- 1Department of Thoracic Surgery, The Fourth Hospital of Hebei Medical University (Hebei Tumor Hospital), Shijiazhuang, Hebei, China
- 2Department of Thoracic Surgery, Bao Ding NO.1 Central Hospital, Baoding, Hebei, China
- 3Department of Clinical Laboratory, The Fourth Hospital of Hebei Medical University (Hebei Tumor Hospital), Shijiazhuang, Hebei, China
The debate continues whether the expression of the same rare genetic mutation in multiple primary lung cancers suggests intrapulmonary metastasis or truly multiple primary lung cancers. We report a case of a 54-year-old female patient who presented with multiple nodules in the right lung discovered during a routine examination, persisting for six months. The patient had three central lesions in the right lung’s upper, middle, and lower lobes. She underwent thoracoscopic wedge resection, and the postoperative pathology reported two minimally invasive adenocarcinoma and one adenocarcinoma in situ. Interestingly, genetic testing for lung cancer-related driver genes revealed the presence of the rare RET mutation in all three nodules. This led us to speculate that these nodules might have the exact origin rather than being multiple primaries. To verify this hypothesis, we conducted further testing on these nodules, including whole-exome sequencing (The NGS data was generated from the Illumina sequencing platform by Novogene Co. Ltd, Beijing, China). The results indicated that although all three nodules expressed the RET mutation, there was significant heterogeneity in the gene mutations (differences in the number of cellular mutations, substitution composition levels, and clustering analysis of the three nodules). Thus, the patient was considered to have multiple primary lung cancers. In such cases, whole-exome sequencing can distinguish whether the nodules have the exact origin.
Background
Lung cancer remains the leading cause of cancer-related deaths worldwide (1). With the increasing application of low-dose CT for lung cancer screening, more cases of multiple primary lung cancers (MPLC) are being detected. The traditional diagnostic criteria for distinguishing MPLC from pulmonary metastasis are based on the Martini and Melamed (MM) criteria (2) and the Comprehensive Histologic Assessment (CHA) criteria (3), which mainly rely on histological comparison.
RET gene (proto-oncogene tyrosine-protein kinase receptor RET) is a rare genetic mutation in lung cancer, with only 1-2% incidence (4–6). Most MPLC cases show different mutations in different nodules, but some patients’ nodules exhibit the same mutation, necessitating further evaluation to determine whether they are genuinely MPLC.
Case report
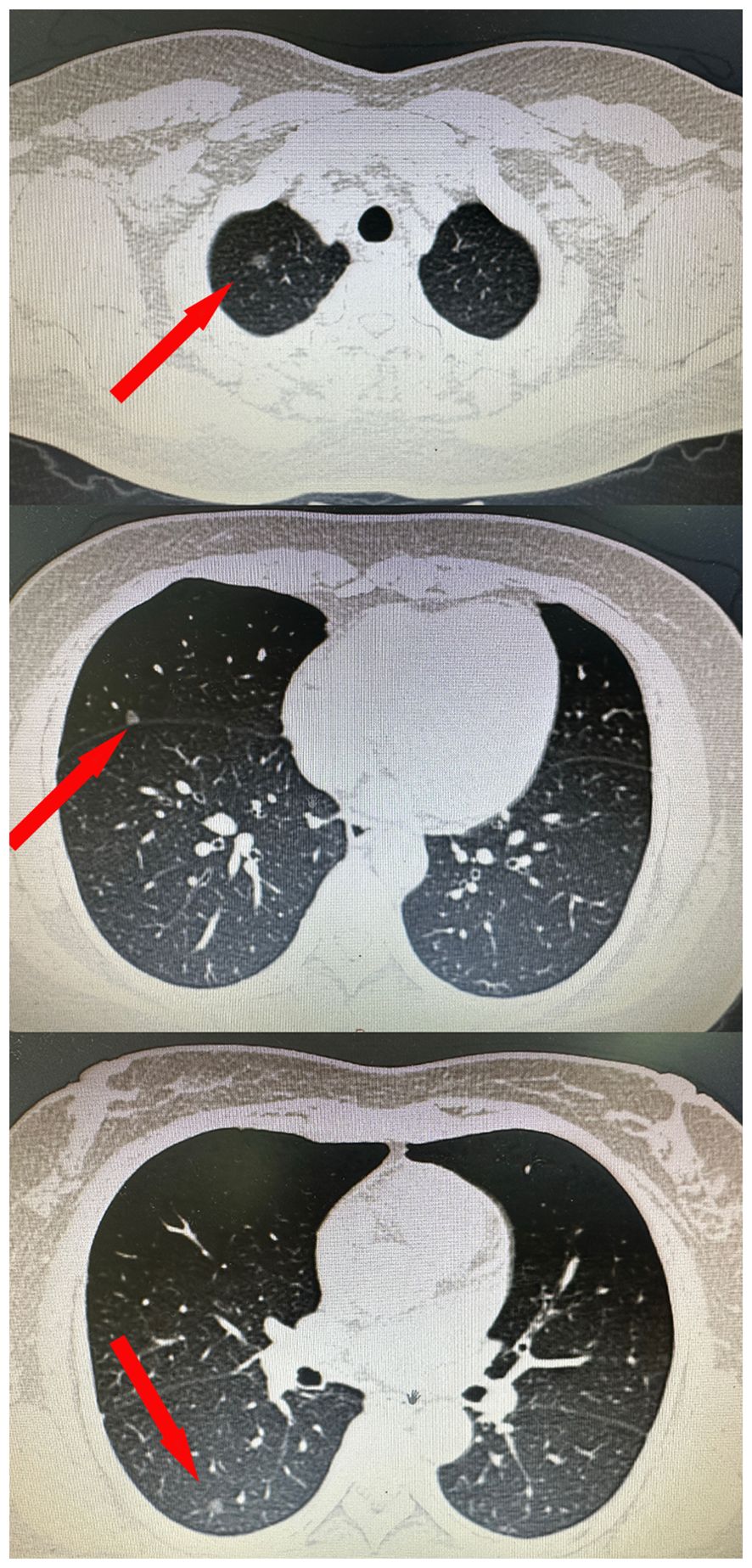
