- 1Center for Complementary Medicine, Department of Medicine II, Medical Center—University of Freiburg, Faculty of Medicine, University of Freiburg, Freiburg, Germany
- 2Institute for Applied Epistemology and Medical Methodology, University of Witten/Herdecke, Freiburg, Germany
- 3Research Group Integrative Medicine, Department of General and Visceral Surgery, University Hospital Ulm, Ulm, Germany
- 4Integrated Curriculum for Anthroposophic Medicine, Faculty of Health, Witten/Herdecke University, Witten, Germany
- 5Department of General, Visceral and Transplant Surgery, University Medical Center of the Johannes Gutenberg University, Mainz, Germany
- 6Department of General and Visceral Surgery, Center of Surgery, Medical Center - University of Freiburg, Freiburg, Germany
- 7Department of Internal Medicine, Section Nursing Science, Erasmus University Medical Center, Rotterdam, Netherlands
Purpose: The purpose of this study was to investigate the effect of rhythmic embrocation (RE), a massage technique, on postoperative stress levels (measured by heart rate variability) in colorectal cancer surgery patients compared to empathic conversation.
Methods: The study included 68 patients who were randomized into three groups: one received RE from professionals, another from students, and the third received empathic conversations. Stress was quantified using heart rate variability before and after the interventions.
Results: The standard deviation of the heartbeat intervals (SDNN) increased more in the professional RE group 9.12 ms (IQR 3.59-12.3 ms) than in the other groups: student RE group 5.68 ms (-0.66-7.5 ms), empathic conversation group 6.64 ms (-1.49-7.38 ms); hence stress decreased more in the professional RE group, although not statistically significant (p= 0.21). Other factors like sleep quality, nausea, pain, and mood did not differ significantly between the groups. No complications were associated with the interventions.
Conclusion: RE was safe and a statistically significant superiority of RE on postoperative stress compared to empathic conversations could not be found. Due to high inter- and intraindividual variability a clear pattern of response of the secondary outcomes to RE in comparison to empathic conversations could not be found. The study was limited by a small sample size, high patient variability, effective co-interventions for sleep, pain and nausea, and by an imbalance between groups. The study indicates that future research on RE should focus on a more narrowly defined patient population, increase the sample size, and select comparison groups that are clearly distinct from each other as well as a clinical context with fewer confounding factors. Furthermore, the patient’s preferences and previous experiences with massage therapy should be considered.
Clinical trial registration: German Clinical Trials Register (www.drks.de), identifier DRKS00023407.
1 Introduction
Colorectal cancer is the fourth most commonly diagnosed cancer, after breast, lung and prostate cancer. About 80% of colorectal cancers are diagnosed at a localized stage, when surgery can be curative (1).
Stress responses to surgery can be assessed by questionnaires, by monitoring sympathetic nervous system activation, pituitary hormone secretion, insulin resistance, immunologic and hematologic changes, and heart rate variability (HRV) (2, 3). Standards for HRV measurement have been developed (4), and HRV is increasingly being used in stress research (3, 5–17). Stress can have a detrimental effect on surgical recovery, highlighting the importance of identifying methods to alleviate it (18).
The implementation of stress-reducing techniques could be beneficial. One such technique is rhythmical embrocation (RE), a manual massage therapy, which was developed in the early 20th century by the physicians Ita Wegman and Margarethe Hauschka (19). RE therapy involves the application of oils or emulsions that a nurse gently massages over the patient’s body in circular or linear strokes (19, 20). This type of massage may support relaxation, and was followed by reductions in heart rate, blood pressure, pain, and improvements in mood, particularly in patients with chronic pain (21, 22).
The primary objective of this study was to investigate the effect of RE-therapy compared to empathic conversation on stress levels in colorectal cancer patients after surgery, as quantified by parameters of HRV. Secondary objectives included investigating the influence of RE-therapy on sleep quality, nausea and vomiting, pain level, analgesics use, sleep medication, mood, degree of mobilization, and any adverse events related to the intervention.
2 Methods
2.1 Trial design
The study was conducted as a two-center, randomized, controlled, open-label, three-arm, parallel-group trial. Patients were randomized 1:1:1 to the three groups. The trial was originally designed as a single-center study. As recruitment slowed down during the COVID-19 pandemic, an additional center was added and randomization was performed using a block randomization method stratified by center.
2.2 Participants
Individuals diagnosed with colorectal cancer and scheduled for surgery were eligible for this study. Inclusion criteria: patients in an inpatient setting after colorectal cancer surgery; the ability to complete questionnaires or answer questions; age 18 years or older; legal competence; comprehension of the trial’s nature and related procedures, along with the capacity to comply with them; proficiency in the German language; provision of written informed consent, obtained in accordance with international guidelines and local laws. Individuals were excluded from the study if they exhibited any of the following conditions: severe surgical complications; severe cardiac complications; sepsis; cardiac conditions that might interfere with HRV analysis, such as severe arrhythmias or the presence of a pacemaker; severe psychiatric disorders; pregnancy or breastfeeding; clinically significant comorbidities that could critically affect the patient’s adherence to the protocol; hypersensitivity to skincare products; skin disorders in the back or feet area; isolated nursing; participation in a clinical trial within the three months preceding the start of this study, or simultaneous participation in studies interfering with the current study.
2.3 Settings and locations
The study was conducted in the surgical departments of the University Medical Center Freiburg and the Evangelisches Diakoniekrankenhaus Freiburg, both located in southwestern Germany.
2.4 Interventions
RE-therapy was administered in two of the 3 study groups – in one group by RE-professionals, in the other group by nursing students. The third group of patients received empathic conversations with a nursing student. The nursing students who administered RE had received training in three teaching units of 3.5 hours each from two certified professionals (23). RE was applied as recommended (24) and with standardized procedure with the team (for a detailed description see the Description of the intervention in the Supplementary Material).
The interventions were started on the evening of the day the patient was discharged from the intensive care unit (ICU) following surgery. Consequently, the interval between surgery and the commencement of the intervention varied in days according to the duration of the patient’s stay on the ICU.
The participants received RE on the back (while sitting on the edge of the bed or lying on their side) and the feet (while lying on their back) with 2 mL of high-quality pharmacopoeial almond oil (25) for approximately 10 minutes, scheduled between 8 and 10 am and again between 6 and 10 pm. The intensity of the back massage ranged from 1 to 3 on a scale where 1 represented ‘gentlest massage possible’, and 10 = ‘very intense massage`, while the feet massage ranged from 1 to 5. RE of the back and feet were selected in discussion with several RE experts regarding the setting and condition of the patients and the goal of reducing stress in this setting.
The control intervention involved a 10-minute empathic conversation conducted during the same time periods. A list of suggested questions and topics was provided to the health professional students conducting the interviews. Following the intervention, all patients were instructed to rest for a period of 20 minutes. The staff and patients in the same room were informed about the intervention and resting period and were kindly requested not to interrupt during these periods. A sign was posted on the door indicating ‘study intervention in progress, please do not disturb until x:xx’.
