
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 11 September 2024
Sec. Head and Neck Cancer
Volume 14 - 2024 | https://doi.org/10.3389/fonc.2024.1438269
This article is part of the Research Topic Advanced Head and Neck Cancer: from Organ Preservation Strategies to extended resections and reconstruction View all 8 articles
 Philipp Lampert1*
Philipp Lampert1* Jakob Fenske1
Jakob Fenske1 Jonas Wüster1
Jonas Wüster1 Steffen Koerdt1
Steffen Koerdt1 Kilian Kreutzer1
Kilian Kreutzer1 Philipp Ruf1
Philipp Ruf1 Sara Checa2
Sara Checa2 Max Heiland1
Max Heiland1 Claudius Steffen1†
Claudius Steffen1† Carsten Rendenbach1†
Carsten Rendenbach1†Objective: Miniplates offer superior clinical handling and facilitate postoperative removal after mandibular reconstruction but unfavorable load distribution under high stress has been shown. This study aimed to compare the clinical outcome of patient-specific 3D-printed (PS-3D) titanium miniplate with reconstruction plate fixation in three-segmental LCL-type reconstructions for the first time.
Methods: Patients undergoing three-segmental LCL-type mandibular reconstruction after malignant tumor resection between April 2017 and July 2023 were analyzed in a retrospective single-center study. Inclusion criteria were primary reconstruction using a fibula free flap and PS-3D titanium mini- or reconstruction plate fixation. Complication rates were recorded and analyzed within 6 months after surgery using the N – 1 Chi2- and unequal variance t-test.
Results: 38 patients (10 females, 28 males; mean age 61.4 ± 7.6 years) met the inclusion criteria. In 14 patients (36.8%) miniplates were used in the anterior region. Rates of fixation failure, plate exposure, incomplete osseous union, wound infection, soft tissue, and overall complications did not differ significantly between the two plate systems.
Conclusion: Complication rates did not differ significantly between PS-3D mini- and reconstruction plates in three-segmental LCL-type mandibular reconstructions. Given their advantages in clinical handling and postoperative removal, PS-3D miniplates can be a viable alternative also in larger mandibular reconstructions.
Mandibular segmental resection is the first-line treatment for oral carcinomas infiltrating the mandible (1). To restore chewing function, osseous free flap reconstruction followed by dental implant placement remains the gold standard (2). While superior to other reconstructive methods, post-operative complications remain, most notably osseous non-union, plate exposure and soft tissue complications (3, 4).
A significant risk factor for these complications are large mandibular defects, often requiring multi-segment flaps for reconstruction (5, 6). These extensive reconstructions necessitate a plate system capable of withstanding the increased mechanical stress of fixating multiple segments over a longer distance, while also promoting bone regeneration through beneficial strain (7, 8).
Recently, the use of patient-specific 3D-printed (PS-3D) plates has become increasingly common in mandibular reconstruction due to more predictable plate design and simplified surgical handling (9, 10). Nevertheless, plate-related complication rates have not improved significantly (4). In fact, the increased stiffness of PS-3D reconstruction plates is assumed to cause higher rates of osseous non-union (4, 11).
PS-3D miniplates were introduced by our group in 2022, to address some of the potentially complication-inducing properties of PS-3D reconstruction plates by allowing higher inter-osteotomy movements (IOM) and facilitating removability after surgery (8, 12, 13). Due to the reduced size of miniplates and the use of monocortical screws, plate removal can be performed via an intraoral approach in an outpatient setting with dental implantation in the same surgery resulting in significantly reduced treatment time and cost (12). In single-segment reconstructions, Ruf et al. demonstrated increased beneficial mechanical straining when using PS-3D miniplate fixation in the canine region over PS-3D reconstruction plate fixation (14). However, miniplates exhibited uneven load distribution when used for fixation at the mandibular angle, an area known to be associated with higher stress than the symphysis (15). To overcome this problem, a combined plate system for single-segment mandibular reconstructions using fibula free flaps was proposed: A shortened reconstruction plate at the mandibular angle and a pair of miniplates at the symphysis (16).
