
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol., 07 March 2025
Sec. Head and Neck Cancer
Volume 15 - 2025 | https://doi.org/10.3389/fonc.2025.1539070
This article is part of the Research TopicMultidisciplinary Management of Oral Cancer: Diagnosis, Treatment, and RehabilitationView all 7 articles
 Georg Hoene1*†‡
Georg Hoene1*†‡ Nikolaus von Hahn1†‡
Nikolaus von Hahn1†‡ Tim Mathea1‡
Tim Mathea1‡ Boris Schminke1‡
Boris Schminke1‡ Kathi Goldstein1‡
Kathi Goldstein1‡ Martin Leu2‡
Martin Leu2‡ Henning Schliephake1‡
Henning Schliephake1‡ Susanne Wolfer1‡
Susanne Wolfer1‡Background: The COVID-19 pandemic necessitated the widespread use of face masks in medical settings. In the treatment of patients with head and neck tumors or other malignancies, where non-verbal communication and emotional expression are critical, face masks may potentially impair the physician-patient relationship. This study aimed to assess the impact of face masks on perceived empathy and the quality of physician-patient communication in this patient cohort.
Methods: A prospective case-control study as part of the postoperative follow-up consultations was conducted at the Department of Oral and Maxillofacial Surgery, University Medical Center Goettingen, utilizing the Consultation and Relational Empathy (CARE) measure. Patients were divided into two groups: in the case group, clinicians wore face masks throughout the entire consultation, while in the control group, masks were worn only during the clinical examination. The primary outcome was the difference in CARE scores, reflecting the perceived empathy of the clinician.
Results: No significant difference in mean CARE scores was observed between the two groups (p=0.454), indicating that wearing a face mask did not significantly affect patients’ perception of clinician empathy. However, a significant positive correlation was found between patients’ familiarity with the clinician and higher CARE scores (p=0.003). Other variables, such as patient health status and consultation duration, did not significantly influence CARE scores.
Conclusion: Wearing face masks does not significantly impair perceived empathy in the context of physician-patient communication. Familiarity with the clinician emerged as a key factor in enhancing the quality of the interaction. These findings underscore the importance of fostering long-term, trust-based physician-patient relationships, particularly during periods of pandemic-related protective measures such as mask mandates.
Effective communication between physician and their patients is a fundamental aspect of clinical practice (1). Particularly the lower part of the face is of importance in terms of its role in the expression of emotions and moods (2, 3). The use of a face mask covering the entire lower face of the clinician has been shown to impair and distort the perception of certain emotions (4, 5). Additionally, wearing a face mask has been demonstrated to negatively impact communication, further complicating the physician-patient interaction (6, 7).
In response to the alarming rise in SARS-CoV-2 infection rates, the federal government enacted a nationwide mask mandate at the end of April 2020 in Germany (8). The wearing of a face mask constituted an essential component of the protection measures implemented in response to the Coronavirus, both in public spaces and in medical facilities. While medical face masks (such as surgical masks) serve primarily to protect others from the droplets of exhaled air produced by the wearer (external protection), particle-filtering half masks (such as FFP2 and FFP3 masks) are also capable of protecting the wearer from infection (self-protection) (9). Masks were a mandatory requirement at the Goettingen University Medical Center from the inception of the measures in April 2020 until April 2023. This was implemented with due diligence by both medical staff and patients (10).
The efficacy of face masks in preventing the transmission of SARS-CoV-2 has been substantiated by several studies (11–13) They demonstrated that the use of face masks can reduce the risk of infection with SARS-CoV-2 in medical staff by up to 70%. In contrast with the evidence supporting the efficacy of face masks, the requirement to wear them has been a topic of ongoing controversy and political debate (14). A number of factors have been identified as influencing the acceptance of mandatory face masks, including socioeconomic and psychological characteristics, risk perception of the pandemic, empathy, trust in healthcare professionals and political attitudes (15, 16).
The existing literature also identifies several adverse effects associated with mask wearing. These include voice fatigue (17), eye dryness (18), dermatological diseases (19), discomfort (20) and obstruction of oxygen exchange (21).
Furthermore, the use of face masks has been found to have a detrimental impact on interpersonal communication, which is a crucial aspect of the physician-patient relationship. Studies have indicated that wearing a face mask can impede understanding speech (22), diminish the quality of medical consultations (23) and impair emotion recognition accuracy as well as perceived closeness (6). The reduction in speech volume, the inability to lip-read, and the dampening of certain sound frequencies result in significant communication difficulties, particularly for patients with hearing loss. Additionally, the absence of visual cues further exacerbates these challenges, especially in noisy environments (24–26).
The facial region plays a pivotal role in the expression of emotions and moods. In terms of the recognition of different emotions, the existing literature indicates that the mouth region is of particular importance for the recognition of happiness, neutral expressions and anger (2, 3, 27). In their study, Tsantani et al. (2022) demonstrated that wearing a face mask results in a reduction in the perceived intensity of intended emotions and an increase in the perceived intensity of unintended emotions (5). In general, individuals tend to have greater difficulty correctly categorizing the emotions of mask wearers (28). The perception of the emotion anger is not influenced by the act of wearing a face mask (5, 29).
A distinctive instrument utilized in the assessment of patient-centered care is the Consultation and Relational Empathy (CARE) Measure. The instrument was developed in 2004 by Mercer and coworkers at the Departments of General Practice at the Universities of Glasgow and Edinburgh. It is a measuring instrument that records the clinicians clinical empathy from the patient’s perspective. The CARE questionnaire allows patients to assess the ‘human’ aspects of their consultations, offering direct feedback to clinicians on the strengths and weaknesses of their empathy. Its robust internal consistency and reliability have been validated across multiple languages and diverse clinical contexts. Built on a solid theoretical and empirical foundation, the questionnaire is applicable to a broad spectrum of diseases. As a result, our findings may be transferable to similar clinical settings, though additional validation is needed (30, 31). It has since been translated into numerous languages and utilized in diverse countries (32–38). This study employs the German version of the questionnaire, as presented by Neumann et al. (2008). Its robust internal consistency and reliability have been widely acknowledged and confirmed across different languages and clinical contexts.
In the studies conducted by Mercer and colleagues, the original version of the CARE questionnaire demonstrated high internal consistency, with Cronbach’s alpha coefficients ranging from 0.92 to 0.94 (30). Other authors have reported a higher internal consistency with a Cronbach’s alpha of 0.97 in their translated version (36, 38). Effective differentiation between the various clinicians is possible with only 15 to 20 patient ratings per clinician, provided that interrater reliability exceeds 0.8 (33).
In contrast to other measurement instruments, the CARE questionnaire is distinguished by its provision of additional explanations of specific clinician behaviors to respondents, utilizing synonymous and antonymous definitions (32).
