- 1Department of Stomatology, Zhuhai Hospital of Integrated Traditional Chinese and Western Medicine, Zhuhai, China
- 2Department of Epidemiology and Health Statistics, Xiangya School of Public Health, Central South University, Changsha, China
- 3School of Public Health, Jiangxi Provincial Key Laboratory of Preventive Medicine, Nanchang University, Nanchang, China
- 4Nursing Department, Xiangtan Central Hospital, Xiangtan, China
Background: Lip and oral cavity cancer (LOC) is one of the common malignant tumors of the head and neck, posing significant health and economic burdens. The BRICS, including Brazil, Russia, India, China, and South Africa, represent a large global population, presenting unique public health challenges. This study aims to evaluate the epidemiological trends and variations in the burden of LOC across BRICS in a timely manner.
Methods: Data on the number, all-age rate, age-standardized rate, and relative change in LOC incidence from 1992 to 2021 within BRICS were obtained from the Global Burden of Disease study (GBD) 2021, and we analyzed global and BRICS-specific LOC incidence trends over 30 years. Furthermore, age-period-cohort model was applied to estimate net drift, local drift, age, period and cohort effects between 1992 and 2021.
Results: In 2021, the BRICS nations reported 194.74 thousand new LOC cases, constituting 46.2% of the global total. From 1992 to 2021, all BRICS countries witnessed a significant rise in LOC cases, with China leading at 259.06%. The age-standardized incidence of LOC increased by over 20% in the Russian Federation, India, and China, while Brazil and South Africa exhibited marginal changes (Brazil: 0.75%; South Africa: -7.87%). Rising LOC trends were prevalent across most age groups in China, India, and the Russian Federation, particularly affecting older adults (60-94 years). Age, period, and cohort effects were deteriorating in China and India, contrasting with improvements in Brazil and South Africa.
Conclusion: LOC incidence has increased across BRICS, with temporal trends not consistently aligning with economic growth and exhibiting significant variation among countries. Brazil’s experience highlights the efficacy of oral health and tobacco control measures in mitigating LOC, especially in fast-developing nations. Prevention should target men and elderly in China and India, and women in other areas.
Introduction
Lip and oral cavity cancer (LOC) is a type of squamous cell carcinoma of the head and neck, which is one of the common malignant tumors of the head and neck, usually occurring on the lips, tongue, gums, floor of the mouth, upper and lower jaws (1). The Global Burden of Disease (GBD) 2019 study indicates that the number of Disability-Adjusted Life Years (DALYs) attributable to lip and oral cancer reached 5.51 million person-years in 2019, ranking 13th in the global malignant tumor burden of disease parity, resulting in an estimated 370,000 new cases and 199,000 deaths in 2019 (2, 3). Although the mortality and disease burden of LOC are not high in the total cancer population, the quality of life of those who survive is significantly reduced due to the severe impact on eating (4). Furthermore, there is a notable geographical variation in the incidence of oral cancer, with the situation being particularly critical in low- and middle-income countries in comparison to high-income countries (5).
Brazil, Russian Federation, India, China and South Africa (BRICS) were grouped together due to their fast-growing economies and their collective population accounting for nearly half of the global total (6). All BRICS countries are high-burden countries for LOC disease, with DALYs in BRICS countries exceeding half of the global LOC burden (7). Previous studies have tracked the global LOC burden and assessed global LOC incidence trends over time, but few studies have analyzed LOC incidence trends in the BRICS countries (3, 8). Studies on the incidence of LOC have been conducted in Brazil and China, providing information on the incidence of LOC in the BRICS countries (9–11). However, these studies were not exhaustive in terms of the countries included and comparisons between BRICS countries were not made. Given the widely recognized link between economic prosperity and improved health widely recognized, many policymakers view the BRICS countries as pivotal for altering global health as their economies grow rapidly (12). It is therefore of great importance to regularly assess, update and compare LOC incidence within the BRICS countries and to evaluate their progress in LOC prevention and treatment. The BRICS countries and other high-burden countries require this information to inform the allocation and strategic adjustment of healthcare resources.
The aim of this study was to analyze the incidence of LOC in the BRICS countries from 1992 to 2021, visualized by age, sex and year, providing an up-to-date epidemiological overview of LOC in the BRICS countries. Subsequently, the impact of age, period and birth cohort on changes in LOC incidence over the past 30 years was further assessed using the age-period-cohort (APC) model. The findings of this study therefore represent a significant addition to the existing evidence on the burden of LOC in the BRICS countries, providing valuable insights into healthcare resource allocation and future health policy formulation.
Method
Data sources
The data used in this study were obtained from GBD 2021 public dataset, which can be accessed at the Global Health Data Exchange GBD Results Tool (https://ghdx.healthdata.org/gbd-2021). GBD 2021 provides multilevel data on the burden of disease for 371 diseases and injuries in 204 countries and territories around the world, covering the most comprehensive burden of disease, risk, death and disease-related disability on health, and is the most important database for understanding the global burden of disease (7, 13, 14). GBD 2021 includes several significant updates: 19,189 new DALY data sources, 12 new causes, and various methodological improvements. Additionally, it incorporates the impact of the COVID-19 pandemic on the burden of disease (7).
In GBD 2021, LOC is defined according to the International Classification of Diseases, 9th edition (ICD-9): 140-145.9, 210.0-210.6, 235.0 and 10th edition (ICD-10): C00-C08.9, D10.0-D10.5, D11-D11.9 (14). In this study, we extracted estimates of LOC incidence from GBD 2021 by sex (female, male, and both), age (0-94 years), and year (since 1992) for the BRICS countries from 1992 to 2021. The 95% uncertainty intervals (UIs) were obtained by replicating the sample 1000 times, with upper and lower bounds determined by the 2.5th and 97.5th percentiles of the uncertainty distribution (7). Methodological information and details of the modelling strategy for GBD 2021 have been published elsewhere (7, 13, 14). The relevant data were anonymized and publicly available, and the informed consent waiver was reviewed and approved by the University of Washington Institutional Review Board.