To date, this combined plate system has clinically only been evaluated for single- and two-segmental reconstructions where a tendency towards reduced complication rates compared to single PS-3D reconstruction plate fixation was registered (17). However, its behavior in high-stress LCL-type (18) reconstructions has not yet been evaluated clinically or biomechanically and is therefore of great interest.
We hypothesized that a combined PS-3D mini- and reconstruction plate osteosynthesis would not lead to increased complication rates compared to single reconstruction plate fixation in three-segmental LCL-type mandibular reconstructions using fibula free flaps.
This retrospective single-center cohort study was designed at the department of Oral and Maxillofacial Surgery at Charité – Universitätsmedizin Berlin. Patients operated between April 2017 and July 2023 were deemed eligible for study enrollment. Follow-up documentation was analyzed until January 2024. Ethical approval was obtained from the local ethics committee (EA2/138/18).
Inclusion criteria were fixation using a single PS-3D reconstruction plate bridging the entire three-segmental LCL-type defect or two shortened reconstruction plates at the mandibular angle in combination with PS-3D miniplates at the anterior region. Reconstructions involving the mandibular ramus were not included as biomechanical behavior and stress exhibited on the plates was assumed to differ significantly. The minimum follow up period was 6 months after surgery. To establish a homogenous cohort, only patients who received a fibula free flap as primary reconstruction following malignant tumor resection were included, as other common indication such as osteoradionecrosis are associated with poor clinical outcome themselves. We reviewed but excluded patients who suffered a flap loss within the follow-up period.
The computer aided design/computer aided manufacturing (CAD/CAM) workflow of PS-3D plate design has previously been described in detail by our department (12, 17). All plates were manufactured by KLS Martin SE & Co. KG (Tuttlingen, Germany) using a titanium 3D-printing process. Reconstruction plates were designed with a thickness of 2.0 mm and height of 8.0 mm, mini plates with a thickness of 1.0 mm and height of 5.0 mm. Plate length was adjusted individually for each case. Miniplates were fixated with four 2.0 x 7.0 mm monocortical screws per plate, used in pairs at the corpus-symphysis intersegmental gaps and supported by two 6-hole reconstruction plates at the distal intersegmental gaps (Group 