
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol., 08 April 2025
Sec. Gastrointestinal Cancers: Gastric and Esophageal Cancers
Volume 15 - 2025 | https://doi.org/10.3389/fonc.2025.1519922
As a common malignant tumor, esophageal cancer is easy to relapse and distant metastasis, and the prognosis is very poor. Colon and rectal metastasis of esophageal cancer is extremely rare. This study reports a case of colorectal and rectal metastasis in an esophageal squamous cell carcinoma patient. The patient was a 65-year-old man who presented with progressive swallowing obstruction. Gastroscopy and pathological biopsy revealed low-differentiated squamous cell carcinoma in the lower esophagus (32cm from the incisor). After completing the relevant examination, the patient was evaluated by the thoracic surgeon and showed no indication of surgery. Then the patient was received 2 cycles of Abraxane plus cisplatin with Sintilimab. After the treatment, the esophageal lesion was examined by Chest CT, and assesses again by the surgeon again and radical radiotherapy was recommended without indication of surgery. After radiotherapy, the patient underwent comprehensive imaging examination. Abdominal CT showed mass in the lower abdomen. Colonoscopy and pathological biopsy showed squamous cell carcinoma of colon and rectum. According to the pathological type and tumor monism, and communication with the pathologist, the patient was diagnosed to be esophageal cancer with rectal and colon metastasis. Through this case report, we hope to deepen the understanding of rare esophageal squamous cell metastasis, and comprehensive examination should be conducted before initial treatment to evaluate the tumor status.
Esophagus cancer is a common malignant tumor of digestive system. According to CLOBOCAN 2024, there are about 600,000 new cases of esophageal cancer in the world, and about 540,000 deaths, while nearly half of the global incidence and death cases of esophageal cancer occur in China (1). At the same time, the incidence and mortality of esophageal cancer in China are ranked sixth and fourth respectively in the incidence and death of malignant tumors in China, posing a serious threat to human