- Division of Biliary Tract Surgery, Department of General Surgery, West China Hospital, Sichuan University, Chengdu, Sichuan, China
Objective: The superiority of laparoscopic liver resection (LLR) and open liver resection (OLR) in obese patients remains controversial. The study aims to assess the available literature and compare the perioperative outcomes of LLR and OLR for liver tumors in obese patients.
Methods: We searched PubMed, Cochrane Library, Embase, and Web of Science databases for studies comparing LLR and OLR. Odds ratios (ORs) and mean differences (MDs) with 95% confidence intervals (CIs) were calculated.
Results: Nine studies were included, with a total of 1116 patients (LLR group: 482 patients; OLR group: 634 patients). Compared with OLR, LLR has lower overall morbidity (OR 0.47, 95% CI 0.34, 0.64), major complications (OR 0.45, 95% CI 0.25, 0.82), surgical site infection (OR 0.18, 95% CI 0.07, 0.48), bile leak (OR 0.45, 95% CI 0.22, 0.95), less blood loss (MD, -329.12 mL; 95% CI, -623.35, -34.88), and shorter length of stay (MD, -5.20 days; 95% CI, -7.43, -2.97). There were no significant differences in mortality, operation time, liver failure, and blood transfusion between the two groups.
Conclusions: LLR for obese patients is safe and feasible. Compared to OLR, it offers better short-term outcomes. Further randomized controlled trials to verify the potential advantages of LLR over OLR are warranted.
1 Introduction
In recent years, with changes in lifestyle, the prevalence of obesity and its related diseases is rising worldwide (1, 2). Previous evidence has shown that obesity is associated with a variety of diseases, such as diabetes, hypertension, cardiovascular disease, and some types of malignancy (3, 4). A meta-analysis of 28 cohort studies involving 8,135,906 participants showed that elevated body mass index (BMI) was associated with the development of primary liver cancer (HR, 1.69; 95%CI 1.50-1.90), and the risk of primary liver cancer increased with increasing BMI (5). In addition, obesity also increases the degree of technical difficulty of surgery and is a risk factor for postoperative complications (6). Zimmitti et al. (7) found that obesity not only increased the operation time, but also increased the intraoperative blood loss and wound and respiratory related complications. How to improve the outcomes of obese patients after liver resection is a serious problem for surgeons.
Compared with traditional open surgery, laparoscopic surgery has the advantages of less damage to the abdominal wall, less intraoperative blood loss and faster postoperative recovery (8). Laparoscopic surgery has been widely used in liver resection. However, the superiority of laparoscopic liver resection (LLR) over open liver resection (OLR) in obese patients remains controversial. A retrospective study by Yoon et al. (9) showed that LLR can significantly reduce the blood loss, the incidence of complications, and the length of hospital stay. However, Yu et al. (10) found no significant differences in intraoperative blood loss, operation time, and postoperative hospital stay between LLR and OLR. To date, meta-analyses comparing the use of LLR versus OLR in obese patients are lacking.
Therefore, the objective of our meta-analysis was to compare perioperative outcomes between LLR and OLR for liver tumors in obese patients. These results may help provide evidence-based medical evidence for surgeons in selecting appropriate surgical approaches for obese patients.
2 Methods
2.1 Search strategy
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (11). The study protocol was registered with the PROSPERO database.
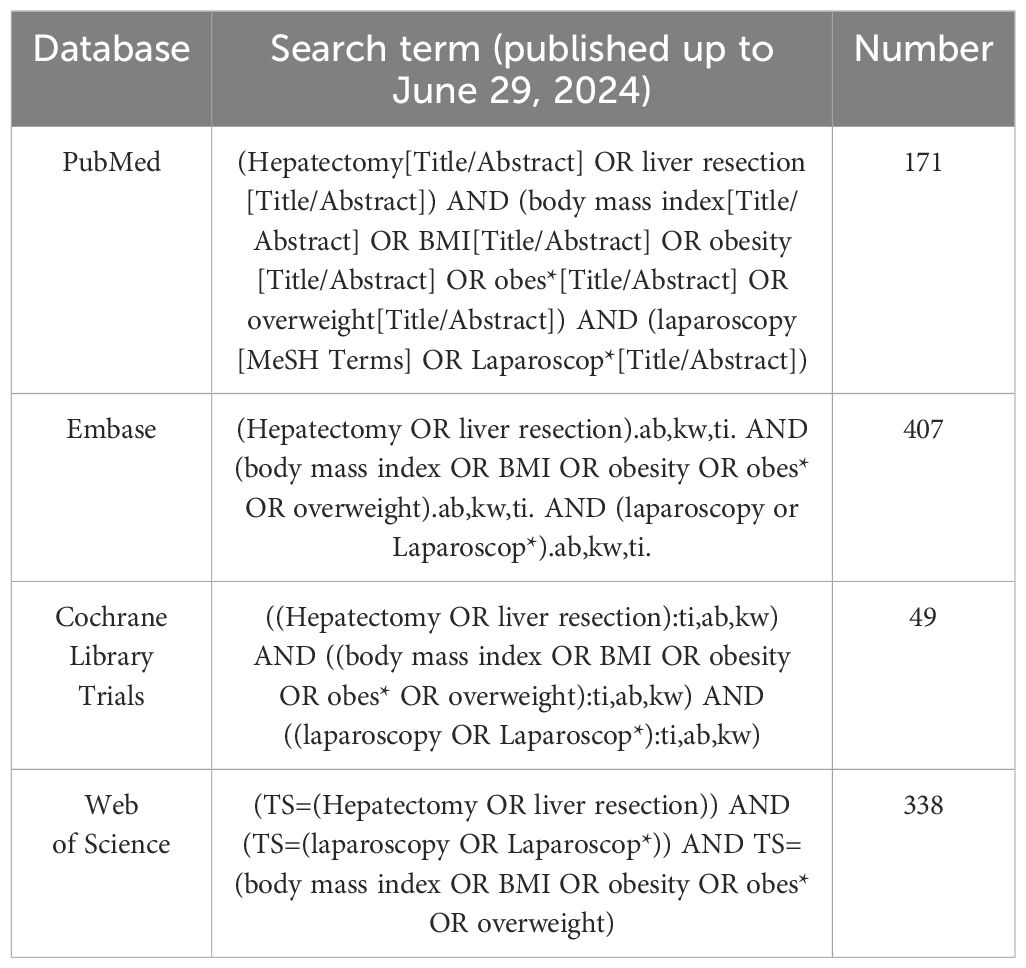
A systematic search using the EMBASE, Web of Science, PubMed, and Cochrane Library databases was conducted up to July 22, 2024. The detailed search strategy is presented in Table 1. In addition, we checked the reference lists of the identified articles and related reviews to further screen for eligible studies. No language restrictions were applied during the search process.
