- 1Department of Ophthalmology, BenQ Medical Center Affiliated to Nanjing Medical University, Nanjing, China
- 2Department of Ophthalmology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
Background: The pathophysiologic mechanisms underlying early-onset myopia remain unclear; in this study, we investigate the pathogenesis by examining the interrelationships between axial length to corneal curvature radius ratio () and choroidal blood flow.
Methods: This cross-sectional study included 202 eyes from myopic children, categorized into 141 eyes with mild myopia, 47 eyes with moderate myopia, and 14 eyes with high myopia. Optical coherence tomography angiography (OCTA) was used to measure choroidal blood flow perfusion within a 6 mm × 6 mm area of the macular region, divided into nine subareas based on ETDRS partitioning: macular fovea, nasal side 1, superior 1, temporal side 1, inferior 1, nasal side 2, superior 2, temporal side 2, and inferior 2. Data on corneal curvature and ocular axial length were collected to calculate the , with equivalent spherical lens power, gender, and age gathered for group comparisons, and the correlation between AL/CR and choroidal blood flow perfusion volume was analyzed.
Results: was significantly negatively correlated with choroidal blood flow perfusion (). Linear regression and mediation analyses indicated that for each unit increase in choroidal blood perfusion volume in nasal region 1, decreased by an average of 0.421 units. This relationship is mediated by several factors, with axial length serving as a key mediator.
Conclusion: correlates with choroidal blood flow perfusion, indicating a link between refractive biological parameters and ocular blood circulation. Myopia is an ischemic eye condition that warrants attention to fundus microcirculation changes in myopic children.
Introduction
In recent years, the rising incidence of myopia has made it a global public health issue (1, 2), particularly among adolescents, children, and individuals who engage in prolonged close-up visual tasks. Epidemiological surveys indicate a yearly increase in childhood myopia worldwide, especially in East Asia, where the prevalence approaches 50% in some regions (3). Myopia not only affects children’s learning and quality of life but also increases the risk of high myopia and associated complications in adulthood, including retinal detachment, glaucoma, and myopic macular degeneration (4). Previous studies have shown that axial length (AL) is a crucial biological parameter affecting the eye’s refractive state (5, 6). With increasing myopia severity, the eye’s axial length gradually increases. However, axial length alone is insufficient to accurately predict refractive state, as it does not account for corneal curvature(CR). During early myopia development, corneal curvature may increase to compensate for axial elongation. When axial elongation exceeds a certain threshold, corneal flattening can no longer compensate for refractive changes, potentially leading to myopia. Grosvenor first identified a positive correlation between AL and CR, noting that increases in AL are accompanied by proportional increases in CR (7). As AL gradually increases, parallel light converges in front of the retina, with surrounding hyperopic defocus prompting a gradual transition to a myopic refractive state. Therefore, the ratio can, to some extent, indicate the refractive status in myopic patients. A recent domestic study involving adolescents and children aged 4–18 years indicated that corneal compensation reaches its upper limit when (8, 9). This ratio is typically below 3 in individuals without myopia, whereas most myopic individuals have an. exceeding 3. Higher ratios correlate with more severe myopia. Thus, the ratio can serve as a rapid assessment tool for myopia in adolescents and children, in conjunction with non-dilated pupils optometry and visual acuity testing, as well as a screening method for myopia progression.
Recent studies indicate that changes in choroidal thickness and blood flow are closely related to myopia development (10). As myopic diopter increases and the eye axis elongates, choroidal thickness gradually decreases. Studies suggest that changes in choroidal thickness are not only key indicators of myopia development but may also play a role in regulating eyeball growth and myopia progression. Increased choroidal thickness may help slow myopia progression (11), whereas choroidal thinning may be linked to its rapid progression. Choroidal thinning may result from mechanical stretching due to axial elongation, leading to reduced choroidal blood flow and subsequent retinal ischemia and hypoxia. Additionally, reduced choroidal blood flow may lead to scleral ischemia and hypoxia (12, 13), affecting eyeball growth and myopia development. The application of optical coherence tomography angiography (OCTA) allows for high-resolution, noninvasive evaluation of the retinal and choroidal microvascular structures and blood flow (14). With OCTA, researchers have observed a decrease in the vascular density of the retina and choroid and a decrease in choroidal blood flow in patients with high myopia (15). These changes may relate to myopia development and pathological ocular changes.
The ratio is a key indicator for assessing the eye’s refractive state. In myopic children, changes in often closely correlate with increasing myopia. Choroidal blood flow and thickness are critical parameters reflecting fundus microcirculation. In myopic children, abnormal choroidal blood flow and thickness changes may be closely linked to myopia onset and progression. The ratio, choroidal thickness, and choroidal blood flow are significant topics of research within the field of ophthalmology. However, there is a scarcity of studies examining the correlation between AL/CR and choroidal thickness and blood flow in myopic children. Investigating the distribution characteristics of ocular biological parameters—such as axial length (AL), AL/CR, choroidal thickness, and choroidal blood flow—in myopic children and understanding their relationship with myopia is critical. In this paper, the correlation between AL/CR and choroidal blood flow in children with myopia was evaluated by using a novel statistical analysis method, which provides a new perspective for understanding the pathophysiological mechanism of myopia, aiming to reveal how these parameters affect the occurrence of myopia in children, and whether they can also be an important clinical indicator for evaluating myopia status and myopia prevention and control in children.
Materials and methods
Study design and subjects
The research subjects were myopic children who visited the optometry clinic of Nanjing Mingji Hospital affiliated with Nanjing Medical University from December 2022 to June 2024. There were a total of 202 subjects, and data from the right eye was selected for all of them, with a total of 202 eyes included in the study. Each enrolled subject obtained written informed consent to participate.
Inclusion criteria: Participants were aged between 6 and 12, in good health without systemic or ocular diseases, underwent mydriasis with tropicamide,, in both eyes and had normal eye movements.
Exclusion criteria: 1. Systemic underlying diseases; 2. Organic eye lesions (e.g., keratitis, conjunctivitis, trichiasis); 3. Orthokeratology lens wear; 4. Opaque refractive media affecting image acquisition (e.g., congenital cataracts, severe vitreous opacity); 5. Strabismus, amblyopia, or poor fixation ability; 6. Patients undergoing retinal red light therapy.
Data were categorized into three groups based on spherical equivalent (SE) after mydriatic refraction with tropicamide: mild, moderate, and high myopia. The groups were defined as follows: Mild myopia:; Moderate myopia: ; High myopia: .