health (2). The epidemiology of esophageal cancer shows that the distribution of esophageal cancer patients in China is geographically distributed, which may be related to the living habits of patients, mainly including hot food and pickled food (3, 4). Esophageal cancer patients have no obvious symptoms in the early stage of the disease. When esophageal fistula occurs, patients may have fever, cough, sputum and other symptoms (5, 6). The common distant metastasis of esophageal cancer includes supraclavicular lymph node metastasis and metastasis of liver, lung, brain, bone, but the metastasis of rectum, colon is very rare. We report a rare case of rectal and colonic metastasis of lower esophageal squamous cell carcinoma.
All procedures performed in human participants met the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
The patient was a 67-year-old man who presented to the hospital in March 2024 with progressive swallowing obstruction for more than 1 month. Gastroscopy was performed on the patient, and new organisms were found in the esophagus 33-37 cm away from the incisor. The lesions occupied more than 2/3 of the lumen, resulting in stenosis of the lumen (Figure 1A). Esophageal pathological examination of the patient revealed esophageal squamous cell carcinoma (Figure 1B). Further, the patient underwent upper gastrointestinal angiography, which showed that irregular filling defects were observed in the lower esophagus (Figure 1C). The results of chest CT showed that the wall of the lower esophagus was significantly thickened, about 1.8 cm at the thicker part, and the surrounding fat space was blurred. A mass soft tissue density shadow was observed in the hepatogastric space, which was indistinctly separated from the lower esophagus, with a size of 4.9×2.3 cm (Figure 1D). After assessed by the thoracic surgeon, the patient had no indications for surgery and received neoadjuvant chemotherapy and immunotherapy. The patients were treated with 2-cycle TP (Abraxane 400 mg, d1, cisplatin 120 mg, d1) combined with sindillimab (200mg, d1) on 2024-03-28 and 2024-4-18 respectively. Chest CT reexamination showed that the lower esophageal wall was thickened, with the thicker