Face masks are a critical component of infection control in oral and maxillofacial surgery, particularly during high-risk procedures, where minimizing transmission risks is paramount. Despite their clinical importance, limited research has examined their potential impact on physician-patient communication within this specialized setting. This study specifically aimed to assess whether wearing face masks influences the quality of communication and perceived empathy in patients with head and neck cancer. To the best of our knowledge, this represents the first investigation addressing these factors in the context of oral and maxillofacial surgery, thus filling a significant gap in the existing literature.
This prospective, single-center case-control study was conducted at the Department of Oral and Maxillofacial Surgery, University Medical Center Goettingen, between November 14, 2023, and April 9, 2024, as part of postoperative follow-up consultations. The sample size calculation was based on key parameters from Mercer et al. (2005) and Mercer et al. (2011), which demonstrated the high internal consistency of the CARE questionnaire (Cronbach’s alpha 0.92–0.94) and its effectiveness in differentiating clinicians with 15–20 patient ratings per clinician (interrater reliability > 0.8) (31, 33). Using G*Power software (v. 3.1.9.6; University of Düsseldorf), the required minimum sample size was determined to be 122 patients (61 per group) based on a significance level of 0.05, a power of 0.95, and an effect size of 0.6.
Inclusion criteria comprised adult patients aged 18 years or older with the capacity to provide informed consent, undergoing postoperative follow-up consultations. Exclusion criteria included severe cognitive impairments, language barriers, or physical disabilities (e.g., vision or hearing loss) that could hinder study participation. Both groups included patients with tumors in the oral cavity, oropharynx, nasopharynx, hypopharynx, or facial region.
Patients were manually assigned to the case or control group in a structured manner using an alternating and consecutive method to ensure balanced distribution and minimize bias. In the case group, clinicians wore face masks throughout the entire consultation. In the control group, masks were used only during the direct clinical examination, adhering to standard practices for procedural sterility (hygiene), protection of vulnerable individuals from pathogen transmission (patient protection), and the broader reduction of infection spread within the clinical environment (infection control). This allocation approach ensured comparability between the groups while reflecting real-world clinical settings.
Clinical and pathological data were extracted from digital medical records to support exploratory analyses. Parameters included patient age, gender, tumor location, TNM stage, recurrence status, and surgical therapy. Additionally, clinician-related data, such as gender and mask usage, were documented.
The study employed the German version of the Consultation and Relational Empathy (CARE) questionnaire, originally developed by Mercer et al. (2004) and translated by Neumann et al. (2008) (30, 32). The CARE questionnaire consists of ten items, rated on a 5-point Likert scale (strongly disagree to strongly agree), designed to measure the quality of consultations in terms of empathy, communication, and relational aspects. No modifications were made to the original instrument for this study.
The questionnaire was administered by a single interviewer to ensure consistency, and patient responses were anonymized to maintain confidentiality. After receiving an oral explanation of the study, patients signed an informed consent form. Responses were recorded either manually on paper and later digitized or directly via tablet or smartphone using a QR code. The questionnaire comprised three sections: (1) health status over the past two weeks, familiarity with the clinician, consultation duration, and face mask usage; (2) general attitudes and acceptance of face masks; and (3) feedback on consultations conducted with or without masks.
The study was conducted in accordance with the tenets of the Declaration of Helsinki and reviewed and approved by a local ethics committee (vote number 33/8/23).
The statistical analysis was conducted using R (version 4.3.1; R Core Team, 2024). Since the Shapiro-Wilk test indicated that the data did not follow a normal distribution, the Mann-Whitney U test was used for group comparisons. Multiple linear regression analysis was performed to evaluate the relationships between independent variables (IVs) and the dependent variable (mean CARE scores), ensuring compliance with Gauss-Markov assumptions.
To enable comparability among IVs and assess their relative impact on the dependent variable, Z-standardization was applied. This transformation normalized the IVs to a mean of 0 and a standard deviation of 1, allowing for unit-independent comparison. All statistical tests were conducted at a significance level of α = 0.05.
Table 1 summarizes the baseline characteristics of the patient cohort. The study included 93 men and 68 women, with a mean age of 69 years. Health status over the previous two weeks was rated as “acceptable” by 39% of patients, “satisfactory” by 37%, and “terrible” by only 2%.
The majority of patients (79%) were diagnosed with oral squamous cell carcinoma (SCC), followed by cutaneous SCC (7%), salivary gland carcinoma (6%), adenoid cystic carcinoma (3%), and basal cell carcinoma (3%). Merkel cell carcinoma and lentigo malignant melanoma accounted for 1% of cases categorized as “other.” AJCC staging indicated that 66% of patients presented with early-stage tumors (Stages 0-II), while 34% were classified as advanced-stage (Stages III-IVC). AJCC staging was not applied to basal cell carcinoma cases. At the time of the study, 12% of the patient cohort had documented evidence of disease recurrence.
Most patients (97.5%) underwent primary surgical treatment, with only 2.5% receiving radiotherapy or chemotherapy as their primary modality. Among surgical cases, local defect closure was slightly more common than microvascular reconstruction. Microvascular techniques included the use of fibula, forearm flap, scapula, or anterolateral thigh (ALT) grafts, while local closure involved regional flaps such as submental island flaps, temporalis muscle flaps, nasolabial flaps, supraclavicular artery island flaps, or facial artery musculomuscular flaps. A small proportion of cases (2%) utilized full-thickness skin from the forearm, iliac crest, or omentum majus, classified as “other”.
The specific characteristics relevant to the consultation are outlined in the subsequent sections. The patient cohort consisted of 161 individuals (93 male, 68 female) with a mean age of 69 years (SD = 11.73, range: 34–95). Most patients (79%) had oral squamous cell carcinoma, followed by cutaneous squamous cell carcinoma (7%), salivary gland carcinoma (6%), adenoid cystic carcinoma (3%), and basal cell carcinoma (3%). A small proportion of cases (2%) were categorized as “other,” including rare tumor types. Regarding tumor stage, 66% of patients presented with early-stage tumors (AJCC 0–II), whereas 34% were classified with advanced stages (III–IVc). Tumor recurrence was documented in 12% of the cohort.
Nine clinicians (six male, three female) participated, with face masks worn throughout consultations in 40% of cases (case group) and only during direct clinical examinations in 60% (control group).
The CARE score showed no significant differences between case and control groups (31.83 vs. 33.01; p = 0.454). The correlations are shown in Figure 1. Familiarity with the clinician varied among patients, with 38% indicating they knew the clinician “well,” 11% “very well,” 24% “not at all,” 5% “not well,” and 22% reporting a “neutral” level of familiarity. A significant positive correlation was observed between familiarity and higher CARE scores (p = 0.009). Neither tumor stage, recurrence status, nor consultation duration significantly influenced CARE values. Fifty percent of consultations lasted between 15 and 30 minutes, with max. 45 minutes. In the case group, a positive trend was observed, with CARE scores increasing as the consultation duration lengthened. However, this relationship was not evident in the control group. Overall, statistical analysis showed that consultation duration had no significant influence on CARE values (p = 0.32).