Measurement of ocular biological parameters
Visual acuity, intraocular pressure, comprehensive optometry, and fundus photography were performed by an experienced optometrist. A slit lamp examination was conducted by a senior physician to exclude conditions that might affect the results of this study, such as eyelid trichiasis, conjunctivitis, keratitis, keratoconus, and congenital cataracts.
The ocular optical measurement instrument (Anshikang ASK-Swan600, China) employs partial coherence interferometry (PCI) to measure the axial length of the eye and corneal curvature.
The axial length is typically measured from the center of the cornea to the distance between the optic nerve and the foveal center of the retina, with the unit of measurement being millimeters (mm).
Corneal curvature refers to the degree of curvature of the cornea, describing its shape. denotes the corneal curvature value along the line where the cornea is relatively flat, while indicates the corneal curvature value in the direction of greater convexity, representing flat K and steep K, respectively. The unit of measurement for corneal curvature is diopter (D).
To avoid the influence of mydriasis on measurement results, the examinee is instructed to undergo a biometry examination prior to the mydriasis examination. Each examinee undergoes five measurements, and the average value is recorded. All examinations are conducted by the same experienced examiner.
AL/CR is the ratio of the axial length of the eye to the average radius of corneal curvature. The calculation method is as follows:
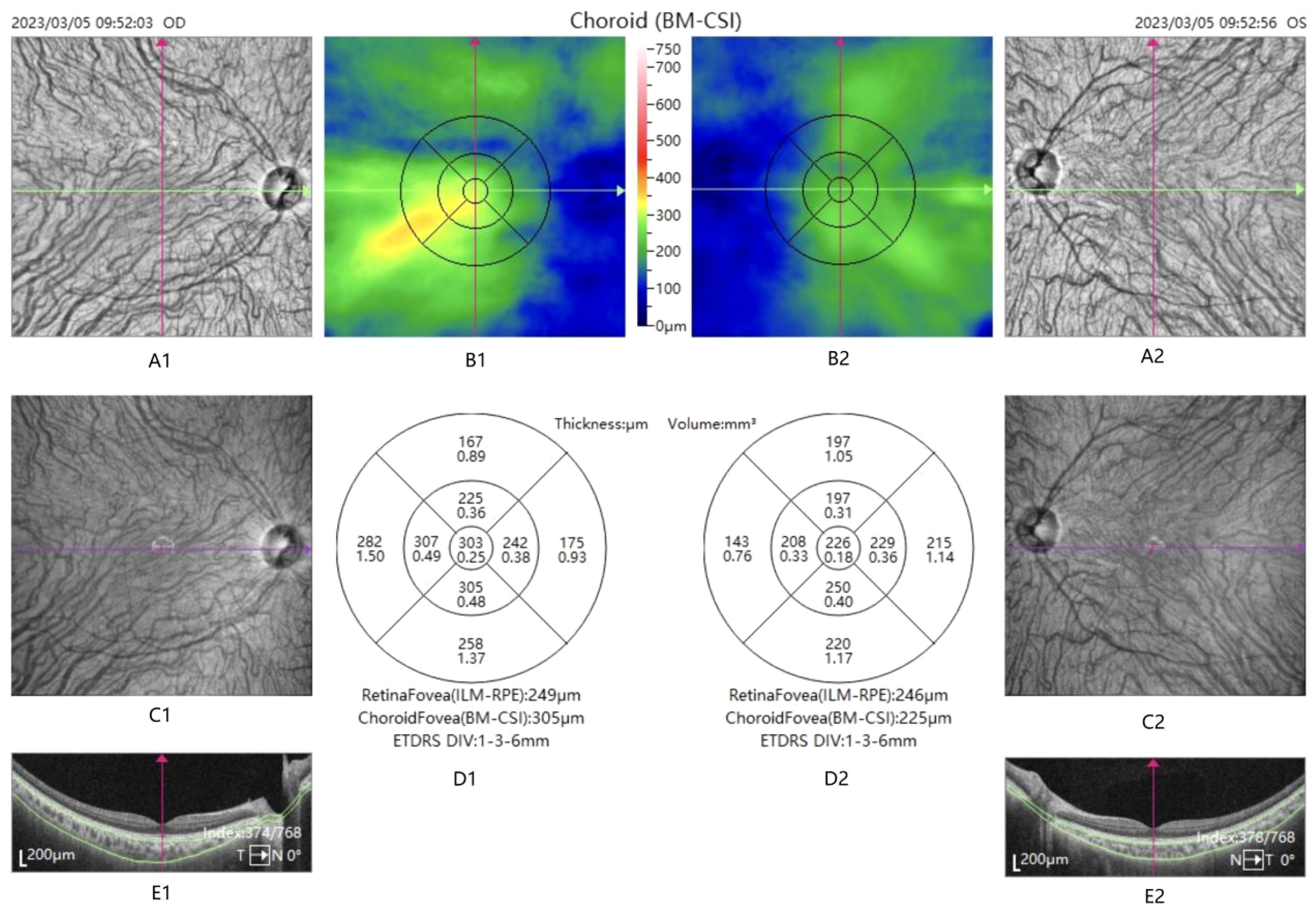
OCTA (TowardPi, China) measures choroidal blood flow. Optical Optical Coherence Tomography Angiography (OCTA) is a novel ophthalmic imaging technique that directly observes the blood flow of the retina, choroid, and optic nerve under non-invasive conditions. Utilizing long wavelengths and high-speed scanning, TowardPi OCTA provides an in-depth analysis of the retinal and choroidal microvascular systems, as well as quantitative assessments of blood flow. OCTA was employed to image choroidal blood flow in the macula of all patients. The scan area was divided according to the ETDRS zone, with three concentric circles having diameters of 1 mm, 3 mm, and 6 mm drawn around the fovea, which were defined as the inner ring, the outer ring, and the fovea. Each ring encompasses four areas—upper, lower, temporal, and nasal—and is divided into a total of nine subregions. These nine regions are designated in an anticlockwise direction from the inside out: macular fovea, nasal side 1, superior 1, temporal side 1, inferior 1, nasal side 2, superior 2, temporal side 2, and inferior 2. (See Figure 1) The unit of measurement for choroidal blood flow perfusion volume is cubic millimeters (mm³).
