- 1Department of Public Health, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia
- 2Department of Health Promotion and Behavioral Science, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 3Department of Health Systems and Policy, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Adult Health Nursing, School of Health Sciences, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 5Department of Health Promotion and Health Behaviour, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 6Department of Emergency and Critical Care Nursing, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 7Amref Health Africa, West Gondar Zonal Health Department, SLL Project, Gondar, Ethiopia
- 8Department of Health Promotion, School of Public Health, College of Medicine Health Sciences, Wollo University, Dessie, Ethiopia
Introduction: Cervical cancer is a prevalent cancer among women in low and middle-income countries, but it can be largely prevented through screening programs and HPV vaccination. This study aimed to determine the level of knowledge, attitudes, and practices regarding cervical cancer screening among healthcare providers in Sub-Saharan African countries.
Methods: Systematic review and meta-analysis were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines. Relevant databases including PubMed, Cochrane Library, AJOL, Google Scholar, and ScienceDirect databases were used to retrieve and search articles. The study included published and unpublished research written in English between January 2013 and May 16, 2024 for studies reporting knowledge, attitude, and practice towards cervical cancer screening among healthcare providers in Sub-Saharan Africa. This review has been registered on PROSPERO. The heterogeneity of the data was evaluated using the I2 statistic. A meta-analysis was conducted using STATA 17 software, with a 95% confidence interval. The researchers also conducted publication bias and sensitivity analysis.
Results: The review included 30 studies involving 7542 healthcare providers. The pooled magnitude of good knowledge status towards cervical cancer was 67.93% (95% CI: 53.36–82.50) whereas the pooled magnitude of positive attitude towards cervical cancer was 55.26% (95% CI: 34.28– 76.23). The results also showed that about 49.68% (95% CI: 33.18–66.17) of healthcare providers had good knowledge status about cervical cancer screening, 66.63%(95% CI: 50.36– 82.89) had a positive attitude towards it, and only 17.23% (95% CI; 6.08-28.37) had ever screened for cervical cancer.
Conclusion: The overall magnitude of knowledge and attitude of healthcare providers in Sub-Saharan Africa towards cervical cancer and its screening was suboptimal. Furthermore, a low percentage of female healthcare providers in the region had undergone screening for cervical cancer. As a result, policymakers and program administrators should focus on improving the knowledge, attitude, and practices of healthcare providers to meet the global health goal of cervical cancer screening and effectively eliminating cervical cancer. Healthcare providers must serve as role models for other women who should also undergo screening.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42023495241.
Introduction
Cervical cancer is the fourth most prevalent cancer among women on a global scale, comprising approximately 604,000 new cases and leading to 342,000 deaths worldwide (1). The majority of deaths from cervical cancer occur in underdeveloped or developing countries, accounting for about 85% of the total. In low-income and middle-income countries, the death rate from cervical cancer is 18 times higher compared to wealthier countries (2). The number of new cases and deaths from cervical cancer in sub-Saharan Africa is expected to increase over the next 20 years starting from 2013 (3). In comparison, Northern Africa has made significant progress in reducing the occurrence and death rate of cervical cancer, making it the region with the lowest rates in Africa (4).
The risk factors for cervical cancer consist of human papillomavirus infection (HPV), having multiple sexual partners, starting sexual activity at a young age, giving birth to multiple children, having a low socioeconomic status, and smoking tobacco (5–7). Around 70% of cervical cancer cases can be attributed to HPV types 16 and 18 (8). HPV disrupts the normal activity of cells, causing noticeable alterations in the epithelial cells located in the transformation zone of the cervix (9). It is the most common sexually transmitted infection globally. It is most frequently found in teenage and young adult women, which aligns with the timing of their first sexual experiences (10).
This cancerous disease takes a long time to develop into malignant tumors, with the presence of precancerous lesions indicating the ongoing infection (11). It takes between 10 to 15 years for cervical cancer to develop (12). Cervical cancer is a fatal illness when it becomes invasive, but it can be prevented through effective screening programs by identifying and treating premalignant lesions (13). Although vaccines can provide significant protection against HPV for women who have never been exposed to the virus, such as young girls and teenagers, those who have previously been vaccinated will still need to undergo cervical cancer screening later in life to protect against other strains of HPV not included in the vaccines (14). There are several methods for cervical screening, including Pap smear test, HPV DNA test, visual inspection with acetic acid (VIA), or visual inspection with Lugol’s iodine (VILI) (15–19). Properly identifying precancerous lesions and HPV infection through cervical cancer screening methods could significantly decrease cervical cancer deaths (20).
The World Health Assembly has adopted the Global Strategy for eliminating cervical cancer, aiming to achieve it by 2030. This strategy includes three global targets known as 90-70-90, which aim to have 90% of girls vaccinated against HPV by the age of 15, screen 70% of women aged 35-45, and provide treatment to 90% of women diagnosed with cervical disease (21). This strategy aims to eradicate cervical cancer as a major public health issue worldwide, with a goal of reducing the incidence rate to below 4 cases per 100,000 women per year. A global plan to eliminate cervical cancer by 2030 in low- and lower-middle-income countries is projected to reduce the incidence rate by 42% by 2045 and 97% by 2120, preventing over 74 million new cases. Additionally, it is estimated that 300,000 cervical cancer deaths will be prevented by 2030, with over 62 million deaths averted by 2120 (21). The World Health Organization recommends that women in the general population begin cervical cancer screening at age 30. However, women with HIV should be screened more often (every 3 to 5 years) due to their significantly higher risk of developing cervical cancer. For women who receive negative results on VIA or cytology tests, it is recommended to undergo regular screening every three to five years. In women who test negative on an HPV test, rescreening should be done after a minimum interval of five years (22). Healthcare providers are vital in educating people about the risk factors and prevention of cervical cancer, raising awareness to implement effective screening programs and decrease the number of cases. They are influential in encouraging individuals to seek care and have the expertise to educate them on the disease, its causes, risk factors, and screening options, ultimately impacting their screening behavior (23).
Globally, a substantial 40.0% of women were not aware that HPV is responsible for over 95 percent of cervical cancer cases. Among those uninformed about the HPV-cervical cancer link, a notable 39.1% had refrained from undergoing cervical cancer screening, surpassing the global average of 31.2% (1). Furthermore, 31.2% of individuals worldwide have never undergone cervical cancer screening. A large percentage (39.1%) of women who are unaware of the link between HPV and cervical cancer have never been screened for the disease, which is higher than the worldwide average (1). Specifically, Saudi Arabia (55.8%) and Serbia (36.5%) have the highest percentages of women who have never undergone cervical cancer screening. This discrepancy highlights an awareness gap that influences cervical cancer screening rates (1).
However, not all women undergo cervical cancer screening, with the highest risk being among those who have never been screened for cervical cancer till their diagnosis. Additionally, women without health insurance and recent immigrants are less likely to receive cervical cancer screening (24, 25). The rate at which individuals participate in cervical cancer screening can differ based on their understanding of the disease and screening options, as well as other factors like personal opinions, beliefs, attitudes, cultural influences, and the attitude of their partner (26). Previous studies in sub-Saharan Africa have shown that women face numerous obstacles in accessing cervical cancer screening services, including delayed diagnosis, weak health systems, limited funding, lack of information, high costs, societal and cultural beliefs, low awareness, and lack of clear government policies (27–29).
Around 90% of health workers in Turkey had positive attitudes toward cancer screening tests whereas practice-level screening methods were low, with only 4.2% performing pap smears (30). About 74.6% of women in South India had heard about cervical cancer whereas 76.9% knew about screening methods (31). More than half of the women (62.5%) have a positive attitude towards screening. More than three-fourths of women (349; 86.6%) do not have practice toward cervical cancer screening (31). A recent study conducted in Libya found that healthcare providers in health facilities were not adequately informing women about cervical cancer screening (32).
Although there were several studies conducted regarding knowledge, attitudes, and practice level towards cervical cancer screening among healthcare providers in Sub-Saharan Africa, there is a lack of consistent evidence regarding these healthcare providers’ knowledge, attitudes, and practices. The magnitude of good knowledge, positive attitudes, and ever been practices regarding cervical cancer screening among healthcare providers in Sub-Saharan Africa varies significantly, with rates ranging from as low as 4.89% (33) to as high as 97.4% (34) for knowledge, 30.7% (35) to 97.4% (34) for attitudes, and 8.7% (35) to 72.6% (36) ever screened for cervical cancer. Thus, this review aimed to assess knowledge, attitudes, and practices related to cervical cancer screening among healthcare providers in Sub-Saharan Africa. It is crucial to regularly evaluate and address any gaps in their knowledge as having sufficient knowledge is vital for fostering positive attitudes and effective practices. Healthcare professionals are seen as examples to others and have the responsibility to educate the communities they work with about cervical cancer (37). The results of this study will be utilized by policymakers and program planners to enhance and assess cervical cancer screening services and strategies. The study also will provide baseline information for the future.
Materials and methods
Information sources and search strategy
Relevant databases include PubMed, Cochrane Library, AJOL, Google Scholar, and Science Direct. We searched articles from January 2013 and May 16, 2024, that were published in peer-reviewed journals or filed as completed dissertations with observational study design. We used a search strategy by combining the following key terms: knowledge, attitude, practice, cervical cancer, uterine cervical neoplasms, cervical cancer screening, health care provider, health professional, health personnel, health care workers, and Sub-Saharan Africa. We used both free texts, OR, AND, Boolean, and Medical subject heading [MeSH]terms in our search. Also, Gray literature of observational studies and official websites of international and local organizations and universities were searched. The study protocol was registered on PROSPERO, with the registration number CRD42023495241.
Study inclusion and exclusion criteria
This study included English-language research articles and doctoral dissertations conducted in Sub-Saharan Africa between January 2013 and May 16, 2024. The focus was on cross-sectional studies that examined the knowledge, attitude, and practice of healthcare providers toward cervical cancer screening. Only studies published in peer-reviewed journals or completed dissertations were considered. Our review included studies which assessed the knowledge, attitudes, and practices of various healthcare providers in sub-Saharan Africa towards cervical cancer screening, including physicians, nurses, midwives, anesthetists, pharmacy professionals, optometry professionals, laboratory professionals, dentistry professionals, public health officers, and health extension workers. Studies that did not assess the knowledge, attitude, and practice of health care providers towards cervical cancer screening, as well as those conducted outside of Sub-Saharan Africa or not involving health professionals, were excluded. This study excluded case reports, case series, earlier reviews, and qualitative studies on cervical cancer screening uptake. Moreover, articles that were not fully accessible were excluded after attempting to contact the authors via email at least twice.
Data extraction and data quality assessment
After searching in relevant databases, the study was imported into Endnote version 20.6 and duplicates were removed. Then, three reviewers (AMD, EKB, and TFA) assessed the title and abstract to determine the eligibility of the article for full-text review. The full texts of the remaining papers were downloaded for further analysis, and full-text reviews were conducted. Finally, after applying inclusion and exclusion criteria, eligible studies were exported to Microsoft Excel version 2019 using a standardized data extraction checklist. Data were extracted using a standardized data extraction spreadsheet format prepared in Microsoft Excel. The data abstraction format includes the author/s name, year of publication, study area, study design, sample size, prevalence of knowledge, prevalence of attitude, and prevalence of cervical cancer practice.
The data quality was assessed using Joanna Briggs Institute’s (JBI’s) critical appraisal checklist for those included studies. Three authors (ETF, DE, and MGT) independently assessed the quality of each article. Whenever necessary, another reviewer (AAT) was involved and any discrepancy was resolved through discussion and consensus. In conclusion, studies that scored 6 or higher out of 9 were classified as being of high quality (38). The studies included in the analysis had quality scores ranging from 6 to 9. Besides, studies that had methodological flaws, incomplete reporting of results; or those for which full text was not available were excluded from the final analysis. Study researchers made two separate attempts to contact article authors whenever additional study information was needed (Table 1).
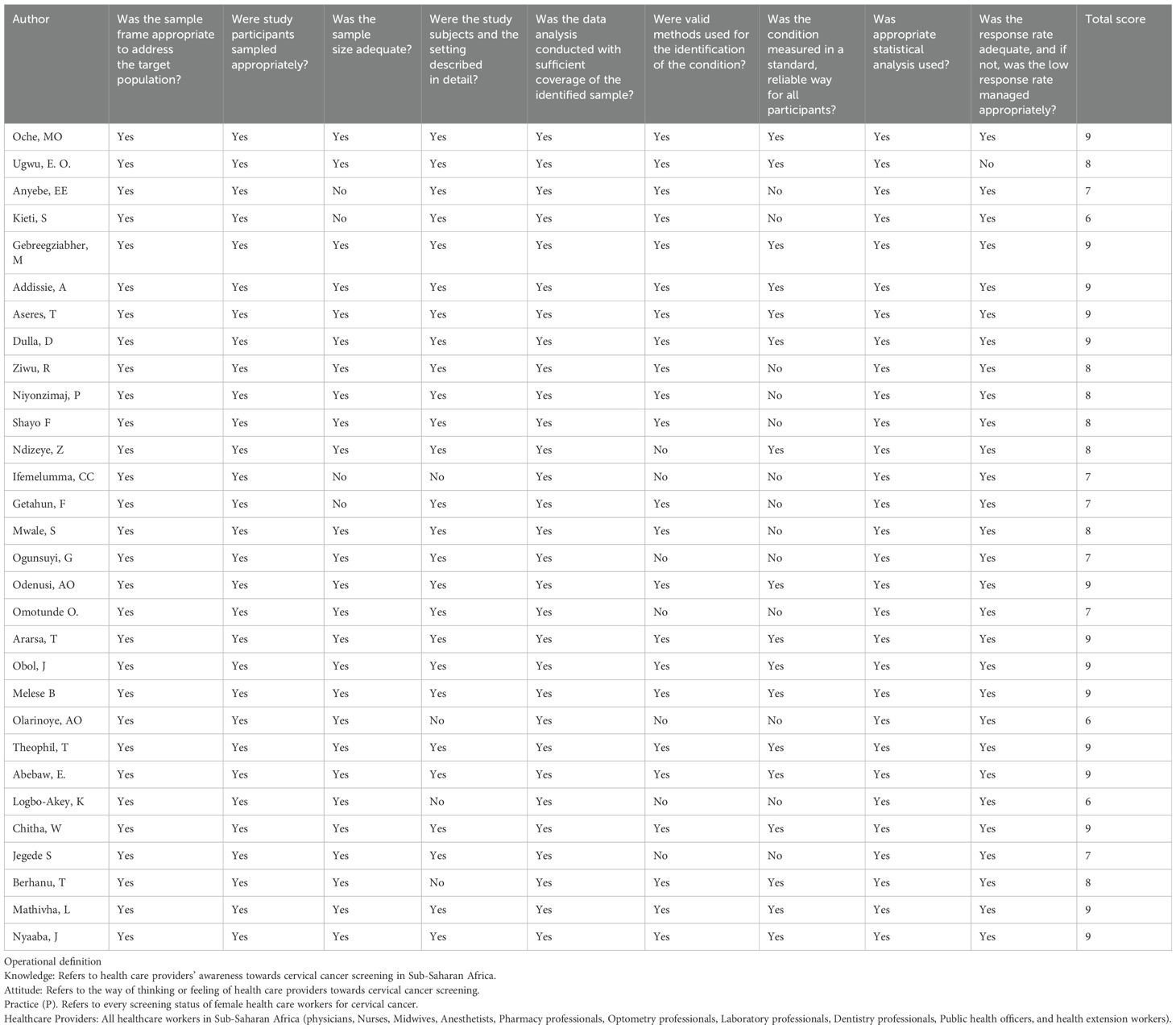
Table 1. Methodological quality assessment of included studies using the JBI critical appraisal checklist for prevalence studies.
Data processing and analysis
Data from Microsoft Excel was transferred to STATA software version 17 for further statistical analysis. The heterogeneity of the study results was evaluated using Cochrane’s Q statistics, and I2 statistics (39). The results were presented using a forest plot, tables, and graphs. The test results showed significant heterogeneity, so we used a random-effect meta-analysis model to determine the overall knowledge status, attitude, and practice level. Subgroup analyses were conducted based on geographical region to address the possible source of heterogeneity. We also employed various statistical tests, including funnel plot asymmetry, Egger’s test, and Begg’s test, to examine the presence of publication bias (40). Visual inspection of funnel plots can help identify publication bias, but it is not enough to rely solely on subjective interpretations (41). It is recommended to use additional statistical tests, such as Egger’s test (42) and Begg’s test (43), to more accurately assess the presence and severity of publication bias. Both meta-regression and, nonparametric trim and fill analysis were carried out to detect the source of publication bias and to adjust the pooled magnitude of attitude and practice of health providers respectively. The researchers also conducted sensitivity analyses to determine how each study affected the overall findings on knowledge, attitude, and practice toward cervical cancer screening. They did this by excluding one study at a time.
Results
Selection of eligible studies
This systematic review and meta-analysis have been reported by the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statements. Initially, 1264 articles related to knowledge, attitude, and practice towards cervical cancer screening were found. Of these, 935 duplicates and 281 articles by title and abstract were removed. After a thorough review, 18 articles were deemed irrelevant and excluded from the analysis. Ultimately, 30 articles were found to be suitable for the review and were included in the analysis (Figure 1).