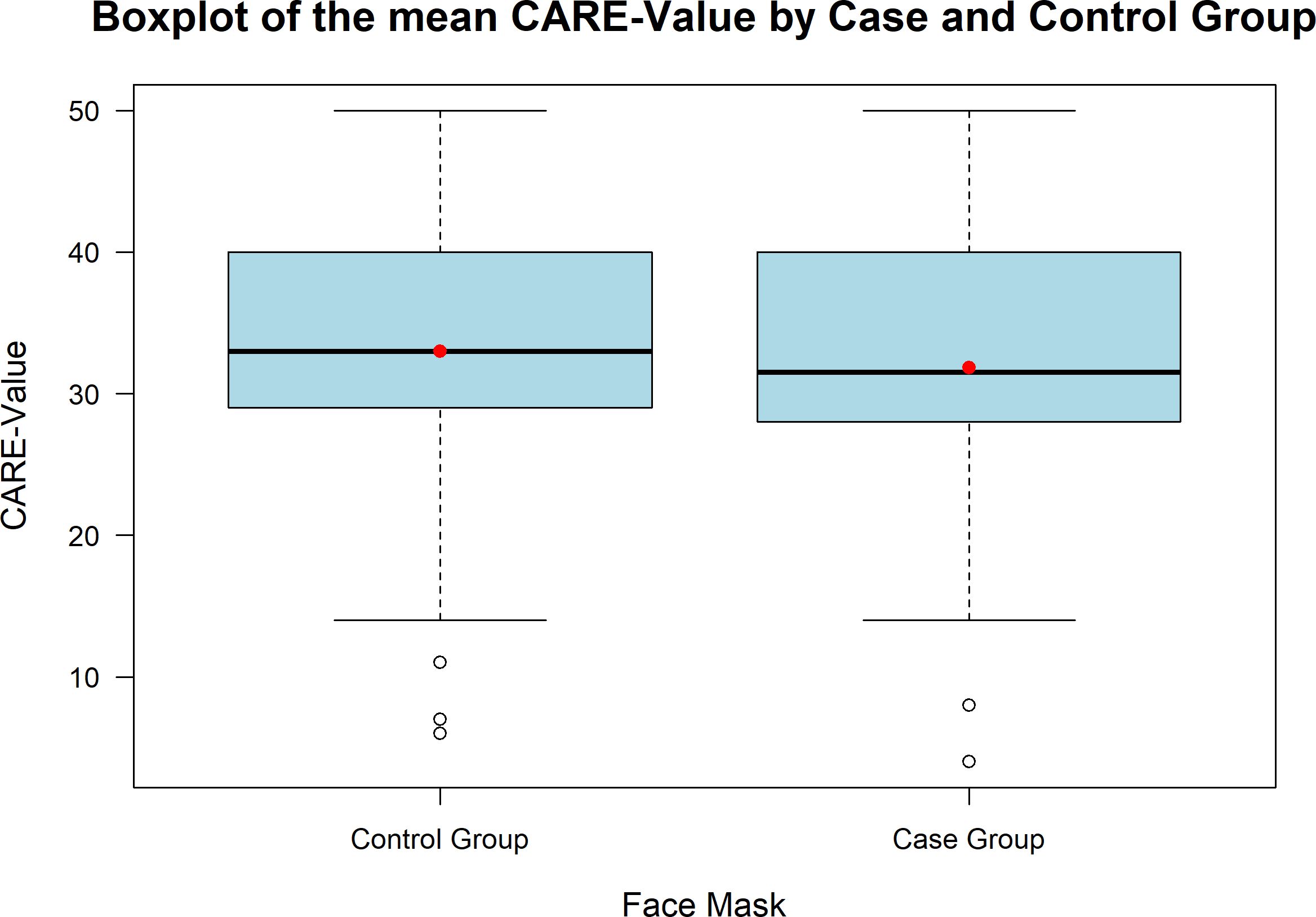
Figure 1. Boxplot of mean CARE scores for the case and control groups. Both groups show similar distributions, with a median CARE-Value around 35. The control group exhibits a slightly wider range and more outliers. The case group involved full face mask use during consultations, while the control group had partial usage.
Table 2 highlights the patients’ difficulties associated with the face mask, along with the reasons for these challenges. It is notable that only 5% of the patients reported feeling highly impaired by the face mask, while 76% of the patients indicated that they did not perceive any impairment. When queried about the underlying causes of this impairment, 21% of the patients indicated that they were unable to accurately identify the face and facial expressions of the clinician, while 73% of the patients did not perceive any of the provided response options to be an accurate representation of their experience. The variables presented in Table 3 were answered by the entire patient population (n=161). The data indicates that only 11% of patients would prefer their clinician to wear a face mask for the entirety of the consultation. Most patients (48%) indicated that they would not prefer their clinician to wear a face mask for the entirety of the consultation. The question regarding the relevance of face masks in preventing the spread of respiratory infections in hospitals yielded less definitive responses. While 42% of the patients considered a face mask to be relevant, 32% were opposed to its use.
Familiarity with the clinician from previous consultations was significantly associated with higher CARE scores (p = 0.009). Both the case and control groups exhibited higher CARE values when patients reported knowing their clinician “very well.” This relationship is illustrated in Figure 2. A Kruskal-Wallis test was performed to analyze CARE scores across different levels of familiarity and group assignments, revealing significant differences (p = 0.0433). Post-hoc analysis using a Dunn test showed a significant difference between patients in the case group who were “not at all” familiar with their clinician and those in the control group who were “very well” familiar (p = 0.0147), with an effect size (r = -0.283).