A1, A2, C1, C2: enface structure chart. B1,B2: choroidal thickness map. D1,D2: divided into 9 subareas based on ETDRS partitioning: macular fovea, nasal side 1, superior 1, temporal side 1, inferior 1, nasal side 2, superior 2, temporal side 2, and inferior 2. The upper data is the choroidal thickness and the lower data is the choroidal blood flow perfusion volume. E1, E2: OCT Structure chart.
To ensure that mydriasis did not affect the measurement results, the doctor conducted the OCTA examination prior to inducing mydriasis. All examinations were performed by an experienced specialist examiner. The final results were comprehensively evaluated by an experienced specialist physician, and images with blurring or positional shifts during scanning were excluded from consideration.
Statistical analysis
All the data of each group were statistically analyzed using SPSS 26.0 software, and the measurements were expressed as . Comparisons between groups were conducted using the ANOVA test, and Pearson correlation analyses were performed on the and choroidal blood flow perfusion volume across different divisions. Based on the results of the correlation analysis, linear regression analysis and intermediary effect analysis were performed on the and choroidal blood perfusion volume in zone 1 of the nasal side. A was considered statistically significant.
Results
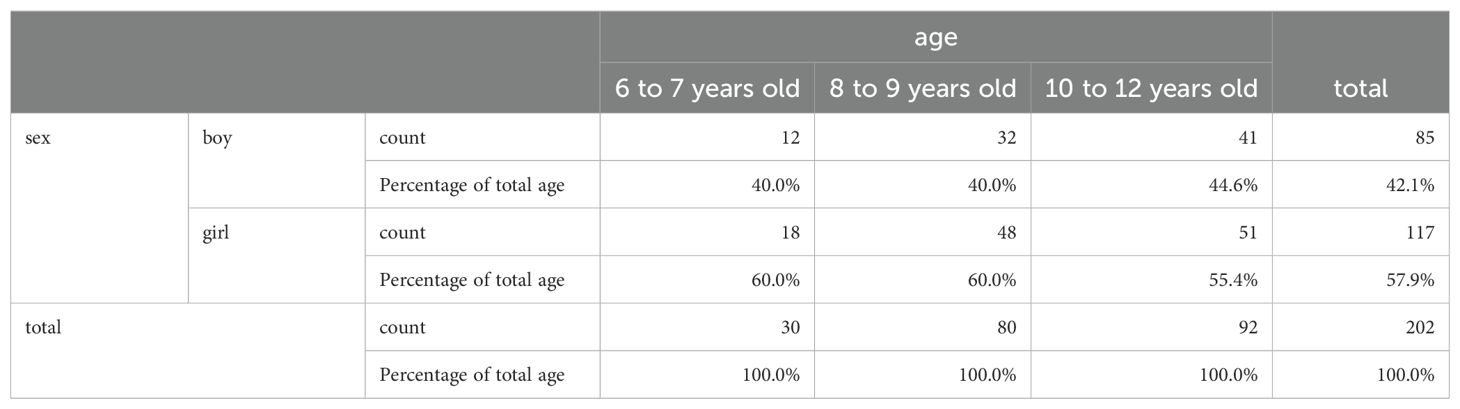
A total of 202 myopic children aged 6 to 12 years were included in this study, with only data from the right eye selected for enrollment, resulting in a total of 202 eyes. Among the participants, 85 were boys (42.6% of the total) and 117 were girls (57.4% of the total). The age distribution was as follows: 30 children aged 6 to 7 years, comprising 12 boys and 18 girls; 80 children aged 8 to 9 years, including 32 boys and 48 girls; and 117 children aged 10 to 12 years, consisting of 41 boys and 76 girls. These results indicate that the prevalence of myopia is higher among girls than boys in all age groups. (See Table 1).
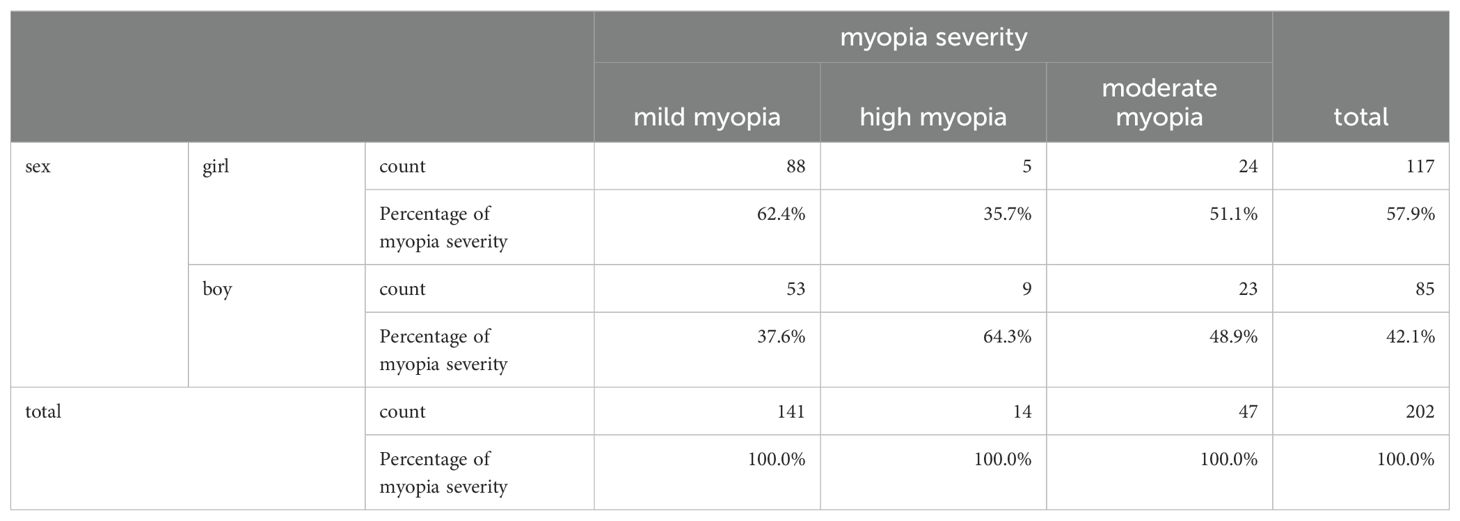
Myopic children were categorized into three groups according to spherical equivalent (SE): the mild myopia group consisted of 141 children, accounting for 69.8% of the total, with 53 boys and 88 girls. The moderate myopia group comprised 47 children, representing 23.2% of the total, including 23 boys and 24 girls. The high myopia group included 14 children, accounting for 6.9% of the total, comprising 9 boys and 5 girls. The majority of children with myopia have mild myopia; however, a certain proportion of children exhibit high myopia. In the mild and moderate myopia groups, the incidence is higher among girls, while in the high myopia group, the incidence is higher among boys. (See Table 2).