1) (Table 1). The reconstruction plates were fixated to the mandibular stumps using 2.0 mm bicortical screws while 7.0 mm monocortical screws were used for fixation of the free flap to protect the vascular pedicle (Group 2) (Table 1). For the first postoperative week, low molecular weight heparin (Fraxiparine 0.3 ml twice a day) was administered. Patients that received radiotherapy were treated according to the current German Cancer Guideline for Oral Cavity Cancer (1). The total dose administered was between approximately 70 Gy.
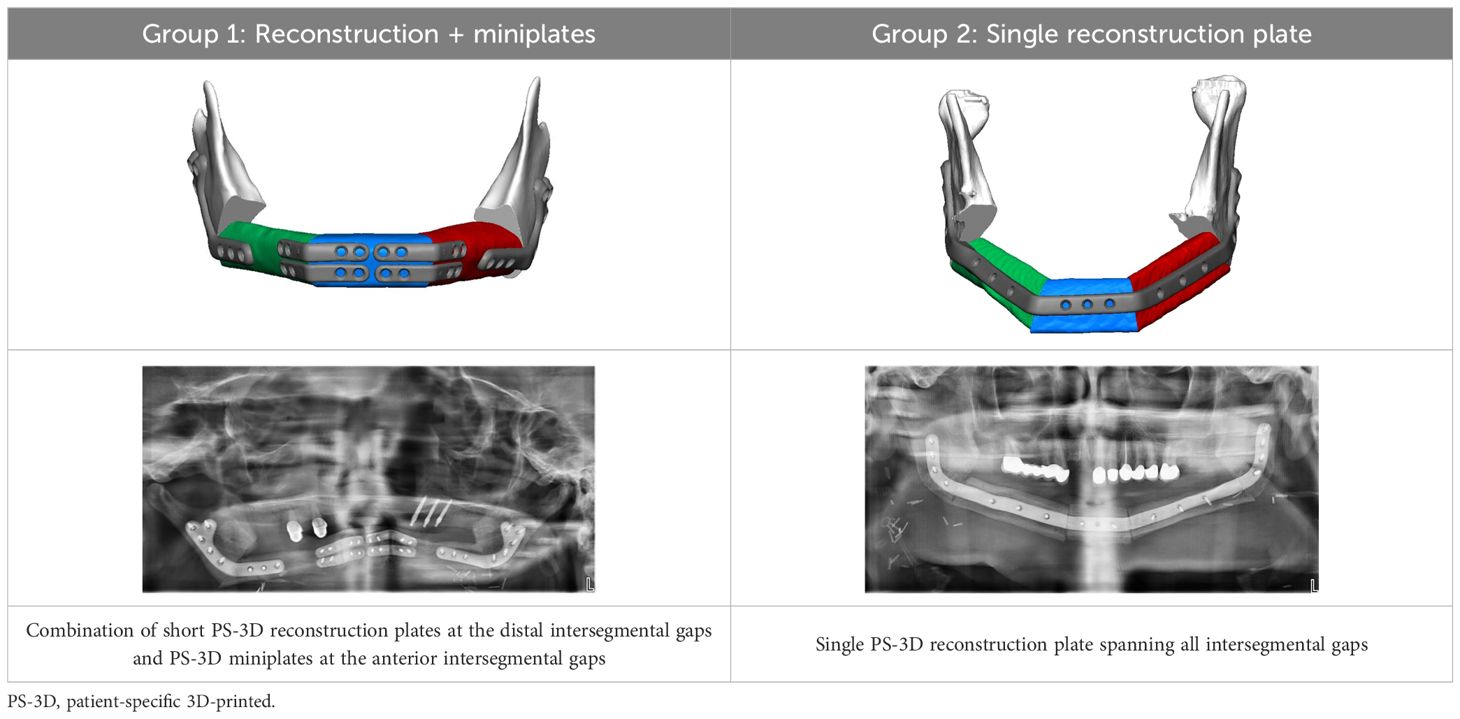
Table 1. 3D planning, clinical execution, and description of the two plate systems compared in this study.
All data was captured and managed using REDCap electronic data capture tools hosted at Charité – Universitätsmedizin Berlin (RRID: SCR_003445) (19, 20). Medical charts of all patients were screened for patient- and disease-related information: age at surgery, sex, body mass index (BMI), nicotine consumption, alcohol abuse, atherosclerosis, adjuvant radio- and chemotherapy. Information about the fixation system and use of an intraoral skin paddle was taken from the surgeon’s report. The follow-up documentation was screened for any of the predefined outcomes within a follow-up period of 6 months (Table 2). Radiographic images were taken 6 months after surgery and analyzed for osseous union.
Data engineering and statistical analysis was performed using the Python Programming Language version 3.11.5 (RRID: SCR_008394) and the Scipy Stats module (21–23). There was no missing data among predictor variables. Records with missing data in outcome variables were excluded in the respective analyses. Numeric variables were tested for normality using the Shapiro-Wilk-Test and analyzed for significant differences between the two plate groups using the unequal variance t-test (24). Nominal variables were tested for significance using the N - 1 Chi2-test as recommended by Campbell (25). Our study’s level of significance was set at p ≤ 0.05. In addition, inclusion of the null value in the 95%-confidence interval (CI) of an odds ratio (OR) was recorded as non-significant, while non-inclusion was recorded as significant.
355 patients were initially identified as eligible for study enrollment. Patients were excluded as per the previously described criteria. Of the remaining 39 patients, 1 (2.6%) patient belonging to the reconstruction plate group suffered a flap loss within the follow-up period. This case was excluded, resulting in a study population of 38 patients (Figure 1).
