low-cost healthcare coverage for those with limited incomes, pregnant women, and people with disabilities [1, 2]. In January 2021, ~73.8 million individuals were enrolled in the Medicaid program [3]. However, participation rates of general dentists in the Medicaid or the Children Health Insurance Program (CHIP) have always been low, with only 43% participating in these programs [4]. The low dentist acceptance rate of Medicaid patients is a significant problem, leading to access to dental care issues [5]. Some of the difficulties that Medicaid patients report in accessing dental health care services include difficulty finding dentists who accept Medicaid patients, excessive wait times, rude behavior by dental staff and dentists, and discrimination by dentists because they are enrolled in Medicaid [5]. On the other hand, some studies examining barriers to dentists accepting Medicaid patients found that the most common obstacles are complicated paperwork, frequent regulations changes, slow reimbursement, and fingerprint requirements [5–7]. Low reimbursement rates and Medicaid patients missing their dental appointments have also been cited as barriers for dentists to participate in Medicaid [8, 9].
Despite Medicaid's administrative drawbacks, many dentists still participate in this program and provide dental care services to those in need. A few earlier studies described the characteristics of dentists who accept and do not accept Medicaid patients. Studies show that non-Caucasian and ethnic minority dentists served more Medicaid patients than other groups [10, 11]. Dentists in group practices accepted more Medicaid patients than solo practitioners [10], while pediatric dentists provided more care to Medicaid patients than general dentists [12, 13]. Previous studies show that male dentists and those working in non-metropolitan areas accepted more Medicaid patients than their counterparts [13–15].
A study of Iowa dentists showed that, in general, dentists who accepted Medicaid-enrolled patients had significantly higher altruistic attitudes compared to those who did not [14]. A recent study found that pediatric dentists who took new Medicaid-enrolled children every month were significantly more likely to report a willingness to advocate for community water fluoridation [16]. However, this study did not assess their participation in an activity advocating for water fluoridation or other advocacy-related activities (ARAs).
Public health advocacy involves speaking out selflessly on behalf of a program or a population and actively promoting a cause or principle [17]. A health care professional can participate in two broad advocacy-related activities (ARAs). First, as an “agent” by helping individual patients navigate and utilize health care services. Second, as an “activist” by helping advance the health of the communities and populations [18]. To be an advocate, one should be compassionate, and socially responsible. Likewise, dentists who are willing to provide services to new Medicaid-enrolled children every month, despite knowing the financial and administrative setbacks of the Medicaid program, can be considered compassionate and socially responsible. Therefore, we explored the relationship between participating in different ARAs and accepting new Medicaid-enrolled children in clinical practice to provide dental services. We hypothesized that Pediatric Dentists (PDs) participating in various ARAs would be at higher odds of accepting new Medicaid-enrolled children into their dental practice.
Methods
Survey instrument
This cross-sectional study was conducted using a 14-item pilot-tested survey instrument. The questions were adapted from previously conducted research studies and published advocacy toolkits [19–23]. The survey collected the following data but was not limited to: age, gender (Male/Female), year graduated from the pediatric dental residency program, type of practice setting in which PDs worked primarily (Solo practice, single group specialty, group multi-specialty, county health department, community health center, Federally Qualified Health Center (FQHCs), State or federal correctional facility clinic, other state government clinical setting, military facility clinic, Veteran Affairs (VA) clinic, academic institution, Indian Health Service), location of the primary practice (Rural/Sub-urban/Urban/Inner City), and previous training in oral health advocacy during dental education (Yes, during residency training/Yes, during predoctoral training/Yes, during both residency and predoctoral training/No training). Using a check box option, dentists were asked to select all ARAs they participated in after graduating from their pediatric dental residency training. The list of 8 ARAs include: (1) Write to an editor of a leading newspaper urging them to report on particular oral health or overall health issue (2) Communicate on Facebook or Twitter or by E-mail to promote better health, (3) Discuss a significant health issue during a town hall meeting or a public forum, (4) Participate in a community rally for a great cause, (5) Advocate for community water fluoridation at city/ local water board meetings, (6) Work with a coalition or group to improve the health of the community, (7) Donated dental services on Give Kids a Smile Day, at free clinics or through community outreach, and (8) Participation in other advocacy efforts (open-ended response).