The mean values of axial lengths for the mild myopia group, moderate myopia group, and high myopia group were 24.19 ± 0.34 mm, 25.21 ± 0.67 mm, and 26.45 ± 0.78 mm, respectively, with statistically significant differences between the groups (P < 0.001).
The mean values of in the mild myopia, moderate myopia, and high myopia groups were 3.09 ± 0.08, 3.26 ± 0.07, and 3.33 ± 0.06, respectively, with statistically significant differences between the groups (). Both axial length and exhibited a pronounced upward trend with the increasing severity of myopia.
The mean values of choroidal blood flow perfusion volume in the macular fovea for the mild myopia, moderate myopia, and high myopia groups were 0.208 ± 0.047, 0.187 ± 0.047, and 0.156 ± 0.265, respectively, with statistically significant differences between the groups (). As the degree of myopia increases, the choroidal blood flow volume gradually decreases. (See Tables 3, 4).
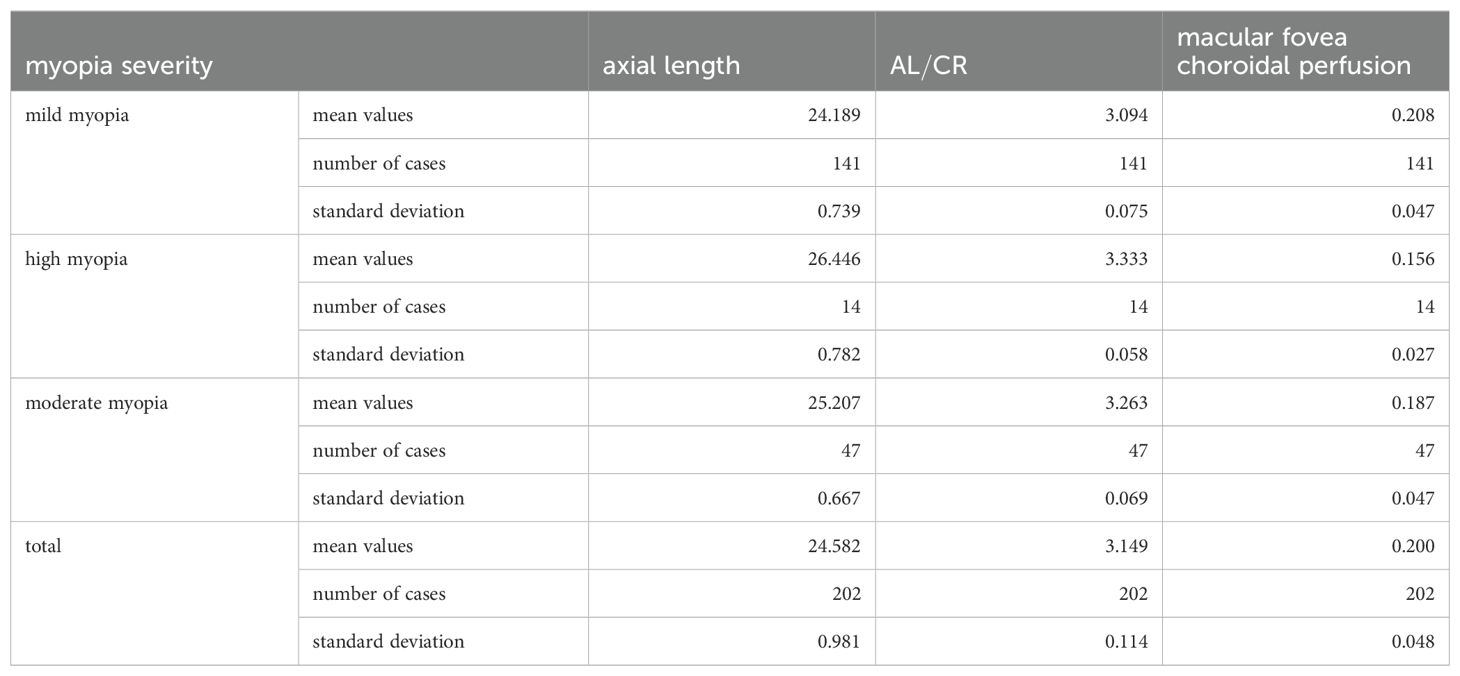
Table 3. Mean values of axial length, , and macular fovea choroidal perfusion after grouping by myopia severity.
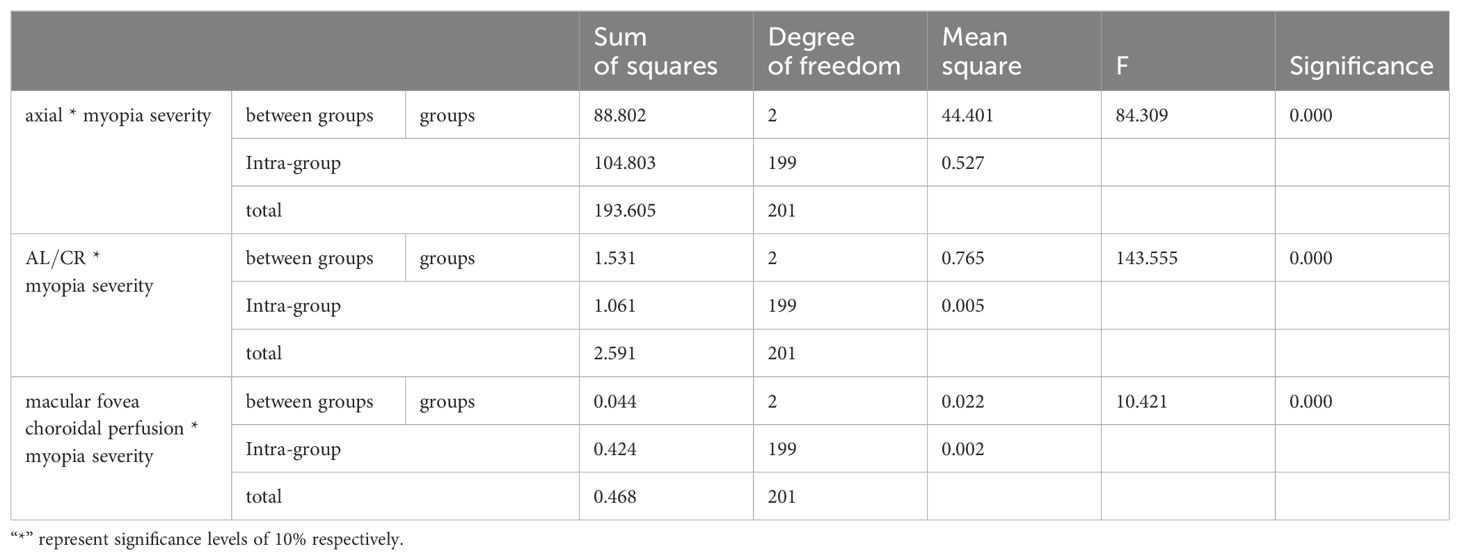
Table 4. ANOVA results of the mean axial, , and macular fovea choroidal perfusion after grouping by myopia severity.
