- 1Breast Center, Cancer Hospital of Shantou University Medical College, Guangdong, Shantou, China
- 2Nursing Department, Shantou University Medical College, Guangdong, Shantou, China
- 3Department of General Surgery, The Second Affiliated Hospital of Shantou University Medical College, Shantou, China
- 4Department of Neurosurgery, The First Affiliated Hospital of Shantou University Medical College, Shantou, China
- 5Nursing Department, Cancer Hospital of Shantou University Medical College, Guangdong, Shantou, China
Background: Breast cancer-related lymphedema (BCRL) is a common and debilitating complication following breast cancer treatment. Despite its significant impact on patients’ quality of life, bibliometric analyses focusing on BCRL are scarce. This study aims to explore global research trends on BCRL from 2000 to 2023, identify existing knowledge gaps, and highlight emerging focus areas through a bibliometric approach.
Methods: A comprehensive search was conducted using the Web of Science (WOS) database to retrieve literature published between January 2000 and November 2023. Bibliometric analyses and visualizations were performed using R Studio, CiteSpace, and VOSviewer. Key data extracted included publication trends, contributing countries and institutions, leading authors, journals, research categories, and keywords. Outcome measures for analysis included the number of publications, citation counts, author productivity, and keyword co-occurrence.
Results: A total of 919 eligible publications from 52 countries and regions, 1,163 institutions, and 3,550 authors were identified. These publications appeared in 255 journals, with “Lymphology” emerging as the journal with the highest citation count. The USA was the most prolific contributor to the field. The annual number of publications demonstrated a consistent upward trend. Keyword co-occurrence analysis revealed prominent research hotspots, including “lymphedema,” “women,” “breast cancer,” “arm lymphedema,” and “quality of life.” Emerging keyword trends from 2021 to 2023 highlighted “prevention” and “validity” as pivotal research frontiers.
Conclusions: This bibliometric study highlights the growing interest in breast cancer-related lymphedema research and identifies key areas for future investigation, including prevention, diagnosis, and treatment strategies. The results underscore the need for further exploration of these emerging research areas to improve patient outcomes.
1 Introduction
Lymphedema, defined as tissue swelling caused by the abnormal accumulation of protein-rich fluid, results from lymphatic system dysfunction (1). It is a common secondary complication of cancer treatments, particularly following breast cancer therapies (2). Approximately one in five breast cancer survivors develop arm lymphedema (3), with a cumulative incidence of 11.9% observed in a study of 5,549 patients within five years post-surgery (4). In the United States, the incidence of breast cancer peaks among white women around age 80, whereas in Asian countries, rates tend to plateau or decline after age 50 (5). This condition is often triggered by lymphatic damage caused by surgical interventions such as mastectomy and axillary lymph node dissection or by radiotherapy (6, 7). Additional risk factors, such as elevated body mass index and advanced cancer stages (8), further contribute to the development of breast cancer-related lymphedema (BCRL) (9).
BCRL can affect the affected side’s arm, hand, finger, breast, or body. With the arm being the most commonly impacted area. Symptoms include pain, swelling, and restricted joint mobility (10), and complications may include recurrent infections, skin fibrosis, and chronic pain. These symptoms often progress and may become irreversible (11). BCRL significantly impairs functioning, work performance, and social interactions (12), imposing a substantial economic burden (12). Additionally, the condition adversely affects mental health, leading to emotional distress, reduced self-esteem, social isolation, and dissatisfaction with physical appearance (13). For individuals in physically demanding occupations, BCRL reduces work capacity and further diminishes their quality of life (14, 15). Effective management involves early symptom detection, clinical assessment, and objective measurements (16). Preventive strategies, including risk assessment, patient education, and early intervention, are essential for mitigating symptoms and improving quality of life (17–19).
As the most commonly diagnosed cancer worldwide, breast cancer poses a significant public health challenge (20), with BCRL being a critical concern (21). Despite advances in understanding and managing BCRL, research gaps persist, particularly regarding the integration of clinical practices with global research trends. Addressing these gaps is crucial for developing comprehensive clinical guidelines and improving patient care. Bibliometric analysis, which quantitatively evaluates academic literature, provides valuable insights into research productivity, thematic priorities, and collaborative networks within a field (22). This study employs bibliometric methods to examine the evolution of BCRL research, identify emerging themes, and analyze collaboration patterns (23). The findings aim to guide researchers, clinicians, and policymakers by highlighting areas requiring further investigation, ultimately contributing to better outcomes for breast cancer survivors.
2 Methods
2.1 Data source and processing
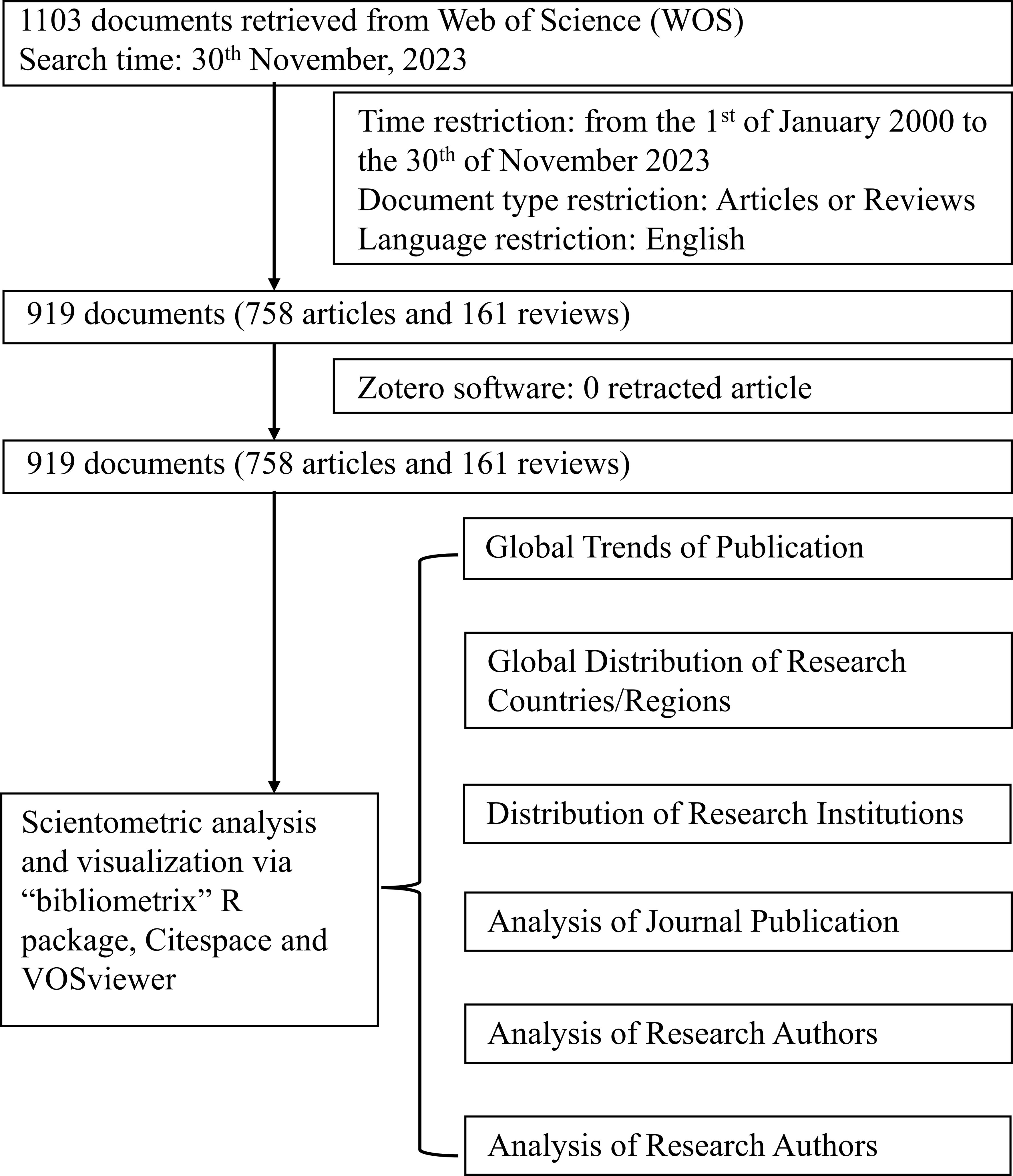
On November 30, 2023, data on the correlation between lymphedema and breast cancer were extracted from the Web of Science (WOS) database, which provides access to billions of cited references across various disciplines (24). The search covered publications from January 1, 2000, to November 30, 2023. The search parameters were configured as follows: Search In = “Web of Science Core Collection” and Editions = “Science Citation Index Expanded (SCI-EXPANDED)–1975-present.” Medical Subject Headings (MeSH) terms and entry terms such as “exosome” and “breast cancer” were employed as part of the search strategy. The search query was structured as follows: TS=(“Breast Neoplasm” OR “Breast Tumor” OR “Breast Cancer” OR “Mammary Cancer” OR “Breast Malignant Neoplasm” OR “Breast Malignant Tumor” OR “Breast Carcinoma”) AND TS=(“Breast Cancer Lymphedema” OR “Breast Cancer Treatment Related Lymphedema” OR “Breast Cancer Related Arm Lymphedema” OR “Breast Cancer Related Lymphedema” OR “Postmastectomy Lymphedema” OR “Post-mastectomy Lymphedema”). This search yielded 1,103 records. To refine the dataset, document types were limited to articles and reviews, and the language was restricted to English. After a detailed review, the dataset was reduced to 919 records, comprising 758 articles and 161 review articles. Exclusions were made based on specific criteria, including 102 meeting abstracts, 35 editorial materials, 26 letters, nine corrections, one book review, one expression of concern, and ten non-English publications. No retracted articles were identified using Zotero software. Ultimately, the final dataset consisted of 919 publications, with 758 articles (82.48%) and 161 review articles (17.52%).
2.2 Data analysis
The “Analyze Results” function in WOS was utilized to extract preliminary information, including publication years, document types, research areas, authors, affiliations, journals, publishers, countries/regions, languages, funding agencies, and open access status. For deeper analysis, the R package bibliometrix (version 4.3.1) was used to compute annual publication counts, analyze trending topics, and generate collaborative and thematic maps (25). CiteSpace (version 6.1), a visualization software developed by Chaomei Chen (27), was employed to conduct visual analyses, including identifying the top 50 references with the strongest citation bursts and performing dual-map overlay analyses. VOSviewer (version 1.6.18) was used to construct co-citation maps, analyze co-authorship patterns, and evaluate keyword co-occurrence networks. It also assessed collaboration networks among countries, institutions, and authors (26). Nodes in the visualizations represent individual entities, with colors indicating cluster membership. The size of each node reflects the count or frequency of entities within the cluster while connecting lines illustrate the strength of collaboration or co-occurrence between entities (27). The complete retrieval strategy, the number of identified records, and the analysis process are illustrated in Figure 1.
