- 1Department of Nursing, Shanghai Proton and Heavy Ion Center, Fudan University Cancer Hospital, Shanghai, China
- 2Shanghai Key Laboratory of Radiation Oncology, Shanghai, China
- 3Shanghai Engineering Research Center of Proton and Heavy Ion Radiation Therapy, Shanghai, China
Objective: To retrieve, extract, integrate and evaluate evidence on the rehabilitation of dysphagia in patients undergoing radiotherapy for head and neck cancer (HNC), and to provide a basis for the development of a rehabilitation management protocol for dysphagia in patients undergoing radiotherapy for HNC.
Methods: An evidence-based systematic search of the literature related to the rehabilitation of dysphagia in patients with HNC during radiotherapy was conducted from January 2013 to March 2023, and the corresponding evaluation tools were selected according to the different types of literature for quality evaluation. “The Joanna Briggs Institute (JBI) evidence pre-grading system was used to evaluate the quality of the evidence.
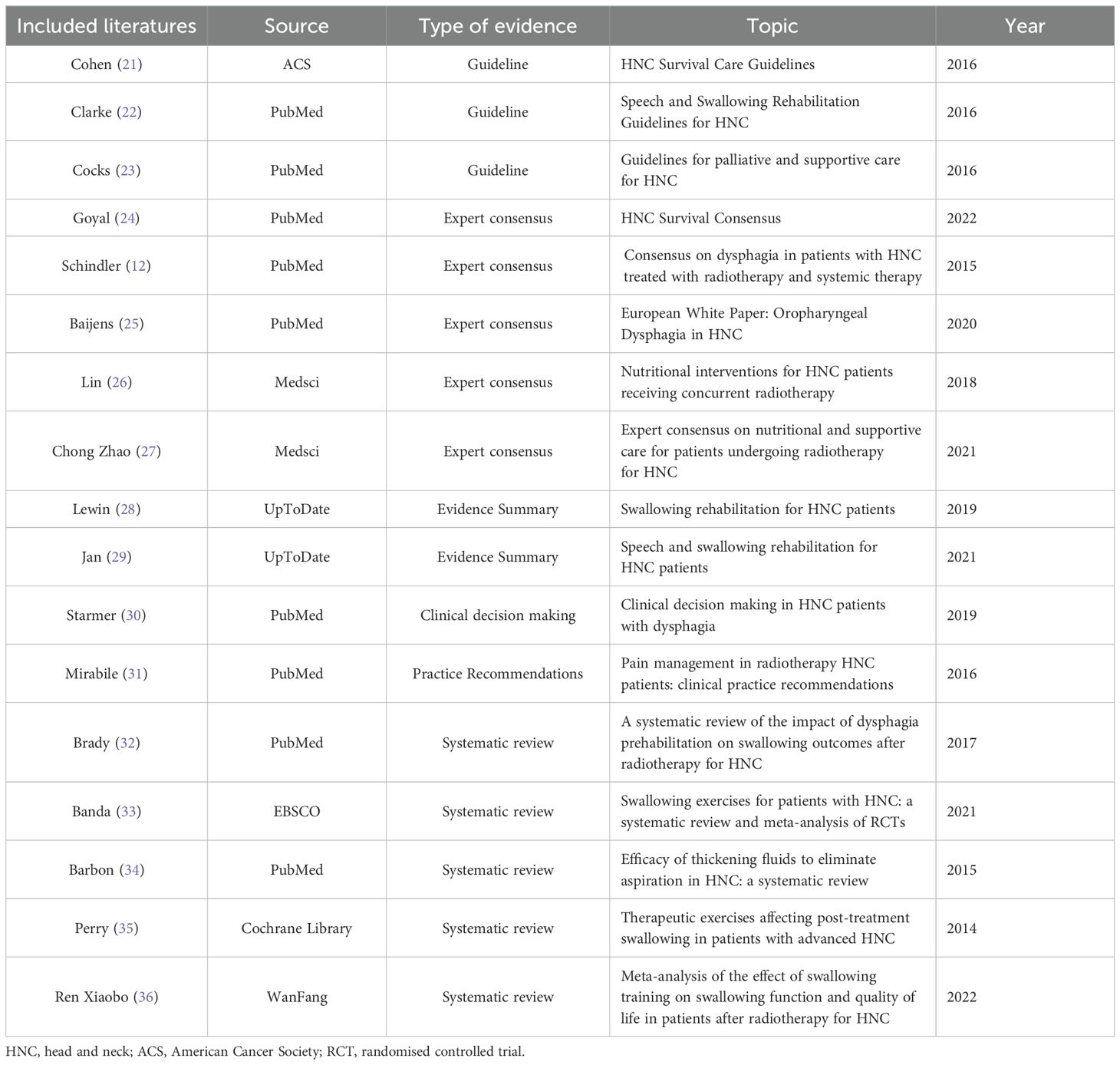
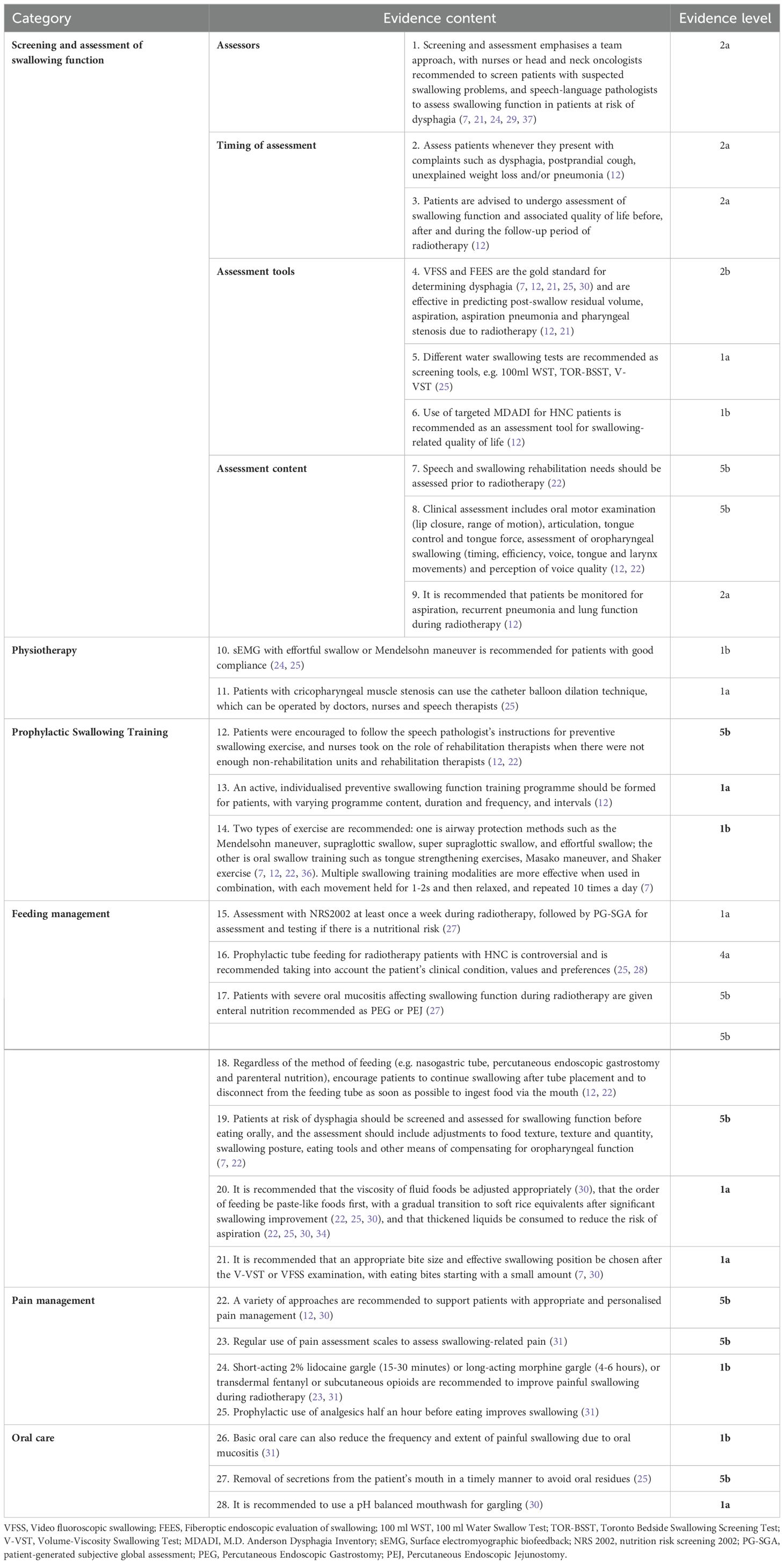
Results: A total of 17 articles were included, including 3 guidelines, 5 expert articles, 1 clinical decision, 1 practice recommendation, 2 evidence summaries and 5 systematic evaluations. A final total of 28 pieces of evidence were summarised, including 6 areas of swallowing disorder screening and assessment, physiotherapy, preventive swallowing function training, feeding management, pain control, and oral care.
Conclusion: This study forms a multidisciplinary collaborative evidence summary for the rehabilitation management of dysphagia in patients undergoing radiotherapy for HNC, but the application of some of the evidence needs to be carried out in the context of the clinical setting and patient-specific circumstances for the rehabilitation evidence selected for patients’ dysphagia to improve their swallowing function and their swallowing-related quality of life and reduce the occurrence of related complications.
Introduction