The baseline characteristics of the study population are shown in (Table 3). All numeric variables were normally distributed. The patient collective was homogenous and differed significantly only in defect length between the two plate groups (p = .038): Patients who received the combined plate system had a mean defect length of 129.6 mm (± 17.3) while the other group had a slightly lower mean defect length of 113.5 mm (± 26.5). An intraoral skin paddle was used slightly less often with the combined plate system (42.9% vs. 66.7%, p = .157) while adjuvant chemotherapy was more common in the reconstruction plate group (50.0% vs. 28.6%, p = .203).
Complication rates did not differ significantly between the two plate groups. One case of fixation failure occurred in the combined plates group due to a loosening of miniplates at the anterior mandibular segment. Imaging data from within the follow-up period was missing for 5 patients, resulting in a reduced number of cases analyzed for osseous union. Plate exposure occurred intraorally only (Table 4).
This study is the first to analyze the postoperative outcome of PS-3D miniplate fixation in three-segmental LCL-type mandibular reconstructions. We chose a combined system of two six-hole PS-3D reconstruction plates at both distal intersegmental gaps with PS-3D miniplates at the anterior gaps based on biomechanical findings by Ruf et al. (Figure 1) (14). This combined plate system had previously shown a tendency towards reduced complication rates in mandibular single- and two-segmental reconstructions and offers superior clinical handling when compared to single PS-3D reconstruction plate fixation (17).
Patient characteristics did not significantly differ between the two plate groups, except for defect length, which was longer in the combined plate group (129.6 ± 17.3 vs. 113.5 ± 29.3 mm, p = .038). While statistically significant, the absolute mean difference of 16.1 mm is relatively small and, if anything, may have slightly disadvantaged the new combined plate system due to the increased defect length.
In our study, the combined plate system was not inferior compared to single reconstruction plate fixation, as complication rates did not differ significantly. While higher fixation failure (7.1% vs. 0.0%, p = .190) and wound infection rates (50.0% vs. 25.0%, p = .122) were observed, this may be related to our study’s limited sample size of 38 patients. It does not imply an inferiority of miniplates as the difference was not significant and may be related to randomness. However, further biomechanical and clinical analyses are recommended.
The present study’s flap loss rate of 2.6% is lower than previously described rates ranging from 4.7% to 9.4%, although our follow-up time of 6 months was shorter than that of some other studies (3, 26). By only including patients who underwent fibula free flap reconstruction following malignant tumor resection, we avoided potential confounders arising from different flap types and surgical indications. This established a homogenous cohort of 38 patients which did not differ significantly between the two plate groups. An intraoral skin paddle was used slightly less often with the combined system (42.9% vs. 66.7%, p = .157). This difference is mainly due to our team’s recent shift in operating technique, favoring the use of muscle tissue over a skin island to avoid a bulky soft tissue mass in the oral cavity. As miniplates were introduced later, a skin paddle was used less often in those surgeries.
Several studies have previously compared conventional mini- and reconstruction plates, recently summarized in a meta-analysis by Sobti et al. (26). Their findings showed plate exposure and fixation failure rates to be significantly higher among conventional miniplates which contrasts with our findings showing no significant differences between PS-3D mini- and reconstruction plates (p = .260 and p = .190). However, their rates of 32.5% for conventional mini- and 18.8% for conventional reconstruction plates were lower than our plate exposure rates of 42.9% and 25.0% for PS-3D mini- and reconstruction plates, respectively. This is in line with prior studies reporting on moderately increased complication rates for PS-3D plates (4, 27). While there was no case of extraoral plate exposure in the present study, the increased rate of intraoral plate exposure among miniplates can be attributed to a less frequent use of skin paddles by our team. In our experience, however, initial plate exposure of CAD/CAM miniplates typically does not lead to additional complications like osseous non-union or wound infection. Furthermore, this study did not compare conventional with PS-3D plates, and differences in complication definition and recording prevent cross-study comparisons.