3 Results
3.1 Global publication trends
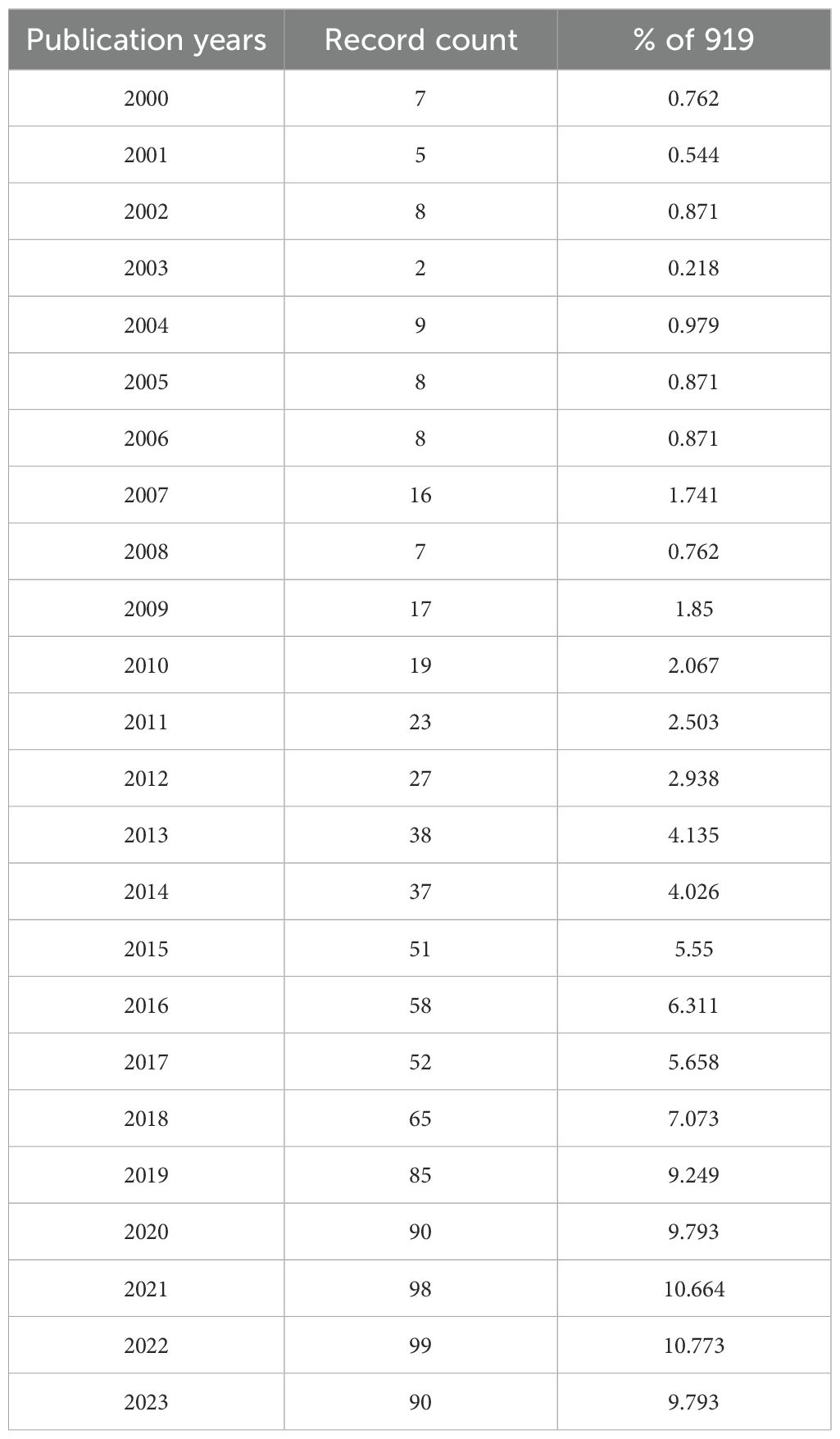
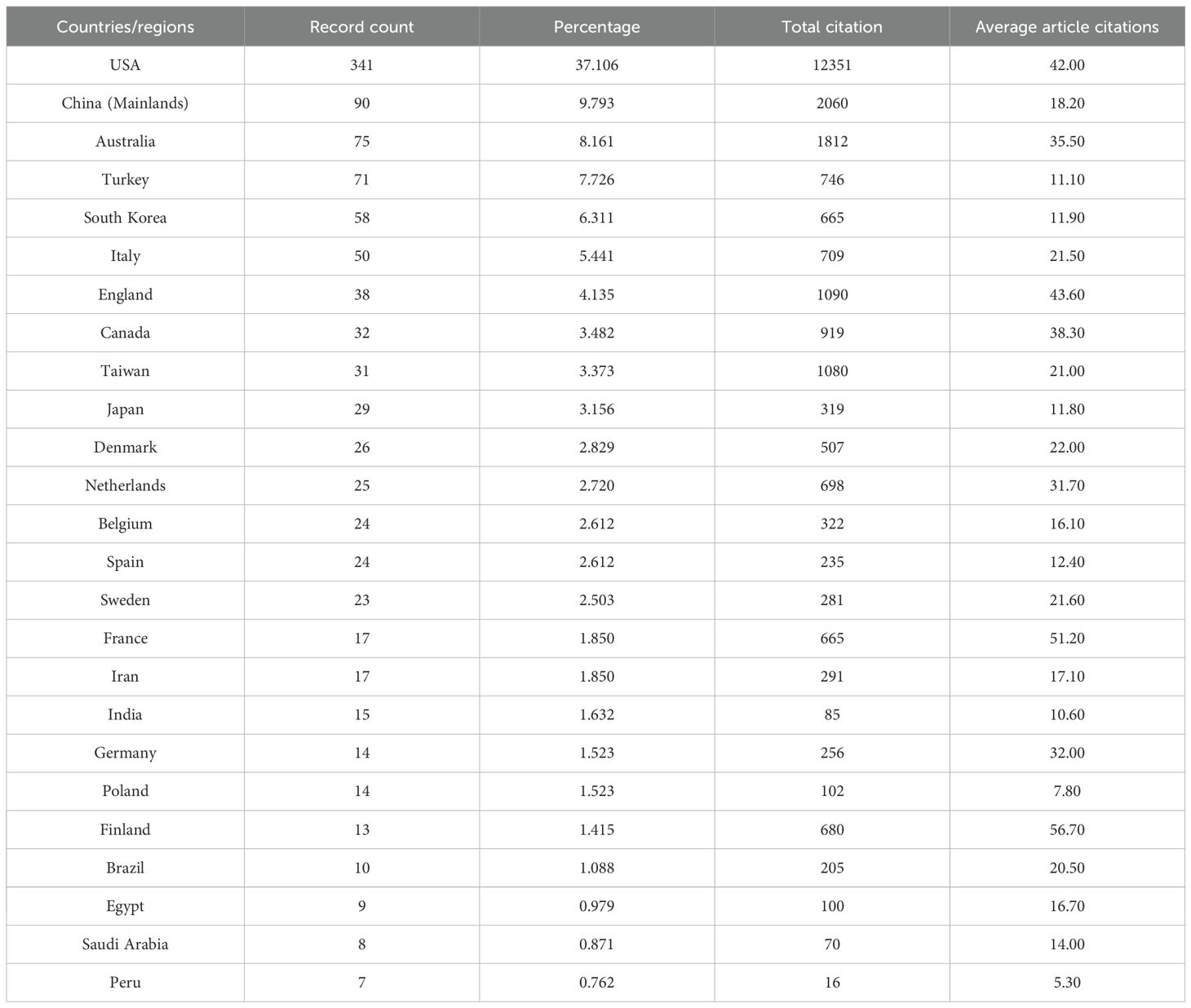
From January 1, 2000, to November 30, 2023, a total of 919 publications related to BCRL were retrieved from the WOS. This dataset included 758 articles (82.48%) and 161 review articles (17.52%). The annual distribution of these publications is presented in Table 1. As shown in Figure 2, the number of publications steadily increased from 7 (0.76%) in 2000 to a peak of 99 (10.77%) in 2022. The apparent decrease in 2023 reflects the data collection cutoff date of November 30, 2023. On average, 40 papers were published annually, with an average growth rate of 12.81%. Both annual and cumulative publication trends demonstrate exponential growth, underscoring the rapid development and heightened interest in this research area.
3.2 Global distribution of research countries/regions
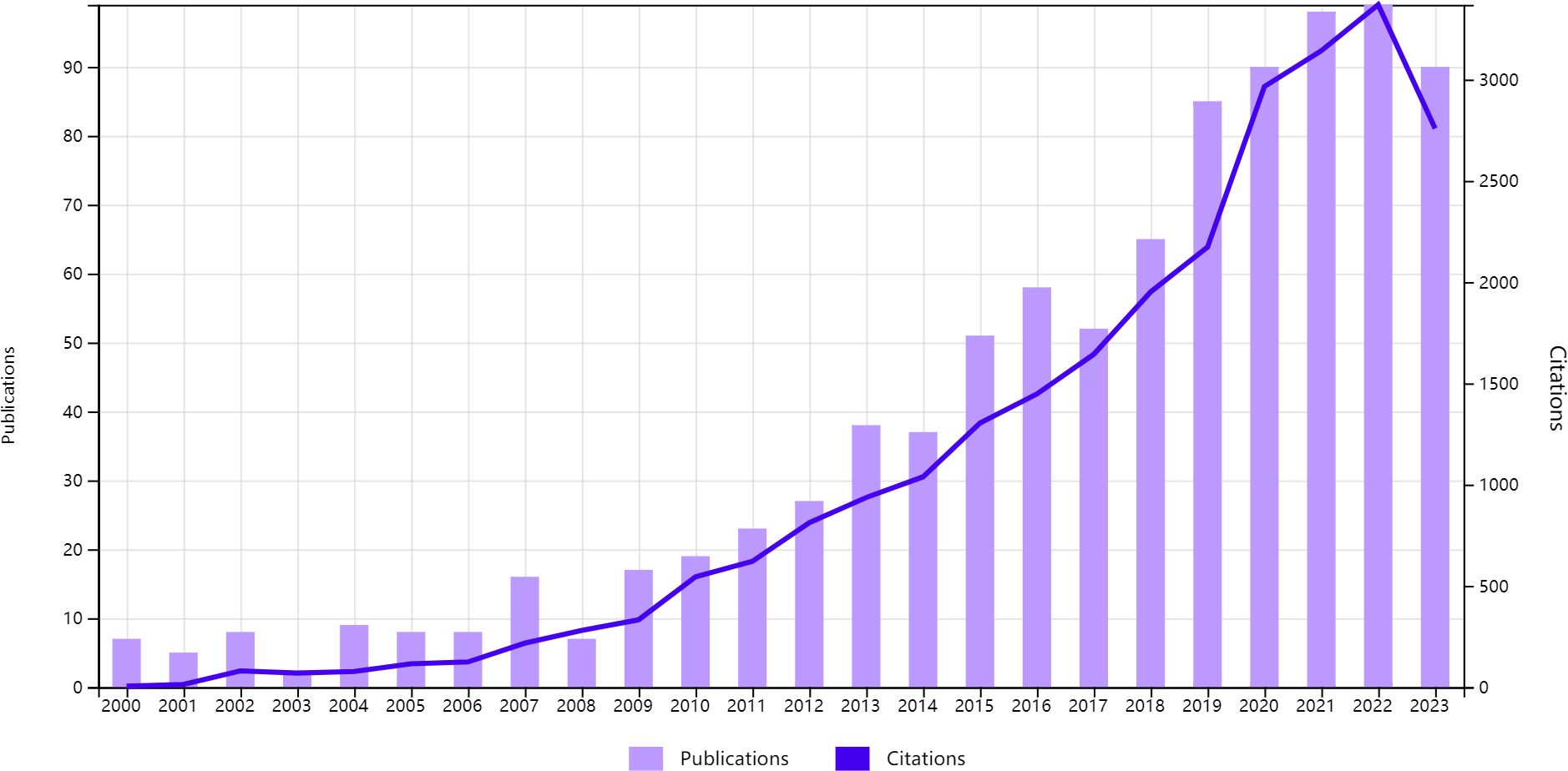
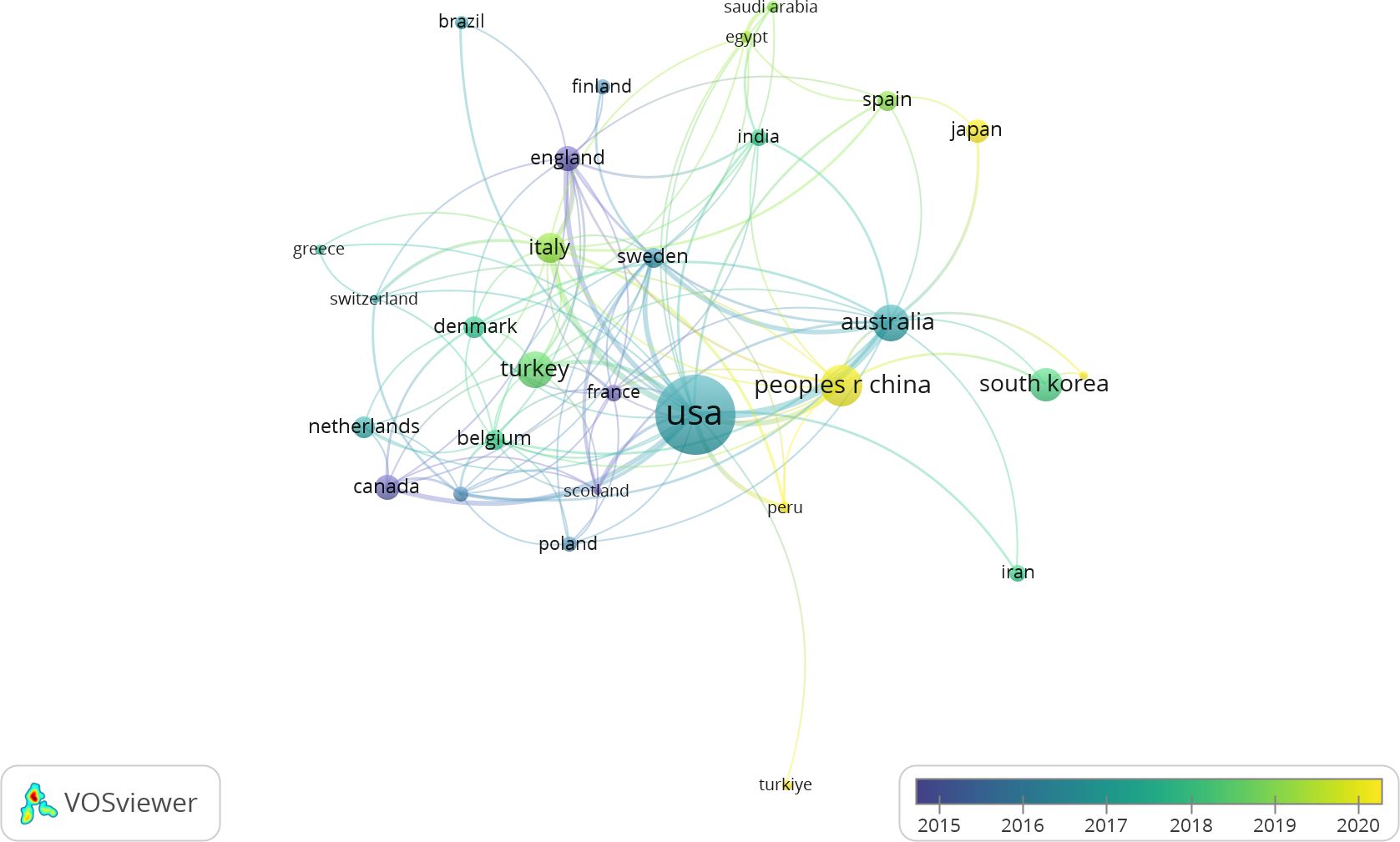
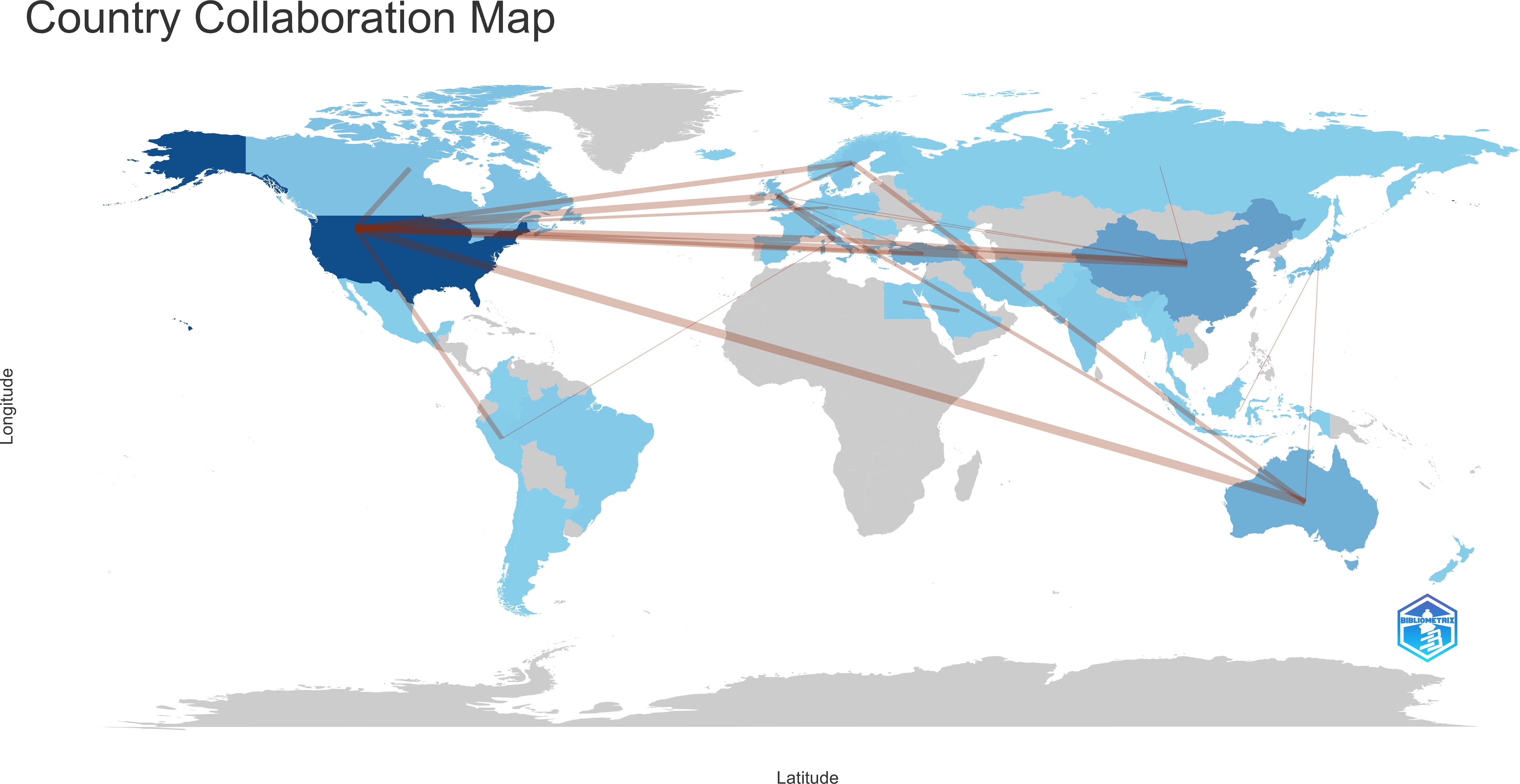
Between January 1, 2000, and November 30, 2023, 52 countries/regions contributed to this field. The top 25 contributors are detailed in Table 2, with the USA leading with 341 publications (37.11%), followed by China (90 publications, 9.79%) and Australia (75 publications, 8.16%). Among 29 countries/regions with at least five publications, an international collaborative network was identified (Figure 3). This network highlights extensive global collaboration, particularly among the USA, UK, Italy, and