The case involves a 54-year-old female patient who sought medical evaluation due to the existence of multiple pulmonary nodules in her right lung over six months. A computed tomography (CT) scan performed at our institution identified three nodules within her right lung’s upper, middle, and lower lobes (Figure 1). The postoperative pathological report indicated that the upper lobe nodule was carcinoma in situ with a diameter of 0.6cm. The middle and lower lobe nodules were microinvasive adenocarcinomas measuring 0.5cm in diameter. All three nodules were predominantly lepidic, and two microinvasive adenocarcinoma had acinar components. Postoperative genetic examination confirmed RET mutation in all three nodules. Considering that RET mutation is rare in lung cancer cases, we performed whole exon sequencing (7) on these three nodules to differentiate between multiple primary lung cancers and intrapulmonary metastatic cancer. The results demonstrated varying somatic mutations among the three nodules: 257, 242,105, respectively. Among these mutations, nine were shared, while others were independent. In addition, 6 substitution analysis and 96 substitution analysis showed differences in 3 nodules (t test, p<0.05). The mutation characteristics of the sample and 78 known mutation characteristics were cluster analyzed, and the similarity was found to be low. Based on these findings, we conclude that this patient has multiple primary lung cancers.
Discussion
Recent years have seen an increase in lung cancer detection due to low-dose CT screening, with over 60% of cases presenting as ground-glass opacities, and up to 10% of patients having multiple ground-glass nodules (8). Most of these cases are considered MPLC (9, 10), although some studies suggest the possibility of metastasis (11). Next-generation sequencing (NGS) is becoming increasingly important in the molecular typing of lung cancer for treatment decisions. Studies have shown that different ground-glass nodules in the same patient often have different gene mutations, and even when nodules exhibit the same gene mutation, their mutation spectra can differ, suggesting the possibility of MPLC. Yanagitani (12) has reported on a 55-year-old woman with advanced lung adenocarcinoma with metastasis in both lungs who showed multiple metastatic ground glass nodules on CT. In recent years, two additional criteria introduced by the American College of Chest Physicians (ACCP) and the International Association for the Study of Lung Cancer (IASLC) emphasize using histological features, immunohistochemistry (IHC), clinical characteristics, and molecular features to differentiate between multiple primary lung cancers and intrapulmonary metastasis (13, 14).