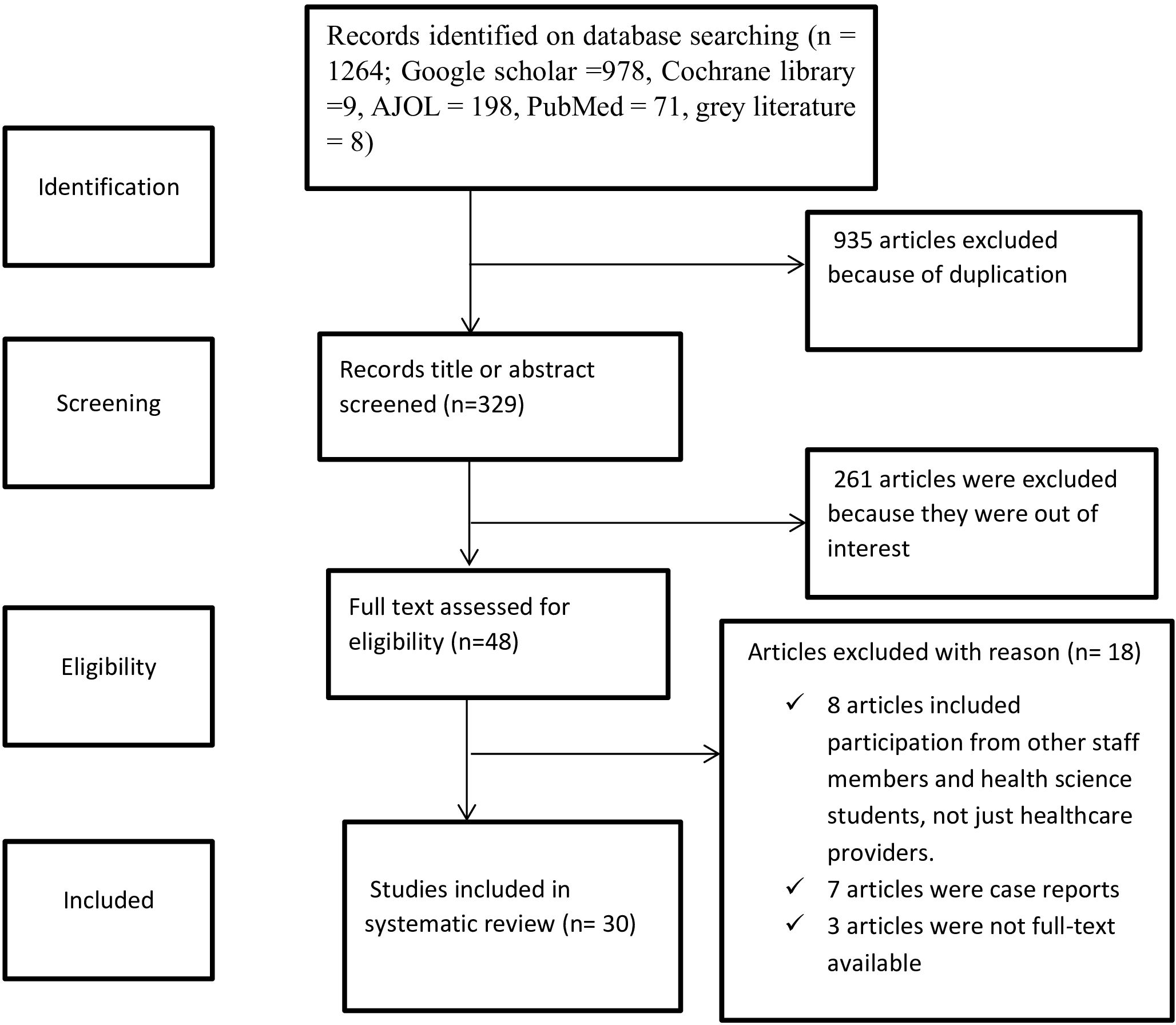
Figure 1. PRISMA flow diagram of knowledge, attitude and practice towards cervical cancer screening among health care providers in Sub-Saharan Africa, 2023.
Characteristics of included studies
A total of 30 studies with a total sample of 7542 healthcare providers were included in this systematic review and meta-analysis. All the studies in this review were conducted using a cross-sectional study design and were published between 2013 and 2023. Among the 30 studies included, 14 were carried out in Eastern Africa (35, 44–56), 12 studies in Western Africa (23, 34, 57–66), and 4 studies in Southern Africa (67–70). Out of the total number of studies, 7 included both male and female participants (45, 51, 52, 54, 67, 69, 71), while 23 studies only included female healthcare Providers. The pooled magnitude of knowledge status towards cervical cancer screening was determined using 15 studies (34, 35, 46–50, 52, 59–61, 64–66, 69), while the pooled magnitude of attitude towards cervical cancer screening was assessed using 9 studies (34, 35, 47–50, 64, 66, 67). Additionally, 23 studies (23, 34, 35, 45–49, 53–60, 62, 64–66, 68–70) were used to assess the pooled magnitude of practice to ever screened status towards cervical cancer among female healthcare providers in Sub-Saharan Africa. Two studies (51, 71) did not provide the pooled results but instead reported on knowledge status regarding various screening methods such as pap smear, VIA, VILI, colposcopy, and HPV DNA test. Out of the total studies reviewed, 9 were unpublished (46, 49, 52, 53, 56, 58, 64, 67, 70) and the remaining 21 of them were published research (Table 2).
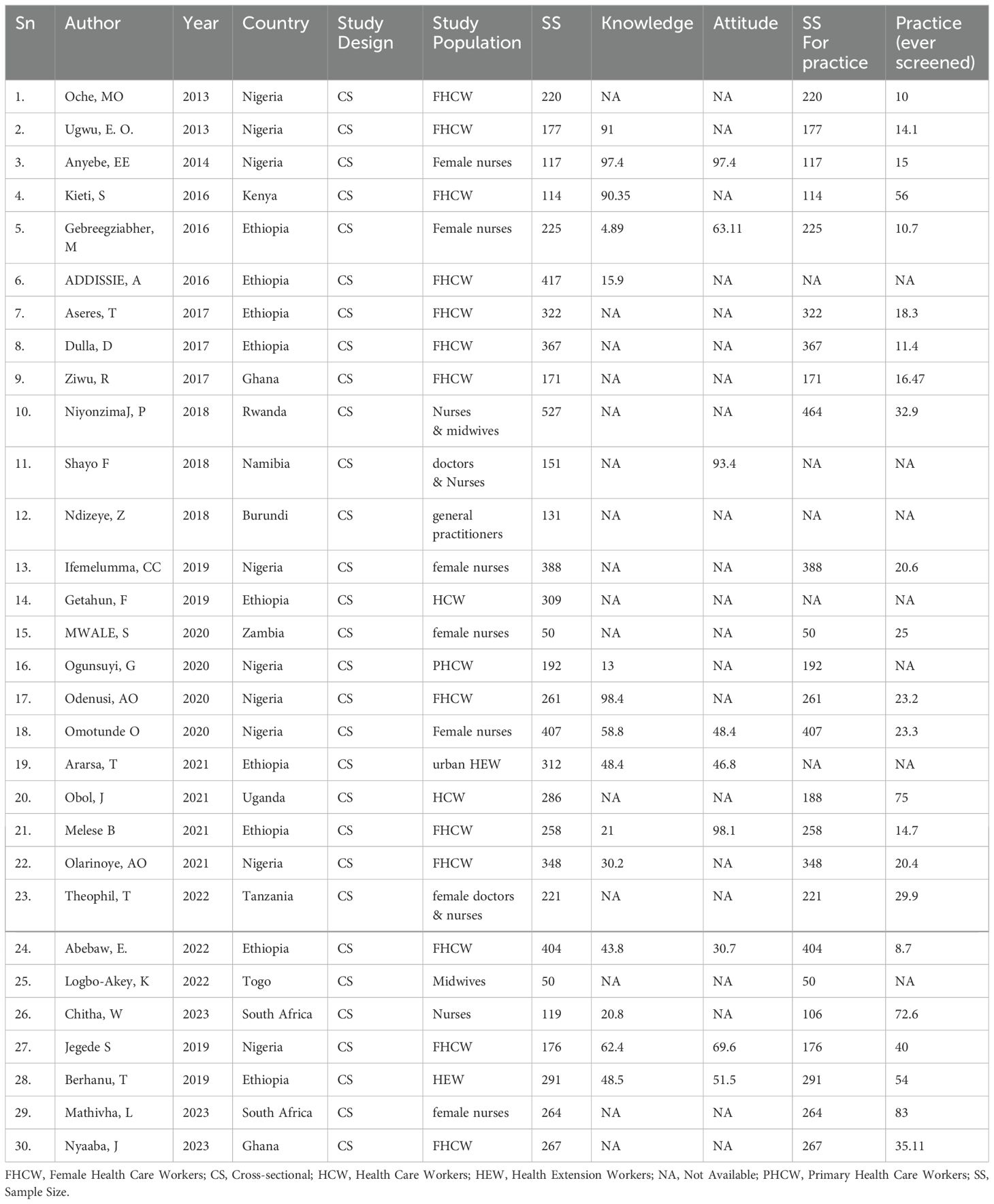
Table 2. Characteristics of the included studies in meta analysis for knowledge, attitude and practice of healthcare providers towards cervical cancer screening in Sub Saharan Africa, 2023.
Pooled magnitude of knowledge and attitude status of health care providers towards cervical cancer
This study assessed the level of knowledge and attitude toward cervical cancer among healthcare providers in Sub-Saharan Africa. Accordingly, the pooled level of good knowledge status about cervical cancer based on 9 included studies (48, 52–55, 57, 59, 60, 71) in Sub-Saharan Africa was 67.93% (95% CI: 53.36–82.50) (Figure 2). Moreover, the pooled magnitude of positive attitude of health care providers towards cervical cancer based on 2 included studies (52, 54) in Sub-Saharan Africa was 55.26% (95% CI: 34.28– 76.23) (Figure 3).
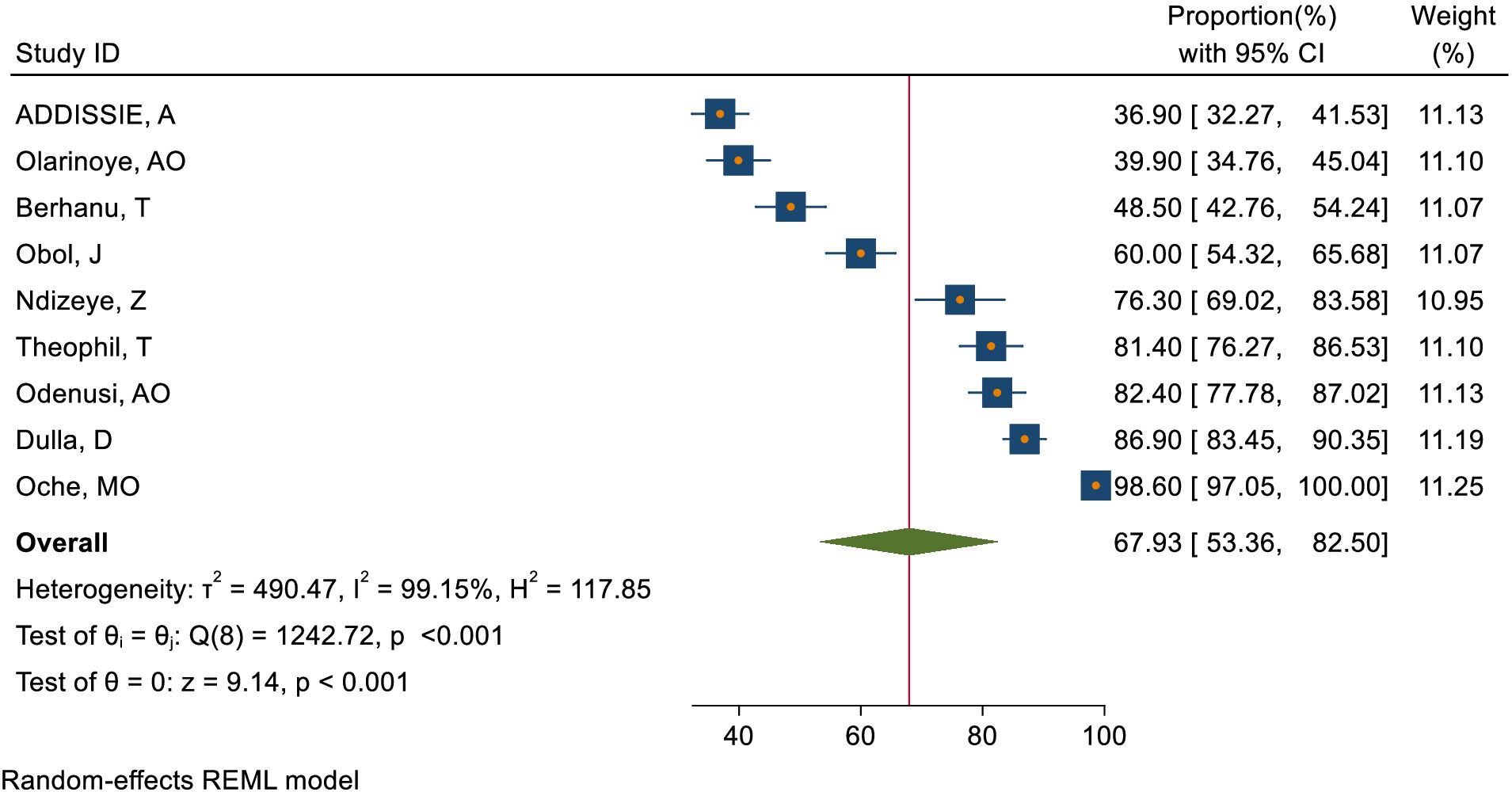
Figure 2. Overall magnitude of goods knowledge status of healthcare providers towards cervical cancer in Sub-Saharan Africa, 2023.
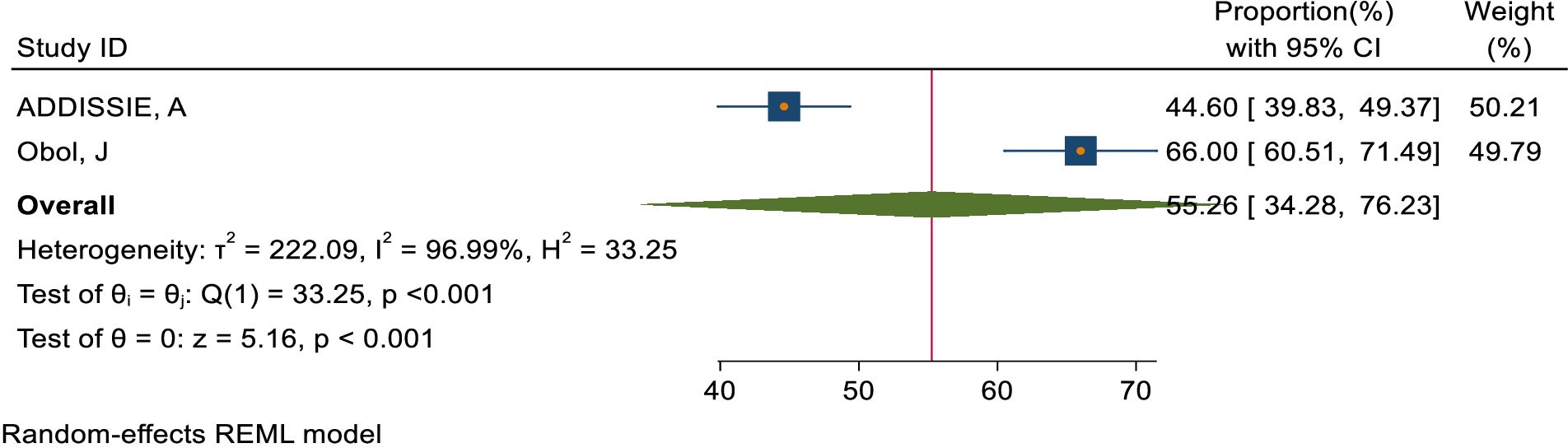
Figure 3. Overall magnitude of positive attitude status of healthcare providers towards cervical cancer in Sub-Saharan African, 2023.
Overall knowledge status of health care providers regarding causes, risk factors, signs and symptoms, outcomes, and prevention methods of cervical cancer
Healthcare providers have a good knowledge status of 42.51% regarding the causes of cervical cancer, 73.51% regarding the risk factors, 76.85% regarding the symptoms, 81.7% regarding the outcomes, and 72.75% regarding the prevention methods (Figure 4).
