- 1Ophthalmology Clinic, University Hospital Ostrava, Ostrava, Czechia
- 2Faculty of Medicine and University Hospital Cologne, Department of Ophthalmology, University of Cologne, Cologne, Germany
- 3Faculty of Medicine, Department of Craniofacial Surgery, University of Ostrava, Ostrava, Czechia
- 4Center for Integrated Oncology (CIO) Aachen – Bonn – Cologne - Duesseldorf, Cologne, Germany
Introduction: The lateral tarsal strip is one of the basic surgical techniques in ophthalmic plastic surgery. It is used in many indications, predominantly in ectropion repair. Even though there are alternatives, it is probably one of the most popular techniques in ophthalmic plastic surgery. The lateral tarsal strip is also part of bigger surgical procedures (such as midface lifting, entropion surgery, reconstruction surgery, or a part of some surgical approaches to the orbit). The aim of this review is to assess the most common ways of usage of the lateral tarsal strip, to cover its alternatives, and to discuss the future of this technique.
Methods: We have search PubMed and Web of Science and went through articles about lateral tarsal strip. We have also searched for other techniques that used the lateral tarsal strip and included these articles in our review. We have analyzed the major articles and made a review about the topic.
Results: As a natural part of many advanced surgical techniques and as a major surgical technique for lower eyelid ectropion repair, the lateral tarsal strip remains an important part of modern ophthalmic plastic surgery.
Introduction
The lateral tarsal strip (LTS) procedure is a very popular technique that aims primarily to improve the ectropion in the lower eyelid with increased laxity (1). Nevertheless, as a technique used for a long time, nowadays, its indications and uses are much wider.
This article aims to present the possible indications of the LTS procedure and to discuss its role in modern oculoplastic surgery.
The LTS was firstly introduced in 1979 by Anderson and Gordy (1). From that time, it got widespread popularity, as it was promoted by many prominent ophthalmic plastic surgeons.
There always has been scientific discussion about the indications of the technique, and LTS has been compared to other “traditional” techniques in many studies (2).
Mostly, the LTS was considered equal or superior to many other techniques that aim to improve lower eyelid laxity. The LTS remains widely popular, especially for involutional ectropion and entropion repair.
Methods
We have searched Web of Science and PubMed. We used the following key word to search for the topic: lateral tarsal strip. We included articles that were focused on the LTS. We excluded articles that described alternative techniques of the surgery without comparison to LTS that was the aim of our article. We also preferred research and review articles to case reports. We have tried to cover most of the important topics that involve modern usage of the LTS. Table 1 shows the selection of the articles.