Head and neck cancer (HNC) refers to malignant tumours that occur in the area from the base of the skull to the supraclavicular and anterior cervical spine, including the neck, otorhinolaryngology and oral and maxillofacial parts (1), and it is currently the sixth most common malignant tumour and the seventh most common cause of tumour-related death worldwide (2). Radiotherapy serves as the sole treatment modality for early-stage head and neck tumors and plays a crucial role in the management of advanced-stage cases, where it is often combined with surgery or concurrent chemotherapy (3). Dysphagia is a common adverse effect due to radiotherapy for HNC (4). It is a process in which the patient is unable to effectively transport food into the stomach due to impaired structure and/or function of the jaw, tongue and lips, soft palate and pharynx (5). Approximately 30% to 80% of HNC patients can develop varying degrees of dysphagia after conventional radiotherapy (6–8), and also have adverse consequences including malnutrition, reduced psychosocial functioning, aspiration and aspiration pneumonia, and poor social participation and quality of life, which cause great harm to patients (9–11). The mechanism of dysphagia during radiotherapy is different from that of central nervous system damage in stroke patients. In HNC, many factors affect the structure and function of the swallowing organs, such as mucosal damage, pain, dry mouth due to irradiation, or muscle and soft tissue fibrosis and cricopharyngeal muscle narrowing as treatment progresses, resulting in decreased swallowing function (12, 13). The current state of fragmented and inadequate research, both domestically and internationally, hinders rapid access to comprehensive, scientific rehabilitation guidance for healthcare professionals. While domestic expert consensus on dysphagia is primarily used to guide stroke patients, there is limited evidence regarding the practice of rehabilitation management of dysphagia due to radiotherapy in HNC patients. To address this gap, our study will adopt an evidence-based approach to systematically search, collate, and summarize the evidence on the mechanism of dysphagia during radiotherapy in HNC patients. The goal is to provide scientific and effective evidence for the rehabilitation of swallowing function during radiotherapy in HNC patients, which is crucial for improving their quality of life.