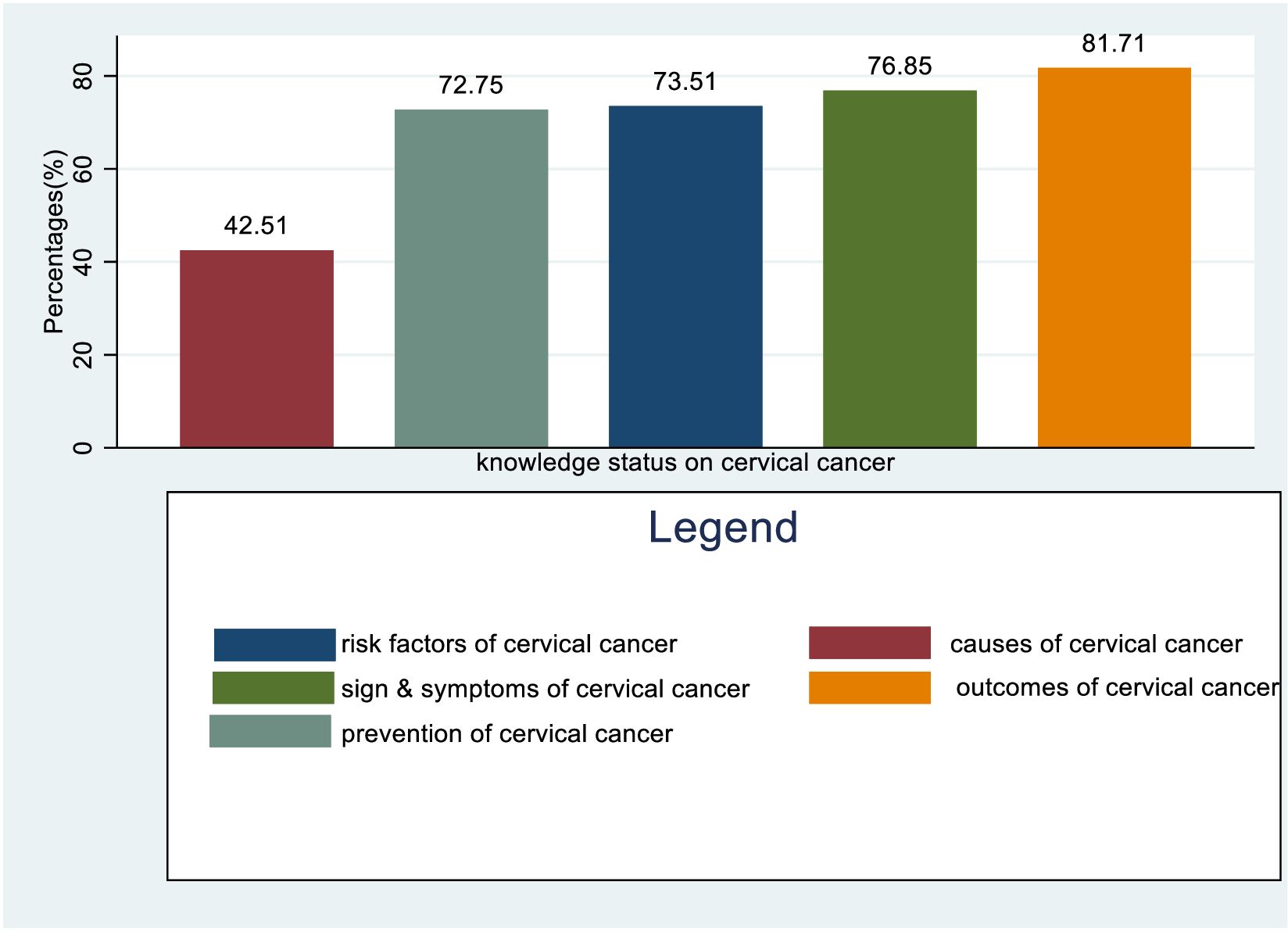
Figure 4. Overall Knowledge status of healthcare providers towards causes, risk factors, symptoms, outcome, and prevention methods of cervical cancer in Sub-Saharan Africa, 2023.
Knowledge status of health care providers towards risk factors of cervical cancer
About 66.38%, 52.47%, 52.06% and 50.46% of healthcare providers know HPV infection, HIV, early sexual intercourse, and STI mention as a risk factor for cervical cancer respectively. In contrast, about 1.98% do not mention any of the risk factors (Figure 5).
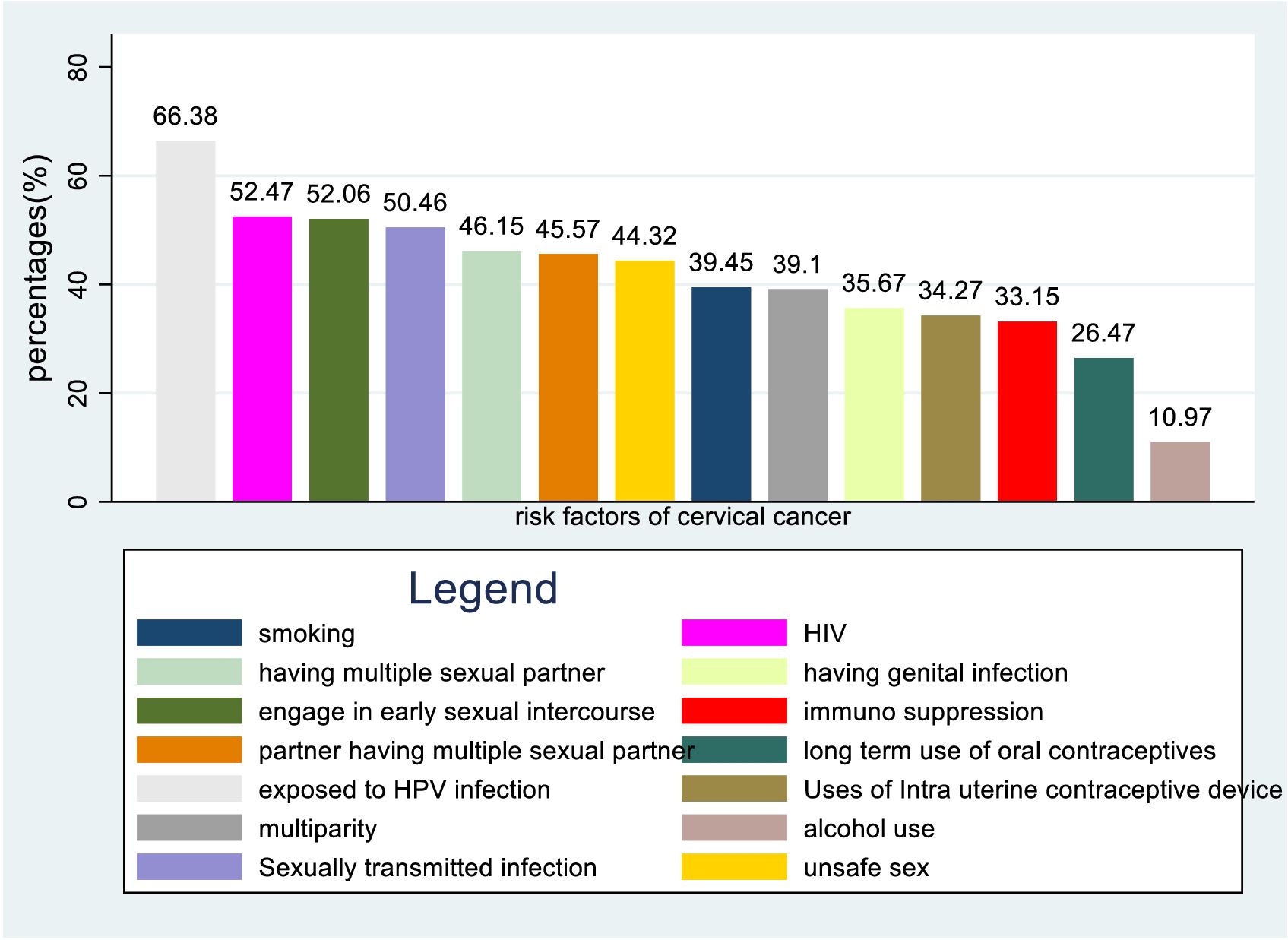
Figure 5. Bar graph for knowledge status of healthcare providers towards risk factors of cervical cancer in Sub-Sahara Africa, 2023.
Knowledge status of health care providers regarding signs and symptoms of cervical cancer
Around 65.56%, 60.99%, 56.93%, and 54.55% of healthcare providers were aware of postcoital bleeding, abnormal menstruation, bleeding during sexual intercourse, and foul-smelling vaginal discharge as potential signs and symptoms of cervical cancer. Less than half of healthcare providers are knowledgeable about certain symptoms and conditions, such as painful sexual intercourse (47.5%), postmenopausal bleeding (41.73%), pelvic or back pain (39.16%), and contact bleeding (23.96%). A small percentage (4.62%) do not know any of the signs and symptoms, while an even smaller percentage (2.3%) are unaware of weight loss as a potential symptom (Figure 6).
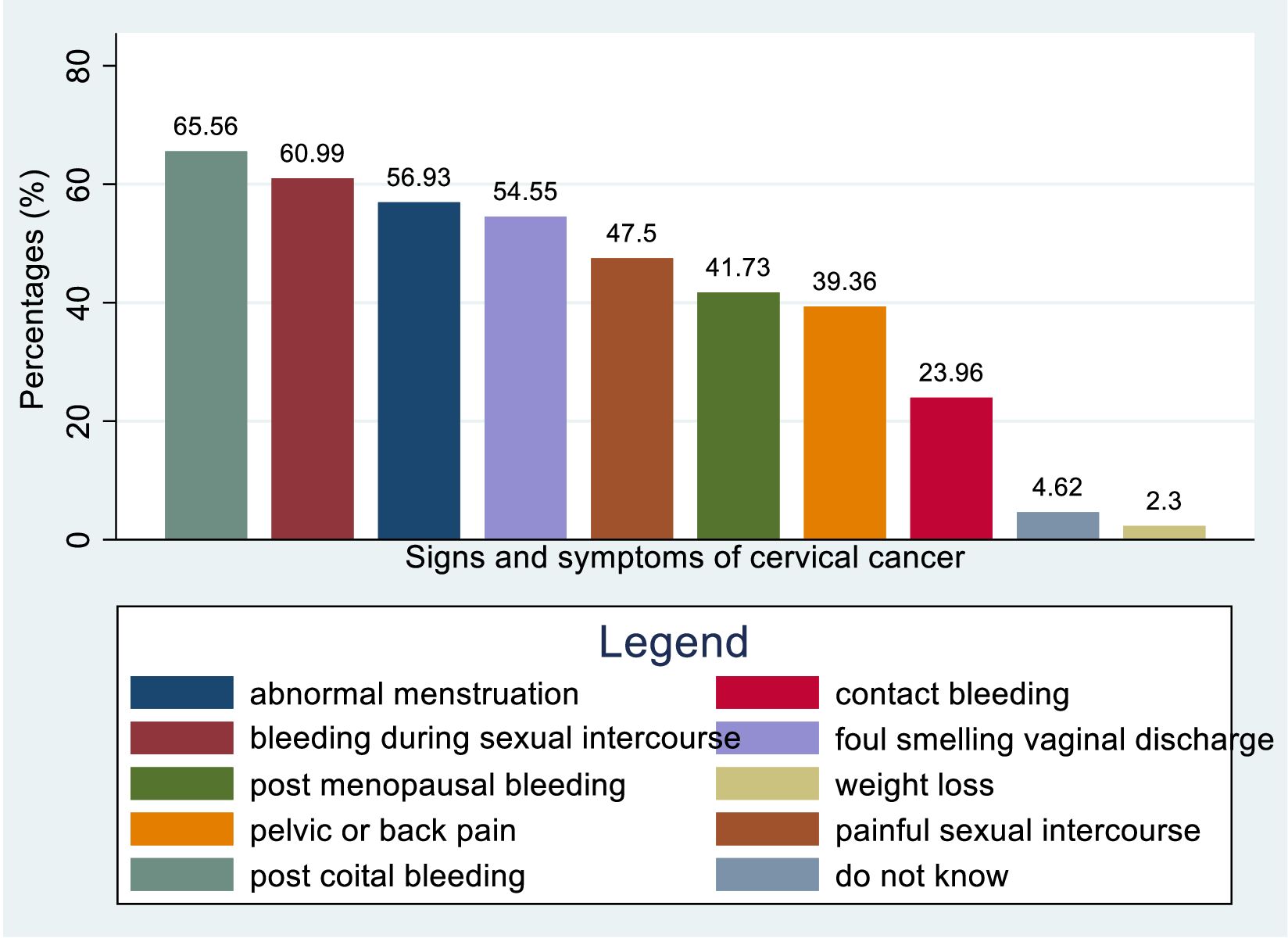
Figure 6. Bar graph for knowledge status of healthcare providers towards symptoms and signs of cervical cancer in Sub-Sahara Africa, 2023.
The overall magnitude of knowledge, attitude, and practice status toward cervical cancer screening
This study assessed knowledge status, attitude, and practice toward cervical cancer screening among healthcare providers in Sub-Saharan Africa. The pooled level of good knowledge towards cervical cancer screening was 49.68% (95% CI: 33.18–66.17) (Figure 7) whereas the pooled magnitude of positive attitude toward cervical cancer screening among healthcare providers in Sub-Saharan Africa was 66.63% (95% CI: 50.36– 82.89) (Figure 8). On the other hand, the pooled magnitude of ever screened for cervical cancer among female healthcare providers in Sub-Saharan Africa was 30.78% (95% CI: 21.69–39.88) (Figure 9). Since this result had a significant publication bias, the true pooled magnitude of female healthcare providers ever screened for cervical cancer was found to be 17.23% (95% CI; 6.08-28.37) after accounting for publication bias through trim and fill analysis.
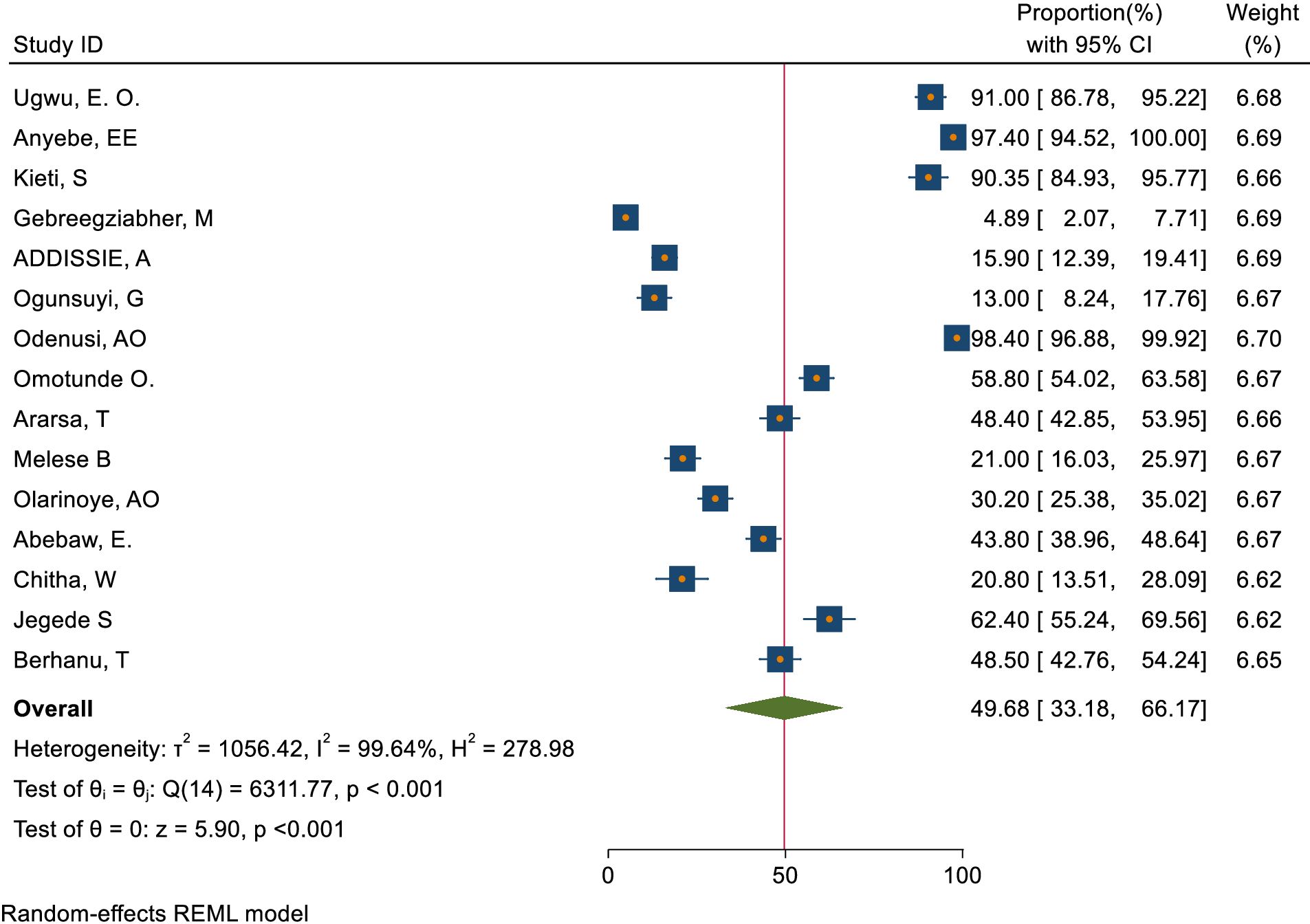
Figure 7. Overall magnitude of good knowledge status of health care providers towards cervical cancer screening in Sub-Saharan Africa, 2023.