Data collection
The survey was adapted into an online format using the Survey Monkey® (www.surveymonkey.com) platform. The online survey was administered to 5,591 pediatric dentists (PD) who were members of the American Academy of Pediatric Dentistry (AAPD) practicing in the US. The AAPD provided the list of active PD members and their emails (n = 5,591). PDs were given a choice to opt-out after being introduced to the purpose of the study. After the initial email message with the survey link was sent to the PDs in January 2019, three additional reminders at 2-week intervals were sent to improve the response rate. The survey was open for completion until the end of March 2019.
Statistical data management
Several new variables were created. A “years since graduation” variable was calculated by subtracting the year the PD reported graduating from pediatric dental residency from the year the survey was conducted (2019). A new variable (Practice Location) reflecting the primary practice location was dichotomized into rural/suburban areas or urban/inner-city practices. Dental “practice settings” were recategorized into safety-net settings (county health department, community health center, FQHCs, state or federal correctional facility clinic, other state government clinical setting, military facility clinic, Veteran Affairs clinic, Academic Institution, and Indian Health Service) vs. non-safety net settings (solo practice, group single-specialty practice, and group multi-specialty practice). A new variable, “prior training in oral health advocacy during dental education” (Yes/No), was created. Those who had oral health advocacy training during pediatric dental residency, predoctoral training, or residency and predoctoral training were considered to have received training during dental education. In contrast, those without exposure were considered not to have been trained in advocacy during dental education.
Outcome variable
Accepting new Medicaid-enrolled children every month by PDs into their primary clinical dental practice (Yes/No) was used as the primary outcome variable.
Primary independent variable
A new cumulative score variable was created to determine the mean number of ARAs that PDs participated in after graduating from the pediatric dental residency program by summing all the positive responses to the 8 ARA statements (cumulative score range 0 to 8). A higher cumulative score indicates that PDs participated in more ARAs.
Statistical analysis
Descriptive analysis was performed to understand the characteristics of the study sample. Frequency, means, standard deviations (SD), and proportions were derived. Chi-square tests and Student t-tests were performed to compare dentists who accepted new Medicaid-enrolled children every month to those who did not. Multivariable logistic regression model determining the association between participating in various ARAs (primary independent variable) and acceptance of Medicaid-enrolled children every month (outcome variable) by PDs was conducted, controlling for the following variables: age, gender, years since graduation, practice location, practice setting, and prior advocacy training during dental education.
Results
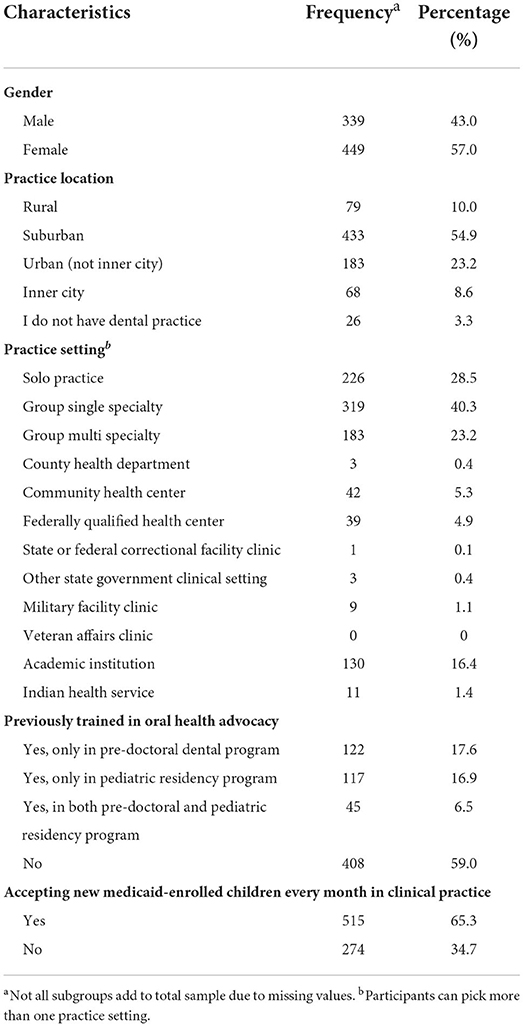
Out of 5,591 PDs to whom the online surveys were sent, 123 emails were not deliverable. In addition, 328 PDs opted out of the study. The total adjusted response rate was 14.4%, with 789 PDs responding to the survey. The mean age of the participants was 45.1 ± 12.8 years, with the mean years since graduation from pediatric dental residency training of 15± 13.2 years. Most responding dentists were females (57%), practicing in suburban locations (55%) and in group single-specialty settings (40%). Approximately 65% reported accepting new Medicaid-enrolled children monthly. Most PDs answered that they were not previously trained in oral health advocacy during dental education (59%) (Table 1).