Technique
The LTS is mostly performed under local anesthesia. It begins with a lateral canthotomy and cantholysis (Figure 1A). The lower branch of the lateral canthal tendon is separated, and the lower eyelid is then fully released from its insertion.
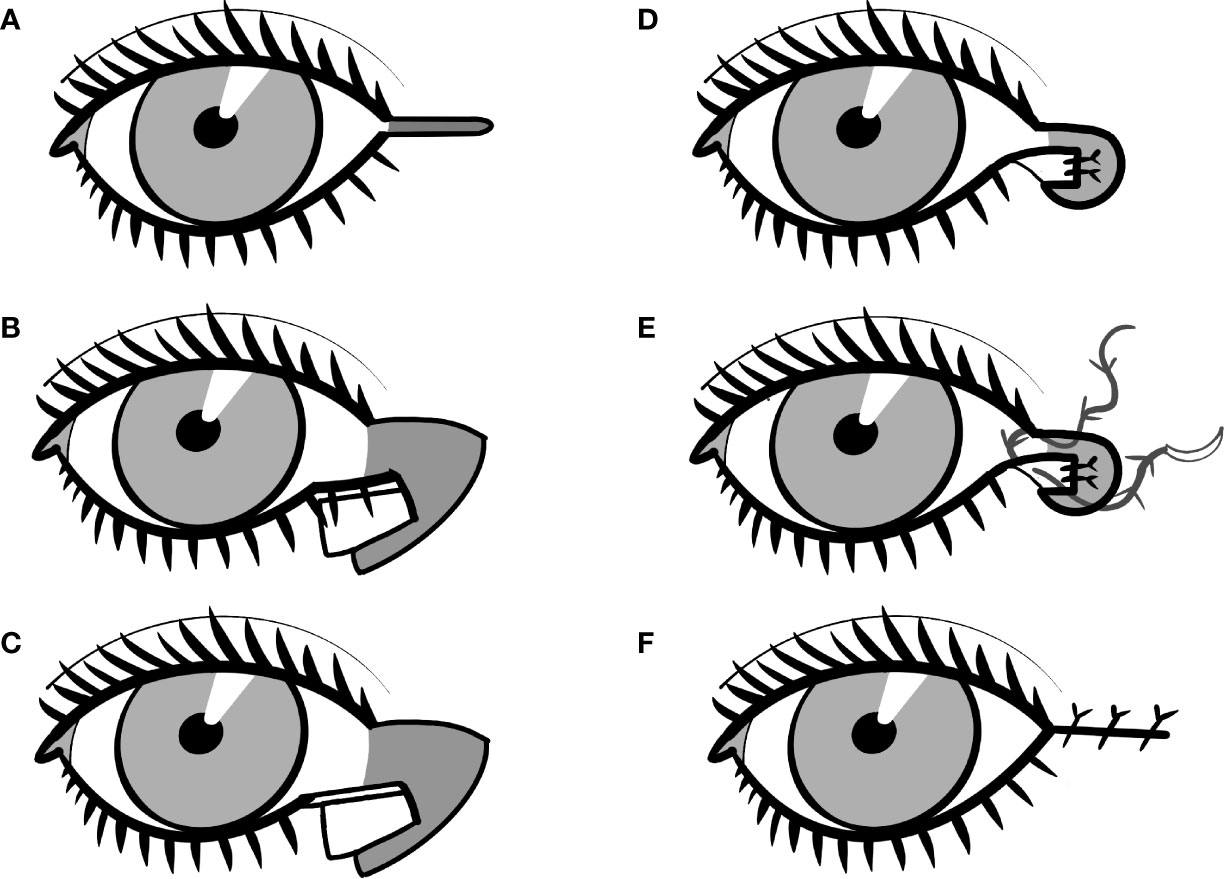
Figure 1 The schematic presentation of the lateral tarsal strip technique. (A) A lateral canthotomy and cantholysis and the lower branch of the lateral canthal tendon is separated and the lower eyelid is then fully released from its insertion. (B) The lateral portion of the anterior lamella of the lower eyelid is cut. (C) The superior portion of the eyelid’s margin is cut off at about the size of the anterior lamella cut. (D) The tarsal strip is secured to the periosteum of the medial part of the lateral orbital wall. (E) Canthopexy is performed with an absorbable suture. (F) The muscle and skin are then closed in two layers.
The lateral portion of the anterior lamella of the lower eyelid is cut (Figure 1B), and the superior portion of the eyelid’s margin is cut off at about the size of the anterior lamella cut (Figure 1C). The tarsal conjunctiva is cleaned with a scalpel or cauterization, although some authors do not recommend this step as necessary. Now, the so-called “tarsal strip” is prepared for reattachment.
The new position of the eyelid is tested. When more lateral movement of the tarsal strip is needed, lower eyelid retractors are cut with scissors.
The tarsal strip is secured to the periosteum of the medial part of the lateral orbital wall (Figure 1D). The surgeon can use either absorbable or permanent sutures. The choice could not be only based on the surgeon’s preference but varies with the primary diagnosis. In most cases, the LTS is sufficient with absorbable sutures (3). Nevertheless, some authors advocate, e.g., in paralytic ectropion to use non-absorbable sutures (4). Again, there is not much evidence in literature to support one type of suture, and the decision is therefore dependent on the surgeon’s preference.
The skin and orbicularis muscle are adjusted to correspond to the new eyelid position. Canthopexy is performed with an absorbable suture (Figure 1E). The muscle and skin are then closed in two layers (Figure 1F).
Mostly antibiotic ointments are administered after the surgery. The stitches are removed in 7–10 days.
Possible indications
Indications of LTS include several diagnoses such as involutional ectropion and entropion, paralytic ectropion, and esthetic or even orbital surgery. Some are more frequent, others less; all of them show the wide variety of problems that can be addressed by LTS surgery. In some indications, LTS is only an additional technique in a “bigger” surgical approach; in others, the LTS is the sole technique.