Australia. Initially, research was concentrated in developed countries such as England and Canada but later expanded to include the USA and Asian nations, especially China and Japan. Figure 4 presents a collaborative world map, which visually represents publication volumes and collaborative ties, with the USA dominating this research domain.
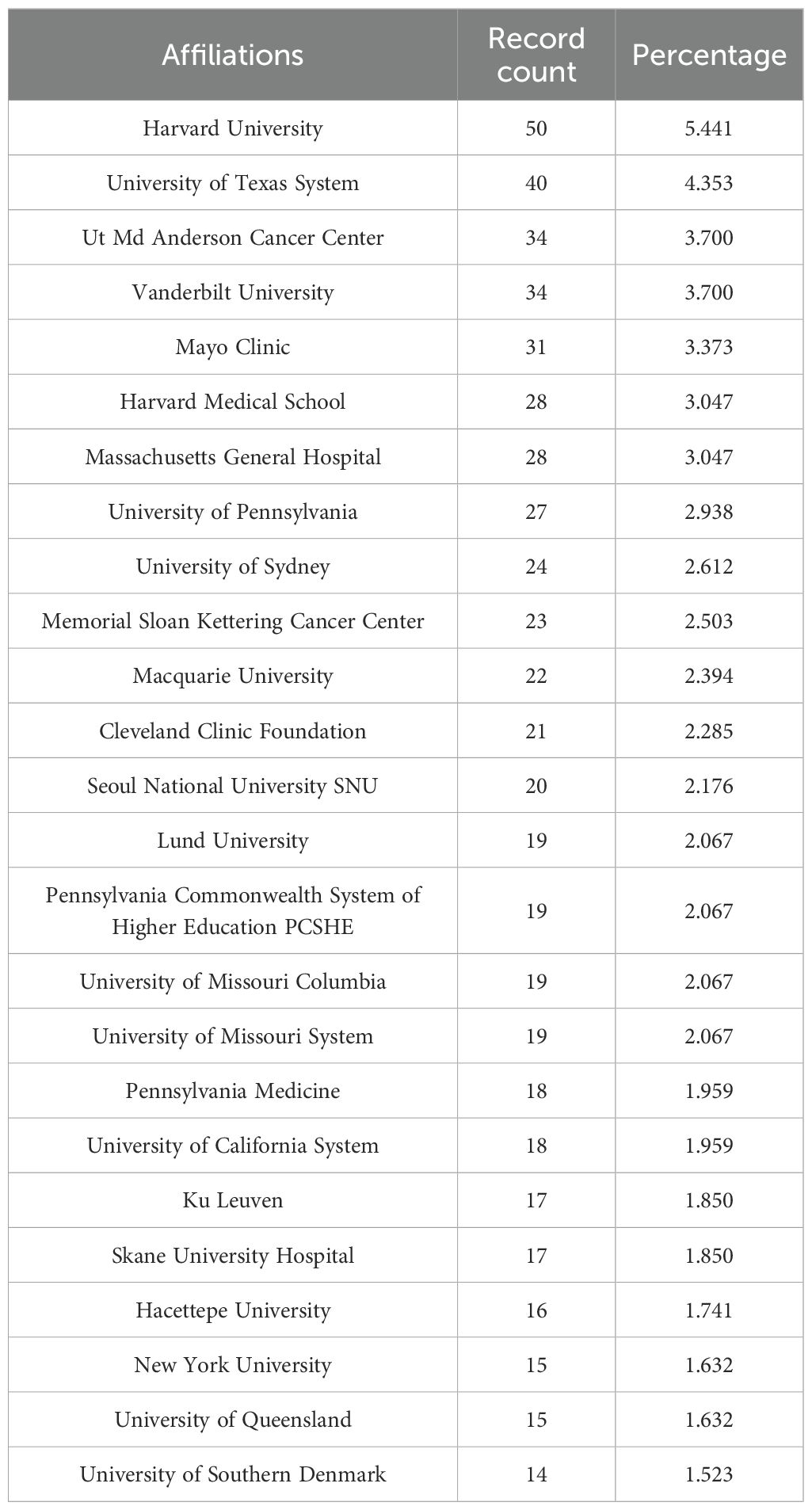
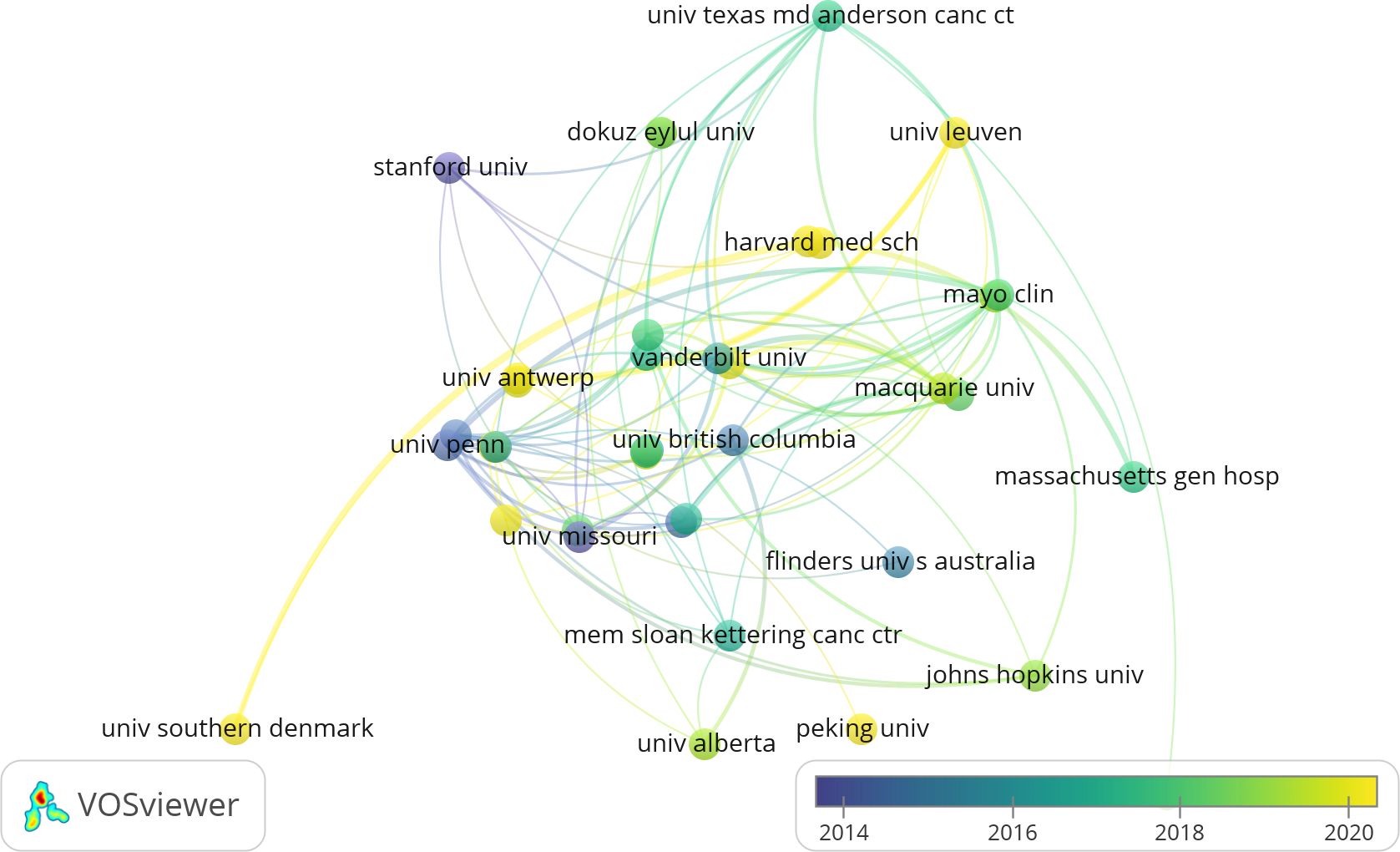
3.3 Distribution of research institutions
Between January 1, 2000, and November 30, 2023, 1,163 institutions were active in BCRL research. Thirteen institutions published 20 or more articles, with Harvard University (50 publications, 5.44%) and the University of Texas System (40 publications, 4.35%) leading the field (Table 3). Collaborative networks among 46 institutions with at least eight publications each are illustrated in Figure 5. Larger circles in the network represent institutions with higher publication counts, while the number of connecting lines reflects the degree of collaboration. Leading institutions included Vanderbilt University (34 publications), UT MD Anderson Cancer Center (32 publications), Mayo Clinic (29 publications), University of Pennsylvania (26 publications), and Memorial Sloan Kettering Cancer Center (23 publications). Recently, institutions such as Stanford University, the University of Pennsylvania, and the University of Missouri have initiated new studies, while the University of Southern Denmark and Peking University have emerged as active contributors.