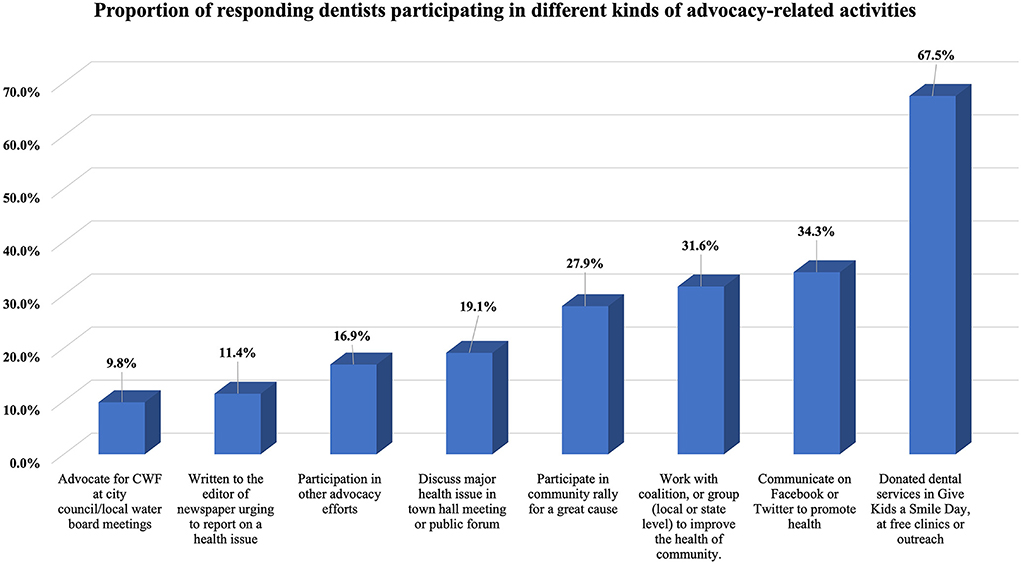
The mean number of ARAs participated by PDs since graduating from a pediatric dental residency program was 2.2 ± 1.8, with Figure 1 demonstrating the distribution of ARAs. The most frequently practiced ARA was donating dental services in Give Kids a Smile day, at free clinics or through community outreach (64.5%), Facebook/Twitter communication to promote good health (34.3%), and coalition collaboration to improve community health (31.6%). The least performed activities were writing newspaper editorials/letters about oral health or overall health issue (11.4%) and community water fluoridation advocacy at city council/local water board meetings (9.8%). Nearly 17% indicated that they participated in other types of ARAs or in events representing advocacy, which include (but are not limited to): AAPD advocacy or lobby day, dental legislative day, visiting capitol hill to meet with legislators, testifying before a state legislative committee, non-profit fundraising, and membership on state advisory committees, etc.
