
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 13 February 2025
Sec. Hematologic Malignancies
Volume 15 - 2025 | https://doi.org/10.3389/fonc.2025.1528536
 Soo How Lim1,2*†
Soo How Lim1,2*† Tian Er Poh1,2
Tian Er Poh1,2 Hong Chin Wee2,3
Hong Chin Wee2,3 Nur Shazwaniza Binti Awang Basry4
Nur Shazwaniza Binti Awang Basry4 Mohd Syazwan Bin Tajul Arifin5
Mohd Syazwan Bin Tajul Arifin5 Kar Ying Yong1,6
Kar Ying Yong1,6Primary urethral plasmacytoma is an extremely rare form of solitary plasmacytoma, with only 10 cases reported in the literature. It involves localized clonal proliferation of plasma cells without systemic disease. This report presents a 29-year-old man with acute urinary retention and a urethral mass, confirmed as solitary plasmacytoma. The patient was treated with 45 Gy of local radiotherapy, resulting in complete tumor resolution without recurrence or progression at a 2-year follow-up. Given its rarity, treatment strategies for primary urethral plasmacytoma are not well-defined. Radiotherapy is preferred over surgery in young patients due to the radiosensitivity of plasma cell tumors and its ability to preserve sexual and urinary function. A review of previous cases treated with radiotherapy alone, using doses of 40–50 Gy, showed favorable outcomes with no recurrences reported over follow-up periods ranging from 6 months to 12 years. Only one patient experienced minor long-term complications. This report highlights the effectiveness of radiotherapy as a primary modality for managing primary urethral plasmacytoma, offering excellent local control while preserving organ function. Individualized treatment plans should consider patient age, fertility concerns, and tumor characteristics. Further research is necessary to optimize treatment protocols and long-term surveillance strategies due to the potential risk of recurrence or progression to multiple myeloma.
Solitary plasmacytoma (SP) is a localized neoplasm characterized by monoclonal proliferation of the B cells without systemic involvement, which can be further divided into solitary bone plasmacytoma and solitary extramedullary plasmacytoma. Solitary extramedullary plasmacytoma predominantly involves the soft tissues with the aerodigestive tract being the most frequently affected site (1). Solitary extramedullary plasmacytoma of the urethra is extremely rare. To date, there have been just 10 published reports of primary urethral plasmacytoma (PUP) (Table 1). We reported a case of PUP of a young gentleman who was successfully treated with radiotherapy alone with no evidence of relapse in 2 years and with no short-term and long-term radiation adverse effects. We aim to elucidate the treatment modalities of PUP and to provide a more refined approach to its management in clinical practice.
A 29-year-old married man, with no known medical history, presented with acute urinary retention requiring urgent suprapubic catheter (SPC) insertion. He reported a 2-month history of painless growth on the penis. On physical examination, a fungating mass, measuring 2 × 3 cm, was observed at the tip of the glans (Figure 1A). A wedge biopsy of the glans revealed florid granulomatous inflammation with atypical plasma cell infiltration with predominance of lambda light chain expression suggestive of plasma cell neoplasm (PCN). However, bone marrow examination ruled out plasma cell neoplasm, and the patient had no end-organ damage such as hypercalcemia, renal impairment, anemia, or bone lesions. He had no detectable paraprotein too. Contrast-enhanced computed tomography (CECT) of the neck, thorax, abdomen, and pelvis revealed bilateral inguinal lymphadenopathy, with the largest node on the right inguinal side measuring 2.4 × 2.0 × 2.8 cm, and bilateral iliac lymphadenopathy, with the largest node on the right external iliac side measuring 1.6 × 3.0 cm (Figure 2) . Excisional biopsies of the bilateral inguinal lymph nodes showed no malignancy. Diagnostic antegrade flexible cystoscopy revealed meatal stenosis and a distal urethral mass extending to the base of the penis. Histology showed a neoplastic cells with a plasmacytic appearance, including binucleated and multinucleated forms (Figure 3).
