- 1Private Dental Practice, Gaithersburg, MD, United States
- 2Department of Global Health, Boston University School of Public Health, University of Massachusetts Medical Center, Boston, MA, United States
- 3Center for Deaf Health Equity, Gallaudet University, Washington, DC, United States
Introduction: Despite the significant number of deaf and hard of hearing (DHH) people living in the U.S., oral health research on DHH people who use American Sign Language (ASL) is virtually nonexistent. This study aims to investigate dental needs among mid-to-older DHH women and identify social determinants of health that may place them at higher risk for unmet dental health needs as the primary outcome.
Methods: This cross-sectional study uses data drawn from Communication Health domain in the PROMIS-DHH Profile and oral health data from the National Health and Nutrition Examination Survey. Both measures were administered in ASL and English between November 2019 and March 2020. Univariate and bivariate analysis included only complete data, and multivariable logistic regression analyses were conducted on multiply imputed data.
Results: Out of 197 DHH women (41 to 71+ years old) who answered the dental visit question, 48 had unmet dental needs and 149 had met dental needs. Adjusting for sociodemographic variables, disparity in dental needs was observed across education [OR (95% CI): 0.45(0.15, 1.370)] and communication health [0.95 (0.90, 1.01)].
Discussion: Our study is the first to describe DHH mid-to-older women's access to oral health care. DHH women who do not have a college degree may be impacted. Further research is needed to elucidate the particular risk factors, including cultural, to which DHH individuals from marginalized racial groups are susceptible to unmet oral health needs.
Conclusions: Evidence shows that DHH ASL users who have less years of education or are single experience barriers in accessing dental care.
Introduction
In the United States, about 9% of the population has hearing loss that may be congenital or age-related, and ~500,000 are American Sign Language (ASL) users [1, 2]. Despite the significant number of DHH people living in the U.S., oral health research on deaf and hard of hearing (which will hereon be referred to as “DHH”) people who specifically use ASL is virtually non-existent. No dental or oral health care studies included measures or survey interviews that are fully accessible to DHH people who use ASL.
Disparities in accessing dental care and maintaining good oral health [3, 4], which are informed by socioeconomic factors, can take a toll on an individual's comprehensive wellbeing [5–7]. Considering these disparities, coupled with the understanding that DHH people have historically faced communication and information barriers in healthcare [8], we intend to determine whether oral health disparities among the general population from marginalized groups are also reflected within the DHH community.
In the general oral health literature, disparities in dental health care are observed among adults who self-identify as Persons of Color (POC), have a high school education or lower, and have low income. Studies have found that untreated cavities have a higher prevalence among non-Hispanic Black or Mexican-American adults and adults with less than a high school education, as well as 40% of low-income adults or adults without private health insurance [5, 7]. Specifically, over 40% of low-income and non-Hispanic Black adults among US adults ages 20–62 have untreated tooth decay. Older adults with low income also experience oral health issues at higher rates, with complete tooth loss being two times as common among adults over 75 than adults aged 65–74 as of 2011-2012 [6]. Untreated oral diseases may impact overall physical health and create a cycle in which already disadvantaged individuals continue to be burdened with high financial costs and poor health outcomes.
The inexorable connection between oral health and overall physical health, including chronic diseases (e.g., cancer, depression, and cardiovascular issues), emphasizes the need to encourage good oral hygiene for all [2, 4, 9]. A large survey conducted in Maryland identified health literacy as playing an essential role in quality of dental care and primary prevention of dental issues and diseases [9]. Research has also identified financial and socioeconomic factors as significant barriers to dental care, oral health literacy, and consequently, good oral health [5, 6]. For example, non-elderly adults were more likely to face financial barriers in all types of care, including dental, than children under 21 years of age by Medicare and elderly adults who have the optional benefit of dental care coverage with Medicaid [10].
As aforementioned above, research clearly supports the finding that barriers to health communication and knowledge are associated with poor health outcomes among DHH people from underserved groups. However, research on oral health in the DHH community that uses ASL is virtually non-existent. This study is the first to date to gather dental needs data from mid-to-older DHH women through a fully accessible survey interview method. Results will be used to identify subgroups who are at disparity for dental needs and also improve oral health outcomes among DHH people who use ASL.