Bivariate analysis showed no differences between the PDs who accepted and did not accept new Medicaid-enrolled children every month by age and gender (Table 2). A significant difference between those who accepted vs. not accepted new Medicaid-enrolled children every month was observed by practice location (p < 0.0001), practice setting (p = 0.001), and prior training in advocacy during dental education (p < 0.0001). Statistically significant differences by years since graduation were observed between dentists who accepted and did not accept new Medicaid-enrolled children every month (p = 0.02). PDs who accepted new Medicaid-enrolled children every month reported participating in a higher number of ARAs after graduating from the pediatric dental residency program than PDs who did not accept new Medicaid children every month (p = 0.006).
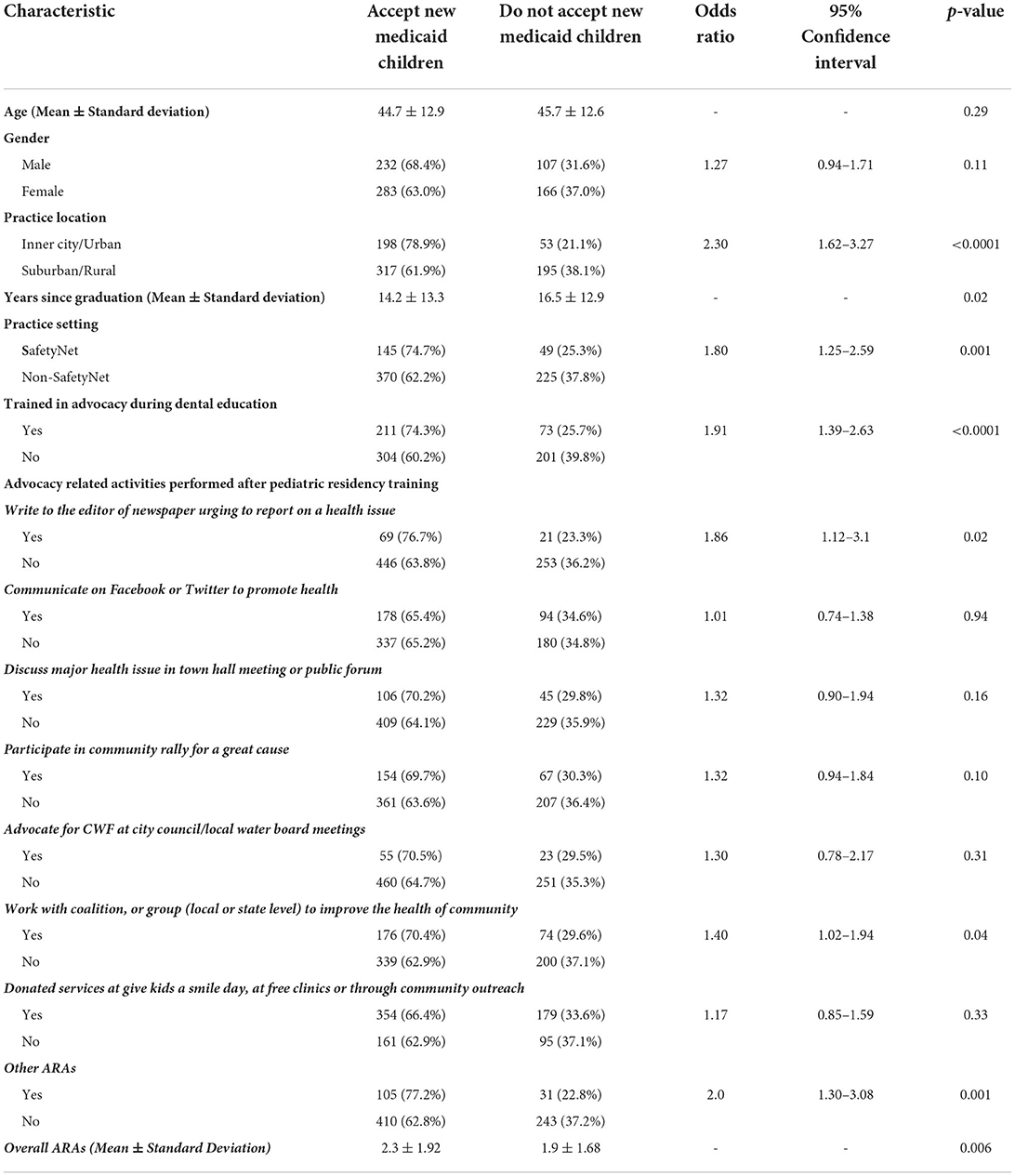
Table 2. Comparisons of pediatric dentists who accept and do not accept new Medicaid-enrolled children every month.