The main advantage of the LTS is the possibility of proper eyelid repositioning and rejuvenation of its lateral fixation (5). Many authors also advocate that, mostly in involutional ectropion, the LTS offers sufficient correction in most cases (6). On the other hand, some studies showed better or the same results with alternative techniques (2, 7). Nevertheless, the LTS remains a technique of choice for many oculoplastic surgeons (8).
Most of the studies of the LTS are based on classic eyelid measurements, patient observations, two-dimensional (2D) photography analysis, or the surgeon’s observations (6, 9, 10). Stereophotography measurements are more and more common in oculoplastic surgery nowadays, and they are proven to be objective, reproducible, and accurate (11–14). These measurements are now standardized with modern investigation protocols that help to perform very objective and reliable measurements (15–17).
As they are works that are using stereophotogrammetry in assessing the lower eyelid and its laxity and tension, more objective research should be presented on this topic to provide definitive arguments for the LTS as a major surgical technique (18, 19).
Involutional lower eyelid ectropion
As horizontal eyelid laxity is the major problem of many lower eyelids with ectropion, the LTS is a classic technique that is used in its repair. Involutional ectropion is the major cause of ectropion and it is caused by age, loosening the tension of the orbicularis muscles and both medial and lateral canthal tendons (20).
The success rate of the LTS in this indication is very high (21). The technique is often performed in a standardized manner as written above, and it can be further combined with additional techniques, mostly 3-snip and medial canthoplasty, to affect the medial canthal area as well.
The 3-snip punctoplasty presents a surgical opening (or widening) of the lower eyelid punctum to improve lacrimal drainage (22). Some studies confirm the qualities of the technique (22–24). The technique can be done with scissors or with a punch instrument (25). It is often combined with LTS or done alone.
When medial laxity is also prominent, the LTS can be combined with medial spindle—through the conjunctival incision, the inverting suture is induced to rotate the medial part of the eyelid inward (26). In more severe medial ectropion, the LTS can be combined with a medial canthopexy—from single or two skin incisions, the medial canthus is stabilized with sutures (27, 28).
Even though alternatives to the LTS are often presented in the literature, such as the Bick procedure, the LTS remains the technique of choice in involutional lower eyelid ectropion for most surgeons, as it is easy to perform, highly successful, and with good cosmetic and functional results (6, 21).
Involutional lower eyelid entropion
The choice of surgery for lower eyelid entropion depends on its etiology. The LTS positively affects all three major components of involutional entropion: horizontal eyelid laxity, weakening of the eyelid retractors, and override by the orbicularis muscle (29). The loss of tone and laxity are proven consequences of aging (30). Nevertheless, many authors combine the LTS with other procedures for involutional entropion repair.
Commonly, the LTS is combined with lower eyelid retractor plication. It was proven that this combination is more successful than retractor plication alone (31, 32) and that combined surgeries with the LTS are more successful than, e.g., Wies procedure in involutional entropion (33). There is also some experience that these combined surgeries are less prone to recurrence than plication surgeries alone, although further research is needed (34). Another possibility is the combination of the LTS with everting sutures (35). The combined surgery of everting sutures with the LTS has been proven to be more successful than everting sutures alone (36). On the other hand, one study stated that Bick’s procedure with lower lid retractor plication has a lower recurrence rate than the LTS with retractor plication/reinsertion (29).
Cicatricial ectropion
The cicatricial cause of ectropion is often more challenging than involutional reasons, since the scar presents strong traction downward that makes the probability of surgical failure higher. The LTS was proven to be useful in managing cicatricial lower eyelid ectropion. In some cases, the LTS itself can provide sufficient correction (37). Mostly, the LTS is combined with another technique—free skin graft, spacer graft for posterior lamella insufficiency, or cheek-midface lifting (38–40).
Paralytic ectropion
Several series confirm good results when using the LTS in paralytic ectropion (4, 41). Many advocate the combination of the LTS with lateral (often minimal in size) tarsorrhaphy (42, 43). Surgeons often aim to a higher postoperative position of the lower eyelid in paralytic LTS, as it is presumed that the surgery could be only temporarily successful with some recurrence rate (43). Some papers show that the combination of the LTS with reanimation surgery has higher success in 3-year follow-up (44).