Materials and Methods
Measures
This study uses data drawn from the Communication Health Scale in the PROMIS-Deaf Profile and oral health questions in the National Health and Nutrition Examination Survey (NHANES). Below are the communication and oral health items that were asked and used for the purpose of this study.
PROMIS-Deaf Profile: Communication Health [11] (Responses: Always, Often, Sometimes, Rarely, Never).
• I feel my life is good even though I am deaf or hard of hearing.
• I am satisfied with the way I communicate with deaf/hh people.
• In general, I feel people accept me as a person who is deaf or hard of hearing.
• People who are close to me accept me as a person who is deaf or hard of hearing.
• I am able to easily get the information I need to make decisions.
• People closest to me share the same communication and language.
• People close to me make an effort to communicate with me because I am deaf or hard of hearing.
• I have friends who are like me and can understand what it is like to be deaf or hard of hearing.
National Health and Nutrition Examination Survey (NHANES) [12].
• About how long has it been since {you/SP} last visited a dentist? Include all types of dentists, such as, orthodontists, oral surgeons, and all other dental specialists, as well as dental hygienists.
Procedure
Following the institution's human subjects review board's approval, DHH women were recruited through purposive sampling between November 2019 and March 2020. After they filled out an appointment form, a project coordinator contacted them to schedule an interview consisting of two parts: (1) filling out demographics and PROMIS-Deaf Communication Health [11] online survey that is fully accessible in ASL and English, and (2) completing a face-to-face interview with a DHH female research staff fluent in ASL. The face-to-face interview could be completed either in person or through a videoconferencing platform. The total time spent on completing the demographics and NHANES oral health interview was 1 h or less, and each person was given a $25 gift card for their participation.
Quantitative Analysis Plan
All respondents included in this analysis identified with being female. Sociodemographic variables included age in years, education, race/ethnicity, marital status, health status, and language preference. A new variable was created based on the total number of household members and the total household pre-tax income as a surrogate measure of household poverty. Another measured characteristic included the PROMIS Communication Health T-Score. For a robust sample size to increase the power of racial/ethnic group analysis, African-American/Black group (n = 5), Asian/Other (n = 7) and Latinx (n = 11) were combined into a Persons of Color group. The Persons of Color group (n = 23) was then compared to the white group (n = 25). Univariate and bivariate analysis included only complete data, and multivariable logistic regression analyses were conducted on multiply imputed data.
Summary statistics [proportions, means and standard deviations (SD)] of sociodemographic and health sample characteristics were obtained for the full female sample, with met and unmet dental health needs. A bivariate analysis tested the association of characteristics and PROMIS Communication Health T-Scores with met and unmet dental health needs in the previous 12 months using a Fisher's Exact Test (categorical variables) or T-Test (continuous variables).
Nine (4%), 1(0.5%), 26(13%), 35 (17%) and 49 (24%) subjects had missing data for outcome, education, income, health status and PROMIS Communication Health Score. We created 20 multiply-imputed datasets assuming data was Missing at Random (i.e., missingness depends only on the observed data). Odds Ratios (OR) and 95% Confidence Intervals (CI) were obtained from multivariable logistic regression models fit to each of these datasets. The models evaluated the association of having unmet dental health needs with Age in years (41–50, 51–60, 61–70, ≥71), Race/Ethnicity {white (Ref), Education [HS degree (Ref), Some college, College graduate], Marital Status [Divorced/Widowed/Separated/Never Married (Ref), Married/Living with Partner], and Health Status [Poor/Fair, Good, Very Good/Excellent (Ref)]}. Results were combined from these 20 datasets using the methods described in Rubin [13]. The p-values from the 20 regressions were combined as described in Li et al. ([14], Significance levels from repeated p-values with multiply-imputed data).
Further analysis was limited to data from DHH mid-to-older women who self-reported having unmet dental health needs. All analyses were conducted in SAS 9.4 (SAS Institute Inc., Cary, NC) and a two-sided p-value < 0.05 was considered statistically significant.