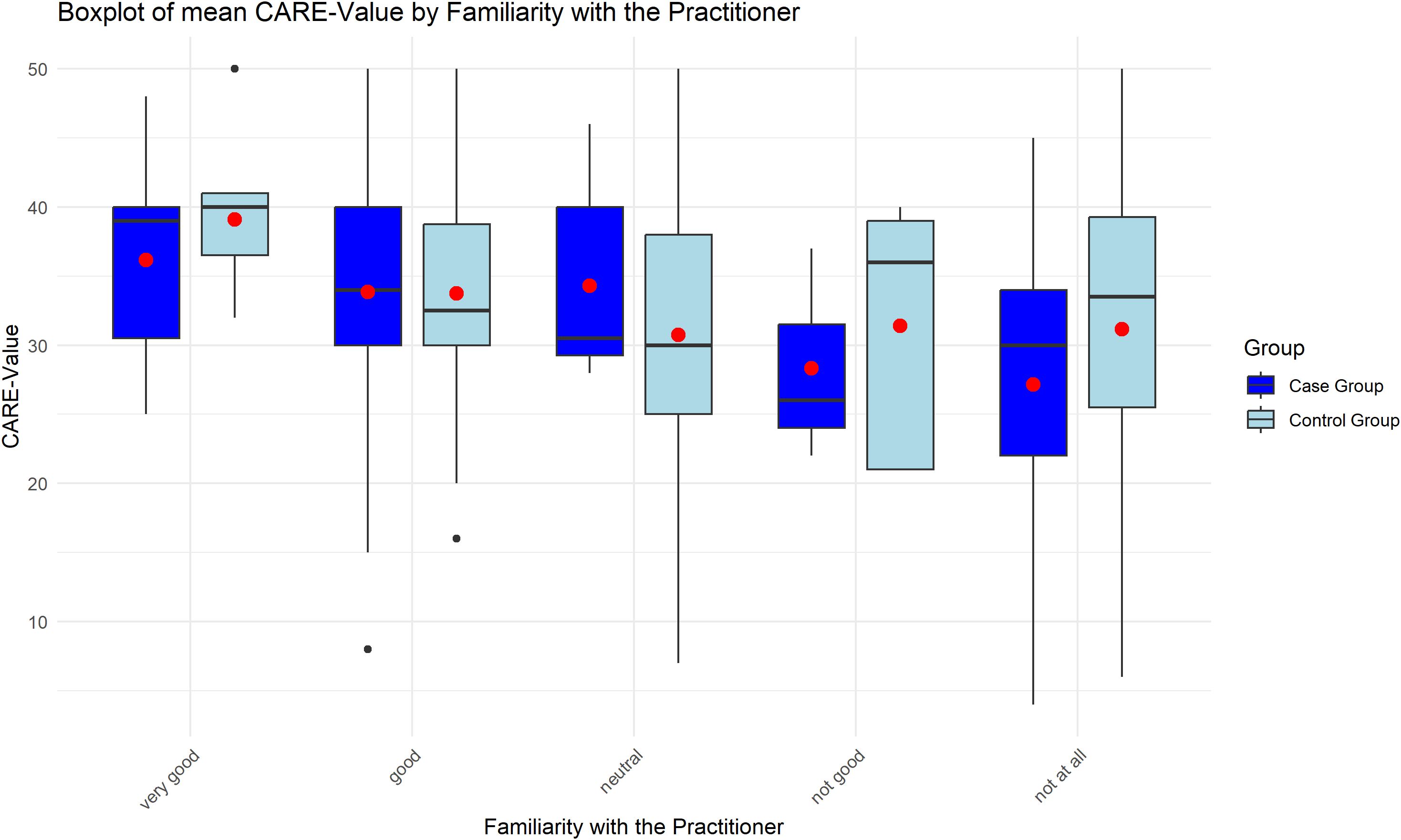
Figure 2. The graph shows a significant correlation between prior familiarity with the clinician and higher CARE scores (p=0.009), indicating improved patient-perceived empathy when the clinician was well-known.
CARE scores also demonstrated a potential relationship with patients’ self-assessed health status. Patients who rated their health as “very good” reported the highest CARE values; however, this observation did not reach statistical significance (p = 0.10). Due to the small number of patients rating their health as “very poor” (n = 3), these responses were combined with “poor” for the analysis.
The results of the multiple linear regression analysis are summarized in Table 4. Among the variables analyzed—health status, tumor stage, recurrence, familiarity with the clinician, clinician gender, consultation duration, and mask usage—only “familiarity with the clinician” was found to be statistically significant (β = 1.73, p = 0.003). None of the other variables had a significant effect, as indicated by p-values exceeding 0.05.
The regression model (F[7,151] = 2.305, p = 0.029) accounted for 9.65% of the variance in CARE scores, with an adjusted R² of 0.055, indicating a modest explanatory capacity. “Familiarity with the clinician” emerged as the most influential predictor, while the remaining variables, including face mask usage, did not significantly impact CARE scores.
This study investigated the impact of face mask use on the quality of communication and the perceived empathy of clinicians, as assessed from the perspective of patients with oral and maxillofacial tumors. The findings revealed that wearing a face mask during consultations did not significantly influence CARE scores, suggesting that mask use does not impair patients’ perception of clinician empathy. Notably, familiarity with the clinician emerged as the only significant factor positively affecting CARE scores, while tumor stage, recurrence, consultation duration, and clinician gender showed no significant effects. These results indicate that mask-wearing by clinicians does not interfere with perceived communication or empathy and that patients generally accept the use of face masks during consultations. The patient cohort comprised a total of 68 women and 93 men. Similar studies have reported a gender distribution favoring women (39, 40), with a lower mean age compared to our cohort. Additionally, the mean age of the patients was found to be lower in these studies. While Wong et al. (2013) reported the largest patient distribution in the 45-64 age group, Pandya et al. (2022) reported the largest patient distribution in the 50-60 age group (39, 40). The mean age of the patients in the present study was 69 years, with an age range of 34 to 95 years. This demographic profile is consistent with that of other head and neck-cancer patient collectives described in the literature, thereby ensuring the representativeness of the sample (41).
The recurrence rate of oral squamous cell carcinoma in our study was 12%, which is lower than the rates reported in other publications. These other publications reported recurrence rates of 20% (42) or 16% (43). As our study was the inaugural investigation into the correlation between a recurrence situation or high tumor stages of the patients in relation to the mean CARE values, it is not feasible to cite existing literature. The relationship between tumor recurrence, advanced tumor stages, and the use of face masks during consultations remains underexplored. Our findings suggest that patients prioritize effective communication and trust over the visibility of facial expressions, even in advanced disease stages. This indicates that empathy perception is less influenced by face masks and more by the clinician’s verbal communication and demeanor.
While existing literature extensively explores the CARE measure and the effects of face masks independently, few studies combine these topics as our study does. In this context, the aforementioned studies by Wong et al. (2013) and Pandya et al. (2022) stand out due to their methodology (39, 40).
While Wong et al. (2013) identified a significant negative influence of the face mask on the mean CARE value, Pandya et al. (2022) were unable to confirm this significance, a finding that is consistent with our study. The application of a face mask had no discernible impact on the mean CARE scores. It is important to note that Wong et al. (2013) had access to a significantly larger patient population than our study, and that their data set included general medical consultations, which differs from our specialist patient population. Furthermore, Wong et al. (2013) were able to distribute the number of consultations with and without a face mask in a more balanced manner. Pandya et al. (2022) conducted their study in an orthopedic department, which is a more specialized field. The size of the patient population was like that of our study, but the distribution of cases and controls was significantly more heterogeneous. In contrast to our study, patients were only allocated to the case or control group based on their stated preference for or rejection of face masks, rather than based on a consultation with or without face mask. The differences in findings between studies may be attributed to contextual factors, such as the timing of data collection and societal attitudes towards face masks. During the COVID-19 pandemic, mask-wearing became a widely accepted practice associated with infection prevention and safety. This shift in perception may have mitigated potential negative effects of masks on communication and empathy, which were more pronounced in studies conducted prior to the pandemic, when mask-wearing was less common.
