- 1Department of Nuclear Medicine, The Second Affiliated Hospital of Soochow University, Suzhou, China
- 2Shanghai Key Laboratory of Molecular Imaging, Shanghai University of Medicine and Health Sciences, Shanghai, China
- 3Department of Oncology, Xuyi People’s Hospital, Xuyi, China
- 4Department of Nuclear Medicine, The First Affiliated Hospital of Soochow University, Suzhou, China
- 5State Key Laboratory of Radiation Medicine and Protection, Soochow University, Suzhou, China
- 6National Health Commission (NHC) Key Laboratory of Nuclear Medicine and Jiangsu Key Laboratory of Molecular Nuclear Medicine, Wuxi, China
Purpose: Parathyroid carcinoma (PC) is an extremely rare disease, typically presenting with marked elevations of serum calcium concentrations and associated with significantly increased parathyroid hormone (PTH) levels. Although it progresses slowly, approximately25% of PC patients have lung metastases. In the present study, we aimed to evaluate the role of technetium-99m methoxy isobutyl isonitrile (Tc-99m-MIBI; sestamibi) SPECT/CT scintigraphy in the preoperative localization of parathyroid adenomas, incidental metastases findings of PC, and ectopic parathyroid tissue.
Methods: We presented a rare case alongside a review of the relevant literature.
Results: We described an unusual case of a 25-year-old female patient with co-occurrence of PC and lung metastasis. The primary PC lesion showed no radioactive uptake, while the lung metastasis presented as a hyperfunctioning nodule, successfully localized using Tc-99m-MIBI SPECT/CT and confirmed through surgical and pathological examination.
Conclusions: This case emphasized the uniqueness of Tc-99m-MIBI SPECT/CT imaging in diagnosing PC and metastatic lesions. The appropriate application of this technique may help avert the aggressive clinical progression of PC.
Introduction
Primary hyperparathyroidism (PHPT) is a common cause of hypercalcemia, with parathyroid adenomas accounting for 80%-85% of cases, hyperplasia for 10-15%, and parathyroid carcinoma (PC)comprising less than 1% (1–3). PC is a highly aggressive endocrine tumor, with more than 90% of cases associated with excessive parathyroid hormone (PTH), and its annual incidence is estimated less than 1 case per million (4). Although recent developments in biochemical, molecular, and radiological techniques, PC remains an elusive disease to recognize clinically. Accurate diagnosis is difficult for various reasons, such as its rarity, the lack of specificity, and overlapping symptoms with parathyroid adenoma (PA). Therefore, most cases of PC are detected incidentally and confirmed by histopathology and characterized by vascular or capsular invasion (5).
Tc-99m-MIBI SPECT/CT, ultrasonography (US), X-ray computed tomography (CT) and magnetic resonance imaging (MRI) are recommended for accurate localization of parathyroid lesions prior to invasive parathyroidectomy. Among these, Tc-99m-MIBI and US of the neck are the most commonly utilized imaging modalities in clinical practice. However, Tc-99m-MIBI SPECT/CT plays an irreplaceable role in the accurate localization of parathyroid lesions, especially in detecting ectopic or metastatic lesions.
In the present study, we presented a rare case of nonfunctional PC with functional lung metastasis. While the primary parathyroid lesion exhibited no radioactive concentration, the lung metastasis showed a high concentration of radioactivity, was accurately localized through Tc-99m-MIBI SPECT/CT and confirmed by surgical and pathological examination. In the present study, we aimed to evaluate the characteristics of PC and assess the critical role of Tc-99m-MIBI SPECT/CT in localizing both primary PC and distant metastases. Moreover, the patient provided informed consent for publication of this case.
Case presentation
A 25-year-old female presented with a 3-year history of episodic chest tightness and shortness of breath, which had worsened over the past 3 months. Initially, these symptoms appeared after emotional agitation, with episodes of chest discomfort and distress resolving with rest and without special treatment. In recent months, her condition deteriorated, manifesting as severe fatigue, low spirits, nausea, vomiting, anorexia, bone pain, and weight loss.
On August 18, 2017, she first consulted to the Gastroenterology Department of our hospital, and a gastroscopy revealed chronic gastritis. Three days later, she was referred to the Cardiology Department for evaluation due to a short Q-T interval identified on an electrocardiogram (ECG). For further evaluation and management, she was subsequently admitted with a preliminary diagnosis of “cardiomyopathy”.
On admission, her physical examinations revealed a heart rate of 100 beats/min and backache, with no other significant findings. Her medical history included a myomectomy performed in 2014, with no history of head or neck radiation exposure or a family history of thyroid or parathyroid cancer.
At the time of hospitalization, laboratory tests revealed severe hypercalcemia (5.37 mmol/L; normal range: 2.0-2.7 mmol/L) and a significantly increased serum PTH level (613.3 pg/mL; normal range: 12-88 pg/mL). Tumor marker assays and thyroid function tests were unremarkable. The patient was referred to the Endocrinology Department where she received calcium-lowering therapy.