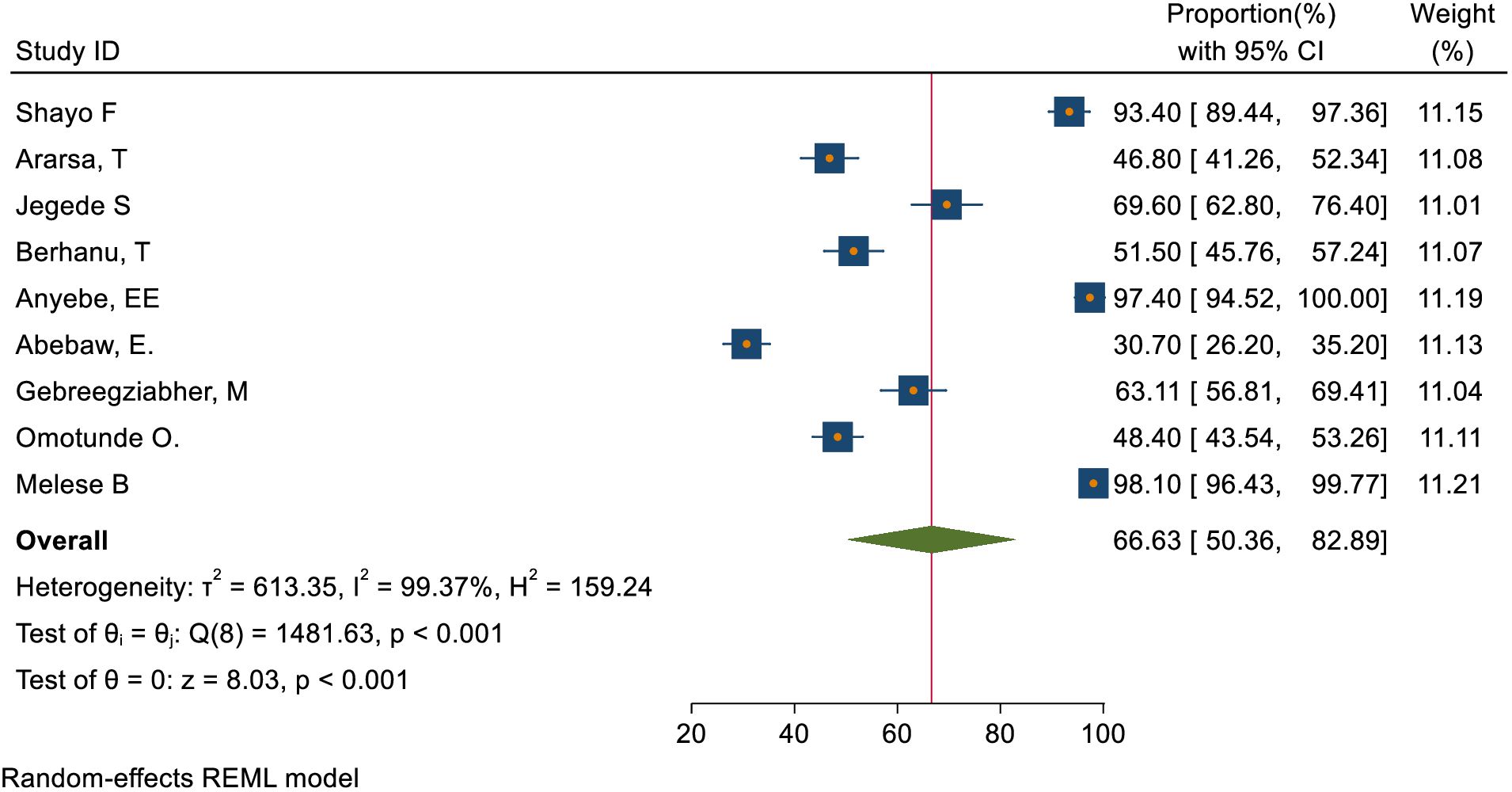
Figure 8. Overall magnitude of positive attitude of healthcare providers towards cervical cancer screening in Sub-Saharan Africa, 2023.
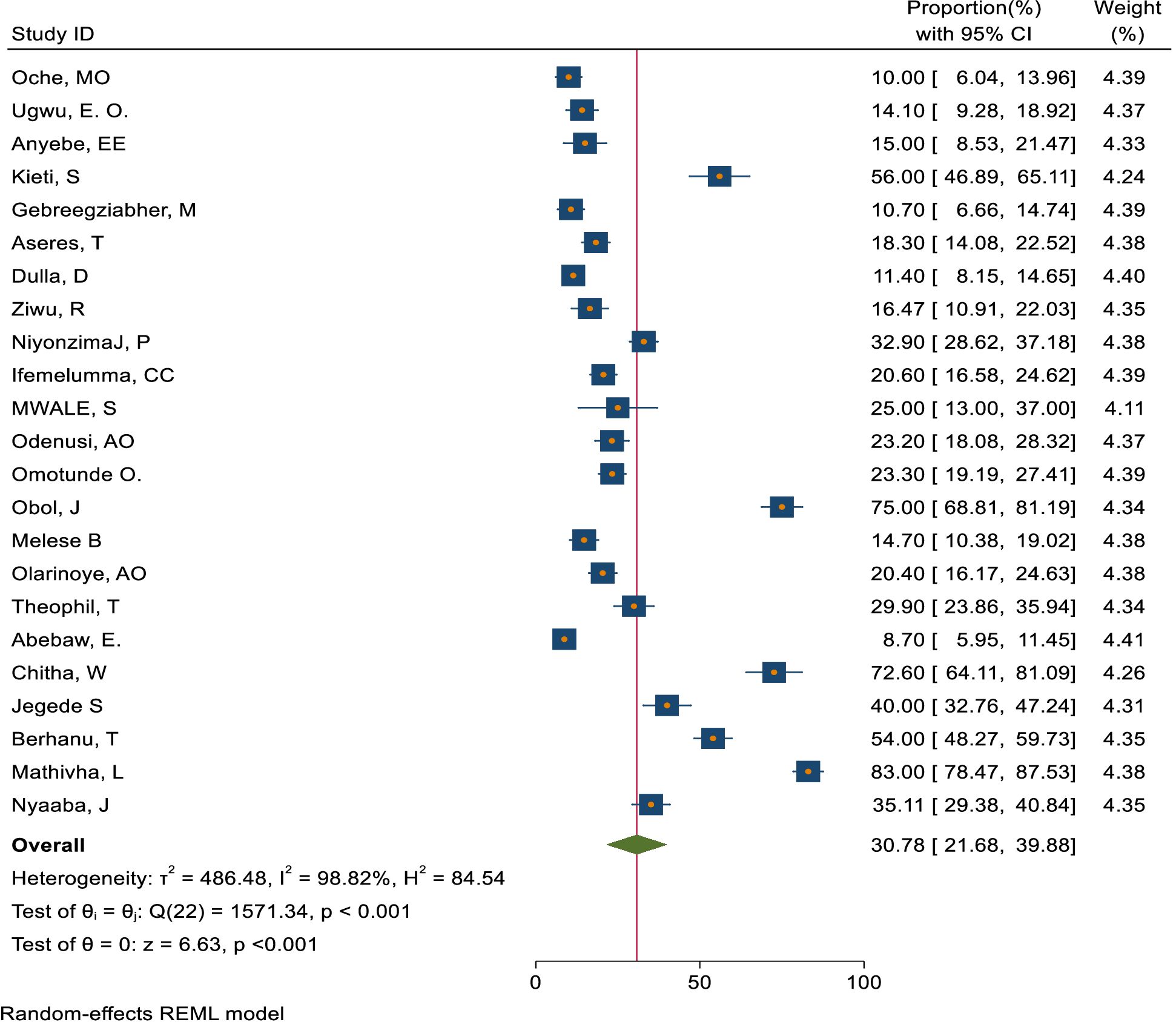
Figure 9. Overall magnitude of practice to ever screened for cervical cancer screening among female healthcare providers in Sub-Saharan Africa, 2023.
Subgroup analysis
Subgroup analysis was carried out based on geographical regions. Accordingly, the pooled magnitude of knowledge status towards cervical cancer screening among healthcare providers was 38.92% (95% CI: 17.83– 60.01) in East Africa, 64.50%(95% CI: 39.54–89.47) in Western Africa, and 20.80%(95% CI: 13.51– 28.09) in Southern Africa respectively (Figure 10). Similarly, the pooled magnitude of positive attitudes toward cervical cancer screening among healthcare providers was 58.11%(95% CI: 35.85– 80.36) in East Africa, 71.86%(95% CI: 43.93-99.80) in Western Africa, and 93.40%(95% CI: 89.44– 97.36) in Southern Africa respectively (Figure 11). Besides, the pooled magnitude of healthcare providers ever screened for cervical cancer was 31.00%(95% CI: 16.71– 45.30) in East Africa, 21.64%(95% CI: 16.01–27.27) in Western Africa, and 60.54%(95% CI: 25.80– 95.28) in Southern Africa respectively (Figure 12).
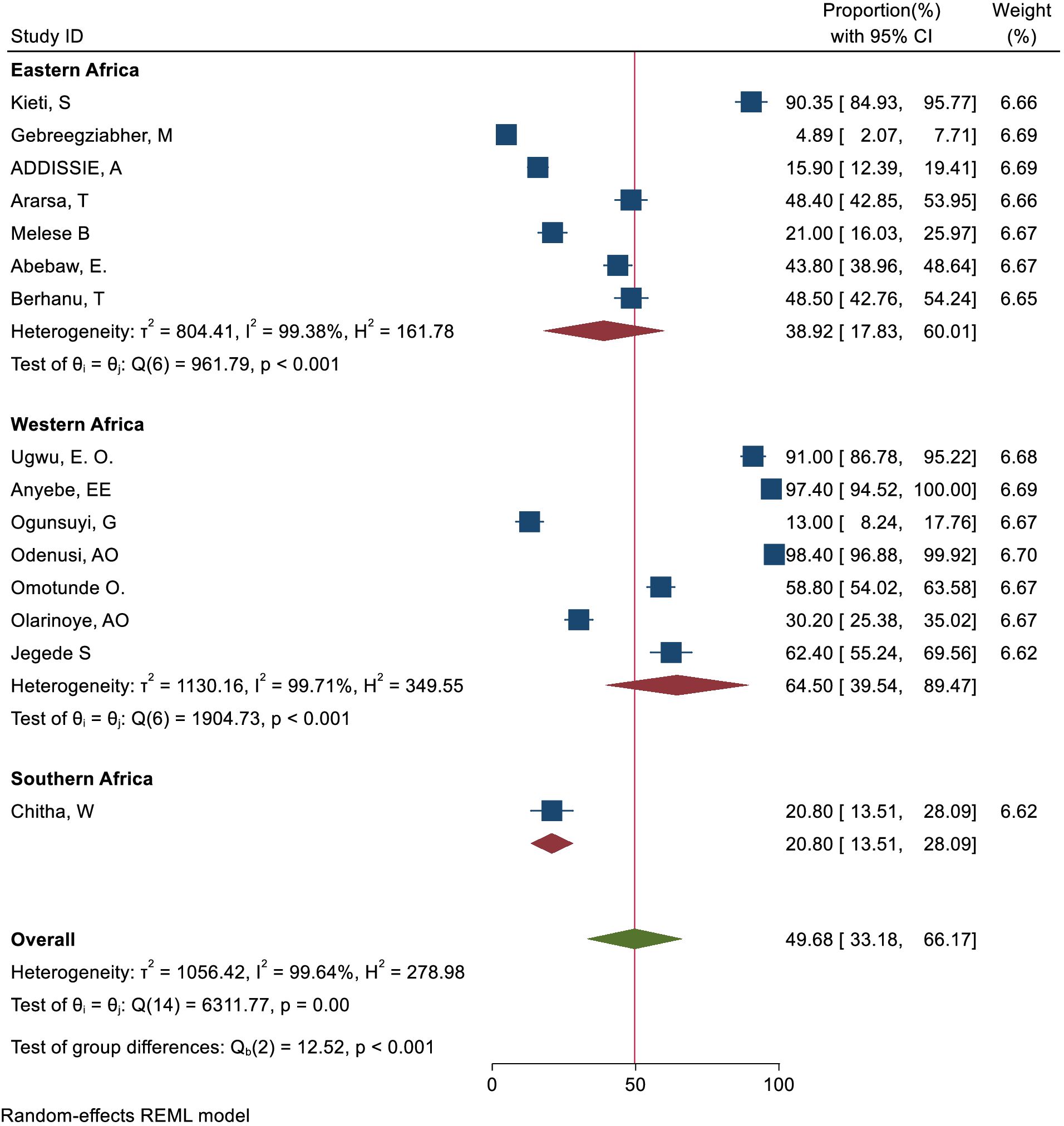
Figure 10. Subgroup analysis-based study area of knowledge status towards cervical cancer screening among health care providers in Sub-Sahara Africa, 2023.
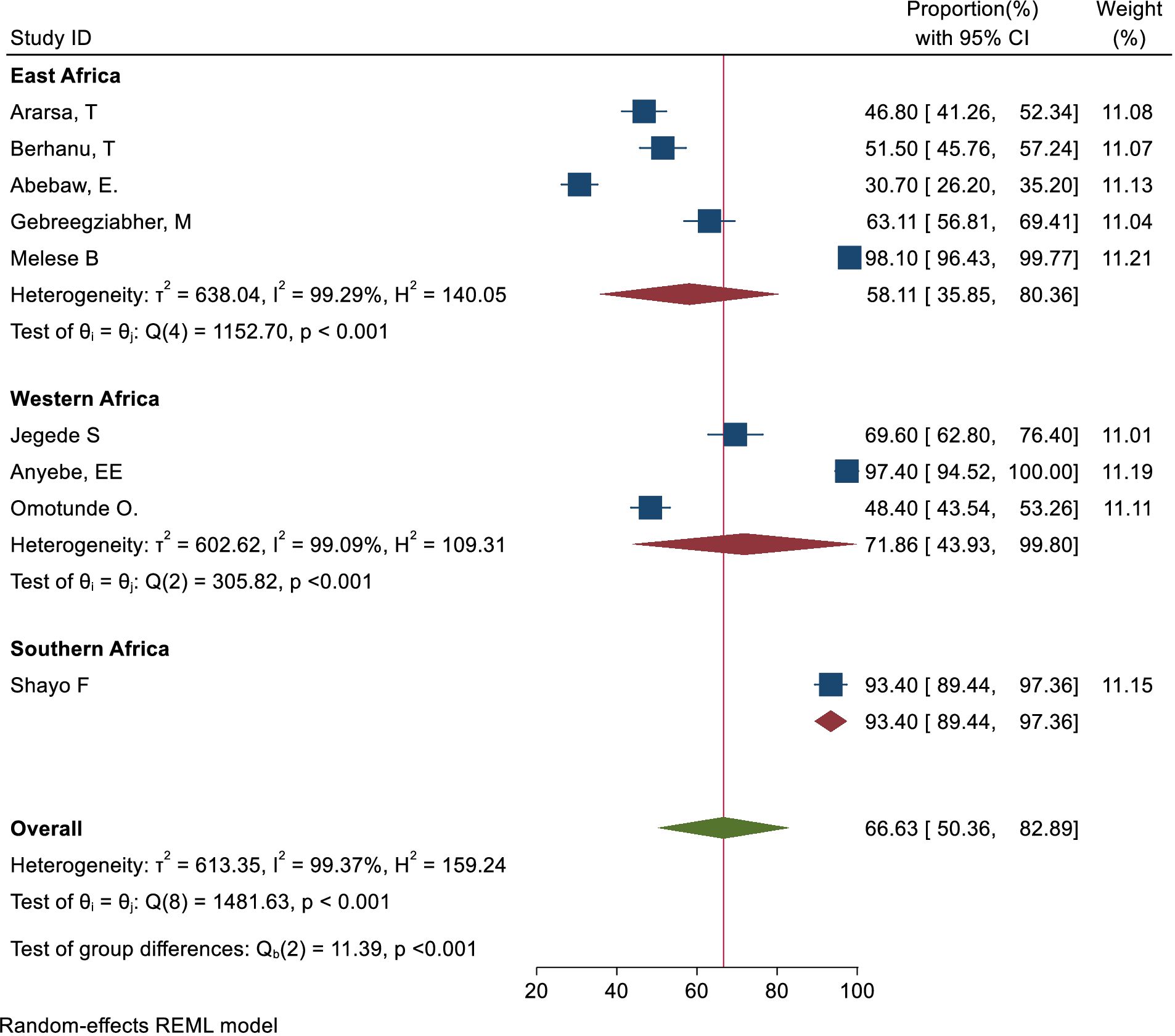
Figure 11. Sub group analysis-based study area of attitude status towards cervical cancer screening among healthcare providers in Sub Sahara Africa, 2023.
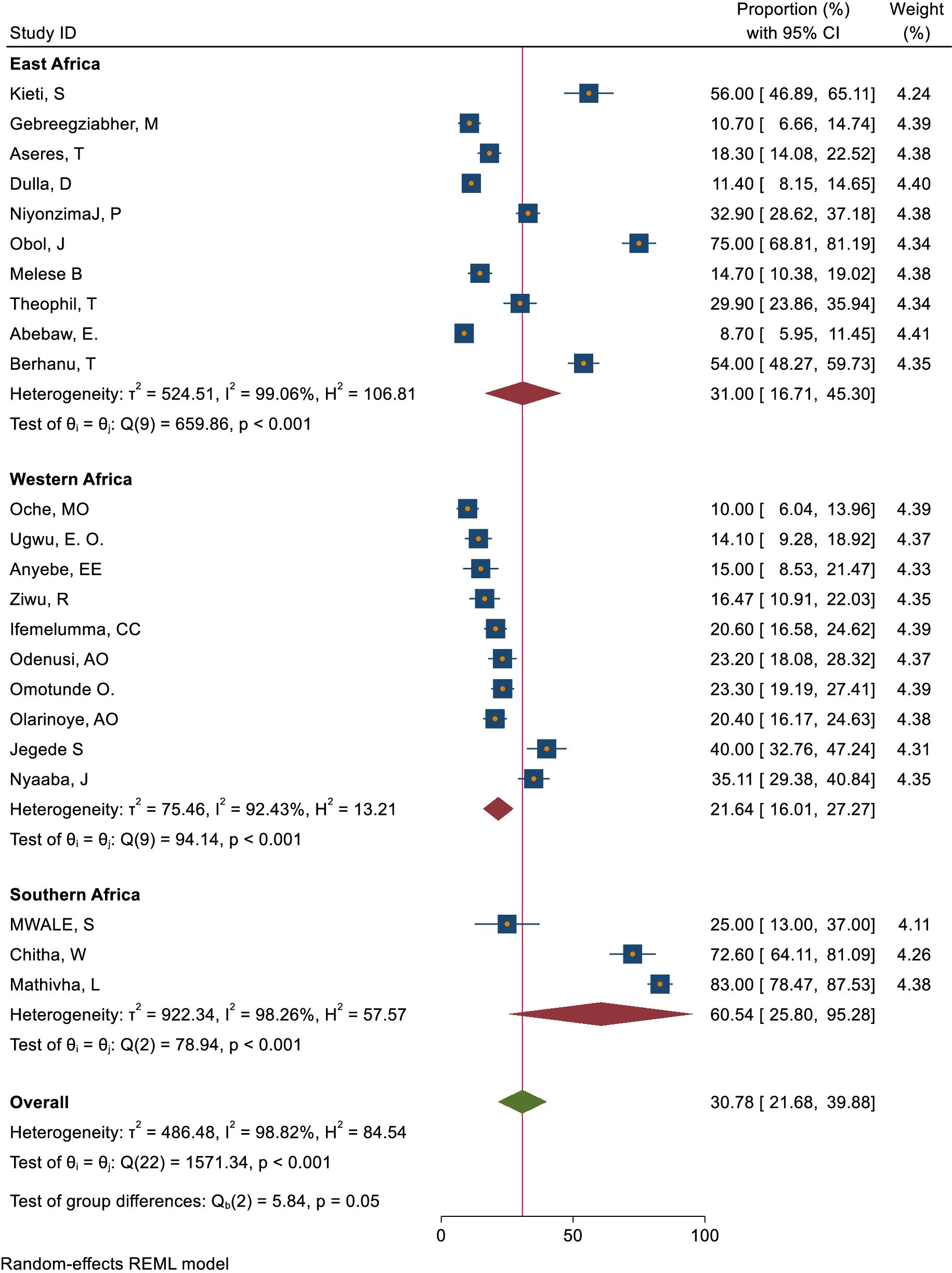
Figure 12. Sub group analysis-based on study area practices to ever screen for cervical cancer among healthcare providerd in Sub Sahara Africa, 2023.
