- 1Graduate Institute of Public Health, China Medical University, Taichung, Taiwan
- 2School of Medicine, Tzu Chi University, Hualien, Taiwan
- 3Department of Neurological Institute, Taichung Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan
- 4Department of Health Services Administration, China Medical University, Taichung, Taiwan
- 5Department of Healthcare Administration, Asia University, Taichung, Taiwan
- 6Department of Medical Research, China Medical University Hospital, China Medical University, Taichung, Taiwan
Introduction: To reduce mortality, the Taiwan government has vigorously promoted free cancer screening and preventive health screening services. Cancers are usually advanced by the time they are discovered in the emergency department. Through this study, we aimed to understand the characteristics of cancer patients diagnosed through the emergency department and thus identify high-risk populations by comparing cancer staging and survival rates in patients diagnosed in the emergency department and those diagnosed in the non-emergency department.
Methods: The retrospective study enrolled a total of 389,043 patients over the age of 20 who were newly diagnosed with one of the five major cancers (including lung cancer, colorectal cancer, breast cancer, prostate cancer, and oral cancer) between 2008 and 2017 and analyzed their diagnostic pathway, cancer stage at diagnosis, and survival time.
Results: Of the study participants, 59,423 patients (about 15.3%) were diagnosed with cancer through the emergency department. We found that a sizable proportion of older people and patients with low education and low incomes were diagnosed through emergency department visits, and those with a health condition comorbidity severity of 3 had the highest proportion diagnosed by the emergency department, advanced stages at diagnosis, and risk of death. These can be classified as high-risk groups. In addition, 76.4% of patients diagnosed in the emergency department had advanced cancer, and the risk of death was 1.46 times higher than that of patients diagnosed in the non-emergency department. Although cancer screening is available, it does not reduce the proportion of patients with advanced cancer who are diagnosed through or at the time of diagnosis in the emergency department.
Conclusions: The present study found that the government’s cancer screening did not affect the proportion or number of cancers diagnosed through emergency department visits. Therefore, the government should focus on more cancer screening, health education in high-risk groups, and strengthening the link between emergency and oncology departments to reduce the risk of death for patients diagnosed through emergency department visits.
Introduction
Cancer has always been a major global health issue. According to the 2021 cancer registry report by the Health Promotion Administration of Taiwan, 121,762 people were newly diagnosed with cancer in 2021, with a crude incidence rate of 520.9 per 100,000 people and an age-standardized incidence of 306.5. The six most common cancers were lung, colorectal, breast, liver, oral, and prostate cancers (1). The 2021 cancer registry report of Taiwan disclosed that the main stages of breast, colorectal, and prostate cancers at diagnosis were stages 0 to 2, while those of lung and oral cancers were stages 3 to 4 (1). Cancer ranks first among the top 10 causes of death in Taiwan. From 2017 to 2021, the 5-year relative survival for the top 10 cancers in Taiwan was 62.1%, including 90.2% for breast cancer, 87.1% for prostate cancer, 64.1% for colorectal cancer, 57.0% for oral cancer, 40.1% for lung cancer, and 36.4% for liver cancer (1). The survival rates of liver cancer and lung cancer were low.
Cancer staging is one of the main factors affecting the survival rate of patients with cancer: the survival rate decreases as the cancer stage increases (2, 3). Early diagnosis and treatment of cancer may significantly improve survival rates (4, 5); therefore, surveilling high-risk groups is important for early cancer diagnosis (6). The Taiwan’s government aimed to reduce cancer mortality and prevent cancer from harming people’s health through early detection and treatment. To this end, the government planned free screening services for the four major cancers (breast, cervical, colorectal and oral cancers). Statistics show that patients who undergo cancer screening have lower cancer staging when diagnosed compared to those who do not undergo screening (7–9). Patients who undergo more screening tests have a higher chance of being diagnosed with early-stage cancer (8).