We designed the study with the three groups described above to discriminate an effect between RE and empathic attention and to further evaluate whether a difference in outcomes can be seen between experts performing RE and students performing RE after only a short training in RE.
2.5 Outcomes
The primary outcome, ‘level of stress’, was assessed by analyzing HRV recorded overnight (starting between 6 and 10 pm and stopping between 8 and 10 am) on days 1 and 5 (days are counted from arrival at normal ward after surgery and intensive care unit) using a one-channel electrocardiogram (ECG) device, the Bittium Faros 180 (26). The devices were installed on the patient by the study personnel (students, RE experts). The data were analyzed in accordance with the 1996 guideline of the Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (4). The primary metric utilized was the standard deviation of the N-N intervals (SDNN), expressed in milliseconds (ms), which serves to quantify the variability of heartbeats and indicates vagal activity. A higher SDNN indicates greater vagal activity and a lower stress level in the organism.
The secondary outcomes were evaluated as follows:
Sleep quality was evaluated using the Richards-Campbell Sleep Questionnaire (RCSQ) (27) on days 2, 3 and 6 after arrival on the normal ward after surgery and intensive care unit admission. The questionnaire generates a total score, ranging from 0 (indicating the worst possible sleep) to 100 (indicating the best sleep).
The severity of nausea experienced within the previous 24 hours was quantified on days 1, 3, and 6 using a 10-cm visual analogue scale (VAS), with endpoints ranging from “no nausea” to “worst imaginable nausea” (28, 29).
The intensity of pain experienced over the previous 24 hours was quantified on days 1, 3, and 6 using a 10-cm visual analogue scale (VAS), with endpoints ranging from “no pain” to “strongest imaginable pain.”
Information regarding the consumption of analgesics, sedatives, and emetics was obtained from the patient’s medical chart. Analgesics were classified according to the World Health Organization (WHO) analgesic ladder, with group 1 comprising non-opioid analgesics, group 2 low-potent opioids, group 3 high-potent opioids, and group 4 invasive pain management (pain catheter) (30).
Mood was assessed on days 1, 3, and 6 using the Mehrdimensionaler Befindlichkeitsfragebogen (MDBF), a validated questionnaire that measures well-being in terms of pleasantness, wakefulness, and calmness (31). The results are presented on a scale from 24, which represents the lowest mood, to 120, which represents the highest mood.
The activity level of the subjects was evaluated at baseline and on day 6 using the Evaluationsbogen Mobilität (EboMo), a simple scoring tool for assessing activity level, especially in settings such as nursing homes. The responses were recorded on a scale from 14, indicating severely limited mobility, to 56, representing unrestricted mobility (32). Patients were queried about complications associated with the intervention at each encounter with the study team.
2.6 Change to trial outcomes
The initial definition of the primary outcome was the final HRV measurement. However, a significant proportion of ECG recordings could not be analyzed with respect to HRV parameters due to the presence of numerous artefacts in the ECG. Furthermore, due to the higher variability observed in HRV measurements as expected within the patient sample, we deemed it more meaningful to consider the change between these two measurements. This provides insight into the change in stress during the trial period. In the following section, we provide both outcomes.
2.7 Sample size
The sample size calculation was based on the data of a previous trial investigating perioperative stress with HRV parameters as outcome measure. In that trial, significant changes in the standard deviation of the distribution of normal-to-normal intervals (SDNN) had been recorded at different perioperative time points (5). The preoperative SDNN was 116 milliseconds (ms); on the first postoperative day it was 65 ms, and on postoperative day seven it was 87 ms [approximate values as the actual values are not given in the article text, but only displayed as a bar chart; the bar chart was converted into numbers using WebPlotDigitizer (33)]. Based on these figures, we assumed the median SDNN in the conversation group to be 80 ms on postoperative day 5. In the intervention groups, we assumed a faster recovery of the SDNN; i.e., 110 ms on day 5 (therefore we set SD = 30 ms). In the previous trial, the standard deviation was around 30 (SD = 30 ms) for all measurements. Based on a t-distribution, a two-tailed α=0.05 and a power of 0.8, we calculated a sample size of 17 patients per group, and thus 51 in total. Assuming a dropout rate of 20%, we therefore planned to include at least 60 patients.
2.8 Interim analyses
No interim analysis was performed and there was no early termination of the study.
2.9 Randomization and sequence generation
The allocation sequence was generated by an independent researcher using the website Randomization.com (34).
No stratification was used; we used block randomization by center.
2.10 Allocation and implementation
The participants were enrolled by a physician during the preoperative visit. Upon the patient’s arrival at the normal ward after surgery, the inclusion and exclusion criteria were re-evaluated. Upon the inclusion of a new patient, the investigator and the trial assistant were duly informed. Subsequently, the investigator or the trial assistant transmitted the sequential number of the new patient to the independent researcher via electronic means. Upon receipt of this information, the independent researcher transmitted the intervention code from the allocation list in response.
2.11 Blinding
It was not feasible to conduct a blind study of study staff who were directly involved in the intervention. Study staff providing RE were instructed not to disclose to the patients whether they were being treated by RE experts or students. The patients receiving RE were informed that they would not receive information regarding the identity of their treating RE professionals. The data collection and analysis were conducted in a manner that ensured blinding to the treatment group assignments.
2.12 Data management
HRV data were extracted and analyzed using Matlab (35). Data documented by patients themselves – with possible assistance of the study staff and data obtained by study staff in interviews was collected on paper and managed using REDCap (Research Electronic Data Capture) tools hosted at the University Medical Center Freiburg (36). REDCap is a secure, web-based application designed to support data capture for research studies. The application provides: 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources. The data was entered into REDCap 10.0.28 into fields with prespecified data ranges and plausibility checks. The datasets from Matlab and REDCap were then merged by patient ID in R version 4.2.0 (37).
2.13 Statistical methods
Data analysis was performed using R version 4.2.0 (37) an intention-to-treat approach using the full analysis set. A p-value < 0.05 was considered statistically significant. For the primary outcome ‘level of stress’, the SDNN was calculated from HRV during sleep based on recordings from day 1 and day 5, and the difference between these two measurements was calculated. The testing sequence was as follows: the mean of the empathic conversation group was compared with the mean of the expert RE group using the T-test; if the null hypothesis (no difference between the groups) could be rejected, the empathic conversation group was compared to the student RE group; if the null hypothesis could also be rejected in this comparison, the expert RE group was compared with the student RE group. If the data did not fulfil the criteria for parametric testing, non-parametric tests were used. The same procedures were applied to the secondary outcomes. The per-protocol group was defined in the study protocol as having no missing data in the primary outcome (HRV of day 1 and day 5) and having participated in more than 5 of 8 treatment sessions.