3.4 Analysis of journals
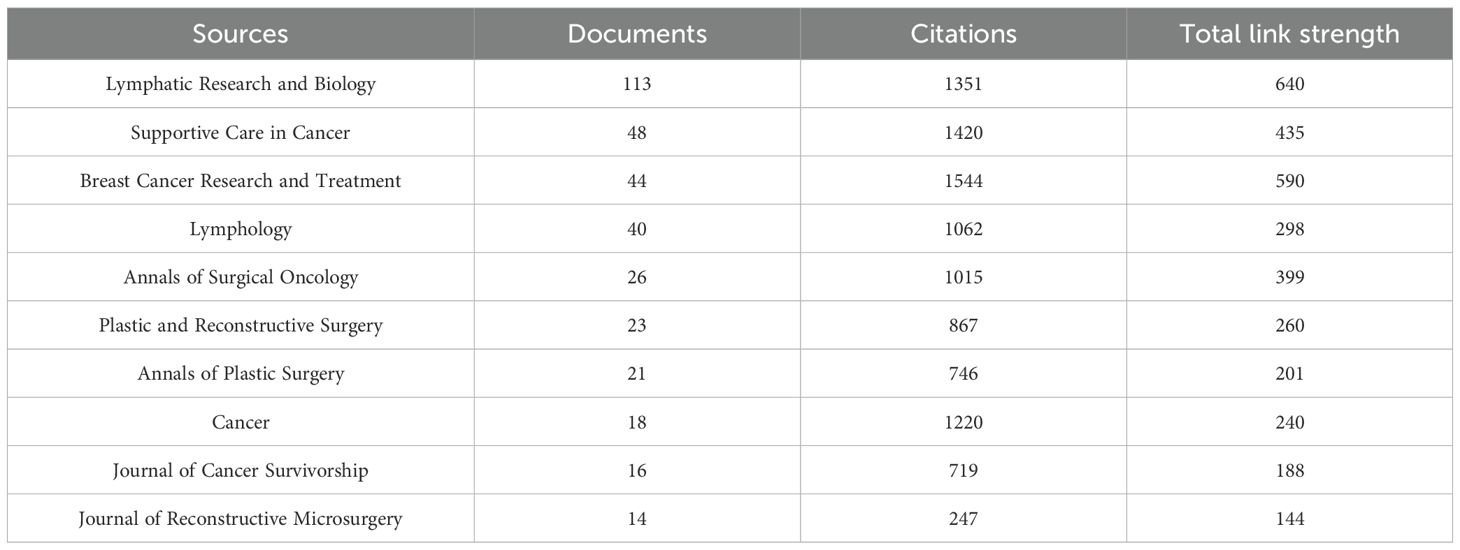
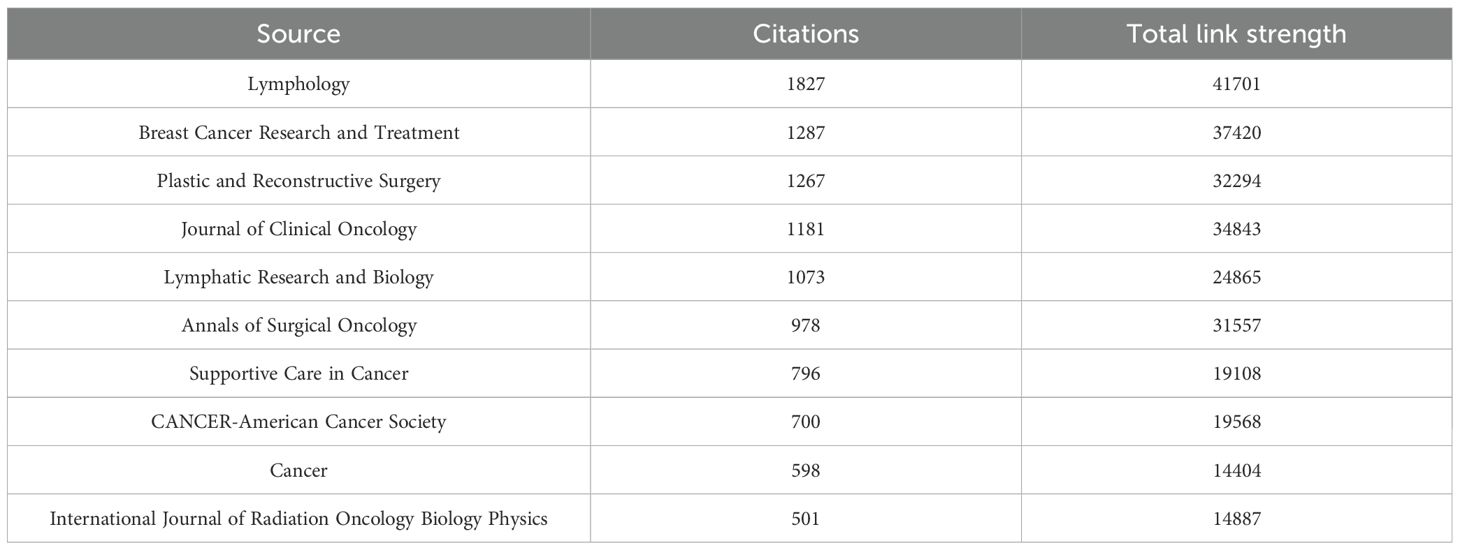
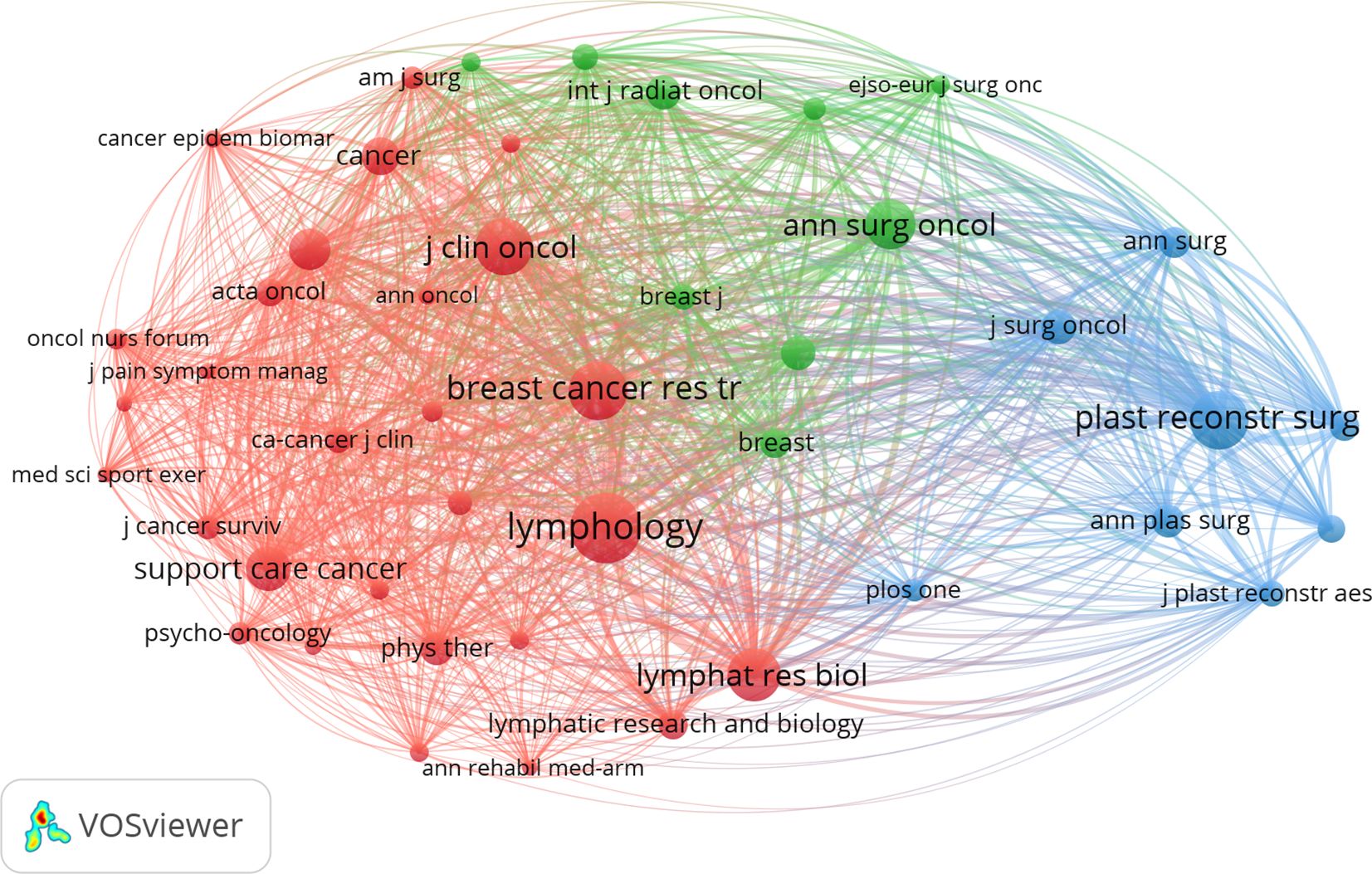
A total of 255 journals published research on BCRL. Table 4 lists the top ten journals by publication count, led by Lymphatic Research and Biology with 113 publications, followed by Supportive Care in Cancer (n=48) and Breast Cancer Research and Treatment (n=44). Journals such as Annals of Surgical Oncology, Plastic and Reconstructive Surgery, and Annals of Plastic Surgery primarily focus on surgical aspects of BCRL. Breast Cancer Research and Treatment had the highest citation count (1,544 citations), followed by Supportive Care in Cancer (1,420 citations). Cocitation analysis, conducted with a citation threshold of 120, identified 45 sources, with Lymphology as the most cited journal, followed by Breast Cancer Research and Treatment and Plastic and Reconstructive Surgery (Table 5). A network map (Figure 6) revealed three clusters, with Breast Cancer Research and Treatment forming the central node of the red cluster, which had the highest total link strength.