In addition to being detected through screening, cancer is mostly identified when patients seek medical treatment for symptoms. When patients visit an emergency department with critical symptoms, the severity of their disease can also vary. Research statistics from some countries indicate that most patients diagnosed with cancer through outpatient clinics have early-stage cancer, while most patients diagnosed through the emergency department have advanced cancer with relatively severe symptoms (10–12). Studies have compared differences between patients with cancer diagnosed in outpatient clinics and those diagnosed through emergency departments: the cancer stage of patients diagnosed through emergency departments was found to be more advanced than that of patients diagnosed in outpatient clinics. Moreover, the condition of patients diagnosed with cancer through emergency departments was often life-threatening, and their prognosis was worse than that of patients diagnosed through outpatient clinics (13).
The routes to diagnosis are through outpatient clinics and emergency departments. A study conducted in the United Kingdom used data from the English Cancer Patient Experience Survey in 2010 to analyze 4,647 emergency cases with 18 different cancers. The researchers determined that 1,349 (29%) patients diagnosed with cancer had no cancer-related outpatient medical records (11). The prognosis of patients diagnosed with cancer through the emergency department was worse than that of patients diagnosed through the outpatient clinic. For example, the cancer stage of colorectal, lung, breast, and prostate cancers in patients diagnosed through the emergency department is more advanced than that of the same cancers diagnosed through the outpatient clinic (10). Analysis of cancer diagnosis cases through the emergency department showed that 30% of patients were diagnosed with stage 4 cancer; of those patients diagnosed with cancer through the emergency department, 33%, 32%, 59%, and 39% of patients were diagnosed with stage 4 breast, colorectal, lung, and prostate cancers, respectively (13).
Breast, colorectal, lung, prostate, and oral cancers are five of the top six cancers in Taiwan. To date, in Taiwan, no studies have explored the difference in cancer stage and survival between patients diagnosed in outpatient clinics and those diagnosed in the emergency department. Therefore, in the current study, the probability and risks of diagnosis of the five major cancers in Taiwan through outpatient clinics and emergency departments were analyzed. The differences in cancer stage and related factors for mortality risks were also compared between routes to diagnosis, and the differences in routes to diagnosis and cancer stage at diagnosis were compared between the presence and absence of a free cancer screening policy. These findings may serve as a reference for formulating future cancer prevention strategies.
Methods
Data sources
This study adopts a retrospective cohort study design. The data for this study was obtained from the Taiwan cancer registry files (managed by the Health Promotion Administration) for the period 2008 to 2017, which were used to recruit research participants, their cancer stage at diagnosis, and date of diagnosis. We also associate this data with the National Health Insurance Research Database (NHIRD), the cause of death file of the Ministry of Health and Welfare, and household registration data from 2006 to 2018 to obtain the route to diagnosis, personal characteristics, economic status, environmental factors, health status, cancer treatment, characteristics of the main medical institutions, and mortality of the participants. Diagnose cancer according to the third edition of the International Classification of Oncology Diseases (ICD-O-3), which identifies cancer categories according to the primary site, histology, behavior code, and classification. All cancer diagnosis dates were based on the cancer registry file records. The NHIRD consists of all medical records, including outpatients, emergency department (ED) visits, and inpatient records. Since the cancer registry file does not provide all cancer patient medical records, we need to link the cancer registry file to the National Health Insurance Research Database, which provides all medical records for all patients in Taiwan. The outpatient and ED medical records were obtained from “the Outpatient Care Files,” and the inpatient medical records were obtained from “the Inpatient Care Files” in the NHIRD.