3 Results
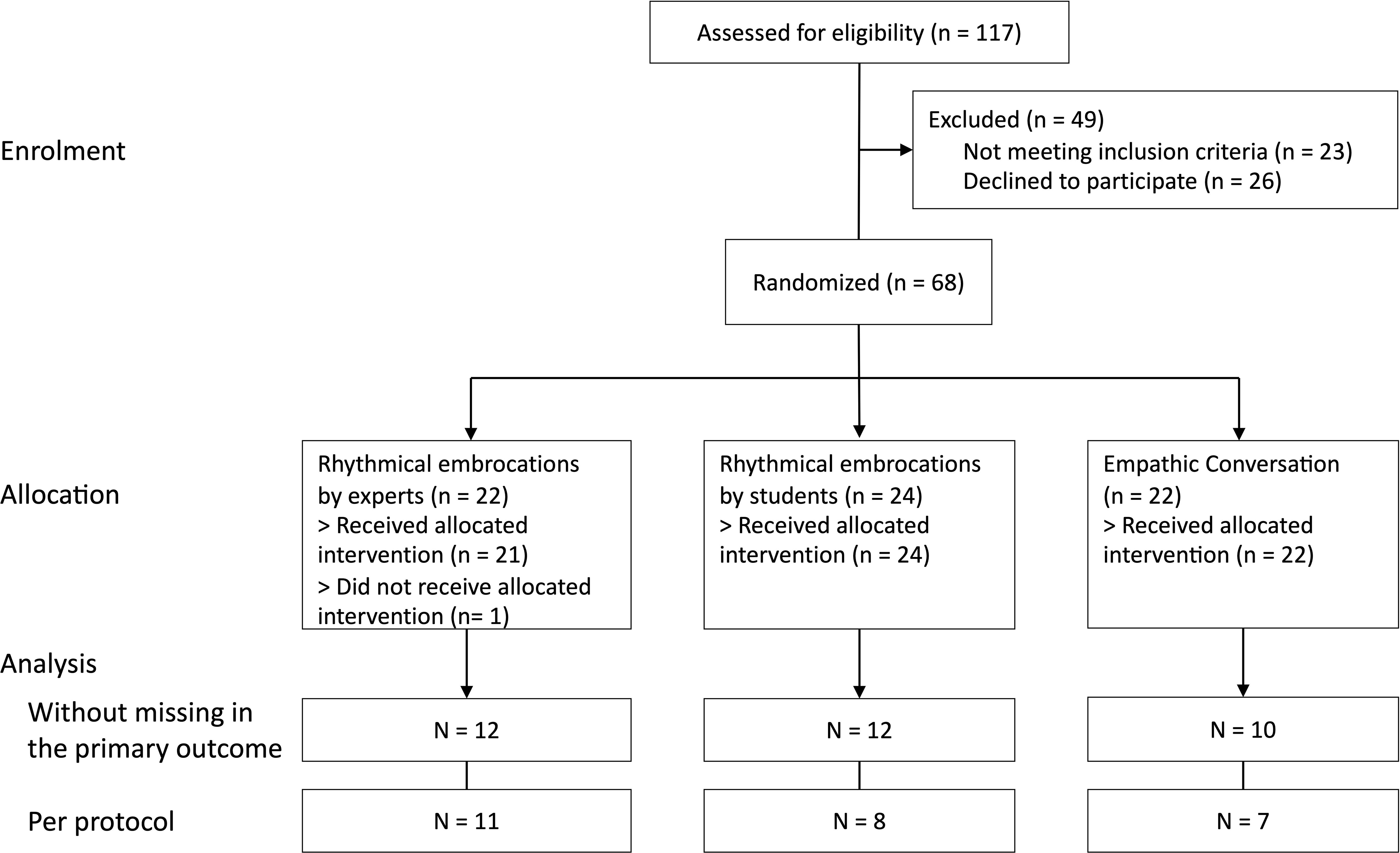
From January 2021 until January 2022, 68 patients were recruited and randomly assigned to one of the three study groups: 22 to the expert RE group; 24 to the student RE group and 22 patients to the empathic conversation group (Figure 1). The patients in the expert RE group received a median (range) of 6 (0-8) interventions, while those in the student RE group received 7 (2-8) interventions, and those in the empathic conversation group 7 (2-8) interventions. There were 5 drop-outs; 3 in the expert RE group and 1 in each of the other groups; reasons for dropping out in the expert RE group were complications of the surgical procedures (1 patient) and unspecified (2 patients); reasons for dropping out in the other groups were patients’ wishes (1 patient in each group). There were no intervention-specific drop-outs.
3.1 Baseline data
The demographic characteristics of the patients in each group are presented in Table 1. The mean age of the entire sample was 68 years (range 31-83 years), with an equal distribution of age across all three groups. The proportion of women in the entire sample was 39.7% (n=27). A significant difference in tumor localization was observed between the three groups (Kruskal Wallis: p = 0.02) especially between the student RE group and the empathic conversation group (Dunn’s-Test: p = 0.0076; see Table 1).
