
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 11 December 2024
Sec. Cancer Imaging and Image-directed Interventions
Volume 14 - 2024 | https://doi.org/10.3389/fonc.2024.1484918
Fibroepithelial polyps are rare benign tumors originating from the mesoderm and are more commonly found in the renal pelvis and distal ureter and less frequently in the proximal ureter or bladder. This case report presents a fibroepithelial polyp occurring in the bladder of the fetus, showcasing its two-dimensional ultrasound, three-dimensional ultrasound, color Doppler, and spectral Doppler ultrasound findings, providing a reference for the accurate diagnosis of this condition.
Fibroepithelial polyps (FEPs) are rare benign tumors originating from the mesoderm and are more commonly found in the renal pelvis and distal ureter and less frequently in the proximal ureter or bladder (1). This case report describes a fibroepithelial polyp occurring in the fetal bladder, analyzing its prenatal and postnatal ultrasound findings as well as prognosis.
A 31-year-old pregnant woman, G0P0, presented to our hospital due to the discovery of a fetal bladder mass at an outside facility. A targeted ultrasound examination at our hospital revealed a hypoechoic mass measuring 1.2 × 0.6 × 1.3 cm, located adjacent to the posterior wall of the fetal bladder. The mass had a relatively regular shape and exhibited homogeneous internal echogenicity. Slow flow imaging showed a small amount of blood flow signal at the base of the mass (Figure 1), with a resistive index (RI) of 0.78. Three-dimensional ultrasound showed a thin, stalk-like echo connecting the weak echoic mass to the posterior wall of the bladder (Figure 2), with a relatively smooth bladder wall. MRI examination showed an abnormal signal in the form of a thick strip protruding from the posterior wall of the bladder into the bladder, with an undetermined nature. The patient was followed up with an ultrasound every 2–4 weeks. Prior to delivery at 40 weeks, the examination revealed that the mass had enlarged to 1.2 × 1.0 × 1.4 cm, with uneven internal echoes and an irregular shape. Chromosome examination showed no abnormalities in the fetus. The pregnant woman gave birth to a male baby at 40 weeks of gestation, with a birth weight of 3,030 g. After birth, urination was normal, and regular ultrasound examinations of the urinary system revealed an elongated hypoechoic structure located slightly to the right side of the bladder neck, measuring approximately 0.8 × 0.7 × 1.2 cm. The shape appeared somewhat irregular with relatively clear margins. Within it, a hyperechoic structure of approximately 0.4 cm in diameter was visible, accompanied by posterior acoustic shadowing (Figure 3). No obvious blood flow signals were detected within the mass, and the hypoechoic structure was contiguous with the posterior wall of the bladder. The infant underwent cystoscopy, transurethral bladder tumor resection, and bladder cystostomy at 10 months of age, during which a tumor measuring approximately 1.6 × 1.4 × 1.2 cm in size was found on the posterior wall of the bladder, with a tough texture and a stalk on the surface and was connected to the posterior wall of the bladder, approximately 1 cm away from the opening of the bilateral ureters. Pathological examination showed that the mass was a fibroepithelial polyp (Figure 4).

Figure 1. At 26 weeks of gestation, a hypoechoic mass is observed protruding from the posterior wall of the fetal bladder into the bladder cavity, with slow flow revealing minimal blood flow signals at the base of the mass.