Materials and methods
Retrieval strategy
The search was top-down according to the “6S” pyramid model and was based on a combination of free words and subject terms. English search terms “ ‘head and neck’ OR nasopharynx OR oropharynx OR larynx OR mouth OR hypopharynx” AND “tumor OR cancer OR neoplasm OR malignancy OR carcinoma” AND “dysphagia OR ‘deglutition disorder’ OR ‘swallowing disorder’ “ AND “care OR rehabilitation OR exercise OR physical therapy OR physical activity OR nursing”; Computer searches BMJ Best Practice, Up To Date, National Institute for Health and Clinical Excellence (NICE),Guidelines International Network(GIN), National Guideline Clearinghouse (NGC), Registered Nurses’ Association of Ontario (RNAO), Scottish Intercollegiate Guidelines Network (SIGN), Guidelines International Network(GIN), New Zealand Guidelines Group (NZGG), National Health and Medical Research Council (NHMRC), American Cancer Society (ACS), WHO Guidelines, China Guideline Clearinghouse (CGC), National Comprehensive Cancer Network (NCCN), Oncology Nursing Society (ONS), Medsci etc. guide network, and PubMed, Web of Science, CINAHL, Embase, Joanna Briggs Institute (JBI), Cochrane library, China Biology Medicine disc (CBM), China National Knowledge Infrastructure (CNKI), Wanfang Database etc. comprehensive database. The literature was searched for publications from January 2013 to March 2023. In addition, the references of the selected literature were searched for articles that contained expert consensus, evidence summaries, and best practice articles on swallowing rehabilitation for HNC patients during radiotherapy.
Literature inclusion and exclusion criteria
Inclusion criteria were determined according to the evidence-based questions constructed by PIPOST: (i) the population to which the evidence was applied was HNC patients undergoing radiotherapy; (ii) the study content was rehabilitation measures for dysphagia; (iii) the implementers of the evidence were nurses, doctors, rehabilitation workers, nutritionists and other health promoters; (iv) the outcome indicators were swallowing function, nutritional status and swallowing-related quality of life; (v) the places where the evidence was applied were wards, rehabilitation centres and the community; (vi) the types of studies were guidelines, expert consensus, practice recommendations, clinical decision-making, evidence summaries, and systematic evaluations; (vii) the literature was published in Chinese or English. Exclusion criteria: (i) guidelines interpreted or directly translated; (ii) literature type was review; (iii) literature with incomplete information or full text not available; (iv) literature that has been updated; (v) duplicate publications.
Literature screening and data extraction
Two researchers with systematic evidence-based training and experience in head and neck oncology independently screened the literature for inclusion and exclusion criteria by reviewing the titles, abstracts, and full texts. They extracted basic information and data from the selected studies and cross-checked the results. Any discrepancies were resolved through discussion with a third researcher to reach a consensus.
Literature quality evaluation
Two researchers, who are Master’s students trained in a systematic evidence-based program at Fudan University, independently evaluated and graded the quality of evidence for inclusion. If any disagreements arise, a third investigator, who is a PhD candidate with extensive clinical and research experience, was sought to participate in decision-making and proofread the translation of the English evidence. 1) Guidelines: Guidelines were evaluated using the Appraisal of Guidelines for Research and Evaluation II (AGREE II) (14), which includes six domains: scope objectives, personnel involved, and development rigor, with 23 entries each representing a score of 1-7 from “strongly disagree” to “strongly agree”. Scores were standardized to the highest possible percentage of scores in the domain. 2) Expert consensus: the evaluation criteria developed by the JBI Center for Evidence-Based Health Care in its 2016 edition was used (15), which included six entries to label sources of opinion, reference to other literature, and state conclusions (16). 3) Clinical decision: evaluation was performed using an evaluation tool (critical appraisal for summaries of evidence, CASE) (17). 4) Practice recommendations, evidence summary: the original literature supporting their evidence was traced and evaluated for quality using the appropriate evaluation tool based on the type of literature. 5) Systematic reviews or Meta-analysis: the quality of the evaluation was assessed using the Assessment of Multiple Systematic Reviews (AMSTAR) tool (18), which includes 11 entries for evaluating evidence-based questions, search strategy, literature quality assessment, data extraction and synthesis, as well as publication bias (19).
Evidence extraction, integration and evaluation
The content analysis method was used to extract evidence from the literature, which included general characteristics, research themes, and main contents of the literature. When evidence from different sources had complementary or consistent conclusions, a combined or general expression was used. However, if there were conflicting evidence from different sources, the principles of evidence-based priority, high-quality evidence priority, and latest published authoritative literature priority were followed. We graded the aggregated evidence using the Joanna Briggs Institute (JBI) Levels of Evidence and Grades of Recommendation system (2014 version) (20) from the Australian JBI Centre for Evidence-Based Healthcare. This system categorizes the evidence into five levels, from high to low, based on the study design of the included literature.
