- 1Department of Ophthalmology, School of Medicine, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
- 2Department of Optometry, College of Medicine and Health Sciences, Comprehensive Specialized Hospital, University of Gondar, Gondar, Ethiopia
Purpose: The purpose of this study is to measure the proportion, types of glaucoma, and associated factors among outpatient departments at the University of Gondar Comprehensive Specialized Hospital Tertiary Eye Care and Training Center, Northwest Ethiopia.
Methods: An institution-based cross-sectional study design was conducted on 934 participants who were selected by a simple random sampling method at entrance of tertiary eye care and training Center from September to November 2021. A structured questionnaire was used to collect the data through interviews, and the presence or absence, type, and stage of glaucoma were determined by reviewing the chart. The questionnaire was adapted from a previous study, and the data were entered into Epi Info version 7 and analyzed using SPSS version 20. Descriptive data were analyzed in terms of proportion, frequency, mean, and standard deviation. Binary logistic regression was utilized to identify determinant factors, with significance considered at a p-value less than 0.05.
Results: A total of 934 study participants with an 85.33% response rate took part in the study. The mean age of the study participants was 55.67 SD ± 13.21 years. The proportion of glaucoma was 13.4% [(95% CI: (10.9, 15.8)], with Primary Open Angle glaucoma accounting for 96.3% of the total number of glaucoma cases. The age groups of 56-66 [AOR=3.80(95% CI: 1.99-7.26)], 67-87 [AOR=5.34(95% CI: 2.70-10.45)] and those who completed college or university [(AOR= 5.41(95% CI: 2.12-13.82)] were significantly associated with the presence of glaucoma.
Conclusion: This study shows a high proportion of glaucoma compared to other studies, with Primary Open Angle Glaucoma being the most prevalent type. Increasing age and higher education level were significantly linked to the presence of glaucoma. Further research is needed to explore the relationship between education level and glaucoma.
Introduction
Glaucoma is a progressive optic neuropathy characterized by thinning of the neuroretinal rim with excavation and an increase in the optic cup- to- disc ratio and deformation of the lamina cribrosa. Visual field loss is not detected in the early stage and visual acuity remains safe initially; however, its progression can lead to complete loss of vision (1).
Globally, glaucoma is the second leading cause of blindness, with about 3.6 million people becoming blind from glaucoma (2, 3). Primary open-angle glaucoma is high in Africa (2–4). The prevalence of glaucoma globally is increasing, with an estimated 76.0 million cases by the year 2020, and projected to raise to 111.8 million by 2040 (4, 5). It is much higher in Sub-Saharan Africa, where approximately half of glaucoma patients are unilaterally blind at their presentation to the hospital (6).
Many studies have shown that the prevalence rate of glaucoma increases with age (7–9). In Ethiopia, a national survey of low vision and blindness by 2005/6 showed that 5.2% (10), and in North shoa Merhabete woreda 27.7% of blindness is due to glaucoma (11).
Glaucoma decreases the quality of life, especially for elderly patients (12). Community screening is needed for early detection of the disease and treatment accordingly.
Even though a low vision survey was done in Gondar hospital, the real magnitude of glaucoma is hidden. This study aims to fill the gap about the proportion and type of glaucoma as well as the age-specific magnitude of glaucoma.
Glaucoma is a public health issue in Ethiopia but there are no sufficient reports about the magnitude of the disease, especially in the study area. Diagnosing glaucoma at the community level requires more instruments and experienced ophthalmic professionals. This study might provide insight into the magnitude of the disease and risk factors that contributing for the presence of glaucoma.
Materials and methods
Study design and setting
An institution-based cross-sectional study design was used to measure the proportion and associated factors of glaucoma among outpatient ophthalmic patients at the University of Gondar Comprehensive Specialized Hospital Tertiary Eye Care and Training Center, Northwest Ethiopia from September to November 2021.
Source population
All adult outpatients who visited the University of Gondar Comprehensive Specialized Hospital Tertiary Eye Care and Training Center.
Study population
All adult outpatients who attended the eye care center during the study period.
Inclusion criteria
All adult outpatients whose aged 40 years or older included in the study.
Exclusion criteria
Those unable to communicate, and mentally ill.