While other studies (4, 6, 44) have tested the effects of face masks on emotional and empathic perception with static and decontextualized stimuli, Scheibe et al. (2023) employed a similar methodological approach to that used in our own study (45). The researchers employed dynamic stimuli to examine the correlation between perceived empathy and the use of a face mask. Similarly, this study found that wearing a face mask had no negative impact on perceived empathy. Scheibe et al. (2023) demonstrated that individuals can compensate for missing mouth cues by relying on alternative information channels, such as voice pitch, dynamic eye movement, and verbal content, when provided with dynamic, context-rich information. Therefore, individuals are sufficiently motivated to identify and empathize with their interaction partner if they are provided with sufficient information. We were unable to confirm the previously reported negative impact of wearing a face mask on patients’ empathy towards their doctor, as described in the study by Grundmann et al., 2021 (6). It remains unclear whether this discrepancy is due to differences in study design or the use of the CARE questionnaire as a measurement instrument.
As a potential influencing factor on the mean CARE value, we examined the health status of the patients over the previous two weeks. While Wong et al. (2013) reported a linear correlation between poor health and lower CARE scores, our findings only partially confirmed this correlation (39). Although the highest CARE scores were awarded to patients with a ‘very good’ state of health, this was not a statistically significant finding (p=0.10). Similarly, the study by Mercer et al. (2011) found no significant influence of patient health status on mean CARE score (33).
The factor ‘familiarity with the clinician’ was found to exert a significant influence on the mean CARE value during our study. In both the case and control groups, higher CARE values were assigned if patients indicated that they had a high level of familiarity with their clinician, based on previous consultations. The results suggest that in the control group (no mask), greater familiarity with the clinician improved empathy perception, while in the case group (mask), limited familiarity corresponded to lower CARE scores. These findings align with those of previous studies in the field. In their study, Pandya et al. (2022) report that the factor ‘ clinician familiarity’ was significant and exerted a greater influence on the mean CARE score than wearing a face mask (40). Wong et al. (2013) conducted a more detailed investigation into the interactive effect of wearing a face mask and the factor ‘familiarity with the clinicians’ (39). They also found that patients who already knew their clinician will give better CARE scores overall. However, the wearing of a face mask by the clinician had a greater influence on this group of patients, resulting in a significant reduction in the positive effect of ‘familiarity with the clinician’ and a significant increase in CARE scores.
This, however, gives rise to the question of how patients define their knowledge of a clinician. As Freeman et al. (2002) demonstrate in their study, this topic is inherently complex and does not necessarily correlate with the frequency of previous consultations with the same clinician (46). It is assumed that a good physician-patient relationship is more indicative of a patient’s familiarity with their clinician. To further promote this, the long-term care of patients by a clinician was identified as an essential process (47). Additionally, the factor ‘familiarity with the clinicians’ was found to have a positive effect on patient empowerment, specifically in relation to how patients dealt with their own illness (46, 48).
In contrast to the studies by Fung et al. (2009), Mercer et al. (2011) and Wong et al. (2013), our findings revealed no statistically significant correlation between the duration of the consultation and the mean CARE value (33, 39, 49). Similarly, Pandya et al. (2022) reached the same conclusion (40). Although a longer consultation duration in the case group resulted in higher CARE values, as observed in the study by Wong et al. (2013), this outcome was not replicated in the control group (39). Wong et al. (2013) also observed an increase in the mean CARE value per minute, with a value of 0.32. In other studies longer consultation duration was also found to have no impact on general patient satisfaction (50, 51). In this context, the authors emphasize that the quality of the medical consultation, rather than the duration of the consultation, is the determining factor in patient satisfaction.
Our study found no statistically significant differences in mean CARE scores based on clinician gender, contrasting with other studies reporting higher empathy scores for female clinicians and medical students (52–55). Furthermore, Hojat et al. (2002) demonstrated that surgical disciplines, including oral and maxillofacial surgery, exhibited lower empathy scores compared to other specialties (56). However, it is important to note that the gender distribution of clinicians in our study was significantly skewed towards male clinicians, and that the authors conducted their studies with different empathy scales and without the confounding factor of wearing a face mask.
In the present study, the methodology was consistent with that of previous studies in the comparative literature, which also focused on adult participants (6, 39, 40, 44, 45). Considering the above, it is pertinent to inquire as to the extent to which wearing a face mask affects children’s perception and the factors that may be involved in this process.
Despite the absence of any negative impact on patients’ perceived empathy, our study revealed that only a modest proportion of patients (11%) would prefer their clinician to wear a face mask throughout the entirety of the consultation. Moreover, less than half of the patients considered a mask to be relevant in preventing respiratory infections. In this context, it is necessary to identify the relevant factors influencing the acceptance of a face mask in society and to understand how this acceptance can be increased for possible future pandemics. Various approaches to this topic can be found in the scientific literature.
Although negative attitudes toward face masks are prevalent in the general population, often linked to discomfort and impaired communication (57, 58), our findings reveal that patients who experienced consultations with mask-wearing clinicians did not report such negative effects on perceived empathy or communication. This discrepancy suggests that in the clinical setting, the structured and professional nature of healthcare environments may mitigate concerns commonly associated with mask use, highlighting their protective role without compromising interpersonal interactions. Furthermore it has been demonstrated that individuals are more inclined to utilize a face mask if they are convinced of its efficacy (59–61). It is therefore imperative to enhance public awareness of the efficacy of face masks in preventing infection. It can be posited that a favorable disposition towards face masks and their efficacy is more likely to encourage individuals to utilize them in their everyday lives (60).
In their respective studies, Lau et al. (2004) and Sim et al. (2014) highlight the pivotal role of individual risk perception in the decision to wear a mask (59, 62). Individuals who perceive themselves to be highly susceptible to infectious diseases are more likely to wear them. The lack of knowledge about a disease can result in some segments of the population failing to recognize the necessity for protective measures (63).
Ensuring equal allocation of clinicians to the case and control groups posed a challenge due to varying duty rosters, rotation schedules, and clinical emergencies. In our clinic, patients are assigned to clinicians based primarily on availability and operational needs. Although efforts were made to minimize familiarity bias, patient preferences may have influenced assignments, and this potential limitation should be considered when interpreting the findings. It should be noted, however, that this study was not artificially constructed; rather, it reflected the actual day-to-day work in the Department of Oral and Maxillofacial Surgery at the University Medical Centre Goettingen.