part about 1.2 cm, and the surrounding fat space was blurred. In the hepatogastric space, there was a dense mass of soft tissue with an unclear boundary between the lower end of the esophagus and the adjacent gastric wall, with a size of 3.7×1.9 cm (Figures 2A, B). After 2 cycles of chemotherapy combined with immunotherapy, the esophageal lesions and lymph nodes in the hepatogastric space were all reduced, but the fatty space around the esophagus was still fuzzy. According to the evaluation of the surgeon, the patient had no operation opportunity. 2024-04-29, the patient received radiotherapy with a dose of P-GTV 50 Gy/25 Fx for esophageal tumor lesions and hepatic and gastric space lymph node lesions(Figure 2C). The completion time of radiotherapy was 2024-06-09. 2024-07-07, the patient returned to the hospital and underwent upper gastrointestinal angiography, and the results showed that irregular and mild stenosis about 1.1cm in length was observed in the lower thoracic section of the esophagus, and the expansion was slightly limited, and the passage of contrast agent was not significantly hindered. Chest CT showed that the wall of the lower esophagus was significantly thickened, about 1.3cm at the thicker part, and the surrounding fat space was blurred. Multiple nodules were found in the hepatogastric space, which was indistinct from the lower esophagus (Figure 2D). After admission, the patient underwent abdominal CT scan due to the symptoms of blood in stool for nearly 1 month. Abdominal CT results showed a 4.9 x 4.4 cm mass in the right lower abdomen, which was closely related to the ascending colon, and the rectovesical space lesions were closely related to the adjacent anterior rectal wall (Figures 3A, B). Further, the colonoscopy results showed that the neoplasm was found at 10 cm and the lumen was narrowed by the tumor. The neoplasm was found at 70 cm (ascending colon) and the lumen was narrowed significantly (Figures 3C, D). Pathological results showed that: “Ascending colon 70 cm” and “rectum” check see carcinoma, immunohistochemistry, CK5/6 (+), about (+), P40 (+), Ki67 (about 40%) +, CK7 (-), CK20 (-), CDX - 2 (-), SATB2 (-), ascending colon and rectum saw