Floppy eyelid syndrome
Floppy eyelid syndrome is characterized by high laxity of the upper eyelid that leads to reactive papillary conjunctivitis. It could be seen in patients with sleep apnea, obesity, or keratoconus (45, 46). Initially, it was treated with horizontal eyelid shortening techniques. Nowadays, several modern techniques are used. According to some authors, the LTS in the upper eyelid is considered to be superior to wedge resection techniques (47). Some surgeons recommend combination with medial canthopexy (48).
Cheek-midface lift
The LTS is a natural part of the cheek-midface lift technique. The cheek-midface lift is a popular technique for facial rejuvenation in esthetic surgery (49). Also, some reconstruction indications have been described, e.g., for cicatricial ectropion after lower eyelid blepharoplasty or for severe ectropion with a negative vector (50–52).
Congenital malpositions
The LTS can also be used in children. Congenital ectropion is very rare, especially the one that is developed because of high lid laxity. But one of the most commonly mentioned indications is congenital euryblepharon. Euryblepharon is characterized by bilateral enlargement of the palpebral fissure with lateral ectropion (53). There are case reports about surgical treatment of epiblepharon with the LTS or with cheek-midface lifting (54).
Anophthalmic lower eyelid correction
Proper position of the lower eyelid is important in anophthalmic patients. Loss of volume and higher laxity can lead to malposition of the prosthesis. This leads not only to esthetic concerns of the patients but also to significant discomfort and dry eye (55, 56). Even though this is preventable, sometimes the LTS could aid to improve the fitting of the prosthesis (57). It was even in the first article by Anderson that introduced the LTS as a surgical technique—the initial indication for the LTS was the usage in anophthalmic sockets (1).
Esthetic surgery
Canthoplasty is often mentioned in esthetic surgery as stabilization for lower eyelid blepharoplasty (58). However, some surgeons rather combine lower blepharoplasty with the LTS to get better stabilization (59). Microincision is often used to prevent a visible scar in the lateral canthus (60).
With the growing popularity of the transconjunctival approach, it can be presumed that the LTS will be used in lower eyelid blepharoplasty less frequently, as most of the iatrogenic lower eyelid retraction occurs after transcutaneous blepharoplasty (61, 62).
The LTS is often part of the correction of the iatrogenic lower eyelid retraction after excessive blepharoplasty. It is often used with other techniques, such as grafting or cheek-midface lift (39, 50).
Tumor resection
Some reports describe the usage of the LTS in the reconstruction of later lower eyelid defects that are in the lateral canthal area. The LTS can be combined with a periosteal flap or even free tarsal grafts and then covered with a myocutaneous transposition flap with very good results (63).
Surgical approach to the orbit
In anterior orbitotomy, releasing the lower eyelid from its insertion can play a significant role in getting a better approach to the orbit. It allows the surgeon a better approach to the lower and lateral orbit. Canthotomy or cantholysis is often used in the transconjunctival approach (64). With lateral canthotomy and cantholysis, the surgeon can reach a much wider and deeper space (65). The LTS is then used for repair at the end of the surgery.
Conclusions
The LTS procedure remains an important basic technique in ophthalmic plastic surgery. Safe, fast, and easy to combine with other techniques, it can be used in a wide range of lower eyelid malposition indications.