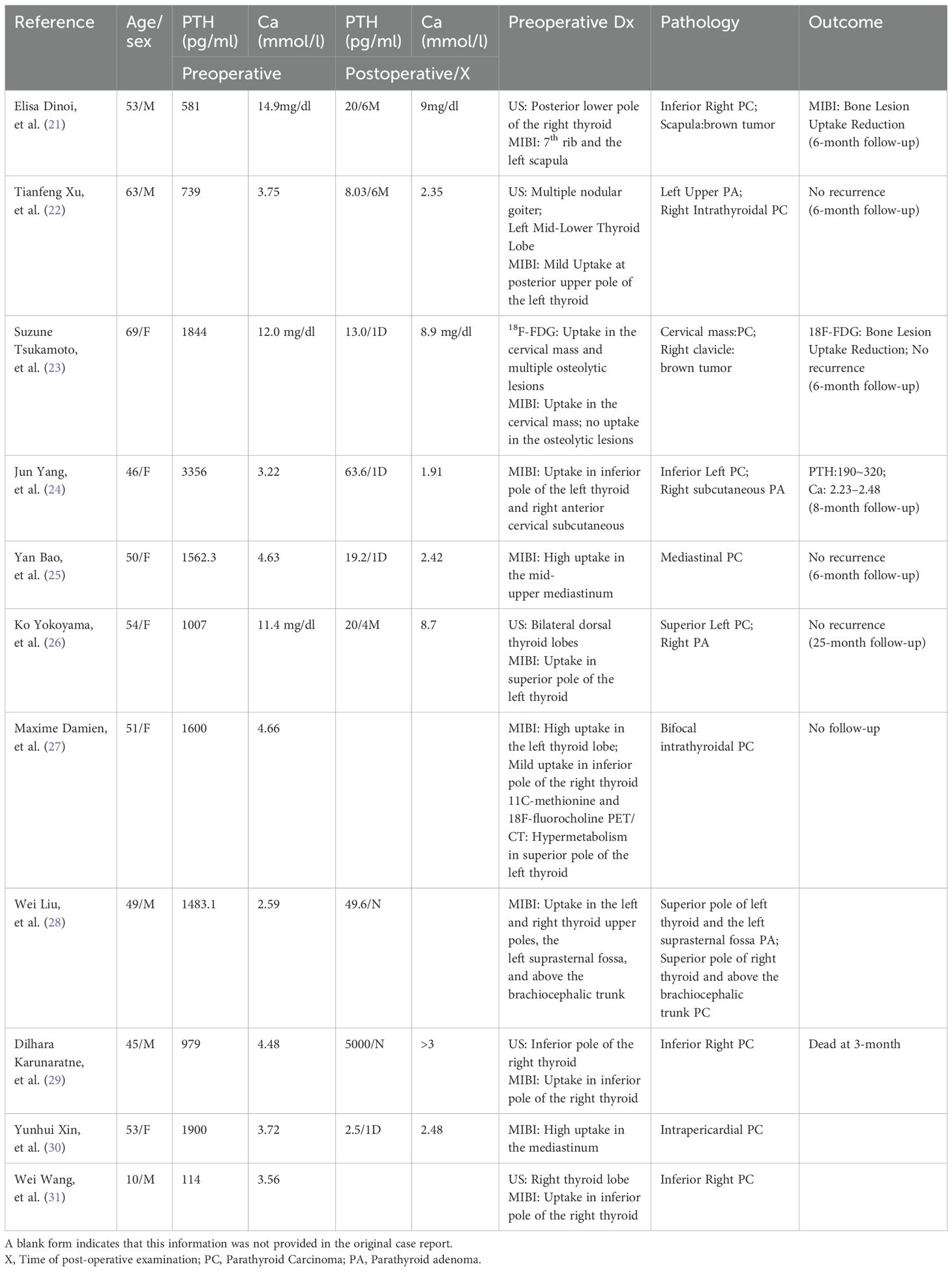
An initial parathyroid ultrasound revealed no abnormalities, likely due to operator experience. A repeat US performed by an experienced radiologist identified an abnormal echo posterior to the right lower thyroid lobe, suspicious for parathyroid lesion (Figure 1). However, dual-phase Tc-99m-MIBI parathyroid scintigraphy failed to detect any parathyroid tumor on both early and delayed images (Figure 2A).