squamous cell carcinoma (Figures 3E, F). Based on the antitumor treatment timeline (Figure 4) and the examination results of the patient, the diagnosis of lower esophageal squamous cell carcinoma with distant metastasis was clear. Since the patient had incomplete intestinal obstruction accompanied by hematochezia, it was recommended to perform tumor reduction for the lesions of rectum and colon after the evaluation of the surgeon. Unfortunately, after communicating with the patient’s family, the patient and the patient’s family finally chose not to undergo surgery and chemotherapy after considering the patient’s condition and economic situation, and returned to the local hospital for palliative care.
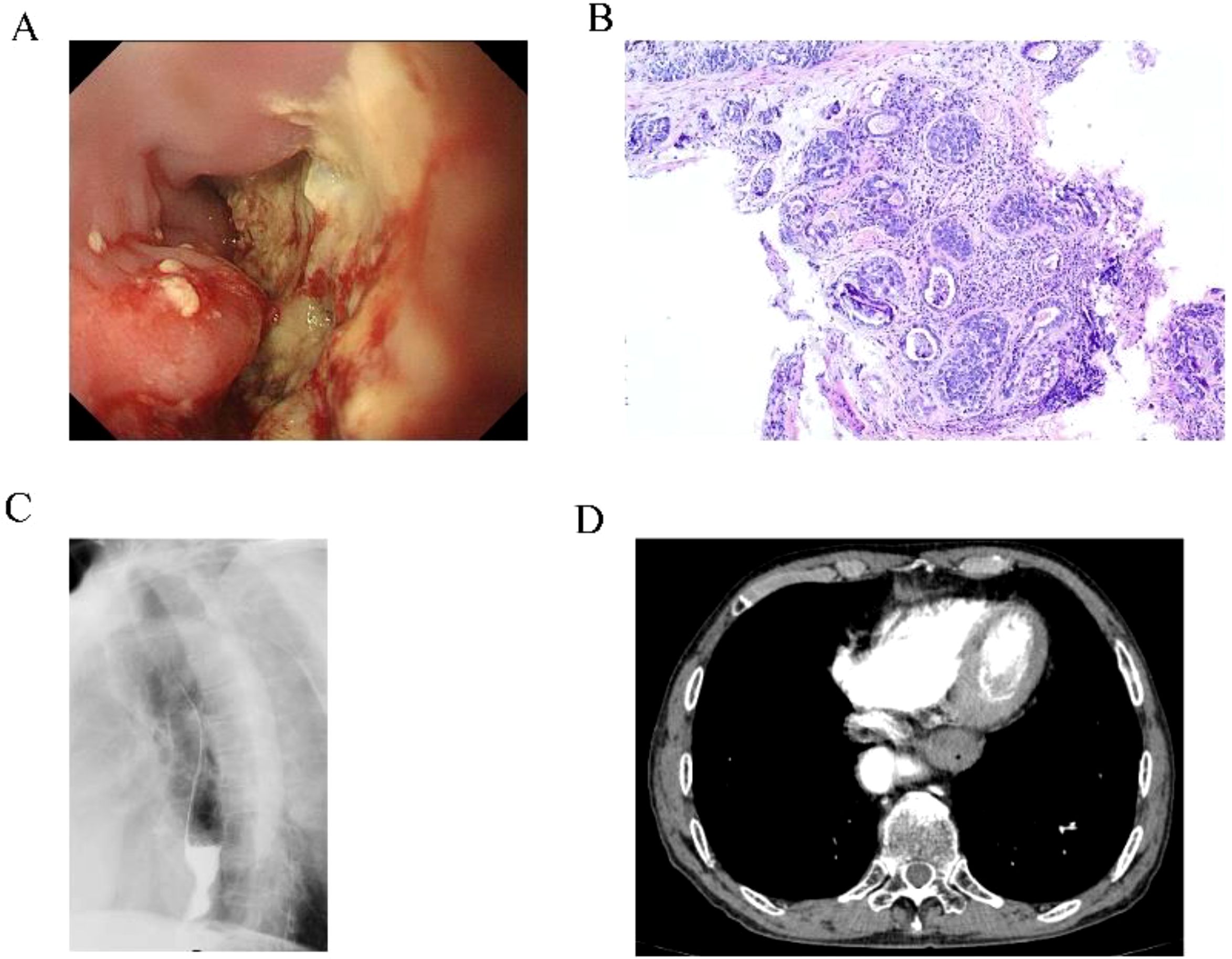
Figure 1. Pre-treatment examination results of the patients. (A) Gastroscopy results showed neoplasm in the lower esophagus. (B) The lesion site of the esophagus showed squamous cell carcinoma. (C) Gastrointestinal angiography showed stenosis of the lower esophagus. (D) Chest CT showed thickening of the lower wall of the esophageal tube with stenosis.
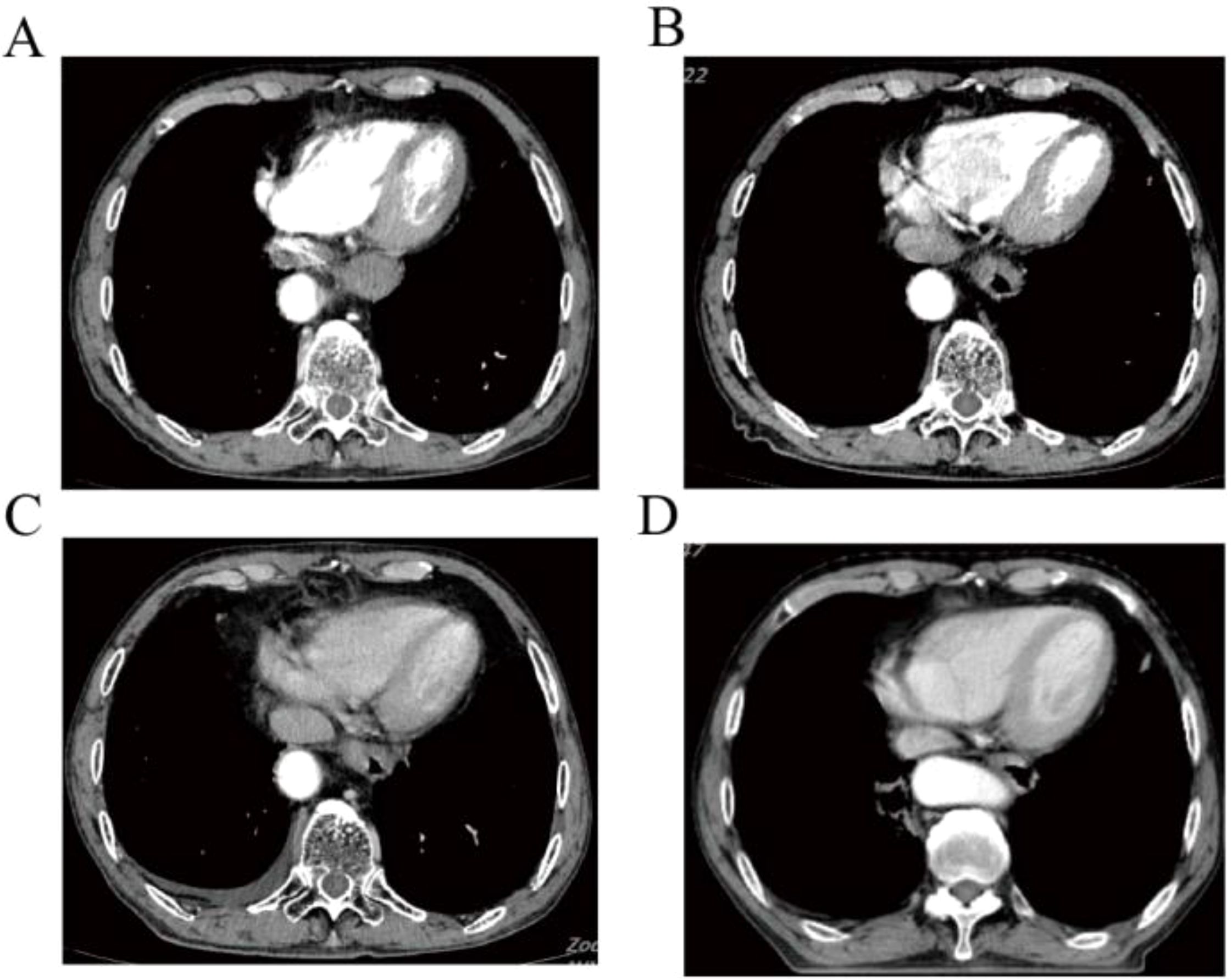
Figure 2. Chest CT of shows the changes of esophageal lesions of anti-tumor therapy. (A) Esophageal lesions before treatment. (B) Esophageal lesions after 2 cycles of chemotherapy combined with immunotherapy. (C) Esophageal lesions before radiotherapy. (D) Esophageal lesions on chest CT were reexamined after radiotherapy.
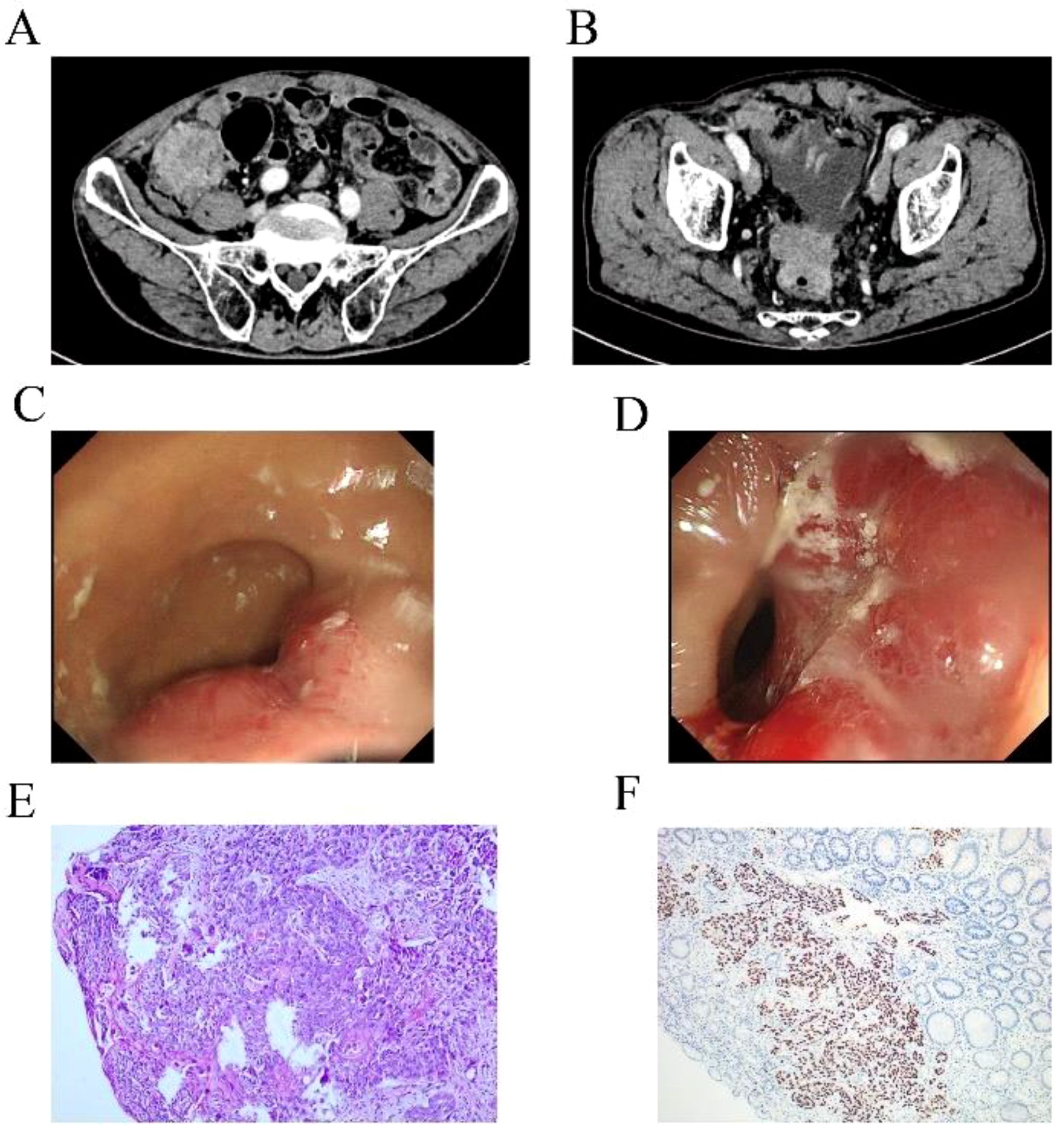
Figure 3. Examination results of rectal and colon metastases. (A, B) Abdominal CT showed space-occupying lesions of colon and rectum. (C, D) Colonoscopy of colon and rectum found new organisms. (E, F) HE staining and immunohistochemical results supported squamous cell carcinoma.
Due to the deep anatomical structure and hidden onset, most patients with esophageal cancer have been locally advanced or advanced at the time of clinical treatment. The metastasis of esophageal cancer can be divided into lymphatic metastasis, blood metastasis and direct spread metastasis (7). Studies have shown that about 20 percent of patients develop distant metastases at first visit (8). When patients develop