Sample size determination
The sample size needed to assess the proportion rate of glaucoma was determined using the single population proportion formula on the following assumption. Level of significance (α) = 5% (with confidence level of 95%), Marginal error (w) = 2%, P=0.098 (hospital-based prevalence rate of glaucoma in Gondar 2020) (13), Z-value of 1.96 was used at 95% CI (n= sample size, P= proportion, w= marginal error).
After adding 10% for non-response, the final sample size was calculated to be 934.
Sampling technique
To select 934 patients, the average number of patients who attended ophthalmic services per day was 65, taken from the patient record book of the eye care service for the last month, and the estimated number of patients were seen per month were 1950. Thus K for this study was 2(k=N/n=1950/934≈2.25). The first participant was selected by simple random sampling, then every 2nd patient was selected until the required sample size was achieved.
Data collection tools and procedures
Data collection involved two components; patient medical chart review and a face-to-face interview using a structured questionnaire. The clinical characteristics including the diagnosis, type of glaucoma and its stage were obtained by reviewing the patient’s chart. The structured questionnaire includes socio-demographic characteristics and it is based on patient self-responses.
Operational definitions
Glaucoma
Those patients who had glaucoma confirmed by MSc holder senior clinical optometrists and residents with fully investigated by using Volk lens, Gonioscope as well as FDT and the diagnosis is cross-check over by glaucoma specialist.
Primary open angle glaucoma
Patients those who have deep anterior chamber by slit lamp examination and have open angle by Gonioscope examination.
Primary open angle glaucoma
Patients those who have shallow anterior chamber by slit lamp examination and have closed angle by Gonioscope examination.
Stages of glaucoma
Early: Optic nerve abnormalities consistent with glaucoma but no visual field abnormalities and cup to disc ratio (CDR)< 0.65. Moderate: optic nerve abnormalities consistent with glaucoma and glaucomatous visual field abnormalities in one hemifield, and not within 5 degrees of fixation and moderate glaucomatous disc features of vertical CDR = 0.7–0.85. Advanced: patients who have CDR of 0.85 – 0.95 and glaucomatous visual field abnormalities in bug both hemifields, and/or loss within 5 degrees of fixation in at least one hemifield, and who can perceive light. Absolute: patients who have CDR of ≥ 0.95 and with a vision of no light perception (NLP) (14).
Visual acuity
It is used the ICD 12 definition of visual impairment. Mild/No visual impairment: 6/6 – 6/18, Moderate visual impairment: 6/18 – 6/60, Severe visual impairment 6/60 – 3/60, Blindness: < 3/60 (15).
Data quality control
The questionnaire which was developed from different literature (14, 15) was translated into the local language, Amharic, and back- translated into English by experts and senior ophthalmologists. Pre-testing was done on 7% of the questionnaires out site the study area. Data collectors (ophthalmic nurses) received two days of training on the questionnaire, study purpose, and how to approach respondents. Daily supervision was conducted, and filled questionnaires were checked for completeness and consistency by the supervisor and principal investigator.
Data processing and analysis
The data were entered to EPI INFO 7 and analyzed using SPSS version 20. Descriptive statistics such as proportion, percentage, mean and standard deviation were used to summarize the data. Bivariable and multivariable binary logistic regression were used to identify the factors associated with proportion of glaucoma. Model fitness was checked by using the Hosmer and Lemeshow goodness of fit test. A p-value of < 0.05 was considered statistically significant. The strength of association was assessed by using an adjusted odds ratio with a 95% confidence interval.
Results
Socio-demographic characteristics of study participants
A total of 934 study participants with an 85.33% response rate participated in the study. The mean age of participants was 55.67 SD ± 13.21 years. More than half of the participants were females 438(55.0%) and majority resided in urban areas 554(69.5%) (Table 1).