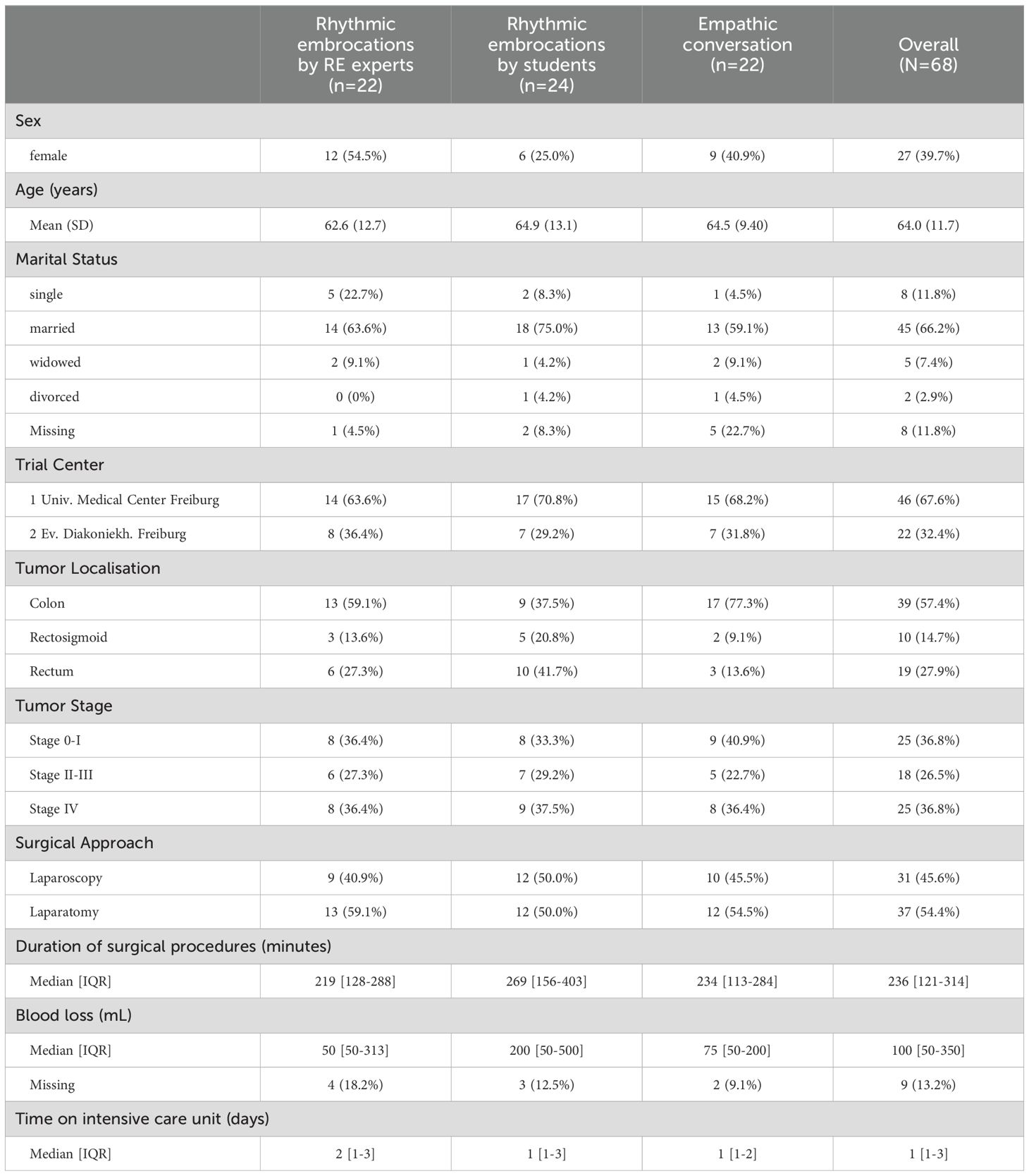
Table 1. Demographics of the patients, oncological and surgical characteristics per randomization group.
3.2 Outcomes
3.2.1 Primary outcome
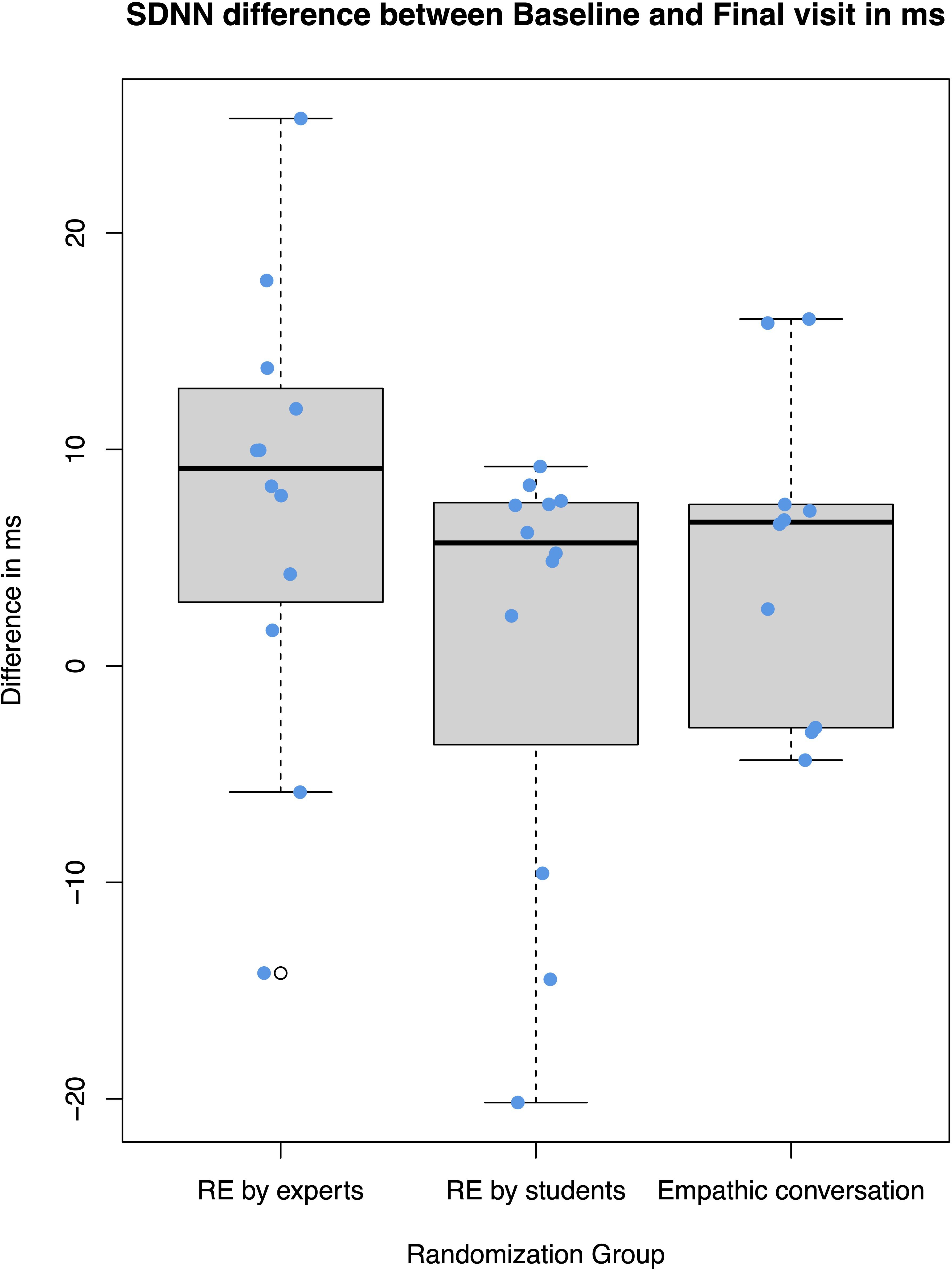
The primary endpoint, stress, was assessed by monitoring heart rate variability overnight from day 1 to day 2 and day 5 to day 6. The analysis was performed on an intention-to-treat basis using the full analysis set. However, many electrocardiogram recordings were affected by artifacts, resulting in data availability for 34 (50%) patients; comprising 12 from the expert RE group, 12 from the student RE group, and 10 from the empathic conversation group. Reasons for the artefacts were high skin resistance at the location of the electrodes in several patients and excessive movement in some patients. The mean SDNN of the final measurement was 46.4 ms (SD 20.0 ms) in the RE expert group, 36.6 (19.8) in the student RE group, and 42.1 (13.7) in the empathic conversation group. The Kruskal-Wallis-Test showed no statistically significant differences between the groups. The median change SDNN between the two measurements was an increase of 9.12 ms (IQR 3.59-12.3 ms) in the expert RE group, 5.68 ms (-0.66-7.5 ms) in the student RE group, 6.64 ms (-1.49-7.38 ms) in the empathic conversation group (see Figure 2); without statistical significant difference between the groups (Kruskal-Wallis: p= 0.21). For missing data of the HRV variables, we performed multiple imputation by chained equations in R; however, there were still no statistically significant effects between groups (for details, see the Supplementary Material).