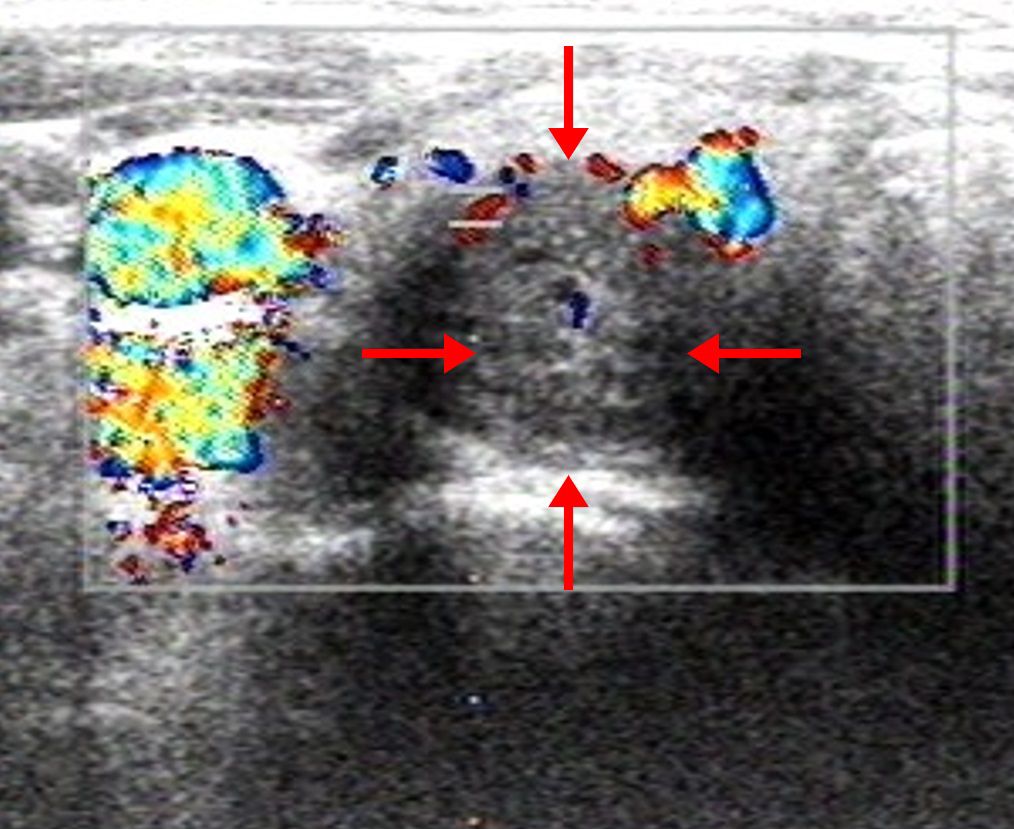
Figure 1. Parathyroid US of the patient. A 29×24×16 mm cystic- solid mixed-echo area in the posterior of the right lower thyroid gland with well-defined borders.
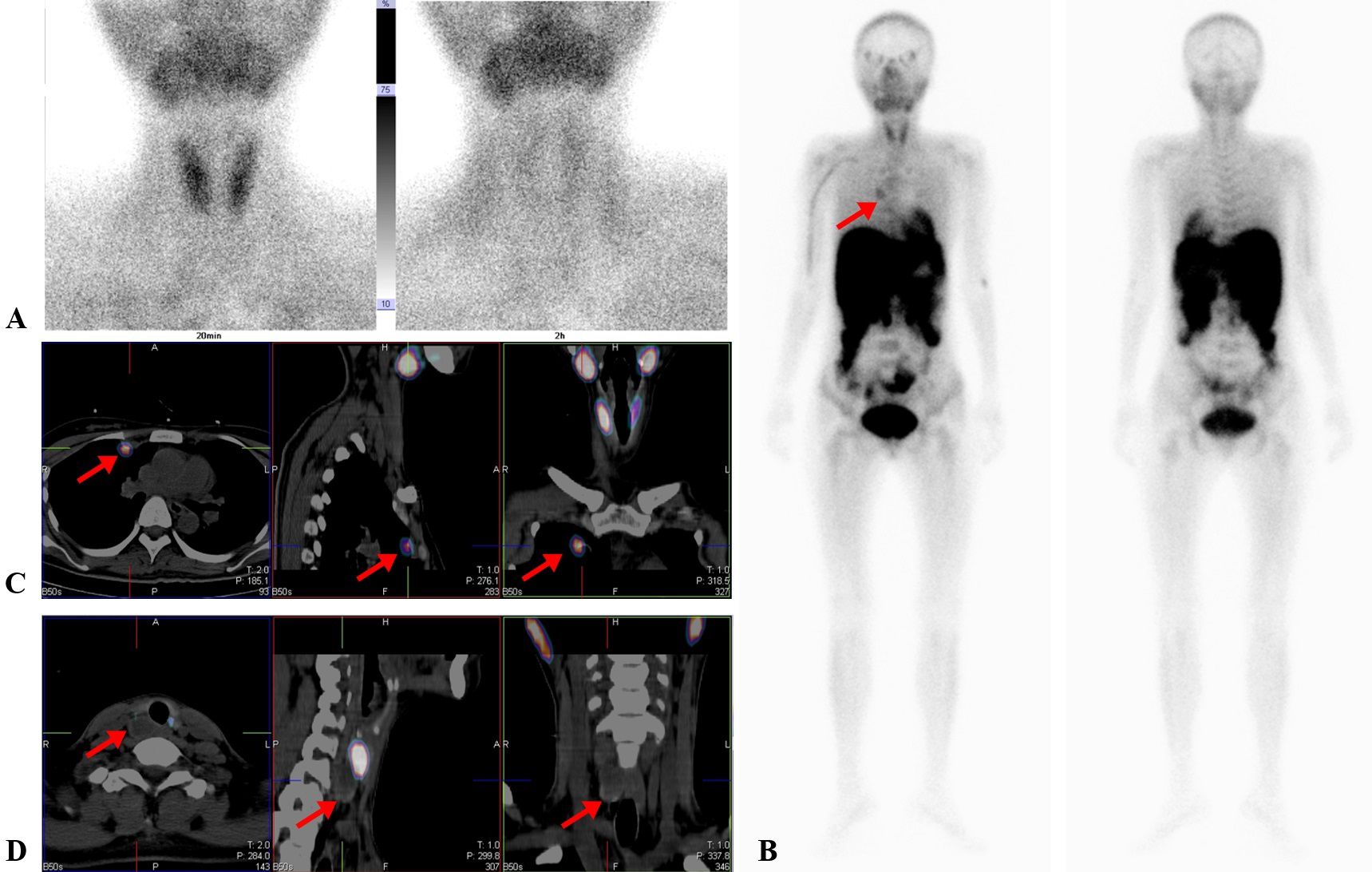
Figure 2. Dual-phase Tc-99m-sestamibi scintigraphy and SPECT/CT scans of the patient. (A) Early and delay imaging of dual-phase Tc-99m-sestamibi parathyroid scintigraphy. The thyroid gland was developed clearly in the early image and quickly decreased in the delayed image, whereas no radiotracer uptake was revealed at the lower pole of the right thyroid lobe both in early and delayed imaging. (B) Tc-99m-MIBI SPECT demonstrated a metastatic lesion in the right chest (arrow). (C) Tc-99m-MIBI SPECT/CT fusion images showed that high radiotracer uptake in the area of the right chest coincided with a mass in the upper right lung through CT scan (arrow). (D) Tc-99m-MIBI SPECT/CT fusion images showed that no survival of accumulation in the posterior of the right lower thyroid gland with low density (arrow).
Subsequently, an imagological diagnosis was performed to localize potential hyperfunctioning parathyroid tissues. ATc-99m-MIBI whole-body scan (WBS) revealed a hyperfunctioning nodule in the right chest on both early and delayed images (Figure 2B). Delayed Tc-99m-MIBI SPECT/CT fusion images showed that the abnormal Tc-99m-MIBI uptake was located in the area of the right upper lung (Figure 2C), while the low-density lesion posterior to the right thyroid lobe showed no uptake (Figure 2D).
Based on clinical symptoms, laboratory results, and radiological image features, we initially suspected that the chest lesion was the metastasis of PC. However the possibility of an ectopic parathyroid gland could not be completely excluded at that stage.
The patient was subsequently referred to the Department of General Surgery, where she underwent a parathyroidectomy followed by a pneumonectomy. During the initial right parathyroidectomy, a 1.5×2.0 cm mass was identified posterior to the right thyroid gland. of the lesion displayed central areas of hemorrhage and necrosis. Subsequently, an operation of right lung wedge resection was carried out, disclosing a soft and friable mass about 2.0×3.0 cm near the horizontal fissure in the middle lobe of the right lung, densely adherent to the pleura.
Intraoperative parathyroid hormone assay showed a significant declined, although the level remained elevated at 112.5 pg/mL (normal range: 12-88 pg/mL).Notably, serum calcium normalized to 2.57 mmol/L (normal range: 2.0-2.7 mmol/L) 30 minutes post-operation.
Histopathology and immunohistochemistry (IHC) results revealed that the cervical lesion in the posterior right thyroid lobe was PC, and the lung lesion was determined to be a metastasis site of the PC (Figure 3).
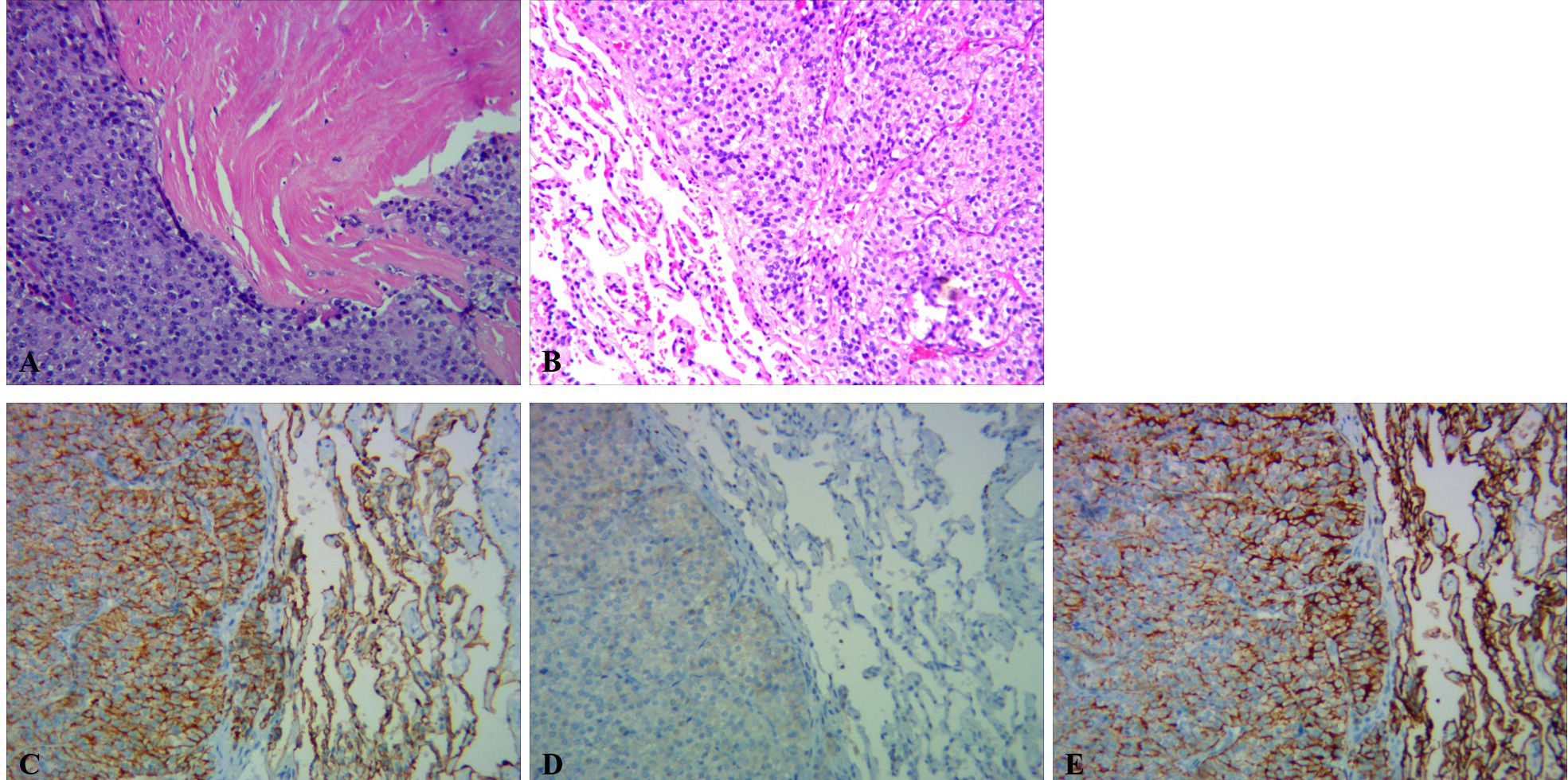
Figure 3. Histological sections of the PC and pulmonary lesion. (A) Histopathology (hematoxylin-eosin staining) of PC. The tumor had a solid growth pattern, which invaded the surrounding soft tissues with prominent necrosis (×100). (B) Histopathology (hematoxylin-eosin staining) of the pulmonary lesion. The pulmonary lesion was predominantly solid with round and atypical spindle stromal cells. (C–E) IHC of the pulmonary lesion staining revealed that the lesional cells were positive for AE1-AE3 (C), Bcl2 (D), and CK7 (E), respectively (×100).
At one month post-operation, follow-up laboratory tests showed a persistently elevated PTH level of 323.8 pg/mL (normal range: 12-88 pg/mL), despite a normal serum calcium level of 2.15 mmol/L (normal range: 2.0-2.7 mmol/L). Neck and chest CT scans revealed the presence of metastatic nodules in both lungs (Figure 4).
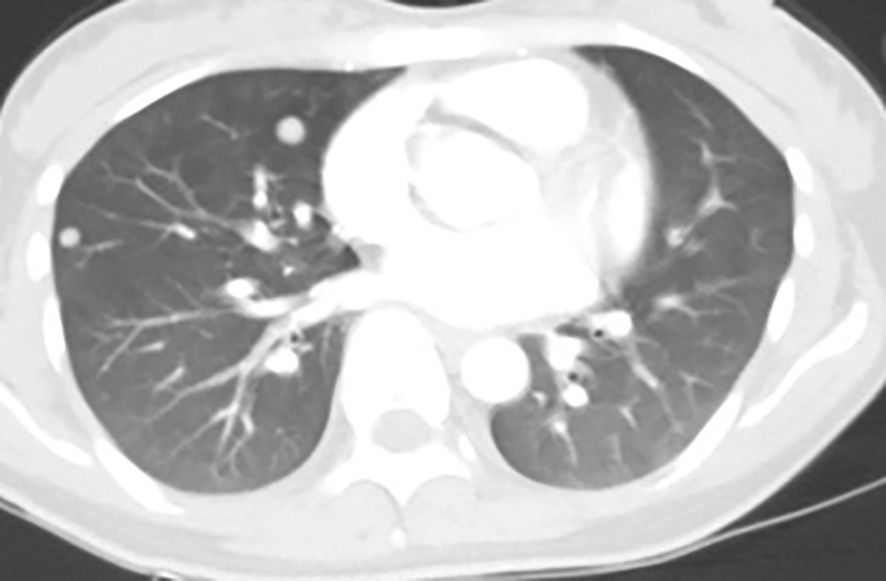
Figure 4. CT scan of the chest showed numbers of nodules with tissue density distributed on both lungs.