distant metastases, the disease progresses rapidly, the treatment is poor, the prognosis is poor, and the median time to formation is only 3-5 months (9). The common distant metastasis organs of esophageal cancer are mainly lung, liver and bone (6). Metastasis of esophageal cancer to the rectum and colon is rare (10, 11), malignant bowel obstruction (MBO) is even rarer. MBO is a common end-stage event in patients with advanced tumors. Studies have shown that the incidence of MBO in advanced tumors is 5% to 43%, with the highest risk of ovarian cancer (5% to 51%) and gastrointestinal tumors (10% to 28%) (12, 13). The average time from cancer diagnosis to MBO was 14 months (14). For patients with MBO, the goal of treatment is to improve the quality of life and prolong survival. In this case, MBO was diagnosed by abdominal CT and colonoscopy after the appearance of blood in stool. After general surgical consultation, palliative tumor reduction is recommended. For MBO patients, whether to perform surgery is still controversial. Although studies have shown that MBO patients receiving surgery compared to conservative treatment, patients do not benefit significantly (15). However, the study of Reed et al. (16) showed that compared with conservative treatment, surgical treatment can prolong the survival time of patients (15 months VS 3 months). The National Comprehensive Caner Network (NCCN) recommends systemic palliative chemotherapy plus immunotherapy for patients with stage IV esophageal squamous cell carcinoma, combined with local therapy if necessary (17). After standard first-line chemotherapy combined with immunotherapy, the esophageal primary lesion was controlled, but the colorectal metastasis site advanced, and tumor reduction surgery was recommended. Unfortunately, the patient refused to undergo tumor reduction surgery and was discharged automatically.
The mechanism of rectal metastasis of esophageal cancer remains unclear. It has been suggested that lymphatic metastasis is one of the possible causes, because of the abundance of lymph in the esophagus, tumor cells may retrograde through the lymphatic system to the colorectal, resulting in colorectal metastasis (11, 18).