3.2.2 Per protocol analysis
Data of 26 patients were included in the per protocol analysis: 11 patients from the expert RE group, 8 from the student RE group, and 7 from the empathic conversation group. The median and IQR of the SDNN increase between the two measurements was 8.30 ms (2.94-10.9 ms) in the expert RE group, 5.68 ms (-0.664-7.5 ms) in the student RE group and 6.55 ms (-0.116-7.1 ms) in the empathic conversation group (Kruskal-Wallis: p=0.34).
3.2.3 Secondary outcomes
Sleep quality was assessed using the Richards-Campbell-Sleep-Questionnaire (RCSQ). Across all groups, a decrease of sleep quality from night 1 to night 2 was observed (see Figure 3). The median difference of the RCSQ between the 2nd and the 5th night was 7.1 (IQR -9.40-28.3) in the RE expert group, 12.0 (-7.6-28.8) in the RE student group and 3.5 (-22.5-15.1) in the empathic conversation group; (Kruskal-Wallis: p=0.65).
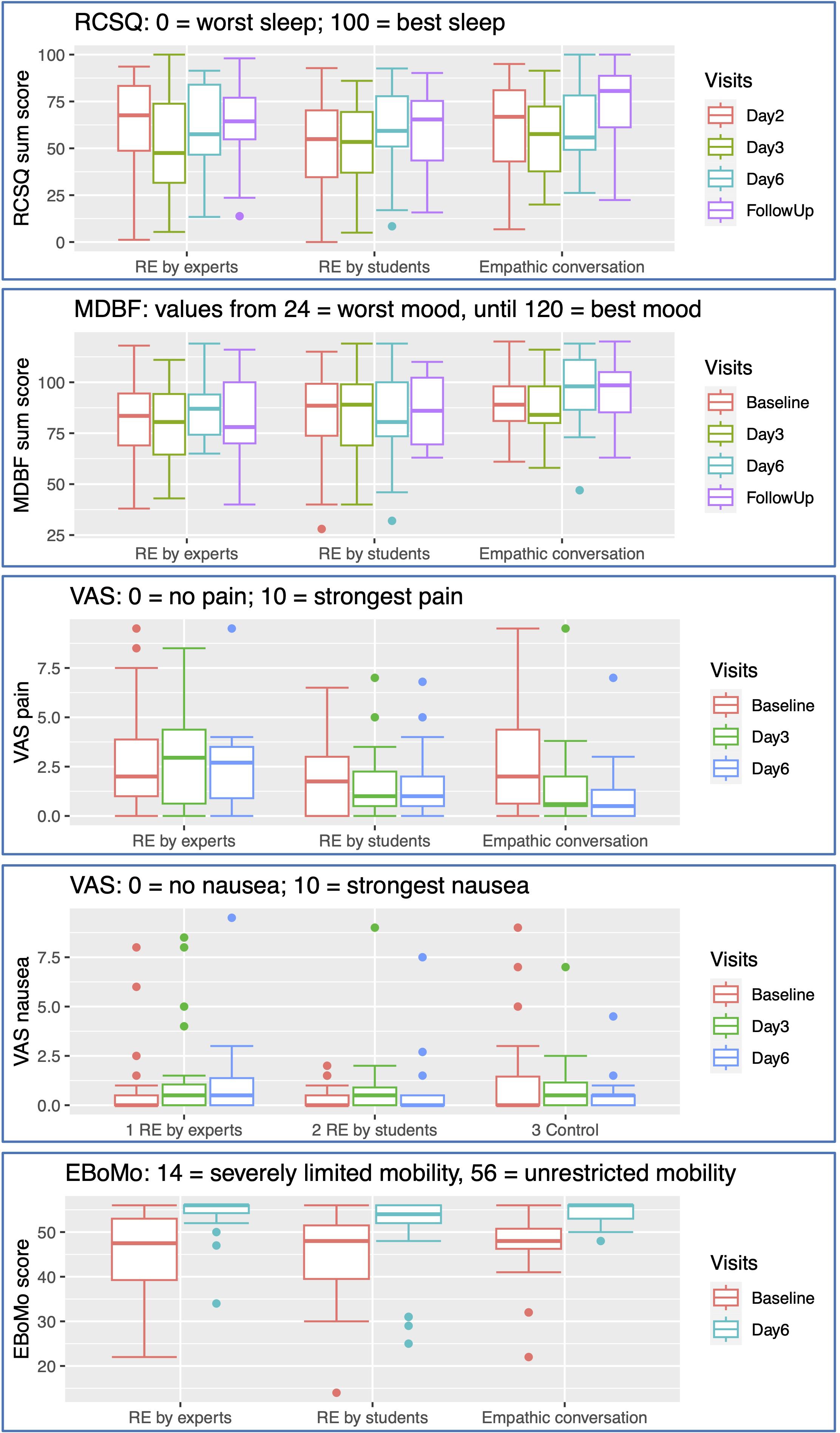
Figure 3. Secondary Outcomes: RCSQ, Richard-Campbells-Sleep-Questionnaire; MDBF, Mehrdimensionaler Befindlichkeitsfragebogen (multidimensional mood questionnaire); VAS, visual analogue scale; EBoMo, Evlauationsbogen Mobilität (evaluation sheet mobility).
MDBF at Baseline, day 3, day 6 and follow up after 30 days. The median improvement of mood from day 1 to day 6 was 3.5 (IQR -9.0-21.8) in the RE expert group, 4.5 (-7.5-8.0) in the RE student group: and 11.5 (0.5-17.8) in the empathic conversation group; (Kruskal-Wallis: p=0.31).
Pain intensity was generally rated low; median difference in pain scores between day 1 and day 6 were 0 in the RE expert group (IQR -2-1), -0.25 in the RE student group (-1.75-1.50) and -0.75 in the empathic conversation group (-4-0); (Kruskal-Wallis: p= 0.28).
Nausea was generally rated low; the median difference in nausea scores between day 1 and day 6 was 0.0 (IQR -0.5-0.5) in the RE expert group, 0.15 (0-0.925) in the RE student group and 0.0 (-0.500-0.125); (Kruskal-Wallis: p= 0.15).