Results
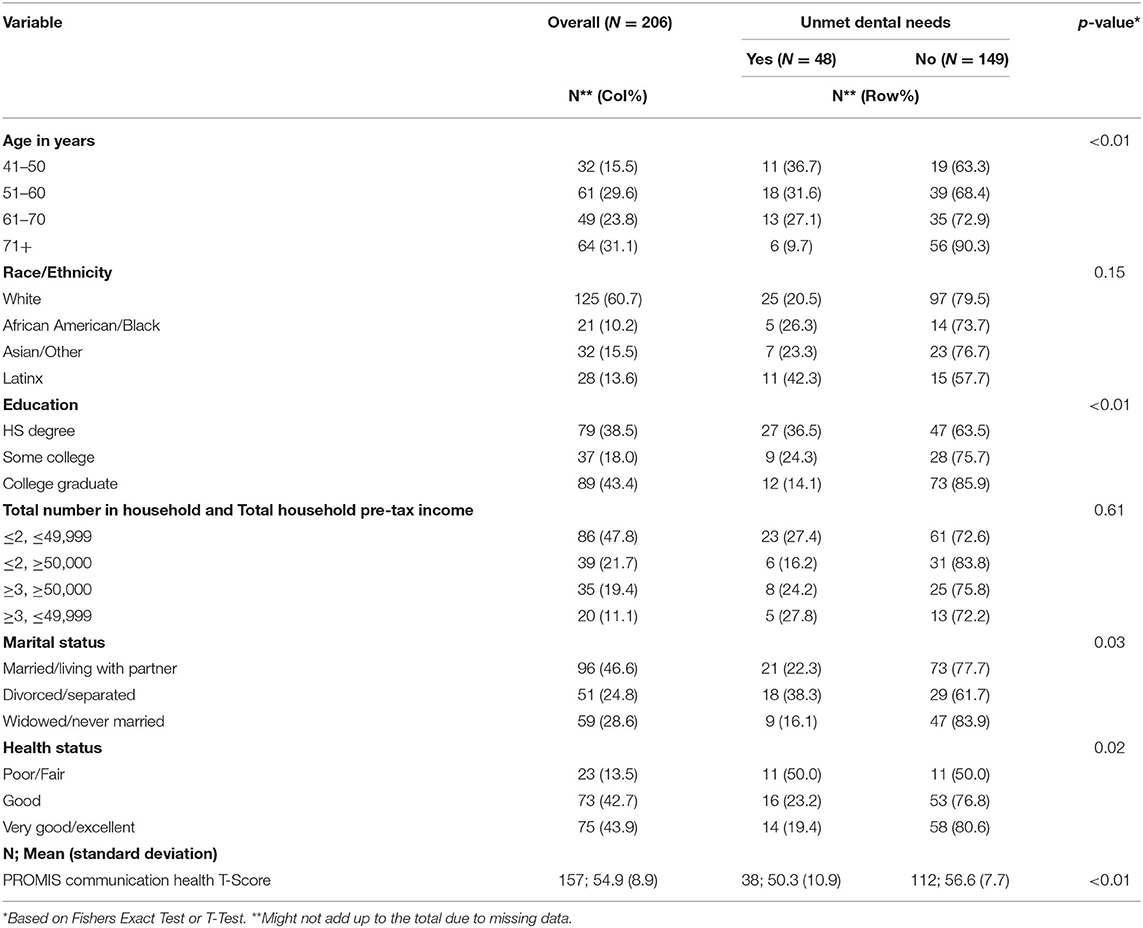
As shown in Table 1, 206 DHH mid-to-older women (48% with < =2 total household members and < =$49,999 total household pre-tax income; 47% married or living with a partner) participated in an interview about their oral health. Majority of the sample self-identified as white (61%). About 39% of the sample had a high school education or lower while 18% completed some college and 43% self-reported having a college degree that could include an associate degree or higher. When asked to rate their health, 44% of the sample self-rated as very good or excellent.