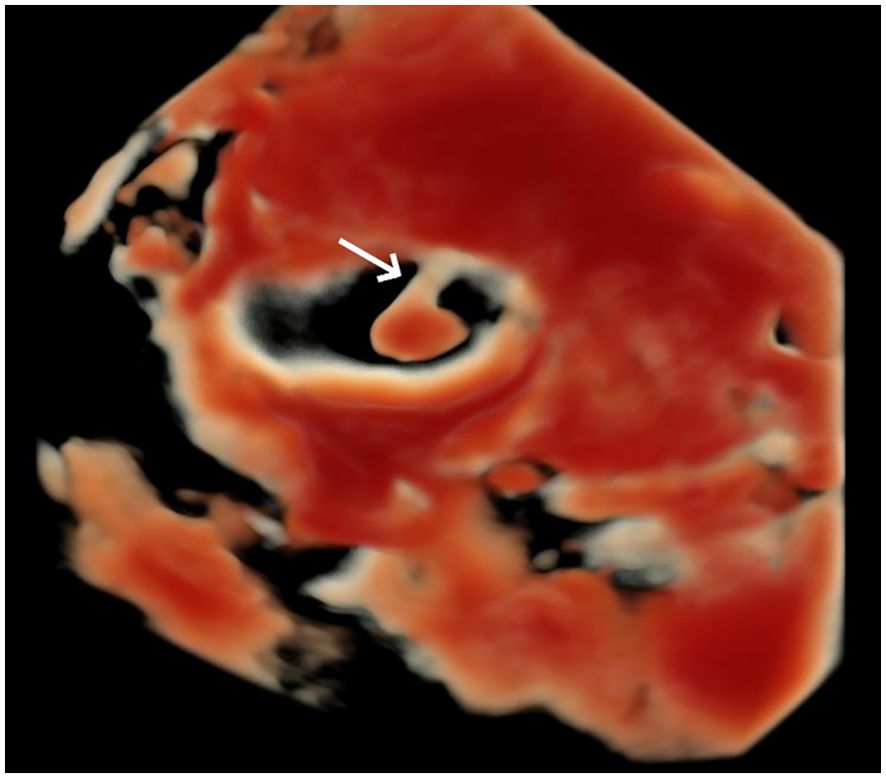
Figure 2. Three-dimensional ultrasound surface imaging in HD-LIVE mode shows the mass with a relatively regular shape, connected to the posterior bladder wall by a stalk-like echo (arrow).
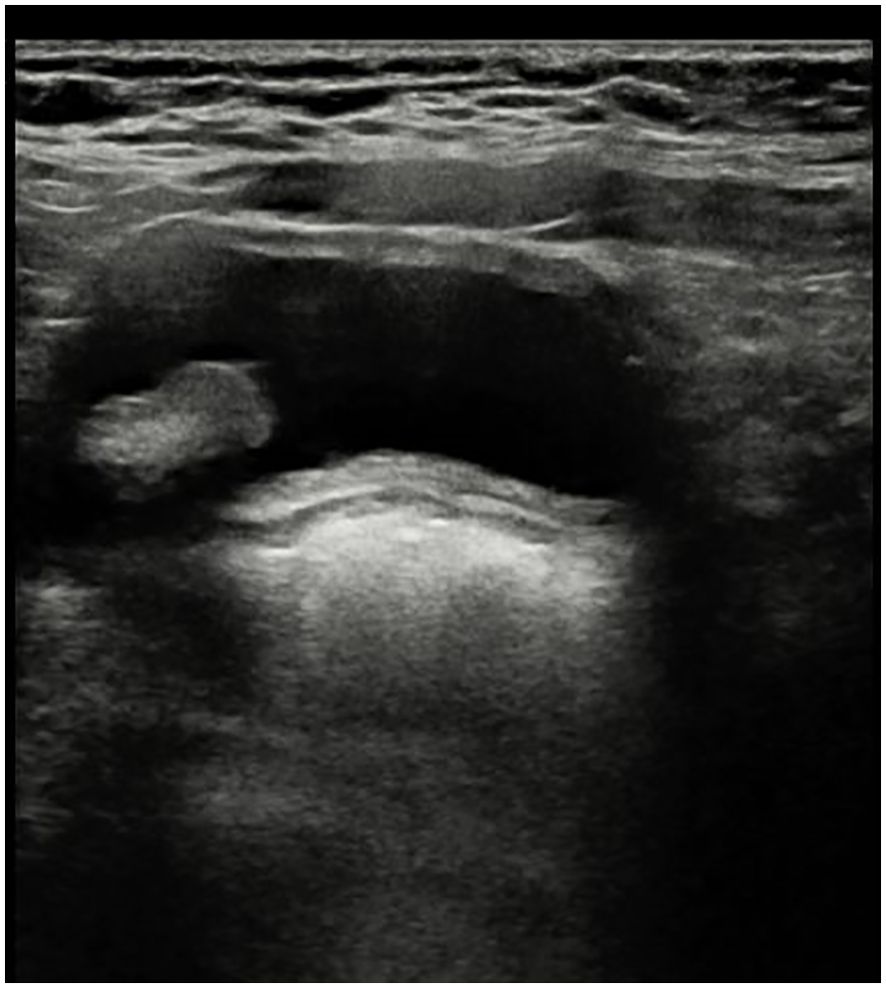
Figure 3. Follow-up examination at 10+ months after birth shows a hypoechoic mass located on the right side of the bladder, elongated in shape with uneven internal echoes and areas of increased echogenicity.