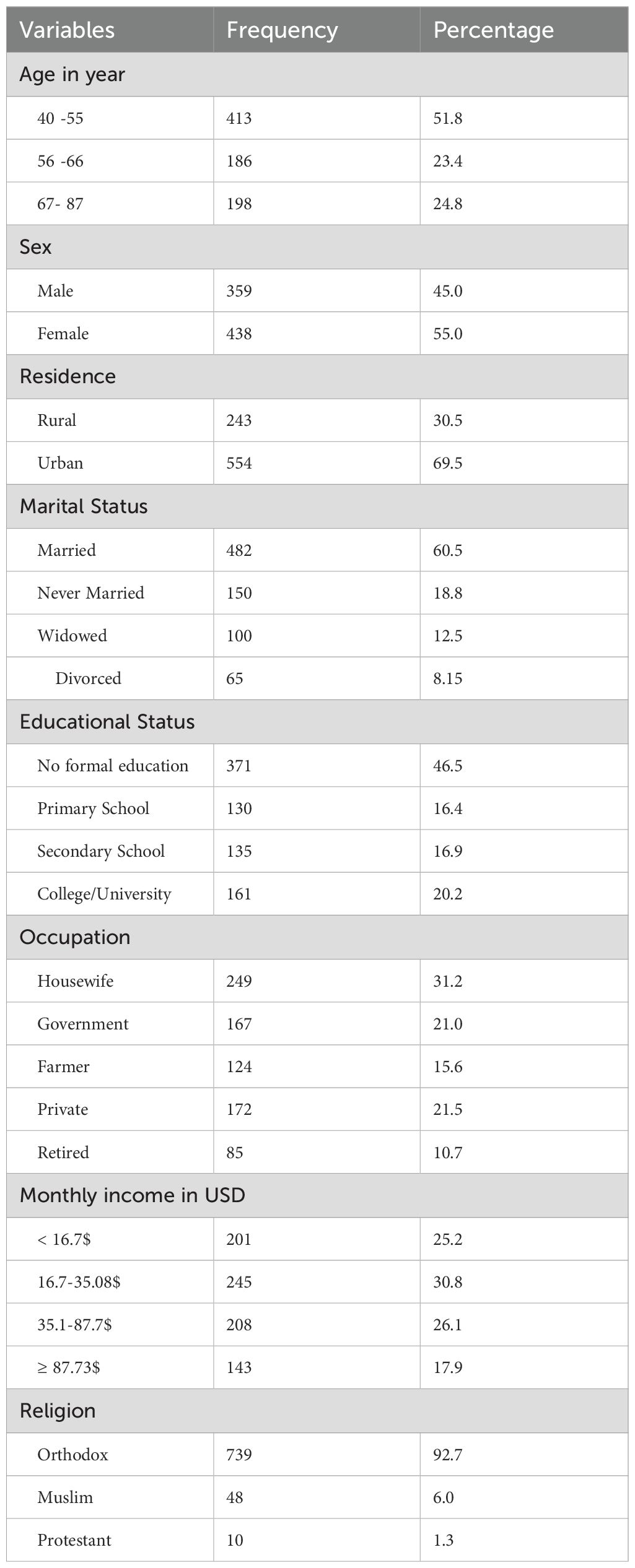
Table 1. Socio-demographic characteristics of the study participants among patient who were attending outpatient department in university of Gondar Comprehensive Specialized Hospital Tertiary Eye Care and Training Center, Northwest Ethiopia, 2021.
Clinical characteristics of study participants
The proportion of glaucoma was 107(13.4%) with Primary Open-Angle Glaucoma (POAG) being the most common type 103(12.9%), zero primary angle closure glaucoma and 4(3.7%) secondary open and closed angle glaucoma. Nearly half (47.6%) of study participants had mild or no visual impairment, and 13.4% of visual impairment were caused glaucoma. Most participants 592(74.3%) had no systemic illness (Table 2).