Statistical analysis
Descriptive analysis of LOC incidence
This study provides a statistical description of the incidence characteristics of LOC in the BRICS countries from 1992 to 2021. It examines the epidemiological characteristics and trends of LOC within the BRICS countries by analyzing the incidence across different sex and age groups.
Age−period−cohort modelling analysis of incidence data
The APC modeling is a common statistical tool for extracting information hidden in epidemiological results. It analyzes disease risk and explores influencing factors in terms of age, period and cohort dimensions to extract and reveal possible information about disease patterns (15, 16). In this study, the age-period-cohort model with Intrinsic Estimator (IE) method was used to assess the independent effects of age, period and birth cohort on LOC incidence. Age, period, and cohort effects were calculated via Poisson regression, expressed as follows:
where represents the response variable of the net effect on LOC incidence for group ; and represent the number of incidences and the population at risk, respectively. , , and represent the coefficients of age, period, and birth cohort of the APC model, respectively. represents the intercept of the model.
In the APC model, the results of the model provide several important indicators: net drift, local drift, longitudinal age curve, period relative risk (RR) and cohort relative risk. Net drift, which represents the log-linear trend by period and cohort for the whole population; local drift, which represents the log-linear trend by period and cohort for each age group; longitudinal age curve, which represent the expected age-specific rates in the reference cohort adjusted for period effects; and period (or cohort) RR, which represents the RR of the population across different periods (or cohorts) adjusted for both age and cohort (or period) (17).
The APC model required that the age group data and the period group data be structured in the same manner. We therefore grouped the LOC incidence, population data according to the following rules. Age group: the total population was divided into 16 age groups at 5-year intervals: 15-19 years to 90-94 years. Period group: This was divided into 6 consecutive 5-year periods, from 1992-1996 (median 1994) to 2017-2021 (median 2019). Birth cohort group: birth cohort was calculated as period - age, divided into 21 consecutive birth cohorts (from 1900-1904 to 2000-2004). In the APC model of this study, the period (2002-2006) and the birth cohort (1950-1954) were used as reference groups for calculating the RR. When the RR value is greater (less) than 1, it indicates that the risk of LOC incidence is increased (decreased). We obtained estimated parameters using APC analyses with the age-period-cohort web tool designed by the National Cancer Institute and plotted using the R statistical program (version 4.2.3). To test the significance of evaluable parameters and functions, the Wald χ2 test was used, and all statistical tests were two-sided.
The study is reported according to Strengthening the Reporting of Observational Studies in Epidemiology criteria, and a checklist is provided as online appendix material.
Result
Incidence of lip and oral cavity cancer trends from 1992 to 2021
