
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 18 February 2025
Sec. Head and Neck Cancer
Volume 15 - 2025 | https://doi.org/10.3389/fonc.2025.1551514
This article is part of the Research Topic Early Diagnosis in Head and Neck Cancer: Advances, Techniques, and Challenges View all 6 articles
Squamous cell carcinoma of the thyroid (SCCT) represents a rare subtype of thyroid malignancy characterized by a poor prognosis and is frequently misdiagnosed as subacute thyroiditis (SAT). This report discusses a case of SCCT that was recurrently misdiagnosed with neck pain as the initial clinical presentation. An 80-year-old Asian female presented multiple times to the department of emergency, department of vascular and thyroid surgery, and department of endocrinology due to a painful neck mass. Ultrasonography identified a cystic solid mass in the right thyroid lobe, measuring 4.55 cm*3.2 cm. Enhanced computed tomography (CT) scanning revealed a significant enlargement of the right thyroid lobe, with an irregular mass exhibiting indistinct boundaries and blurred surrounding spaces. Laryngoscopic examination demonstrated immobilization of the right vocal cord and inadequate glottic closure. The erythrocyte sedimentation rate (ESR) was elevated to 94 mm/h. Thyroid function tests indicated subclinical thyrotoxicosis. The patient was initially diagnosed with subacute thyroiditis, and her symptoms improved following treatment with glucocorticoids and analgesics. One month following treatment, the patient experienced dyspnea, and subsequent computed tomography (CT) imaging revealed tracheal compression and narrowing, which contributed to the respiratory distress. A biopsy of the tumor was conducted, and pathological examination confirmed the presence of squamous cell carcinoma. To definitively diagnose SCCT, pathological examination and immunohistochemical analysis are required. Early and accurate diagnosis is essential for developing appropriate treatment strategies and enhancing patient survival rates. It is imperative for clinicians to comprehend this rare and life-threatening disease to enhance treatment efficacy.
Squamous cell carcinoma of the thyroid (SCCT) represents a rare subtype of thyroid malignancy, comprising approximately 0.1-0.4% of all thyroid cancer cases (1–3). This neoplasm is characterized by its highly aggressive nature and poor prognosis. Survival rates are notably low and the median survival duration ranges from 7.7 to 9.1 months (2–4). Patients with SCCT typically present at an advanced stage due to the prevalence of local metastases (55.4%), extrathyroidal extension (64%), and distant metastases (11.7%) (2, 4). The clinical manifestations of SCCT are predominantly influenced by tumor size and anatomical location, manifesting as a neck mass, hoarseness due to recurrent laryngeal nerve invasion, dyspnea from tracheal compression, and dysphagia resulting from esophageal invasion (3, 5). Previous findings suggest that laryngoscopy of vocal cord function is effective in evaluating the recurrent laryngeal nerve function ahead of surgery (6). In contrast, subacute thyroiditis (SAT) is an inflammatory disorder of the thyroid gland, the pathogenesis and clinical course determinants of which have remained elusive for decades (7). Women constitute 75-80% of SAT cases (7, 8). The predominant symptoms reported by SAT patients include anterior neck pain, frequently radiating to the jaw, ears, and upper mediastinum, as well as nocturnal fever (7–9). The most common laboratory finding in SAT is an elevated erythrocyte sedimentation rate (ESR), which can sometimes reach values in the triple digits (7, 9). C-reactive protein (CRP) levels are also elevated in many cases, although CRP is considered a less specific marker for SAT (9). Additionally, there may be an increase in the white blood cell count (WBC) (7, 9). The treatment regimen for SAT typically involves the administration of non-steroidal anti-inflammatory drugs (NSAIDs) to alleviate pain and inflammation, along with corticosteroids to further reduce inflammation (10). Subacute thyroiditis is generally self-limiting, with most patients recovering spontaneously within a few weeks to several months, necessitating regular follow-up (7). In this report, we present a case of SCCT that was repeatedly misdiagnosed with neck pain as the initial clinical manifestation.