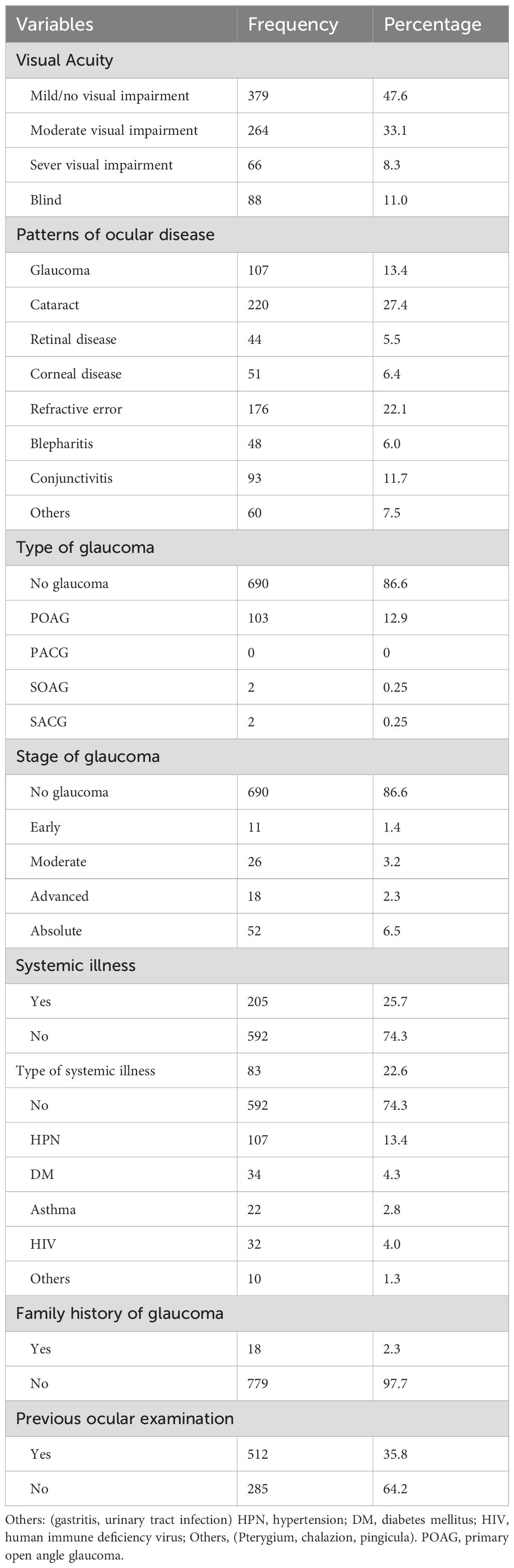
Table 2. Clinical characteristics of the study participants among patients who were attending outpatient department at university of Gondar Comprehensive Specialized Hospital Tertiary Eye Care and Training center, Northwest Ethiopia, 2021.
Factors associated with the presence of glaucoma
The proportion of glaucoma was 107 (13.4%) (95% CI: 10.9 - 15.8%). POAG accounted for 103(12.9%). Participants in the age groups of 56-66 and 67-87 were three times and five times more likely to have glaucoma than those in the age group of 40-55. Participants who finished college or university were 5 times more likely to have glaucoma as compared to those who have not formal education (Table 3).
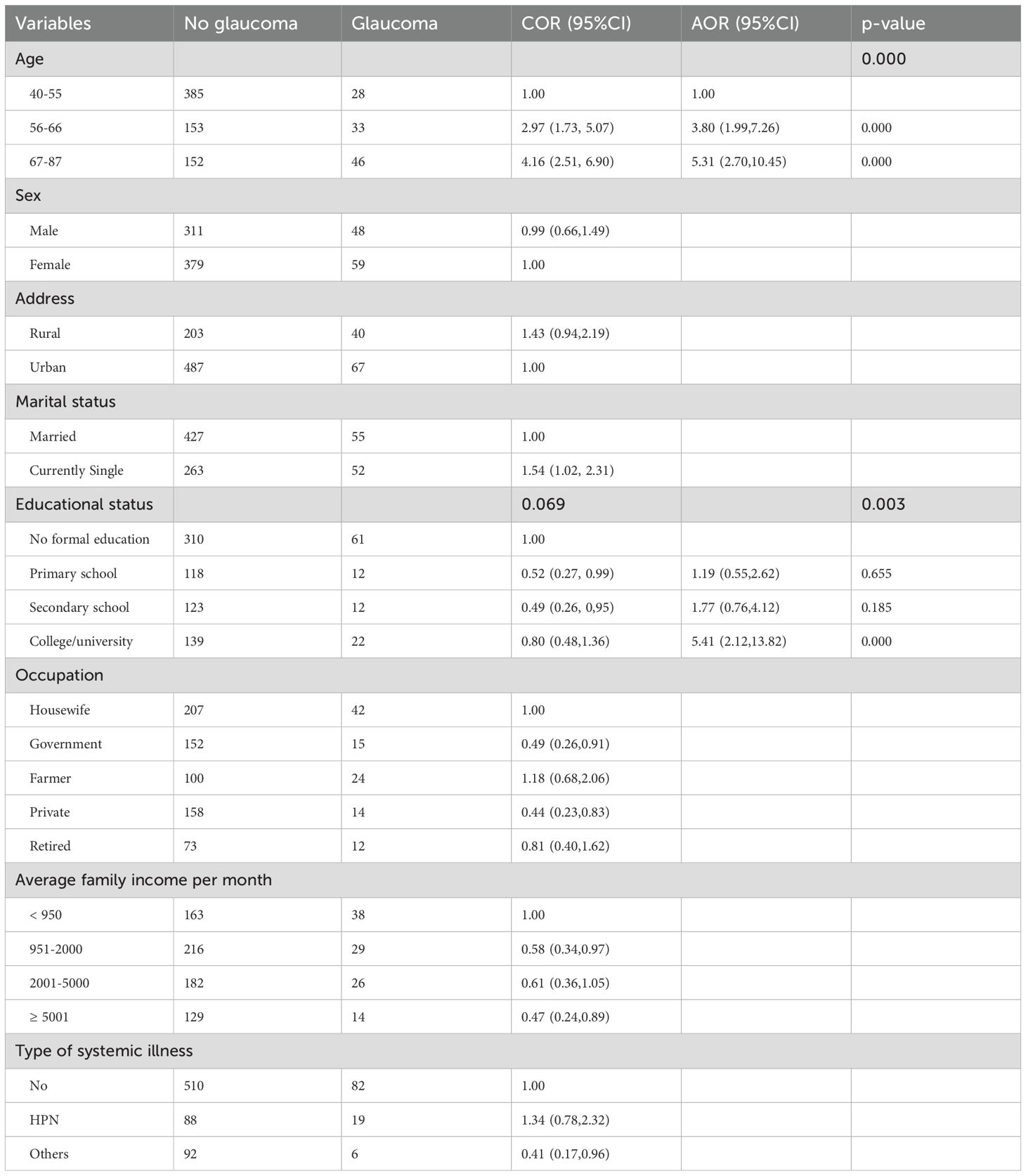
Table 3. factors associated with disease of glaucoma among outpatient department at university of Gondar Comprehensive Specialized Hospital Tertiary Eye Care and Training Center, Northwest Ethiopia, 2021.
Discussion
The study showed that the proportion of glaucoma was 107 (13.4%) (95% CI 10.9- 15.8) which is higher than in other studies conducted in Singapore and Brazil (3.4%) (14, 16), Cameroon (5.5%) (17) Nigeria (7.3%) (18), Kenya (4.3%) (19), in Ghana (8.5%) (20) in Jimma 10.24% (21), and in Gondar 9.79% (13). This difference might be due to the age of respondents and the fact that our institution is a tertiary eye care center. These factors might increase the magnitude of glaucoma cases compared to studies done in Debre Tabor 2.6% (22). This could be attributed to the large sample size of our study.
Regarding the type of glaucoma in this study, Primary- Open Glaucoma (POAG) accounts for 103(12.9%). It accounts 96.3% of the total glaucoma cases, which is almost similar to studies done in Ghana (9.43%) (20), and higher in Brazil (2.4%) (16), Cameroon (4.3%) (17), and Nigeria (6.2%) (18). It is lower than the studies conducted in Jimma 42.55% (21) and in Debre Tabor, 44.50% (22). The variation might be due to high sample size of our study and the fact that it is institution-based, which affects the age distribution of the result.
In consistent with several studies, as age increases, the risk of glaucoma increases (20, 21). Indian studies have shown that individual aged ≥70 years were 4% more likely to have glaucoma (7), while studies in Debre Tabor found that those over 60 year were 3 times more likely to have glaucoma (22). In this study, the age group of 56-66 was three times and 67-87 was five times more likely to have glaucoma than the age group of 40-55. Studies have also indicated that as age increases, intraocular pressure also increases, with thinner central corneal thickness and higher mean ocular perfusion pressure (23). Additionally, morphological studies have shown that outflow ability decreases with age, resulting in increased intraocular pressure due to the accumulation of extracellular materials in the trabecular meshwork (24).