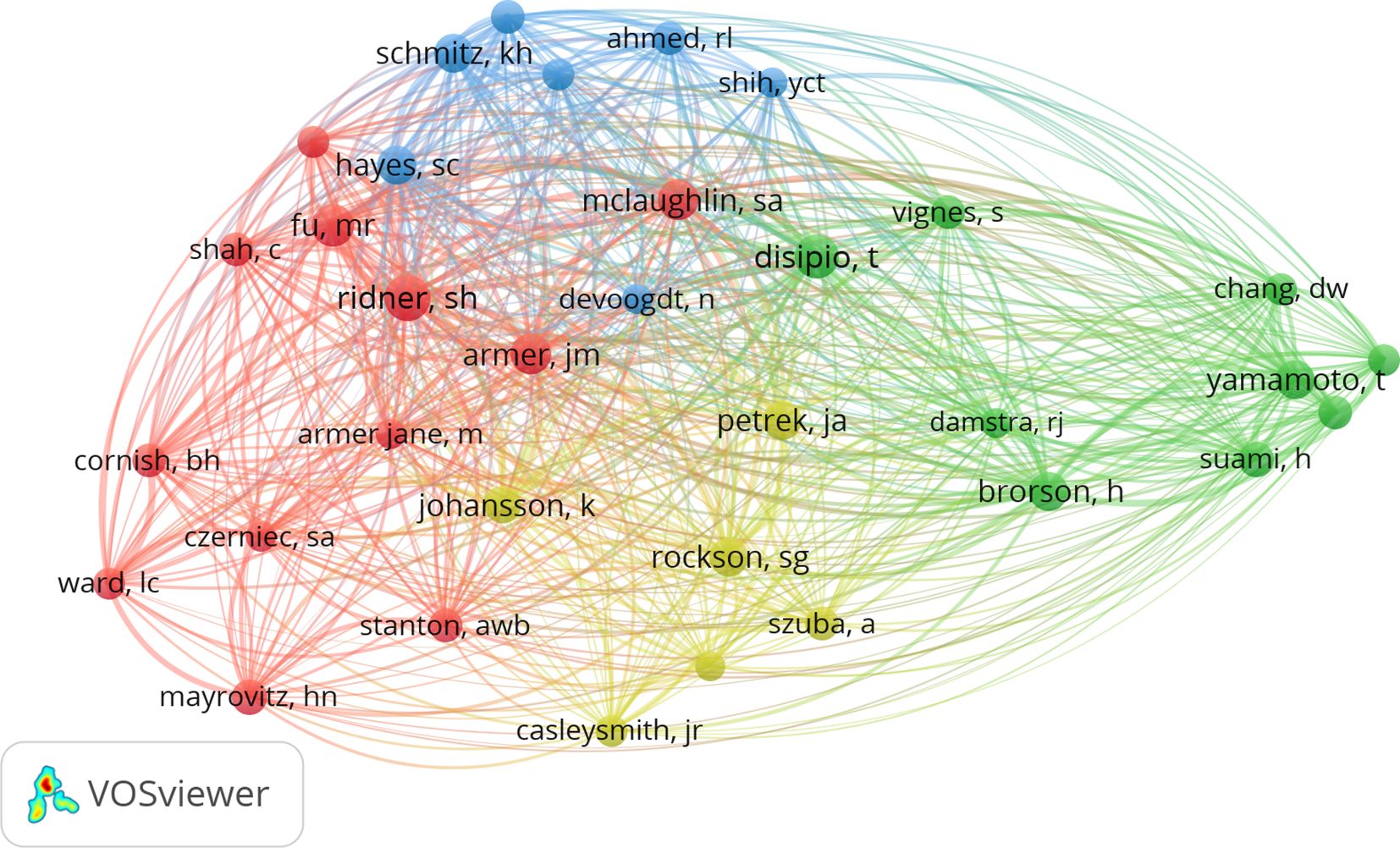
3.5 Analysis of research authors
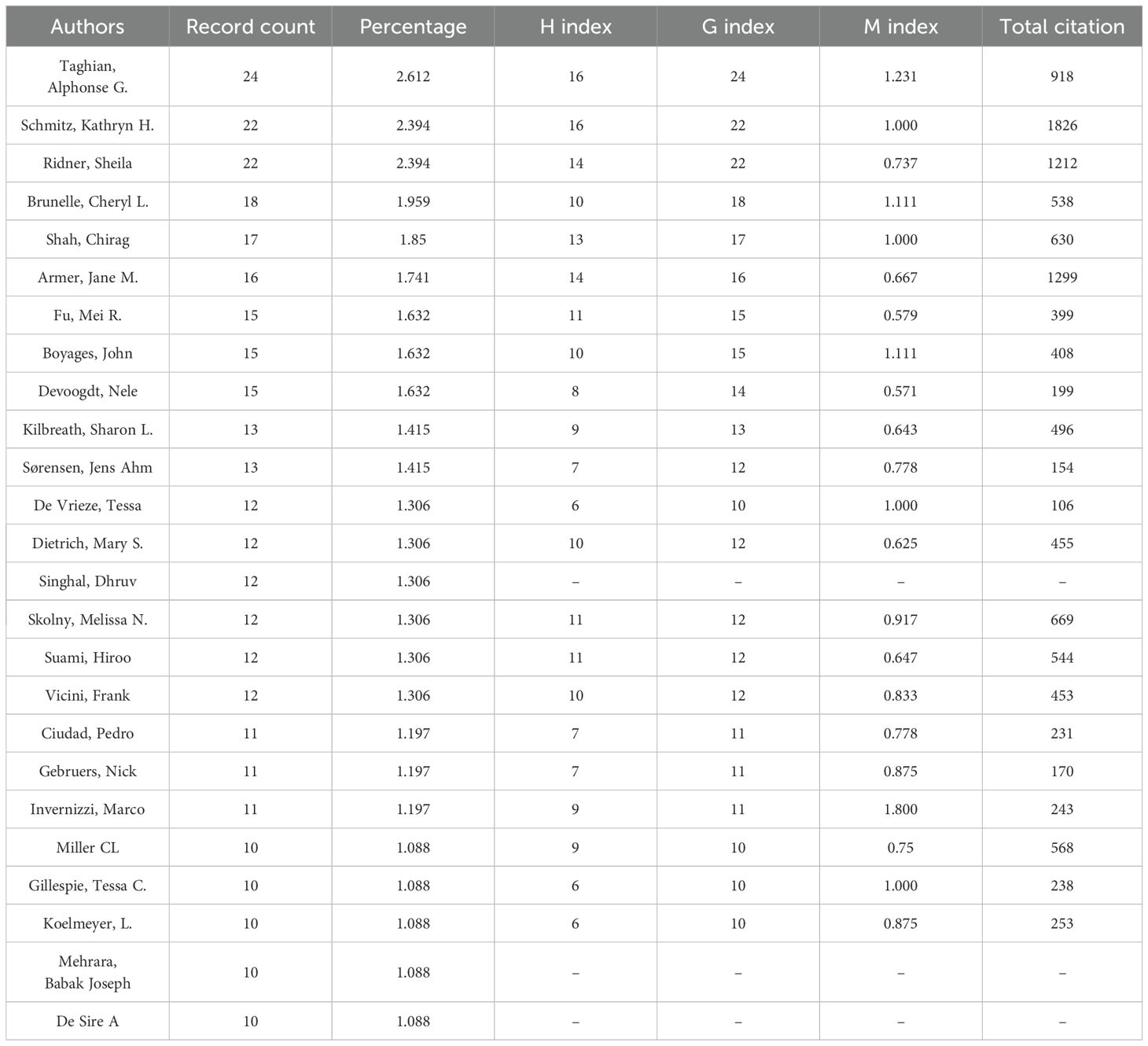
Between January 1, 2000, and November 30, 2023, 3,550 authors contributed to BCRL research (Table 6). The most prolific authors were Taghian, Alphonse G. (24 publications), Schmitz, Kathryn H., and Ridner, Sheila (22 publications each). Scientific productivity and impact were assessed using the h-index, g-index, and m-index (28). Taghian, Alphonse G. achieved the highest h-index with 16, g-index, and m-index among all authors. A cocitation network map (Figure 7) revealed collaborative patterns among these researchers.
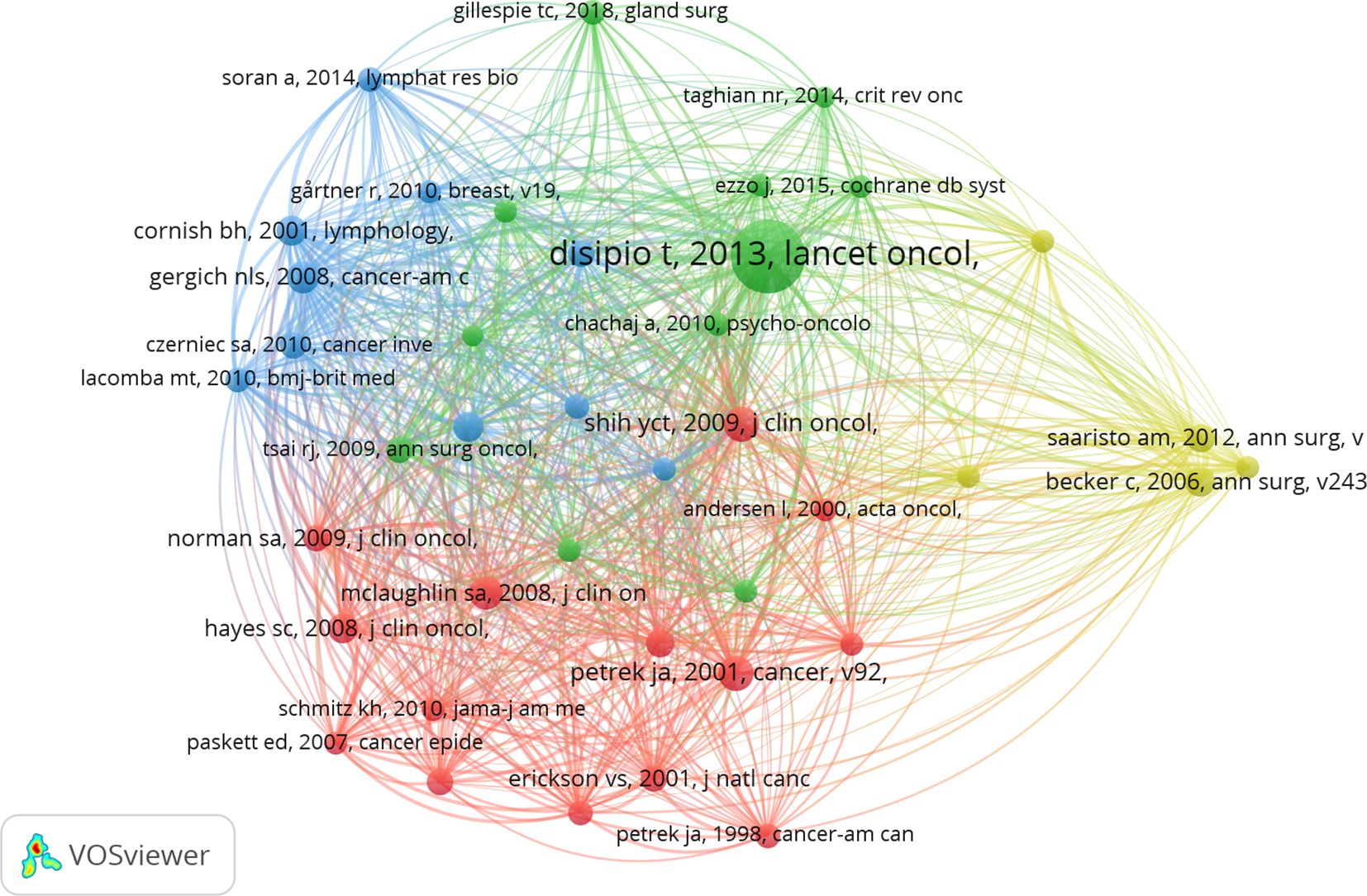
3.6 Analysis of publications
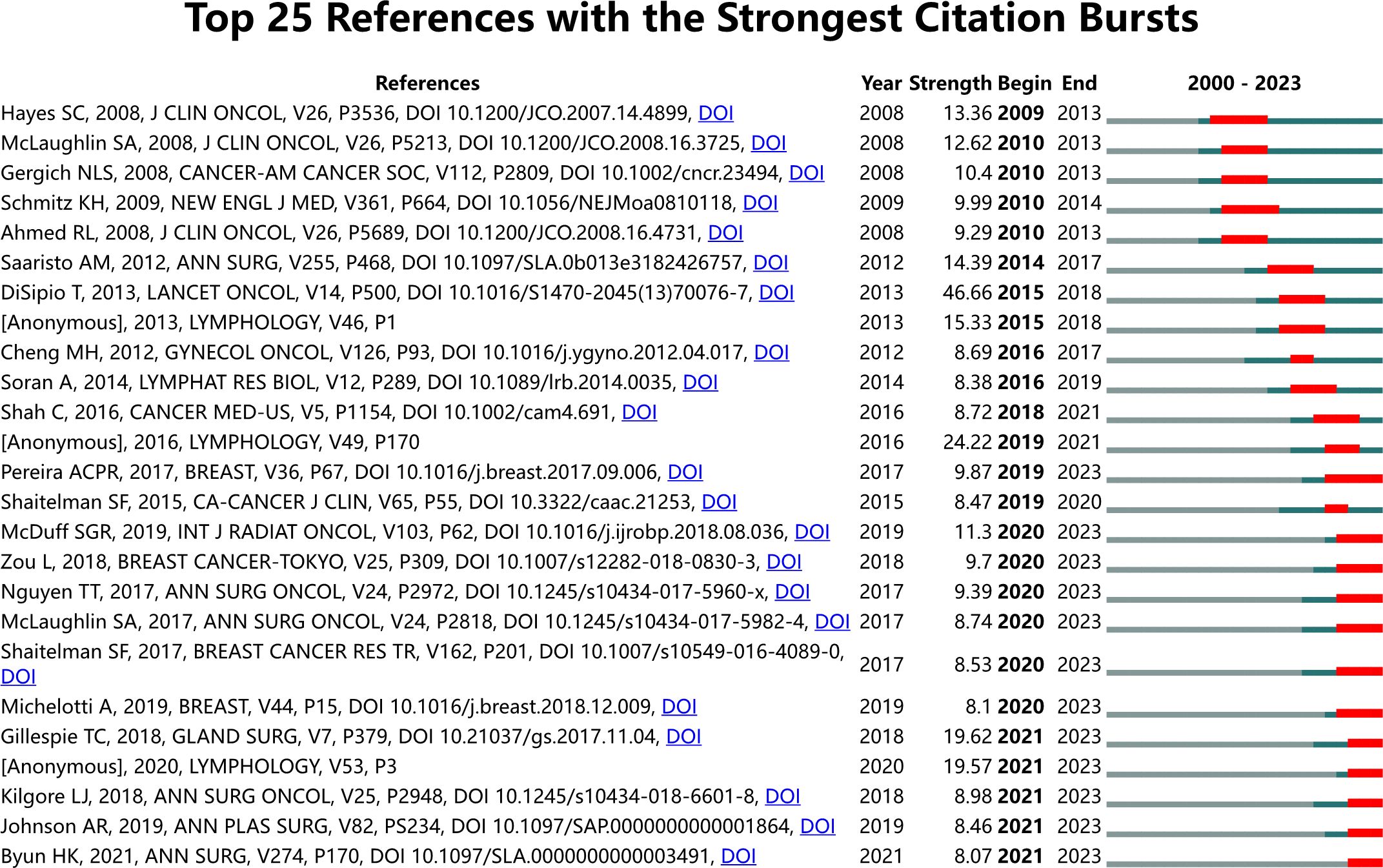
The top 10 publications ranked by global citation count are listed in Table 7. Anne G. Warren’s “Lymphedema: A Comprehensive Review,” published in Annals of Plastic Surgery in 2007, received the highest citation count, providing a systematic approach to evaluating and managing lymphedema patients. Schmitz, Kathryn H. authored two randomized controlled trials on the safety of weightlifting in women with BCRL. Cocitation analysis using VOSviewer identified 93,571 references across four clusters (Figure 8). The most frequently cited reference was Tracey DiSipio’s “Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis,” published in Lancet Oncology in 2013. This study, which included 72 articles, reported an overall arm lymphedema incidence of 17%. Citation burst analysis (Figure 9) identified references such as “Risk of Lymphedema Following Contemporary Treatment for Breast Cancer” as having ongoing influence in the field.