The multivariable logistic regression model showed that the odds of a PD accepting new Medicaid-enrolled children every month increased by 13% for each additional unit increase in ARA completed, with other variables being held constant [Odds ratio (OR): 1.13, 95% CI: 1.03–1.25, p = 0.01] (Table 3). PDs practicing in inner-city or urban areas (OR: 2.08, 95% CI: 1.43–3.03, p = 0.0001), safety net settings (OR: 2.05, 95% CI: 1.31–3.20, p = 0.002), and with prior advocacy training during dental education (OR: 1.61, 95% CI: 1.1–2.34, p = 0.01) were at higher odds of accepting new Medicaid-enrolled children every month compared to their counterparts. Age (p = 0.0001) and years since graduation (p < 0.0001) were also significant predictors.
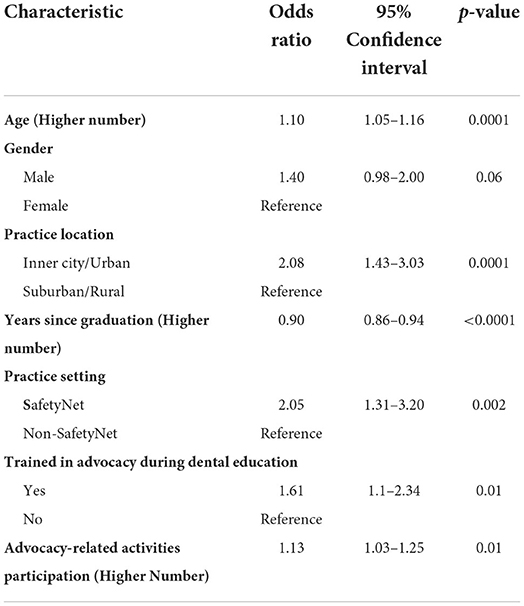
Table 3. Multivariable logistic regression results showing pediatric dentists' acceptance of new Medicaid-children every month in clinical practice.
Discussion
In our study, we assessed if PDs participating in different ARAs were more inclined to take new Medicaid-enrolled children into their dental practice every month. We tested this hypothesis because advocacy is an essential attribute of the dental profession, which provides a voice to fight for a good cause for those less empowered in the community. One way the healthcare community can demonstrate social responsibility is by providing care to Medicaid recipients. Medicaid serves vulnerable populations and aims to help reduce health disparities in the community by providing care to those who cannot get it [24]. Therefore, we expected that those performing one or more ARAs would be more inclined to be accepting new Medicaid-enrolled children in their clinical practice. The results proved that our assumption was correct.
According to the American Dental Association, around 73% of PDs participated in the Medicaid and CHIP programs for child dental services in 2019 [4], while our study found a lower participation rate (65%). We specifically asked about PD's new acceptance of Medicaid-enrolled children every month to identify whether this activity was a consistent and ongoing practice, rather than reflecting Medicaid registration without providing care or providing care to a pre-existing Medicaid patient pool.
We were surprised that the responding dentists, on average, had participated in only two types of ARAs post-graduation (out of eight possible ARAs). This low level of participation could be due to PD's interest in performing a specific kind of ARA or their confidence levels in participating in a particular ARA compared to others. The most-reported ARA was providing free dental care services and communicating on social media to promote health, which was far more frequent than activities like advocating for community water fluoridation at city council meetings (the least reported ARA). PDs may find communicating with the public on social media more meaningful or easier to accomplish, especially when technology and internet use are ubiquitous. In addition, making a social media post or communication does not require much additional time or resources. On the other hand, advocating for water fluoridation in city council meetings may require different skills and more time from a pediatric dentist's everyday busy life. This reasoning is supported by a prior study assessing PDs' willingness to advocate for water fluoridation, which found that almost 13% of unwilling dentists expressed lack of time as a significant barrier [16].