Educational level was found to be significantly associated with the presence of glaucoma. Participants who completed their college or university (AOR=5.41(95% CI: 2.12, 13.82) were five times more likely to have glaucoma than those with no formal education. This could be because, individual with higher education may have more frequent eye examinations due to having awareness about the disease and a higher demand for vision and early detection of visual impairment. In this study 70% of participants who finished college or university had previous ocular examination compared to 59% of those with no formal education. In this study 81% of educated participants had no visual impairment compared to only 25% of illiterate participants. This may lead to an increased rate of glaucoma detection and further investigation may be needed in this area.
Strength and limitation of the study
Strength of the study
This study determined the true prevalence of glaucoma and identifies different the types of glaucoma along with their associated factors.
Limitation of the study
The study not include pediatric population and was limited to hospital settings only, therefore it did no capture data on the community population.
Conclusion
The study found higher proportion of glaucoma compared to other studies, with primary open-angle glaucoma (POAG) being the most common type. Increasing age and higher level of education were significantly associated with the prevalence of glaucoma. Further research is needed to explore the relationship between education level and glaucoma.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics statement
The study was conducted following the Declaration of Helsinki and approved by the institutional review board of the University of Gondar, college of medicine, and health science school of medicine’s ethical review committee. Informed verbal consent was obtained from each respondent. Patient information was obtained with no identifier and confidentiality was maintained. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BY: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Software, Writing – original draft, Writing – review & editing. FA: Data curation, Methodology, Supervision, Writing – original draft, Writing – review & editing. ZB: Methodology, Supervision, Writing – review & editing. EW: Data curation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Financial support for this study was provided by Light for the World for data collection.
Acknowledgments
We would like to thank Light for the world for financial support and the University of Gondar for providing diagnostic materials for the study. Our gratitude also goes to the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Casson RJ, Chidlow G, Wood JP, Crowston JG, Goldberg I. Definition of glaucoma: clinical and experimental concepts. Clin Exp ophthalmology. (2012) 40:341–9. doi: 10.1111/j.1442-9071.2012.02773.x
3. Steinmetz JD, Bourne RR, Briant PS, Flaxman SR, Taylor HR, Jonas JB, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness about VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Global Health. (2021) 9:e144–e60.
4. Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. The global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. (2014) 121:2081–90. doi: 10.1016/j.ophtha.2014.05.013
5. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J ophthalmology. (2006) 90:262–7. doi: 10.1136/bjo.2005.081224
6. Olawoye O, Azuara-Blanco A, Chan VF, Piyasena P, Crealey GE, O’Neill C, et al. A review to populate A proposed cost-effectiveness analysis of glaucoma screening in sub-saharan africa. Ophthalmic Epidemiol. (2021), 1–11.
7. Paul C, Sengupta S, Choudhury S, Banerjee S, Sleath BL. Prevalence of glaucoma in Eastern India: the hooghly river glaucoma study. Indian J ophthalmology. (2016) 64:578. doi: 10.4103/0301-4738.191497
8. Wensor MD, McCarty CA, Stanislavsky YL, Livingston PM, Taylor HR. The prevalence of glaucoma in the Melbourne Visual Impairment Project. Ophthalmology. (1998) 105:733–9. doi: 10.1016/S0161-6420(98)94031-3
9. Bikbov MM, Gilmanshin TR, Zainullin RM, Kazakbaeva GM, Arslangareeva II, Panda-Jonas S, et al. Prevalence and associated factors of glaucoma in the Russian Ural Eye and Medical Study. Sci Rep. (2020) 10:1–14. doi: 10.1038/s41598-020-77344-z
10. Berhane Y, Worku A, Bejiga A, Adamu L, Alemayehu W, Bedri A, et al. Prevalence and causes of blindness and low vision in Ethiopia. Ethiopian J Health Dev. (2007) 21:204–10.