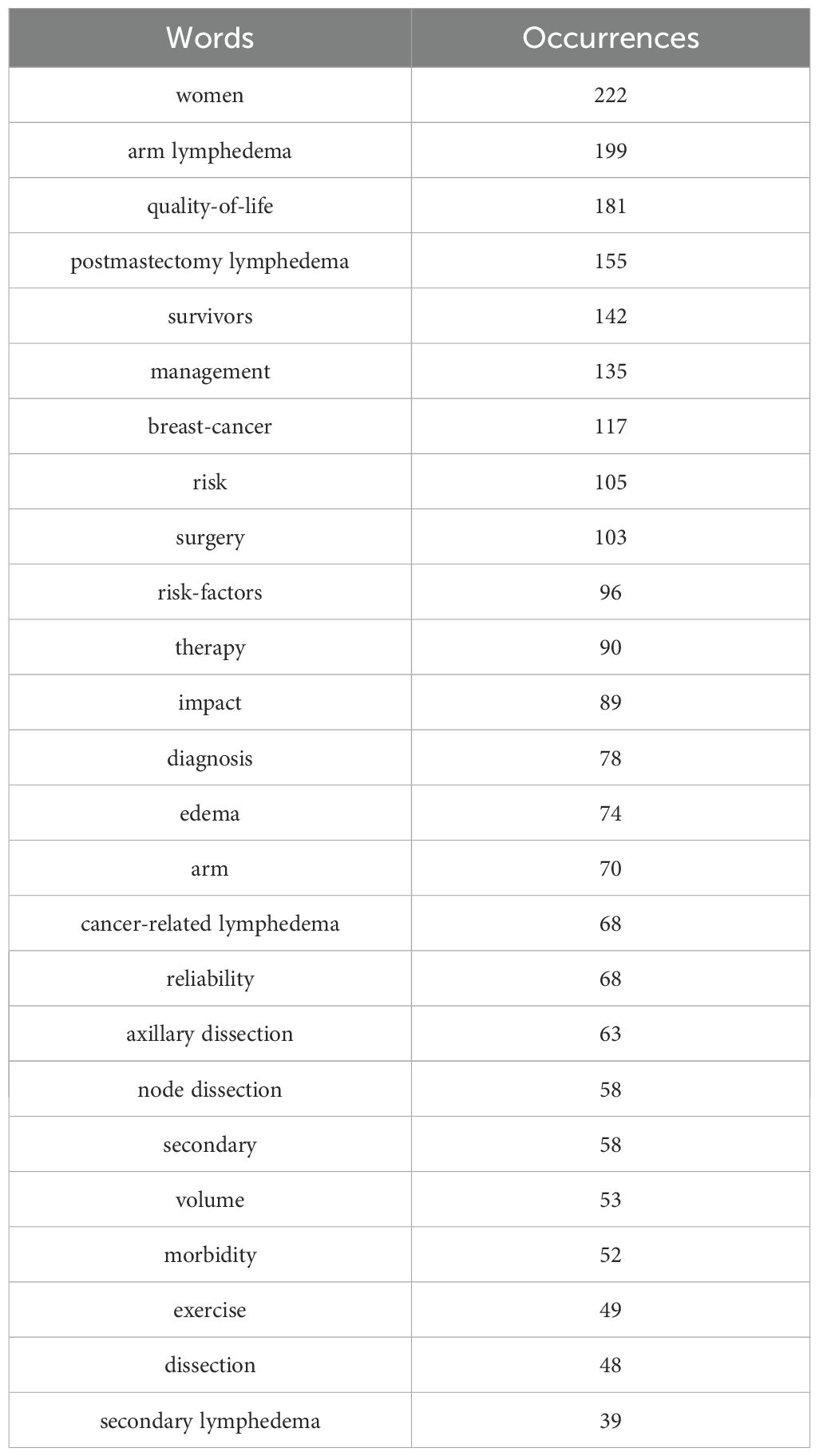
3.7 Analysis of keywords
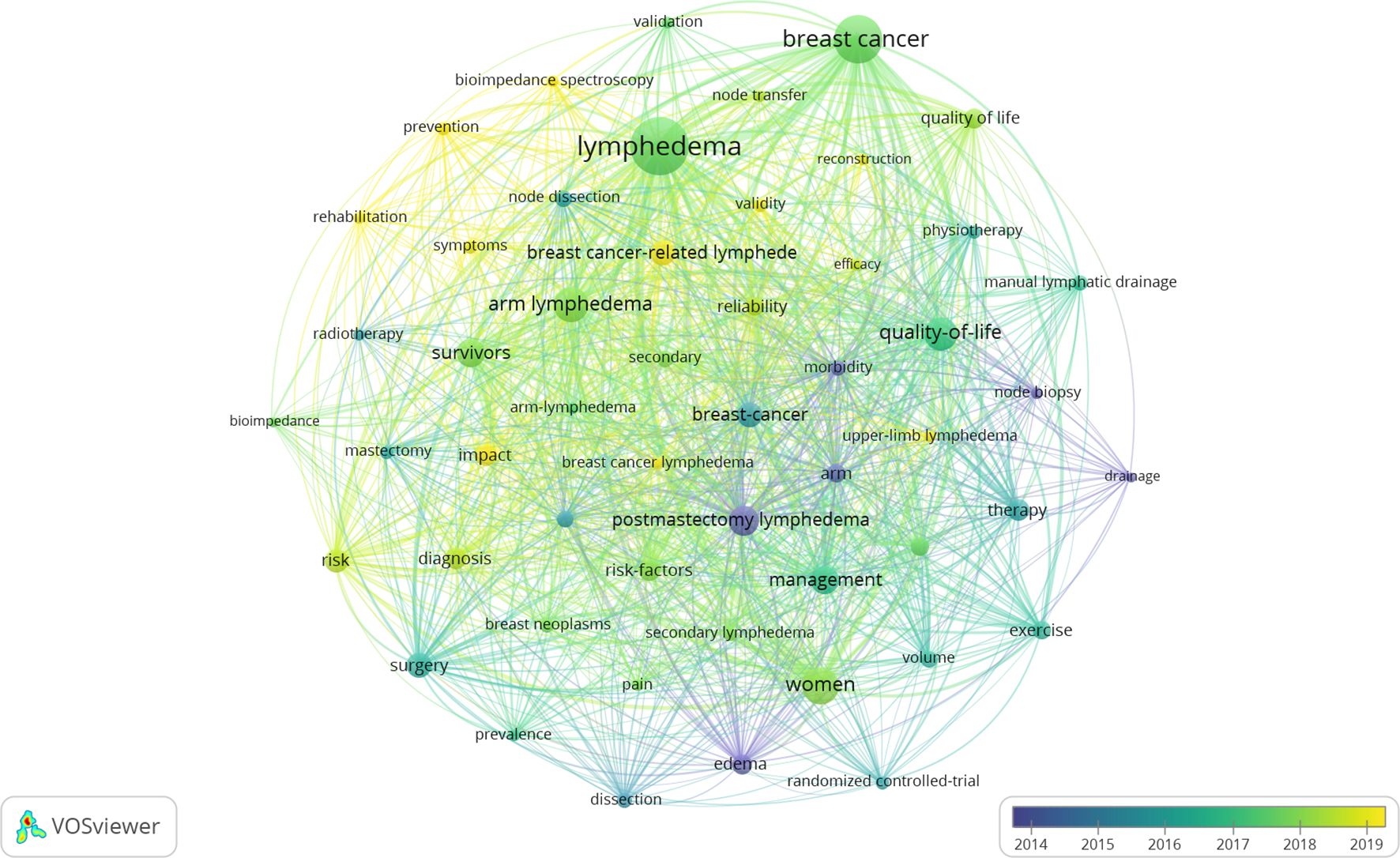
A total of 2,184 keywords were extracted from the collected records, providing insights into thematic evolution and research hotspots in breast cancer-related lymphedema (BCRL). The top 25 most frequently used keywords are presented in Table 8. Using VOSviewer, the 52 most common keywords were visualized with a minimum occurrence threshold set at 30 (Figure 10). Deeper shades in the visualization represent more frequently occurring keywords, while proximity to the central yellow block indicates higher citation frequency and relevance. Frequently appearing keywords included “lymphedema,” “breast cancer,” and “women,” underscoring their significance in the field over the past two decades. Other prominent terms included “arm lymphedema,” “quality of life,” and “postmastectomy lymphedema”. Co-occurrence analysis identified five thematic clusters: management and quality of life (15 in red), women’s surgery (13 in green), symptoms and validity (11 in blue), therapy (7 in yellow), and breast cancer-related lymphedema (6 in purple).
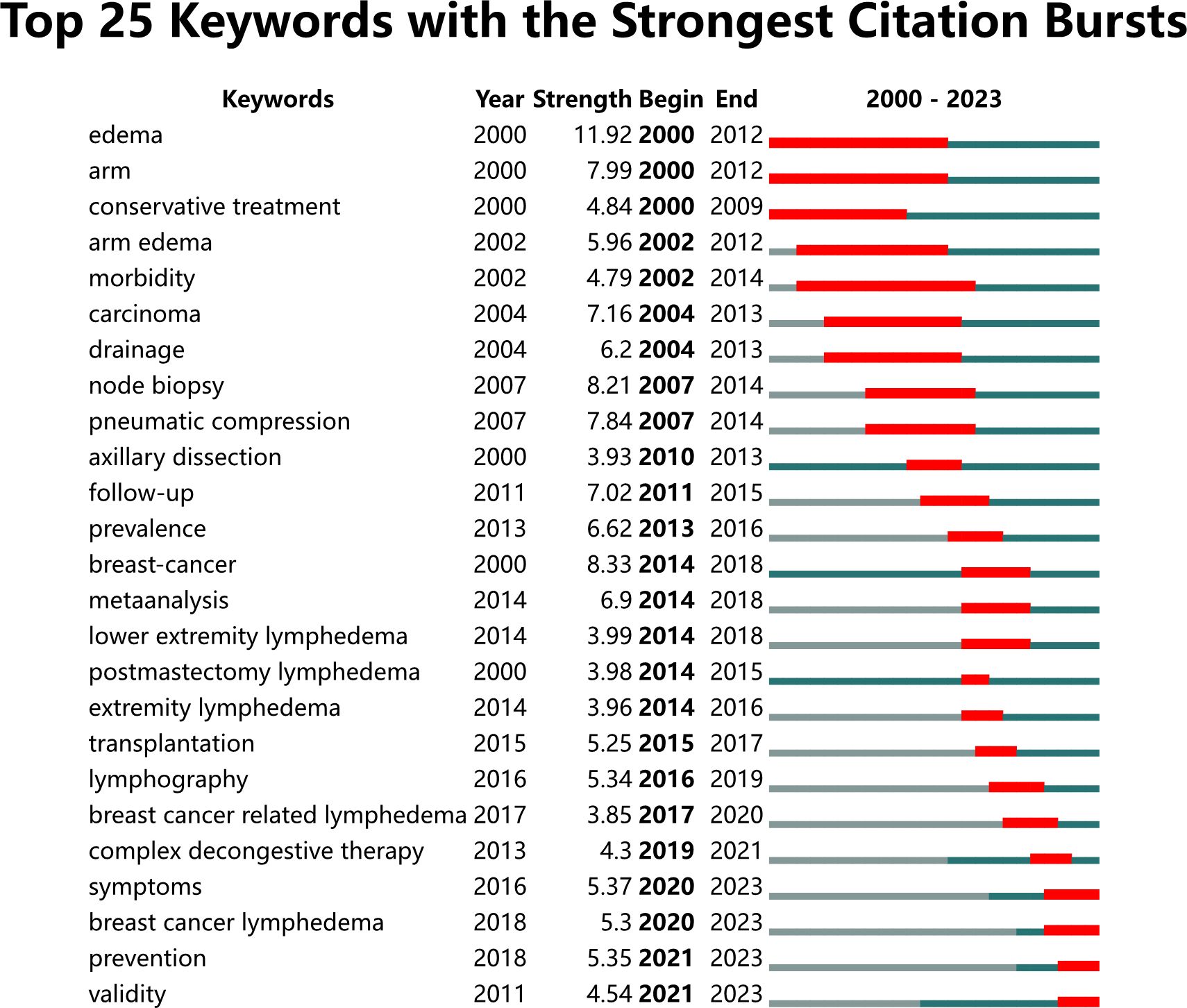
To explore emerging terms and research trends, an analysis of burst term keywords characterized by delayed emergence and extended influence was conducted. Twenty-five keywords with the strongest bursts were identified (Figure 11). The figure includes authors, publication years, and catalog information on the left, while burst-related metrics (burst value, start year of attention, and decline year) are listed on the right. From 2000 to 2023, significant keywords included “edema” (2000–2012), “arm” (2000–2012), “conservative treatment” (2000–2009), “arm edema” (2002–2012), “morbidity” (2002–2014), “carcinoma” (2004–2013), “drainage” (2004–2013), and “node biopsy” (2007–2014). Over the past 23 years, terms such as “edema,” “breast cancer,” and “node biopsy” displayed the most intense bursts, highlighting their prominence and marking pivotal areas for future research.