Studies on multiple nodules being primary cancers or lung metastases are limited. Most research is based on targeted genes (9, 10, 15), with few based on genomics (11). Gene targeting for multiple nodules has not found any evidence of intrapulmonary metastasis. Generally, each nodule’s driver gene mutations are highly distinct (9). Next-generation sequencing (NGS) is the most commonly used targeted sequencing technology, allowing for the simultaneous sequencing of millions of DNA fragments and providing sensitive, economical, and high-throughput detection. Therefore, NGS is gaining more and more attention as an auxiliary means in histopathological diagnosis, especially in lung cancer, where molecular typing contributes to treatment selection (16, 17) Research by Park et al. (18) indicated that, by second-generation sequencing of 16 patients with multiple ground-glass nodules, most patients with multiple ground-glass nodules have different gene mutations in each nodule. However, a few patients have the same gene mutation. However, the mutation spectrum is different, suggesting that even if each nodule shows the same gene mutation, the possibility of multiple primary lung cancers still needs to be considered.
Zhou et al. ‘s (19) study showed that whole exon sequencing could distinguish multiple primary tumors from intrapulmonary metastases, including CNV(Copy Number Variation) analysis, somatic mutation, 6 substitution analysis, 96 substitution analysis and other methods. This study suggests that pulmonary metastasis exists in multiple nodules, but the number of multiple nodules is not related to the probability of pulmonary metastasis. Other genomic profiling studies (20–22) have also reported sizeable genetic heterogeneity among multiple lesions of MPLC. Applying genomic analysis may be crucial for accurately managing patients with multiple nodules.
The RET gene is a proto-oncogene located on the long arm of chromosome 10. It encodes for a tyrosine kinase receptor and is involved in the proliferation, apoptosis, and invasion of tumor cells, affecting the development and progression of tumors (4). The formation of tumors is primarily associated with RET gene fusions, which account for only 1-2% of lung cancers. This report presents a unique case where a patient’s CT scan revealed three ground-glass nodules, considered to be multiple primary lung cancers. Postoperative pathology reported that the nodule in the right upper lobe was a 0.6 cm in situ carcinoma, the nodule in the right middle lobe was a 0.5 cm minimally invasive adenocarcinoma, and the nodule in the right lower lobe was also a 0.5 cm minimally invasive adenocarcinoma. However, postoperatively, genetic testing revealed that all three nodules expressed the RET mutation, an occurrence with an extremely low probability. We conducted whole-exome sequencing to assess further whether the patient’s nodules were intrapulmonary metastases. The results of whole exon sequencing showed (Figure 2) that the number of somatic mutations in the three nodules differed, 257,242,105, respectively, and only 9 were common among the three nodules. In contrast, other mutations were independent of each other. However, the mutations in the single nucleic acid showed that the proportion of mutations in each nodule was different, and the mutation spectrum of different nodules in patients was significantly inconsistent at the level of substitution composition (t-test,p<0.05). The mutation features of the three samples were clustered with 78 known mutation features in the COSMIC website, and the three mutation features were not similar to any of the known 78 features (cosine similarity <0.9), the cosine similarity between the three mutation features being less than 0.9.The similarity is not high. Therefore, we conclude that this patient has multiple primary lung cancers.