A further limitation was the established recall system of the outpatient clinic. In the initial two-year period, patients are to be seen at eight-week intervals. In the subsequent three-to-four-month period of the third year, and in the six-month period of the fourth and fifth years, patients are to be seen at these intervals. Furthermore, patients may request to be seen at individually customized, longer intervals after the fifth year. While a considerable number of patients could be interviewed daily at the outset of the data collection period, the number of interviews conducted subsequently declined. This discrepancy arose because patients with shorter recall intervals were interviewed only once, while patients with longer recall intervals were excluded entirely due to the limited study timeframe, which spanned from November 2023 to April 2024.
The cancellation of appointments and the death of patients resulted in a further reduction in the patient population. A total of 161 patients were interviewed. To ensure the reliability of the results, further research should be conducted at other clinics with a larger case and control group in the future.
In contrast to the findings of other studies (39, 40), this study made a distinction between consultations conducted by female and male clinicians. Furthermore, achieving an even gender distribution of consultations presented a challenge in this context. Most consultations were conducted by male clinicians. However, this reflects the current gender distribution among the Department of Oral and Maxillofacial Surgery at the University Medical Center Goettingen. Furthermore, the exclusion criteria and the collective were reduced by the presence of language barriers or physical impairments of the patients (e.g. vision loss, hearing loss, writing difficulties).
The wearing of a face mask had no significant impact on physician-patient communication or the perceived empathy of the clinician. Neither tumor recurrence nor advanced tumor stages significantly influenced patients’ empathy ratings, likely because verbal communication and trust-building play a greater role than non-verbal cues like facial expressions. The only significant factor influencing mean CARE scores was patients’ familiarity with their clinician.
It is of the utmost importance to learn from past experiences to enhance preparedness for future pandemics.
Our findings indicate that face masks worn by clinicians do not negatively affect empathy as perceived by patients. However, only a limited proportion of patients expressed a preference for clinicians to wear a face mask throughout consultations. This may reflect factors such as comfort, communication preferences, or a general reluctance toward mask use. While we did not specifically assess patients’ knowledge of mask efficacy, these results emphasize the need for clear communication regarding the protective role of masks in preventing infections. To promote mask acceptance in clinical practice, strategies should focus on building trust within the clinician-patient relationship and ensuring safety in the clinical setting. Increased societal support for mask use in healthcare settings, particularly during future public health crises, may further enhance their acceptance and effectiveness.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics Committee of the University Medical Center Göttingen. The approval reference number is 33/8/23. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
GH: Writing – original draft, Writing – review & editing. NH: Writing – original draft, Writing – review & editing. TM: Data curation, Formal Analysis, Writing – review & editing. BS: Formal Analysis, Validation, Writing – review & editing. KG: Investigation, Writing – original draft. ML: Conceptualization, Project administration, Writing – original draft. HS: Supervision, Validation, Writing – review & editing. SW: Conceptualization, Investigation, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. We acknowledge support from Open Access Publication Funds of Goettingen University.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be constrained as a potential conflict of interest.
The author(s) declare that Generative AI was used in the creation of this manuscript. This manuscript utilized generative AI (OpenAI’s ChatGPT) for language refinement and editing. All scientific content, data, and conclusions were exclusively developed and verified by the authors.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. (2002) 15:25–38.
2. Kestenbaum R. Feeling happy versus feeling good: The processing of discrete and global categories of emotional expressions by children and adults. Dev Psychol. (1992) 28:1132–42. doi: 10.1037/0012-1649.28.6.1132
3. Guarnera M, Magnano P, Pellerone M, Cascio MI, Squatrito V, Buccheri SL. Facial expressions and the ability to recognize emotions from the eyes or mouth: A comparison among old adults, young adults, and children. J Genet Psychol. (2018) 179:297–310. doi: 10.1080/00221325.2018.1509200
4. Carbon C-C. Wearing face masks strongly confuses counterparts in reading emotions. Front Psychol. (2020) 11:566886. doi: 10.3389/fpsyg.2020.566886
5. Tsantani M, Podgajecka V, Gray KLH, Cook R. How does the presence of a surgical face mask impair the perceived intensity of facial emotions? PloS One. (2022) 17:e0262344. doi: 10.1371/journal.pone.0262344
6. Grundmann F, Epstude K, Scheibe S. Face masks reduce emotion-recognition accuracy and perceived closeness. PloS One. (2021) 16:e0249792. doi: 10.1371/journal.pone.0249792
7. Ribeiro VV, Dassie-Leite AP, Pereira EC, Santos ADN, Martins P, Irineu RDA. Effect of wearing a face mask on vocal self-perception during a pandemic. J Voice. (2022) 36:878.e1–7. doi: 10.1016/j.jvoice.2020.09.006
8. Die Bundesregierung. Maskenpflicht in ganz Deutschland. Die Bundesregierung informiert | Startseite(2020). Available online at: https://www.bundesregierung.de/breg-de/themen/coronavirus/maskenpflicht-in-deutschland-1747318 (Accessed February 15, 2024).
9. Koch-Institut R. Mund-Nasen-Bedeckung im öffentlichen Raum als weitere Komponente zur Reduktion der Übertragungen von COVID-19. Epidemiol Bull. (2020) 19:3–5. doi: 10.25646/6731
10. Weller S. Ab Ostersamstag, 8. April 2023: Keine Maskenpflicht mehr. Besuchsregelung bleibt (2023). Available online at: https://www.umg.eu/news-detail/news-detail/detail/news/keine-maskenpflicht-mehr-besuchsregelung-bleibt/ (Accessed March 15, 2024).