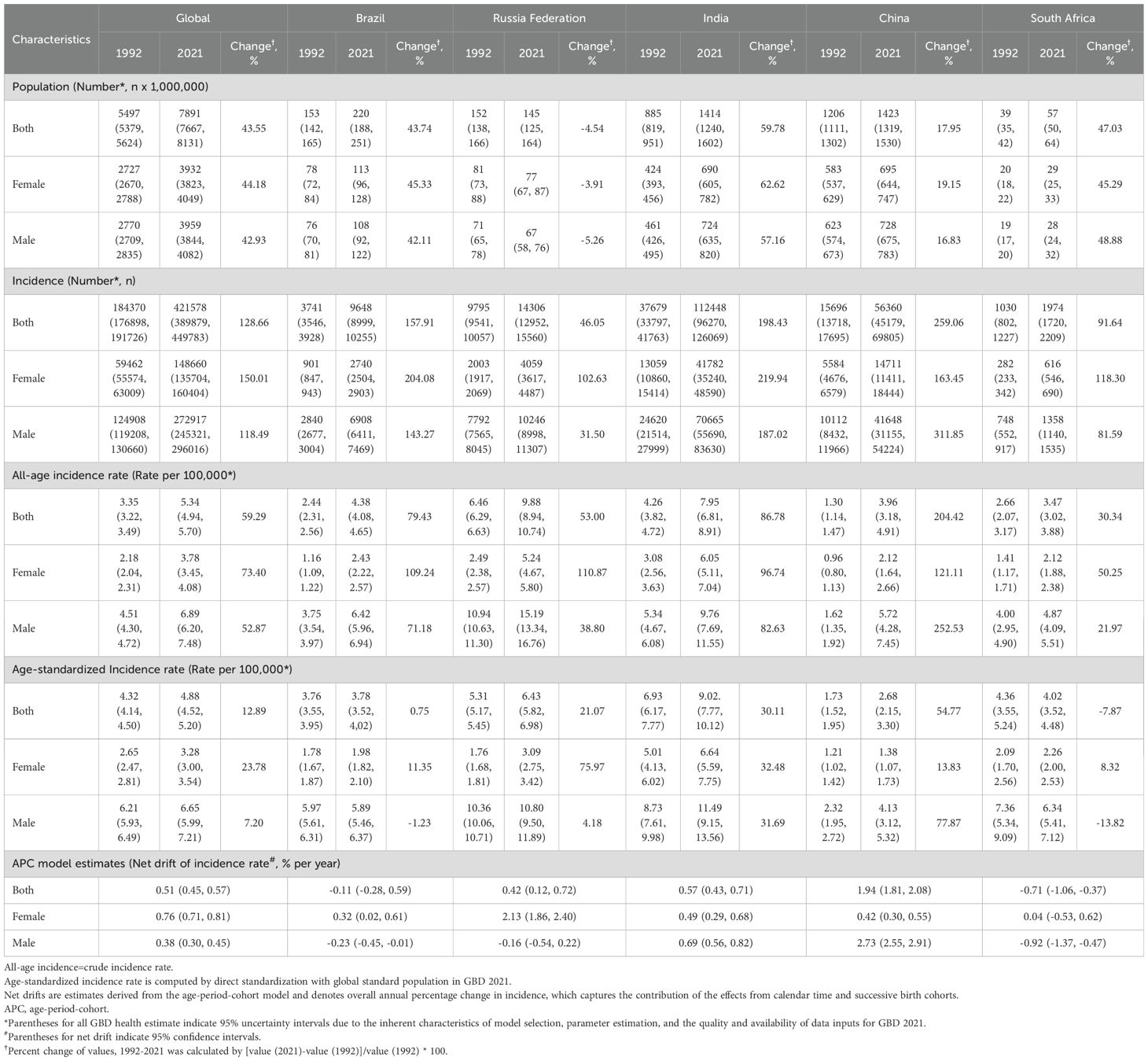
Table 1 shows the population, total incidence, all-age incidence rate, age-standardized incidence rate, and net drift of incidence for the world and BRICS countries. In 2021, there were 421.58 thousand (95% UI 389.88, 449.78) global LOC cases, with BRICS countries accounting for 194.74 thousand cases, or 46.2% of the total. Over the past 30 years, LOC incidence has increased significantly in all BRICS countries, with China experiencing the highest growth at 259.06%. India led in LOC cases with 112.45 thousand (95% UI 96.27, 126.07) cases.
From 1992 to 2021, the global all-age LOC incidence rate rose from 3.35 (95% UI 3.22, 3.49) per 100,000 to 5.34 (95% UI 4.94, 5.70) per 100,000, a 59.29% increase. All BRICS countries, excluding South Africa and Russia Federation, experienced incidence rate increases above the global average, with China’s rate showing the highest increase at 204.42%. Despite this high growth, China’s incidence rate did not lead; Russian Federation had the highest incidence rate in 2021 at 9.88 (95% UI 8.94, 10.74) per 100,000. Over the past 30 years, the global age-standardized incidence rate increased by 12.89%. In the BRICS countries, Russian Federation, India, and China saw higher increases in age-standardized rates than the global average, while South Africa experienced a decrease of 7.87%. The APC model’s net drift estimates also indicated rising incidence rates in Russian Federation, India, and China, with China having the highest annual increase at 1.94% (95% CI 1.81%, 2.08%).
Time trends in lip and oral cavity cancer incidence across different age groups
Figure 1A shows the annual percentage change in LOC incidence rates for each 5-year age group from 15 to 94 years. Globally, most age groups have local drift values above 0, with females generally having higher local drift values than males. Among the BRICS countries, China, India, and Russian Federation show positive local drift values for most age groups, indicating increasing LOC incidence rates. In South Africa, nearly all age groups have negative local drift values, suggesting a decline in incidence rates. Regarding gender differences, females in Brazil and Russian Federation typically have higher local drift values than males. In China, males have consistently higher local drift values across all age groups. In India and South Africa, males have higher local drift values in younger age groups, while females have higher values in older age groups.
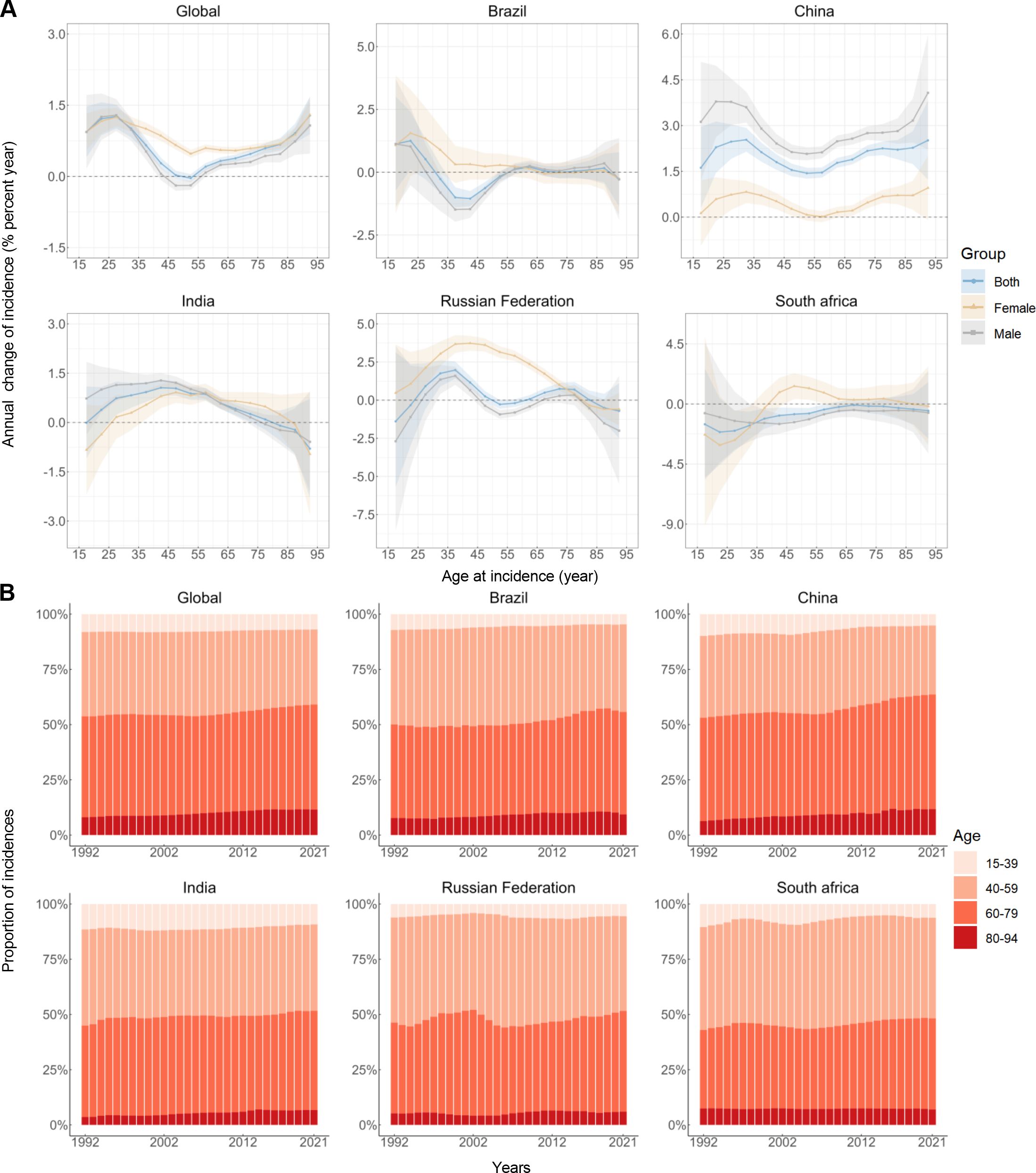
Figure 1. Local drifts of incidence rate and age distribution of incidences in global and BRICS, 1992–2021. (A) Local drifts of lip and oral cavity cancer incidence rate (estimates from age-period-cohort models) for 16 age groups (15-19 to 90-94 years), 1992–2021. The dots and shaded areas indicate the annual percentage change of incidence rate (% per year) and the corresponding 95% CIs. (B) Temporal change in the relative proportion of lip and oral cavity cancer incidences across age groups (15-39, 40-59, 60-79, 80-94 years), 1992–2021.