Ultimately, while complication rates seem to be significantly higher among conventional miniplates compared to conventional reconstruction plates, the same cannot be said for the combined system of PS-3D mini- and reconstruction plates analyzed in this study, as complication rates did not differ significantly compared to the reconstruction plate group. This is particularly beneficial since miniplates by design offer considerable advantages over reconstruction plates in clinical handling. Due to their reduced size, plate removal can be performed via an intraoral approach in an outpatient setting with dental implantation in the same surgery (28). This contrasts with reconstruction plate fixation, where achieving a similar outcome would often require intraoperative plate cutting and hospitalization, resulting in considerably higher costs (17).
The fixation failure rate of 2.6% remains lower than previously reported rates between 7.7% and 12.4% (3, 29). It resulted from one case of plate loosening from the combined plate group, were both miniplate fixations at the anterior mandibular region loosened and were slightly dislocated. Our experience has shown that correct handling of miniplate fixation is highly relevant and can prevent post-operative plate loosening. Cutting guides need to be positioned with great precision and continuous additional rinsing during drilling is essential to prevent heat damage in the drilling holes. We further recommend pre-fixation of all plates at the harvesting side prior to vessel ligation without fully tightening any screw. Only once the 3-segmental fibula free flap can be placed in the desired position between the residual mandibular stumps without putting stress on plates or screws should the three posterior screws be inserted in the mandibular stump on each side and all other screws fixated definitively. Compression with 2 hands from the lateral side during anterior screw fixation is sometimes necessary to avoid rotation and consequently mispositioning of the segments. Only a very thin muscle cuff and periosteum should remain on top of the lateral fibula during flap harvesting to enable sufficient miniplate fixation with mono-cortical screws in a load-sharing manner through frictional loading between the fibula segments and fixation plates.
Bone regeneration is essential to prevent osseous non-union but has been shown to be sensitive to suboptimal mechanical conditions (30, 31). Unfavorable inter-osteotomy movements (IOMs) due to inadequate load distribution may therefore lead to an incomplete osseous union, in turn resulting in chronic overload on the osteosynthesis material. This can potentially lead to fixation failure, especially if patients regain their full bite force. Despite theoretical advantages of PS-3D miniplates in bone regeneration in single-segment reconstructions (14), the present clinical study revealed no difference in osseous non-union rates compared to PS-3D reconstruction plate fixations (64.3% vs. 52.6%, p = .510) in LCL-type reconstructions. While our observed rates are in line with studies by Knitschke et al. for conventional and PS-3D reconstruction plates (27, 29), Kreutzer et al. found a significantly reduced osseous non-union rate for the combined plate system in single- and two-segmental reconstructions (6.7% vs. 46.2%, p = .029) (17). Given that LCL-type reconstructions usually result in postoperative toothlessness and thus permanently reduced bite forces, miniplates would have been assumed to be particularly beneficial in such low-stress scenarios as this has been shown to result in increased beneficial straining in single-segment reconstructions (14). High rates of incomplete osseous union for miniplate fixations, as seen in the present study, are therefore unexpected but may be related to the increased instability of three-segmental LCL reconstructions. Whether a load-bearing reconstruction plate is beneficial due to its rigid fixation remains to be investigated by future biomechanical studies, as such an effect could not be proven in the present clinical study.
Nevertheless, it should not be overlooked that patients requiring LCL-type reconstructions due to malignant tumors are more likely to also receive adjuvant radiotherapy, a known risk factor inhibiting osseous union (27). Furthermore, we screened patients for osseous union 6 months after surgery, limiting comparability to other studies with a longer follow-up period, as Knitschke et al. have shown osseous union rates to improve considerably over time (27). Further biomechanical studies employing bite force analyses are needed to analyze how mechanical strains in LCL-type reconstructions can be improved. Existing biomechanical analyses, focused only on single-segment reconstructions, may not accurately reflect the mechanical stresses present in more extensive defects (32).