Approximately 41% of the responding participants reported being trained in public health advocacy during dental school. We discovered that receiving advocacy training during dental education made PDs 65% more likely to accept new-Medicaid enrolled children every month than those without training. Previous studies show that integrating a legislative advocacy project into undergraduate or graduate-level courses positively impacts students' knowledge, values, and attitudes [25, 26] and self-efficacy skills [27]. The findings from these studies and our study indicate the importance of integrating advocacy training during dental education. Advocacy training may sensitize students and prepare them to accept and provide dental services to underserved Medicaid patients with high dental care needs. However, due to the cross-sectional nature of this data, we cannot determine if advocacy training during dental education directly impacted PD's willingness to accept new-Medicaid enrolled children. This association needs to be explored further.
Practice location and practice settings were two factors that were strongly associated with accepting new Medicaid-enrolled children by PDs. In our study, those working in urban/inner-city (metropolitan) areas were more likely to accept Medicaid children. This finding contrasts with previous studies where dentists from rural or non-metropolitan areas were more likely to take Medicaid patients [13, 28]. PDs working in safety-net settings were significantly more likely to accept new Medicaid children than those working in non-safety net environments. This is expected since serving Medicaid and uninsured patients is the sole safety-net setting mission [29]. We also found that for every unit increase in PD's age, there was a 10% increase in accepting Medicaid-enrolled children indicating that older PDs were more likely than younger PDs to accept new Medicaid-enrolled children. Again, this finding contrasts with a few other previous studies where age was not a significant predictor of Medicaid participation [13, 14].
Our study is not without limitations. First, the response rate was very low, which increased the chances of non-response bias. Though the response rate was low, the sample size was adequate for multivariable logistic regression analysis with good power. Secondly, as this survey was voluntary and was self-reported, there is a chance that PDs may have over-reported their actual level of ARA participation, leading to a possible social desirability bias. Lastly, as the nature of the study was cross-sectional, we could not determine a causal relationship between being trained in advocacy during dental school and acceptance of new Medicaid enrolled children every month. In addition, we did not inquire about the frequency with which they performed a particular ARA, which would shed more light on the global scope of PD involvement in public health advocacy.
Conclusions
PDs who participated in more ARAs were more likely to accept new Medicaid-enrolled children every month in their clinical practice to provide dental care services. Training in oral health advocacy during dental education may enhance advocacy practices/behaviors of PDs, such as the ARAs measured in this study. Advocacy training has the potential to promote participation in ARAs after graduation, and enhance other socially responsible behaviors like accepting new Medicaid patients in clinical practice to provide dental care services.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was reviewed and approved as exempt by the Institution Review Board at Temple University (Protocol number: 25568). The patients/participants provided their written informed consent to participate in this study.
Author contributions
JL, CD, EC, SW, and SS were involved in developing the survey and data collection. AS and VB was involved in analyzing the data, preparing the manuscript, and completed the first draft of the work. VB was involved in conceptualizing the project, developing the survey, study design, collecting the data, reviewing, and submitting the manuscript. All authors revised the manuscript critically for important intellectual content, reviewed the manuscript, and approved the final version to be published.
Funding
This study was funded by the Temple University Kornberg School of Dentistry (TUKSoD), Philadelphia, PA. The study was conducted while all authors were at TUKSoD.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Rudowitz R, Garfield R, Hinton E. 10 Things to Know About Medicaid: Setting the Facts Straight. (2019). Available online at: https://www.kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-setting-the-facts-straight/ (accessed June 07, 2021).
3. Centers for Medicaid Medicare Services. Medicaid and CHIP Enrollment Data: January 2021 Medicaid and CHIP ENROLLMENt Data Highlights. (2021). Available online at: https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html (accessed March 23, 2022).