Results
General characteristics of included literatures
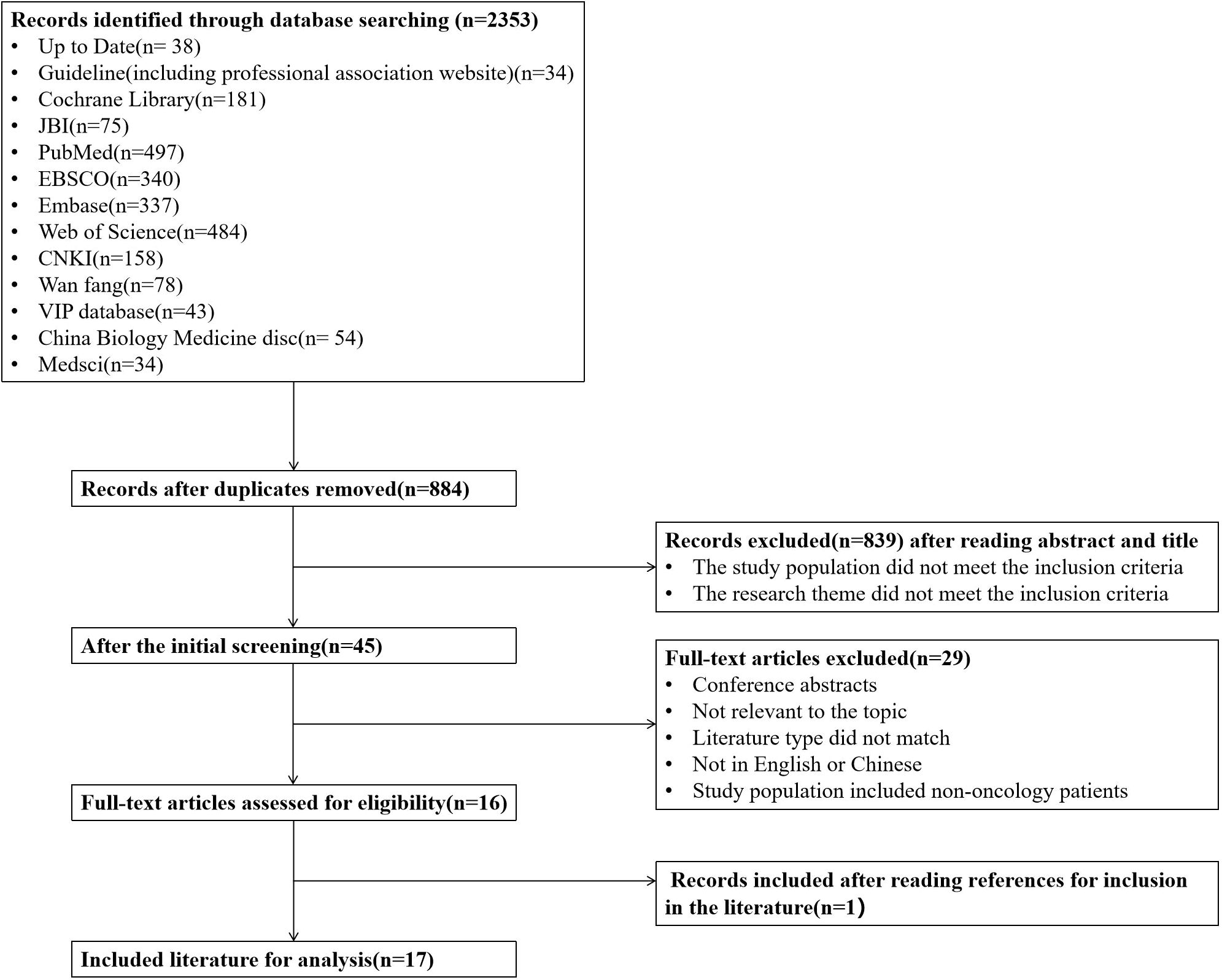
An initial search yielded a total of 2,353 articles, which were reduced to 1,469 after removing duplicates. Following a review of titles, abstracts, and full texts to eliminate non-compliant literature, 16 articles were included in the study, consisting of 3 guidelines, 5 expert consensus articles, 2 evidence summaries, 1 clinical decision, and 5 systematic reviews. One clinical practice recommendation for managing painful swallowing due to radiation oral mucositis was also extracted based on the topics covered and references cited in the included literature. In total, 17 articles were ultimately included. Table 1 provides an overview of the basic characteristics of the literature included, while Figure 1 shows a flowchart detailing the literature screening process.
Quality evaluation results of the included literature
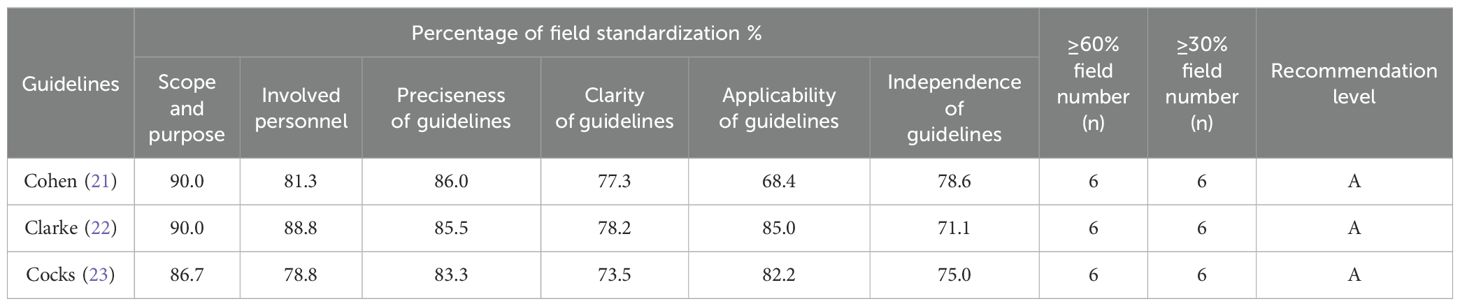
Quality evaluation results of the guidelines
Three guidelines were included in this study. The guidelines were evaluated using AGREE II and the results are shown in Table 2, all with a recommendation level of A. The overall quality was high and inclusion was granted.
Quality evaluation results of expert consensuses
Five expert consensus articles were included in this study. The quality evaluation criteria were evaluated using the JBI Center for Evidence-Based Health Care (2016) expert consensus evaluation criteria (15), and all entries were rated as “yes” and were included for overall high quality.
Quality evaluation results of clinical decision
One clinical decision was included in this study and was evaluated using the quality assessment tool CASE (17). The study by Starmer et al. (30) was evaluated as “partially yes” for “whether potential bias was avoided” and “yes” for the rest of the entries, which was of good overall quality and was included.