The correlation test results between and macular fovea choroidal perfusion (r=-0.315, P<0.001), nasal 1 choroidal perfusion (r=-0.323, P<0.001), temporal 1 choroidal perfusion (r=-0.314, P<0.001), superior 1 choroidal perfusion (r=-0.264, P<0.001), inferior 1 choroidal perfusion (r=-0.162, P<0.001), nasal 2 choroidal perfusion (r=-0.302, P<0.001), temporal 2 choroidal perfusion (r=-0.303, P<0.001), superior 2 choroidal perfusion (r=-0.195, P< 0.001), and inferior 2 choroidal perfusion (r=-0.178, P<0.001).
According to the results of the Pearson correlation analysis, we can find a negative correlation between the and the choroidal perfusion volume, and the largest correlation coefficient and the strongest correlation with the choroidal perfusion volume of the nasal side 1 region.
Based on the results of Pearson correlation analysis, a linear regression model was established by choosing choroidal blood perfusion in region 1 of the nasal side as the predictor variable and as the dependent variable. The adjusted R-squared value was 0.100, , and the model as a whole was statistically significant. The regression coefficient value of and choroidal blood perfusion volume in region 1 of the nasal side was -0.421 (), indicating that when choroidal blood perfusion volume increases by 1 unit, the will decrease by an average of 0.421 units. (See Figure 2).
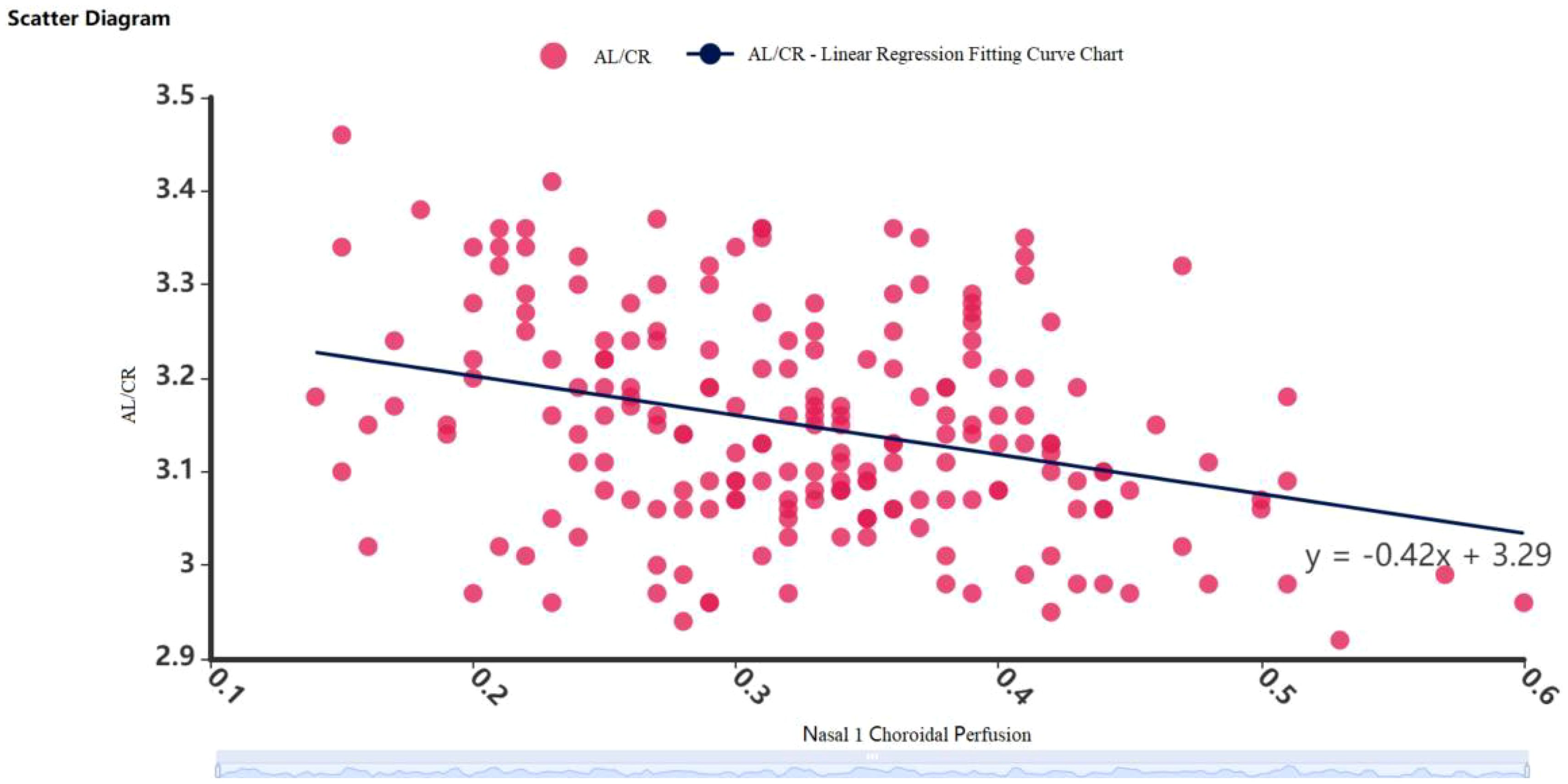
Figure 2. Scatter diagram of linear regression between and choroidal blood flow perfusion volume in the nasal side 1 region.