Mobility was generally rated high; the median difference in mobility scores between day 1 and day 6 was 6.5 (IQR 3-16.3) in the RE expert group, 6. 0 (3.75-10.3) in the RE student group and 8.0 (2.75-9.25) in the empathic conversation group; (Kruskal-Wallis: p= 0.79).
The measurements of the secondary outcomes at the different visits are detailed in Figure 3.
Regarding pain medication, need of opioids at the final visit was not equally distributed between the groups. However; the high proportion of missing data renders this result inconclusive (for details see the figure on pain medication in the Supplementary Material). The overall use of sedatives was low in all groups (see Supplementary Material).
3.3 Complications
The study team assessed potential complications associated with the intervention at each patient encounter. No complications associated with the intervention were documented during the entire study period.
4 Discussion
The results of this study indicate that RE was safe and a significant superiority of RE over empathic conversations regarding the primary objective could not be found when compared with empathic conversation. Regarding the primary objective, a relevant part of the data were missing, due to technical issues of the HRV recording. Furthermore, the variability of the HRV results was higher than expected. In addition, groups were imbalanced regarding gender and tumor type, patients received effective treatments for pain, sleep, and nausea, which may have influenced the outcomes.
With regard to the HRV data, the technical difficulties encountered in the measurement of HRV resulted in the inability to analyze 50% of the data. Nevertheless, the extent of data loss was relatively evenly distributed across the groups. HRV can be calculated from short time periods of several minutes to record changes after an intervention, as Seifert et al. demonstrated in their trial on rhythmical massage in healthy young women (38). In our trial, we decided to calculate HRV from complete long-term measurements overnight to assess overall stress level rather than sudden changes. However, these long-term measurements are more susceptible to other stress triggers, which can vary in the clinical setting and throughout the course of a cancer disease. We did not ask about stress in another questionnaire, as we wanted to collect physiological parameters on this issue that would not be influenced by biases in the use of questionnaires.
Empathic conversation was chosen as a control intervention to differentiate between the mere effect of empathic caring time and the specific effect of RE. However, empathic conversations can have a strong effect on patients as well. Previous studies on empathic conversation have demonstrated changes in immunologic blood cells and a reduction in the duration of a common cold (39). Empirical evidence also exists demonstrating the impact of empathic conversation on stress, anxiety, and outcomes in chronic disease and cancer (40–45).
The Sars-CoV-2 pandemic introduced a number of significant alterations to the surrounding conditions of our trial. For instance, regular emphatic conversations were also conducted during the period of contact restrictions, where regular conversations with friends and family members were dramatically reduced. Consequently, the empathic conversations may have exerted a more profound influence than they would have done in the absence of the restrictions on regular visits.
The secondary endpoints were analyzed just for exploratory reasons. Also here, the sample displayed higher variability than expected and the groups were partially imbalanced. To investigate an effect, a larger sample size would be needed. For example, the tumor locations were distributed differently in the groups. Regarding the measurement of sleep quality, the first night at the normal ward unexpectedly was better than the following nights. However, this is a well-known phenomenon in sleep research, that a sleep dept can be developed in nights with disturbed sleep and a subsequent night with less disturbance – such as those at the normal ward after nights at the ICU – tend to be rated better than the following nights when no sleep debt is present (46). Rating of sleep in the second night at the normal ward was comparable to results from intensive care units and rating of the sleep at home in the follow up was comparable to sleeping at home from other populations (47). Mood was comparable to other studies of the perioperative mood change – although a definite trend within the postoperative period could not be seen in our trial (48). Patients’ pain, nausea and vomiting were closely monitored by the surgical ward and treated with medication. Therefore, it was difficult to discern any additional influence of the study interventions. We did not evaluate non-oncological comorbidities or factors that could potentially restrict the patients’ physical status. Given the small sample size, these unassessed factors may have further increased the heterogeneity of patient symptoms and outcomes.
The efficacy of massage interventions in the postoperative period has been the subject of various studies, which have yielded disparate results. Two studies with 58 and 113 patients conducted by the Mayo Clinic revealed that massage with additional resting time had a significantly positive impact on pain, anxiety, tension, and satisfaction in patients who had undergone cardiovascular surgery in comparison with resting time alone. This led to the incorporation of massage into the postoperative routine of the clinic (49). In contrast, a study conducted by the Cleveland Clinic found that postoperative massage had no effect on mood, pain, anxiety, or physiological measurements, with the exception of a reduction in postoperative blood pressure in patients undergoing cardiovascular surgery when compared to usual care alone (50). The discrepancy in these results can be attributed to a number of factors, such as individual tailoring of the massage treatment to the individual patient, type of massage and openness for touch and massage in general. Although participation in our trial was entirely voluntary, we did not inquire as to whether the patients would like to be massaged, whether they had previously had positive or negative experiences with massage, or whether they had any concerns about being touched by another person. To avoid amplifying expectation effects, we refrained from asking the participants whether they found the intervention pleasant. However, recent research on therapeutic touch indicates that the patient’s attitude toward the type of touch can be a determining factor in whether the therapy is perceived as calming or stressful (51, 52).
5 Conclusion
For future studies in RE, it is recommended that more robust and less error-prone measurement methods be employed. At the outset of the intervention, the post-operative stress had presumably already partially subsided, resulting in an effect size that was smaller than anticipated. The heterogeneity was considerable, and the number of test subjects should have been larger. Some symptoms were alleviated with medication, leaving little room for additional relief. Future studies should investigate areas that are insufficiently relieved by medication or at the time of greatest intensity. Previous experience with massage should be sought and included in the evaluation.
Data availability statement
The datasets presented in this article are not readily available because Data sharing was not included in the ethical review of the trial. Requests to access the datasets should be directed to Paul Werthmann, cGF1bC53ZXJ0aG1hbm5AdW5pa2xpbmlrLWZyZWlidXJnLmRl.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the University Medical Center Freiburg under the number 356/20 on 20th October 2020. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. The study was accredited by the study box of the German Cancer Society on 23.11.2020 under the identifier ST-D481.
Author contributions
PW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. DC: Conceptualization, Data curation, Software, Writing – original draft, Writing – review & editing. MJ: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. AL: Investigation, Writing – original draft, Writing – review & editing. GN: Investigation, Writing – original draft, Writing – review & editing. RH: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. Mv: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. GK: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The trial was funded by the Dr. Hauschka Stiftung, Bad Boll/Eckwälden, Germany, the Christophorus Stiftung, Stuttgart Germany and the Software AG - Stiftung, Darmstadt, Germany. The funding had no influence on the design, conduct, analysis interpretation and publication of the study. We acknowledge support by the Open Access Publication Fund of the University of Freiburg.