Quality evaluation results of practice recommendations and evidence summary
One practice recommendation and two evidence summaries were included in this study, which were evaluated for quality according to the type of primary literature using the appropriate evaluation tool. The overall quality was good and was included.
Quality evaluation results of systematic reviews
Five systematic reviews were included in this study and evaluated using the AMSTAR tool (18). In the study by Banda et al. (33), “Was a pre-design protocol provided?” was evaluated as “unclear”, while all other entries were evaluated as “yes”. In the study by Perry et al. (35), “Is a list of included and excluded studies provided?” was evaluated as “unclear” and the rest of the entries were evaluated as “yes”. In the study of Barbon et al. (34), “Do the inclusion criteria include the publication status of the literature, e.g. grey literature?”, “Do the conclusions drawn reasonably take into account the methodological quality of the included studies?”, “Was the potential for publication bias assessed” were evaluated as “unclear” and “Were the essential characteristics of the included studies described?” was evaluated as “no”, the rest of the evaluation results were “yes”. In the study by Brady et al. (32), all the entries were “yes” except “Is the method of combining results appropriate?” was evaluated as “no”. All the evaluation entries of the study by Ren et al. (36) were evaluated as “yes”, with high overall quality.
Summary and description of evidence
The evidence related to the 17 included literature will be extracted and summarised by this research team and discussed by two clinical nursing experts and two postgraduate students in clinical practice, resulting in a synthesis of evidence from six areas of swallowing function screening and assessment, physiotherapy, preventive swallowing function training, feeding management, pain control and oral care, resulting in 28 pieces of evidence, with the aim of providing healthcare professionals with better guidance for HNC patients Swallowing function exercises to prevent or alleviate dysphagia provide an evidence-based basis in Table 3.
Discussion
This study provides evidence-based evidence on dysphagia to facilitate the rehabilitation of dysphagia in HNC patients undergoing radiotherapy by maximising the role of care. This study summarises the evidence related to swallowing rehabilitation for HNC patients undergoing radiotherapy in six areas: screening and assessment of dysphagia, physiotherapy, preventive swallowing function training, feeding management, pain control, and oral care, which may provide some guidance for patients’ clinical practice.
Dysphagia screening and assessment facilitates early identification and management of swallowing function
Guidelines and consensus developed in different countries have successively provided recommendations on who should be screened and assessed for dysphagia, the purpose, timing and tools to facilitate early identification and management of dysphagia. The main aim of screening is to identify those at risk of dysphagia and to determine whether further investigations are needed (38). Therefore, it is generally recommended that nurses complete the screening of patients suspected of having swallowing problems, and other professionals may also be involved. It is also recommended that patients at risk of dysphagia should be referred to a speech and language therapist for a detailed swallowing assessment as soon as possible (7, 21, 24, 29, 37). Currently, several guidelines and consensus recommendations recommend the video fluoroscopic swallowing screening (VFSS) and fiberoptic endoscopic evaluation of swallowing (FEES) as the gold standard for the diagnosis of dysphagia (7, 12, 21, 25, 30). Although they are effective in predicting the onset of dysphagia in patients, they are costly, time-consuming and difficult to implement clinically (12, 38). Therefore, it should be clear what the purpose of the examination is with the intended message and it should not be misused. Researchers both domestically and internationally are continually seeking simpler and more convenient scales and assessment methods for screening and evaluating dysphagia. However, compared to the objective results obtained from patients who undergo FEES and VFSS, the sensitivity, specificity, and predictive values of subjective scales and other screening methods remain insufficient (12). Among the available screening tools, the M.D. Anderson Dysphagia Inventory (MDADI) is a relatively practical subjective dysphagia screening tool and is specifically designed for assessing swallowing-related quality of life in HNC patients, which is currently its primary application. However, the optimal method for screening dysphagia in HNC patients is yet to be determined.
Physiotherapy methods for dysphagia are an effective way to improve dysphagia
Physiotherapy is commonly used to improve the physiological function of swallowing muscles in HNC patients who are undergoing radiotherapy, with the goal of achieving safe and effective swallowing. The most evidence-based physiotherapy treatments recommended by guidelines or consensus include surface electromyographic biofeedback (sEMG) training combined with catheter balloon dilation techniques (24, 25). sEMG training helps to enhance the strength and coordination of swallowing muscles under the guidance of a speech-language pathologist, and there is strong evidence that combined swallowing training is more effective (24, 25, 39). The catheter balloon dilation technique is a safe and reliable method to improve stenosis of the cricopharyngeal muscle caused by irradiation during radiotherapy, and can be performed by head and neck physicians, nurses, and speech-language pathologists (25, 39). While hand-held inductive electrical stimulation can also be used as an adjunct to swallowing therapy in radiotherapy patients, it is not widely available (39). Therefore, selection of appropriate physiotherapy treatment for dysphagia in HNC patients undergoing radiotherapy should be guided by professionals and based on the appropriate mechanism for this specific population.
Prophylactic swallowing training facilitates the rehabilitation of swallowing function
Prophylactic swallowing training is a method to enhance the strength and coordination of muscle groups and improve the physiological function of swallowing. It enhances the strength of swallowing-related muscles and prevents the occurrence of dysphagia or reduces the severity of dysphagia by strengthening the control of jaw, lip and tongue movements, and soft palate and vocal cord closure movements (40, 41). Currently, rehabilitation functional training referred to in guideline and consensus relies heavily on specialist speech-language pathology (12, 22), with nurses often playing their role in non-rehabilitation units, less developed areas and where there are insufficient rehabilitation practitioners (39). Although prophylactic swallowing training is recommended in a number of guidelines and consensus studies, the content and efficacy of prophylactic swallowing training programmes for patients have not been standardised in current meta-analyses and systematic evaluations. Therefore, more studies with large samples of high-quality randomized controlled trials are needed (33, 35).