Author contributions
AK - manuscript concept, writing AR - writing, data collection LH - revision of the manuscript, co-writing, clinical analysis. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Anderson RL, Gordy DD. The tarsal strip procedure. Arch Ophthalmol (1979) 97(11):2192–6. doi: 10.1001/archopht.1979.01020020510021
2. Vahdani K, Ford R, Garrott H, Thaller VT. Lateral tarsal strip versus bick's procedure in correction of eyelid malposition. Eye (London England) (2018) 32(6):1117–22. doi: 10.1038/s41433-018-0048-9
3. Hsuan J, Selva D. The use of a polyglactin suture in the lateral tarsal strip procedure. Am J Ophthalmol (2004) 138(4):588–91. doi: 10.1016/j.ajo.2004.05.060
4. Jue MS, Yoo J, Kim MS, Park HJ. The lateral tarsal strip for paralytic ectropion in patients with leprosy. Ann Dermatol (2017) 29(6):742–6. doi: 10.5021/ad.2017.29.6.742
5. Dryden RM, Edelstein JP. Lateral palpebral tendon repair for lower eyelid ectropion. Ophthalmic Plast Reconstr Surg (1988) 4(2):115–8. doi: 10.1097/00002341-198804020-00012
6. Kam KY, Cole CJ, Bunce C, Watson MP, Kamal D, Olver JM. The lateral tarsal strip in ectropion surgery: is it effective when performed in isolation? Eye (London England) (2012) 26(6):827–32. doi: 10.1038/eye.2012.34
7. Dulz S, Green S, Mehlan J, Schüttauf F, Keserü M. A comparison of the lateral tarsal strip with everting sutures and the quickert procedure for involutional entropion. Acta Ophthalmol (2019) 97(6):e933–6. doi: 10.1111/aos.14093
8. Georgescu D. Surgical preferences for lateral canthoplasty and canthopexy. Curr Opin Ophthalmol (2014) 25(5):449–54. doi: 10.1097/icu.0000000000000094
9. Mora AM, Córdoba CM, Padilla FD, Duran DF. Lateral tarsal strip through osteotomies for recurrent ectropion and eyelid laxity correction. Eur J Ophthalmol (2022). doi: 10.1177/11206721211073036
10. López-García JS, García-Lozano I, Giménez-Vallejo C, Jiménez B, Sánchez ÁV, de Juan IE. Modified lateral tarsal strip for involutional entropion and ectropion surgery. Graefe's Arch Clin Exp Ophthalmol = Albrecht Von Graefes Archiv Fur Klin Exp Ophthalmol (2017) 255(3):619–25. doi: 10.1007/s00417-016-3536-2
11. Liu J, Guo Y, Arakelyan M, Rokohl AC, Heindl LM. Accuracy of areal measurement in the periocular region using stereophotogrammetry. J Oral Maxillofac Surg (2021) 79(5):1106. doi: 10.1016/j.joms.2020.12.015
12. Liu J, Rokohl AC, Guo Y, Li S, Hou X, Fan W, et al. Reliability of stereophotogrammetry for area measurement in the periocular region. Aesthet Plast Surg (2021) 45(4):1601–10. doi: 10.1007/s00266-020-02091-5
13. Guo Y, Rokohl AC, Schaub F, Hou X, Liu J, Ruan Y, et al. Reliability of periocular anthropometry using three-dimensional digital stereophotogrammetry. Graefe's Arch Clin Exp Ophthalmol = Albrecht Von Graefes Archiv Fur Klin Exp Ophthalmol (2019) 257(11):2517–31. doi: 10.1007/s00417-019-04428-6
14. Li S, Rokohl AC, Guo Y, Heindl LM. 2D photos are great, but what about 3D imaging? Graefe's Arch Clin Exp Ophthalmol (2021) 260:1799–800. doi: 10.1007/s00417-021-05479-4
15. Guo Y, Liu J, Ruan Y, Rokohl X, Hou S, Li R, et al. A novel approach quantifying the periorbital morphology: A comparison of direct, 2-dimensional, and 3-dimensional technologies. J Plast Reconstr Aesthet Surg JPRAS (2021) 74(8):1888–99. doi: 10.1016/j.bjps.2020.12.003
16. Guo Y, Schaub F, Mor JM, Jia R, Koch KR, Heindl LM. A simple standardized three-dimensional anthropometry for the periocular region in a European population. Plast Reconstr Surg (2020) 145(3):514e–23e. doi: 10.1097/prs.0000000000006555