When asked specifically about visiting a dentist, 197 answered this question and were therefore included in subsamples of unmet dental needs (n = 48) and met dental needs (n = 149). Between these two subsamples, disparity was observed across multiple characteristics. Nine DHH women did not indicate whether their needs were met or not. Table 1 shows that unmet needs were higher among the younger DHH women with lower education and lower income than their counterparts (older, higher education and higher income). Thirty-one percent (n = 11) of Persons of Color had unmet dental needs compared with 21% (n = 25) of White and 23% (n = 7) of Asian/Other DHH women.
The proportion of unmet dental needs was higher for divorced/separated women compared to other groups. For example, 38% (n = 18) of divorced/separated women had unmet dental needs while only 22% (n = 21) of women who were married or living with partners 16% (n = 9) of those widowed/never married had unmet needs. The unmet dental needs were proportionally higher for DHH women who self-reported their health as being poor or fair (50%) compared to DHH women whose reported health were very good or excellent (19%). The average PROMIS communication health score was lower among those with unmet needs (mean = 50.3; SD = 10.9) than those without unmet needs (56.6; 7.7) (p < 0.01).
After adjusting for other variables in Table 2, results from multivariable logistic regression model indicate that education was statistically significant (p = 0.02) for unmet dental needs. Compared with DHH women with a high school education or lower, those with some college had 55% reduced odds [OR (95% CI): 0.45 (0.15, 1.37)] and those with a college education had 76% reduced odds [OR (95% CI): 0.24 (0.09, 0.64)] of having unmet oral needs. In other words, DHH women who did not have any years of college education had higher odds of experiencing unmet dental needs.
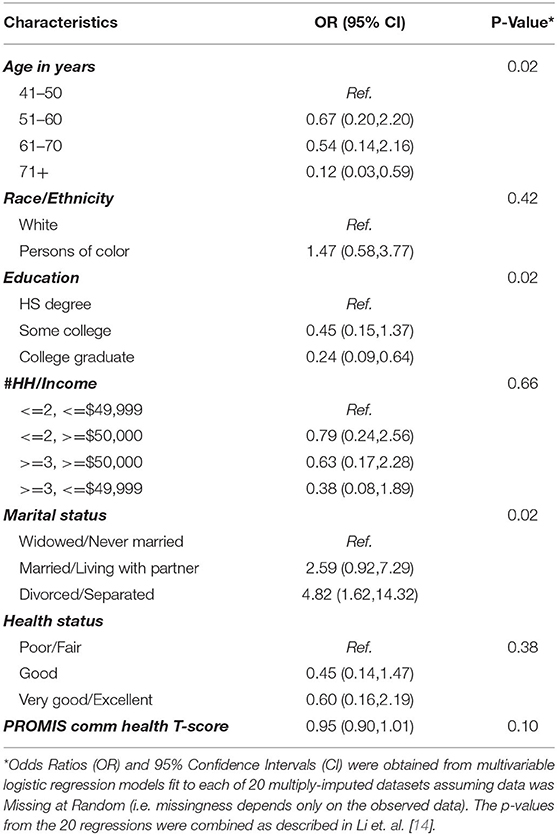
Table 2. Odds Ratios (OR) and 95% Confidence Interval (CI) obtained from logistic regressions to evaluate the association of characteristics with unmet dental needs (n = 48).
Although not statistically significant, the odds of unmet needs were relatively higher for those who were Persons of Color compared to white [1.47 (0.58, 3.77)], single compared to those who are married or living with partner [2.59 (0.92, 7.29)]; and divorced or separated [4.82 (1.62, 14.32)] compared with those widowed or never married. The odds decreased with increasing age from 0.67 (0.20, 2.20) for 51–60 years to 0.12 (0.03, 0.59) for 71+ years, and were lower for those who had 3 or more number of household members and < =$49,999 income [0.38 (0.08, 1.89] than those with < =2 members and < =$49,999 total household income, and those with very good/excellent health [0.60 (0.16, 2.19)] compared with those reporting poor/fair health. The odds of unmet needs also decreased per unit of increase in PROMIS Communication Health T-Score [0.95 (0.90, 1.01)].