Feeding management helps improve swallowing function and swallowing-related quality of life for patients
Nutrition is a primary concern for patients with dysphagia, and maintaining oral feeding has been shown to improve swallowing function and quality of life (42, 43). Some research suggests that nutritional support or prophylactic gastrostomy may benefit HNC patients undergoing treatment, whether or not chemotherapy is involved (12), use of these interventions should be based on the patient’s clinical status, values, and preferences (28). If a patient experiences severe oral mucositis that interferes with eating, enteral nutrition is often recommended to improve feeding (27). It is important to encourage patients to continue swallowing both before and after feeding tube placement, regardless of the method used (such as nasogastric tube, percutaneous endoscopic gastrostomy and parenteral nutrition) (12, 22).
Effective feeding management for patients with dysphagia requires consideration not only of the amount of nutrition, but also the method of food delivery, the nature of the food, and meal preparation (22). The national expert consensus recommends establishing a nutritional management team that includes a professional dietitian to screen patients for malnutrition risk during radiotherapy and whenever dysphagia is indicated. Additionally, compensatory oropharyngeal function, such as adjusting food properties, swallowing posture, and eating tools, is considered an important aspect of swallowing rehabilitation for patients who are able to swallow (7, 22). However, selection of appropriate food properties and swallowing posture for patients with dysphagia should be based on clinical and instrumental assessment (7, 30). Therefore, it is important to select evidence-based interventions tailored to the individual swallowing profile and preferences of HNC patients undergoing radiotherapy, to ensure safe and effective food intake and improve overall nutrition.
Pain control helps maintain the patient’s normal swallowing process
For HNC patients during radiotherapy, mucosal and surrounding tissue pain in the irradiated area has a major impact on the patient’s swallowing process and compliance with swallowing function training (30). Some guidelines and consensus suggest that patients with dysphagia should be supported with appropriate and individualised pain management to reduce mucosal pain and maintain a normal swallowing process (12, 23), while disuse atrophy and fibrosis can be reduced and long-term swallowing function optimised (31). However, current guidelines and consensus do not give adequate recommendations for dysphagia due to mucosal pain in patients; therefore, this study was supplemented with evidence on the management of swallowing pain in HNC patients treated with radiotherapy by searching relevant reference searches of the included literature (31). Evidence 22 to 25 supplemented the evidence on the management of painful swallowing mainly in terms of pain assessment, timing of medication administration and basic oral care.
Oral care helps to improve the safety and effectiveness of patients’ swallowing and improves their swallowing efficiency
Many HNC patients often experience sensory loss during radiotherapy due to mucosal and submucosal damage, resulting in inadequate cleaning of oral secretions and food debris. Consensus and clinical decision states that enhanced oral care can reduce the risk of aspiration of oral secretions and aspiration pneumonia (30, 39), while reducing the frequency and extent of painful swallowing and improving patients’ swallowing efficiency (31). Evidence recommends the use of pH-balanced mouthwashes for gargling in HNC patients during radiotherapy (30). Current recommendations for oral care for HNC patients with dysphagia during radiotherapy are inadequate and lack diversity, and it is recommended that more high-quality studies be conducted in the future to provide more reliable and targeted oral care options for patients.
Conclusion
This study summarises the evidence on the rehabilitation management of HNC patients during radiotherapy and provides a reference for improving swallowing function, nutritional status and swallowing-related quality of life. The etiology and mechanisms of dysphagia during radiotherapy for HNC patients are complex, and there are geographical and cultural differences in the evidence across countries and regions in terms of ethnicity, values and healthcare delivery systems.
Author contributions
YZ (1st author): Data curation, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. HW: Methodology, Writing – original draft, Writing – review & editing. YZ (3rd author): Writing – original draft, Writing – review & editing. SW: Data curation, Methodology, Writing – original draft. MZ: Data curation, Methodology, Writing – original draft. XL: Formal analysis, Methodology, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Health Science and Technology Project (PW2022D-10) of the Shanghai Pudong New Area Health Commission and the Fudan University Fuxing Nursing Research Fund Project (FNF202204).
Acknowledgments
We are grateful to the Fudan University library for providing us with databases and facilitating access to the literatures.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
HNC, head and neck cancer; AGREE II, Appraisal of Guidelines for Research and Evaluation II; CASE, critical appraisal for summaries of evidence,; AMSTAR, Assessment of Multiple Systematic Reviews; ACS, American Cancer Society; VFSS, Video fluoroscopic swallowing; FEES, Fiberoptic endoscopic evaluation of swallowing; 100 ml WST, 100 ml Water Swallow Test; TOR-BSST, Toronto Bedside Swallowing Screening Test; V-VST, Volume-Viscosity Swallowing Test; MDADI, M.D. Anderson Dysphagia Inventory; sEMG, Surface electromyographic biofeedback; NRS 2002, nutrition risk screening 2002; PG-SGA, patient-generated subjective global assessment; PEG, Percutaneous Endoscopic Gastrostomy; PEJ, Percutaneous Endoscopic Jejunostomy.
References
1. Lydiatt WM, Patel SG, O'Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, et al. Head and neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA: A Cancer J Clin. (2017) 67(2):122–37. doi: 10.3322/caac.21389
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin. (2021) 71(3):209–49. doi: 10.3322/caac.21660
3. Crowder SL, Douglas KG, Pepino MY, Sarma KP, Arthur AE. Nutrition impact symptoms and associated outcomes in post-chemoradiotherapy head and neck cancer survivors: A systematic review. J Cancer Survivorship. (2018) 12(4):479–94. doi: 10.1007/s11764-018-0687-7
4. Wang X, Eisbruch A. IMRT for head and neck cancer: Reducing xerostomia and dysphagia. J Radiat Res. (2016) 57(Suppl 1):i69–i75. doi: 10.1093/jrr/rrw047
5. Dou Z, Lan Y, Wan GF, Xie MQ. Assessment and treatment of swallowing disorders. People's Medical Publishing House (2009).