Our study is associated with some limitations that should be mentioned. While our focus on a homogenous cohort strengthens the internal validity of our findings, it comes at the cost of excluding other relevant surgical indications such as osteoradionecrosis and flaps other than fibula free flaps. Additionally, three-segmental LC-type reconstructions and those including the mandibular ramus were excluded from the present study, as these reconstructions are assumed to differ substantially from the studied LCL-type reconstructions regarding the mechanical stress exhibited on plate system and transplant. We chose a follow-up time of 6 months as most complications tend to occur within this time frame and relatively few patients had to be excluded due to an incomplete follow-up. However, long-term complications occurring later than 6 months post-surgery were not captured and should be evaluated in future studies. Ultimately, our study’s retrospective design comes with inherent limitations, only allowing limited generalization of the results.
Our study found no significant differences in complication rates between PS-3D mini- and reconstruction plates. Given the established benefit of easier postsurgical miniplate removal in the anterior mandibular region, clinical superiority over single PS-3D reconstruction plate fixation can be inferred. Further research is needed to understand load distribution and failure mechanisms specifically in multi-segment mandibular reconstructions, as biomechanical conditions may differ considerably from single-segment reconstructions. Perioperative functional analyses can thereby help identify strategies to improve osseous healing in large mandibular reconstructions.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the ethics committee of Charité - Universitätsmedizin Berlin. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
PL: Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. JF: Investigation, Writing – review & editing. JW: Writing – review & editing, Resources. SK: Resources, Writing – review & editing. KK: Writing – review & editing, Resources. PR: Validation, Writing – review & editing. SC: Writing – review & editing, Validation. MH: Funding acquisition, Project administration, Resources, Supervision, Validation, Writing – review & editing. CS: Conceptualization, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing. CR: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Validation, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the German Research Foundation (DFG, RE 4803/1-1).
MH and KK received speaker remuneration and research funding for other projects by KLS Martin SE & Co. KG. CR served as a consultant and received research funding for other projects by KLS Martin SE & Co. KG.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. German Cancer Society, German Cancer Aid, AWMF. German Guideline Program in Oncology: Oral Cavity Cancer. AWMF (2021). Available at: https://www.leitlinienprogrammonkologie.de/leitlinien/mundhoehlenkarzinom/.
2. Molteni G, Gazzini L, Sacchetto A, Nocini R, Comini LV, Arietti V, et al. Mandibular reconstruction in head and neck cancer: which is the gold standard? Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-Laryngol Soc EUFOS Affil Ger Soc Oto-Rhino-Laryngol - Head Neck Surg. (2023) 280:3953–65. doi: 10.1007/s00405-023-08050-5
3. Ritschl LM, Mücke T, Hart D, Unterhuber T, Kehl V, Wolff K-D, et al. Retrospective analysis of complications in 190 mandibular resections and simultaneous reconstructions with free fibula flap, iliac crest flap or reconstruction plate: a comparative single centre study. Clin Oral Investig. (2021) 25:2905–14. doi: 10.1007/s00784-020-03607-8