2.2 Study selection
Studies included in this meta-analysis were chosen according to the PICOS (Patient, Intervention, Comparison, Outcomes, Study Type) criteria, as shown below: (1) Patient: Obese patients undergoing liver resection for liver tumors. Obesity is defined as BMI ≥30 (for Western studies) in accordance to the WHO classification or BMI ≥25 in accordance to the International Obesity Task Force (for Asian population) (2); (2) Intervention: LLR; (3) Comparison: OLR; (4) Outcomes: Primary outcomes encompassed mortality, overall morbidity and major complication. Secondary outcomes included blood loss, operation time, surgical site infection, liver failure, bile leak, blood transfusion, and length of stay; (5) Study type: randomized controlled trials (RCTs), cohort studies, and case-control studies.
The exclusion criteria were as follows: reviews, letters, single-arm studies, animal studies, case reports, editorials, conference abstracts, and repeated publications were excluded.
2.3 Data extraction
Data from all eligible studies were independently extracted by two authors, and any disagreements were resolved by discussion with a third-party author. The extracted data included author name, year of publication, study design, country, study population (sample size, age, diagnosis, and sex), and perioperative outcomes (mortality, morbidity, blood loss, operation time, blood transfusion, and length of stay). When data of interest were unavailable, the corresponding author was contacted to obtain the missing data.
2.4 Quality assessment
The quality assessment was conducted independently by two authors using the Newcastle-Ottawa Scale (NOS), which assigns a score on a 9-point scale. A score of ≥7 indicates high quality, and scores of 5–6 indicate moderate quality. Any discrepancies were resolved through discussion, with intervention by a third author whenever necessary.
2.5 Statistical analysis
Odds ratios (ORs) with corresponding 95% confidence intervals (CI) were calculated for qualitative variables and mean difference (MD) for quantitative data. The I² statistic was used to assess the degree of heterogeneity. A random-effects model was used if I² > 50%; otherwise, a fixed-effects model was employed (12). To explore the robustness of the results, we adopted the one-study exclusion method to evaluate the impact of each study on the pooled effect size. The meta-analysis was performed using the Review Manager software (version 5.3). Statistical significance was set at P-value of less than 0.05.
3 Results
3.1 Literature retrieval
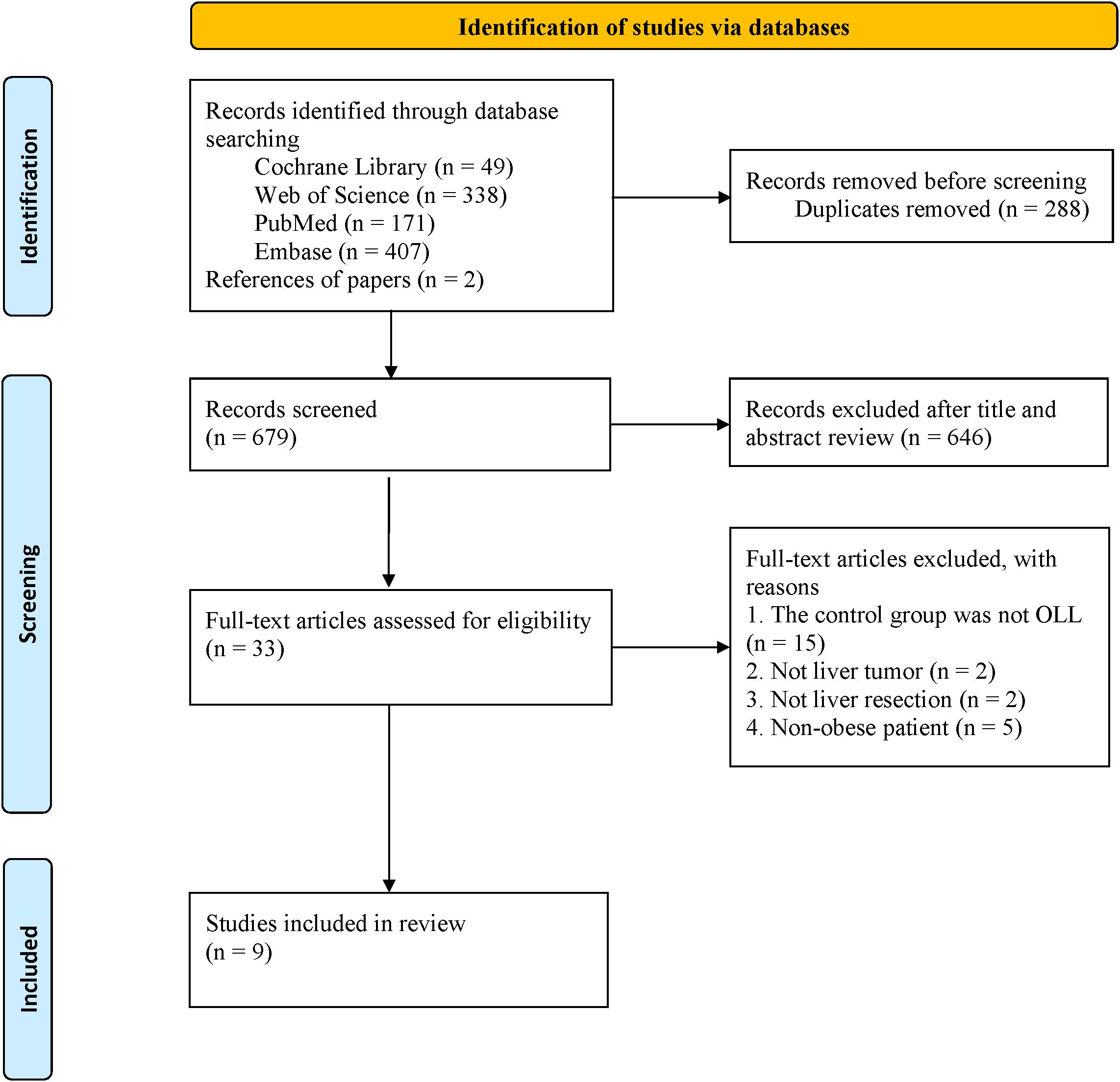
A total of 967 articles were retrieved from the database search. This included 288 duplicates, which were removed. After reviewing titles and abstracts, 646 papers were excluded, and the full texts of the remaining 33 studies were evaluated. Finally, 9 studies (1, 6, 9, 10, 13–17) were included in the final analysis (Figure 1).