4. American Dental Association,. Dentist Participation in Medicaid or CHIP. (2019). Available online at: https://www.google.com/url?sa=tandrct=jandq=andesrc=sandsource=webandcd=andved=2ahUKEwjt5vrChJD3AhWbJEQIHTBXBsAQFnoECAsQAQandurl=https%3A%2F%2Fhttp://www.ada.org%2F-%2Fmedia%2Fproject%2Fada-organization%2Fada%2Fada-org%2Ffiles%2Fresources%2Fresearch%2Fhpi%2Fhpigraphic_0820_1.pdfandusg=AOvVaw08b20BU-w594gxe9l3u6pF (accessed April 12, 2022).
5. Mofidi M, Rozier RG, King RS. Problems with access to dental care for medicaid-insured children: what caregivers think. Am J Public Health. (2002) 92:53–8. doi: 10.2105/AJPH.92.1.53
6. Logan HL, Catalanotto F, Guo Y, Marks J, Dharamsi S. Barriers to medicaid participation among florida dentists. J Health Care Poor Underserved. (2015) 26:154–67. doi: 10.1353/hpu.2015.0000
7. United States General Accounting Office,. Report to Congressional Requesters. Factors Contributing to Low Use of Dental Services by Low-Income Populations. (2000). Available online at: https://www.gao.gov/assets/hehs-00-149.pdf (accessed May 28, 2021).
8. Kateeb ET, McKernan SC, Gaeth GJ, Kuthy RA, Adrianse NB, Damiano PC. Predicting dentists' decisions: a choice-based conjoint analysis of Medicaid participation. J Public Health Dent. (2016) 76:171–8. doi: 10.1111/jphd.12126
9. Chi DL, Kateeb ET. Factors influencing dentists' willingness to treat Medicaid-enrolled adolescents. J Public Health Dent. (2021) 81:42–9. doi: 10.1111/jphd.12391
10. Al Agili DE, Pass MA, Bronstein JM, Lockwood SA. Medicaid participation by private dentists in Alabama. Pediatr Dent. (2007) 29:293–302.
11. Okunseri C, Bajorunaite R, Abena A, Self K, Iacopino AM, Flores G. Racial/ethnic disparities in the acceptance of Medicaid patients in dental practices. J Public Health Dent. (2008) 68:149–53. doi: 10.1111/j.1752-7325.2007.00079.x
12. Garg S, Rubin T, Jasek J, Weinstein J, Helburn L, Kaye K. How willing are dentists to treat young children?: a survey of dentists affiliated with Medicaid managed care in New York City, 2010. J Am Dent Assoc. (2013) 144:416–25. doi: 10.14219/jada.archive.2013.0135
13. Morris PJ, Freed JR, Nguyen A, Duperon DE, Freed BA, Dickmeyer J. Pediatric dentists' participation in the California medicaid program. Pediatr Dent. (2004) 26:79–86.
14. McKernan SC, Reynolds JC, Momany ET, Kuthy RA, Kateeb ET, Adrianse NB, et al. The relationship between altruistic attitudes and dentists' Medicaid participation. J Am Dent Assoc. (2015) 146:34–41.e3. doi: 10.1016/j.adaj.2014.11.014
15. Reynolds JC, McKernan SC, Damiano PC, Kuthy RA. A tale of two public dental benefit programs: Iowa dentist participation in traditional medicaid versus a medicaid expansion program. BMC Oral Health. (2019) 19:89. doi: 10.1186/s12903-019-0771-z
16. Vishnevetsky A, Mirman J, Bhoopathi V. Effect of advocacy training during dental education on pediatric dentists' interest in advocating for community water fluoridation. J Dent Educ. (2018) 82:54–60. doi: 10.21815/JDE.018.008
17. Breitrose P. University of Kansas Work Group for Community Health and Development. Chapter 30, section 1: Developing a plan for assessing local needs and resources. Community toolbox kit. Available online at: https://ctb.ku.edu/en/table-of-contents/advocacy/advocacy-principles/overview/main (accessed April 05, 2022).