17. Guo Y, Hou X, Rokohl AC, Jia R, Heindl LM. Reliability of periocular anthropometry: A comparison of direct, 2-dimensional, and 3-dimensional techniques. Dermatol Surg (2020) 46(9):e23–31. doi: 10.1097/dss.0000000000002243
18. Hou X, Rokohl AC, Meinke MM, Li S, Liu J, Fan W, et al. A novel standardized distraction test to evaluate lower eyelid tension using three-dimensional stereophotogrammetry. Quant Imaging Med Surg (2021) 11(8):3735–48. doi: 10.21037/qims-20-1016
19. Hou X, Rokohl AC, Meinke MM, Liu J, Li S, Fan W, et al. Standardized three-dimensional lateral distraction test: Its reliability to assess medial canthal tendon laxity. Aesthet Plast Surg (2021) 45(6):2798–807. doi: 10.1007/s00266-021-02440-y
20. Jordan DR, Anderson RL. The lateral tarsal strip revisited. the enhanced tarsal strip. Arch Ophthalmol (1989) 107(4):604–6. doi: 10.1001/archopht.1989.01070010618042
21. Hou X, Guo Y, Li S, Lin M, Jia R, Rokohl A, et al. Lateral tarsal strip procedure for involutional ectropion: A retrospective analysis of 85 cases and a comprehensive literature review. Adv Ophthalmol Pract Res (2021) 1(1):100004. doi: 10.1016/j.aopr.2021.100004
22. Caesar RH, McNab AA. A brief history of punctoplasty: the 3-snip revisited. Eye (2005) 19(1):16–8. doi: 10.1038/sj.eye.6701415
23. Murdock J, Lee WW, Zatezalo CC, Ballin A. Three-snip punctoplasty outcome rates and follow-up treatments. Orbit (2015) 34(3):160–3. doi: 10.3109/01676830.2015.1014513
24. Tamer SS, Abdelghany AA, Elshafei AM, Abdelrahman Abdallah RM. Three-snip punctoplasty versus perforated plugs for management of lacrimal punctal stenosis. Eur J Ophthalmol (2021) 31(2):796–803. doi: 10.1177/1120672120925035
25. Wong ES, Li EY, Yuen HK. Long-term outcomes of punch punctoplasty with Kelly punch and review of literature. Eye (London England) (2017) 31(4):560–5. doi: 10.1038/eye.2016.271
26. Nowinski TS, Anderson RL. The medial spindle procedure for involutional medial ectropion. Arch Ophthalmol (1985) 103(11):1750–3. doi: 10.1001/archopht.1985.01050110146045
27. Sodhi PK, Verma L, Pandey RM, Ratan SK. Appraisal of a modified medial canthal plication for treating laxity of the medial lower eyelid. J Cranio-maxillo-facial Surg (2005) 33(3):205–9. doi: 10.1016/j.jcms.2005.01.006
28. Kelly CP, Cohen AJ, Yavuzer R, Moreira-Gonzalez A, Jackson IT. Medial canthopexy: A proven technique. Ophthalmic Plast Reconstr Surg (2004) 20(5).
29. Poon JS, Vahdani K, Thaller VT. Comparison of four combined procedures for correction of involutional lower eyelid entropion. J Craniofac Surg (2019) 30(4):1239–44. doi: 10.1097/scs.0000000000005466
30. Damasceno RW, Avgitidou G, Belfort R Jr., Dantas PE, Holbach LM, Heindl LM. Eyelid aging: pathophysiology and clinical management. Arq Bras Oftalmol (2015) 78(5):328–31. doi: 10.5935/0004-2749.20150087
31. Ranno S, Sacchi M, Gilardi D, Lembo A, Nucci P. Retractor plication versus retractor plication and lateral tarsal strip for eyelid entropion correction. Eur J Ophthalmol (2014) 24(2):141–6. doi: 10.5301/ejo.5000369
32. Ho SF, Pherwani A, Elsherbiny SM, Reuser T. Lateral tarsal strip and quickert sutures for lower eyelid entropion. Ophthalmic Plast Reconstr Surg (2005) 21(5):345–8. doi: 10.1097/01.iop.0000179370.96976.ee
33. Serin D, Buttanri IB, Karslioglu S, Sevim MS, Buttanri B, Akbaba M. The efficacy of the combined procedure in involutional entropion surgery: a comparative study. Korean J Ophthalmol KJO (2013) 27(6):405–8. doi: 10.3341/kjo.2013.27.6.405
34. Boboridis KG, Bunce C. Interventions for involutional lower lid entropion. Cochrane Database Syst Rev (2011) 12):Cd002221. doi: 10.1002/14651858.CD002221.pub2