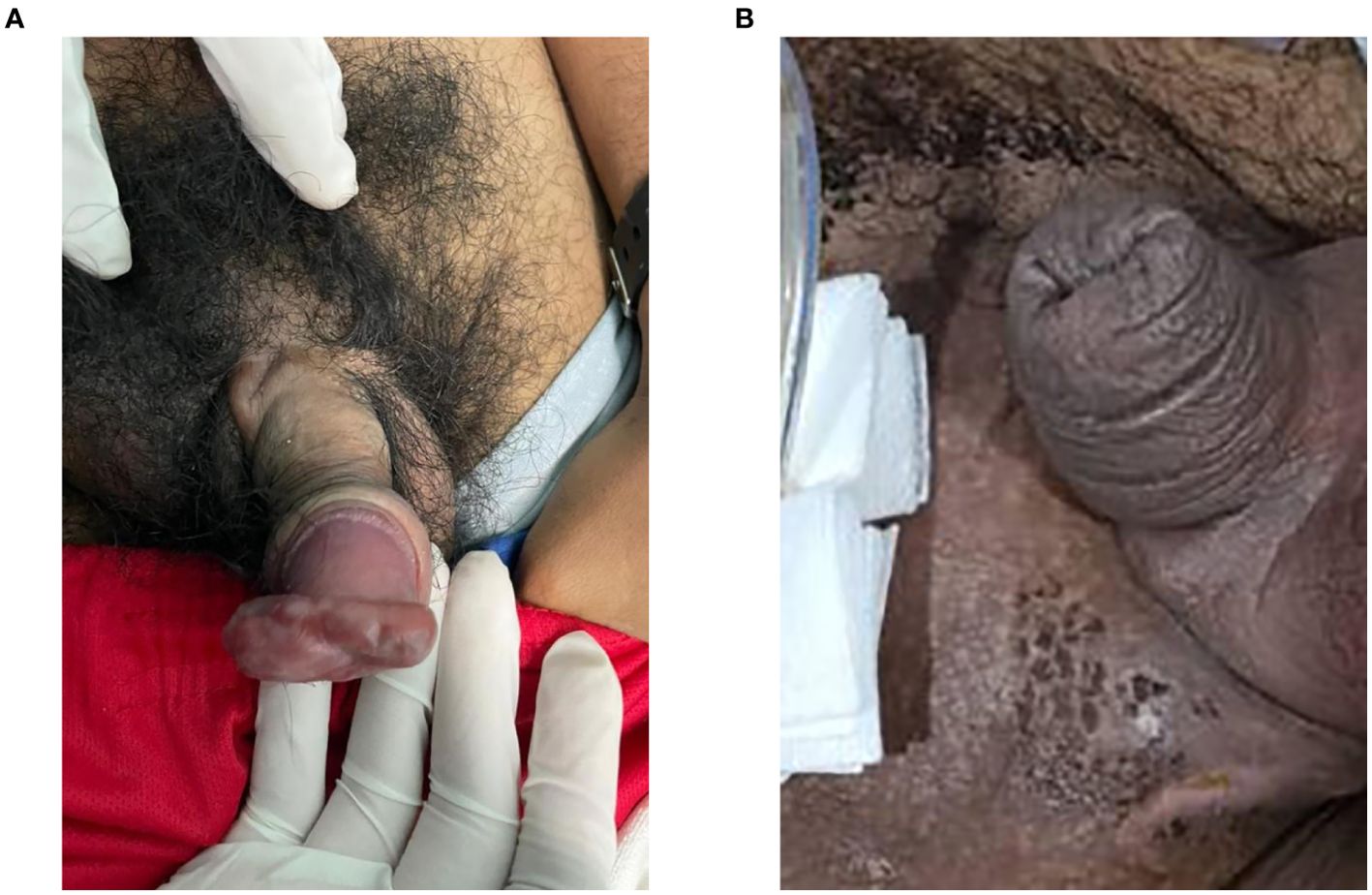
Figure 1. (A) Mass of fungating tumor at the tip of the penile glans measuring 2 × 3 cm. (B) Resolution of the penile mass.

Figure 2. Contrast-enhanced computed tomography (CECT) pelvis in axial view showed enlarged iliac lymph node and inguinal lymph nodes with necrotic center.
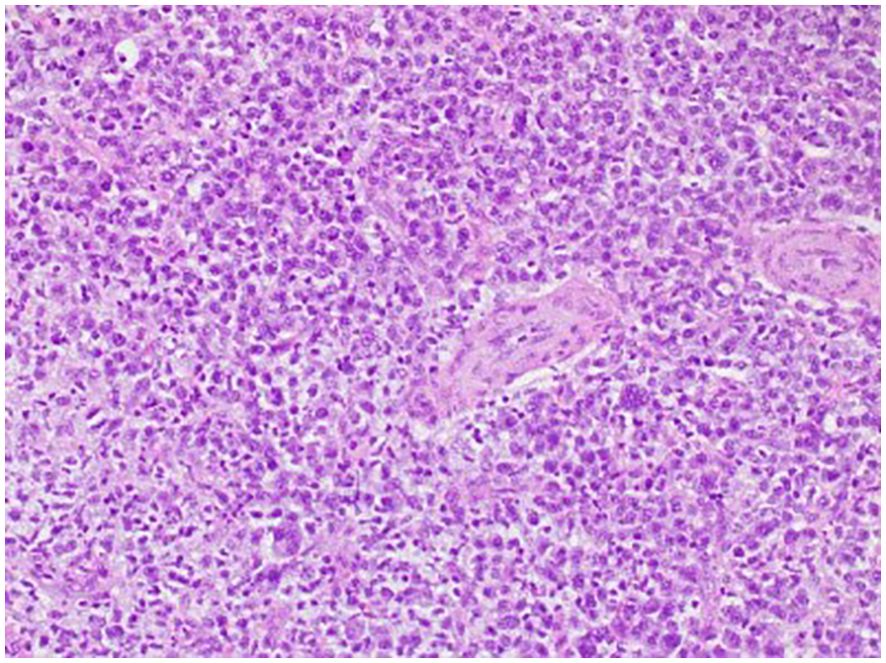
Figure 3. Histology of the glans penis. Neoplastic cells with a plasmacytoid appearance, including binucleated and multinucleated forms, are present.