11. Coclite D, Napoletano A, Gianola S, Del Monaco A, D’Angelo D, Fauci A, et al. Face mask use in the community for reducing the spread of COVID-19: A systematic review. Front Med. (2021) 7:594269. doi: 10.3389/fmed.2020.594269
12. Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, van der Westhuizen H-M, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci USA. (2021) 118:e2014564118. doi: 10.1073/pnas.2014564118
13. Boulos L, Curran JA, Gallant A, Wong H, Johnson C, Delahunty-Pike A, et al. Effectiveness of face masks for reducing transmission of SARS-CoV-2: a rapid systematic review. Phil Trans R Soc A. (2023) 381:20230133. doi: 10.1098/rsta.2023.0133
14. Taylor S, Asmundson GJG. Negative attitudes about facemasks during the COVID-19 pandemic: The dual importance of perceived ineffectiveness and psychological reactance. PloS One. (2021) 16:e0246317. doi: 10.1371/journal.pone.0246317
15. Young DG, Rasheed H, Bleakley A, Langbaum JB. The politics of mask-wearing: Political preferences, reactance, and conflict aversion during COVID. Soc Sci Med. (2022) 298:114836. doi: 10.1016/j.socscimed.2022.114836
16. Kim D, Carson RT, Whittington D, Hanemann M. Support for regulation versus compliance: Face masks during COVID-19. Public Health Pract. (2023) 5:100324. doi: 10.1016/j.puhip.2022.100324
17. Shekaraiah S, Suresh K. Effect of face mask on voice production during COVID-19 pandemic: A systematic review. J Voice. (2021) 38:446–57. doi: 10.1016/j.jvoice.2021.09.027
18. Burgos-Blasco B, Arriola-Villalobos P, Fernandez-Vigo JI, Oribio-Quinto C, Ariño-Gutierrez M, Diaz-Valle D, et al. Face mask use and effects on the ocular surface health: A comprehensive review. Ocul Surf. (2023) 27:56–66. doi: 10.1016/j.jtos.2022.12.006
19. İnan Doğan E, Kaya F. Dermatological findings in patients admitting to dermatology clinic after using face masks during Covid-19 pandemia: A new health problem. Dermatol Ther. (2021) 34:e14934. doi: 10.1111/dth.14934
20. Shenal BV, Radonovich LJ, Cheng J, Hodgson M, Bender BS. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J Occup Environ Hyg. (2012) 9:59–64. doi: 10.1080/15459624.2012.635133
21. Kisielinski K, Giboni P, Prescher A, Klosterhalfen B, Graessel D, Funken S, et al. Is a mask that covers the mouth and nose free from undesirable side effects in everyday use and free of potential hazards? IJERPH. (2021) 18:4344. doi: 10.3390/ijerph18084344
22. Sfakianaki A, Kafentzis GP, Kiagiadaki D, Vlahavas G. Effect of face mask and noise on word recognition by children and adults. Proceedings of the 12th International Conference of Experimental Linguistics (ExLing 2021) (2021), 217–20. doi: 10.36505/ExLing-2021/12/0055/000528
23. Dondé C, Pouchon A, Pelluet A, Bougerol T, Polosan M. The impact of wearing a face mask on the psychiatric interview: a national survey during the COVID-19 pandemic. Psychiatr Q. (2022) 93:435–42. doi: 10.1007/s11126-021-09962-3
24. Lee E, Cormier K, Sharma A. Face mask use in healthcare settings: effects on communication, cognition, listening effort and strategies for amelioration. Cognit Res. (2022) 7:2. doi: 10.1186/s41235-021-00353-7
25. Rahne T, Fröhlich L, Plontke S, Wagner L. Influence of face surgical and N95 face masks on speech perception and listening effort in noise. PLoS One. (2021) 16(7):e0253874. doi: 10.21203/rs.3.rs-343284/v1
26. Moon I-J, Jo M, Kim G-Y, Kim N, Cho Y-S, Hong S-H, et al. How does a face mask impact speech perception? Healthcare. (2022) 10:1709. doi: 10.3390/healthcare10091709
27. Guarnera M, Hichy Z, Cascio MI, Carrubba S. Facial expressions and ability to recognize emotions from eyes or mouth in children. Eur J Psychol. (2015) 11:183–96. doi: 10.5964/ejop.v11i2.890
28. Noyes E, Davis JP, Petrov N, Gray KLH, Ritchie KL. The effect of face masks and sunglasses on identity and expression recognition with super-recognizers and typical observers. R Soc Open Sci. (2021) 8:201169. doi: 10.1098/rsos.201169
29. Proverbio AM, Cerri A. The recognition of facial expressions under surgical masks: the primacy of anger. Front Neurosci. (2022) 16:864490. doi: 10.3389/fnins.2022.864490
30. Mercer SW. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Family Pract. (2004) 21:699–705. doi: 10.1093/fampra/cmh621
31. Mercer SW, McConnachie A, Maxwell M, Heaney D, Watt GCM. Relevance and practical use of the Consultation and Relational Empathy (CARE) Measure in general practice. Fam Pract. (2005) 22:328–34. doi: 10.1093/fampra/cmh730
32. Neumann M, Wirtz M, Bollschweiler E, Warm M, Wolf J, Pfaff H. Psychometric evaluation of the German version of the “Consultation and Relational Empathy” (CARE) measure at the example of cancer patients. Psychother Psychosom Med Psychol. (2008) 58:5–15. doi: 10.1055/s-2007-970791
33. Mercer SW, Fung CS, Chan FW, Wong FY, Wong SY, Murphy D. The Chinese-version of the CARE Measure reliably differentiates between doctors in primary care: a cross-sectional study in Hong Kong. BMC Family Pract. (2011) 12:43. doi: 10.1186/1471-2296-12-43
34. Aomatsu M, Abe H, Abe K, Yasui H, Suzuki T, Sato J, et al. Validity and reliability of the Japanese version of the CARE Measure in a general medicine outpatient setting. Family Pract. (2014) 31:118–26. doi: 10.1093/fampra/cmt053
35. Hanževački M, Jakovina T, Bajić Ž, Tomac A, Mercer S. Reliability and validity of the Croatian version of Consultation and Relational Empathy (CARE) Measure in primary care setting. Croat Med J. (2015) 56:50–6. doi: 10.3325/cmj.2015.56.50
36. Crosta Ahlforn K, Bojner Horwitz E, Osika W. A Swedish version of the Consultation and Relational Empathy (CARE) measure. Scand J Prim Health Care. (2017) 35:286–92. doi: 10.1080/02813432.2017.1358853
37. García Del Barrio L, Rodríguez-Díez C, Martín-Lanas R, Costa P, Costa MJ, Díez N. Reliability and validity of the Spanish (Spain) version of the consultation and relational empathy measure in primary care. Family Pract. (2021) 38:353–9. doi: 10.1093/fampra/cmaa135
38. Park K-Y, Shin J, Park H-K, Kim YM, Hwang SY, Shin J-H, et al. Validity and reliability of a Korean version of the Consultation and Relational Empathy (CARE) measure. BMC Med Educ. (2022) 22:403. doi: 10.1186/s12909-022-03478-5
39. Wong CKM, Yip BHK, Mercer S, Griffiths S, Kung K, Wong MC, et al. Effect of facemasks on empathy and relational continuity: a randomised controlled trial in primary care. BMC Fam Pract. (2013) 14:200. doi: 10.1186/1471-2296-14-200
40. Pandya S, Sedani AB, Syros A, Yakkanti RR, Dodds SD, Aiyer AA. The effects of face masks on the doctor-patient relationship in orthopaedics. Iowa Orthop J. (2022) 42:267–73.