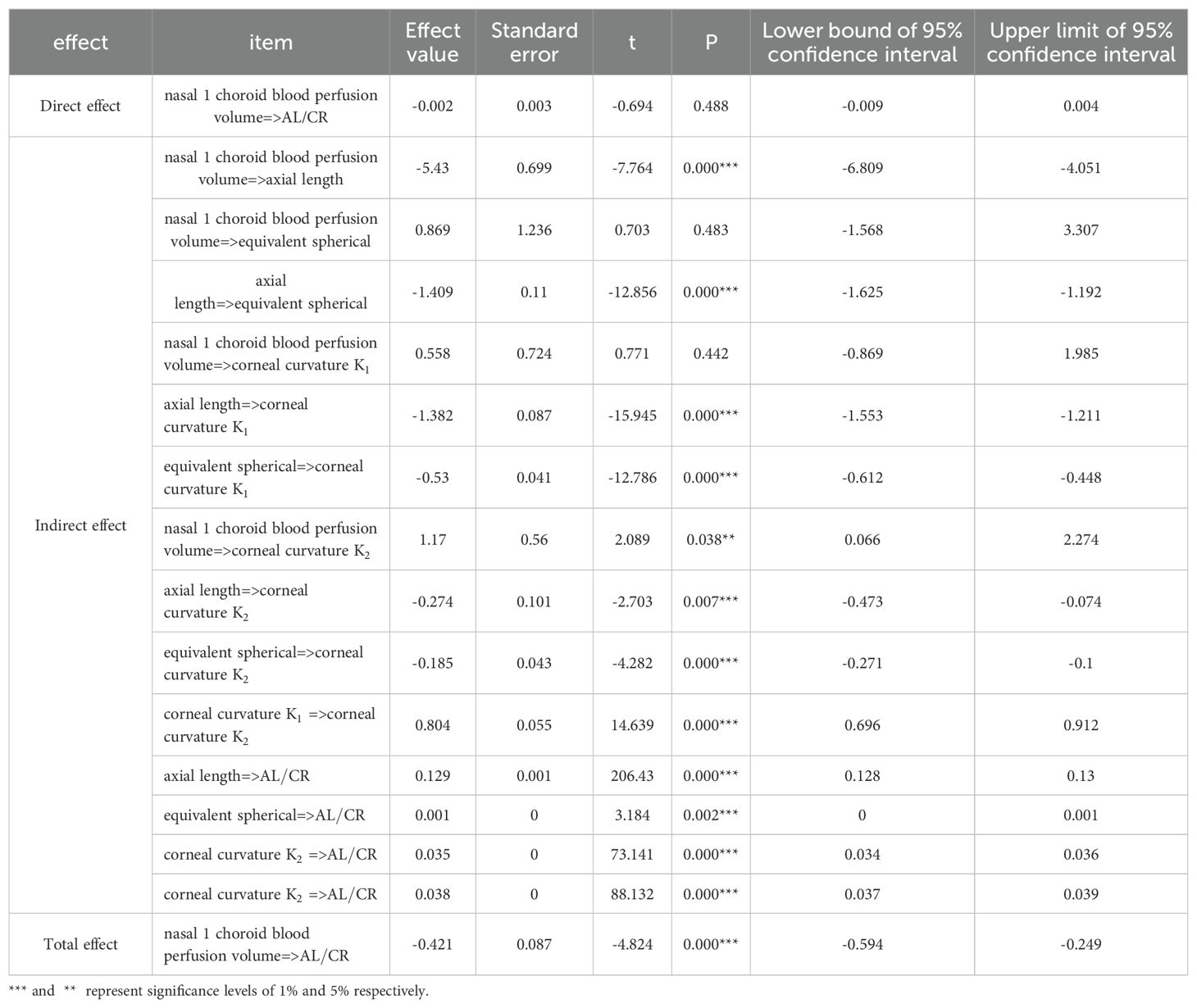
To further investigate the relationship between choroidal blood perfusion volume, , axial length, corneal curvature, and equivalent spherical lens power, we designated as the dependent variable (Y), nasal 1 choroidal blood perfusion volume as the independent variable (X), and equivalent spherical lens power, axial length, corneal curvature , and corneal curvature as mediating variables to construct a mediation model. (See Table 5).
In the chain mediation analysis, this study systematically explored the pathway of the nasal side 1 blood flow volume on the AL/CR, the sequence of mediating variables (axial length, refractive power, corneal curvature K1, and corneal curvature K2). First, the direct effect analysis showed that the nasal side 1 blood flow volume had no significant direct effect on the axial ratio (effect size=-0.002, P=0.488), indicating that there was no strong direct correlation between the two. This finding emphasizes the importance of mediating variables in explaining the relationship between the two.
Then, an indirect effect analysis revealed the mediating pathway. Nasal 1 blood flow volume had a significant indirect negative impact on the AL/CR through the mediating effect of the eye axis (effect size = -5.43, P < 0.001), indicating that the eye axis is the mediator through which nasal 1 blood flow volume affects the axis ratio. At the same time, the negative impact of nasal 1 blood flow volume on the eye axis was also significant (effect size = -5.43, P < 0.001), further supporting the validity of this pathway.
However, the indirect effect of nasal side 1 blood flow volume on the AL/CR through refractive index (equivalent spherical power) was not significant (effect size = 0.869, P = 0.483), although refractive index was significantly influenced by eye axis (effect size = -1.409, P < 0.001). This suggests that although there is a strong correlation between eye axis and refractive index, refractive index does not play a significant mediating role in the pathway from nasal side 1 blood flow volume to AL/CR.
Additionally, the corneal curvature K1 and K2 also played an important role in the chain mediation effect. The direct effect of nasal side 1 blood flow volume on corneal curvature K1 was not significant (effect size=0.55, P=0.442), but it had a significant positive effect on corneal curvature K2 (effect size=1.17, P=0.038). There was a significant strong positive correlation between corneal curvature K1 and K2 (effect size=0.804, P<0.001), and both were significantly positively correlated with the AL/CR (effect size=0.035 and 0.038, P<001). These findings suggest that corneal curvature is not only an important component of the axial structure of the eye, but also an important mediator of the indirect effect of nasal side 1 blood flow volume on the AL/CR.
Finally, the total effect analysis showed that the total effect of nasal side 1 blood flow volume on the ratio of axial length to curvature was a significant negative effect (effect size=-0.421, P<0.001). This result was the result of the combined action of multiple mediating variables, with the axial length and corneal curvature playing a crucial mediating role.