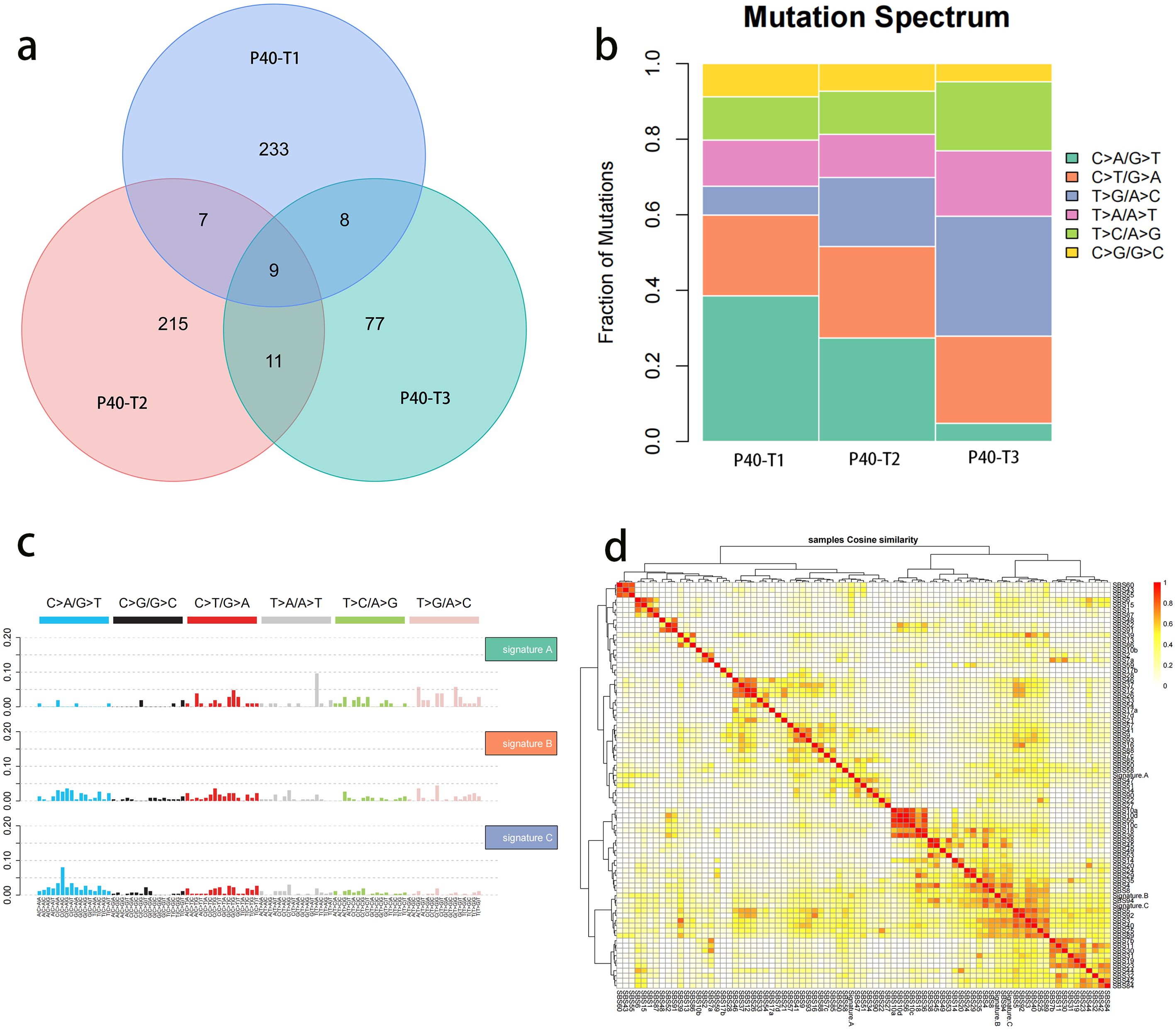
Figure 2. Analysis of total exon results of three nodules. (A) Number of somatic mutations in three nodules. Colored circles represent different nodules, and the intersection is the common mutation of the three nodules. (B) The abscissa in the mutation spectrum histogram is the sample name, the ordinate is the proportion of each mutation type in the sample, and different colors represent different SNV types. (C) Proportion of each mutation feature in different samples. The abscissa represents the sample, and the ordinate represents the proportion of each mutation feature. (D) Cluster analysis of the mutation features of samples and 78 known mutation features. The darker the color is, the closer the cosine value is to 1, signifying that the higher the feature similarity is, the more likely it is the same feature.