FEPs in the urinary system can occur in any part of the urinary tract, including the renal pelvis, ureters, bladder, and urethra, with the most common occurrence in the posterior urethra. FEPs in the bladder are rare, and they are more prevalent in men than in women (2). The pathogenesis of FEPs in the bladder is not yet clear, but chronic infections, obstruction, trauma, or congenital factors may contribute to their development. Bladder FEPs are usually seen in infants and children, with few reported cases in adults; literature searches reveal no reports from the fetal period. The clinical symptoms associated with bladder FEPs are related to the site and size of the mass, primarily manifesting as hematuria, urinary tract infections, and difficulties in urination (3). Ultrasound has become the preferred diagnostic method for bladder FEPs due to its non-invasive nature, convenience, and high reproducibility. Other diagnostic methods include CT, MRI, cystourethrography, and cystoscopy. The characteristic ultrasound appearance features a solid echo mass connected to the bladder wall through a thin stalk, with clear boundaries, poor internal blood flow, and no signs of invasion into the bladder wall. Differentiation from other malignant tumors in the bladder, such as the most common pediatric rhabdomyosarcoma, is necessary (4). Bladder rhabdomyosarcoma typically occurs in the trigonal area of the bladder, often presenting with infiltrative growth resembling a grape-like mass. It usually lacks a stalk or has a wide-based stalk, with a larger volume and richer blood flow compared to FEPs. There is a certain probability that FEPs in the bladder may undergo squamous metaplasia and further develop into urothelial carcinoma; once detected, surgical removal is recommended. Surgical methods include traditional open surgery or transurethral resection of bladder polyps, the latter of which has the advantages of being less invasive and promoting quicker recovery, making it the preferred approach. The probability of recurrence after removal of FEPs is low, but long-term follow-up observation is still necessary (5, 6).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Medical Ethics Committee of West China Second University Hospital, affiliated with West China Second University Hospital of Sichuan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
XC: Writing – original draft, Writing – review & editing. HL: Funding acquisition, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was partially supported by a grant from the Ministry of Science and Technology of the People’s Republic of China (Project No. 2022YFC2703301).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Keçeli AM, Dönmez Mİ, Kılınç ANU. Fibroepithelial polyp at the bladder neck presenting with gross hematuria in a 5-year-old boy. J Endourology Case Rep. (2020) 6:107–9. doi: 10.1089/cren.2019.0125
2. Rousseau S, Peycelon M, Grosos C, Bidault V, Poupalou A, Martin G, et al. Management of lower urinary tract fibroepithelial polyps in children. J Pediatr Surg. (2021) 56:332–6. doi: 10.1016/j.jpedsurg.2020.05.030
3. Agarwal S, Sharma D, Pandey S, Sankhwar S. Benign fibroepithelial bladder polyp: A rare cause of childhood haematuria. BMJ Case Rep. (2018). doi: 10.1136/bcr-2018-226050
4. Shelmerdine SC, Lorenzo AJ, Gupta AA, Chavhan GB. Pearls and pitfalls in diagnosing pediatric urinary bladder masses. RadioGraphics. (2017) 37:1872–91. doi: 10.1148/rg.2017170031
5. Zhu S, He L, Zheng C, Hou Y. Bladder mulberry-like fibroepithelial polyp with calcification and squamous cell metaplasia mimicking bladder carcinoma: case report and literature review. J Int Med Res. (2020) 48:1–6. doi: 10.1177/0300060519896911
Keywords: fibroepithelial polyp, prenatal diagnosis, ultrasound, benign tumor, fetal bladder
Citation: Chen X and Luo H (2024) Ultrasound findings of fibroepithelial polyp in the fetal bladder: a case report. Front. Oncol. 14:1484918. doi: 10.3389/fonc.2024.1484918
Received: 22 August 2024; Accepted: 25 November 2024;
Published: 11 December 2024.
Edited by:
Hiroo Uchida, Nagoya University Graduate School of Medicine, JapanReviewed by:
Liviu Bilteanu, Carol Davila University of Medicine and Pharmacy, RomaniaCopyright © 2024 Chen and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Luo, bHVvaG9uZ2NkMTk2OUAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.