Figure 1B illustrates the temporal trends in LOC cases by age group. In 1992, 53.73% of global LOC cases occurred in individuals aged 60 and above; by 2021, this proportion increased to 59.05%. A similar pattern of increasing LOC cases among the elderly (60-94 years) was observed in all BRICS countries, with China showing the highest increase from 53.09% to 63.61%. Additionally, except for South Africa, the main affected age group in these countries has shifted from middle-aged to younger elderly individuals (60-79 years). Between 2019 and 2021, the proportion of LOC cases in the very elderly population decreased in Brazil, China, and South Africa.
Age, period and cohort effects on lip and oral cavity cancer incidence
Figure 2 presents the estimated age, period, and cohort effects for the world and BRICS countries. Overall, a similar age effect pattern is observed in all countries except Russian Federation, with risk increasing as age increases. Notably, China’s male incidence rates rise sharply in old age. In Russian Federation, male risk decreases rapidly after age 60-64, while female risk continues to rise, unlike in other countries. Gender differences in age effects are seen in all BRICS countries, with males having higher risks than females (Figure 2A).
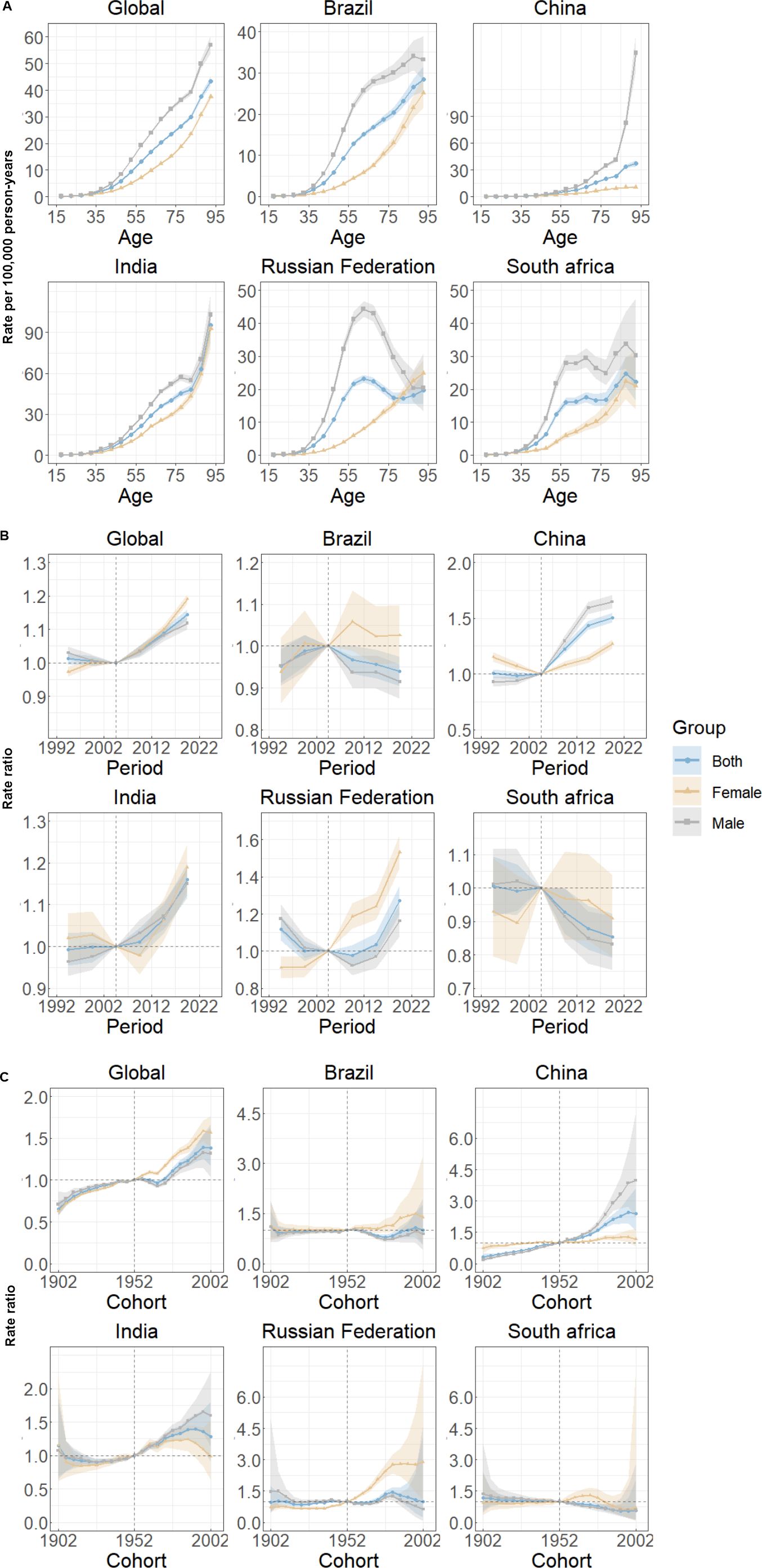
Figure 2. Age, period and cohort effects on lip and oral cavity cancer incidence in global and BRICS. (A) Age effects are shown by the fitted longitudinal age curves of incidence rate (per 100,000 person-years) adjusted for period deviations. (B) Period effects are shown by the relative risk of incidence rate (incidence rate ratio) and computed as the ratio of age-specific rates from 1992–1996 to 2017–2021, with the referent cohort set at 2002–2005. (C) Cohort effects are shown by the relative risk of incidence rate and computed as the ratio of age-specific rates from the 1902 cohort to the 2002 cohort, with the referent cohort set at 1952. The dots and shaded areas denote incidence rates or rate ratios and their corresponding 95% CIs.
Over the past 30 years, the period effects for the world, China, and India show a similar “J” shape, with risk increasing and remaining above 0 after 2004. In Brazil and South Africa, period effects continuously decline, indicating effective control of LOC incidence rates over time. In Russian Federation, period effects show a “U” shape, with risk decreasing initially and then rising. Gender differences in period effects are evident, with distinct regional characteristics (Figure 2B).
Cohort effects over the past 30 years show that for the world, China, and India, the risk increases for individuals born after 1900. In Brazil, Russian Federation, and South Africa, cohort effects remain relatively stable, with a slight decline in South Africa for cohorts born after 1950-1954. Gender differences in cohort effects are also present, with China and India showing similar patterns, and Brazil, Russian Federation, and South Africa exhibiting another pattern (Figure 2C).
Discussion
LOC is a low mortality cancer with a high survival rate if detected and treated early. However, surgery as the primary treatment modality leads to changes in facial morphology and difficulties in chewing and swallowing, which contributes to some extent to the disability burden of patients with LOC (1). Controlling LOC incidence is crucial for reducing its disease burden. Over the past three decades, despite significant advances in diagnosis and treatment of LOC (18, 19), global incidence and age-standardized incidence rates have continued to rise.