Discussion
Our study is the first to describe DHH mid-to-older women's access to oral health care. All DHH women in our sample used ASL. Within this sample, DHH women who reported low-perceived communication health (e.g., not being accepted as a DHH person by others; difficulty with letting others know about their communication needs) were more likely to have unmet dental needs. This is consistent with a national patient-reported outcomes study that reported lower Global Health status (worse overall health) among DHH adults with worse communication health scores [11]. The Kushalnagar et al. study also found that worse communication health scores were associated with lower levels of education and self-identifying as belonging to a marginalized group.
DHH women with financial struggles may not have easy access to oral health care and those who do not have a college degree may be impacted even more. A review of the literature identifies financial issues as a significant barrier to dental care and good oral health [5, 6]. Our study's finding of an inverse relationship between age and unmet needs is consistent with a study that reported younger adults being at higher risk for financial barriers to dental care [10]. Our results highlight how the dental care system is characterized by inequities that place younger or uneducated DHH women at higher risk for adverse dental health outcomes. Efforts in not only making communication accessible but also taking the time to educate them can have a positive impact in ensuring that their dental needs are met.
A well-designed study conducted by Schneidewind et al., [15] simulated DHH patients who needed new appointments in health and dental offices. This study found that, compared to medical offices, dental offices were far more likely to deny appointment requests from new DHH patients because they needed an interpreter to communicate with the dentist, despite the existence of the federal law that requires effective communication in medical and dental offices. The authors speculated that the higher rejection rate was because dental clinics were less likely to be affiliated with a health care system that may be more equipped to provide accessibility and accommodation. Regardless, communication and attitudinal barriers toward DHH people must be removed to ensure that the DHH individual receives equitable access to dental care. Sign language interpreters are readily available and accessible to accommodate DHH women who communicate best in ASL. For DHH women who prefer English-based communication, speech-to-text transcription or writing on a whiteboard can help clarify potential misunderstandings between the DHH patient and dentist.
Dentists should not stop at communication-related accessibility; they must also take appropriate actions to mitigate social determinants that contribute to poor dental health outcomes. Literature shows that if an individual has adverse childhood experiences in their early years and does not have a college education, they are more likely to experience unmet dental care compared to individuals who have had access to education and health [16]. For our DHH sample, we speculate that the likelihood of dental care being unmet is much higher when a DHH individual self-identifies as belonging to a marginalized racial or ethnic group, does not have a college education, and uses ASL.
While it is not possible to conduct intersectional analysis on multiple intersecting variables (e.g., age, race/ethnicity), we did find an increased odds of unmet needs among mid-to-older DHH women of color after adjusting for correlates. This finding is consistent with research that reported Mexican Americans as less likely to receive preventative dental care and being more likely to experience adverse oral health outcomes, such as periodontitis, in comparison to other ethnic groups in the U.S. [17, 18]. Research has also shown that individuals who are black and U.S. natives or those who are Latinx and do not speak English in the U.S. disproportionately experience barriers to dental care, driven by linguistic and cultural communication barriers, lack of oral health knowledge, and financial difficulties, which may explain why DHH women of color who use ASL reported greater odds of unmet oral health needs in comparison to DHH women who self-identify as white [19, 20]. The intersectionality of multiple marginalized identities is likely to exacerbate the barriers to receiving adequate oral health care among the DHH community. Further research is needed to elucidate the particular risk factors, including cultural, to which DHH individuals from marginalized racial/ethnic groups are susceptible to unmet oral health needs.
Suggested actions toward reducing oral health disparities for DHH patients with less years of education or low oral health literacy include allowing as many questions as possible to be asked and taking time to educate DHH patients. Some DDH patients may carry a belief that dental visits should be reserved for pain-related reasons. Dental schools typically provide cultural humility training as part of their dental curriculum, and dentists are responsible to educate the patients about the importance of dental health care while respecting patients as individuals with a wide range of experiences and beliefs. Dental schools are also often affiliated with a health care system that is equipped to provide interpreting services; dental teams should work together to ensure that interpreting services are set up to accommodate DHH dental patients. Dentists who encounter these DHH patients have the responsibility to accept them as patients and provide appropriate accommodation, including in-person interpreting and video remote interpreting if preferred by the DHH patient (see [21], for a review).