The patient, an 80-year-old Asian woman with no history of smoking, presented multiple times to the department of emergency, the department of vascular and thyroid surgery, and the department of endocrinology over the past three months due to a painful neck mass. Ultrasound examination identified a cystic solid mass in the right thyroid lobe measuring 4.55 cm*3.2 cm (Figure 1A). The tumor exhibited an indistinct boundary, a regular shape, a predominance of solid components, and an absence of blood flow signals. An enhanced computed tomography (CT) scan revealed a significant increase in the volume of the right thyroid lobe, characterized by an irregular mass with indistinct boundaries and blurred surrounding spaces. The adjacent structures were compressed and displaced, and the trachea was compressed and shifted to the left. The lesion measured approximately 50mm*42mm*60mm and exhibited heterogeneous enhancement post-contrast, with patchy areas of non-enhancing necrosis observed internally (Figures 1B, C). Laryngoscopic examination indicated immobilization of the right vocal cord and inadequate glottic closure. The ESR was elevated to 94 mm/h. Laboratory tests showed increased levels of free thyroxine 4, thyroglobulin antibodies, thyroperoxidase antibodies, and thyroglobulin, while thyrotropin-stimulating hormone levels were decreased. Based on these findings, the patient was diagnosed with subacute thyroiditis, and her symptoms improved following treatment with glucocorticoids and analgesics. However, one-month post-treatment, the patient developed dyspnea, and subsequent CT imaging demonstrated tracheal compression and narrowing, contributing to the respiratory distress. A biopsy of the tumor was performed, revealing squamous cell carcinoma upon pathological examination. Immunohistochemical analysis showed positive staining for CKpan, CK5/6 (Figure 2), P40, P63, and CK7, while negative staining was observed for NapsinA, TTF-1, CD56, CgA, Syn, Pax-8, Tg, and Vimentin. The Ki67 proliferation index was determined to be 70%. These results confirmed the diagnosis of SCCT. Suffering from shortness of breath, the patient was treated with a tracheal stent and later moved to the oncology department for further care. Three months after being diagnosed, the patient is still alive.
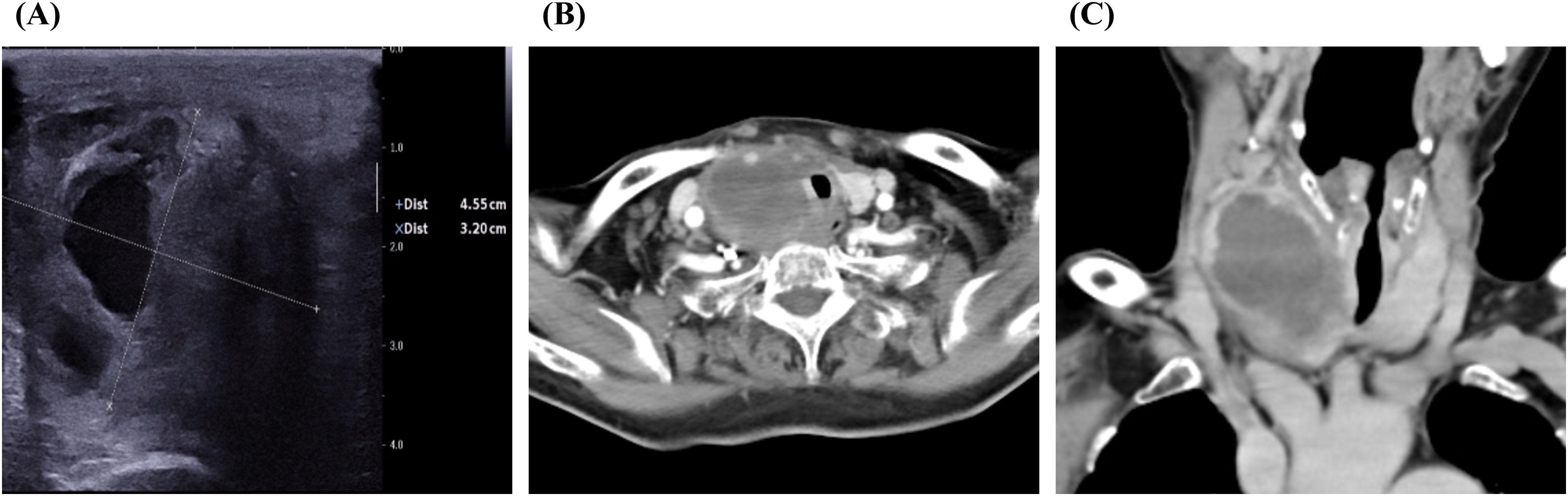
Figure 1. Typical image of imaging examination. (A) Ultrasound image of the tumor. (B) CT image of thyroid tumor in coronal section. (C) CT image of thyroid tumor in axial section.