3.2 Study characteristics and quality assessment
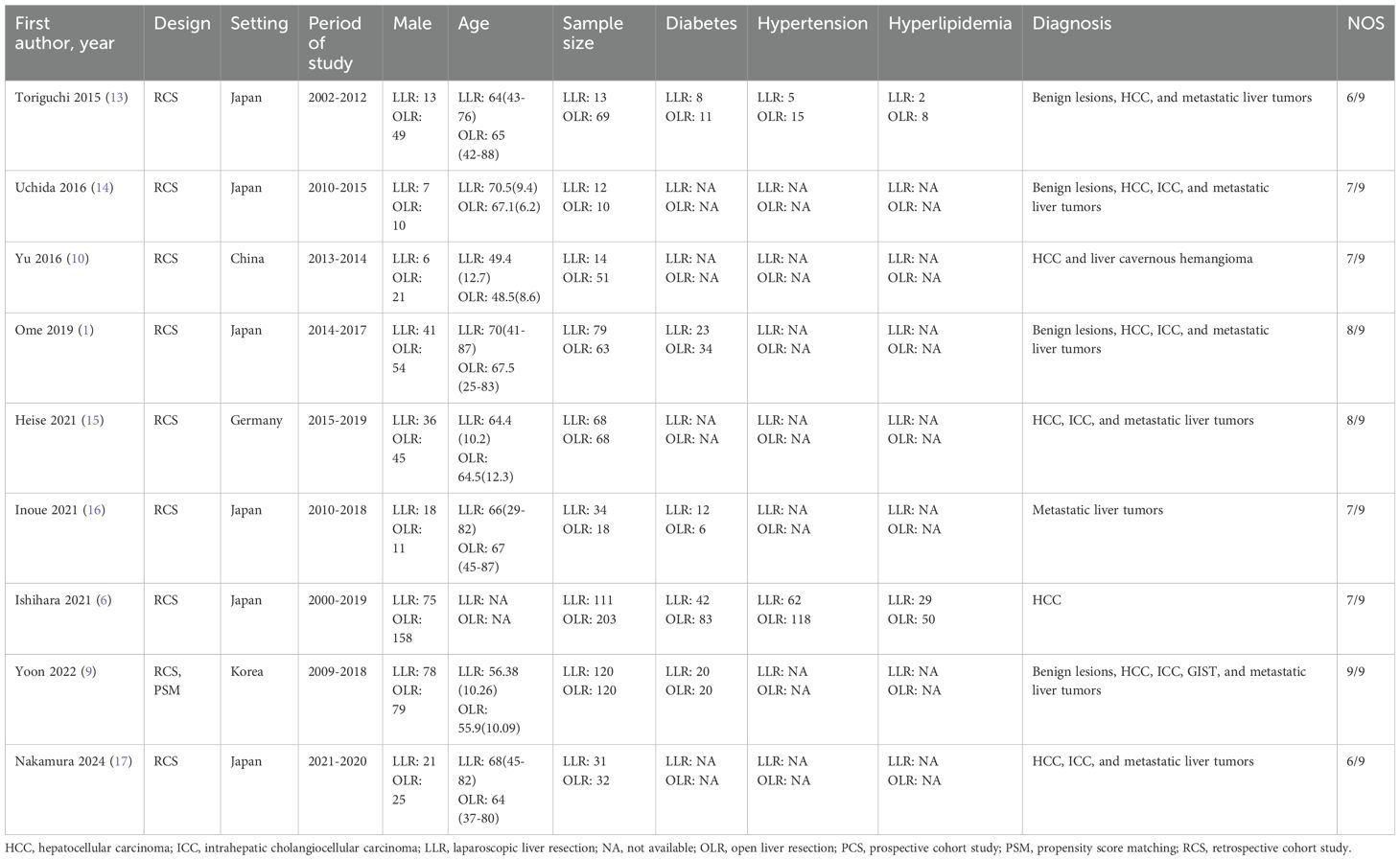
The main characteristics of the 9 included studies are summarized in Table 2. The studies were published between 2015 and 2024 and included 1116 patients (LLR group: 482 patients; OLR group: 634 patients). Indications for operative management were for malignancy only in 4 studies (6, 15–17), whilst benign and malignant disease processes were included in 5 studies (1, 9, 10, 13, 14). The included patients were mainly from Japan, Korea, Germany, and China. All studies (1, 6, 9, 10, 13–17) were considered of moderate to high quality, achieving a score of ≥6 based on the NOS (Table 2).
3.3 Meta-analysis
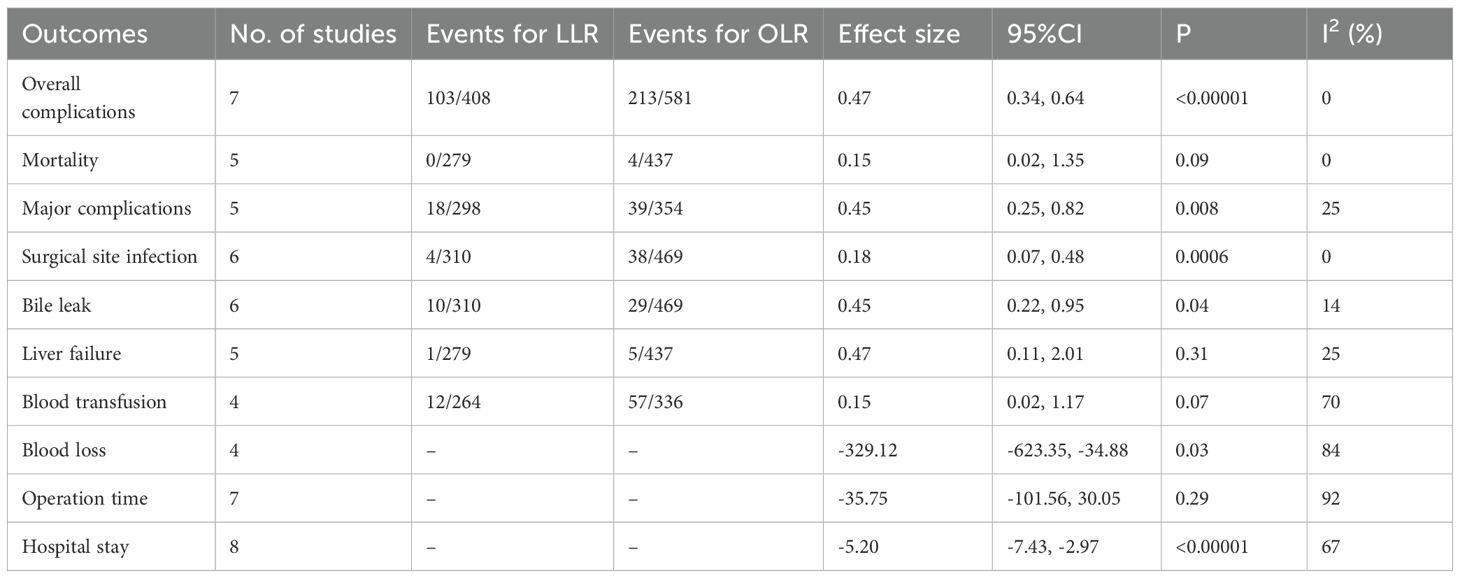
3.3.1 Mortality
Five studies (1, 6, 13, 15, 16) reported data on mortality. The combined results of the 5 studies showed that there was no significant difference between the LLR group and the OLR group regarding this outcome with low heterogeneity (OR 0.15, 95% CI 0.02, 1.35; Heterogeneity: I2 = 0%, P = 0.92) (Figure 2A) (Table 3).