Traditional imaging methods for clinical evaluation of esophageal cancer patients with distant metastasis mainly include ultrasound, CT and MRI (19, 20). It has been reported that the sensitivity of CT in the diagnosis of distant metastasis of esophageal cancer is only 37% ~ 66%, which is largely dependent on pathological diagnosis. Although MRI is more sensitive than CT in the external invasion of esophageal cancer, it is not better than CT in the preoperative staging of esophageal cancer. Conventional imaging is based on histomorphological changes and is a local examination. positron emission computed tomography/computed tomography (PET/CT), PET/CT integrates molecular imaging function and anatomical structure imaging, which can reflect the morphological characteristics and metabolic status of the lesion, and show the heterogeneity and treatment-induced changes within the tumor in a non-invasive manner. PET/CT examination makes up for the above shortcomings, it can detect functional metabolic abnormalities earlier before the lesion morphological changes, and has its absolute advantages in the diagnosis of distant metastasis of esophageal cancer (20). Since pelvic imaging examination is not a routine examination item for esophageal cancer, pelvic imaging examination was lacking when the patient was first diagnosed. After the occurrence of hematochezia in patients, relevant examinations were improved to finally determine the colon and rectal metastasis of esophageal cancer. From the perspective of the diagnosis and treatment process of this patient, PET/CT examination of tumor patients at the first diagnosis can find uncommon tumor metastasis sites, and provide more information for tumor staging and treatment plan.
To our knowledge, this is only the first reported case of esophageal squamous cell carcinoma with colonic and rectal metastasis. From the diagnosis and treatment of this patient, we need to learn the following lessons: 1. For newly diagnosed patients with esophageal cancer, complete imaging examination, especially PET/CT, is of great significance to find rare tumor metastasis and accurate tumor staging. 2. Multi-disciplinary treatment (MDT) is very necessary, and the implementation of MDT can enable patients to get timely, standardized and effective treatment. 3. Strengthen doctor-patient communication and establish patients’ confidence in treatment.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
JY: Writing – original draft, Writing – review & editing, Data curation. WG: Writing – original draft, Writing – review & editing, Data curation. XP: Writing – original draft, Writing – review & editing, Data curation. YT: Writing – review & editing, Visualization. YZ: Writing – review & editing, Visualization. BZ: Writing – review & editing, Visualization. YG: Writing – review & editing, Data curation. DM: Writing – review & editing, Data curation.
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by funds from Nanchong Social Science Federation Project (NO. NC24B260); The Affiliated Hospital of North Sichuan Medical College introduced high-level talents research start-up Project (No. 2023-2GC016).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bray F, Laversanne M, Sung H, Siegel RL, Soerjomataram I, Jemal A, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2024) 74(3):229–63. doi: 10.3322/caac.21834
2. Xia C, Dong X, Li H, Cao M, Sun D, He S, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl). (2022) 135(5):584–90. doi: 10.1097/CM9.0000000000002108
3. Jiang Q, Shu Y, Jiang Z, Zhang Y, Pan S, Jiang W, et al. Burdens of stomach and esophageal cancer from 1990 to 2019 and projection to 2030 in China: Findings from the 2019 Global Burden of Disease Study. J Glob Health. (2024) 14:04025. doi: 10.7189/jogh.14.04025
4. Yang CS, Chen X, Tu S. Etiology and prevention of esophageal cancer. Gastrointest Tumors. (2016) 3:3–16. doi: 10.1159/000443155