A marked heterogeneity exists in the incidence and long-term trends of LOC across the BRICS nations. Notably, the Russian Federation, India, and China each witnessed a surge exceeding 50% in the crude incidence of LOC between 1992 and 2021. Upon adjusting for variations in age distribution, the age-standardized incidence of LOC in these countries has still escalated by over 20% during the past three decades. This persistent increase implies the presence of additional, fundamental factors that are driving the observed rise in LOC incidence, beyond the influence of demographic shifts alone. China and India have experienced a significant increase in population over the past three decades (20), and this demographic expansion has been a significant contributing factor to the rise in the number of local LOC incidents. Local drift indicates that the incidence of LOC is increasing at a faster rate in all age groups in China, specifically among those aged 25-59 in India, and 25-45 in Russian Federation. Currently, both China and the Russian Federation are grappling with rapid population aging, contrasting with India’s youthful demographic profile (20). The combination of demographic changes and high risk of incidence in specific age groups will result in continued growth in the incidents and incidence of LOC in China and India. Between 1992 and 2021, LOC age-standardized incidence in Brazil and South Africa did not change much (Brazil: 0.53%, South Africa: -7.80%), but crude incidence increased. Local drift suggests that the incidence in most age groups has not maintained its growth and has even declined. The risk of LOC varies significantly among the BRICS countries, reflecting the influence of cultural practices, socioeconomic conditions, and healthcare systems. Tobacco use, alcohol consumption, betel nut chewing, and Human papillomavirus (HPV) infection are well-recognized risk factors for LOC (21), though their relative impact differs across regions due to variations in lifestyle, public health policies, and access to healthcare services. To further understand the factors influencing LOC incidence in these regions, we examined age, period, and cohort effects.
In Brazil, the age effect contributed to an increase in oral cancer incidence, while the period and cohort effects demonstrated positive trends, reflecting the country’s commendable progress in healthcare improvements and effective control of key risk factors. The National Oral Health Policy (PNSB) in Brazil prioritizes prevention and early diagnosis of oral cancer. Since its implementation in 2004, access and continuity of oral health services have improved through the expansion of Primary Health Care, the use of oral health teams (OHT) in the Family Health Strategy, and the establishment of Specialized Dental Care Centers for early diagnosis and treatment of LOC patients (22, 23). Tobacco exposure is the largest and recognized contributor to LOC (24). A 2019 report by the World Health Organization (WHO) highlights Brazil’s success in tobacco control under the guidance of the Framework Convention on Tobacco Control (25). Brazil has benefited greatly from PNSB programs and tobacco restrictions.