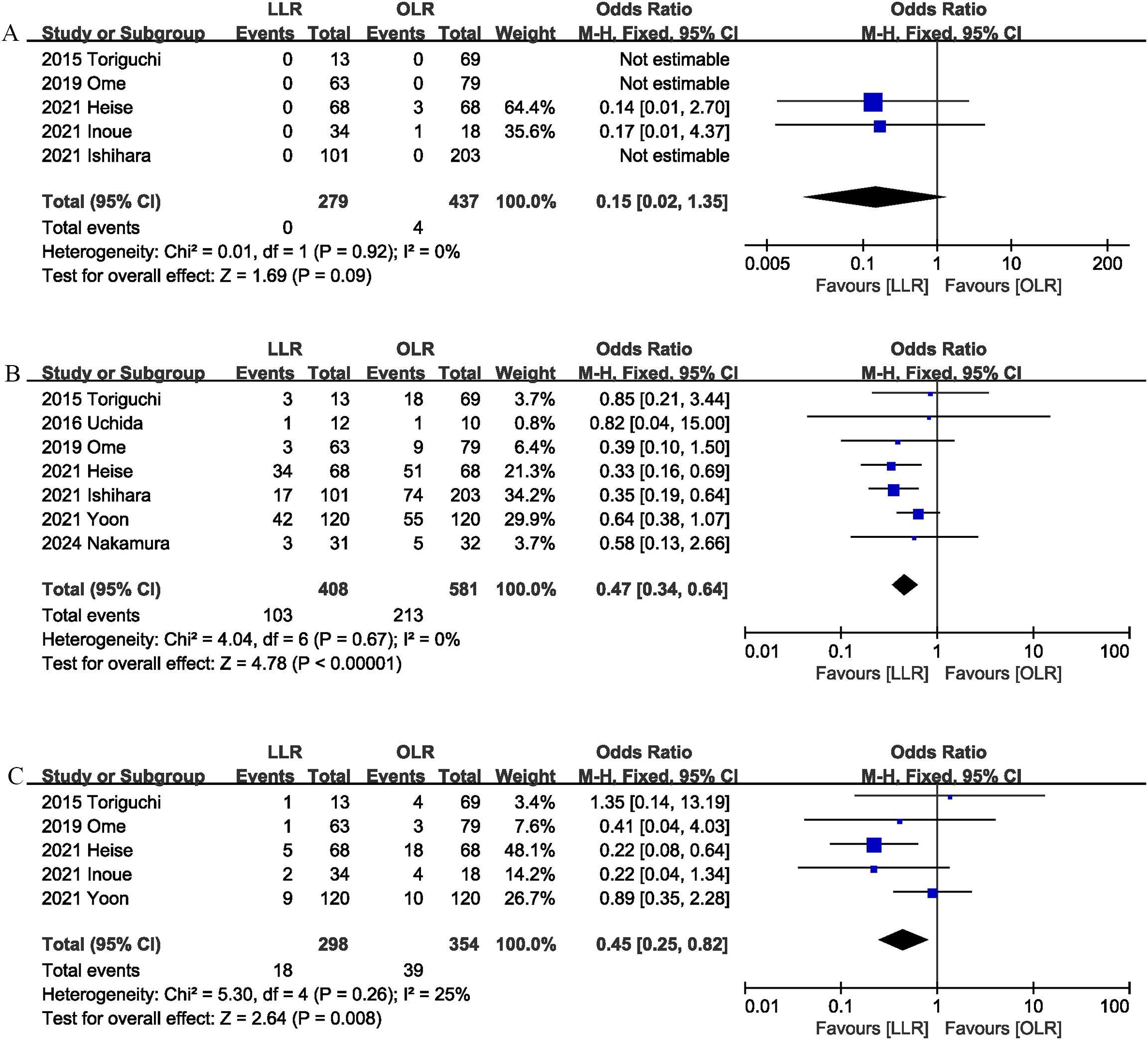
Figure 2. Comparison of primary outcomes between the two groups. (A) mortality, (B) overall morbidity, and (C) major complications.
3.3.2 Morbidity
Seven studies (1, 6, 9, 13–15, 17) assessed overall complication. The pooled results suggested that LLR significantly reduced the overall complication rate (OR 0.47, 95% CI 0.34, 0.64, P < 0.00001), with low heterogeneity (I2 = 0%, P = 0.67) (Figure 2B).
3.3.3 Major complications
Major complications (Clavien–Dindo ≥ 3) was evaluated in 5 studies (1, 9, 13, 15, 16), and the pooled results showed that LLR had lower major complications rate than OLR (OR 0.45, 95% CI 0.25, 0.82; heterogeneity: I2 = 25%, P = 0.26) (Figure 2C).
3.3.4 Blood loss
Four studies (9, 10, 14, 16) provided information on intraoperative blood loss. The combined results showed that LLR significantly reduced the blood loss (MD, -329.12 mL; 95% CI, -623.35, -34.88, P = 0.03; I2 = 84%) (Figure 3A).