6. Zhang J, Huang Y, Lan M, Lang JY. Clinical efficacy and prognosis analysis of intensity-modulated radiotherapy for young adult nasopharyngeal carcinoma. Cancer Prev Treat. (2018) 31(2):117–22. doi: 10.3969/j.issn.1674-0904.2018.02.009
7. De Felice F, De Vincentiis M, Luzzi V, Magliulo G, Tombolini M, Ruoppolo G, et al. Late radiation-associated dysphagia in head and neck cancer patients: Evidence, research, and management. Oral Oncol. (2018) 77:125–30. doi: 10.1016/j.oraloncology.2017.12.021
8. Nguyen NP, Moltz CC, Frank C, Vos P, Smith HJ, Karlsson U, et al. Evolution of chronic dysphagia following treatment for head and neck cancer. Oral Oncol. (2006) 42(4):374–80. doi: 10.1016/j.oraloncology.2005.09.003
9. Murphy BA, Gilbert J. Dysphagia in head and neck cancer patients treated with radiation: Assessment, sequelae, and rehabilitation. Semin Radiat Oncol. (2009) 19:35–42. doi: 10.1016/j.semradonc.2008.09.007
10. Nguyen NP, Moltz CC, Frank C, Vos P, Smith HJ, Karlsson U, et al. Dysphagia following chemoradiation for locally advanced head and neck cancer. Ann Oncol. (2004) 15(3):383–8. doi: 10.1093/annonc/mdh101
11. Nund RL, Ward EC, Scarinci NA, Cartmill B, Kuipers P, Porceddu SV. The lived experience of dysphagia following non-surgical treatment for head and neck cancer. Int J Speech-Language Pathol. (2014) 16(3):282–9. doi: 10.3109/17549507.2013.861869
12. Schindler A, Denaro N, Russi EG, Pizzorni N, Bossi P, Merlotti A. Dysphagia in head and neck cancer patients treated with radiotherapy and systemic therapies: Literature review and consensus. Crit Rev Oncology/Hematol. (2015) 96(2):372–84. doi: 10.1016/j.critrevonc.2015.06.005
13. Wang JJ, Jiang RS, Yen TT, Liang KL. Risk factors for recurrent pneumonia in post-irradiated patients with nasopharyngeal carcinoma. J Chin Med Assoc. (2017) 80(9):558–62. doi: 10.1016/j.jcma.2017.01.006
14. Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G. AGREE II: Advancing guideline development, reporting, and evaluation in healthcare. Can Med Assoc J. (2010) 182(18):E839–42. doi: 10.1503/cmaj.090449
15. The Joanna Briggs Institute. The Joanna Briggs Institute critical appraisal tools for text and opinion papers. The Joanna Briggs Institute (2017). Available at: https://joannabriggs.org/ebp/critical_appraisal_tools.
16. Gu Y, Zhang HW, Zhou YF, Hu Y, Xing WJ. Methodological quality assessment of the JBI Center for Evidence-Based Health Care’s quality assessment tool on different types of research - systematic evaluation. J Continuing Educ Nurses. (2018) 33(8):701–3. doi: 10.16821/j.cnki.hsjx.2018.08.008
17. Foster MJ, Shurtz S. Making the critical appraisal for summaries of evidence (CASE) for evidence-based medicine (EBM): Critical appraisal of summaries of evidence. J Med Library Assoc. (2013) 101:192–8. doi: 10.3163/1536-5050.101.3.008
18. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Method. (2007) 7(1):10. doi: 10.1186/1471-2288-7-10
19. Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: Methodological development, conduct, and reporting of an umbrella review approach. Int J Evidence-Based Healthcare. (2015) 13(3):132–40. doi: 10.1097/XEB.0000000000000055
20. Wang CHQ, Hu Y. JBI evidence pregrading and evidence recommendation level system (2014 version). J Advanced Pract Nurs. (2015) 30(11):964–7. doi: 10.16821/j.cnki.hsjx.2015.11.002
21. Cohen EE, LaMonte SJ, Erb NL, Beckman KL, Sadeghi N, Hutcheson KA, et al. American Cancer Society head and neck cancer survivorship care guideline. CA: A Cancer J Clin. (2016) 66(3):203–39. doi: 10.3322/caac.21343
22. Clarke P, Radford K, Coffey M, Stewart M. Speech and swallow rehabilitation in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. (2016) 130(S2):S176–80. doi: 10.1017/S0022215116000608
23. Cocks H, Ah-See K, Capel M, Taylor P. Palliative and supportive care in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. (2016) 130(S2):S198–207. doi: 10.1017/S0022215116000633
24. Goyal N, Day A, Epstein J, Goodman J, Graboyes E, Jalisi S, et al. Head and neck cancer survivorship consensus statement from the American Head and Neck Society. Laryngoscope Invest Otolaryngol. (2022) 7(1):70–92. doi: 10.1002/lio2.702
25. Baijens LWJ, Walshe M, Aaltonen L, Arens C, Cordier R, Cras P, et al. European white paper: Oropharyngeal dysphagia in head and neck cancer. Eur Arch Oto-Rhino-Laryngol. (2021) 278(2):577–616. doi: 10.1007/s00405-020-06507-5
26. Lin MC, Shueng PW, Chang WK, Mu-Hsin Chang P, Feng HC, Yang MH, et al. Consensus and clinical recommendations for nutritional intervention for head and neck cancer patients undergoing chemoradiotherapy in Taiwan. Oral Oncol. (2018) 81:16–21. doi: 10.1016/j.oraloncology.2018.03.016
27. China Anti-Cancer Association Oncology Nutrition and Support Committee Oncology Radiotherapy Nutrition Group. Expert consensus on nutrition and supportive treatment for patients undergoing radiotherapy for head and neck cancer. Chin J Radiat Oncol. (2018) 27:1–6. doi: 10.3760/cma.j.issn.1004-4221.2018.01.001
28. Lewin JS, Teng MS, Kotz T. Speech and swallowing rehabilitation of the patient with head and neck cancer. UpToDate (2019). Available online at: https://www.uptodate.com/contents/speech-and-swallowing-rehabilitation-of-the-patient-with-head-and-neck-cancer.