18. Dobson S, Voyer S, Regehr G. Perspective: agency and activism: rethinking health advocacy in the medical profession. Acad Med. (2012) 87:1161–4. doi: 10.1097/ACM.0b013e3182621c25
19. American Academy of Pediatrics (AAP). Section on Oral Health (SOOH) Advocacy Tool Kit. (2018). Available online at: https://www.aap.org/en-us/Documents/SOOH%20Advocacy%20Toolkit_031918.pdf (accessed February 20, 2022).
20. American Academy of Pediatric Dentistry. Advocacy Training: A Guide to Assist Programs in Developing Curricula to Address Standard 4, 26. and 4.27 on Advocacy. (2016). Available online at: https://www.aapd.org/globalassets/media/advocacy/advocacytrainingguide-final.pdf (accessed June 27, 2022).
21. Bhoopathi V, Vishnevetsky A, Mirman J. Pediatric dentists who accept new Medicaid-enrolled children report a higher willingness to advocate for community water Fluoridation. BMC Oral Health. (2019) 19:115. doi: 10.1186/s12903-019-0812-7
22. Bhoopathi V, Jacob M, Reusch C. Oral Health Advocacy Toolkit: Strategies and Resources for Dental Schools and Dental Hygiene Programs. (2019). Available online at: https://dentistry.temple.edu/sites/dentistry/files/Oral_Health_Advocacy_Toolkit.pdf (accessed March 25, 2022).
23. Bono LK, Rogo EJ, Hodges K, Frantz AC. Post-graduation effects of an advocacy engagement project on alumni of a dental hygiene program. J Dent Edu. (2018) 82:118–29. doi: 10.21815/JDE.018.017
24. Institute of Medicine (US) Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public's Health in the 21st Century. Washington, DC: National Academies Press (US) (2002). https://www.ncbi.nlm.nih.gov/books/NBK221239/ (accessed March 19, 2022).
25. Rogo EJ, Bono LK, Peterson T. Developing dental hygiene students as future leaders in legislative advocacy. J Dent Educ. (2014) 78:541–51. doi: 10.1002/j.0022-0337.2014.78.4.tb05704.x
26. Bono LK, Rogo EJ, Hodges KO. Legislative advocacy: undergraduate and graduate student learning outcomes. J Dent Hyg. (2021) 95:50–7.
27. Meyer BD, Fearnow B, Wolcott MD. Introducing legislative advocacy into the dental school curriculum: a mixed-methods evaluation. J Dent Educ. (2020) 84:1378–87. doi: 10.1002/jdd.12336
28. Ku L, Han X, Chen C, Vujicic M. The association of dental education with pediatric Medicaid participation. J Dent Educ. (2021) 85:69–77. doi: 10.1002/jdd.12390
29. Institute Institute of Medicine (US) Committee on the Changing Market Managed Care and the Future Viability of Safety Net Providers Ein Lewin M Altman S editors. Americas's Health Care Safety Net: Intact but Endangered 4. How Safety Net Providers Are Adapting to the New Environment. Washington, DC: National Academies Press (US). (2000). https://www.ncbi.nlm.nih.gov/books/NBK224525/ (accessed March 19, 2022).
Keywords: advocacy, Medicaid, pediatric dentist, social responsibility, medicaid acceptability
Citation: Singh AD, Lavin J, DiStefano C, Chon E, Weinstein S, Slutsky S and Bhoopathi V (2022) Pediatric dentists' participation in advocacy and acceptance of new medicaid children in clinical practice. Front. Oral. Health 3:923124. doi: 10.3389/froh.2022.923124
Received: 18 April 2022; Accepted: 05 July 2022;
Published: 03 August 2022.
Edited by:
Marco Magalhaes, University of Toronto, CanadaReviewed by:
Noha Gomaa, Western University, CanadaBeau Meyer, The Ohio State University, United States
Copyright © 2022 Singh, Lavin, DiStefano, Chon, Weinstein, Slutsky and Bhoopathi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vinodh Bhoopathi, VmJob29wYXRoaUBkZW50aXN0cnkudWNsYS5lZHU=
†These authors have contributed equally to this work
 Arjun Deo Singh1
Arjun Deo Singh1 Vinodh Bhoopathi
Vinodh Bhoopathi