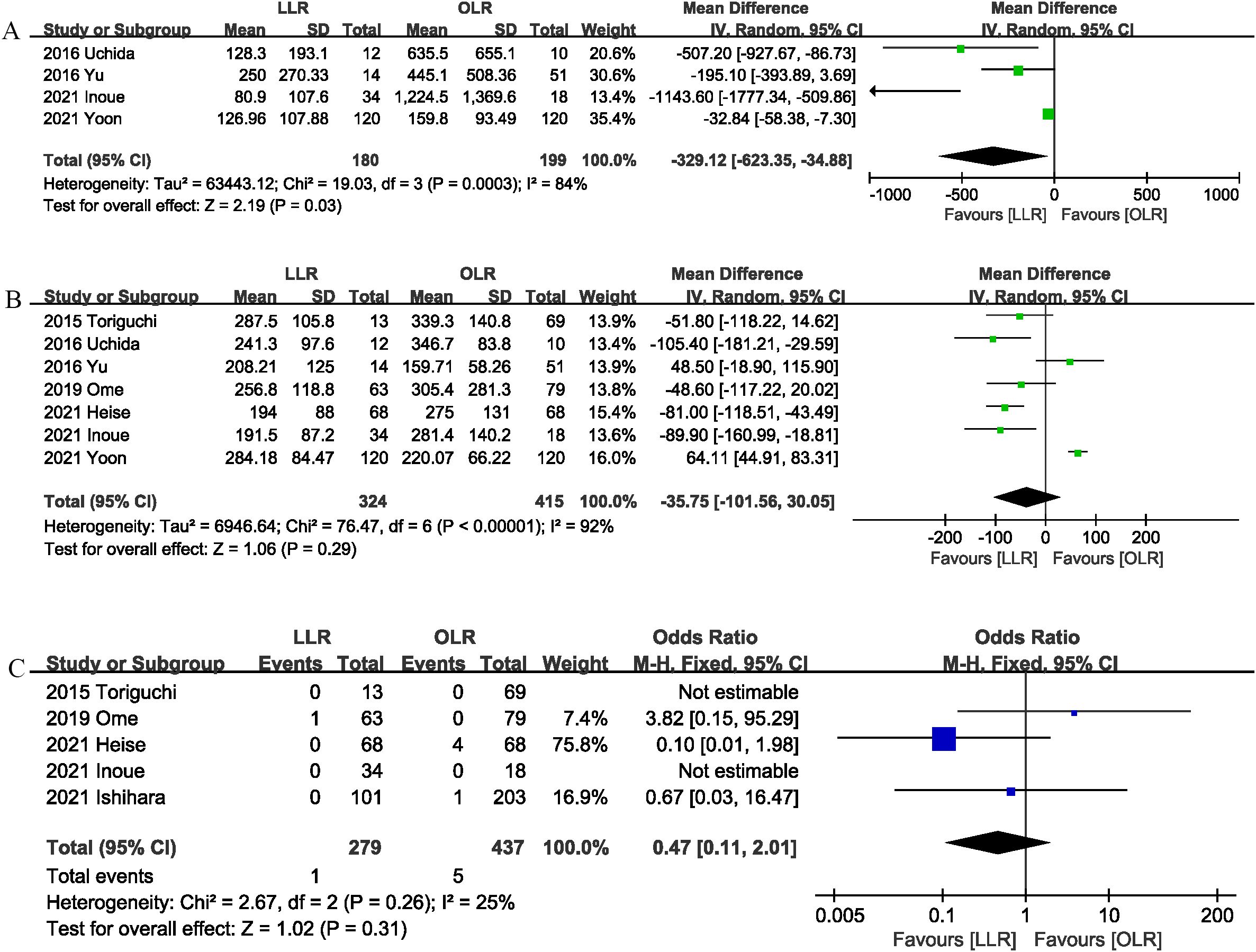
Figure 3. Comparison of secondary outcomes between the two groups. (A) intraoperation blood loss, (B) operation time, and (C) liver failure.
3.3.5 Operation time
The operation time was reported in 7 trials (1, 9, 10, 13–16). The combined results showed that the LLR group has similar operation time as compared with the OLR group (MD, -35.75 mins; 95% CI, -101.56, 30.05, P = 0.29) (Figure 3B).
3.3.6 Liver failure
Liver failure was reported in 5 studies (1, 6, 13, 15, 16), and the combined effect size suggested that the liver failure rates were comparable between the two groups (OR 0.47, 95% CI 0.11, 2.01, P = 0.31; I2 = 25%) (Figure 3C).
3.3.7 Blood transfusion
Four studies (1, 9, 13, 15) reported blood transfusion. No significant differences were observed between the two groups (OR 0.15, 95% CI 0.02, 1.17, P = 0.07), and heterogeneity was low (I2 = 70%, P = 0.02) (Figure 4A).
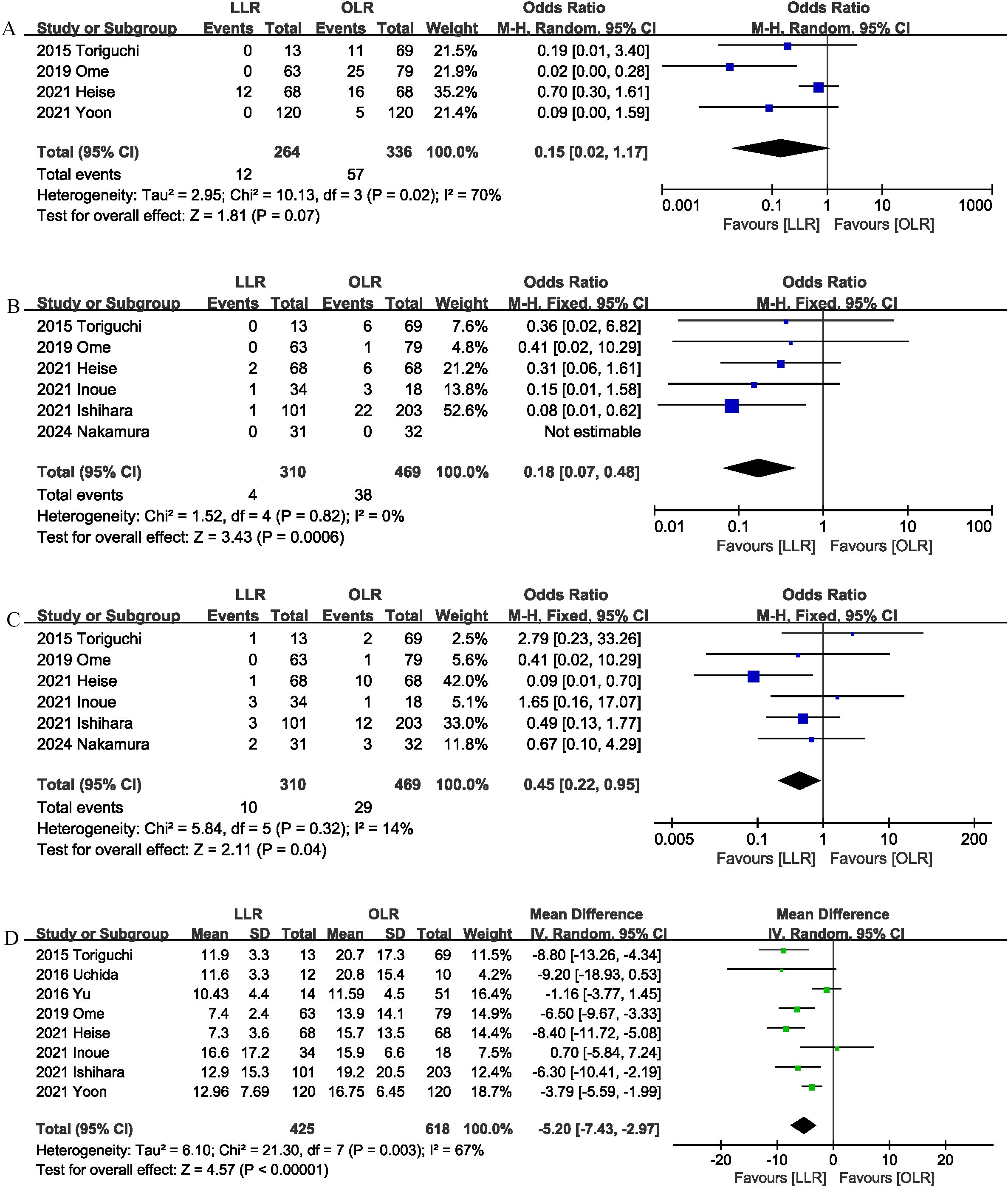
Figure 4. Comparison of secondary outcomes between the two groups. (A) blood transfusion, (B) surgical site infection, (C) bile leak, and (D) length of stay.