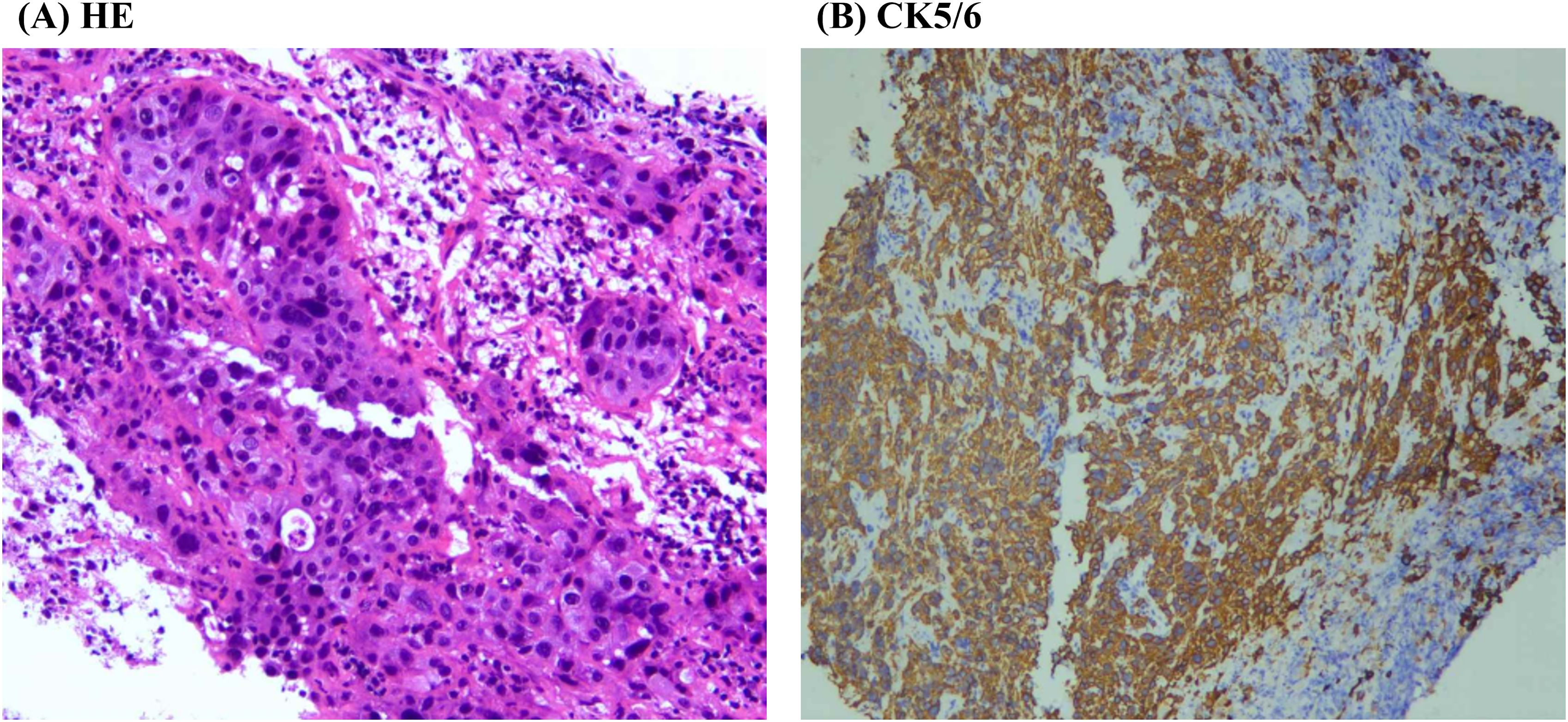
Figure 2. Typical diagram of pathological examination. (A) HE staining image of thyroid tumor. (B) Immunohistochemical results of CK5/6 in the thyroid tumor.