35. Barnes JA, Bunce C, Olver JM. Simple effective surgery for involutional entropion suitable for the general ophthalmologist. Ophthalmology (2006) 113(1):92–6. doi: 10.1016/j.ophtha.2005.06.039
36. Scheepers MA, Singh R, Ng J, Zuercher D, Gibson A, Bunce C, et al. A randomized controlled trial comparing everting sutures with everting sutures and a lateral tarsal strip for involutional entropion. Ophthalmology (2010) 117(2):352–5. doi: 10.1016/j.ophtha.2009.06.056
37. Goddard L, Chesnut C. Simultaneous lateral tarsal strip and medial spindle procedures for cicatricial ectropion. Dermatol Surg (2019) 45(7):898–905. doi: 10.1097/dss.0000000000001757
38. Salgarelli AC, Francomano M, Magnoni C, Bellini P. Cicatricial iatrogenic lower eyelid malposition in skin cancer surgery: results of a combined approach. J Craniomaxillofac Surg (2012) 40(7):579–83. doi: 10.1016/j.jcms.2011.10.014
39. Patel BC, Patipa M, Anderson RL, McLeish W. Management of postblepharoplasty lower eyelid retraction with hard palate grafts and lateral tarsal strip. Plast Reconstr Surg (1997) 99(5):1251–60. doi: 10.1097/00006534-199704001-00007
40. Procianoy F, Barbato MT, Osowski LE, Bocaccio FJ, Bakos L. Cicatricial ectropion correction in a patient with pyoderma gangrenosum: case report. Arq Bras Oftalmol (2009) 72(3):384–6. doi: 10.1590/s0004-27492009000300020
41. Vásquez LM, Medel R. Lagophthalmos after facial palsy: Current therapeutic options. Ophthalmic Res (2014) 52(4):165–9. doi: 10.1159/000365519
42. Kwon KY, Jang SY, Yoon JS. Long-term outcome of combined lateral tarsal strip with temporal permanent tarsorrhaphy for correction of paralytic ectropion caused by facial nerve palsy. J Craniofac Surg (2015) 26(5):e409–12. doi: 10.1097/scs.0000000000001875
43. Chang L, Olver J. A useful augmented lateral tarsal strip tarsorrhaphy for paralytic ectropion. Ophthalmology (2006) 113(1):84–91. doi: 10.1016/j.ophtha.2005.06.038
44. Lisman RD, Smith B, Baker D, Arthurs B. Efficacy of surgical treatment for paralytic ectropion. Ophthalmology (1987) 94(6):671–81. doi: 10.1016/s0161-6420(87)33395-0
45. Salinas R, Puig M, Fry CL, Johnson DA, Kheirkhah A. Floppy eyelid syndrome: A comprehensive review. Ocul Surf (2020) 18(1):31–9. doi: 10.1016/j.jtos.2019.10.002
46. Pham TT, Perry JD. Floppy eyelid syndrome. Curr Opin Ophthalmol (2007) 18(5):430–3. doi: 10.1097/ICU.0b013e3282ced08e
47. Ezra DG, Beaconsfield M, Sira M, Bunce C, Shah-Desai S, Verity DH, et al. Long-term outcomes of surgical approaches to the treatment of floppy eyelid syndrome. Ophthalmology (2010) 117(4):839–46. doi: 10.1016/j.ophtha.2009.09.009
48. Compton CJ, Melson AT, Clark JD, Shipchandler TZ, Nunery WR, Lee HB. Combined medial canthopexy and lateral tarsal strip for floppy eyelid syndrome. Am J Otolaryngol (2016) 37(3):240–4. doi: 10.1016/j.amjoto.2016.01.007
49. Hachach-Haram N, Kirkpatrick WN. Midface-lifting: evolution, indications, and technique. Facial Plast Surg FPS (2013) 29(4):289–94. doi: 10.1055/s-0033-1349366
50. Kopecky A, Koch KR, Schroedl F, Rokohl AC, Nemcansky J, Heindl LM. [Cheek-midface lift for revision following failed excessive lower eyelid blepharoplasty]. Der Ophthalmol Z Der Dtsch Ophthalmol Ges (2019) 116(5):472–6. doi: 10.1007/s00347-018-0831-9
51. Kopecký A, Rokohl AC, Wawer Matos PA, Němčanský J, Heindl LM. Cheek-midface lifting with lateral canthoplasy for the repair of complex iatrogenic lower eyelid ectropion. Eur J Ophthalmol (2021). doi: 10.1177/11206721211039334
52. Jacono AA, Stong BC. Combined transconjunctival release and midface-lift for postblepharoplasty ectropion repair. Arch Facial Plast Surg (2010) 12(3):206–8. doi: 10.1001/archfacial.2010.31