Discussion
The present study reveals the complex relationship among these parameters through detailed measurements and analyses of sex, age, , and choroidal blood flow perfusion in myopic children aged 6 to 12 years. Although the myopic population predominantly exhibits mild myopia, a notable percentage of high myopia is now observed. Furthermore, the prevalence of myopia is relatively higher in girls for moderate and mild myopia, while it is significantly greater in boys for high myopia. The study indicates that is more pronounced in the group of myopic children, showing a corresponding increase with the progression of myopia. This finding suggests that is not merely a static assessment criterion; rather, it represents an evolving process that accurately describes the trajectory of myopia. The changes in choroidal blood perfusion volume also provide valuable reference information. We found that as gradually rises, the choroidal perfusion volume exhibits a decreasing trend. The early stage of myopia is characterized not only by changes in the axial length of the eye but also by alterations in the overall configuration of the eye and the role of depth regulation (16). This phenomenon can be explained biologically; the elongation of the eye’s axial length may cause the choroid to become thinner (17, 18) and more susceptible to stretching, thereby reducing the vascular mobility space and compromising blood transport pathways. Additionally, the contraction of the ciliary muscle during near work may transmit tension to the posterior pole of the eye, contributing to the elongation of the eye axis (19). In this process, the ciliary muscle may become hypertrophic (20), competing for a portion of choroidal blood perfusion, which exacerbates choroidal ischemia and hypoxia, leading to scleral hypoxic remodeling (12)and further elongation of the eye axis.
Our study found the strongest negative correlation between AL/CR and choroidal blood perfusion volume in nasal zone 1, corroborating the findings reported by Luo et al. In their investigation, Luo et al. observed that choroidal blood vessel distribution diminished progressively with increasing degrees of myopia, with the most pronounced alterations occurring in the nasal region of the macula, as well as the temporal and inferior areas surrounding the optic disc (21). Our results provide further validation of their conclusions. The mechanisms underlying these observations may be related to the compromised integrity of the papillon-macular bundle. Jonas et al. demonstrated that as axial length increases, both the parapapillary gamma zone (the peripapillary sclera devoid of overlying choroid, Bruch’s membrane, and deep retinal layers) and the delta zone (characterized by the absence of blood vessels with diameters exceeding 0.5 mm within the gamma zone) expand, accompanied by a gradual reduction in choroidal perfusion (22). Consequently, the papillon-macular tract may play a pivotal role in the onset and progression of myopia.
This study also further elucidated the significant specificity of the AL/CR ratio in myopic children within a clinical setting. With the progression of myopia, the AL/CR ratio exhibited a marked upward trend. This phenomenon suggests that the AL/CR ratio can serve not only as a critical reference index for the diagnosis of myopia but also as a dynamic indicator of myopia progression, independent of traditional optometric methods to some extent. Thus, this research provides a novel scientific foundation for the early diagnosis and prevention of myopia. Furthermore, the study highlighted the significant correlation between choroidal blood flow and the degree of myopia. As myopia worsens, there is a noticeable decreasing in choroidal blood flow. This relationship underscores the interaction between refractive biological parameters of the eye and ocular hemodynamics. The findings are further supported by the observation that an increase in the AL/CR ratio coincided with reduction in choroidal blood flow, reinforcing the interconnectedness of these factors in the context of myopia progression.
The study focused on children aged 6 to 12 years, a critical period for the development of myopia. During this time, mild myopia is more prevalent, whereas moderate and high myopia may require a longer duration to develop or may be influenced by specific genetic factors. In the sample, the proportion of children with moderate and high myopia was small, which means the findings may primarily reflect the characteristics of those with mild myopia. As a result, the study may not fully represent the entire population of myopic children, potentially impacting the generalizability and external validity of the results.
The data collection and analysis in this study were primarily based on a single-center cross-sectional study design. Although a correlation was identified between and choroidal blood flow, the exact causality of this relationship remains uncertain. Future studies should consider expanding the sample size and enhancing collaborative efforts among multiple research centers, adopting a longitudinal research strategy to track changes in ocular parameters over various time periods. This approach will help ensure that the research results are more broadly applicable and trustworthy. Furthermore, due to the technical limitations of the examination equipment, it was not possible to determine whether some of the blood with reduced choroidal perfusion was redistributed into the ciliary muscle. It is hoped that more advanced measurement tools and optimized experimental procedures will become available in the future to observe and analyze the pathophysiological processes associated with reduced choroidal perfusion.
The present study focused on the relationship between and choroidal blood flow in myopic children aged 6 to 12 years. As myopia progressed, exhibited a significant upward trend, while choroidal blood perfusion gradually decreased. This trend suggests a close relationship between the refractive biological parameters of the eye and fundus blood flow, indicating that decreased choroidal perfusion in the fundus is evident even in the early stages of myopia, which can be classified as an ischemic fundus disease. By integrating multiple factors such as the refractive biological parameters of the eye and the condition of fundus blood flow, we can gain a more comprehensive understanding of the biological mechanisms underlying childhood myopia and provide robust scientific support for the development of more effective myopia prevention and control strategies.