SCCT is an exceedingly rare and highly aggressive malignancy, typically associated with a poor prognosis and a survival rate often less than one year (3). The literature frequently recommends ultrasonography, computed tomography (CT)/magnetic resonance imaging (MRI), and fine needle aspiration cytology (FNAC) as diagnostic tools for thyroid nodules (11). Despite the availability of various diagnostic methods, including clinical assessment, diagnostic imaging, and endoscopy, early diagnosis of SCCT remains challenging (12). Particularly when the clinical presentation involves a sudden painful neck mass, there is a high risk of misdiagnosis as SAT. Furthermore, treatment for SAT often alleviates patient pain, which can further contribute to diagnostic errors. In our study, the patient was initially diagnosed with SAT; however, the definitive diagnosis was not established until she was readmitted to the hospital due to dyspnea and subsequently underwent a pathological examination.
SCCT typically occurs in an older demographic compared to conventional papillary thyroid carcinoma, with 76% of cases diagnosed in individuals aged between 60 and 80 years, and over 60% of reported cases occurring in those aged 60 or older (3, 13, 14). Patients are commonly present with a rapidly enlarging neck mass that invades adjacent structures and is often associated with cervical lymphadenopathy. The mass effect of the tumor can lead to obstructive symptoms, including dysphagia, dyspnea, hoarseness, and neck pain (14). The prognosis for patients with thyroid squamous cell carcinoma is generally poor, with a documented median survival of 8 months and a 2-year survival rate of 14% (3, 14). SCCT requires aggressive treatment involving a multidisciplinary approach. Patients who undergo radical surgery exhibit the highest survival rates (15, 16), while the response to radiotherapy is poor, and the tumor is relatively resistant to chemotherapy (1, 3, 4, 13, 17). At present, surgery is seen as an effective way to lessen tumor load and symptoms of local invasion, with successful surgical removal of SCCT tumors linked to better median overall survival (2), but radical surgery might lead to more severe complications. Additionally, SCCT does not uptake iodine, rendering radioactive iodine therapy ineffective (3). SCCT is an aggressive malignant neoplasm characterized by low incidence and poor prognosis (18–20). Prompt and precise diagnosis is crucial for formulating effective treatment strategies and enhancing patient survival rates. In the present case, a lack of clinical experience resulted in a misdiagnosis of SAT for a duration of three months, thereby overlooking the presence of SCCT.
Definitive diagnosis of thyroid cancer relies on pathological examination and immunohistochemical analysis. In primary thyroid squamous cell carcinomas, thyroglobulin and thyroid transcription factor-1 (TTF-1) are infrequently detected (21, 22), with previous studies indicating positivity rates of only 4% (1/25) and 17% (3/18), respectively (3). In thyroid malignancies, excluding well-differentiated thyroid cancers, the paired box gene 8 (PAX-8) protein is considered a more sensitive indicator of thyroid origin than TTF-1 or thyroglobulin (3); however, PAX-8 is present in limited quantities in primary squamous cell carcinomas. The proteins p63 and p40 serve as sensitive markers for squamous cell differentiation, with p40 being more specific than p63 in distinguishing squamous cell carcinoma (23). Notably, all 10 cases of primary thyroid squamous cell carcinoma reported in the literature demonstrated p63 positivity (3). Cytokeratin 5/6, a high molecular weight cytokeratin, serves as a marker for squamous cell carcinoma (24). In the literature, cytokeratin 5/6 has consistently tested positive for primary thyroid squamous cell carcinoma. Additionally, cytokeratin 7 was positive in 13 out of 14 reported cases of primary thyroid squamous cell carcinoma (3). In our case, the tumor exhibited positive staining for CK5/6, P40, P63, and CK7, while showing negative staining for Napsin A, TTF-1, CD56, Chromogranin A, Synaptophysin, Pax-8, thyroglobulin, and vimentin. These findings confirmed the diagnosis of SCCT.