This case report indicates that for patients with multiple lung cancers, each nodule exhibits independent genetic characteristics, including in cases of rare mutations. The case presented here involved three nodules, all RET mutations, with an incidence of less than one in a hundred thousand. Through whole-exome sequencing analysis, it was shown that despite the presence of the same mutation in all nodules, genetic heterogeneity still exists among them. Genetic testing cannot be used as a basis to distinguish between multiple primary lung cancers and intrapulmonary metastasis, but further differentiation can be achieved through whole-exome sequencing.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://www.ncbi.nlm.nih.gov/, PRJNA1000732, https://www.ncbi.nlm.nih.gov/, PRJNA1000739.
Ethics statement
The studies involving humans were approved by The Fourth Hospital of Hebei Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from primarily isolated as part of your previous study for which ethical approval was obtained. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YH: Writing – original draft. YG: Conceptualization, Writing – review & editing. QS: Writing – review & editing, Investigation. YL: Formal analysis, Writing – review & editing. SX: Conceptualization, Writing – review & editing. MG: Visualization, Writing – review & editing. QL: Resources, Supervision, Writing – review & editing. GL: Supervision, Resources, Writing – review & editing. SW: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Joint Health Commission of Hebei Province (20201076).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. (2023) 73:17–48. doi: 10.3322/caac.21763
2. Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg. (1975) 70:606–12. doi: 10.1016/S0022-5223(19)40289-4
3. Girard N, Deshpande C, Lau C, Finley D, Rusch V, Pao W, et al. Comprehensive histologic assessment helps to differentiate multiple lung primary nonsmall cell carcinomas from metastases. Am J Surg Pathol. (2009) 33:1752–64. doi: 10.1097/PAS.0b013e3181b8cf03
4. Li AY, McCusker MG, Russo A, Scilla KA, Gittens A, Arensmeyer K, et al. RET fusions in solid tumors. Cancer Treat Rev. (2019) 81:101911. doi: 10.1016/j.ctrv.2019.101911
5. Takeuchi K, Soda M, Togashi Y, Suzuki R, Sakata S, Hatano S, et al. RET, ROS1 and ALK fusions in lung cancer. Nat Med. (2012) 18:378–81. doi: 10.1038/nm.2658
6. Kohno T, Ichikawa H, Totoki Y, Yasuda K, Hiramoto M, Nammo T, et al. KIF5B-RET fusions in lung adenocarcinoma. Nat Med. (2012) 18:375–7. doi: 10.1038/nm.2644
7. Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The sequence alignment/map format and SAMtools. BIOINFORMATICS. (2009) 25:2078–9. doi: 10.1093/bioinformatics/btp352
8. Lee CT. Multifocal ground-glass opacities: multifocal origin versus intrapulmonary metastasis. J Thorac Dis. (2018) 10:1253–5. doi: 10.21037/jtd.2018.03.25
9. Wu C, Zhao C, Yang Y, He Y, Hou L, Li X, et al. High discrepancy of driver mutations in patients with NSCLC and synchronous multiple lung ground-glass nodules. J Thorac Oncol. (2015) 10:778–83. doi: 10.1097/JTO.0000000000000487
10. Liu M, He WX, Song N, Yang Y, Zhang P, Jiang GN. Discrepancy of epidermal growth factor receptor mutation in lung adenocarcinoma presenting as multiple ground-glass opacities. Eur J Cardiothorac Surg. (2016) 50:909–13. doi: 10.1093/ejcts/ezw113
11. Li R, Li X, Xue R, Yang F, Wang S, Li Y, et al. Early metastasis detected in patients with multifocal pulmonary ground-glass opacities (GGOs). Thorax. (2018) 73:290–2. doi: 10.1136/thoraxjnl-2017-210169