3.3.8 Surgical site infection
Surgical site infection was evaluated in 6 studies (1, 6, 13, 15–17), and the pooled results showed that LLR had lower surgical site infection rate than OLR (OR 0.18, 95% CI 0.07, 0.48, P = 0.0006) (Figure 4B).
3.3.9 Bile leak
Six studies (1, 6, 13, 15–17) compared bile leak rates between the LLR and OLR groups. The combined results showed that LLR effectively reduced the bile leak rate (OR 0.45, 95% CI 0.22, 0.95; heterogeneity: I2 = 14%, P = 0.32) (Figure 4C).
3.3.10 Length of stay
The length of the hospital stay was reported in 8 studies (1, 6, 9, 10, 13–16). According to the results of this meta-analysis, the length of hospital stay was significantly shorter in the LLR group than in the OLR group (MD, -5.20 days; 95% CI, -7.43, -2.97, P < 0.00001) (Figure 4D).
3.4 Sensitivity analysis
Sensitivity analysis showed that no single study affected the overall effect size of the mortality, overall morbidity, operation time, surgical site infection, liver failure, or length of stay. The sensitivity analysis suggested that the total effect size of major complication changed significantly when the study by Heise et al. (15) (OR, 0.67; 95% CI, 0.32, 1.39, P = 0.28; I2 = 0%). The size of the pooled effect of the blood transfusion was influenced by Heise et al. (15) (OR, 0.06; 95% CI, 0.01, 0.33, P = 0.001; I2 = 0%). The size of the pooled effect of the bile leak was influenced by Ishihara et al. (6) (OR, 0.43; 95% CI, 0.18, 1.07, P = 0.07; I2 = 32%) or Heise et al. (15) (OR, 0.72; 95% CI, 0.31, 1.65, P = 0.43; I2 = 0%). The total effect size of the blood loss was influenced by Inoue et al. (16) (MD, -166.48 mL; 95% CI, -375.12, 42.16, P = 0.12), Yu et al. (10) (MD, -493.80 mL; 95% CI, -1090.89, 103.29, P = 0.11) or Uchida et al. (14) (MD, -275.70 mL; 95% CI, -594.37, 42.96, P = 0.09).
4 Discussion
To our knowledge, this is the first meta-analysis to evaluate the short-term outcomes of LLR versus OLR for liver tumors in obese patients. The pooled results of this study showed that, compared with OLR, LLR significantly reduced postoperative morbidity, major complications, surgical site infection and bile leak, intraoperative blood loss, and length of hospital stay. In addition, there were no significant differences between the two groups in postoperative mortality, liver failure, and operation time. These results have important clinical value. Because obesity is a widespread medical condition worldwide, it affects a large percentage of liver resection patients. Our study provides evidence to support the use of LLR in obese patients, and these results may help surgeons to provide a valuable reference when selecting the appropriate surgical approach for obese patients.
Postoperative complications not only prolong the length of hospital stay of patients, increase the cost of patients, but also affect the long-term survival of patients (18, 19). Matsuda et al. (19) found that postoperative complications significantly reduced 5-year overall survival and disease-free survival in patients undergoing liver resection. In obese patients, the increased thickness of the abdominal wall and the large amount of fat in the abdominal cavity add additional technical challenges during open surgery, limiting hand movement and visual range (6, 20). Obesity has been shown to be an important risk factor for increased morbidity after open surgery (6, 9, 21). Previous studies have shown that the total postoperative complications in obese patients undergoing OLR are as high as 41%, which is consistent with the results of our meta-analysis (7). In our included study, the overall complication rate after OLR was 36.2%, while laparoscopic surgery significantly reduced the overall complication rate (24.8%). In addition, our results suggest that laparoscopic surgery also reduces the risk of major complications. This may be due to the fact that in laparoscopic surgery, pneumoperitoneum and high-power microscopy (even deep in caudal view) can provide sufficient free space and a better field of view to perform the procedure. Similarly, several studies (22–24) have observed the benefit of laparoscopic surgery in reducing postoperative complications in obese patients in other abdominal procedures, such as appendectomy and colorectal surgery. In addition, our results showed that postoperative mortality was comparable in the laparoscopic and open surgery groups. Previous evidence suggests that obesity may have long-term metabolic and systemic effects on the body, such as metabolic disorders, increased risk of atrial fibrillation, cardiovascular disease, and overall mortality (25, 26). Therefore, the establishment of individualized perioperative management strategies, such as nutritional counseling to establish a healthy and balanced diet, physical exercise (26), and monitoring obesity-related diseases, may help improve surgical outcomes.
Previous studies have shown that the incidence of surgical site infection in obese patients is significantly higher than that in non-obese patients (6, 15, 22). This may be due to the association between obesity and impaired lymphocyte reactive immunity, inadequate collagen formation, and lack of blood vessels under the adipose tissue (27). Our results suggest that LLR can significantly reduce the incidence of postoperative surgical site infection. This is similar to the results of a meta-analysis by Shabanzadeh et al. (27), which included 8 RCTs and 36 observational studies, showing that laparoscopic surgery significantly reduced the risk of surgical site infection in obese patients undergoing bariatric surgery and non-bariatric surgery (OR = 0.19; 95% CI 0.08-0.45). This may be due to the fact that laparoscopic surgery induces a milder pro-inflammatory response than open surgery and better preserves postoperative immune function (28). In addition, the smaller surgical trauma of laparoscopic surgery may also be the reason for the lower incidence of surgical site infections (27).