Discussion
PC was first described by De Quervain in 1904 (6). It occurs either as part of a genetic syndrome or sporadically, with an overall incidence of 3.5 to 5.7 per 10 million (7). Most PCs secrete high levels of PTH, leading tohypercalcemia associated with PHPT. Symptoms of hypercalcemia range from nonspecific manifestations, such as anorexia, nausea, vomiting, fatigue, and weakness, to more severe complications like polyuria, polydipsia, nephrocalcinosis, and renal failure. Moreover, other symptoms of hyperparathyroidism include bone pain, and fractures, which are similar to PA and difficult to differentiate.
Sharretts M et al. reported that PC patients were associated with serious hypercalcemia, high PTH level, and younger age, and these patients were prone to hypercalcemic crisis, renal dysfunction, and skeletal system changes (8). Current guideline of PC suggests that the possibility of PC should be considered in patients with greatly increased PTH level (>5-fold normal or >500 pg/mL) and severe hypercalcemia (>14 mg/dL) (4). In this case, the patients presented with a PTH level of 613.3 pg/mL and serum calcium of 96.66 mg/dL, strongly suggesting PC.
PC is a slow-growing disorder, with metastases occurring late, primarily in bones, lungs, and liver. The survival of PC patients with distant metastases is extremely low, especially for those with functioning distant metastases, which may also seriously affect the quality of life (9). Surgery remains the primary curative treatment for PC and its metastases, as radiotherapy and chemotherapy have limited role efficacy (4, 10).
In the present case, the patient underwent parathyroidectomy and pneumonectomy which initially reduced PTH and serum calcium levels significantly. However, the PTH level increased again at the one-month follow-up, despite normocalcemia. This suggested possible disease progression(recurrence or metastases), although ectopic parathyroid tissue could not be excluded. Subsequent neck and chest CT scans revealed the presence of metastatic nodules in both lungs.
Parathyroid carcinoma with metastases was associated with a high risk of local and distant recurrence, indicating a poor prognosis (11–14). Early and accurate localization of lesions is crucial for effective management. Non-invasive imaging modalities, such as Tc-99m-MIBI SPECT/CT, US, and CT, are routinely used to localize parathyroid lesions before invasive parathyroidectomy. US is a widely used, cost-effective, and sensitive method for diagnosing parathyroid lesions, but its accuracy depends heavily on the experience of the operator, and this modality has a suboptimal detection rate in silent areas, such as the mediastinum, tracheoesophageal groove, and retroesophageal region (15). CT offers better detection of lesions in the mediastinum but struggles to distinguish lymph nodes from parathyroid glands in the neck.
Tc-99m-MIBI parathyroid scintigraphy is particularly valuable for detecting parathyroid lesions with sensitivity rates of 50%-86% using the dual-phase protocol (16). However, false-negative results can occur due to factors such as o lesion size, cystic changes, hyperthyroidism, thyroiditis, or tumor composition (17). Additionally, up to 10% of PCs are non-functional, leading to false-negative results (8, 18, 19).
In cases where PTH and calcium levels are high but dual-phase Tc-99m-MIBI parathyroid scintigraphy is negative, a whole-body Tc-99m-MIBI (WBS) may be necessary to detect metastatic or ectopic lesions. Despite its high specificity and sensitivity, SPECT alone is limited by its inability to provide anatomical details. The hybrid SPECT/CT system overcomes this limitation by combining functional and anatomical imaging, resulting in improved diagnostic accuracy and image quality (20). Table 1 summarized 11 cases of parathyroid carcinoma similar to this case reported in the past five years.
In our present case, the initial parathyroid US showed no abnormalities, while a subsequent US identified an abnormal parathyroid lesion. This discrepancy was attributed to the experiences of different operators. Moreover, dual-phase Tc-99m-MIBI parathyroid scintigraphy produced false-negative results in both early and delayed phases. The diagnosis of PC was ultimately confirmed intraoperatively and through histopathological examination. The false-negative Tc-99m-MIBI result may be explained by the presence of hemorrhage and necrosis within the parathyroid lesion, as observed during surgery.
Conclusions
Regrettably, there is currently a lack of definitive preoperative diagnostic methods for parathyroid carcinoma (PC). The preferred diagnostic approach remains the combination of ultrasound and Tc-99m-MIBI SPECT/CT imaging. When severe hypercalcemia and parathyroid hormone (PTH) levels are 3-10 times higher than normal, PC should be considered. 18F-FDG PET/CT imaging is considered a sensitive and effective method for the initial staging of parathyroid carcinoma, tumor recurrence, assessment of residual lesions after treatment, and detection of distant metastases. 18F-choline PET/CT also holds significant value in localizing parathyroid carcinoma and seeking out metastatic lesions. A combined diagnostic approach, including imaging and serum biomarkers, can improve the preoperative diagnostic rate of PC.