Knowledge status of healthcare providers towards cervical cancer screening methods and regular cervical cancer screening interval
Around 72.02% of healthcare providers knew about pap smear as a screening method for cervical cancer, while 46.15% were aware of the HPV DNA test. Furthermore, approximately 41.68% knew about both pap smear and VIA, while 35.54% were only aware of VIA. A total of 30.18% were aware of VILI, and 23.92% knew about either VIA or VILI as screening methods for cervical cancer (Figure 13). The overall knowledge status towards knowing the regular interval for cervical cancer screening was 27.34% (95% CI: 18.93– 35.76) (Figure 14).
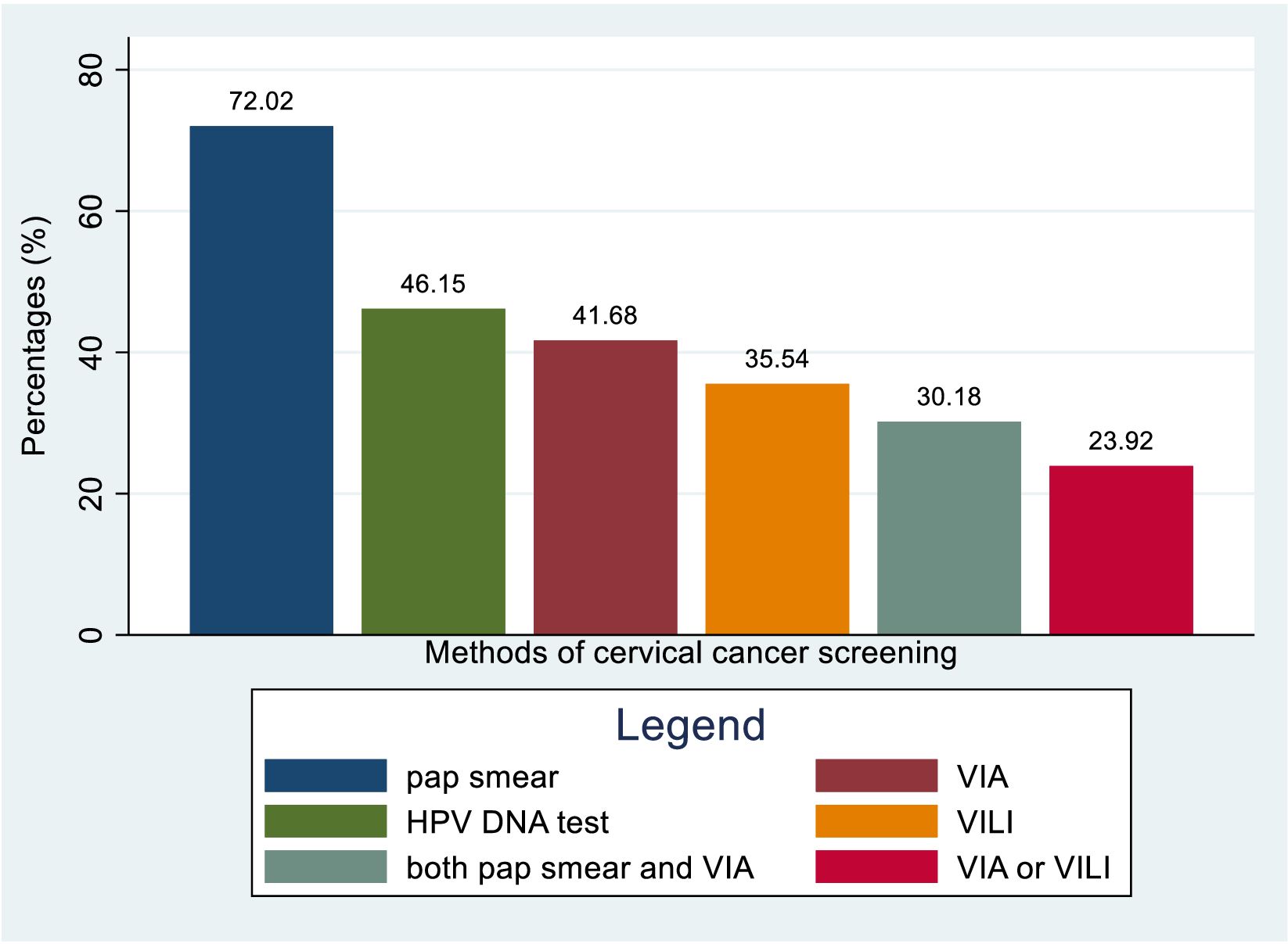
Figure 13. Bar graph for knowledge status of healthcare providers towards different cervical cancer screening methods in Sub-Sahara Africa, 2023.
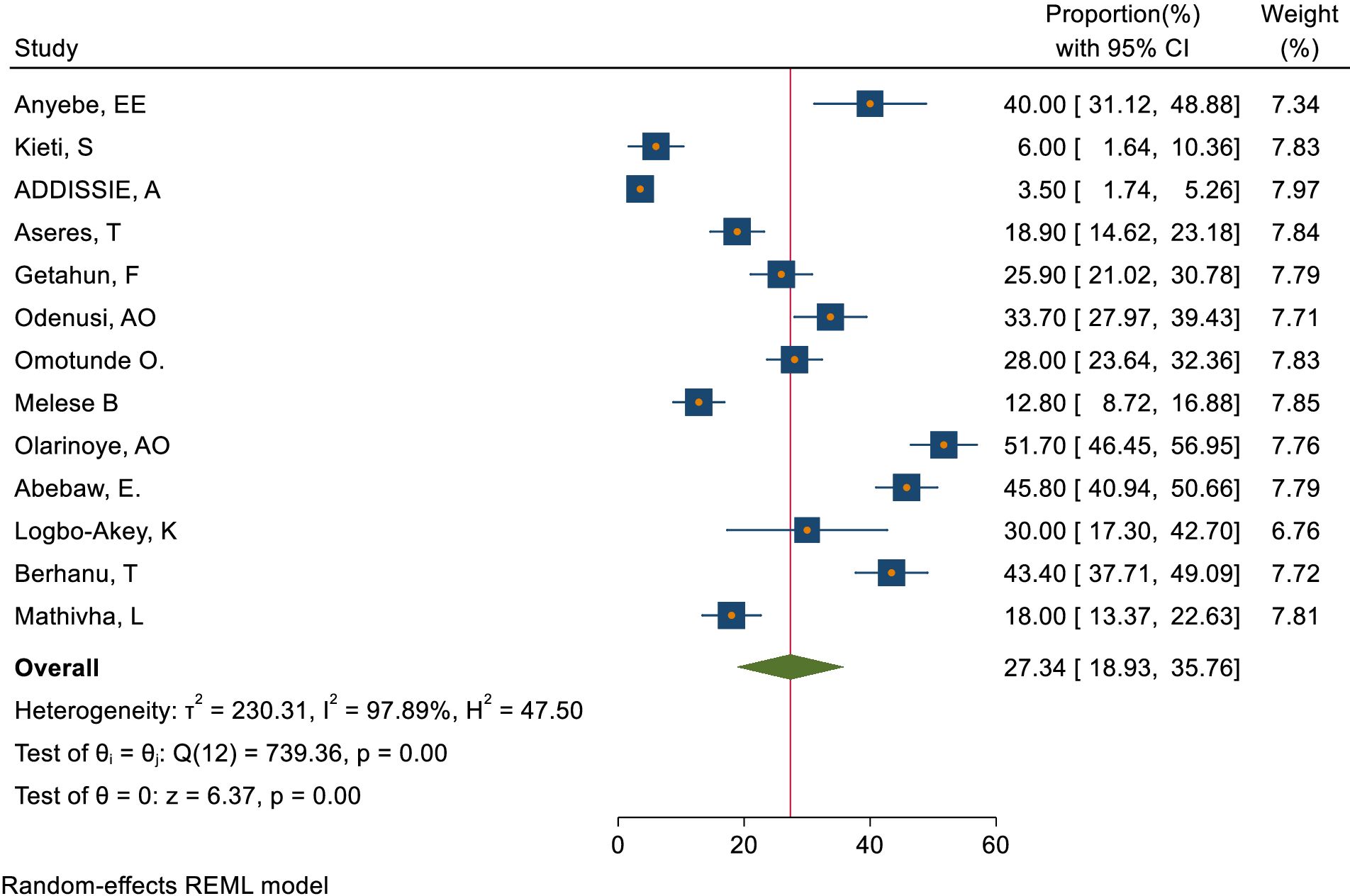
Figure 14. Overall knowledge status of healthcare providers towards knowing the regular interval for cervical cancer screening in Sub-Sahara Africa, 2023.
Reasons for not being screened yet for cervical cancer
A variety of reasons were given by respondents for not being screened. Approximately 28.47% of respondents chose not to get screened because they believed they were healthy. Another 27.97% were afraid of receiving a positive result, while 25.82% were afraid of experiencing pain during the screening. Additionally, 24.38% cited privacy concerns, 22.68% mentioned the cost of screening as a deterrent, 22.28% believed they were not susceptible to the condition being screened for, and 21.62% stated that the service was inaccessible. On the other hand, 19.42% of respondents were not screened due to their husband’s disapproval, 16.66% cited a lack of time, and 16.02% expressed no interest or carelessness. Other reasons included fear of using rusty or dirty equipment (15.9%), being considered too old for screening (14.74%), cultural or religious beliefs (8.22%), and fear of embarrassment (4.29%) (Figure 15).
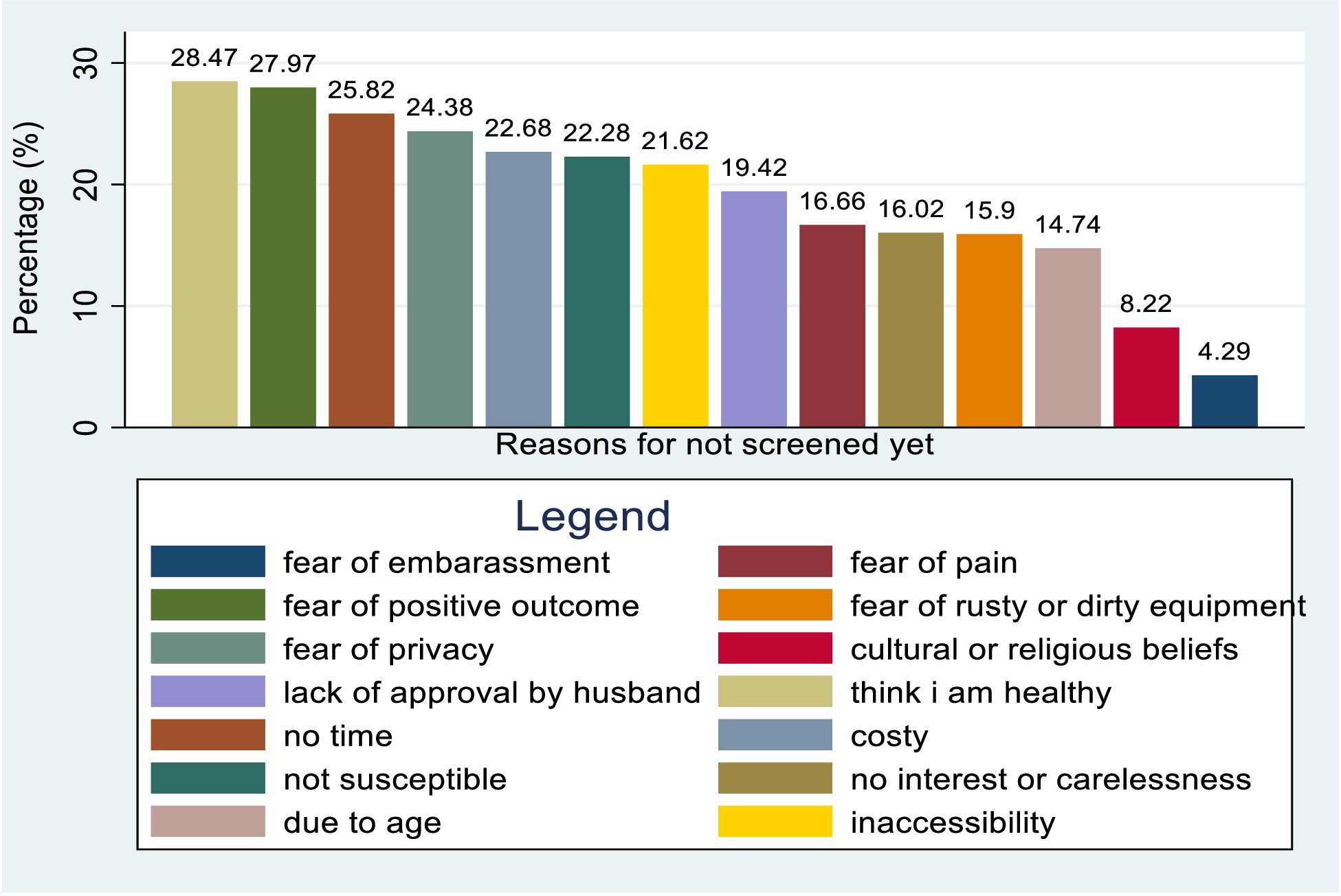
Figure 15. Bar graph indicating reasons for not screened yet for cervical cancer of health care providers towards risk factors of cervical cancer in Sub Sahara Africa, 2023.
Publication bias assessment and sensitivity analysis
The researchers checked for publication bias by visually inspecting a funnel plot, as well as using statistical tests. The funnel plot showed that the included studies were distributed symmetrically. Moreover, both Begg’s and Egger’s tests indicated the absence of publication bias in the knowledge status of healthcare providers towards cervical cancer screening. The tests showed no statistical evidence of publication bias with a p-value greater than 0.05 (P value; Eggers test=0.38, Beggs test=1.00), and the funnel plot was symmetrical (Figure 16). On the contrary, the study found that there was publication bias in the data on healthcare providers’ attitudes towards cervical cancer screening. The funnel plot revealed an uneven distribution of the studies (Figure 17). The Egger’s test found evidence of publication bias (P value=0.04), indicating that there may be a bias in the published studies. However, Begg’s test (P value=0.60) suggested that there is no publication bias regarding the attitude of healthcare providers towards cervical cancer screening. To address this bias, the researchers conducted a trim and fill analysis however the pooled magnitude of attitude did not impute additional studies and the overall magnitude of attitude did not vary from the original findings.
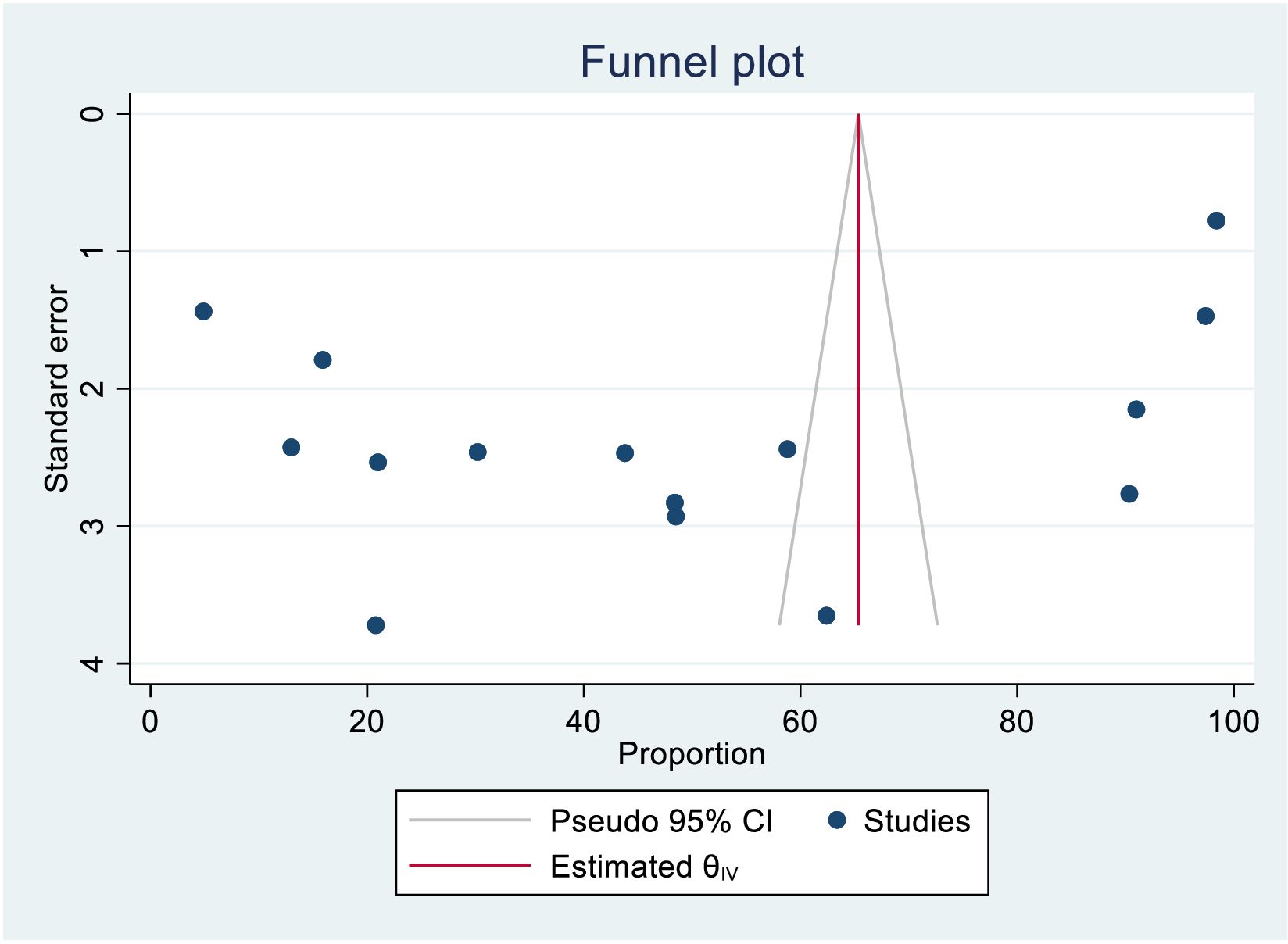
Figure 16. Funnel plot assessment for knowledge status towards cervical cancer screening among healthcare providers in Sub Saharan Africa, 2023.
