Misleading clinical and imaging features in atypical aggressive angiomyxoma of the female vulvovaginal or perianal region: report of three cases and review of the literature
- 1Department of Obstetrics and Gynecology, National Clinical Research Center for Obstetrics and Gynecology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2Key Laboratory of Cancer Invasion and Metastasis (Ministry of Education), Hubei Key Laboratory of Tumor Invasion and Metastasis, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 3Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
By Zhang L, Liu R and Peng J. (2024). Front. Oncol. 14:1373607. doi: 10.3389/fonc.2024.1373607
In the published article, there was an error in Figure 1 as published. The presence of Figure 1B2 can be attributed to an oversight on the part of the authors, who mistakenly included the wrong image. The corrected Figure 1 and its caption Figure 1 "The ultrasound (A1–A10), surgical (B1–B5), and pathological images (C1–C8) of case 1. US: panels (A1–A3) respectively display the median sagittal sections of the transperineal ultrasound in the resting state, maximum contraction state, and maximum Valsalva state of the patient in the lithotomy position preoperatively. In panel (A1), an AAM lesion is observed within the urethrovaginal space; it ascends to the posterior aspect of the bladder in panel (A2) and descends to the vaginal opening in panel (A3) (M represents the AAM lesion). All the lesions appeared as homogeneous hypoechoic masses with well-defined margins. Panels (A4, A5) show the median sagittal sections of perineal ultrasound in the resting state and maximum Valsalva state, respectively, of the patient 7 months post-surgery without any observed lesions. Panels (A6, A8) display the axial planes of HLAM reconstructed by three-dimensional ultrasound in the resting state preoperatively and during the Valsalva maneuver. Panel (A7) displays the axial plane of TUI during the maximum contraction state preoperatively. These axial planes provide information about the size, shape, and location of the AAM lesions. In panel (A6), the lesion is observed protruding posteriorly from behind the urethra toward the vagina; in panel (A7), the lesion has ascended completely above the HLAM; in panel (A8), during the Valsalva maneuver, the lesion descends through the HLAM (M represents an AAM lesion). Panels (A9, A10) demonstrate the axial plane of the HLAM in the resting state and maximum Valsalva state, respectively, 7 months post-surgery for patient without any observed lesions. Surgery: panels (B1, B2) depict the lesion as an oval-shaped mass protruding from the anterior vaginal wall into the vaginal cavity. Panel (B3) displays the completely resected lesion, which is a soft tissue mass measuring 4.0 × 5.0 cm and exhibiting an oval shape with a pink appearance. Panel (B4) displays the lesion upon sectioning, which appears as a gray color with medium soft tissue consistency. Panel (B5) depicts the appearance of the vulva after the procedure has been completed. HE: Panel (C1), at low magnification, shows that the tumor boundary appears indistinct, revealing a myxedema matrix interspersed with thin collagen fibers and blood vessels of varying thickness within the tumor. The tumor exhibits areas of loose and dense cellularity, with spindle cells uniformly scattered in dense regions without apparent organization (HE, ×100). As shown in panel (C2), at high magnification, the tumor cells exhibited a low density and assumed a stellate or fusiform morphology without evident pleomorphism (HE, ×200). IHC: Tumor cells exhibited strong positive staining for desmin in panel (C3) (×100) and panel (C4) (×200), estrogen receptors in panel (C5) (×100) and panel (C6) (×200), and progesterone receptors in panel (C7) (×100) and panel (C8) (×200). US, ultrasonography; U, urethra; M, mass; V, vagina; A, anus; HLAM, hiatus of levator ani muscle; HE, histopathological examination; IHC, immunohistochemistry; AAM, aggressive angiomyxoma; TUI, tomographic ultrasound imaging." appear below.