Acknowledgments
The trial is a research project of PGW in the master’s program Clinical Epidemiology at Erasmus University Rotterdam, the Netherlands and is supervised by MD (Erasmus University Medical Center, Rotterdam, the Netherlands). We thank Harald Hamre and Helmut Kiene (IFAEMM, Freiburg) for advice on analysis and revision of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2025.1439420/full#supplementary-material
Abbreviations
EBoMo, Evaulationsbogen Mobilität (mobility evaluation sheet); ECG, electrocardiogram; HRV, heart rate variability; MDBF, Mehrdimensionaler Befindlichkeitsfragebogen (Multidimensional well-being questionnaire); RCSQ, Richards-Campbell sleep questionnaire; RE, Rhythmical Embrocations according to Wegman/Hauschka; SDNN, standard deviation of the NN intervals; VAS, visual analogue scale.
References
1. Cancer of the colon and rectum - cancer stat facts. SEER. Available online at: https://seer.cancer.gov/statfacts/html/colorect.html (Accessed December 17, 2019).
2. Desborough JP. The stress response to trauma and surgery. Br J Anaesth. (2000) 85:109–17. doi: 10.1093/bja/85.1.109
4. Malik M, Bigger JT, Camm AJ, Kleiger RE, Malliani A, Moss AJ, et al. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Eur Heart J. (1996) 17:354–81. doi: 10.1093/oxfordjournals.eurheartj.a014868
5. Ushiyama T, Nakatsu T, Yamane S, Tokutake H, Wakabayashi H, Ishimura K, et al. Heart rate variability for evaluating surgical stress and development of postoperative complications. Clin Exp Hypertens. (2008) 30:45–55. doi: 10.1080/10641960701813908
6. Amalan S, Vaishali B SPP, Joseph J, Sivaprakasam M. Pre-surgery stress monitoring using heart rate variability measures. In: 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). IEEE, Berlin, Germany (2019). p. 4592–5. doi: 10.1109/EMBC.2019.8856409
7. Borghi-Silva A, Reis M, Mendes R, Melo R, Pantoni C, Quitério R, et al. Heart rate variability in the elderly with chronic obstructive pulmonary disease submitted to acute application of bi-level positive airway pressure. Crit Care. (2005) 9:P87. doi: 10.1186/cc3631
8. Jarczok MN, Koenig J, Wittling A, Fischer JE, Thayer JF. First evaluation of an index of low vagally-mediated heart rate variability as a marker of health risks in human adults: proof of concept. J Clin Med. (2019) 8:1940. doi: 10.3390/jcm8111940
9. Yeh GY, Mietus JE, Peng C-K, Phillips RS, Davis RB, Wayne PM, et al. Enhancement of sleep stability with Tai Chi exercise in chronic heart failure: preliminary findings using an ECG-based spectrogram method. Sleep Med. (2008) 9:527–36. doi: 10.1016/j.sleep.2007.06.003
10. Powezka K, Adjei T, von Rosenberg W, Normahani P, Goverdovsky V, Standfield NJ, et al. A pilot study of preoperative heart rate variability predicting pain during local anesthetic varicose vein surgery. J Vasc Surg: Venous Lymphatic Disord. (2019) 7:382–6. doi: 10.1016/j.jvsv.2018.08.008
11. Tan C, Saito N, Miyawaki I. Changes in heart rate and autonomic nervous activity after orthopedic surgery in elderly Japanese patients. Kobe J Med Sci. (2017) 62:E129–35.
12. Miliauskas P, Zemaityte D, Varoneckas G, Zurauskas A, Tikuisis R. Diagnostic value of heart rate variability in general anesthesia. Medicina (Kaunas). (2002) 38 Suppl 2:97–100.
13. Ledowski T, Stein J, Albus S, MacDonald B. The influence of age and sex on the relationship between heart rate variability, haemodynamic variables and subjective measures of acute post-operative pain. Eur J Anaesthesiol. (2011) 28:433–7. doi: 10.1097/EJA.0b013e328343d524
14. Ushiyama T, Mizushige K, Wakabayashi H, Nakatsu T, Ishimura K, Tsuboi Y, et al. Analysis of heart rate variability as an index of noncardiac surgical stress. Heart Vessels. (2008) 23:53–9. doi: 10.1007/s00380-007-0997-6
15. Scheffler P, Muccio S, Egiziano G, Doonan RJ, Yu A, Carli F, et al. Heart rate variability exhibits complication-dependent changes postsurgery. Angiology. (2013) 64:597–603. doi: 10.1177/0003319712461932
16. Yung MC, Chang Y, Lai ST, Tsou MY, Chan KH. Improved postoperative pain relief via preemptive analgesia in relation to heart rate variability for coronary artery bypass grafting: a preliminary report. Zhonghua Yi Xue Za Zhi (Taipei). (1997) 60:28–35.
17. Spellenberg C, Heusser P, Büssing A, Savelsbergh A, Cysarz D. Binary symbolic dynamics analysis to detect stress-associated changes of nonstationary heart rate variability. Sci Rep. (2020) 10:15440. doi: 10.1038/s41598-020-72034-2
18. Helander EM, Webb MP, Menard B, Prabhakar A, Helmstetter J, Cornett EM, et al. Metabolic and the surgical stress response considerations to improve postoperative recovery. Curr Pain Headache Rep. (2019) 23:1–8. doi: 10.1007/s11916-019-0770-4
19. Layer M. Sich auf der Erde Zuhause fühlen. In: Bertram M, Kolbe HJ, editors. Dimensionen therapeutischer Prozesse in der Integrativen Medizin. Springer Fachmedien Wiesbaden, Wiesbaden (2016). p. 155–68. doi: 10.1007/978-3-658-12149-5_10
20. Heine R, Adams K. Anthroposophische Pflegepraxis: Grundlagen und Anregungen für alltägliches Handeln. Berlin: Salumed-Verlag (2017).
21. Ostermann T, Blaser G, Bertram M, Michalsen A, Matthiessen PF, Kraft K. Effects of rhythmic embrocation therapy with solum oil in chronic pain patients: A prospective observational study. Clin J Pain. (2008) 24:237–43. doi: 10.1097/AJP.0b013e3181602143
22. Bertram M. Rhythmische einreibungen nach wegman/hauschka. In: Bertram M, Kolbe HJ, editors. Dimensionen therapeutischer Prozesse in der Integrativen Medizin. Springer Fachmedien Wiesbaden, Wiesbaden (2016). p. 107–22. doi: 10.1007/978-3-658-12149-5_7
23. International Forum for Anthroposophic Nursing ed. In: Handbook for the Certification of Specialists in Rhythmical Einreibungen according to Wegman/Hauschka (IFAN), 4th ed. Dornach/Switzerland. (2019). Available at: https://anthronursing.care/wp-content/uploads/2024/11/IFAN_Handbuch_ANS_5-DE.pdf (Accessed January 21, 2025).