There is much that needs to be done to move toward dental equity for all. More people face financial barriers to accessing dental care more than any other type of care, regardless of socioeconomic status [10]. For DHH individuals, receiving dental care may be made even more difficult when encountering communication barriers in healthcare settings [8]. The American Dental Association established guidelines for how to work with DHH patients and recommends securing an interpreter to accommodate dental patients who require one to communicate [22]. Yet, many dentists in small private offices may not encounter DHH patients often in their care and may be less familiar with resources as to where to secure qualified interpreters. As such, accessibility resources (e.g., interpreting services or communication services for the deaf) need to be made widely available for dentists who may not be familiar with the procedure associated with making interpreting service requests.
Limitations
Study limitations include a majority of white-identified, fully women-identified mid-to-older DHH respondents, self-selected respondents. Although the full sample is large (N = 204) given the nature of our low incidence and hard-to-reach population of ASL-using DHH women, the number of DHH mid-to-older women with unmet dental needs is small (n = 48), which limited our ability to conduct intersectional analyses. An in-depth qualitative study is recommended to identify recurrent issues that emerge in subsamples of DHH women with intersecting identities.
Future Directions and Recommendations
There is evidence that DHH ASL users experience barriers in accessing not only health care but also dental care. It is not surprising that a subset of DHH ASL users with lower education are at higher risk for unmet dental care. Communication breakdowns between the patient and provider risk misdiagnosis and misconceptions regarding a DHH patient's health if accessible communication services are not readily available [15]. Given the link between communication health and unmet dental needs in our study, dental health professionals and advocates must work together to address the systemic gaps in dental health care and identify strategies to prevent communication barriers that may be associated with missed diagnoses and delayed oral treatments.
Data Availability Statement
The datasets presented in this article are not readily available because this is a marginalized subgroup of mid-to-older DHH women in a small community that uses ASL. The dataset may include identifiable information. Requests to access the datasets should be directed to cG9vcm5hLmt1c2hhbG5hZ2FyQGdhbGxhdWRldC5lZHU=.
Ethics Statement
The studies involving human participants were reviewed and approved by Gallaudet University IRB Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AD contributed to conception of the oral health study. PK designed the study, oversaw data collection, and drafted the methods section. SR performed the statistical analysis and drafted the results section. AD and PK interpreted the results. KJ and NM assisted with the literature review. All authors contributed to manuscript, read, and approved the submitted version.
Funding
This work was supported by National Institute on Deafness and Other Communication Disorders (NIDCD) of the National Institutes of Health (R01DC014463-01A1 and R01DC014463-05S1 to PK).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mitchell RE, Young TA, Bachleda B, Karchmer MA. How many people use ASL in the United States? why estimates need updating. Sign Lang Stud. (2006) 6:306–35. doi: 10.1353/sls.2006.0019
2. Ries PW. Prevalence and characteristics of persons with hearing trouble: United States, 1990-91. Vital Health Stat 10. (1994) 188:1–75.
3. Dörfer C, Benz C, Aida J, Campard G. The relationship of oral health with General health and NCDs: a brief review. Int Dent J. (2017) 67:14–8. doi: 10.1111/idj.12360
4. Griffin SO, Barker LK, Griffin PM, Cleveland JL, Kohn W. Oral health needs among adults in the United States with chronic diseases. J Am Dent Assoc. (2009) 140:1266–74. doi: 10.14219/jada.archive.2009.0050
5. Centers for Disease Control and Prevention (CDC). Oral Health Surveillance Report. (2019). Available online at: https://www.cdc.gov/oralhealth/publications/OHSR-2019-index.html (accessed August 6, 2021).
6. Dye B, Thornton-Evans G, Li X, Iafolla T. Dental caries and tooth loss in adults in the United States, 2011-2012. NCHS Data Brief. (2015) 197:197.