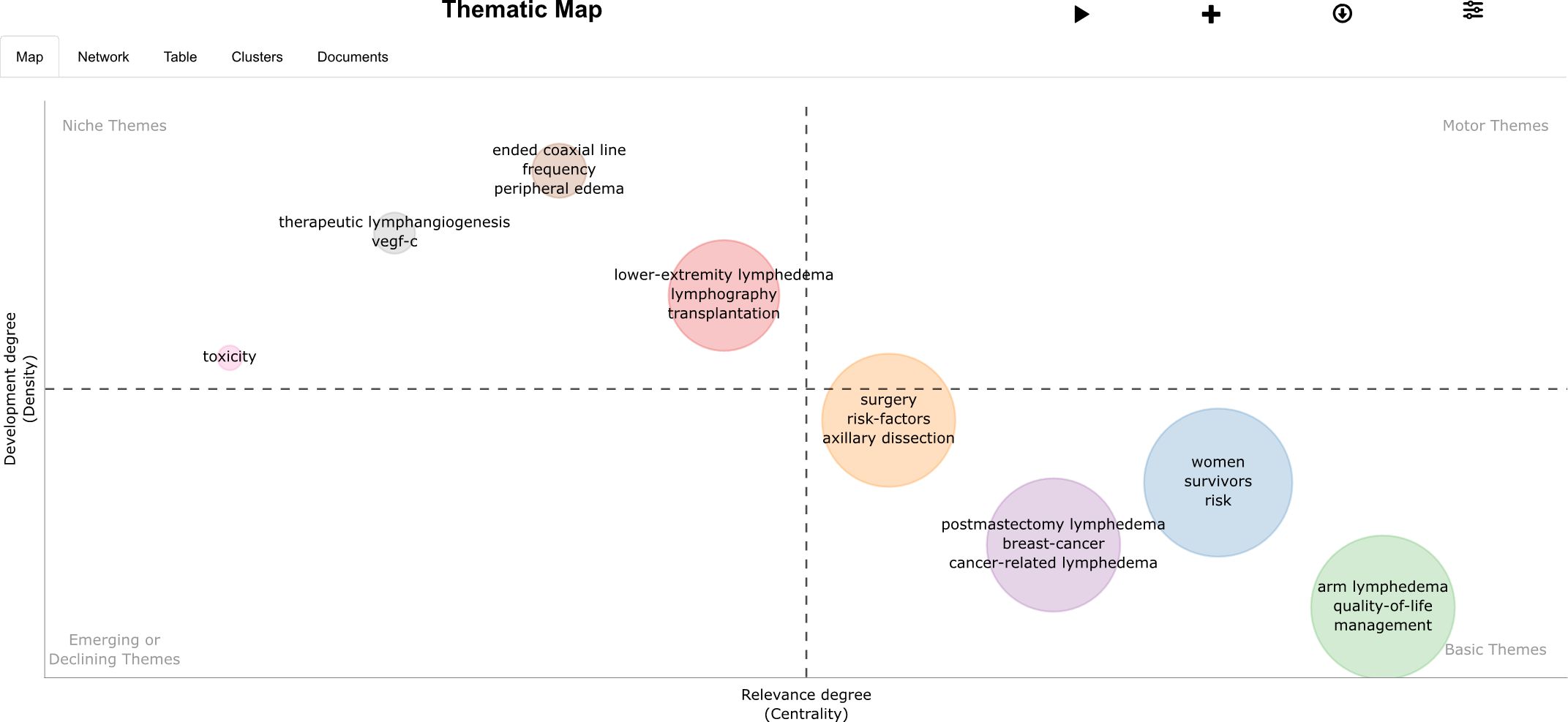
The thematic map of BCRL research (Figure 12) provides a comprehensive overview. The bottom-right corner represents foundational themes, such as surgery, women, postmastectomy lymphedema, and arm lymphedema, forming the core of this research field. The top-left quadrant highlights niche themes, such as therapeutic lymphangiogenesis and lower extremity lymphedema, reflecting specialized or cutting-edge research directions. This analysis identifies dominant trends and emerging research priorities, offering valuable perspectives for understanding the current state of BCRL research and guiding future studies.
3.8 Analysis of research categories
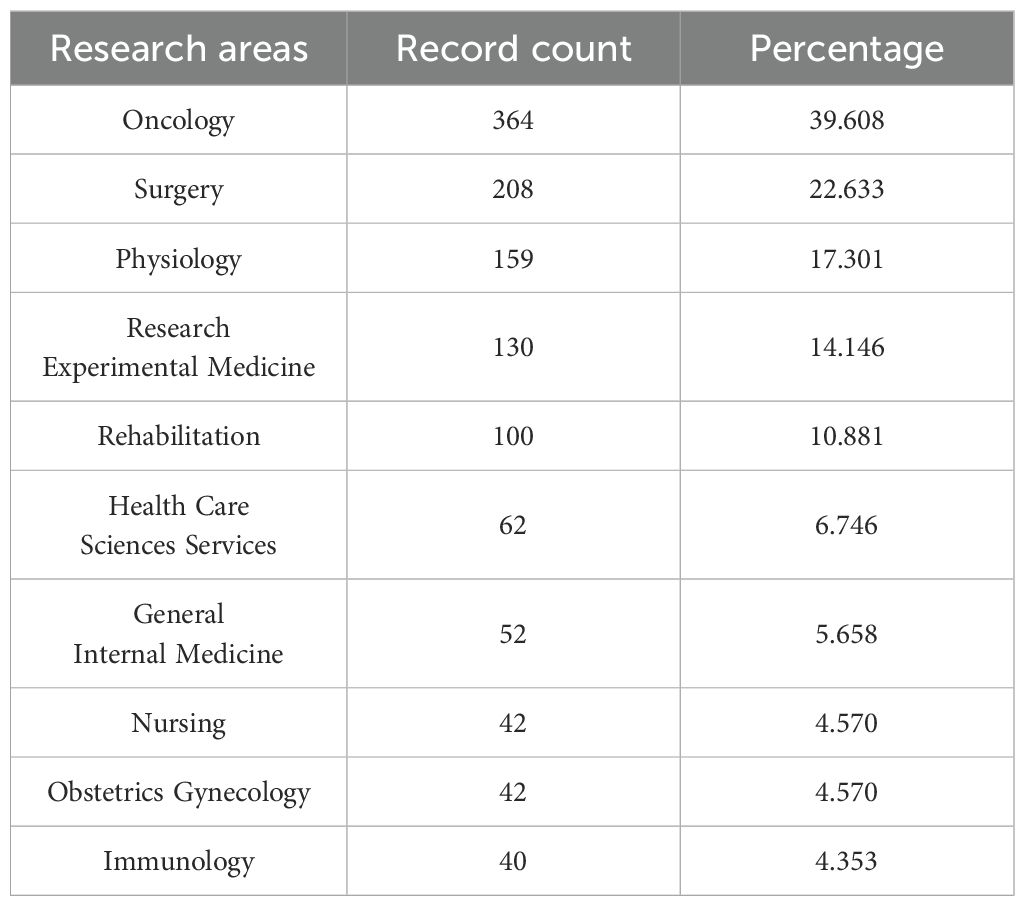
Eighty-one research categories were identified in this field. The top five categories by publication volume are listed in Table 9: “Oncology” (967 publications), “Cell Biology” (308 publications), “Biochemistry and Molecular Biology” (301 publications), “Endocrinology and Metabolism” (286 publications), and “Pathology” (170 publications).
4 Discussion
Unlike traditional literature reviews, bibliometric analysis systematically examines literature within a specific field (29), offering a structured approach to uncover collaboration networks, research trends, key interest areas, and potential developments. In this comprehensive bibliometric study, conducted from January 1, 2000, to November 30, 2023, we utilized R Studio and VOSviewer to map these elements in the context of BCRL. CiteSpace was employed to identify the top 25 citations and keywords with the strongest citation bursts. The analysis covered 919 records published in 255 journals by 3,550 authors affiliated with 1,163 institutions across 52 countries/regions. The findings reveal an increasing trend in publications, peaking in 2022 with 99 outputs, reflecting growing academic interest in the field. While the 2023 output appears lower, this is attributed to the cutoff date of November 30, 2023. The significant global impact of breast cancer, with 2.26 million new cases reported in 2020 (20), underscores the importance of research into its complications, such as lymphedema. As the most diagnosed cancer globally, breast cancer presents an urgent need for studies aimed at preventing and managing lymphedema to improve patient outcomes and quality of life. The increasing scholarly output mirrors deeper investigations into breast cancer survivors’ prognosis and a more nuanced understanding of lymphedema as a treatment-related complication.
The USA leads in publications, citations, and centrality, underscoring its influence and extensive international collaborations. Notable contributions from developing countries, especially China, signal promising progress in the field. However, disparities in publication volume between the USA and other countries/regions remain evident (30). Asian research teams should enhance their global impact by strengthening collaborations with European and American counterparts. Furthermore, institutions active in this field should foster stronger interconnections to support intensive studies on BCRL. Journals in this domain primarily focus on surgical procedures and cancer care, with “Lymphology” prominently emphasizing immunological aspects. Leading authors, such as Kathryn H. Schmitz and Alphonse G. Taghian, have made significant contributions, particularly in assessing the safety of upper-body exercise for breast cancer survivors with lymphedema and exploring the role of physical activity in prevention and rehabilitation (31, 32). The most cited articles in this bibliometric analysis focus on key aspects of BCRL, including arm edema in breast cancer patients, weightlifting safety, lymphedema management, and quality of life. These foundational works, primarily literature reviews published before 2012, continue to influence current research directions. Their enduring relevance highlights their importance as cornerstones in understanding and addressing BCRL, providing a basis for future advancements in the field.
Keyword analysis from 2000 to 2023 identified research hotspots and projected trends, particularly in postoperative arm swelling, the relationship between lymphedema and quality of life, and the effectiveness of management strategies. BCRL arises from treatments like surgery and radiotherapy as well as metastases, necessitating comprehensive management encompassing prevention, diagnosis, and treatment (33). Prevention begins with postoperative screening for BCRL risks, such as surgical techniques for lymph node resection, radiation exposure, and obesity (34). Education enables patients to recognize early symptoms (35), such as limb swelling and restricted mobility. Preventive measures include maintaining skin hygiene, avoiding trauma, and using compression cannulas to delay the onset of arm edema within the first year post-surgery (36, 37).
Diagnosis relies on self-reported symptoms, clinical evaluations, and the International Society of Lymphology (ISL) staging system (38), which classifies lymphedema into stages 0–III. Technological advancements, such as bioimpedance spectroscopy and low-level laser therapy, have improved early detection and management. Treatment focuses on early intervention, emphasizing gradual rehabilitation and avoiding strenuous activities (39). Complex decongestive therapy (CDT)—comprising manual lymph drainage, compression garments, skincare, and exercise—remains the primary treatment (40). However, evidence suggests no definitive superiority of any single treatment in reducing BCRL volume, indicating the need for further research to understand the efficacy of these components across lymphedema stages (41). Rehabilitation strategies, including deep breathing, aerobic exercises, and psychological support, play critical roles in improving patient outcomes and quality of life (42).
This study has several limitations. The limited time frame for data extraction excluded the most recent publications, and the focus on English-language journals may have missed valuable insights from non-English research. Using only the Web of Science (WOS) database may have overlooked relevant works in discipline-specific journals. Manual searches for author affiliation data introduced potential bias, and reliance on VOSviewer for first-author cocitation may have limited the scope of the analysis. Additionally, older articles may not fully represent the current research landscape.
Future studies should address these limitations by including non-English sources and additional databases, while adopting interdisciplinary approaches (43). Research should focus on prevention strategies, improving diagnostic methods, and evaluating long-term treatment efficacy. Exploring the impact of emerging technologies, such as telemedicine and wearable devices, as well as leveraging big data and AI (44), could improve BCRL management and patient quality of life. Collaboration across oncology, rehabilitation, and psychology fields is essential to address the multifaceted nature of BCRL.