12. Yanagitani N, Kaira K, Ishizuka T, Aoki H, Utsugi M, Shimizu Y, et al. Multiple lung metastases presenting as ground-glass opacities in a pulmonary adenocarcinoma: a case report. cases J. (2009) 2:6910. doi: 10.1186/1757-1626-2-6910
13. Kozower BD, Larner JM, Detterbeck FC, Jones DR. Special treatment issues in non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. (2013) 143:e369S–99S. doi: 10.1378/chest.12-2362
14. Detterbeck FC, Franklin WA, Nicholson AG, Girard N, Arenberg DA, Travis WD, et al. The IASLC lung cancer staging project: background data and proposed criteria to distinguish separate primary lung cancers from metastatic foci in patients with two lung tumors in the forthcoming eighth edition of the TNM classification for lung cancer. J Thorac Oncol. (2016) 11:651–65. doi: 10.1016/j.jtho.2016.01.025
15. Chung JH, Choe G, Jheon S, Sung SW, Kim TJ, Lee KW, et al. Epidermal growth factor receptor mutation and pathologic-radiologic correlation between multiple lung nodules with ground-glass opacity differentiates multicentric origin from intrapulmonary spread. J Thorac Oncol. (2009) 4:1490–5. doi: 10.1097/JTO.0b013e3181bc9731
16. Zheng R, Shen Q, Mardekian S, Solomides C, Wang ZX, Evans NR 3rd. Molecular profiling of key driver genes improves staging accuracy in multifocal non-small cell lung cancer. J Thorac Cardiovasc Surg. (2020) 160:e71–9. doi: 10.1016/j.jtcvs.2019.11.126
17. Liu C, Liu C, Zou X, Shao L, Sun Y, Guo Y. Next-generation sequencing facilitates differentiating between multiple primary lung cancer and intrapulmonary metastasis: a case series. Diagn Pathol. (2021) 16:21. doi: 10.1186/s13000-021-01083-6
18. Park E, Ahn S, Kim H, Park SY, Lim J, Kwon HJ, et al. Targeted sequencing analysis of pulmonary adenocarcinoma with multiple synchronous ground-glass/lepidic nodules. J Thorac Oncol. (2018) 13:1776–83. doi: 10.1016/j.jtho.2018.07.097
19. Zhou D, Liu QX, Li MY, et al. Utility of whole exome sequencing analysis in differentiating intrapulmonary metastatic multiple ground-glass nodules (GGNs) from multiple primary GGNs. Int J Clin Oncol. (2022) 27:871–81. doi: 10.1007/s10147-022-02134-8
20. Goodwin D, Rathi V, Conron M, Wright GM. Genomic and clinical significance of multiple primary lung cancers as determined by next-generation sequencing. J Thorac Oncol. (2021) 16:1166–75. doi: 10.1016/j.jtho.2021.03.018
21. Izumi M, Oyanagi J, Sawa K, Fukui M, Ogawa K, Matsumoto Y, et al. Mutational landscape of multiple primary lung cancers and its correlation with non-intrinsic risk factors. Sci Rep. (2021) 11:5680. doi: 10.1038/s41598-021-83609-y
Keywords: multiple primary lung cancer, intrapulmonary metastasis, RET mutation, whole-exome sequencing, histological
Citation: Han Y, Geng Y, Sui Q, Liu Y, Xie S, Gao M, Liu Q, Liu G and Wang S (2024) When multiple primary lung cancers express the same rare mutation: a case report. Front. Oncol. 14:1475193. doi: 10.3389/fonc.2024.1475193
Received: 03 August 2024; Accepted: 21 October 2024;
Published: 13 November 2024.
Edited by:
David Fielding, Royal Brisbane and Women’s Hospital, AustraliaReviewed by:
Gianluca Tedaldi, Scientific Institute of Romagna for the Study and Treatment of Tumors (IRCCS), ItalyTakahiro Nakajima, Dokkyo Medical University, Japan
Copyright © 2024 Han, Geng, Sui, Liu, Xie, Gao, Liu, Liu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shize Wang, NzkxOTM4NTg5QHFxLmNvbQ==
 Yaqing Han
Yaqing Han Yandong Geng2
Yandong Geng2 Shaonan Xie
Shaonan Xie Qingyi Liu
Qingyi Liu Shize Wang
Shize Wang