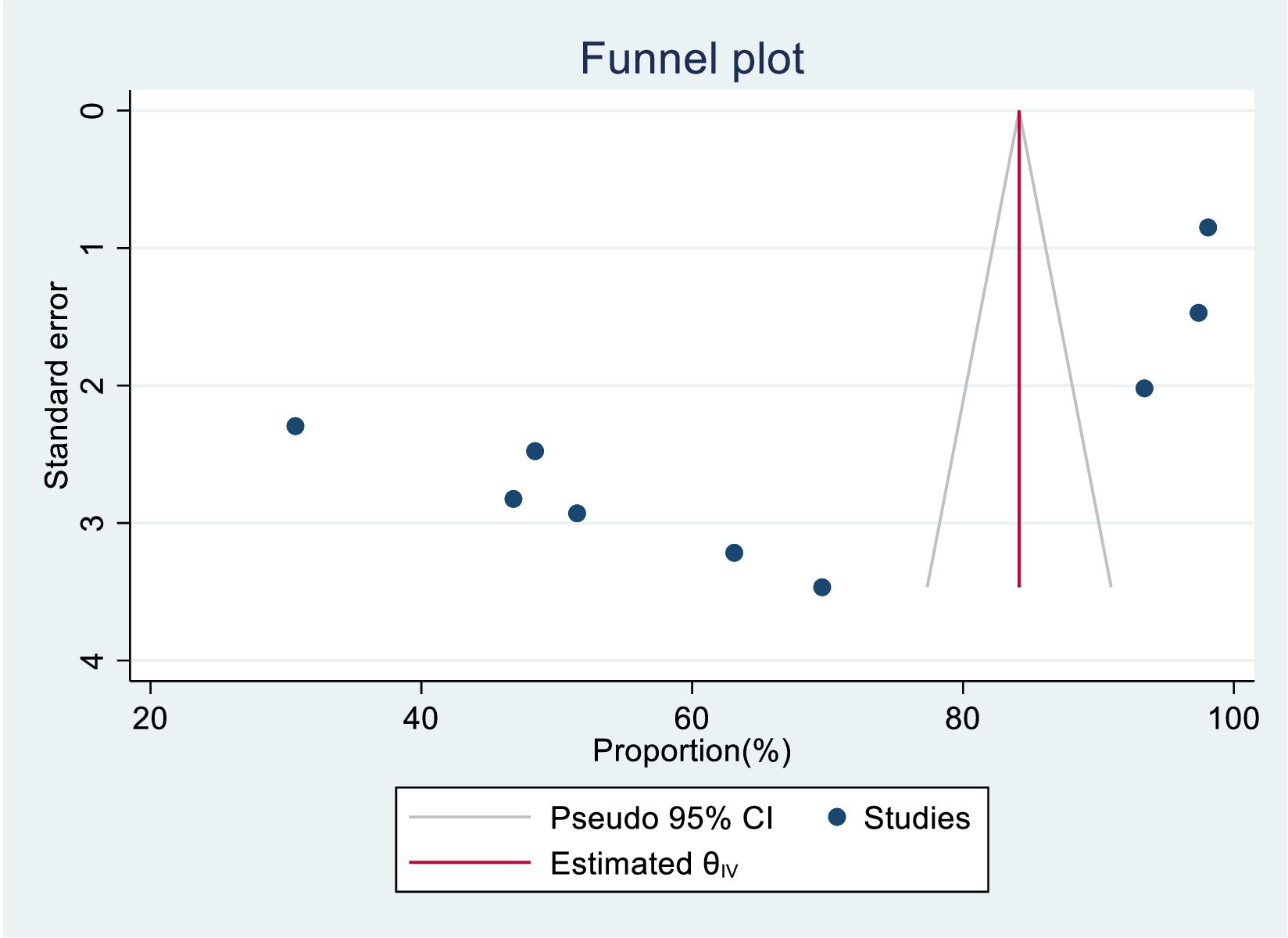
Figure 17. Funnel plot assessment for attitude status towards cervical cancer screening among health care providers in Sub Saharan Africa, 2023.
We also assessed publication bias for the practice of female healthcare providers to ever screened for cervical cancer. Accordingly, Egger’s tests indicated the absence of publication bias in the pooled magnitude healthcare providers ever screened for cervical cancer (P value; Eggers test=0.10). However, Beggs tests showed statistical evidence of publication bias with a p-value less than 0.05(P value; Beggs test=0.04), and the funnel plot was asymmetrical (Figure 18). To address this bias, the researchers conducted a trim and fill analysis, which adjusted the original pooled results of 30.80%(95% CI: 21.69–39.91). The adjusted pooled magnitude of healthcare providers ever screened for cervical cancer was 17.23 (95% CI; 6.08-28.37) after including eight additional studies on the left side. This adjusted result is considered to be a more accurate representation of the true practice of healthcare providers ever screened for cervical cancer. The result of sensitivity analyses revealed that none of the studies included influenced the overall estimate (Figures 19–21).
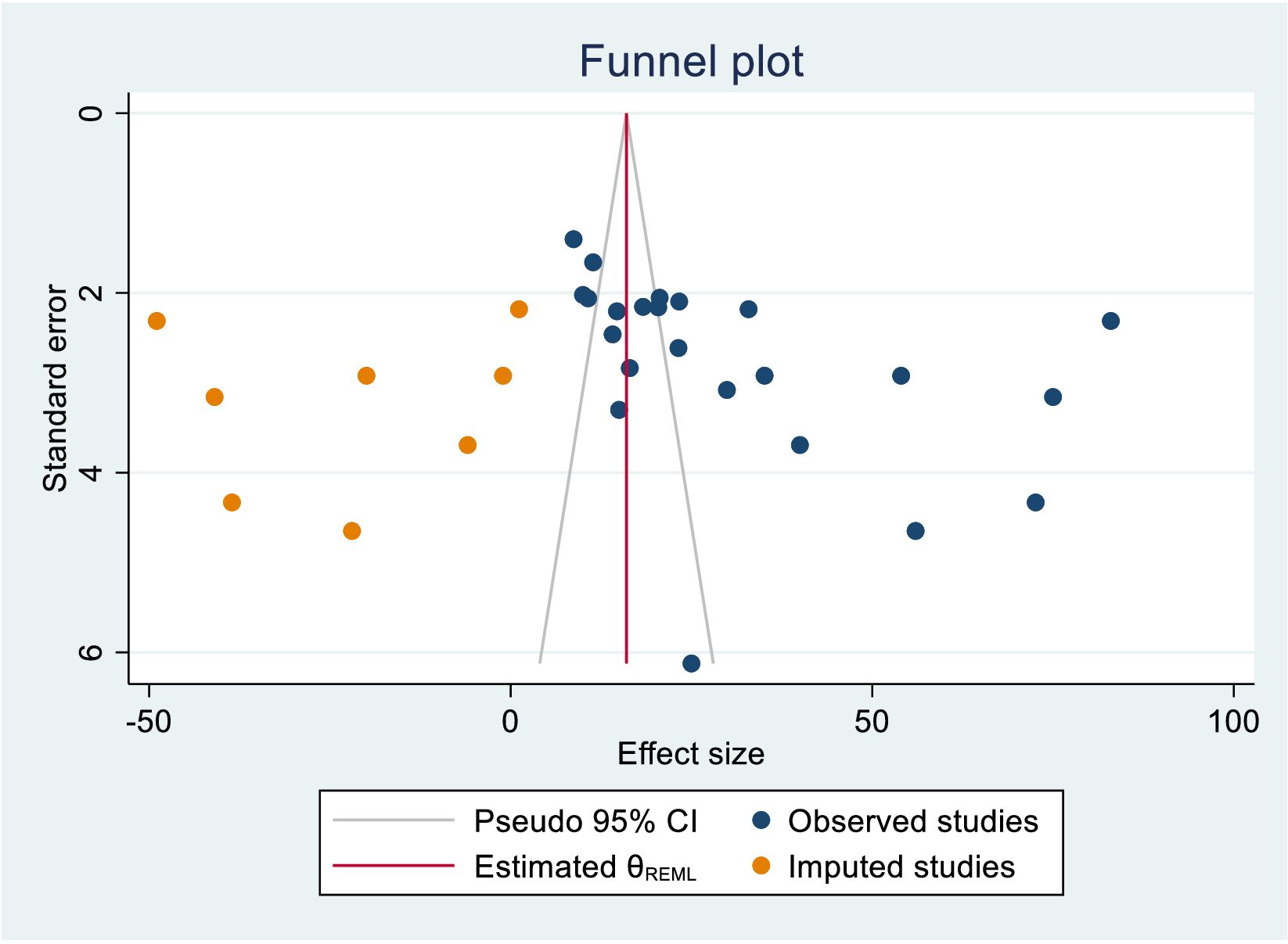
Figure 18. Funnel plot assessment of practice for female healthcare providers to ever screened status towards cervical cancer screening in Sub Saharan Africa, 2023.
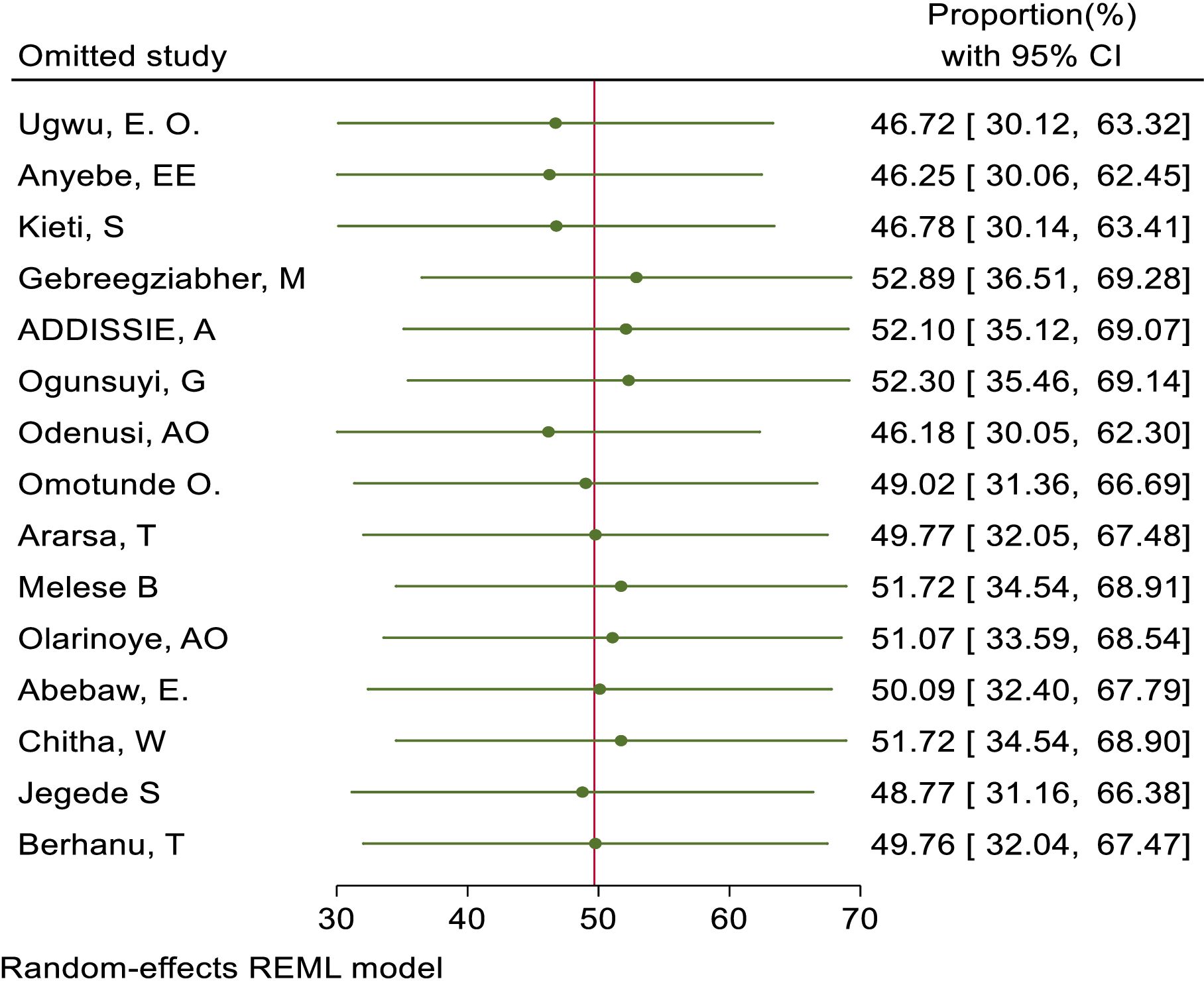
Figure 19. Sensitivity analysis for good knowledge status of health care providers towards cervical cancer screening among health care providers in Sub Saharan Africa, 2023.
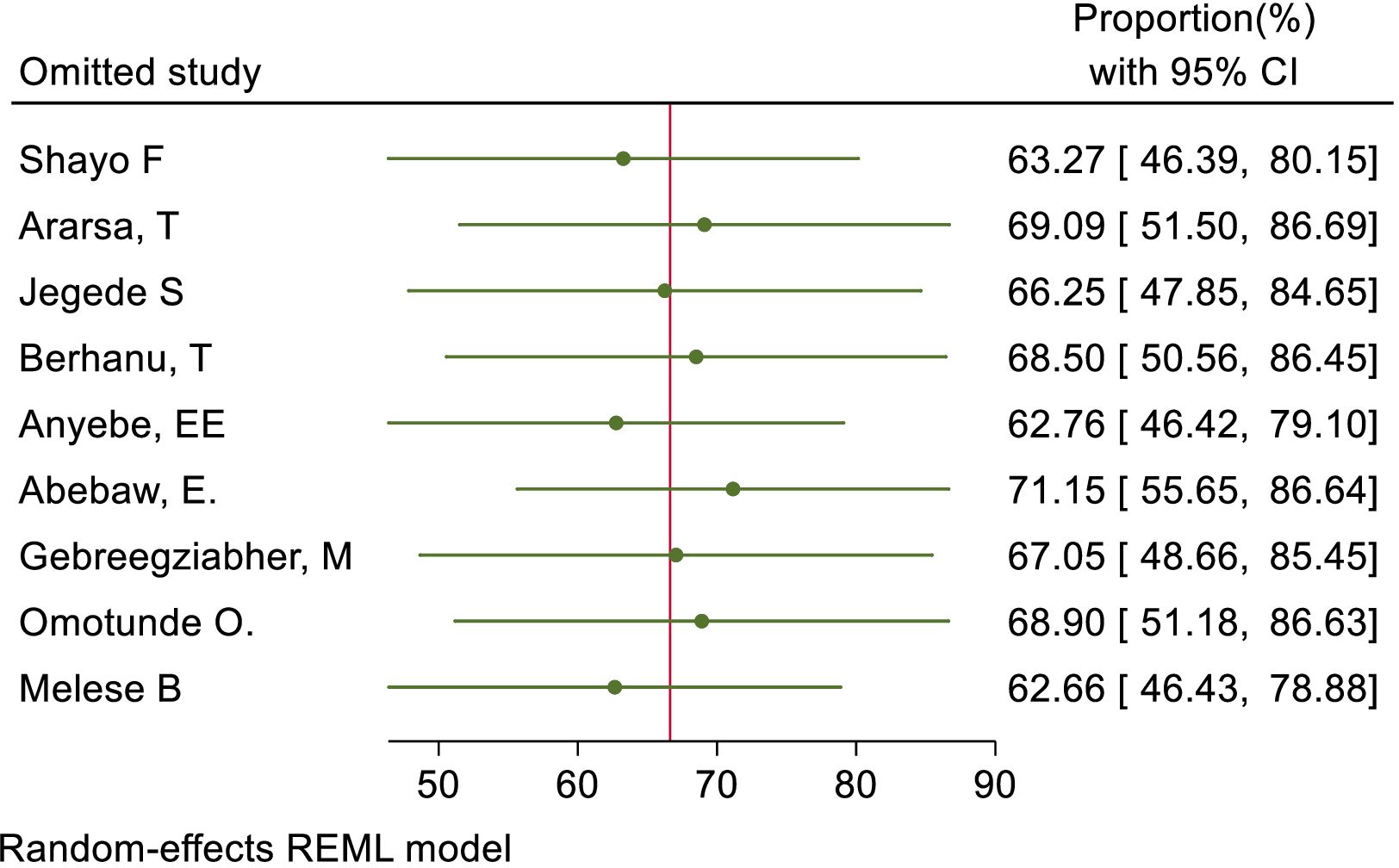
Figure 20. Sensitivity analysis for positive status of respondents towards cervical cancer screening among health care providers in Sub Saharan Africa, 2023.