The patient was diagnosed with PUP. After a multidisciplinary team discussion involving a urologist, an oncologist, and a hematologist, the patient underwent local definitive radiotherapy. A total dose of 45 Gy was delivered in 25 fractions over 5 weeks, targeting the penis and right inguinal lymph nodes. The treatment utilized 6-MV photons, ensuring 95% coverage of the target volume. The radiotherapy was administered using a three-dimensional external beam radiation therapy (3D-EBRT) technique with anterior and posterior fields. One month post-radiotherapy, the penile mass had resolved, with no urinary or sexual dysfunction (Figure 1B). The SPC was removed via flexible cystoscopy. At the 2-year follow-up, the patient remained well, with no long-term radiation side effects and no evidence of progression to multiple myeloma.
The primary treatment modalities for PUP include surgery, radiotherapy, or a combination of both. However, managing young men with PUP poses distinct challenges for treating physicians, especially in relation to fertility preservation and maintaining erectile function. Given these concerns, radiotherapy is often the preferred treatment, especially for patients of reproductive age. Plasma cell tumors are radiosensitive, and radiotherapy has been associated with favorable survival outcomes (2–4). Four case reports have documented successful treatment of PUP in men using radiotherapy alone, with doses ranging from 40 to 50 Gy (5–8). In these cases, no recurrences were reported, with follow-up periods ranging from 6 months to 12 years. All have no reported long-term adverse events except in the study by Stein et al., who reported that one patient experienced intermittent transurethral bleeding post-coitus. These cases highlight the efficacy of radiotherapy in providing local tumor control while preserving organ function. However, Witjes et al. reported a 39-year-old gentleman with PUP who relapsed after 1 year of 46-Gy external radiotherapy but achieved treatment remission following urethrectomy and perineostomy (9).
Surgical resection alone has been less commonly reported. Campbell et al. described a 73-year-old man with distal urethral plasmacytoma who had a prior history of solitary plasmacytoma of the oropharynx treated with surgical excision and radiotherapy 7 years earlier. He underwent distal urethrectomy with preservation of the glans penis and remained in remission for 1 year (10). However, Kraus et al. reported a 35-year-old gentleman with PUP who had local recurrence after 3 months of initial urethrotomy but achieved disease remission after a second urethrotomy and 46 Gy of radiotherapy (11).
There are also three reported cases of PUP in women (12–14). The first two cases by Mark et al. and Su et al. were treated successfully with combined surgery and radiotherapy, with follow-up ranging from 1 year to more than 10 years (9, 10). Lemos et al. reported a case of a woman who responded well to surgical resection alone, with no evidence of relapse after 3 years of follow-up (14).
In conclusion, case reports have shown that radiotherapy alone can achieve favorable outcomes in tumor control while preserving the integrity of the sexual organ, enabling men of reproductive age to maintain their sense of masculinity without experiencing psychological or physical burdens. However, treatment strategies for patients with PUP should be personalized, as individual responses may vary depending on the underlying disease biology. Therefore, if the initial treatment approach fails or proves ineffective, a second alternative or combined treatment modality should be considered. Long-term follow-up and surveillance are crucial to detect any potential relapse or progression to multiple myeloma (15).
“I was really worried at first about the problems I was facing. Before starting treatment, I was told there could be many potential side effects from radiotherapy. But thankfully, I didn’t experience many issues. Now, I’m back at work and feeling so happy with the results.”
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by National Medical Research Register/Medical Research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
SL: Conceptualization, Data curation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. TP: Writing – review & editing. HW: Writing – review & editing. NA: Investigation, Writing – review & editing. MT: Investigation, Writing – review & editing. KY: Conceptualization, Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The National Institute of Health (NIH) covered the article processing charge (APC) for this publication.