In the future, we hope to develop specific targets for biomarkers in parathyroid tissue to facilitate early diagnosis and localization of PC and distant metastases. Such advancements would greatly enhance our understanding and treatment of parathyroid carcinoma, providing patients with more accurate diagnoses and more effective treatment plans.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of The Second Affiliated Hospital of Soochow University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YZ: Writing – original draft. LW: Investigation, Software, Writing – original draft. JY: Writing – original draft. SD: Supervision, Writing – original draft. YS: Supervision, Validation, Writing – review & editing. ZL: Supervision, Validation, Writing – review & editing, Conceptualization. ZH: Investigation, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by The Second Affiliated Hospital of Soochow University Clinical Trial Organization Capacity Enhancement for Nuclear Medicine Specialties[No.SLT201932].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PHPT, primary hyperparathyroidism; PC, parathyroid carcinoma; PA, parathyroid adenoma; PTH, parathyroid hormone; MIBI, methoxyisobutylisonitrile; SPECT/CT, hybrid single photon emission computed tomography/x-ray computed tomography; US, ultrasonography.
References
1. Cetani F, Pardi E, Marcocci C. Parathyroid carcinoma. Front Horm Res. (2019) 51:63–76. doi: 10.1159/000491039
2. Rawat N, Khetan N, Williams DW, Baxter JN. Parathyroid carcinoma. Br J Surg. (2005) 92:1345–53. doi: 10.1002/bjs.5182
3. Cetani F, Frustaci G, Torregrossa L, Magno S, Basolo F, Campomori A, et al. A nonfunctioning parathyroid carcinoma misdiagnosed as a follicular thyroid nodule. World J Surg Oncol. (2015) 13:270. doi: 10.1186/s12957-015-0672-9
4. Wei CH, Harari A. Parathyroid carcinoma: update and guidelines for management. Curr Treat Options Oncol. (2012) 13:11–23. doi: 10.1007/s11864-011-0171-3
5. Lee YS, Hong SW, Jeong JJ, Nam KH, Chung WY, Chang HS, et al. Parathyroid carcinoma: a 16-year experience in a single institution. Endocr J. (2010) 57:493–7. doi: 10.1507/endocrj.k09e-365
6. Schulte KM, Galata G, Talat N. Mediastinal parathyroid cancer. Cancers (Basel). (2022) 14(23):5852. doi: 10.3390/cancers14235852
7. Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM. Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer. (2007) 109:1736–41. doi: 10.1002/cncr.22599
8. Sharretts JM, Kebebew E, Simonds WF. Parathyroid cancer. Semin Oncol. (2010) 37:580–90. doi: 10.1053/j.seminoncol.2010.10.013
9. Fingeret AL. Contemporary evaluation and management of parathyroid carcinoma. JCO Oncol Pract. (2021) 17:17–21. doi: 10.1200/JOP.19.00540
10. Hsu P, Liu C-Y, Chen M-H. Refractory hypercalcemia due to hyperparathyroidism in a patient with metastatic parathyroid carcinoma. J Cancer Res Pract. (2018) 5:84–7. doi: 10.1016/j.jcrpr.2018.01.002
11. Kruljac I, Pavic I, Matesa N, Mirosevic G, Maric A, Becejac B, et al. Intrathyroid parathyroid carcinoma with intrathyroidal metastasis to the contralateral lobe: source of diagnostic and treatment pitfalls. Jpn J Clin Oncol. (2011) 41:1142–6. doi: 10.1093/jjco/hyr094
12. Ng SH, Lang BH. Parathyroid carcinoma in a 30-year-old man: a diagnostic and management challenge. World J Surg Oncol. (2013) 11:83. doi: 10.1186/1477-7819-11-83
13. Tang AL, Aunins B, Chang K, Wang JC, Hagen M, Jiang L, et al. A multi-institutional study evaluating and describing atypical parathyroid tumors discovered after parathyroidectomy. Laryngoscope Investig Otolaryngol. (2022) 7:901–5. doi: 10.1002/lio2.814
14. Erovic BM, Goldstein DP, Kim D, Mete O, Brierley J, Tsang R, et al. Parathyroid cancer: outcome analysis of 16 patients treated at the Princess Margaret Hospital. Head Neck. (2013) 35:35–9. doi: 10.1002/hed.22908
15. Zhang R, Zhang Z, Huang P, Li Z, Hu R, Zhang J, et al. Diagnostic performance of ultrasonography, dual-phase (99m)Tc-MIBI scintigraphy, early and delayed (99m)Tc-MIBI SPECT/CT in preoperative parathyroid gland localization in secondary hyperparathyroidism. BMC Med Imaging. (2020) 20:91. doi: 10.1186/s12880-020-00490-3
16. Chang MC, Tsai SC, Lin WY. Dual-phase 99mTc-MIBI parathyroid imaging reveals synchronous parathyroid adenoma and papillary thyroid carcinoma: a case report. Kaohsiung J Med Sci. (2008) 24:542–7. doi: 10.1016/S1607-551X(09)70014-2