Obesity is associated with increased blood loss and prolonged operation time during liver resection (6). Increased intraoperative blood loss may compromise a patient’s surgical outcome (29, 30). Laparoscopic surgery has the following advantages over open surgery and may help reduce intraoperative blood loss. On the one hand, laparoscopic surgery has a high pneumoperitoneum effect, which reduces the impact of obesity and leads to less blood loss than open surgery. On the other hand, compared with open surgery, laparoscopy can provide a clearer field of view, facilitate fine liver dissection, and reduce intraoperative blood loss (17). We also observed the benefit of laparoscopic surgery in reducing intraoperative blood loss, and the operation time was comparable to that of OLR. In addition, our results suggest that the laparoscopic surgery group had a shorter hospital stay than the open surgery group, which may be associated with lower postoperative complications and less intraoperative blood loss. LLR offers benefits such as reduced complications and faster postoperative recovery. However, the experience of the surgeon may affect the outcome of surgery. Complex LLR is technically demanding and requires a skilled surgeon to perform it. Previous studies have shown that the learning curve for LLR ranges from 15 to 60 cases (31). In addition, the gradual implementation of LLR combined with simulation-based training programs may reduce the impact of the learning curve on clinical outcomes (32).
Our study has several advantages. On the one hand, we conducted a comprehensive literature search that included a wide range of evidence, which increased the reliability of our results. On the other hand, the results of the sensitivity analysis confirm the robustness of our main results.
Our meta-analysis has the following limitations. First, the studies we included were all non-RCTs with potential for bias. Second, some outcome measures (such as blood transfusion rates) are based on data from a small number of studies, and more studies are needed to confirm them. Furthermore, liver resection encompasses various techniques, ranging from partial to major liver resection, with differing risks and levels of technical difficulty. Of the studies we included, five included patients who underwent different liver resection techniques, one included only patients who underwent major liver resection, and three did not describe the details of the liver resection. Therefore, whether LLR is superior to OLR in specific liver resection techniques needs further investigation. For outcomes with low heterogeneity, such as postoperative mortality and operation time, LLR demonstrates clear advantages over OLR with a certain degree of reliability. However, high heterogeneity was found in some outcome measures (intraoperation blood loss, operation time and transfusion rates), hindering the accurate estimation of the outcomes, and these results need to be treated with caution. In addition, comorbidities may affect the outcome of the study. Of the studies we included, only five provided information on comorbidities. Due to limited data, we were unable to further assess the specific impact of comorbidities on the results of the study. Future studies need to adequately balance these confounding factors, such as using PSM or randomized controlled designs. Finally, while BMI is the most widely used and simplest measure of obesity, other measures such as visceral fat measurement, waist and hip circumference, and waist-to-hip ratio may be relevant to surgical outcomes, and future studies need to further consider the impact of these measures on study results.
In conclusion, this meta-analysis, based on currently available evidence, our meta-analysis suggests that laparoscopic surgery is superior to open surgery in terms of intraoperation blood loss, postoperation complications, and length of hospital stay in obese patients. In addition, no significant differences were observed in terms of operation time and postoperation mortality. The benefits of laparoscopic surgery may make it a preferred option for obese patients. High-quality RCTs to validate the benefits of LLR are warranted.
Author contributions
JZ: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. CZ: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. RC: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. GT: Conceptualization, Formal analysis, Software, Writing – original draft, Writing – review & editing. RZ: Conceptualization, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was financially supported by National Natural Science Foundation of China (22004088) and Science & Technology Support Project of Sichuan Province (2023YFS0183).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ome Y, Hashida K, Yokota M, Nagahisa Y, Okabe M, Kawamoto K. The safety and efficacy of laparoscopic hepatectomy in obese patients. Asian J Surg. (2019) 42:180–8. doi: 10.1016/j.asjsur.2017.10.002
2. Bell S, Kong JC, Carne PWG, Chin M, Simpson P, Farmer C, et al. Oncological safety of laparoscopic versus open colorectal cancer surgery in obesity: a systematic review and meta-analysis. ANZ J Surg. (2019) 89:1549–55. doi: 10.1111/ans.15081
3. Kwan B, Waters PS, Keogh C, Cavallucci DJ, O’Rourke N, Bryant RD. Body mass index and surgical outcomes in laparoscopic liver resections: a systematic review. ANZ J Surg. (2021) 91:2296–307. doi: 10.1111/ans.16674
4. Guo C, Liu Z, Lin C, Fan H, Zhang X, Wang H, et al. Global epidemiology of early-onset liver cancer attributable to specific aetiologies and risk factors from 2010 to 2019. J Global Health. (2023) 13:4167. doi: 10.7189/jogh.13.04167
5. Sohn W, Lee HW, Lee S, Lim JH, Lee MW, Park CH, et al. Obesity and the risk of primary liver cancer: A systematic review and meta-analysis. Clin Mol Hepatol. (2021) 27:157–74. doi: 10.3350/cmh.2020.0176
6. Ishihara A, Tanaka S, Shinkawa H, Yoshida H, Takemura S, Amano R, et al. Superiority of laparoscopic liver resection to open liver resection in obese individuals with hepatocellular carcinoma: A retrospective study. Ann Gastroenterol Surg. (2022) 6:135–48. doi: 10.1002/ags3.12506