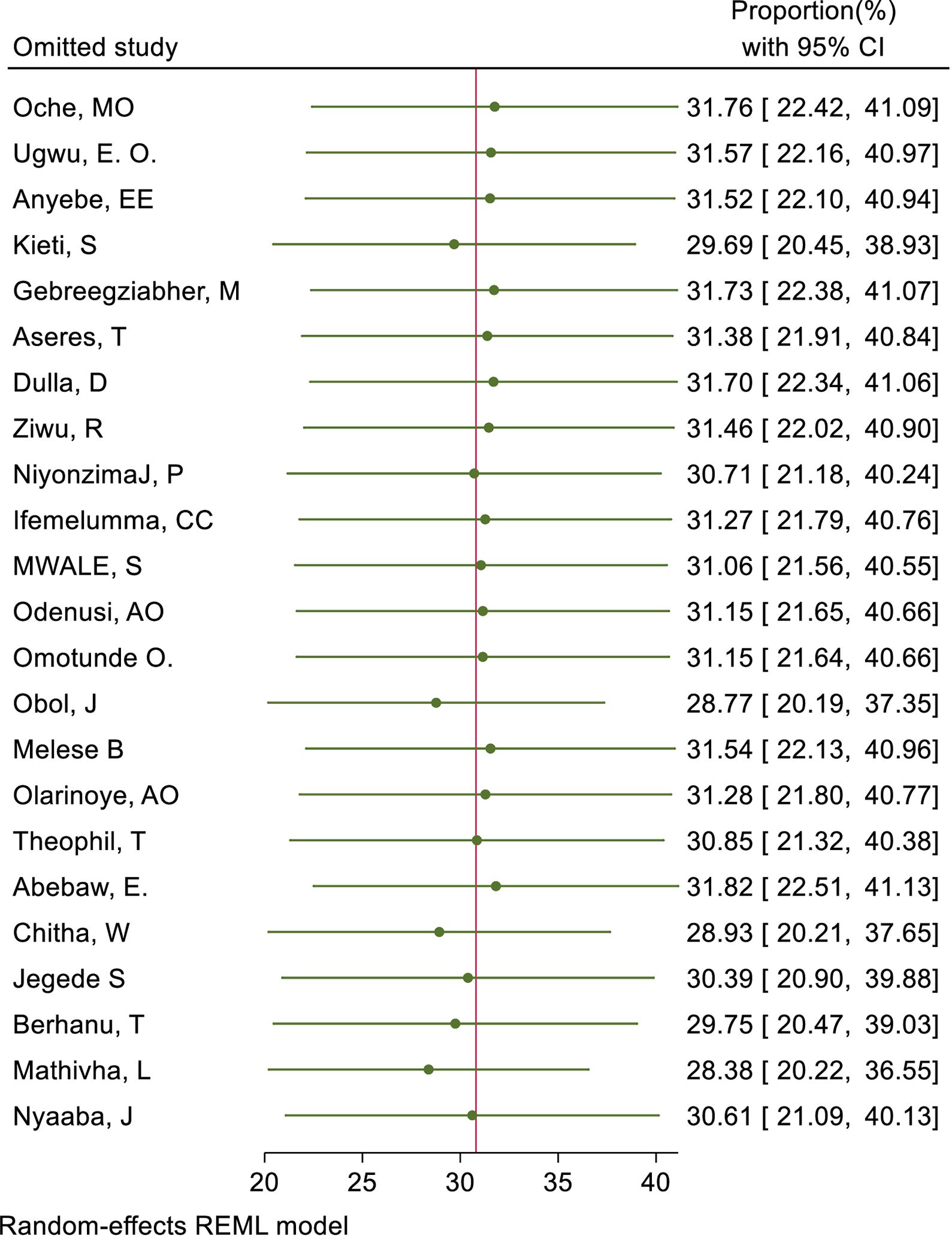
Figure 21. Sensitivity analysis for ever screened practice of female healthcare providers towards cervical cancer in Sub Sahara Africa, 2023.
Meta-regression
Besides, trim and fill analysis for publication bias, meta-regression analysis was performed by considering sample size and publication year for the included studies to identify sources of bias for the pooled prevalence. We included a total of 9 studies (34, 35, 47–50, 64, 66, 67) for attitude towards cervical cancer screening and 23 studies (23, 34, 35, 45–49, 53–60, 62, 64–66, 68–70) for the practice of ever being screened for cervical cancer in our meta-regression analysis. In this analysis, the sample size was a statistically significant source of publication bias for the pooled magnitude of attitude status whereas publication year is the source of publication bias for health care providers’ practice to ever screen for cervical cancer as shown in the values from the meta-regression analysis (Table 3).
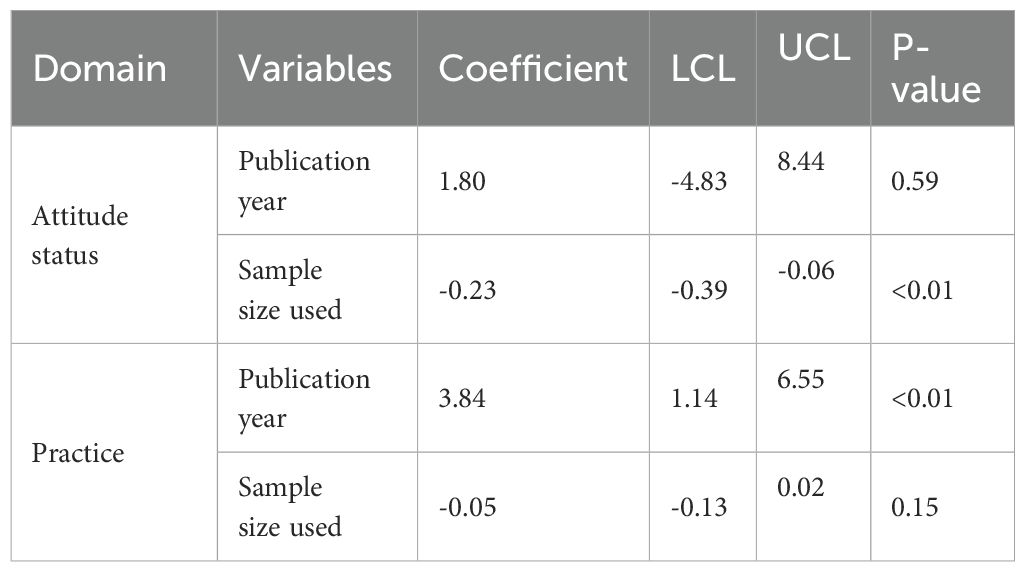
Table 3. Meta-regression of attitude and practice of cervical cancer screening among health care providers in Sub Saharan Africa, 2023.
Discussion
The World Health Assembly aimed to reduce cervical cancer through a 90-70-90 policy, but healthcare providers in sub-Saharan Africa had significant gaps in their knowledge, attitude, and practice towards cervical cancer and its screening. The results of this meta-analysis showed that the pooled magnitude of good knowledge status and positive attitude of healthcare providers towards cervical cancer was 67.93% (95% CI: 53.36–82.50) and 55.26% (95% CI: 34.28–76.23)respectively. This implied that healthcare providers do not have adequate knowledge and a positive attitude towards cervical cancer. This pooled magnitude of knowledge was consistent with 80% in Saudi Arabia (72) and 75.15% in India (73) and it was lower as compared to 92% in Pakistan (74). On the other hand, the pooled magnitude of positive attitudes towards cervical cancer screening was lower as compared to 78% in Pakistan (74). The possible explanation for these discrepancy in the magnitude of knowledge and attitudes towards cervical cancer could results from variations in training, workload, resource limitations, and cultural beliefs within the specific environments being studied. These factors may contribute to the observed differences in understanding and behaviors among individuals.
This review also found that the overall level of good knowledge, positive attitude, and practice of cervical cancer screening among healthcare providers was 49.68% (95% CI: 33.18–66.17), 66.3% (95% CI: 50.36–82.89), and 30.785% (95% CI: 21.68–39.88), respectively. The statement suggests that healthcare providers in sub-Saharan Africa have limited knowledge, attitude, and practice towards cervical cancer screening despite the fact that they are expected to serve as examples for eligible women who should undergo such screening. The overall magnitude of knowledge status towards cervical cancer screening was consistent with overall knowledge of 60.4% in Egypt (75) and 56.3% in China (76). However, it was lower as compared to 86.2% in India (73). Moreover, the overall magnitude of positive attitude status towards cervical cancer screening was also consistent with 53.4% in Egypt (75) but it was lower as compared to 85.47% in India (73) and 90% in Turkey (30). This discrepancy in healthcare providers’ knowledge and attitude towards cervical cancer screening could be attributed to differences in their specialization, experiences, and professional competency levels of health professionals included in their sample. These differences may also be influenced by variations in training and education provided to healthcare professionals in different countries. The limited access to screening services and lack of emphasis on cervical cancer screening in the study location may contribute to this discrepancy, which could be further influenced by variations in access to screening services and information dissemination.
The findings of this study regarding the overall practice of female healthcare providers who had been screened for cervical cancer in Sub-Saharan Africa was consistent with 12.7% in India (73), 26.2% in Saudi Arabia (77), and 26.6% in Sri Lankan (78). The result was not significantly different from a systematic review and meta-analysis conducted on women of reproductive age in Sub-Saharan Africa, where the percentage was 12.87% (79). But it was lower as compared with 42.2% in Qatar (80) and 45.2% in south Turkey (81). This variation might be justified by the extent of the studies and differences in the health service, sociodemographic characteristics of study participants, and setting and study period.
Female healthcare providers reported various reasons for not being screened for cervical cancer, including fear of embarrassment, fear of pain, lack of time, fear of positive outcomes, fear of privacy, lack of availability of services, carelessness, fear of using dirty or rusty equipment, lack of approval from their husbands, cultural and religious beliefs, thinking they are not susceptible to the disease, high costs, feeling healthy, and lack of access to services. This suggests that individuals who perceive themselves as healthy often overlook preventive services, and a lack of awareness about cervical cancer screening contributes to low utilization of these services. This finding was supported by a previous study conducted in India (82) and in Korea (83).
This review also found that 72.02% of healthcare providers know about pap smears as a way to screen for cervical cancer. Around 46.15% are aware of the HPV DNA test as a screening method, while 41.68% know about VIA and 35.54% know about VILI. Additionally, 30.18% are aware of both pap smears and VIA, and 23.92% are aware of either VIA or VILI as screening methods for cervical cancer. Healthcare providers in Sub-Saharan Africa are more knowledgeable and experienced in using pap smears for cervical cancer screening compared to other methods like VIA, VILI, or HPV tests. This is because pap smears have been widely used in healthcare facilities in the region. About 27.34% of healthcare providers were aware of the regular interval for cervical cancer screening. this finding is low as comparable with 39% in Pakistan (74). This difference could be explained by the variations in the sociodemographic characteristics of the study participants and the disparities quality of training they received.
A systematic review in Sub-Saharan Africa found that the COVID-19 pandemic has led to disruptions in cervical cancer screening, diagnosis, and treatment services due to factors such as transportation limitations, staff shortages, and patients’ fears of contracting the virus. To address these challenges, telemedicine and virtual platforms have been utilized for patient consultations and follow-ups during the pandemic in the region (84).
Strengths and limitations of the study
The strengths of this review include being the first to examine the knowledge, attitude, and practice of health providers in sub-Saharan Africa regarding cervical cancer screening. Additionally, the review followed PRISMA guidelines and incorporated both published and unpublished research. However, a limitation of the review is that only studies written in English were included in the review.
Conclusions and recommendation
The level of knowledge, attitude, and practice of cervical cancer screening among healthcare providers in Sub-Saharan Africa was suboptimal. Healthcare providers need to take an active role in promoting women’s health and preventing disease. This involves ensuring that healthcare professionals are knowledgeable about cervical cancer and its screenings, as well as having a positive outlook towards screening and being screened themselves. It is important to educate healthcare providers about misconceptions regarding cervical cancer screening and to increase awareness of the availability of these services in various centers across the country. Given the impact that their knowledge, attitude and practice can have on a large number of clients, it is imperative that swift action be taken. This could include providing training to participants to enhance their understanding, influence their beliefs, and encourage more individuals to utilize screening services. These efforts will help reduce the occurrence of cervical cancer among high-risk women. Hence, Policymakers as well as program implementers need to enhance the level of knowledge, attitude status, and screening habits of healthcare providers towards cervical cancer. Thus, healthcare providers should be role models for all other women for those services delivered to patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
AD: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. EB: Conceptualization, Data curation, Supervision, Visualization, Writing – original draft, Writing – review & editing. TA: Conceptualization, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MT: Conceptualization, Data curation, Investigation, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. EF: Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. DE: Formal analysis, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. HE: Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing. OA: Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. AT: Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. NK: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We gratefully thank the primary authors of the included studies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CIl, Confidence interval; HPV, Human Papilloma Virus Infection; OR, Odds Ratio; PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analysis; VIA, Visual Inspection with Acetic acid; VILI, Visual Inspection Lugol’s Iodine.
References
1. Genomics B. Empowering women's health: BGI Genomics Global 2023 state of cervical cancer awareness report. (2023).
2. Prabhu M, Eckert LO. Development of World Health Organization (WHO) recommendations for appropriate clinical trial endpoints for next-generation Human Papillomavirus (HPV) vaccines. Papillomavirus Res. (2016) 2:185–9. doi: 10.1016/j.pvr.2016.10.002
3. De Vuyst H, Alemany L, Lacey C, Chibwesha CJ, Sahasrabuddhe V, Banura C, et al. The burden of human papillomavirus infections and related diseases in sub-saharan Africa. Vaccine. (2013) 31:F32–46. doi: 10.1016/j.vaccine.2012.07.092
4. Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, et al. ICO/IARC information centre on HPV and cancer (HPV information centre). Human papillomavirus and related diseases in the world Summary Report. (2019) 17(6).
5. Cohen PA, Jhingran A, Oaknin A, Denny L. Cervical cancer. Lancet. (2019) 393:169–82. doi: 10.1016/S0140-6736(18)32470-X
6. Zhang S, Xu H, Zhang L, Qiao Y. Cervical cancer: Epidemiology, risk factors and screening. Chin J Cancer Res. (2020) 32:720. doi: 10.21147/j.issn.1000-9604.2020.06.05
7. Wang Z, Wang J, Fan J, Zhao W, Yang X, Wu L, et al. Risk factors for cervical intraepithelial neoplasia and cervical cancer in Chinese women: large study in Jiexiu, Shanxi Province, China. J Cancer. (2017) 8:924. doi: 10.7150/jca.17416
8. Rerucha CM, Caro RJ, Wheeler VL. Cervical cancer screening. Am Family physician. (2018) 97(7):441–8.
9. Organization WH, Health WHOR, Diseases WHOC, Promotion H. Comprehensive cervical cancer control: a guide to essential practice. World Health Organization (2006).
10. Rodríguez AC, Schiffman M, Herrero R, Wacholder S, Hildesheim A, Castle PE, et al. Rapid clearance of human papillomavirus and implications for clinical focus on persistent infections. J Natl Cancer Institute. (2008) 100:513–7. doi: 10.1093/jnci/djn044
11. Bosch FX, Manos MM, Muñoz N, Sherman M, Jansen AM, Peto J, et al. Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. Obstet Gynecol Surv. (1995) 50:725–7. doi: 10.1097/00006254-199510000-00015
12. Louie KS, De Sanjose S, Mayaud P. Epidemiology and prevention of human papillomavirus and cervical cancer in sub-Saharan Africa: a comprehensive review. Trop Med Int Health. (2009) 14:1287–302. doi: 10.1111/j.1365-3156.2009.02372.x
13. Elfström KM, Herweijer E, Sundström K, Arnheim-Dahlström L. Current cervical cancer prevention strategies including cervical screening and prophylactic human papillomavirus vaccination: a review. Curr Opin Oncol. (2014) 26:120–9. doi: 10.1097/CCO.0000000000000034
14. Bristow RE, Chang J, Ziogas A, Campos B, Chavez LR, Anton-Culver H. Impact of National Cancer Institute Comprehensive Cancer Centers on ovarian cancer treatment and survival. J Am Coll Surg. (2015) 220:940–50. doi: 10.1016/j.jamcollsurg.2015.01.056
15. Koliopoulos G, Nyaga VN, Santesso N, Bryant A, Martin-Hirsch PP, Mustafa RA, et al. Cytology versus HPV testing for cervical cancer screening in the general population. Cochrane Database Syst Rev. (2017) 2017(8). doi: 10.1002/14651858.CD008587.pub2
16. Othman S, Darus F, Arshad R. The influence of coercive isomorphism on corporate social responsibility reporting and reputation. Soc Responsibility J. (2011) 7:119–35. doi: 10.1108/17471111111114585
17. Cuhls KE. Horizon Scanning in Foresight–Why Horizon Scanning is only a part of the game. Futures Foresight Sci. (2020) 2:e23. doi: 10.1002/ffo2.23
18. Devine D, Gaskell J, Jennings W, Stoker G. Trust and the coronavirus pandemic: What are the consequences of and for trust? An early review of the literature. Political Stud Rev. (2021) 19:274–85. doi: 10.1177/1478929920948684
19. Khan MJ, Werner CL, Darragh TM, Guido RS, Mathews C, Moscicki A-B, et al. ASCCP colposcopy standards: role of colposcopy, benefits, potential harms, and terminology for colposcopic practice. J Low Genit Tract Dis. (2017) 21:223–9. doi: 10.1097/LGT.0000000000000338
20. Cruz CT. Usos conceptuales del género y la vulnerabilidad en políticas públicas de atención al Virus del Papiloma Humano (VPH) y al Cáncer Cervicouterino (CaCu) en México. Saúde em Debate. (2022) 46:318–30. doi: 10.1590/0103-1104202213305
21. Organization WH. Global strategy to accelerate the elimination of cervical cancer as a public health problem. World Health Organization (2020).