This study highlights the significant influence of biological parameters, such as AL/CR and choroidal blood flow, on the development of myopia. It involves a detailed analysis of these parameters in myopic children aged 6 to 12. In clinical practice, AL/CR can serve as a valuable screening indicator when combined with measurements of eye axis length and corneal curvature, enabling healthcare professionals to more accurately evaluate the risk of myopia in children. Additionally, by regularly monitoring the structural and functional status of the choroid, clinicians may be able to detect and address potential microcirculation issues in myopic patients in a timely manner.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board of BenQ Medical Center Affiliated to Nanjing Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the minor(s)’ legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
YY: Methodology, Writing – original draft, Writing – review & editing. ZH: Investigation, Writing – original draft, Writing – review & editing. YS: Methodology, Project administration, Writing – original draft, Writing – review & editing. SY: Conceptualization, Methodology, Project administration, Writing – original draft, Writing – review & editing. NS: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to thank all those patients with mild-moderate and high myopia who were willing to undergo the comprehensive optical examinations and consecutive follow-ups, and those who helped to perform the examination and are not listed as co-authors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yang J, Wu S, Zhang C, Yu W, Dai R, Chen Y. Global trends and frontiers of research on pathologic myopia since the millennium: A bibliometric analysis. Front Public Health. (2022) 10:1047787. doi: 10.3389/fpubh.2022.1047787
2. Cui Q, Xu YS, Gu JS, Yang S, Hua XH, Hua DH. Geographic environment-related research advances on children's myopia: intraocular and environmental exposure factors and analytical methods. Zhonghua Yan Ke Za Zhi. (2024) 60(4):378–83. doi: 10.3760/cma.j.cn112142-20230802-00020
3. Liang J, Pu Y, Chen J, Liu M, Ouyang B, Jin Z, et al. Global prevalence, trend and projection of myopia in children and adolescents from 1990 to 2050: a comprehensive systematic review and meta-analysis. Br J Ophthalmol. (2024) 24:bjo-2024-325427. doi: 10.1136/bjo-2024-325427
4. Haarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW. The complications of myopia: A review and meta-analysis. Invest Ophthalmol Vis Sci. (2020) 61:49. doi: 10.1167/iovs.61.4.49
5. Du R, Xie S, Igarashi-Yokoi T, Watanabe T, Uramoto K, Takahashi H, et al. Continued increase of axial length and its risk factors in adults with high myopia. JAMA Ophthalmol. (2021) 139:1096–103. doi: 10.1001/jamaophthalmol.2021.3303
6. Chamberlain P, Lazon de la Jara P, Arumugam B, Bullimore MA. Axial length targets for myopia control. Ophthalmic Physiol Opt. (2021) 41:523–31. doi: 10.1111/opo.12812
7. Grosvenor T. High axial length/corneal radius ratio as a risk factor in the development of myopia. Am J Optom Physiol Opt. (1988) 65:689–96. doi: 10.1097/00006324-198809000-00001
8. He X, Sankaridurg P, Naduvilath T, Wang J, Xiong S, Weng R, et al. Normative data and percentile curves for axial length and axial length/corneal curvature in Chinese children and adolescents aged 4-18 years. Br J Ophthalmol. (2023) 107:167–75. doi: 10.1136/bjophthalmol-2021-319431
9. Matsumura S, Dannoue K, Kawakami M, Uemura K, Kameyama A, Takei A, et al. Prevalence of myopia and its associated factors among Japanese preschool children. Front Public Health. (2022) 10:901480. doi: 10.3389/fpubh.2022.901480
10. Liu Y, Wang L, Xu Y, Pang Z, Mu G. The influence of the choroid on the onset and development of myopia: from perspectives of choroidal thickness and blood flow. Acta Ophthalmol. (2021) 99:730–8. doi: 10.1111/aos.14773
11. Baksh J, Lee D, Mori K, Zhang Y, Torii H, Jeong H, et al. Myopia is an ischemic eye condition: A review from the perspective of choroidal blood flow. J Clin Med. (2024) 13(10):2777. doi: 10.3390/jcm13102777
12. Zhou X, Zhang S, Yang F, Yang Y, Huang Q, Huang C, et al. Decreased choroidal blood perfusion induces myopia in Guinea pigs. Invest Ophthalmol Vis Sci. (2021) 62:30. doi: 10.1167/iovs.62.15.30
13. Zhou X, Zhang S, Zhang G, Chen Y, Lei Y, Xiang J, et al. Increased choroidal blood perfusion can inhibit form deprivation myopia in Guinea pigs. Invest Ophthalmol Vis Sci. (2020) 61:25. doi: 10.1167/iovs.61.13.25
14. Spaide RF, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G. Optical coherence tomography angiography. Prog Retin Eye Res. (2018) 64:1–55. doi: 10.1016/j.preteyeres.2017.11.003
15. Xu Y, Yang W, Niu L, Wang X, Zhou X, Li M. Myopic vascular changes revealed by optical tomography angiography and their association with myopic fundus manifestations. Ophthalmic Res. (2023) 66:1266–77. doi: 10.1159/000531877
16. Ablordeppey RK, Lin C, Benavente-Perez A. The age-related pattern of inner retinal thickening is affected by myopia development and progression. Sci Rep. (2022) 12:22190. doi: 10.1038/s41598-022-26598-w
17. Ulaganathan S, Read SA, Collins MJ, Vincent SJ. Daily axial length and choroidal thickness variations in young adults: Associations with light exposure and longitudinal axial length and choroid changes. Exp Eye Res. (2019) 189:107850. doi: 10.1016/j.exer.2019.107850
18. Xuan M, Wang D, Xiao O, Guo X, Zhang J, Yin Q, et al. Choroidal vascularity and axial length elongation in highly myopic children: A 2-year longitudinal investigation. Invest Ophthalmol Vis Sci. (2024) 65:7. doi: 10.1167/iovs.65.10.7
19. Meng ZY, Yang L, Zhou P. Ciliary muscles contraction leads to axial length extension–The possible initiating factor for myopia. PloS One. (2024) 19:e0301844. doi: 10.1371/journal.pone.0301844
20. Kaphle D, Schmid KL, Davies LN, Suheimat M, Atchison DA. Ciliary muscle dimension changes with accommodation vary in myopia and emmetropia. Invest Ophthalmol Vis Sci. (2022) 63:24. doi: 10.1167/iovs.63.6.24
21. Luo H, Sun J, Chen L, Ke D, Zhong Z, Cheng X, et al. Compartmental analysis of three-dimensional choroidal vascularity and thickness of myopic eyes in young adults using SS-OCTA. Front Physiol. (2022) 13:916323. doi: 10.3389/fphys.2022.916323
Keywords: OCTA, axial length to corneal curvature radius ratio (AL/CR), choroidal blood flow, myopia, children, axial length (AL)
Citation: Ye Y, Hu Z, Su N, Shen Y and Yuan S (2025) Axial length to corneal curvature radius ratio is negatively correlated with choroidal blood flow in myopic children. Front. Ophthalmol. 4:1540410. doi: 10.3389/fopht.2024.1540410
Received: 05 December 2024; Accepted: 11 December 2024;
Published: 06 January 2025.
Edited by:
Dong Ho Park, Kyungpook National University Hospital, Republic of KoreaReviewed by:
Yong Koo Kang, Kyungpook National University, Republic of KoreaJae Rock Do, Kyungpook National University, Republic of Korea
Yu Su, Renmin Hospital of Wuhan University, China
Copyright © 2025 Ye, Hu, Su, Shen and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yeyu Shen, MTY2NjE5NTRAcXEuY29t; Songtao Yuan, c29uZ3Rhb3l1YW5AbmptdS5lZHUuY24=
†These authors have contributed equally to this work
 Yurong Ye
Yurong Ye Zizhong Hu
Zizhong Hu Na Su
Na Su Yeyu Shen
Yeyu Shen Songtao Yuan2*
Songtao Yuan2*