41. Cramer JD, Reddy A, Ferris RL, Duvvuri U, Samant S. Comparison of the seventh and eighth edition american joint committee on cancer oral cavity staging systems. Laryngoscope. (2018) 128:2351–60. doi: 10.1002/lary.27205
42. Wolff K-D, Follmann M, Nast A. The diagnosis and treatment of oral cavity cancer. Deutsches Ärzteblatt Int. (2012) 109:829–35. doi: 10.3238/arztebl.2012.0829
43. Yanamoto S, Yamada S, Takahashi H, Yoshitomi I, Kawasaki G, Ikeda H, et al. Clinicopathological risk factors for local recurrence in oral squamous cell carcinoma. Int J Oral Maxillofac Surg. (2012) 41:1195–200. doi: 10.1016/j.ijom.2012.07.011
44. Marini M, Ansani A, Paglieri F, Caruana F, Viola M. The impact of facemasks on emotion recognition, trust attribution and re-identification. Sci Rep. (2021) 11:5577. doi: 10.1038/s41598-021-84806-5
45. Scheibe S, Grundmann F, Kranenborg B, Epstude K. Empathising with masked targets: limited side effects of face masks on empathy for dynamic, context-rich stimuli. Cogn Emotion. (2023) 37:683–95. doi: 10.1080/02699931.2023.2193385
46. Freeman G, Walker J, Heaney D, Howie J. Personal continuity and the quality of GP consultations: Knowing the doctor or having a regular doctor? Eur J Gen Pract. (2002) 8:90–4. doi: 10.3109/13814780209160846
47. Ridd M, Shaw A, Lewis G, Salisbury C. The patient-doctor relationship: a synthesis of the qualitative literature on patients’ perspectives. Br J Gen Pract. (2009) 59:e116–133. doi: 10.3399/bjgp09X420248
48. Howie JGR, Heaney DJ, Maxwell M, Walker JJ, Freeman GK, Rai H. Quality at general practice consultations: cross sectional survey. BMJ. (1999) 319:738–43. doi: 10.1136/bmj.319.7212.738
49. Fung CSC, Hua A, Tam L, Mercer SW. Reliability and validity of the Chinese version of the CARE Measure in a primary care setting in Hong Kong. Family Pract. (2009) 26:398–406. doi: 10.1093/fampra/cmp044
50. Lemon T, Smith R. Consultation content not consultation length improves patient satisfaction. J Family Med Prim Care. (2014) 3:333. doi: 10.4103/2249-4863.148102
51. Elmore N, Burt J, Abel G, Maratos FA, Montague J, Campbell J, et al. Investigating the relationship between consultation length and patient experience: a cross-sectional study in primary care. Br J Gen Pract. (2016) 66:e896–903. doi: 10.3399/bjgp16X687733
52. Hojat M, Louis DZ, Maxwell K, Markham F, Wender R, Gonnella JS. Patient perceptions of physician empathy, satisfaction with physician, interpersonal trust, and compliance. Int J Med Educ. (2010) 1:83–7. doi: 10.5116/ijme.4d00.b701
53. Borracci RA, Doval HC, Nuñez C, Samarelli M, Tamini S, Tanus E. Measurement of empathy among Argentine cardiologists: Psychometrics and differences by age, gender, and subspecialty. Cardiol J. (2015) 22:52–6. doi: 10.5603/CJ.a2014.0050
54. Santos MA, Grosseman S, Morelli TC, Giuliano ICB, Erdmann TR. Empathy differences by gender and specialty preference in medical students: a study in Brazil. Int J Med Educ. (2016) 7:153–7. doi: 10.5116/ijme.572f.115f
55. Andersen FA, Johansen A-SB, Søndergaard J, Andersen CM, Assing Hvidt E. Revisiting the trajectory of medical students’ empathy, and impact of gender, specialty preferences and nationality: a systematic review. BMC Med Educ. (2020) 20:52. doi: 10.1186/s12909-020-1964-5
56. Hojat, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. AJP. (2002) 159:1563–9. doi: 10.1176/appi.ajp.159.9.1563
57. Capraro V, Barcelo H. Telling people to “rely on their reasoning” increases intentions to wear a face covering to slow down COVID-19 transmission. Appl Cogn Psychol. (2021) 35:693–9. doi: 10.1002/acp.3793
58. Yusof MZ, Fadzil NFZ, Kamaruzi NNNA, Ayazi MSS. Public perception on face mask wearing during COVID-19 pandemic in Malaysia: A cross sectional study. PloS One. (2024) 19:e0303031. doi: 10.1371/journal.pone.0303031
59. Sim S, Moey K, Tan N. The use of facemasks to prevent respiratory infection: a literature review in the context of the Health Belief Model. smedj. (2014) 55:160–7. doi: 10.11622/smedj.2014037
60. Zhang B, Li Z, Jiang L. The intentions to wear face masks and the differences in preventive behaviors between urban and rural areas during COVID-19: an analysis based on the technology acceptance model. IJERPH. (2021) 18:9988. doi: 10.3390/ijerph18199988
61. Bearth A, Siegrist M. The drivers and barriers of wearing a facemask during the SARS-CoV-2 pandemic in Switzerland. J Risk Res. (2022) 25:1085–97. doi: 10.1080/13669877.2022.2038244
62. Lau JTF, Yang X, Tsui H, Pang E, Kim JH. SARS preventive and risk behaviours of Hong Kong air travellers. Epidemiol Infect. (2004) 132:727–36. doi: 10.1017/S0950268804002225
Keywords: oral squamous cell carcinoma, COVID 19, face masks, CARE-Questionnaire, empathy, physician-patient relations, communication barriers, oral and maxillofacial surgery
Citation: Hoene G, von Hahn N, Mathea T, Schminke B, Goldstein K, Leu M, Schliephake H and Wolfer S (2025) Impact of face masks on empathy and communication in head and neck cancer patients: a case-control study. Front. Oncol. 15:1539070. doi: 10.3389/fonc.2025.1539070
Received: 03 December 2024; Accepted: 19 February 2025;
Published: 07 March 2025.
Edited by:
Oreste Iocca, University of Turin, ItalyReviewed by:
Jessica Maldonado-Mendoza, Metropolitan Autonomous University, MexicoCopyright © 2025 Hoene, von Hahn, Mathea, Schminke, Goldstein, Leu, Schliephake and Wolfer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Georg Hoene, R2VvcmcuSG9lbmVAbWVkLnVuaS1nb2V0dGluZ2VuLmRl
†These authors have contributed equally to this work
‡ORCID: Georg Hoene, orcid.org/0000-0003-1025-6758
Nikolaus von Hahn, orcid.org/0000-0002-4069-8023
Tim Mathea, orcid.org/0009-0007-3874-8638
Boris Schminke, orcid.org/0000-0002-8520-9481
Kathi Goldstein, orcid.org/0009-0001-5790-8349
Martin Leu, orcid.org/0000-0002-3883-6837
Henning Schliephake, orcid.org/0000-0002-2008-7188
Susanne Wolfer, orcid.org/0000-0002-4134-2301
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.