4. Rendenbach C, Steffen C, Hanken H, Schluermann K, Henningsen A, Beck-Broichsitter B, et al. Complication rates and clinical outcomes of osseous free flaps: a retrospective comparison of CAD/CAM versus conventional fixation in 128 patients. Int J Oral Maxillofac Surg. (2019) 48:1156–62. doi: 10.1016/j.ijom.2019.01.029
5. Bede SYH, Ismael WK, Hashim EA. Reconstruction plate-related complications in mandibular continuity defects. Oral Maxillofac Surg. (2019) 23:193–9. doi: 10.1007/s10006-019-00762-5
6. Sadr-Eshkevari P, Rashad A, Vahdati SA, Garajei A, Bohluli B, Maurer P. Alloplastic mandibular reconstruction: a systematic review and meta-analysis of the current century case series. Plast Reconstr Surg. (2013) 132:413e–27e. doi: 10.1097/PRS.0b013e31829ad0d9
7. Nanavati N, Walker M. Current concepts to reduce mechanical stiffness in locked plating systems: a review article. Orthop Res Rev. (2014) 6:91–5. doi: 10.2147/ORR.S66014
8. Claes LE, Heigele CA. Magnitudes of local stress and strain along bony surfaces predict the course and type of fracture healing. J Biomech. (1999) 32:255–66. doi: 10.1016/s0021-9290(98)00153-5
9. Pabst A, Zeller A-N, Raguse JD, Hoffmann J, Goetze E. Microvascular reconstructions in oral and maxillofacial surgery - Results of a survey among oral and maxillofacial surgeons in Germany, Austria, and Switzerland. J Cranio-Maxillo-fac Surg Off Publ Eur Assoc Cranio-Maxillo-fac Surg. (2023) 51:71–8. doi: 10.1016/j.jcms.2023.02.003
10. Kraeima J, Glas HH, Merema BBJ, Vissink A, Spijkervet FKL, Witjes MJH. Three-dimensional virtual surgical planning in the oncologic treatment of the mandible. Oral Dis. (2021) 27:14–20. doi: 10.1111/odi.13631
11. Rendenbach C, Hölterhoff N, Hischke S, Kreutzer K, Smeets R, Assaf AT, et al. Free flap surgery in Europe: an interdisciplinary survey. Int J Oral Maxillofac Surg. (2018) 47:676–82. doi: 10.1016/j.ijom.2017.11.013
12. Kreutzer K, Steffen C, Koerdt S, Doll C, Ebker T, Nahles S, et al. Patient-specific 3D-printed miniplates for free flap fixation at the mandible: A feasibility study. Front Surg. (2022) 9:778371. doi: 10.3389/fsurg.2022.778371
13. Steffen C, Sellenschloh K, Willsch M, Soares AP, Morlock MM, Heiland M, et al. Patient-specific miniplates versus patient-specific reconstruction plate: A biomechanical comparison with 3D-printed plates in mandibular reconstruction. J Mech Behav BioMed Mater. (2023) 140:105742. doi: 10.1016/j.jmbbm.2023.105742
14. Ruf P, Orassi V, Fischer H, Steffen C, Duda GN, Heiland M, et al. Towards mechanobiologically optimized mandible reconstruction: CAD/CAM miniplates vs. reconstruction plates for fibula free flap fixation: A finite element study. Front Bioeng Biotechnol. (2022) 10:1005022. doi: 10.3389/fbioe.2022.1005022
15. Orassi V, Duda GN, Heiland M, Fischer H, Rendenbach C, Checa S. Biomechanical assessment of the validity of sheep as a preclinical model for testing mandibular fracture fixation devices. Front Bioeng Biotechnol. (2021) 9:672176. doi: 10.3389/fbioe.2021.672176
16. Ruf P, Orassi V, Fischer H, Steffen C, Kreutzer K, Duda GN, et al. Biomechanical evaluation of CAD/CAM magnesium miniplates as a fixation strategy for the treatment of segmental mandibular reconstruction with a fibula free flap. Comput Biol Med. (2024) 168:107817. doi: 10.1016/j.compbiomed.2023.107817
17. Kreutzer K, Lampert P, Doll C, Voss JO, Koerdt S, Heiland M, et al. Patient-specific 3D-printed mini-versus reconstruction plates for free flap fixation at the mandible: Retrospective study of clinical outcomes and complication rates. J Cranio-Maxillo-fac Surg Off Publ Eur Assoc Cranio-Maxillo-fac Surg. (2023) 51:621–8. doi: 10.1016/j.jcms.2023.09.019
18. Boyd JB, Gullane PJ, Rotstein LE, Brown DH, Irish JC. Classification of mandibular defects. Plast Reconstr Surg. (1993) 92:1266–75.
19. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J BioMed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
20. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J BioMed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
21. Harris CR, Millman KJ, van der Walt SJ, Gommers R, Virtanen P, Cournapeau D, et al. Array programming with numPy. Nature. (2020) 585:357–62. doi: 10.1038/s41586-020-2649-2
22. McKinney W. (2010). Data structures for statistical computing in python, in: Proceedings of the 9th Python in Science Conference, pp. 56–61. doi: 10.25080/Majora-92bf1922-00a
23. Virtanen P, Gommers R, Oliphant TE, Haberland M, Reddy T, Cournapeau D, et al. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat Methods. (2020) 17:261–72. doi: 10.1038/s41592-019-0686-2
24. Ruxton GD. The unequal variance t-test is an underused alternative to Student’s t-test and the Mann–Whitney U test. Behav Ecol. (2006) 17:688–90. doi: 10.1093/beheco/ark016
25. Campbell I. Chi-squared and Fisher-Irwin tests of two-by-two tables with small sample recommendations. Stat Med. (2007) 26:3661–75. doi: 10.1002/sim.2832
26. Sobti N, Ahmed KS, Polanco T, Chilov M, Cohen MA, Boyle J, et al. Mini-plate versus reconstruction bar fixation for oncologic mandibular reconstruction with free fibula flaps: A systematic review and meta-analysis. J Plast Reconstr Aesthetic Surg JPRAS. (2022) 75:2691–701. doi: 10.1016/j.bjps.2022.04.097
27. Knitschke M, Yonan M, Roller FC, Pons-Kühnemann J, Attia S, Howaldt H-P, et al. Osseous Union after Jaw Reconstruction with Fibula-Free Flap: Conventional vs. CAD/CAM Patient-Specific Implants. Cancers. (2022) 14:5774. doi: 10.3390/cancers14235774
28. Mc Goodson A, Thomas C, Maxwell L, Brennan PA, Williams EM. The 3D-printed miniplate-jig system: a new, rapid, precise, and user-friendly approach to miniplate fixation of free-tissue mandibular reconstructions. Br J Oral Maxillofac Surg. (2022) 60:1114–7. doi: 10.1016/j.bjoms.2022.05.006
29. Knitschke M, Sonnabend S, Roller FC, Pons-Kühnemann J, Schmermund D, Attia S, et al. Osseous Union after Mandible Reconstruction with Fibula Free Flap Using Manually Bent Plates vs. Patient-Specific Implants: A Retrospective Analysis of 89 Patients. Curr Oncol Tor Ont. (2022) 29:3375–92. doi: 10.3390/curroncol29050274
30. Claes L. Mechanobiologie der frakturheilung. Unfallchirurg. (2017) 120:13–3. doi: 10.1007/s00113-016-0284-z
31. Steffen C, Fischer H, Sauerbrey M, Heintzelmann T, Voss JO, Koerdt S, et al. Increased rate of pseudarthrosis in the anterior intersegmental gap after mandibular reconstruction with fibula free flaps: a volumetric analysis. Dento Maxillo Facial Radiol. (2022) 51:20220131. doi: 10.1259/dmfr.20220131
Keywords: mandibular reconstruction, patient-specific, 3D-printing, titanium plate, miniplate, fibula flap, pseudarthrosis, CAD/CAM
Citation: Lampert P, Fenske J, Wüster J, Koerdt S, Kreutzer K, Ruf P, Checa S, Heiland M, Steffen C and Rendenbach C (2024) Comparative study of CAD/CAM reconstruction and miniplates for patient-specific fixation in LCL-type mandibular reconstruction. Front. Oncol. 14:1438269. doi: 10.3389/fonc.2024.1438269
Received: 25 May 2024; Accepted: 05 August 2024;
Published: 11 September 2024.
Edited by:
Filippo Marchi, San Martino Hospital (IRCCS), ItalyReviewed by:
Nidal A. L. Deek, Linkou Chang Gung Memorial Hospital, TaiwanCopyright © 2024 Lampert, Fenske, Wüster, Koerdt, Kreutzer, Ruf, Checa, Heiland, Steffen and Rendenbach. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Philipp Lampert, cGhpbGlwcC5sYW1wZXJ0QGNoYXJpdGUuZGU=
†These authors have contributed equally to this work and share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.