7. Zimmitti G, Sijberden JP, Osei-Bordom D, Russolillo N, Aghayan D, Lanari J, et al. Indications, trends, and perioperation outcomes of minimally invasive and open liver surgery in non-obese and obese patients: An international multicentre propensity score matched retrospective cohort study of 9963 patients. Int J Surg. (2022) 107:106957. doi: 10.1016/j.ijsu.2022.106957
8. Chen ZL, Du QL, Zhu YB, Wang HF. A systematic review and meta-analysis of short-term outcomes comparing the efficacy of robotic versus laparoscopic colorectal surgery in obese patients. J robotic Surg. (2024) 18:167. doi: 10.1007/s11701-024-01934-6
9. Yoon YI, Kim KH, Cho HD, Kang WH, Lee SK, Jung DH, et al. Operation and long-term oncologic outcomes of laparoscopic versus open major liver resection in patients with a high body mass index (> 25 kg/m(2)): a propensity score matching analysis. Surg Endosc. (2022) 36:5772–83. doi: 10.1007/s00464-022-09114-z
10. Yu HB, Dong YD, Wang LC, Tian GJ, Mu SM, Cao Y, et al. Laparoscopic Liver Resection can be an Effective Way in Obese Patients: A Single Center of 2-Year Experience. Surg laparoscopy endoscopy percutaneous techniques. (2016) 26:e69–72. doi: 10.1097/sle.0000000000000268
11. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
12. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
13. Toriguchi K, Hatano E, Sakurai T, Seo S, Taura K, Uemoto S. Laparoscopic liver resection in obese patients. World J Surg. (2015) 39:1210–5. doi: 10.1007/s00268-014-2927-y
14. Uchida H, Iwashita Y, Saga K, Takayama H, Watanabe K, Endo Y, et al. Benefit of laparoscopic liver resection in high body mass index patients. World J Gastroenterol. (2016) 22:3015–22. doi: 10.3748/wjg.v22.i10.3015
15. Heise D, Bednarsch J, Kroh A, Schipper S, Eickhoff R, Coolsen M, et al. Laparoscopic hepatectomy reduces postoperation complications and hospital stay in overweight and obese patients. World J Gastrointest Surg. (2021) 13:19–29. doi: 10.4240/wjgs.v13.i1.19
16. Inoue Y, Ishii M, Fujii K, Nihei K, Suzuki Y, Ota M, et al. Safety and efficacy of laparoscopic liver resection for colorectal liver metastasis with obesity. Am Surg. (2021) 87:919–26. doi: 10.1177/0003134820952448
17. Nakamura M, Ashida R, Ohgi K, Yamada M, Kato Y, Otsuka S, et al. Positive impact of laparoscopic hepatectomy versus open hepatectomy on body size-corrected bleeding in obese patients. Surg Today. (2024). doi: 10.1007/s00595-024-02865-3
18. Cosic L, Ma R, Churilov L, Debono D, Nikfarjam M, Christophi C, et al. The financial impact of postoperation complications following liver resection. Medicine. (2019) 98:e16054. doi: 10.1097/md.0000000000016054
19. Matsuda A, Matsumoto S, Seya T, Matsutani T, Kishi T, Yokoi K, et al. Does postoperation complication have a negative impact on long-term outcomes following hepatic resection for colorectal liver metastasis?: a meta-analysis. Ann Surg Oncol. (2013) 20:2485–92. doi: 10.1245/s10434-013-2972-z
20. Ciarrocchi A, Amicucci G. Laparoscopic versus open appendectomy in obese patients: A meta-analysis of prospective and retrospective studies. J minimal Access Surg. (2014) 10:4–9. doi: 10.4103/0972-9941.124451
21. Wee IJY, Kuo LJ, Ngu JC. The impact of robotic colorectal surgery in obese patients: a systematic review, meta-analysis, and meta-regression. Surg Endosc. (2019) 33:3558–66. doi: 10.1007/s00464-019-07000-9
22. Dasari BVM, Baker J, Markar S, Gardiner K. Laparoscopic appendicectomy in obese is associated with improvements in clinical outcome: systematic review. Int J Surg. (2015) 13:250–6. doi: 10.1016/j.ijsu.2014.11.052
23. Woodham BL, Cox MR, Eslick GD. Evidence to support the use of laparoscopic over open appendicectomy for obese individuals: a meta-analysis. Surg Endosc. (2012) 26:2566–70. doi: 10.1007/s00464-012-2233-4
24. Bizzoca C, Zupo R, Aquilino F, Castellana F, Fiore F, Sardone R, et al. Video-laparoscopic versus open surgery in obese patients with colorectal cancer: A propensity score matching study. Cancers. (2021) 13:1844. doi: 10.3390/cancers13081844
25. Käräjämäki AJ, Korkiakoski A, Hukkanen J, Kesäniemi YA, Ukkola O. Long-term metabolic fate and mortality in obesity without metabolic syndrome. Ann Med. (2022) 54:1432–43. doi: 10.1080/07853890.2022.2075915
26. Valsamakis G, Kyriazi EL, Mouslech Z, Siristatidis C, Mastorakos G. Effect of maternal obesity on pregnancy outcomes and long-term metabolic consequences. Hormones (Athens). (2015) 14:345–57. doi: 10.14310/horm.2002.1590
27. Shabanzadeh DM, Sørensen LT. Laparoscopic surgery compared with open surgery decreases surgical site infection in obese patients: a systematic review and meta-analysis. Ann Surg. (2012) 256:934–45. doi: 10.1097/SLA.0b013e318269a46b
28. Wichmann MW, Hüttl TP, Winter H, Spelsberg F, Angele MK, Heiss MM, et al. Immunological effects of laparoscopic vs open colorectal surgery: a prospective clinical study. Arch Surg. (2005) 140:692–7. doi: 10.1001/archsurg.140.7.692
29. Lv X, Zhang L, Yu H, Yu X. Laparoscopic hepatectomy for hepatocellular carcinoma: short- and long-term outcomes with blood loss. Transl Cancer Res. (2021) 10:4303–15. doi: 10.21037/tcr-21-463
30. Bodur MS, Tomas K, Topaloğlu S, Oğuz Ş, Küçükaslan H, Dohman D, et al. Effects of intraoperation blood loss during liver resection on patients’ outcome: a single- center experience. Turk J Med Sci. (2021) 51:1388–95. doi: 10.3906/sag-2008-78
31. Ghamarnejad O, Sahan LA, Kardassis D, Widyaningsih R, Edwin B, Stavrou GA. Technical aspects and learning curve of complex laparoscopic hepatectomy: how we do it. Surg Endosc. (2024) 38:4583–93. doi: 10.1007/s00464-024-11002-7
Keywords: laparoscopic liver resection, open liver resection, obesity, morbidity, meta-analysis
Citation: Zhang J, Zeng C, Chen R, Tang G and Zhou R (2024) Benefits of laparoscopic liver resection for liver tumors in obese patients: a meta-analysis. Front. Oncol. 14:1489261. doi: 10.3389/fonc.2024.1489261
Received: 31 August 2024; Accepted: 07 October 2024;
Published: 22 October 2024.
Edited by:
Zenichi Morise, Fujita Health University, JapanReviewed by:
Yoshihiro Mise, Juntendo University, JapanHiroyuki Nitta, Iwate Medical University, Japan
Copyright © 2024 Zhang, Zeng, Chen, Tang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rongxing Zhou, cm9uZ3hpbmd6aG91QDEyNi5jb20=; Gang Tang, Z2FuZ3RhbmcyMDE3QDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Jie Zhang†
Jie Zhang† Gang Tang
Gang Tang Rongxing Zhou
Rongxing Zhou