53. Gupta AK, Saxena P. Euryblepharon with associated ocular anomalies. J Pediatr Ophthalmol (1976) 13(3):163–4.
54. Yip C-C, McCann JD, Goldberg RA. The role of midface lift and lateral canthal repositioning in the managementof euryblepharon. Arch Ophthalmol (2004) 122(7):1075–7. doi: 10.1001/archopht.122.7.1075
55. Rokohl AC, Adler W, Koch KR, Mor JM, Jia R, Trester M, et al. Cryolite glass prosthetic eyes-the response of the anophthalmic socket. Graefe's Arch Clin Exp Ophthalmol = Albrecht Von Graefes Archiv Fur Klin Exp Ophthalmol (2019) 257(9):2015–23. doi: 10.1007/s00417-019-04395-y
56. Rokohl AC, Trester M, Guo Y, Adler W, Jaeger VK, Lorreck N, et al. Dry anophthalmic socket syndrome - standardized clinical evaluation of symptoms and signs. Ocul Surf (2020) 18(3):453–9. doi: 10.1016/j.jtos.2020.05.001
57. Rokohl AC, Trester M, Pine KR, Heindl LM. Prevention of socket complications in anophthalmic patients. Curr Eye Res (2020) 45(12):1625–6. doi: 10.1080/02713683.2020.1770294
58. De Silva DJ, Prasad A. Aesthetic canthal suspension. Clinics Plast Surg (2015) 42(1):79–86. doi: 10.1016/j.cps.2014.08.005
59. Oestreicher JH, Tarassoly K. The "mini tarsal strip" lateral canthopexy for lower eyelid laser-assisted blepharoplasty-indications, technique and complications in 614 cases. Orbit Feb (2010) 29(1):7–10. doi: 10.3109/01676830903207810
60. Olver JM, Barnes JA. Effective small-incision surgery for involutional lower eyelid entropion. Ophthalmology (2000) 107(11):1982–8. doi: 10.1016/s0161-6420(00)00358-4
61. Castañares S. Ectropion after blepharoplasty prevention and treatment. Aesthet Plast Surg (1978) 2(1):125–40. doi: 10.1007/bf01577946
62. McGraw BL, Adamson PA. Postblepharoplasty ectropion. prevention and management. Arch Otolaryngol–head Neck Surg (1991) 117(8):852–6. doi: 10.1001/archotol.1991.01870200046006
63. Perry CB, Carter K, Allen R. Horizontal tarsal transposition flap and lateral canthal fixation for repair of Large, central lower eyelid defects. Invest Ophthalmol Visual Sci (2013) 54(15):6373–3. doi: 10.4103/0301-4738.191488
64. Lorenz HP, Longaker MT, Kawamoto HK Jr. Primary and secondary orbit surgery: the transconjunctival approach. Plast Reconstr Surg (1999) 103(4):1124–8. doi: 10.1097/00006534-199904040-00003
Keywords: oculoplastic, eyelid, lateral tarsal strip, ectropion, eyelid surgery, oculoplastic surgery
Citation: Kopecký A, Rokohl AC and Heindl LM (2022) The role of the lateral tarsal strip procedure in modern ophthalmic plastic surgery—A review. Front. Ophthalmol. 2:871964. doi: 10.3389/fopht.2022.871964
Received: 08 February 2022; Accepted: 27 June 2022;
Published: 26 August 2022.
Edited by:
Robert Laemmer, University Hospital Erlangen, GermanyReviewed by:
Sun Young Jang, Soon Chun Hyang University Bucheon Hospital, South KoreaMichael Yoon, Harvard Medical School, United States
Copyright © 2022 Kopecký, Rokohl and Heindl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adam Kopecký, YWRhbS5rb3BlY2t5QHdpbmV0LmN6
 Adam Kopecký
Adam Kopecký Alexander C. Rokohl
Alexander C. Rokohl Ludwig M. Heindl
Ludwig M. Heindl