17. Bergenfelz AO, Wallin G, Jansson S, Eriksson H, Martensson H, Christiansen P, et al. Results of surgery for sporadic primary hyperparathyroidism in patients with preoperatively negative sestamibi scintigraphy and ultrasound. Langenbecks Arch Surg. (2011) 396:83–90. doi: 10.1007/s00423-010-0724-0
18. Montenegro FL, Tavares MR, Durazzo MD, Cernea CR, Cordeiro AC, Ferraz AR. Clinical suspicion and parathyroid carcinoma management. Sao Paulo Med J. (2006) 124:42–4. doi: 10.1590/s1516-31802006000100009
19. Al-Kurd A, Mekel M, Mazeh H. Parathyroid carcinoma. Surg Oncol. (2014) 23:107–14. doi: 10.1016/j.suronc.2014.03.005
20. Li Q, Pan J, Luo Q, Wang Y, Bao Y, Jia W. The key role of 99mTc-MIBI SPECT/CT in the diagnosis of parathyroid adenoma: a case report. Arch Endocrinol Metab. (2015) 59:265–9. doi: 10.1590/2359-3997000000048
21. Dinoi E, Prete A, Sardella C, Pierotti L, Della Valentina S, Dal Lago A, et al. The challenge of the differential diagnosis between brown tumors and metastases in parathyroid carcinoma: a case report. Front Endocrinol (Lausanne). (2024) 15:1414896. doi: 10.3389/fendo.2024.1414896
22. Xu T, Zheng X, Wei T. Incidental synchronous intrathyroidal parathyroid carcinomas and papillary thyroid microcarcinoma with compressive neck mass and primary hyperparathyroidism: case report and literature review. BMC Endocr Disord. (2024) 24:125. doi: 10.1186/s12902-024-01656-8
23. Tsukamoto S, Kawabata K, Kawamura H, Takata K, Hosono M. Differentiating brown tumor from bone metastasis in parathyroid cancer using 18 F-FDG PET and 99m tc-MIBI SPECT. Clin Nucl Med. (2024) 49:444–6. doi: 10.1097/RLU.0000000000005115
24. Yang J, Lu X, Zhou P, Liu H, Wang J, Su X. Recurrence hyperparathyroidism caused by synchronous parathyroid carcinoma and parathyromatosis in a patient with long-term hemodialysis. BMC Nephrol. (2023) 24:293. doi: 10.1186/s12882-023-03328-6
25. Bao Y, Kang G, Wu X, Li J, Huang Y, Wang Y. Mediastinal parathyroid carcinoma: a case report and review of the literature. BMC Endocr Disord. (2023) 23:130. doi: 10.1186/s12902-023-01363-w
26. Yokoyama K, Suganuma N, Rino Y. Left parathyroid carcinoma with secondary hyperparathyroidism: a case report. BMC Endocr Disord. (2023) 23:108. doi: 10.1186/s12902-023-01370-x
27. Damien M, Rodriguez A, Kleynen P, Dequanter D, Bouland C. An unusual case of primary hyperparathyroidism: case report of a bifocal intrathyroidal parathyroid carcinoma. Ear Nose Throat J. (2023) 102:NP5–7. doi: 10.1177/0145561320977466
28. Liu W, Huang JM, Guan MC, Xie P. Hyperparathyroidism caused by coexisting parathyroid hyperplasia and unilateral bifocal parathyroid carcinoma. Clin Nucl Med. (2022) 47:985–8. doi: 10.1097/RLU.0000000000004343
29. Karunaratne D, Owens E, Kirkland P, Zainab Al SA, Howlett D. Metastatic parathyroid cancer: a rare cause of hypercalcaemia. BMJ Case Rep. (2021) 4(10):e244302. doi: 10.1136/bcr-2021-244302
30. Xin Y, Zhao T, Wei B, Gu H, Jin M, Shen H, et al. Intrapericardial parathyroid carcinoma: a case report. Endocrine. (2020) 69:456–60. doi: 10.1007/s12020-020-02283-8
Keywords: parathyroid carcinoma, lung metastasis, PTH, Tc-99m-MIBI SPECT/CT, diagnosis, case report
Citation: Zhu Y, Wang L, You J, Deng S, Shi Y, Liu Z and Hong Z (2024) Diagnostic value of Tc-99m-MIBI SPECT/CT in parathyroid carcinoma with lung metastasis: a case report and literature review. Front. Oncol. 14:1501447. doi: 10.3389/fonc.2024.1501447
Received: 25 September 2024; Accepted: 09 December 2024;
Published: 24 December 2024.
Edited by:
Georgios S. Limouris, National and Kapodistrian University of Athens, GreeceReviewed by:
Ioannis Koutelidakis, Aristotle University of Thessaloniki, GreeceSabaretnam Mayilvaganan, Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGI), India
Copyright © 2024 Zhu, Wang, You, Deng, Shi, Liu and Hong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhihui Hong, aG9uZ3poaWh1aTUxNUAxMjYuY29t; Zengli Liu, bGl1emVuZ2xpQDEyNi5jb20=
†These authors have contributed equally to this work and share first authorship
 Yirong Zhu
Yirong Zhu Lian Wang3†
Lian Wang3† Shengming Deng
Shengming Deng Yizhen Shi
Yizhen Shi Zhihui Hong
Zhihui Hong