29. Jan S. Speech and swallowing rehabilitation of the patient with head and neck cancer. UpToDate (2021). Available online at: https://www.uptodate.cn/contents/zh-Hans/speech-and-swallowing-rehabilitation-of-the-patient-with-head-and-neck-cancer.
30. Starmer H, Edwards J. Clinical decision making with head and neck cancer patients with dysphagia. Semin Speech Lang. (2019) 40:213–26. doi: 10.1055/s-0039-1688979
31. Mirabile A, Airoldi M, Ripamonti C, Bolner A, Murphy B, Russi E, et al. Pain management in head and neck cancer patients undergoing chemo-radiotherapy: Clinical practical recommendations. Crit Rev Oncology/Hematol. (2016) 99:100–6. doi: 10.1016/j.critrevonc.2015.11.010
32. Brady R, McSharry L, Lawson S, Regan J. The impact of dysphagia prehabilitation on swallowing outcomes post-chemoradiation therapy in head and neck cancer: A systematic review. Eur J Cancer Care. (2022) 31(3):e13549. doi: 10.1111/ecc.13549
33. Banda KJ, Chu H, Kao C, Voss J, Chiu HL, Chang PC, et al. Swallowing exercises for head and neck cancer patients: A systematic review and meta-analysis of randomized control trials. Int J Nurs Stud. (2021) 114:103827. doi: 10.1016/j.ijnurstu.2020.103827
34. Barbon CE, Steele CM. Efficacy of thickened liquids for eliminating aspiration in head and neck cancer: A systematic review. Otolaryngology–Head Neck Surg. (2015) 152:211–8. doi: 10.1177/0194599814556239
35. Perry A, Lee SH, Cotton S, Kennedy C. Therapeutic exercises for affecting post-treatment swallowing in people treated for advanced-stage head and neck cancers. Cochrane Database Systematic Rev. (2014) 2016(8):CD011112. doi: 10.1002/14651858.CD011112.pub2
36. Ren X, Nan F, Tian Z, Li F. Meta-analysis of the effect of swallowing training on swallowing function and quality of life of patients after radiotherapy for head and neck tumors. Chin J Modern Nurs. (2022) 28(29):4038–45. doi: 10.3760/cma.j.cn115682-20220206-00542
37. Nekhlyudov L, Lacchetti C, Davis NB, Garvey TQ, Goldstein DP, Nunnink JC, et al. Head and neck cancer survivorship care guideline: American Society of Clinical Oncology clinical practice guideline endorsement of the American Cancer Society guideline. J Clin Oncol. (2017) 35(14):1606–21. doi: 10.1200/JCO.2016.71.8478
38. China Swallowing Disorders Rehabilitation Assessment and Treatment Expert Consensus Group. Expert consensus on the assessment and treatment of swallowing disorders in China (2017 edition). Chin J Phys Med Rehabil. (2017) 12:881–92. doi: 10.3760/cma.j.issn.0254-1424.2017.12.001
39. China Expert Consensus Group on Assessment and Treatment of Swallowing Disorder Rehabilitation. Expert consensus on the assessment and treatment of swallowing disorders in China (2017 edition). Chin J Phys Med Rehabil. (2018) 1:1–10. doi: 10.3760/cma.j.issn.0254-1424.2018.01.001
40. Kulbersh BD, Rosenthal EL, McGrew BM, Duncan RD, McColloch NL, Carroll WR, et al. Pretreatment, preoperative swallowing exercises may improve dysphagia quality of life. Laryngoscope. (2010) 116(6):883–6. doi: 10.1097/01.mlg.0000217278.96901.fc
41. Carroll WR, Locher JL, Canon CL, Bohannon IA, McColloch NL, Magnuson JS. Pretreatment swallowing exercises improve swallow function after chemoradiation. Laryngoscope. (2008) 118(1):39–43. doi: 10.1097/MLG.0b013e31815659b0
42. Barbon CEA, Peterson CB, Moreno AC, Lai SY, Reddy JP, Sahli A, et al. Adhering to eat and exercise status during radiotherapy for oropharyngeal cancer for prevention and mitigation of radiotherapy-associated dysphagia. JAMA Otolaryngology–Head Neck Surgery. (2022) 148(10):956–64. doi: 10.1001/jamaoto.2022.2313
Keywords: head and neck neoplasms, radiotherapy, dysphagia, rehabilitation, evidence summary
Citation: Zhang Y, Wan H, Zhu Y, Wang S, Zheng M and Li X (2024) Evidence summary on the rehabilitative management of dysphagia during radiotherapy for head and neck cancer patients. Front. Oncol. 14:1429484. doi: 10.3389/fonc.2024.1429484
Received: 08 May 2024; Accepted: 19 August 2024;
Published: 09 September 2024.
Edited by:
Nerina Denaro, IRCCS Ca ‘Granda Foundation Maggiore Policlinico Hospital, ItalyReviewed by:
Yuri Ueda, Tokyo Medical University Hospital, JapanMaciej Chęciński, Preventive Medicine Center, Poland
Copyright © 2024 Zhang, Wan, Zhu, Wang, Zheng and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongwei Wan, aG9uZ193aHdAYWxpeXVuLmNvbQ==
 Yu Zhang
Yu Zhang Hongwei Wan1,2,3*
Hongwei Wan1,2,3* Shuman Wang
Shuman Wang