11. Teshome T. Prevalence and causes of blindness in Merhabete, North Shoa, Ethiopia. Ethiopian J Health Dev. (2002) 16:71–6. doi: 10.4314/ejhd.v16i1.9828
12. Ayele FA, Zeraye B, Assefa Y, Legesse K, Azale T, Burton MJ. The impact of glaucoma on quality of life in Ethiopia: a case-control study. BMC ophthalmology. (2017) 17:1–9. doi: 10.1186/s12886-017-0643-8
13. Tegegn MT, Belete GT, Ferede AT, Assaye AK. Proportion and Associated Factors of Low Vision among Adult Patients Attending at University of Gondar Tertiary Eye Care and Training Center, Gondar Town, Ethiopia. J Ophthalmol. (2020) 2020. doi: 10.1155/2020/7042905
14. Shen SY, Wong TY, Foster PJ, Loo J-L, Rosman M, Loon S-C, et al. The prevalence and types of glaucoma in Malay people: the Singapore Malay eye study. Invest Ophthalmol Visual science. (2008) 49:3846–51. doi: 10.1167/iovs.08-1759
15. Dandona L, Dandona R. Revision of visual impairment definitions in the International Statistical Classification of Diseases. BMC Med. (2006) 4:1–7. doi: 10.1186/1741-7015-4-7
16. Sakata K, Sakata LM, Sakata VM, Santini C, Hopker LM, Bernardes R, et al. Prevalence of glaucoma in a South Brazilian population: Projeto Glaucoma. Invest Ophthalmol Visual science. (2007) 48:4974–9. doi: 10.1167/iovs.07-0342
17. Ellong A, Mvogo CE, Bella-Hiag AL, Mouney EN, Ngosso A, Litumbe CN. Prevalence of glaucomas in a Black Cameroonian population. Cahiers d’études recherches francophones/Santé. (2006) 16:83–8.
18. Ashaye A, Ashaolu O, Komolafe O, Ajayi BG, Olawoye O, Olusanya B, et al. Prevalence and types of glaucoma among an indigenous African population in southwestern Nigeria. Invest Ophthalmol Visual science. (2013) 54:7410–6. doi: 10.1167/iovs.13-12698
19. Bastawrous A, Mathenge W, Buchan J, Kyari F, Peto T, Rono H, et al. Glaucoma features in an East African population: a six-year cohort study of older adults in Nakuru, Kenya. J glaucoma. (2018) 27:455. doi: 10.1097/IJG.0000000000000941
20. Ntim-Amponsah C, Amoaku W, Ofosu-Amaah S, Ewusi R, Idirisuriya-Khair R, Nyatepe-Coo E, et al. Prevalence of glaucoma in an African population. Eye. (2004) 18:491–7. doi: 10.1038/sj.eye.6700674
21. Daba KT, Gessesse GW, Sori SB. Proportion of Glaucoma among Voluntary People Coming for Glaucoma Screening Program at Jimma University Department of Ophthalmology, Jimma, Ethiopia. Ethiopian J Health Sci. (2020) 30.
22. Wubet GM, Assefa AA. Glaucoma and its predictors among adult patients attending ophthalmic outpatient department: a hospital-based study, North West Ethiopia. BMC ophthalmology. (2021) 21:1–9. doi: 10.1186/s12886-021-02168-y
23. Coleman AL, Miglior S. Risk factors for glaucoma onset and progression. Surv Ophthalmol. (2008) 53:S3–10. doi: 10.1016/j.survophthal.2008.08.006
Keywords: proportion, glaucoma, outpatient department, Gondar, Ethiopia
Citation: Yekunoamelak BZ, Ayele FA, Bogale ZM and Worku EM (2025) Proportion and associated factors of glaucoma among outpatient department at university of Gondar comprehensive specialized hospital tertiary eye care and training center, northwest Ethiopia, 2021. Front. Ophthalmol. 5:1521263. doi: 10.3389/fopht.2025.1521263
Received: 01 November 2024; Accepted: 14 February 2025;
Published: 05 March 2025.
Edited by:
Yu Xiang George Kong, The Royal Victorian Eye & Ear Hospital, AustraliaReviewed by:
Shruthi Karnam, University of California, Berkeley, United StatesDaniel Laroche, New York Eye and Ear Infirmary, United States
Copyright © 2025 Yekunoamelak, Ayele, Bogale and Worku. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zinachew Mulat Bogale, WmluYW11bGF0MzVAZ21haWwuY29t
 Banchamelak Zeraye Yekunoamelak1
Banchamelak Zeraye Yekunoamelak1 Zinachew Mulat Bogale
Zinachew Mulat Bogale