The decline in period and cohort effects in South Africa may reflect advancements in local tobacco regulation and lifestyle changes. Since 1993, South Africa has implemented strict tobacco control policies, including bans on tobacco advertising, restrictions on public smoking, increases in cigarette excise taxes, and health education programs (26). These measures have significantly reduced cigarette consumption, with a 54% decrease in per capita cigarette consumption recorded between 1999 and 2011 (27). In addition, efforts to manage South Africa’s high prevalence of HIV have indirectly strengthened the healthcare system, enabling the development of cancer prevention strategies. However, the healthcare system and public health response to LOC remain weak, as the primary focus has been on HIV prevention and treatment. The high prevalence of HPV—affecting more than 17% of women—and inadequate vaccination coverage exacerbate the risk of HPV-associated oral cancers, particularly in women (28). This may explain the higher risk of developing LOC in women compared to men. Looking ahead, increased investment in cancer prevention strategies and improved efforts to prevent HPV infection, such as expanding vaccination programs, are critical areas where South Africa can focus to reduce the burden of LOC.
In China and India, age, period and cohort effects all contributed to the increase in incidence, with China experiencing the highest incidence increase ratio among the BRICS countries (204.62%) and India the second highest (86.78%). The age effect suggests that in both countries, the risk of LOC incidence is highest in the elderly age groups (>80 years), much higher than in the other BRICS countries. Physical and cognitive decline in the elderly population can lead to difficulties in routine oral care and reduced access to oral care services, which in turn may exacerbate the risk of LOC incidence (29). A systematic review demonstrated that socio-economic inequality is associated with the risk of oral cancer (30). Elderly individuals in the older age groups in China and India often experience extreme poverty, which may explain the high incidence of LOC in these regions. Current dental care systems are costly and fundamentally inadequate for low-income countries to address the ongoing challenges. Countries facing these issues should emphasize the importance of educating populations on proper hygiene practices, which could yield significant public health benefits in the future. Period and cohort effects in both China and India exhibit a ‘J’-shaped trend, indicating a continued rise in the risk of developing LOC. Although a range of public health interventions have been initiated locally, including, tobacco control, limiting alcohol consumption and publicizing the human harms of betel nut chewing, the sustained effectiveness of these measures may not yet be fully realized. Anti-tobacco initiatives have faced challenges in coverage and implementation, with lifestyle inertia posing a significant barrier to achieving long-term gains. For instance, China, which accounts for over 44% of global tobacco consumption, has yet to implement a national smoke-free law (31). In India, male smoking rates tripled between 1998 and 2010 (32). Additionally, betel nut—a World Health Organization classified Group 1 carcinogen—is widely consumed in both countries, leading to severe health consequences (33). Men face a higher risk of developing LOC compared to women, largely due to sociocultural factors. Men are more likely to engage in smoking, alcohol consumption, and betel nut chewing, behaviors that significantly elevate their LOC risk. These findings align with previous research (34).
The Russian Federation was the only country where the age effect was reversed, although only in the male cohort. The period effect and the cohort effect suggested a higher risk of incidence in women. The decline in the age effect for men after 60-64 could be linked to their lower life expectancy. In Russian Federation, where men’s life expectancy rarely exceeds 64 years (14), those who have experienced LOC exposure may have died prematurely. The high risk of LOC development in women has been observed in other studies (35), and the age-standardized increase in smoking prevalence in women may be important, with smoking prevalence in middle-aged women consistently increasing, while smoking prevalence in younger women has been trending downwards, which may explain the characteristics of the female period and cohort effect.
Despite rapid economic growth in the BRICS countries, the period and pace of development vary, leading to differing trends in LOC incidence. Moreover, unique cultural practices and health policies across these nations contribute to region-specific risk factors and areas requiring intervention. However, it is important to acknowledge that successful strategies implemented in one country can offer valuable insights for other regions in reducing the burden of LOC. Brazil’s experience highlights significant gains through the implementation of PNSB and tobacco control, serving as a model for other countries. The cases of South Africa, China, India, and Russia Federation indicate the need for targeted strategies for high-risk groups within the LOC population. The World Health Assembly 2021 resolution on oral health promotes developing a global strategy to achieve universal oral health coverage by 2030 (3). Positive health policy and public health actions may significantly improve LOC prevention and treatment outcomes globally.
To the best of our knowledge, this is the first study to investigate time trends in LOC incidence in the BRICS countries using the latest GBD 2021 data, providing comprehensive coverage of periods and populations. This study also uniquely applies an APC model to examine trends, allowing us to capture important shifts in specific populations and provide targeted recommendations. This study also has some limitations, and the availability and quality of raw data is a limiting factor in estimating LOC incidence data. When high-quality or accessible LOC data from national or local cancer registries were not available, there was some discrepancy in the GLOBOCAN and GBD estimates of LOC (36), although this discrepancy in estimates was not large in the BRICS countries, which underscores the importance of expanding cancer and vital registration systems. Additionally, the GBD study did not stratify LOC, which included various anatomical site cancers with differing pathophysiological determinants, such as cancers of the lip and other parts of the oral cavity. Future studies could improve accuracy by separating LOC into specific categories based on anatomical sites.