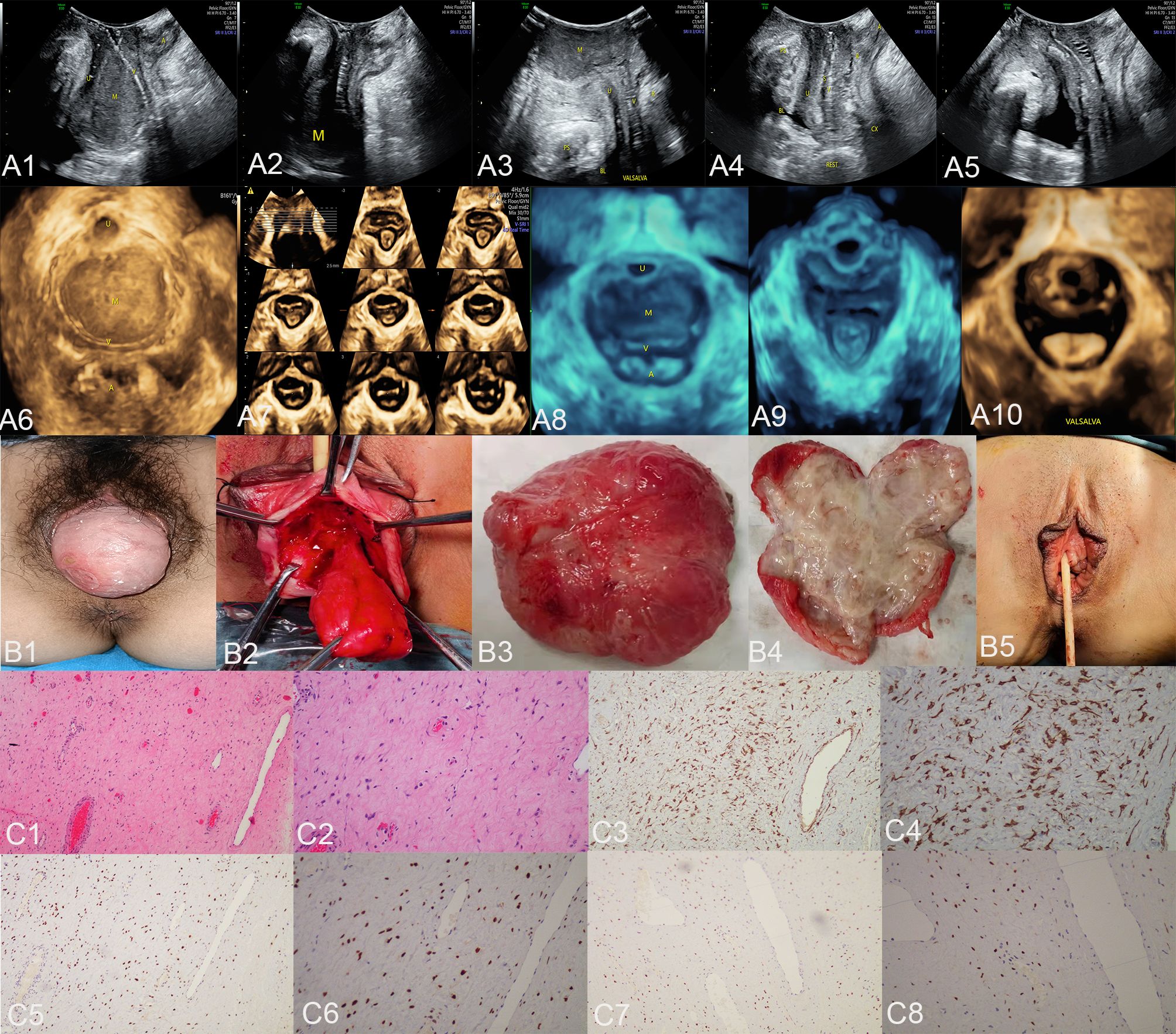
Figure 1 The ultrasound (A1–A10), surgical (B1–B5), and pathological images (C1–C8) of case 1. US: panels (A1–A3) respectively display the median sagittal sections of the transperineal ultrasound in the resting state, maximum contraction state, and maximum Valsalva state of the patient in the lithotomy position preoperatively. In panel (A1), an AAM lesion is observed within the urethrovaginal space; it ascends to the posterior aspect of the bladder in panel (A2) and descends to the vaginal opening in panel (A3) (M represents the AAM lesion). All the lesions appeared as homogeneous hypoechoic masses with well-defined margins. Panels (A4, A5) show the median sagittal sections of perineal ultrasound in the resting state and maximum Valsalva state, respectively, of the patient 7 months post-surgery without any observed lesions. Panels (A6, A8) display the axial planes of HLAM reconstructed by three-dimensional ultrasound in the resting state preoperatively and during the Valsalva maneuver. Panel (A7) displays the axial plane of TUI during the maximum contraction state preoperatively. These axial planes provide information about the size, shape, and location of the AAM lesions. In panel (A6), the lesion is observed protruding posteriorly from behind the urethra toward the vagina; in panel (A7), the lesion has ascended completely above the HLAM; in panel (A8), during the Valsalva maneuver, the lesion descends through the HLAM (M represents an AAM lesion). Panels (A9, A10) demonstrate the axial plane of the HLAM in the resting state and maximum Valsalva state, respectively, 7 months post-surgery for patient without any observed lesions. Surgery: panels (B1, B2) depict the lesion as an oval-shaped mass protruding from the anterior vaginal wall into the vaginal cavity. Panel (B3) displays the completely resected lesion, which is a soft tissue mass measuring 4.0 × 5.0 cm and exhibiting an oval shape with a pink appearance. Panel (B4) displays the lesion upon sectioning, which appears as a gray color with medium soft tissue consistency. Panel (B5) depicts the appearance of the vulva after the procedure has been completed. HE: Panel (C1), at low magnification, shows that the tumor boundary appears indistinct, revealing a myxedema matrix interspersed with thin collagen fibers and blood vessels of varying thickness within the tumor. The tumor exhibits areas of loose and dense cellularity, with spindle cells uniformly scattered in dense regions without apparent organization (HE, ×100). As shown in panel (C2), at high magnification, the tumor cells exhibited a low density and assumed a stellate or fusiform morphology without evident pleomorphism (HE, ×200). IHC: Tumor cells exhibited strong positive staining for desmin in panel (C3) (×100) and panel (C4) (×200), estrogen receptors in panel (C5) (×100) and panel (C6) (×200), and progesterone receptors in panel (C7) (×100) and panel (C8) (×200). US, ultrasonography; U, urethra; M, mass; V, vagina; A, anus; HLAM, hiatus of levator ani muscle; HE, histopathological examination; IHC, immunohistochemistry; AAM, aggressive angiomyxoma; TUI, tomographic ultrasound imaging.
The authors apologize for this error and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: aggressive angiomyxoma, perineal soft tissue mass, vestibular gland cyst, vaginal wall prolapse, ultrasonography, magnetic resonance imaging
Citation: Zhang L, Liu R and Peng J (2024) Corrigendum: Misleading clinical and imaging features in atypical aggressive angiomyxoma of the female vulvovaginal or perianal region: report of three cases and review of the literature. Front. Oncol. 14:1406876. doi: 10.3389/fonc.2024.1406876
Received: 25 March 2024; Accepted: 02 April 2024;
Published: 12 April 2024.
Edited and Reviewed by:
Dragos Eugen Georgescu, Carol Davila University of Medicine and Pharmacy, RomaniaCopyright © 2024 Zhang, Liu and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rong Liu, bGl1cm9uZ2RvY3RvckB0amgudGptdS5lZHUuY24=
 Ling Zhang
Ling Zhang Rong Liu1,2*
Rong Liu1,2*