5 Conclusion
This bibliometric analysis of breast cancer-related lymphedema research from 2000 to 2023 highlights a significant rise in scholarly activity over the past two decades. The USA leads in publication volume and influence, with Lymphology, Breast Cancer Research and Treatment, and Plastic and Reconstructive Surgery as the most productive journals. Alphonse G. Taghian stands out as a key contributor in this field. Despite advancements, challenges remain in developing effective treatments and prevention strategies. With the growing prevalence of breast cancer, addressing BCRL through targeted research in risk screening, prevention, and management is increasingly critical. Collaborative efforts will be essential to improving outcomes for affected patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Author contributions
LC: Writing – original draft. YZ: Writing – original draft. DZ: Writing – original draft. ZL: Writing – review & editing. HC: Writing – review & editing. CC: Writing – review & editing. SY: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This article is supported by the Medical and Health Category Project of Shantou Science and Technology Plan (NO. 210621096491127). Author Chen Ling has received research support from it.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Grada AA, Phillips TJ. Lymphedema. J Am Acad Dermatol. (2017) 77:1009–20. doi: 10.1016/j.jaad.2017.03.022
2. Lawenda BD, Mondry TE, Johnstone PAS. Lymphedema: A primer on the identification and management of a chronic condition in oncologic treatment. CA: A Cancer J Clin. (2009) 59:8–24. doi: 10.3322/caac.20001
3. DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. (2013) 14:500–15. doi: 10.1016/S1470-2045(13)70076-7
4. Byun HK, Chang JS, Im SH, Kirova YM, Arsene-Henry A, Choi SH, et al. Risk of lymphedema following contemporary treatment for breast cancer: an analysis of 7617 consecutive patients from a multidisciplinary perspective. Ann Surg. (2021) 274:170–8. doi: 10.1097/SLA.0000000000003491
5. Sung H, Rosenberg PS, Chen W-Q, Hartman M, Lim W-y, Chia KS, et al. Female breast cancer incidence among Asian and western populations: more similar than expected. JNCI: J Natl Cancer Instit. (2015) 107. doi: 10.1093/jnci/djv107
6. Abouelazayem M, Elkorety M, Monib S. Breast lymphedema after conservative breast surgery: an up-to-date systematic review. Clin Breast Cancer. (2021) 21:156–61. doi: 10.1016/j.clbc.2020.11.017
7. Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zamba GK, Scott-Conner C. The risk of developing arm lymphedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol. (2009) 16:1959–72. doi: 10.1245/s10434-009-0452-2
8. Shen A, Lu Q, Fu X, Wei X, Zhang L, Bian J, et al. Risk factors of unilateral breast cancer-related lymphedema: an updated systematic review and meta-analysis of 84 cohort studies. Support Care Cancer. (2022) 31(1):18. doi: 10.1007/s00520-022-07508-2
9. Warren AG, Brorson H, Borud LJ, Slavin SA. Lymphedema. Ann Plast Surge. (2007) 59:464–72. doi: 10.1097/01.sap.0000257149.42922.7e
10. Brunelle CL, Roberts SA, Horick NK, Gillespie TC, Jacobs JM, Daniell KM, et al. Integrating symptoms into the diagnostic criteria for breast cancer–related lymphedema: applying results from a prospective surveillance program. Phys Ther. (2020) 100:2186–97. doi: 10.1093/ptj/pzaa162
11. Pappalardo M, Starnoni M, Franceschini G, Baccarani A, De Santis G. Breast cancer-related lymphedema: recent updates on diagnosis, severity and available treatments. J Personal Med. (2021) 11:402. doi: 10.3390/jpm11050402
12. De Vrieze T, Gebruers N, Nevelsteen I, Tjalma WAA, Thomis S, De Groef A, et al. Breast cancer-related lymphedema and its treatment: how big is the financial impact? Support Care Cancer. (2020) 29:3801–13. doi: 10.1007/s00520-020-05890-3
13. Gandhi A, Xu T, DeSnyder SM, Smith GL, Lin R, Barcenas CH, et al. Prospective, early longitudinal assessment of lymphedema-related quality of life among patients with locally advanced breast cancer: The foundation for building a patient-centered screening program. Breast. (2023) 68:205–15. doi: 10.1016/j.breast.2023.02.011
14. Gärtner R, Jensen M-B, Kronborg L, Ewertz M, Kehlet H, Kroman N. Self-reported arm-lymphedema and functional impairment after breast cancer treatment – A nationwide study of prevalence and associated factors. Breast. (2010) 19:506–15. doi: 10.1016/j.breast.2010.05.015
15. Vignes S, Fau-Prudhomot P, Simon L, Sanchez-Bréchot M-L, Arrault M, Locher F. Impact of breast cancer–related lymphedema on working women. Support Care Cancer. (2019) 28:79–85. doi: 10.1007/s00520-019-04804-2
16. Kassamani YW, Brunelle CL, Gillespie TC, Bernstein MC, Bucci LK, Nassif T, et al. Diagnostic criteria for breast cancer-related lymphedema of the upper extremity: the need for universal agreement. Ann Surg Oncol. (2022) 29:989–1002. doi: 10.1245/s10434-021-10645-3
17. McEvoy MP, Ravetch E, Patel G, Fox J, Feldman S. Prevention of breast cancer-related lymphedema. Clin Breast Cancer. (2021) 21:128–42. doi: 10.1016/j.clbc.2021.02.009
18. Armer JM, Ostby PL, Ginex PK, Beck M, Deng J, Fu MR, et al. ONS guidelines™ for cancer treatment-related lymphedema. Oncol Nurs Forum. (2020) 47:518–38. doi: 10.1188/20.ONF.518-538
19. Perdomo M, Davies C, Levenhagen K, Ryans K, Gilchrist L. Patient education for breast cancer–related lymphedema: a systematic review. J Cancer Survivorship. (2023) 17:384–98. doi: 10.1007/s11764-022-01262-4
20. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
21. Hayes SC, Janda M, Cornish B, Battistutta D, Newman B. Lymphedema after breast cancer: incidence, risk factors, and effect on upper body function. J Clin Oncol. (2008) 26:3536–42. doi: 10.1200/JCO.2007.14.4899
22. Lim WM, Kumar S. Guidelines for interpreting the results of bibliometric analysis: A sensemaking approach. Global Business Org Excell. (2024) 43:17–26. doi: 10.1002/joe.22229
23. Donthu N, Kumar S, Mukherjee D, Pandey N, Lim WM. How to conduct a bibliometric analysis: An overview and guidelines. J Business Res. (2021) 133:285–96. doi: 10.1016/j.jbusres.2021.04.070
24. Wu H, Li Y, Tong L, Wang Y, Sun Z. Worldwide research tendency and hotspots on hip fracture: a 20-year bibliometric analysis. Arch Osteo. (2021) 16:73. doi: 10.1007/s11657-021-00929-2
25. Darvish H. Bibliometric analysis using bibliometrix an R package. J Scientom Res. (2020) 8:156–60. doi: 10.5530/jscires.8.3.32
26. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. (2009) 84:523–38. doi: 10.1007/s11192-009-0146-3
27. Perianes-Rodriguez A, Waltman L, van Eck NJ. Constructing bibliometric networks: A comparison between full and fractional counting. J Inform. (2016) 10:1178–95. doi: 10.1016/j.joi.2016.10.006
28. Schreiber WE, Giustini DM. Measuring scientific impact with the h-index. Am J Clin Pathol. (2018) 151:286–91. doi: 10.1093/ajcp/aqy137
29. Kokol P, Blažun Vošner H, Završnik J. Application of bibliometrics in medicine: a historical bibliometrics analysis. Health Inf Libraries J. (2020) 38:125–38. doi: 10.1111/hir.12295
30. Zhang Y, Zhang X, Wang X-y, Han DM, Du J-S. Visual analysis of global research output of lymphedema based on bibliometrics. Front Oncol. (2022) 12. doi: 10.3389/fonc.2022.926237
31. Schmitz KH, Ahmed RL, Troxel AB, Cheville A, Lewis-Grant L, Smith R, et al. Weight lifting for women at risk for breast cancer–related lymphedema. JAMA. (2010) 304:2699. doi: 10.1001/jama.2010.1837
32. Schmitz KH, Ahmed RL, Troxel A, Cheville A, Smith R, Lewis-Grant L, et al. Weight lifting in women with breast-cancer–related lymphedema. New Engl J Med. (2009) 361:664–73. doi: 10.1056/NEJMoa0810118
33. McLaughlin SA, DeSnyder SM, Klimberg S, Alatriste M, Boccardo F, Smith ML, et al. Considerations for clinicians in the diagnosis, prevention, and treatment of breast cancer-related lymphedema, recommendations from an expert panel: part 2: preventive and therapeutic options. Ann Surg Oncol. (2017) 24:2827–35. doi: 10.1245/s10434-017-5964-6
34. Liu Y-f, Liu J-E, Zhu Y, Mak YW, Qiu H, Liu L-h, et al. Development and validation of a nomogram to predict the risk of breast cancer-related lymphedema among Chinese breast cancer survivors. Support Care Cancer. (2021) 29(9):5435–45. doi: 10.1007/s00520-021-06122-y
35. Liu X, Sun K, Yang H, Xia L, Lu K, Meng X, et al. Risk factors for the development of severe breast cancer-related lymphedema: a retrospective cohort study. BMC Cancer. (2023) 23(1):361. doi: 10.1186/s12885-023-10814-5
36. Paramanandam VS, Dylke E, Clark GM, Daptardar AA, Kulkarni AM, Nair NS, et al. Prophylactic use of compression sleeves reduces the incidence of arm swelling in women at high risk of breast cancer–related lymphedema: A randomized controlled trial. J Clin Oncol. (2022) 40:2004–12. doi: 10.1200/JCO.21.02567
37. McEvoy MP, Gomberawalla A, Smith M, Boccardo FM, Holmes D, Djohan R, et al. The prevention and treatment of breast cancer- related lymphedema: A review. Front Oncol. (2022) 12. doi: 10.3389/fonc.2022.1062472
38. International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology. Lymphology. (2013) 46:1–11.
39. Hasenoehrl T, Palma S, Ramazanova D, Kölbl H, Dorner TE, Keilani M, et al. Resistance exercise and breast cancer–related lymphedema—a systematic review update and meta-analysis. Support Care Cancer. (2020) 28:3593–603. doi: 10.1007/s00520-020-05521-x
40. Fish ML, Grover R, Schwarz GS. Quality-of-life outcomes in surgical vs nonsurgical treatment of breast cancer–related lymphedema. JAMA Surge. (2020) 155:513. doi: 10.1001/jamasurg.2020.0230
41. Rafn BS, Bodilsen A, von Heymann A, Lindberg MJ, Byllov S, Andreasen TG, et al. Examining the efficacy of treatments for arm lymphedema in breast cancer survivors: an overview of systematic reviews with meta-analyses. eClinicalMedicine. (2024) 67:102397. doi: 10.1016/j.eclinm.2023.102397
42. Greenlee H, DuPont-Reyes MJ, Balneaves LG, Carlson LE, Cohen MR, Deng G, et al. Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA: A Cancer J Clin. (2017) 67:194–232. doi: 10.3322/caac.21397
43. Anuszkiewicz K, Jankau J, Kur M. What do we know about treating breast-cancer-related lymphedema? Review of the current knowledge about therapeutic options. Breast Cancer. (2022) 30:187–99. doi: 10.1007/s12282-022-01428-z
44. Anik AR, Hasan K, Islam MM, Hasan MM, Ali MF, Das SK. Non-invasive portable technologies for monitoring breast cancer related lymphedema to facilitate telehealth: A scoping review. IEEE J Biomed Health Inform. (2023) 27:4524–35. doi: 10.1109/JBHI.2023.3280196
45. Erickson VS, Pearson ML, Ganz PA, Adams J, Kahn KL. Arm edema in breast cancer patients. JNCI J Natl Cancer Instit. (2001) 93:96–111. doi: 10.1093/jnci/93.2.96
46. Becker C, Assouad J, Riquet M, Hidden Gv. Postmastectomy lymphedema. Ann Surge. (2006) 243:313–5. doi: 10.1097/01.sla.0000201258.10304.16
47. Shih Y-CT, Xu Y, Cormier JN, Giordano S, Ridner SH, Buchholz TA, et al. Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: A 2-year follow-up study. J Clin Oncol. (2009) 27:2007–14. doi: 10.1200/JCO.2008.18.3517
48. Ahmed RL, Prizment A, Lazovich D, Schmitz KH, Folsom AR. Lymphedema and quality of life in breast cancer survivors: the iowa women’s health study. J Clin Oncol. (2008) 26:5689–96. doi: 10.1200/JCO.2008.16.4731
49. Hayes SC, Johansson K, Stout NL, Prosnitz R, Armer JM, Gabram S, et al. Upper-body morbidity after breast cancer. Cancer. (2012) 118:2237–49. doi: 10.1002/cncr.v118.8s
Keywords: bibliometric analysis, breast cancer-related lymphedema, arm lymphedema, self-management, rehabilitation, quality of life, prevention
Citation: Chen L, Zheng Y, Zheng D, Li Z, Chen H, Chen C and Yu S (2025) Research trends on lymphedema after mastectomy for breast cancer patients from 2000 to 2023: a scientometric analysis. Front. Oncol. 15:1440966. doi: 10.3389/fonc.2025.1440966
Received: 30 May 2024; Accepted: 16 January 2025;
Published: 04 February 2025.
Edited by:
Walid Kamal, University of Sharjah, United Arab EmiratesReviewed by:
Xiao Long, Peking Union Medical College Hospital (CAMS), ChinaGopal Nambi, Prince Sattam bin Abdulaziz University, Saudi Arabia
Ahmed Abdelmoniem Ibrahim, University of Hail, Saudi Arabia
Copyright © 2025 Chen, Zheng, Zheng, Li, Chen, Chen and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuxian Yu, c3Rfc3h5dUAxNjMuY29t; Chujun Chen, Y2hlbmNodWp1bjIyOUBxcS5jb20=
†These authors have contributed equally to this work and shared first authorship
 Ling Chen1†
Ling Chen1† Yuxian Zheng
Yuxian Zheng Zhiyang Li
Zhiyang Li Shuxian Yu
Shuxian Yu