Conclusion
Between 1992 and 2021, the incidence of LOC has risen in the BRICS nations, with trends not aligning proportionally with socioeconomic advancement. Despite shared economic growth, regional variability in LOC incidence persists. Brazil’s experience suggests that implementing oral health programs and strong tobacco control measures can mitigate LOC incidence. Rapidly developing economies can benefit from similar efforts. Preventive strategies must prioritize at-risk populations, emphasizing men and the elderly in China and India, and increasing vigilance for women’s susceptibility in other countries.
Data availability statement
Publicly available datasets were analyzed in this study. The datasets generated during and/or analyzed during the current study are available in the GBD Data Tool repository (http://ghdx.healthdata.org/gbd-results-tool). This public link to the database of GBD study is open, and the use of data does not require additional consent from IHME.
Author contributions
ZY: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. YW: Conceptualization, Data curation, Formal analysis, Software, Writing – review & editing. YC: Formal analysis, Methodology, Writing – review & editing. PC: Conceptualization, Data curation, Investigation, Project administration, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Special Science and Technology Major Project of Hunan Province (grant number: Z2023146).
Acknowledgments
Thanks to the IHME and the Global Burden of Disease study 2021 collaborations.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Screening, P. D. Q, B. Prevention Editorial. Oral cavity, oropharyngeal, hypopharyngeal, and laryngeal cancers prevention (PDQ®): health professional version. In: PDQ Cancer Information Summaries. National Cancer Institute (US, Bethesda (MD (2024).
2. Kocarnik JM, Compton K, Dean FE, Fu W, Gaw BL, Harvey JD, et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: A systematic analysis for the global burden of disease study 2019. JAMA Oncol. (2022) 8:420–44. doi: 10.1001/jamaoncol.2021.6987
3. Cunha ARD, Compton K, Xu R, Mishra R, Drangsholt MT, Antunes JLF, et al. The global, regional, and national burden of adult lip, oral, and pharyngeal cancer in 204 countries and territories: A systematic analysis for the global burden of disease study 2019. JAMA Oncol. (2023) 9:1401–16. doi: 10.1001/jamaoncol.2023.2960
4. Høxbroe Michaelsen S, Grønhøj C, Høxbroe Michaelsen J, Friborg J, von Buchwald C. Quality of life in survivors of oropharyngeal cancer: A systematic review and meta-analysis of 1366 patients. Eur J Cancer. (2017) 78:91–102. doi: 10.1016/j.ejca.2017.03.006
5. Shrestha AD, Vedsted P, Kallestrup P, Neupane D. Prevalence and incidence of oral cancer in low- and middle-income countries: A scoping review. Eur J Cancer Care (Engl). (2020) 29:e13207. doi: 10.1111/ecc.13207
6. Zou Z, Liu G, Hay SI, Basu S, Belgaumi UI, Dhali A, et al. Time trends in tuberculosis mortality across the BRICS: an age-period-cohort analysis for the GBD 2019. EClinicalMedicine. (2022) 53:101646. doi: 10.1016/j.eclinm.2022.101646
7. Collaborators, G. D. a. I. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2133–61. doi: 10.1016/S0140-6736(24)00757-8
8. Du M, Nair R, Jamieson L, Liu Z, Bi P. Incidence trends of lip, oral cavity, and pharyngeal cancers: global burden of disease 1990-2017. J Dent Res. (2020) 99:143–51. doi: 10.1177/0022034519894963
9. Lima IAB, Almeida RJL, Pontes-Silva A, Ribeiro BF, Figueiredo F, Quaresma FRP, et al. Epidemiological study on the lip and oral cavity cancer in Brazil: connecting science and clinical applicability. Rev Assoc Med Bras (1992). (2022) 68:1337–41. doi: 10.1590/1806-9282.20220806
10. Romagna DV, Oliveira MM, Abreu LG, Stein C, Hugo FN, Teixeira R, et al. Incidence and mortality rates of lip, oral cavity, and pharynx cancers in Brazil: time-trend and age-period-cohort analysis from the last 30 years, Global Burden of Disease Study. Rev Soc Bras Med Trop. (2022) 55:e0286. doi: 10.1590/0037-8682-0286-2021
11. Zhang J, Lu Y, Li H, Zhang N, He R, Zhang R, et al. Lip and oral cavity cancer burden and related risk factors in China: estimates and forecasts from 1990 to 2049. Healthcare (Basel). (2022) 10:1611. doi: 10.3390/healthcare10091611
12. Sahoo PM, Rout HS, Jakovljevic M. Future health expenditure in the BRICS countries: a forecasting analysis for 2035. Global Health. (2023) 19:49. doi: 10.1186/s12992-023-00947-4
13. Collaborators, G. C. o. D. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2100–32. doi: 10.1016/S0140-6736(24)00367-2
14. Collaborators, G. D. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950-2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:1989–2056. doi: 10.1016/S0140-6736(24)00476-8
15. Yang Y. Socail inequalities in happiness in the United States, 1972 to 2004: An age-period-cohort analysis. Am Sociological Rev. (2008) 73:204–26. doi: 10.1177/000312240807300202
16. Cao Y, Chen S, Chen X, Zou W, Liu Z, Wu Y, et al. Global trends in the incidence and mortality of asthma from 1990 to 2019: An age-period-cohort analysis using the global burden of disease study 2019. Front Public Health. (2022) 10:1036674. doi: 10.3389/fpubh.2022.1036674
17. Fan L, Wu Y, Wei J, Xia F, Cai Y, Zhang S, et al. Global, regional, and national time trends in incidence for migraine, from 1990 to 2019: an age-period-cohort analysis for the GBD 2019. J Headache Pain. (2023) 24:79. doi: 10.1186/s10194-023-01619-9
18. Pulte D, Brenner H. Changes in survival in head and neck cancers in the late 20th and early 21st century: a period analysis. Oncologist. (2010) 15:994–1001. doi: 10.1634/theoncologist.2009-0289
19. Harris MS, Phillips DR, Sayer JL, Moore MG. A comparison of community-based and hospital-based head and neck cancer screening campaigns: identifying high-risk individuals and early disease. JAMA Otolaryngol Head Neck Surg. (2013) 139:568–73. doi: 10.1001/jamaoto.2013.3153
20. United Nations. (2022). World Population Prospects 2022. Available online at: https://www.un.org/development/desa/pd/content/World-Population-Prospects-2022 (Accessed May 17, 2024).