The patient in our case report was repeatedly misdiagnosed with SAT due to several factors. Firstly, the patient presented with a sudden painful thyroid tumor and elevated ESR, making it challenging to differentiate from SAT. Secondly, SCCT is exceedingly rare and scarcely documented in the literature, resulting in a lack of awareness among some medical professionals. Through this case report, we aim to enhance clinicians’ understanding of SCCT and emphasize the importance of distinguishing it from SAT. Early and accurate diagnosis is crucial for formulating appropriate treatment strategies and improving patient survival rates. It is important for clinicians to understand this uncommon and life-threatening disease to improve treatment effectiveness.
We thank the patient for granting permission to publish this information.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of Guizhou Provincial People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
ZY: Funding acquisition, Methodology, Validation, Writing – original draft, Writing – review & editing. DT: Data curation, Writing – original draft, Writing – review & editing. PY: Funding acquisition, Writing – original draft, Writing – review & editing. ZJ: Funding acquisition, Resources, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China under Grand 82460590 (PY), 82302286 (ZY), 82060390 (ZJ) and the health research project of Guizhou Province gzwkj2025-302 (ZJ).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Yang S, Li C, Shi X, Ma B, Xu W, Jiang H, et al. Primary squamous cell carcinoma in the thyroid gland: A population-based analysis using the SEER database. World J Surg. (2019) 43(5):1249–55. doi: 10.1007/s00268-019-04906-2
2. Yan W, Chen H, Li J, Zhou R, Su J. Primary squamous cell carcinoma of thyroid gland: 11 case reports and a population-based study. World J Surg Oncol. (2022) 20:352. doi: 10.1186/s12957-022-02814-9
3. Lam AK-Y. Squamous cell carcinoma of thyroid: a unique type of cancer in World Health Organization Classification. Endocrine-Related Cancer. (2020) 27:R177–92. doi: 10.1530/ERC-20-0045
4. Limberg J, Ullmann TM, Stefanova D, Finnerty BM, Beninato T, Fahey TJ 3rd, et al. Prognostic characteristics of primary squamous cell carcinoma of the thyroid: A national cancer database analysis. World J Surg. (2020) 44(2):348–55. doi: 10.1007/s00268-019-05098-5
5. Liao T, Long Y, Li L, Qi Q, Li L, Fu G. Primary thyroid squamous cell carcinoma diagnosed with (18)F-FDG PET/CT: a case report. Front Oncol. (2024) 14:1434811. doi: 10.3389/fonc.2024.1434811
6. Gambardella C, Offi C, Romano RM, De Palma M, Ruggiero R, Candela G, et al. Transcutaneous laryngeal ultrasonography: a reliable, non-invasive and inexpensive preoperative method in the evaluation of vocal cords motility-a prospective multicentric analysis on a large series and a literature review. Updates Surg. (2020) 72(3):885–92. doi: 10.1007/s13304-020-00728-3
7. Stasiak M, Lewiński A. New aspects in the pathogenesis and management of subacute thyroiditis. Rev Endocr Metab Disord. (2021) 22:1027–39. doi: 10.1007/s11154-021-09648-y
8. Batman A, Yazıcı D, Dikbaş O, Ağbaht K, Saygılı ES, Demirci İ, et al. Subacute THYROiditis related to SARS-coV-2 VAccine and covid-19 (THYROVAC study): A multicenter nationwide study. J Clin Endocrinol Metab. (2023) 108(10):e1013–26. doi: 10.1210/clinem/dgad235
9. Stasiak M, Michalak R, Stasiak B, Lewinski A. Clinical characteristics of subacute thyroiditis is different than it used to be - current state based on 15 years own material. Neuro Endocrinol Lett. (2019) 39(7):489–95.