22. Organization WH. WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention: supplemental material: GRADE evidence-to-recommendation tables and evidence profiles for each recommendation. World Health Organization (2013).
23. Ifemelumma C, Anikwe C, Okorochukwu B, Onu F, Obuna J, Ejikeme B, et al. Cervical cancer screening: assessment of perception and utilization of services among health workers in low resource setting. Int J Reprod Med. (2019) 2019:6505482. doi: 10.1155/2019/6505482
24. American Cancer Society. Cancer facts & Figures 2019. Atlanta, Ga: American Cancer Society (2019).
25. American Cancer Society. Cancer prevention & Early detection facts & Figures 2019-2020. Atlanta, Ga: American Cancer Society (2019).
26. Leung SS, Leung I. Cervical cancer screening: knowledge, health perception and attendance rate among Hong Kong Chinese women. Int J women's Health. (2010) 2010:221–8. doi: 10.2147/IJWH
27. Pierz AJ, Randall TC, Castle PE, Adedimeji A, Ingabire C, Kubwimana G, et al. A scoping review: Facilitators and barriers of cervical cancer screening and early diagnosis of breast cancer in Sub-Saharan African health settings. Gynecol Oncol Rep. (2020) 33:100605. doi: 10.1016/j.gore.2020.100605
28. Randall TC, Ghebre R. Challenges in prevention and care delivery for women with cervical cancer in sub-Saharan Africa. Front Oncol. (2016) 6:160. doi: 10.3389/fonc.2016.00160
29. Adedimeji A, Ajeh R, Pierz A, Nkeng R, Ndenkeh JJ, Fuhngwa N, et al. Challenges and opportunities associated with cervical cancer screening programs in a low income, high HIV prevalence context. BMC women's Health. (2021) 21:1–14. doi: 10.1186/s12905-021-01211-w
30. Soylar P, Özer A, Doğan Yüksekol Ö, Ulucan M. Knowledge, attitude, and practice regarding cancer screening tests among health workers in a university hospital in Turkey. J Cancer Education. (2020) 35:718–23. doi: 10.1007/s13187-019-01517-2
31. Sumampouw OJ, Nelwan JE, Rumayar AA. Outline Images Download Cite Share Favorites Permissions ORIGINAL ARTICLE Socioeconomic Factors Associated with Diarrhea among Under-Five Children in Manado Coastal Area, Indonesia. (2019).
32. Hweissa NA, Lim JN, Su T. Health-care providers' perceptions, attitudes towards and recommendation practice of cervical cancer screening. Eur J Cancer Care. (2016) 25:864–70. doi: 10.1111/ecc.2016.25.issue-5
33. Gebreegziabher M, Asefa NG, Berhe S. Factors Affecting the Practices of Cervical Cancer Screening among Female Nurses at Public Health Institutions in Mekelle Town, Northern Ethiopia, 2014: A Cross-Sectional Study. J Cancer Res. (2016) 2016:4743075. doi: 10.1155/2016/4743075
34. Anyebe E, Opaluwa S, Muktar H, Philip F. Knowledge and practice of cervical cancer screening amongst nurses in Ahmadu Bello University Teaching Hospital Zaria. Cancer. (2014) 4(27):33–40.
35. Abebaw E, Tesfa M, Gezimu W, Bekele F, Duguma A. Female healthcare providers’ knowledge, attitude, and practice towards cervical cancer screening and associated factors in public hospitals of Northwest Ethiopia. SAGE Open Med. (2022) 10:20503121221095931. doi: 10.1177/20503121221095931
36. Chitha W, Sibulawa S, Funani I, Swartbooi B, Maake K, Hellebo A, et al. A cross-sectional study of knowledge, attitudes, barriers and practices of cervical cancer screening among nurses in selected hospitals in the Eastern Cape Province, South Africa. BMC Women's Health. (2023) 23:94. doi: 10.1186/s12905-023-02251-0
37. Arulogun OS, Maxwell OO. Perception and utilization of cervical cancer screening services among female nurses in University College Hospital, Ibadan, Nigeria. Pan Afr Med J. (2012) 11(1).
38. Alamneh Y, Adane F, Yirga T, Desta M. Essential newborn care utilization and associated factors in Ethiopia: a systematic review and meta-analysis. BMC pregnancy childbirth. (2020) 20:1–9. doi: 10.1186/s12884-020-2804-7
39. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
40. Rendina-Gobioff G. Detecting publication bias in random effects meta-analysis: An empirical comparison of statistical methods. (2006).
41. Kossmeier M, Tran US, Voracek M. Visual inference for the funnel plot in meta-analysis. Zeitschrift für Psychologie. (2019). doi: 10.1027/2151-2604/a000358
42. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. bmj. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
43. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 1994:1088–101. doi: 10.2307/2533446
44. Ndizeye Z, Vanden Broeck D, Vermandere H, Bogers JP, Van Geertruyden JP. Knowledge and practices of general practitioners at district hospitals towards cervical cancer prevention in Burundi, 2015: a cross-sectional study. Global Health. (2018) 14:4. doi: 10.1186/s12992-018-0321-5
45. NiyonzimaJ P, MatabelleL B, Ntasumbumuyange D, Rulisa S. Cervical cancer prevention knowledge and attitudes: Survey of midwives and nurses in Rwanda. Int J Cancer Tremnt. (2018) 1(1):30–4.
46. Kieti SN. Knowledge, attitude and practices on cervical cancer screening and prevention methods among nurses at two Nairobi hospitals in Kenya. submitted in accordance with the requirements for the degree of master of arts in nursing science at the university of south Africa. (2016).
47. Gebreegziabher M, Asefa NG, Berhe S. Factors Affecting the Practices of Cervical Cancer Screening among Female Nurses at Public Health Institutions in Mekelle Town, Northern Ethiopia, 2014: A Cross‐Sectional Study. J Cancer Res. (2016) 2016(1):4743075.
48. Berhanu T, Mamo E, Tewolde T, Beshir M. Knowledge of cervical Cancer and its screening practice among health extension Workers in Addis Ababa, Ethiopia. Prim Health Care. (2019) 9(1):1–5.
49. Melese Bekele A. Utilization of cervical cancer screening service and associated factors among female health workforces in public health institutions in bale zone. South East Ethiopia: HU (2021).
50. Ararsa T, Tadele N, Ayalew Y, Gela D. Knowledge towards cervical cancer screening and associated factors among urban health extension workers at Addis Ababa, Ethiopia: facility based cross-sectional survey. BMC cancer. (2021) 21:1–9. doi: 10.1186/s12885-021-07952-z
51. Getahun F, Addissie A, Negash S, Gebremichael G. Assessment of cervical cancer services and cervical cancer related knowledge of health service providers in public health facilities in Addis Ababa, Ethiopia. BMC Res Notes. (2019) 12:675. doi: 10.1186/s13104-019-4701-6
52. Addissie A. College Of Healthscience School Of Public Health Assessment Of Knowledge And Attitude Of Cervical Cancer And Screening Among Primary Health Care Workers Of West Wollega Zone, Ethiopia, 2016. ADDIS ABABA UNIVERSITY (2016).
53. Theophil T, Balandya B, Kunambi P, Wangwe PJ, August F. Knowledge, utilization, challenges and factors associated with cervical cancer screening among female doctors and nurses at a tertiary hospital in Tanzania: A cross sectional study. (2022). doi: 10.21203/rs.3.rs-2136119/v1
54. Obol JH, Lin S, Obwolo MJ, Harrison R, Richmond R. Knowledge, attitudes, and practice of cervical cancer prevention among health workers in rural health centres of Northern Uganda. BMC cancer. (2021) 21:1–15. doi: 10.1186/s12885-021-07847-z
55. Dulla D, Daka D, Wakgari N. Knowledge about cervical cancer screening and its practice among female health care workers in southern Ethiopia: a cross-sectional study. Int J Women's Health. (2017) 9:365–72. doi: 10.2147/IJWH
56. Aseres T. Knowledge, practice and associated factors of cervical cancer screening among women health workers in Gondar University teaching and referral hospital. Gondar, Ethiopia: University of Gondar (2016).
57. Oche M, Kaoje A, Gana G, Ango J. Cancer of the cervix and cervical screening: Current knowledge, attitude and practices of female health workers in Sokoto, Nigeria. Int J Med Med Sci. (2013) 5(4):184–90.
58. Ziwu R. Cervical cancer knowledge and screening behaviors amongst female health professionals in some selected health facilities in the La Nkwantanang Madina Municipality in the Greater Accra Region of Ghana. Ensign Global College (2017).
59. Odenusi A, Oladoyin V, Asuzu M. Uptake of cervical cancer screening services and its determinants between health and non-health workers in Ibadan, south-Western Nigeria. Afr J Med Med Sci. (2020) 49(4):573–84.
60. Olarinoye A, Shiru M, Ubom A, Olabinjo A, Abdul I, Ijarotimi O, et al. Knowledge, attitude and uptake of pap smear among female healthcare professionals in a Nigerian teaching hospital. Ann Health Res. (2021) 7:391–402. doi: 10.30442/ahr.0704-07-149
61. Ogunsuyi GO, Ademuyiwa IY, Anorkuru R. Awareness and utilization of cervical cancer screening among primary health care workers in ilesa, osun state. Int J Nursing Midwife Health Related Cases. (2022) 8:39–52. doi: 10.37745/ijnmh.15
62. Nyaaba JA, Akurugu E. Knowledge, barriers and uptake towards Cervical Cancer screening among female health workers in Ghana: A perspective of the Health Belief Model. Int J Afr Nurs Sci. (2023) 19:100587. doi: 10.1016/j.ijans.2023.100587
63. Logbo-Akey KE, Ajavon DR, M’bortche KB, Kambote PY, Patidi KN, Aboubakari AS. Cervical cancer screening by midwives in the kara region of northern Togo: knowledge, attitudes and practices. Open J Obstet Gynecol. (2022) 12:140–6. doi: 10.4236/ojog.2022.122014
64. Jegede Solomon O, Christianah O, Ogun FO. Attitude and uptake of cervical cancer screening among female health care workers in ogbomoso, oyo state.
65. Ugwu E, Obi S, Ezechukwu P, Okafor I, Ugwu A. Acceptability of human papilloma virus vaccine and cervical cancer screening among female health-care workers in Enugu, Southeast Nigeria. Niger J Clin Pract. (2013) 16(2):249–52.
66. Omotunde OI, Amosu Ademola M. Knowledge, perception and cervical cancer screening practices among female nurses working in healthcare facilities in Lagos State, Nigeria. Pharmacology. (2020) 1(1):74–92.
67. Shayo FS. Knowledge, Attitudes and Practices (KAP) on cervical cancer screening health care workers in Oshikoto region. Namibia: University of Namibia (2018).
68. Mathivha L, Ramathuba DU, Maputle MS. Factors affecting participation in cervical screening by female nurses in public health institutions in vhembe district, limpopo province. Nurs Rep. (2023) 13:424–35. doi: 10.3390/nursrep13010039
69. Chitha W, Sibulawa S, Funani I, Swartbooi B, Maake K, Hellebo A, et al. A cross-sectional study of knowledge, attitudes, barriers and practices of cervical cancer screening among nurses in selected hospitals in the Eastern Cape Province, South Africa. BMC Women's Health. (2023) 23:1–12. doi: 10.1186/s12905-023-02251-0
70. Mwale S. Assessment of knowledge on cervical cancer and utilization of cervical cancer screening services among female nurses at Solwezi General Hospital in Zambia. (2020).
71. Ndizeye Z, Vanden Broeck D, Vermandere H, Bogers JP, Van Geertruyden J-P. Knowledge and practices of general practitioners at district hospitals towards cervical cancer prevention in Burundi, 2015: a cross-sectional study. Globalization Health. (2018) 14:1–8. doi: 10.1186/s12992-018-0321-5
72. Aldarmahi A, Alzahrani H, Alqutub S, Alzahrani F. Exploring the attitudes and practices of female doctors towards cervical cancer screening in primary health care centers. J Med Life. (2023) 16:773. doi: 10.25122/jml-2022-0344
73. Chawla B, Taneja N, Awasthi AA, Kaur KN, Janardhanan R. Knowledge, attitude, and practice on screening toward cervical cancer among health professionals in India—A review. Women's Health. (2021) 17:17455065211017066. doi: 10.1177/17455065211017066
74. Syed S. A Survey of Cervical Cancer and Pap Smear Awareness and Utilization of Pap smear test among female health care providers in a Secondary Care Hospital, Pakistan. J Soc Obstetricians Gynaecologists Pakistan. (2018) 8(3):143–7.
75. Mohamed ML, Tawfik AM, Mohammed GF, Elotla SF. Knowledge, attitude, and practice of cervical cancer screening, and HPV vaccination: A cross-sectional study among obstetricians and gynecologists in Egypt. Maternal Child Health J. (2022) 26:565–74. doi: 10.1007/s10995-021-03352-8
76. Di J-L, Song B, Rutherford S, Wu J-L, Ma L, Chen J-Y, et al. Knowledge of cervical cancer screening among health care workers providing services across different socio-economic regions of China. Asian Pacific J Cancer Prev. (2016) 17(6):2965–72.
77. Heena H, Durrani S, AlFayyad I, Riaz M, Tabasim R, Parvez G, et al. Knowledge, Attitudes, and Practices towards Cervical Cancer and Screening amongst Female Healthcare Professionals: A Cross-Sectional Study. J Oncol. (2019) 2019:5423130. doi: 10.1155/2019/5423130
78. Nilaweera R, Perera S, Paranagama N, Anushyanthan A. Knowledge and practices on breast and cervical cancer screening methods among female health care workers: a Sri Lankan experience. Asian Pacific J Cancer Prev. (2012) 13:1193–6. doi: 10.7314/APJCP.2012.13.4.1193
79. Yimer NB, Mohammed MA, Solomon K, Tadese M, Grutzmacher S, Meikena HK, et al. Cervical cancer screening uptake in Sub-Saharan Africa: a systematic review and meta-analysis. Public Health. (2021) 195:105–11. doi: 10.1016/j.puhe.2021.04.014
80. Alali A, Salem M, Elmahdi H, Alkubaisi N, Alwahedi Z, Taher M, et al. Knowledge, attitudes and practices regarding cervical cancer screening among female health care workers in primary healthcare in Qatar. World Family Med Journal: Incorporating Middle East J Family Med. (2016) 99:1–12. doi: 10.5742/MEWFM.2016.92809
81. Coskun S, Can H, Turan S. Knowledge about cervical cancer risk factors and pap smear testing behavior among female primary health care workers: a study from south Turkey. Asian Pacific J Cancer Prev. (2013) 14:6389–92. doi: 10.7314/APJCP.2013.14.11.6389
82. Khatuja R, Mittal S, Asthana U, Verma M, Kadian M. Knowledge and practice of cervical cancer screening in general population and medical personnel: A gap to be bridged. Asian J Med Sci. (2022) 13(2):61–4. doi: 10.3126/ajms.v13i2.40582
83. Tran NT, Taylor R, Choe SI, Pyo HS, Kim OS, So HC. Knowledge, attitude and practice (KAP) concerning cervical cancer and screening among rural and urban female healthcare practitioners in the Democratic People’s Republic of Korea. Asian Pac J Cancer Prev. (2011) 12(11):3023–8.
Keywords: cervical cancer screening, healthcare provider, knowledge, attitude, practice, sub-Saharan Africa
Citation: Delie AM, Bogale EK, Anagaw TF, Tiruneh MG, Fenta ET, Endeshaw D, Eshetu HB, Adal O, Tareke AA and Kebede N (2024) Healthcare providers’ knowledge, attitude, and practice towards cervical cancer screening in Sub-Saharan Africa: systematic review and meta-analysis. Front. Oncol. 14:1436095. doi: 10.3389/fonc.2024.1436095
Received: 21 May 2024; Accepted: 30 July 2024;
Published: 19 August 2024.
Edited by:
Maria Paula Curado, A.C.Camargo Cancer Center, BrazilReviewed by:
Fawaz D. Alshammari, University of Hail, Saudi ArabiaAna Afonso, NOVA University of Lisbon, Portugal
Copyright © 2024 Delie, Bogale, Anagaw, Tiruneh, Fenta, Endeshaw, Eshetu, Adal, Tareke and Kebede. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amare Mebrat Delie, YW1hcmVtZWJyYXQyQGdtYWlsLmNvbQ==
 Amare Mebrat Delie
Amare Mebrat Delie Eyob Ketema Bogale
Eyob Ketema Bogale Tadele Fentabel Anagaw
Tadele Fentabel Anagaw Misganaw Guadie Tiruneh
Misganaw Guadie Tiruneh Eneyew Talie Fenta
Eneyew Talie Fenta Destaw Endeshaw4
Destaw Endeshaw4 Habitu Birhan Eshetu
Habitu Birhan Eshetu Ousman Adal
Ousman Adal Abiyu Abadi Tareke
Abiyu Abadi Tareke Natnael Kebede
Natnael Kebede