5. Liu CQ, Ma YL, Qin Q, Wang PH, Luo Y, Xu PF, Y, et al. Epidemiology of esophageal cancer in 2020 and projections to 2030 and 2040. Thorac Cancer. (2023) 14:3–11. doi: 10.1111/1759-7714.14745
6. Watanabe M, Otake R, Kozuki R, Toihata T, Takahashi K, Okamura A, et al. Recent progress in multidisciplinary treatment for patients with esophageal cancer. Surg Today. (2020) 50(1):12–20. doi: 10.1007/s00595-019-01878-7
7. Wang Y, Yang W, Wang Q, Zhou Y. Mechanisms of esophageal cancer metastasis and treatment progress. Front Immunol. (2023) 14:1206504. doi: 10.3389/fimmu.2023.1206504
8. Shi Y, Ge X, Ju M, Zhang Y, Di X, Liang L. Circulating tumor cells in esophageal squamous cell carcinoma - mini review. Cancer Manag Res. (2021) 13:8355–65. doi: 10.2147/CMAR.S337489
9. Ai D, Zhu H, Ren W, Chen Y, Liu Q, Deng J, et al. Patterns of distant organ metastases in esophageal cancer: a population-based study. J Thorac Dis. (2017) 9(9):3023–30. doi: 10.21037/jtd.2017.08.72
10. Chen J, Zhang S, Chen J. Case report: A case of rectal metastatic squamous cell carcinoma from the esophagus. Front Oncol. (2023) 13:1092868. doi: 10.3389/fonc.2023.1092868
11. Kang M, Zhu L, Yang M, Zhang Y, Wang S, Wang Y. Rare presentation of esophageal squamous cell carcinoma with rectal metastasis: A case report. Oncol Lett. (2023) 26(6):510. doi: 10.3892/ol.2023.14097
12. Idelevich E, Kashtan H, Mavor E, Brenner B. Small bowel obstruction caused by secondary tumors. Surg Oncol. (2006) 15(1):29–32. doi: 10.1016/j.suronc.2006.05.004
13. Cousins SE, Tempest E, Feuer DJ. Surgery for the resolution of symptoms in Malignant bowel obstruction in advanced gynaecological and gastrointestinal cancer. Cochrane Database Syst Rev. (2016) 2016:Cd002764. doi: 10.1002/14651858.CD002764.pub2
14. Tuca A, Guell E, Martinez-Losada E, Codorniu N. Malignant bowel obstruction in advanced cancer patients: epidemiology, management, and factors influencing spontaneous resolution. Cancer Manag Res. (2012) 4:159–69. doi: 10.2147/CMAR.S29297
15. Krouse RS, Anderson GL, Arnold KB, Thomson CA, Nfonsam VN, Al-Kasspooles MF, et al. Surgical versus non-surgical management for patients with Malignant bowel obstruction (S1316): a pragmatic comparative effectiveness trial. Lancet Gastroenterol Hepatol. (2023) 8(10):908–18. doi: 10.1016/S2468-1253(23)00191-7
16. Ayabe RI, Mendoza T, Yennu S, Bruera E, Williams LA, Badgwell: B. Symptom burden in patients with Malignant bowel obstruction treated with or without surgery. J Am Coll Surg. (2023) 236(3):514–22. doi: 10.1097/xcs.0000000000000498
17. Mai Z, Xie J, Leng C, Xie X, Wen J, Yang H, et al. An optimized postsurgery follow-up strategy for patients with esophageal cancer: a cohort study. Int J Surg. (2024) 110(1):332–41.
18. Wang Y, Zhu L, Xia W, Wang F. Anatomy of lymphatic drainage of the esophagus and lymph node metastasis of thoracic esophageal cancer. Cancer Manag Res. (2018) 10:6295–303. doi: 10.2147/CMAR.S182436
19. Zhu C, Mu F, Wang S, Qiu Q, Wang S, Wang L. Prediction of distant metastasis in esophageal cancer using a radiomics-clinical model. Eur J Med Res. (2022) 27(1):272. doi: 10.1186/s40001-022-00877-8
Keywords: esophageal squamous cell carcinoma, rectal metastasis, colon metastasis, treatment, case report
Citation: Yang J, Guo W, Pang X, Tang Y, Zhang Y, Zeng B, Gui Y and Ma D (2025) Esophageal squamous cell carcinoma with colonic and rectal metastases: a rare case report. Front. Oncol. 15:1519922. doi: 10.3389/fonc.2025.1519922
Received: 30 October 2024; Accepted: 27 January 2025;
Published: 08 April 2025.
Edited by:
Zheng Liu, National Cancer Center of China, ChinaReviewed by:
Daming Zhang, First Affiliated Hospital of Harbin Medical University, ChinaCopyright © 2025 Yang, Guo, Pang, Tang, Zhang, Zeng, Gui and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Gui, bnNjbWNneUAxNjMuY29t; Daiyuan Ma, bXNjbWNwaGR5anFAMTYzLmNvbQ==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.