10. Duan L, Feng X, Zhang R, Tan X, Xiang X, Shen R, et al. Short-term versus 6-week prednisone in the treatment of subacute thyroiditis: A randomized controlled trial. Endocr Pract. (2020) 26(8):900–8. doi: 10.4158/EP-2020-0096
11. Grani G, Sponziello M, Filetti S, Durante C. Thyroid nodules: diagnosis and management. Nat Rev Endocrinol. (2024) 20:715–28. doi: 10.1038/s41574-024-01025-4
12. Xin S, Li W, Yuan N, Shen C, Zhang D, Chai S. Primary squamous cell carcinoma of the thyroid: a case report. J Int Med Res. (2021) 49:3000605211004702. doi: 10.1177/03000605211004702
13. Limberg J, Ullmann T, Stefanova D, Finnerty BM, Beninato T, Fahey TJ 3rd, et al. Prognostic characteristics of primary squamous cell carcinoma of the thyroid: a national cancer database analysis. World J Surgery. (2020) 44(2):348–55. doi: 10.1007/s00268-019-05098-5
14. Au J, Alonso J, Kuan E, Arshi A, St John M. Primary squamous cell carcinoma of the thyroid: a population-based analysis. Otolaryngology: Head Neck Surgery. (2017) 157:25–9. doi: 10.1177/0194599817698436
15. Pezzolla A, Docimo G, Ruggiero R, Monacelli M, Cirocchi R, Parmeggiani D, et al. Incidental thyroid carcinoma: a multicentric experience. Recenti Prog Med. (2010) 101(5):194–8.
16. Ruggiero R, Gubitosi A, Conzo G, Gili S, Bosco A, Pirozzi R, et al. Sutureless thyroidectomy. Int J Surg. (2014) 12 Suppl 1:S189–193. doi: 10.1016/j.ijsu.2014.05.011
17. Torrez M, Braunberger RC, Yilmaz E, Agarwal S. Primary squamous cell carcinoma of thyroid with a novel BRAF mutation and High PDL-1 expression: A case report with treatment implications and review of literature. Pathol Res Pract. (2020) 216:153146. doi: 10.1016/j.prp.2020.153146
18. Liu G, Xu X, Chen G, Liu Z. Analysis of primary and secondary squamous cell carcinoma of the thyroid gland: a retrospective study. Gland Surg. (2021) 10:559–66. doi: 10.21037/gs-20-628
19. Hsieh ML, Besch BM, Peterson JEG, Henson C. Primary squamous cell carcinoma of the thyroid treated with concurrent chemoradiation and palliative immunotherapy: a case report. J Med Case Rep. (2022) 16:364. doi: 10.1186/s13256-022-03596-0
20. Chu MMH, Mirza O, Bishop PW, Pothula V. Primary squamous cell carcinoma of the thyroid gland successfully treated with surgical resection and adjuvant chemoradiotherapy. BMJ Case Rep. (2021) 14(3):e241209. doi: 10.1136/bcr-2020-241209
21. Lu Z, Lijun C, Dezhuan D, Hongyi C. Primary squamous cell carcinoma of the thyroid: A systematic review. Asian J Surg. (2022) 45:1016–7. doi: 10.1016/j.asjsur.2022.01.008
22. Ding W, Gao X, Ran X. Progress in diagnosing and treating thyroid squamous cell carcinoma under the 5th edition of WHO classification. Front Endocrinol (Lausanne). (2023) 14:1273472. doi: 10.3389/fendo.2023.1273472
23. Bishop J, Teruya-Feldstein J, Westra W, Pelosi G, Travis W, Rekhtman N. p40 (ΔNp63) is superior to p63 for the diagnosis of pulmonary squamous cell carcinoma. Modern Pathology. (2012) 25:405–15. doi: 10.1038/modpathol.2011.173
Keywords: squamous cell carcinoma of thyroid, thyroid tumor, subacute thyroiditis, misdiagnosis, prognosis
Citation: Yu Z, Tingting D, Jianyong Z and Yunsong P (2025) Repeated misdiagnosis of squamous cell carcinoma of the thyroid: a case report. Front. Oncol. 15:1551514. doi: 10.3389/fonc.2025.1551514
Received: 25 December 2024; Accepted: 30 January 2025;
Published: 18 February 2025.
Edited by:
Giuseppe Pannone, University of Foggia, ItalyReviewed by:
Ludovico Docimo, University of Campania Luigi Vanvitelli, ItalyCopyright © 2025 Yu, Tingting, Jianyong and Yunsong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhang Jianyong, emhhbmdqeTkyQDEyNi5jb20=; Peng Yunsong, cHlzQG1haWwudXN0Yy5lZHUuY24=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.