24. Batschko E-M. Einführung in die rhythmischen Einreibungen: nach Wegman/Hauschka. Stuttgart: Mayer (2011).
25. Deutscher Apotheker-Verlag Doktor Roland Schmiedel. European Pharmacopoeia, 10th edition. (2019).
26. Bittium. Available online at: https://www.bittium.com/medical/bittium-faros (Accessed December 17, 2019).
27. Krotsetis S, Richards KC, Behncke A, Köpke S. The reliability of the German version of the Richards Campbell Sleep Questionnaire. Nurs Crit Care. (2017) 22:247–52. doi: 10.1111/nicc.12275
28. Kim SI, Kim SC, Baek YH, Ok SY, Kim SH. Comparison of ramosetron with ondansetron for prevention of postoperative nausea and vomiting in patients undergoing gynaecological surgery. Br J Anaesth. (2009) 103:549–53. doi: 10.1093/bja/aep209
29. Anderson LA, Gross JB. Aromatherapy with peppermint, isopropyl alcohol, or placebo is equally effective in relieving postoperative nausea. J PeriAnesthesia Nurs. (2004) 19:29–35. doi: 10.1016/j.jopan.2003.11.001
30. Jadad AR, Browman GP. The WHO analgesic ladder for cancer pain management. Stepping up the quality of its evaluation. JAMA. (1995) 274:1870–3. doi: 10.1001/jama.1995.03530230056031
31. Steyer R, Schwenkmezger P, Notz P, Eid M. Testtheoretische Analysen des Mehrdimensionalen Befindlichkeitsfragebogen (MDBF). Diagnostica. (1997) 40:320–328. doi: 10.1037/t12446-000
32. Zegelin A. Zentrale pflegerische Aufgabe: Bewegungsfähigkeit erhalten. Pflegezeitschrift. (2017) 70:9–11. doi: 10.1007/s41906-017-0122-0
33. Drevon D, Fursa SR, Malcolm AL. Intercoder reliability and validity of WebPlotDigitizer in extracting graphed data. Behav Modif. (2017) 41:323–39. doi: 10.1177/0145445516673998
34. Dallal GE. (2021). Available online at: www.randomization.com (Accessed October 2, 2021).
35. MathWorks - makers of MATLAB and Simulink. Available online at: https://www.mathworks.com/ (Accessed February 23, 2021).
36. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J BioMed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
37. R Development Core Team. A language and environment for statistical computing: reference index (2010). Vienna: R Foundation for Statistical Computing. Available online at: http://www.R-project.org/ (Accessed February 23, 2021).
38. Seifert G, Kanitz J-L, Rihs C, Krause I, Witt K, Voss A. Rhythmical massage improves autonomic nervous system function: a single-blind randomised controlled trial. J Integr Med. (2018) 16:172–7. doi: 10.1016/j.joim.2018.03.002
39. Rakel D, Barrett B, Zhang Z, Hoeft T, Chewning B, Marchand L, et al. Perception of empathy in the therapeutic encounter: Effects on the common cold. Patient Educ Couns. (2011) 85:390–7. doi: 10.1016/j.pec.2011.01.009
40. Arora NK. Interacting with cancer patients: the significance of physicians’ communication behavior. Soc Sci Med. (2003) 57:791–806. doi: 10.1016/S0277-9536(02)00449-5
41. Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ: Can Med Assoc J. (1995) 152:1423.
42. Epstein RM, Street RL Jr. Patient-centered communication in cancer care: promoting healing and reducing suffering. (2007). doi: 10.1037/e481972008-001 (Accessed January 21, 2025).
43. Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. (1989) 27:S110–27. doi: 10.1097/00005650-198903001-00010
44. Lelorain S, Brédart A, Dolbeault S, Sultan S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psycho-Oncology. (2012) 21:1255–64. doi: 10.1002/pon.v21.12
45. Van Dulmen AM, Bensing JM. Health promoting effects of the physician-patient encounter. Psychol Health Med. (2002) 7:289–300. doi: 10.1080/13548500220139421
46. Perlis ML, Posner D, Riemann D, Bastien CH, Teel J, Thase M. Insomnia. Lancet. (2022) 400:1047–60. doi: 10.1016/S0140-6736(22)00879-0
47. Ritmala-Castren M, Axelin A, Richards KC, Mitchell ML, Vahlberg T, Leino-Kilpi H. Investigating the construct and concurrent validity of the Richards-Campbell Sleep Questionnaire with intensive care unit patients and home sleepers. Aust Crit Care. (2022) 35:130–5. doi: 10.1016/j.aucc.2021.04.001
48. Lederer A-K, Manteufel I, Knott A, Kousoulas L, Werthmann PG, Storz MA, et al. Surgery as an emotional strain: an observational study in patients undergoing elective colorectal surgery. J Clin Med. (2022) 11:2712. doi: 10.3390/jcm11102712
49. Wang AT, Sundt TM, Cutshall SM, Bauer BA. Massage therapy after cardiac surgery. Semin Thorac Cardiovasc Surg. (2010) 22:225–9. doi: 10.1053/j.semtcvs.2010.10.005
50. Albert NM, Gillinov AM, Lytle BW, Feng J, Cwynar R, Blackstone EH. A randomized trial of massage therapy after heart surgery. Heart Lung. (2009) 38:480–90. doi: 10.1016/j.hrtlng.2009.03.001
51. Löken LS, Wessberg J, Morrison I, McGlone F, Olausson H. Coding of pleasant touch by unmyelinated afferents in humans. Nat Neurosci. (2009) 12:547–8. doi: 10.1038/nn.2312
Keywords: colorectal cancer, rhythmical embrocations, massage, stress, heart-rate-variability
Citation: Werthmann PG, Cysarz D, Jungbluth M, Lederer A-K, Nenova G, Huber R, van Dijk M and Kienle GS (2025) Efficacy and safety of massage for postoperative stress in colorectal cancer patients: a randomized, controlled, three-arm trial. Front. Oncol. 15:1439420. doi: 10.3389/fonc.2025.1439420
Received: 27 May 2024; Accepted: 13 January 2025;
Published: 05 February 2025.
Edited by:
Kerstin Uvnäs Moberg, Swedish University of Agricultural Sciences, SwedenReviewed by:
Ursula Wolf, University of Bern, SwitzerlandLuwen Zhu, Heilongjiang University of Chinese Medicine, China
Copyright © 2025 Werthmann, Cysarz, Jungbluth, Lederer, Nenova, Huber, van Dijk and Kienle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul G. Werthmann, cGF1bC53ZXJ0aG1hbm5AdW5pa2xpbmlrLWZyZWlidXJnLmRl
 Paul G. Werthmann
Paul G. Werthmann Dirk Cysarz
Dirk Cysarz Melanie Jungbluth1
Melanie Jungbluth1 Ann-Kathrin Lederer
Ann-Kathrin Lederer Roman Huber
Roman Huber Monique van Dijk
Monique van Dijk