We would like to thank the Director General of Health Malaysia for his permission to publish the article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Dores GM, Landgren O, McGlynn KA, Curtis RE, Linet MS, Devesa SS. Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: incidence and survival in the United States, 1992–2004. Br J haematology. (2009) 144:86–94. doi: 10.1111/j.1365-2141.2008.07421.x
2. Saba L, Fu C-L, Sarna K, Liang H, Dominguez BG, Greskovich J, et al. Real-world treatment patterns and outcomes of solitary plasmacytoma in the United States: A national cancer database (NCDB) analysis of years 2004-2020. Blood. (2023) 142:2025. doi: 10.1182/blood-2023-181057
3. Li Q-W, Niu S-Q, Wang H-Y, Wen G, Li YY, Xia YF, et al. Radiotherapy alone is associated with improved outcomes over surgery in the management of solitary plasmacytoma. Asian Pacific J Cancer Prev. (2015) 16:3741–5. doi: 10.7314/APJCP.2015.16.9.3741
4. Suh Y-G, Suh C-O, Kim JS, Kim SJ, Pyun HO, Cho J, et al. Radiotherapy for solitary plasmacytoma of bone and soft tissue: outcomes and prognostic factors. Ann Hematol. (2012) 91:1785–93. doi: 10.1007/s00277-012-1510-6
5. Mordkin RM, Skinner DG, Levine AM. Long-term disease-free survival after plasmacytoma of the urethra: a case report and review of the literature. Urology. (1996) 48:149–50. doi: 10.1016/S0090-4295(96)00102-1
6. Gokce O, Acar O, Tunc M, Kilicaslan I, Esen T, Ozcan F. Primary urethral plasmacytoma: a case report and literature review. Kaohsiung J Med Sci. (2008) 24:274–7. doi: 10.1016/S1607-551X(08)70153-0
7. Alcorn SR, Gocke CD, Woodard CA, Tran PT. Solitary plasmacytoma of the penile urethra treated with primary radiotherapy. J Clin Oncol. (2014) 32:e95–7. doi: 10.1200/JCO.2012.48.4246
8. Stein J, Latz S, Ellinger J, Hauser S, Sailer V, Oelmann-Avendano J, et al. Primary urethral plasmacytoma treated with high-dose-rate brachytherapy: A case report. Urol Int. (2016) 97:369–72. doi: 10.1159/000445298
9. Witjes J, De Vries J, Schaafsma H, Bogman M, Barentsz J, Corten R. Extramedullary plasmacytoma of the urethra: a case report. J urology. (1991) 145:826–8. doi: 10.1016/S0022-5347(17)38464-1
10. Campbell CM, Smith JA Jr., Middleton RG. Plasmacytoma of the urethra. J Urol. (1982) 127:986. doi: 10.1016/S0022-5347(17)54157-9
11. Kraus-Tiefenbacher U, Gutwein S, Höpner U, Wawersig C, Ikinger U, Wannenmacher M, et al. Plasmocytoma of the urethra. Onkologie. (2004) 27:166–8. doi: 10.1159/000076907
12. Mark JA, Pais VM, Chong FK. Plasmacytoma of the urethra treated with transurethral resection and radiotherapy. J Urol. (1990) 143:1010–1. doi: 10.1016/S0022-5347(17)40171-6
13. Su W, Zeng L, Zhao D, Fu Y, Tang J. Case report: plasmacytoma of external urethral meatus. Front Endocrinol (Lausanne). (2022) 13:783855. doi: 10.3389/fendo.2022.783855
14. Lemos N, Melo CR, Soares IC, Lemos RR, Lemos FR. Plasmacytoma of the urethra treated by excisional biopsy. Scand J Urol Nephrol. (2000) 34:75–6. doi: 10.1080/003655900750016959
Keywords: plasmacytoma, urethral, treatment modality, radiotherapy, preserve function, case report
Citation: Lim SH, Poh TE, Wee HC, Awang Basry NSB, Tajul Arifin MSB and Yong KY (2025) Radiotherapy as a primary treatment modality for a young man with a primary urethral plasmacytoma: case report and literature review. Front. Oncol. 15:1528536. doi: 10.3389/fonc.2025.1528536
Received: 15 November 2024; Accepted: 20 January 2025;
Published: 13 February 2025.
Edited by:
Nicola Sgherza, AOU Policlinico Consorziale di Bari, ItalyReviewed by:
Jad A. Degheili, Ibn Sina Hospital, KuwaitCopyright © 2025 Lim, Poh, Wee, Awang Basry, Tajul Arifin and Yong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Soo How Lim, cGF0cmlja2NvdzEyM0BnbWFpbC5jb20=
†ORCID: Soo How Lim, orcid.org/0009-0001-3264-3997
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.