21. Kumar M, Nanavati R, Modi TG, Dobariya C. Oral cancer: Etiology and risk factors: A review. J Cancer Res Ther. (2016) 12:458–63. doi: 10.4103/0973-1482.186696
22. Pucca GA Jr., Gabriel M, de Araujo ME, de Almeida FC. Ten years of a national oral health policy in Brazil: innovation, boldness, and numerous challenges. J Dent Res. (2015) 94:1333–7. doi: 10.1177/0022034515599979
23. Cunha ARD, Prass TS, Hugo FN. Mortality from oral and oropharyngeal cancer in Brazil: impact of the National Oral Health Policy. Cad Saude Publica. (2019) 35:e00014319. doi: 10.1590/0102-311x00014319
24. Hashim D, Genden E, Posner M, Hashibe M, Boffetta P. Head and neck cancer prevention: from primary prevention to impact of clinicians on reducing burden. Ann Oncol. (2019) 30:744–56. doi: 10.1093/annonc/mdz084
25. Flor LS, Reitsma MB, Gupta V, Ng M, Gakidou E. The effects of tobacco control policies on global smoking prevalence. Nat Med. (2021) 27:239–43. doi: 10.1038/s41591-020-01210-8
26. Bello B, Fadahun O, Kielkowski D, Nelson G. Trends in lung cancer mortality in South Africa: 1995-2006. BMC Public Health. (2011) 11:209. doi: 10.1186/1471-2458-11-209
27. Winkler V, Mangolo NJ, Becher H. Lung cancer in South Africa: a forecast to 2025 based on smoking prevalence data. BMJ Open. (2015) 5:e006993. doi: 10.1136/bmjopen-2014-006993
28. De Vuyst H, Alemany L, Lacey C, Chibwesha CJ, Sahasrabuddhe V, Banura C, et al. The burden of human papillomavirus infections and related diseases in sub-saharan Africa. Vaccine. (2013) 31 Suppl 5:F32–46. doi: 10.1016/j.vaccine.2012.07.092
29. Patel J, Wallace J, Doshi M, Gadanya M, Ben Yahya I, Roseman J, et al. Oral health for healthy ageing. Lancet Healthy Longev. (2021) 2:e521–7. doi: 10.1016/S2666-7568(21)00142-2
30. Conway DI, Petticrew M, Marlborough H, Berthiller J, Hashibe M, Macpherson LM. Socioeconomic inequalities and oral cancer risk: a systematic review and meta-analysis of case-control studies. Int J Cancer. (2008) 122:2811–9. doi: 10.1002/ijc.v122:12
31. Bai R, Dong W, Chu M, Liu B, Li Y. Trends in mortality due to tracheal, bronchial, and lung cancer across the BRICS: An age-period-cohort analysis based on the Global Burden of Disease Study 1990-2019. Chin Med J (Engl). (2024) 137:2860–7. doi: 10.1097/CM9.0000000000002977
32. Mishra S, Joseph RA, Gupta PC, Pezzack B, Ram F, Sinha DN, et al. Trends in bidi and cigarette smoking in India from 1998 to 2015, by age, gender and education. BMJ Glob Health. (2016) 1:e000005. doi: 10.1136/bmjgh-2015-000005
33. Zhao X, Davey G. Areca nut use among a Chinese ethnic minority, and its health implications. Subst Use Misuse. (2020) 55:1519–24. doi: 10.1080/10826084.2019.1660676
34. Zhang LW, Li J, Cong X, Hu XS, Li D, Wu LL, et al. Incidence and mortality trends in oral and oropharyngeal cancers in China, 2005-2013. Cancer Epidemiol. (2018) 57:120–6. doi: 10.1016/j.canep.2018.10.014
35. Muntyanu A, Nechaev V, Pastukhova E, Logan J, Rahme E, Zubarev A, et al. Burden and geographic distribution of oral cavity and oropharyngeal cancers in the Russian Federation. Front Oncol. (2023) 13:1197287. doi: 10.3389/fonc.2023.1197287
Keywords: lip and oral cavity cancer, incidence, time trend, age-period cohort model, BRICS
Citation: Yu Z, Wu Y, Cao Y and Cheng P (2025) Epidemiological trends and age-period-cohort effects on lip and oral cavity cancer burden across the BRICS from 1992 to 2021. Front. Oncol. 15:1539417. doi: 10.3389/fonc.2025.1539417
Received: 04 December 2024; Accepted: 29 January 2025;
Published: 17 February 2025.
Edited by:
Jelena Milasin, University of Belgrade, SerbiaReviewed by:
Raziye Özdemir, Karabük University, TürkiyeBiljana Radosav Milicic, University of Belgrade, Serbia
Vitomir Konstantinovic, University of Belgrade, Serbia
Copyright © 2025 Yu, Wu, Cao and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhengrong Yu, MTgyOTYxNjk3MTdAMTYzLmNvbQ==
 Zhengrong Yu1*
Zhengrong Yu1* Yuhang Wu
Yuhang Wu Yu Cao
Yu Cao