7. Williams S, Wei L, Griffin SO, Thornton-Evans G. Untreated caries among US working-aged adults and association with reporting need for oral health care. J Am Dent Assoc. (2021) 152:55–64. doi: 10.1016/j.adaj.2020.09.019
8. Reed NS, Betz JF, Kucharska-Newton AM, Lin FR, Deal JA. Hearing loss and satisfaction with healthcare: an unexplored relationship. J Am Geriatr Soc. (2019) 67:624–6. doi: 10.1111/jgs.15689
9. Horowitz AM, Kleinman DV. Oral health literacy: a pathway to reducing oral health disparities in Maryland. J Public Health Dent. (2012) 72:S26–30. doi: 10.1111/j.1752-7325.2012.00316.x
10. Vujicic M, Buchmueller T, Klein R. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Affair. (2016) 35:2176–82. doi: 10.1377/hlthaff.2016.0800
11. Kushalnagar P, Paludneviciene R, Kallen M, Atcherson S, Cella D. PROMIS-Deaf Profile measure: cultural adaptation and psychometric validation in American sign language. J Patient Rep Outcome. (2020) 4:44. doi: 10.1186/s41687-020-00208-7
12. Centers for Disease Control and Prevention. National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (2016).
13. Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley Sons (1987). doi: 10.1002/9780470316696
14. Li K-H, Meng X-L, Raghunathan TE, Rubin DB. Significance levels from repeated p-values with multiply-imputed data. Statistica Sin. (1991) 1:65–92.
15. Schniedewind E, Lindsay RP, Snow S. Comparison of access to primary care medical and dental appointments between simulated patients who were deaf and patients who could hear. JAMA Netw Open. (2021) 4:e2032207. doi: 10.1001/jamanetworkopen.2020.32207
16. Tellez M, Zini A, Estupiñan-Day S. Social determinants and oral health: an update. Curr Oral Health Rep. (2014) 1:148–52. doi: 10.1007/s40496-014-0019-6
17. Aguirre-Zero O, Westerhold C, Goldsworthy R, Maupome G. Identification of barriers and beliefs influencing engagement by adult and teen Mexican-Americans in oral health behaviors. Community Dent Health. (2016)33:44–7.
18. Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. (2012) 91:914–20. doi: 10.1177/0022034512457373
19. Han C. Oral health disparities: racial, language and nativity effects. SSM Popul Health. (2019) 8:100436. doi: 10.1016/j.ssmph0.2019.100436
20. Walker KK, Martínez-Mier EA, Soto-Rojas AE, Jackson RD, Stelzner SM, Galvez LC, et al. Midwestern Latino caregivers' knowledge, attitudes and sense making of the oral health etiology, prevention and barriers that inhibit their children's oral health: a CBPR approach. BMC Oral Health. (2017) 17:61. doi: 10.1186/s12903-017-0354-9
21. Kushalnagar P, Paludneviciene R, Kushalnagar R. Video remote interpreting technology in health care: cross-sectional study of deaf patients' experiences. JMIR Rehabil Assist Technol. (2019) 6:e13233. doi: 10.2196/13233
22. ADA Marketplace - American Dental Association. (n.d.). Have Patience With Your Patients: How to Treat Hearing-Impaired People. Available online at: https://marketplace.ada.org/blog/dental-business/have-patience-with-your-patients-how-to-treat-hearing-impaired-people/ (accessed January 5, 2022).
Keywords: deaf, sign language, women, dental needs, hard of hearing, oral care access, accessibility
Citation: Donald A, Rao SR, Jacobs K, MacDonald N and Kushalnagar P (2022) Unmet Dental Needs Among Mid-to-Older Deaf and Hard of Hearing Women in the U.S. Front. Oral. Health 3:866537. doi: 10.3389/froh.2022.866537
Received: 31 January 2022; Accepted: 29 April 2022;
Published: 20 May 2022.
Edited by:
Marília L. Goettems, Federal University of Pelotas, BrazilReviewed by:
Jessica Klöckner Knorst, Federal University of Santa Maria, BrazilBhojraj Nandlal, JSS Dental College and Hospital, India
Ricardo Cartes-Velásquez, Universidad de Concepción School of Medicine, Chile
Copyright © 2022 Donald, Rao, Jacobs, MacDonald and Kushalnagar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Poorna Kushalnagar, cG9vcm5hLmt1c2hhbG5hZ2FyQGdhbGxhdWRldC5lZHU=
 Andrew Donald1
Andrew Donald1 Poorna Kushalnagar
Poorna Kushalnagar