Study population
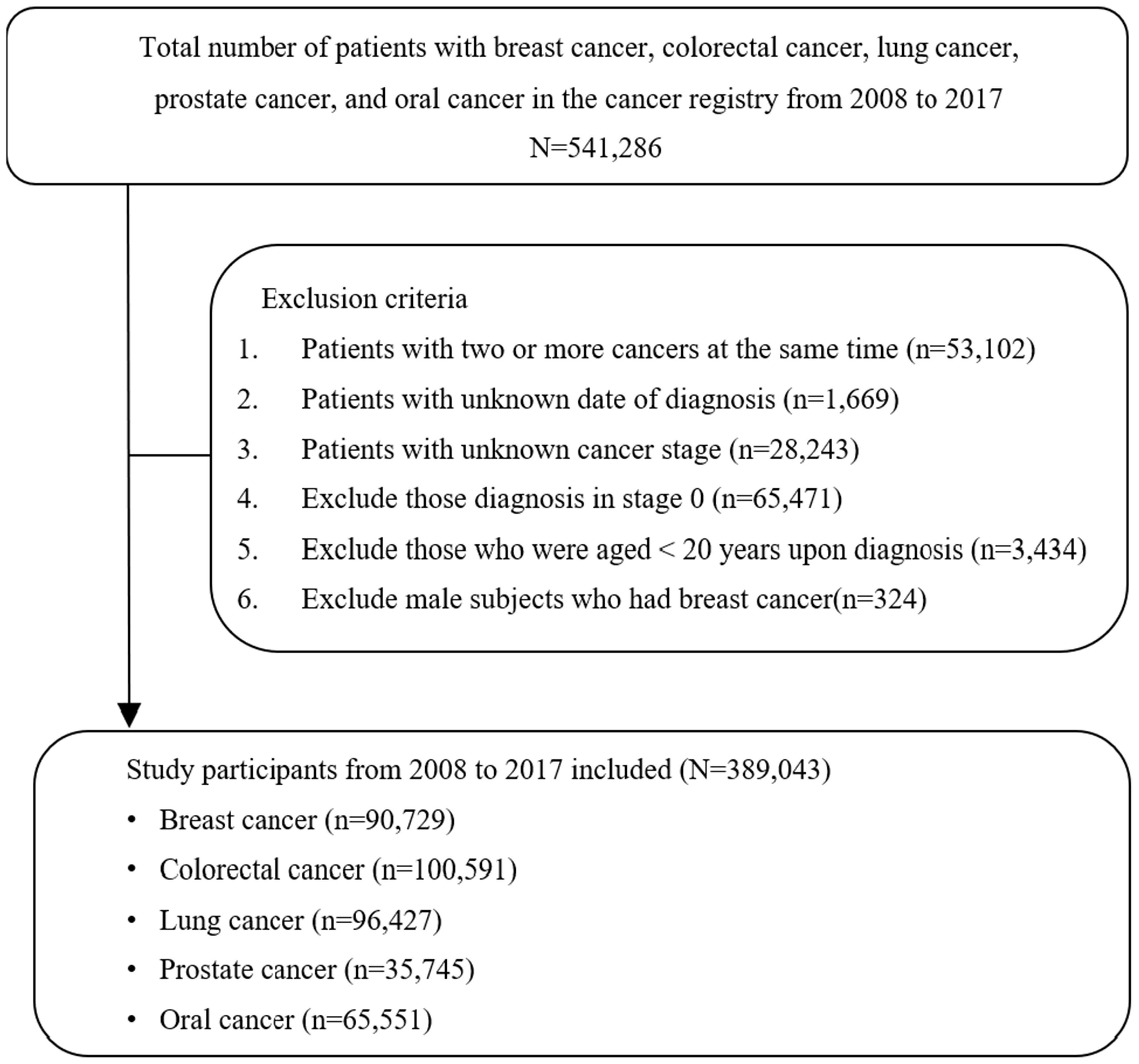
This study focused on patients aged ≥20 years old who were newly diagnosed with one of the five major cancers between 2008 and 2017, including female breast cancer (ICD-O-3 is C50), colorectal cancer (ICD-O-3 is C18-C21), lung cancer (ICD-O-3 is C33-C34), prostate cancer (ICD-O-3 is C61), and oral cancer (ICD-O-3 is C00-C14). In total, 541,286 patients were diagnosed with the five cancers during the study period. After excluding patients who had two or more cancers simultaneously, unknown cancer stage at diagnosis, stage 0, and incomplete data for research variables, a total of 389,043 participants were included in the analysis. Among them, 90,729 patients had breast cancer, 100,591 had colorectal cancer, 96,427 had lung cancer, 35,745 had prostate cancer, and 65,551 had oral cancer. The detailed research participant enrollment process is shown in Figure 1. The cancer-relevant diagnosis codes were listed in the Supplementary Appendix.
Study variables
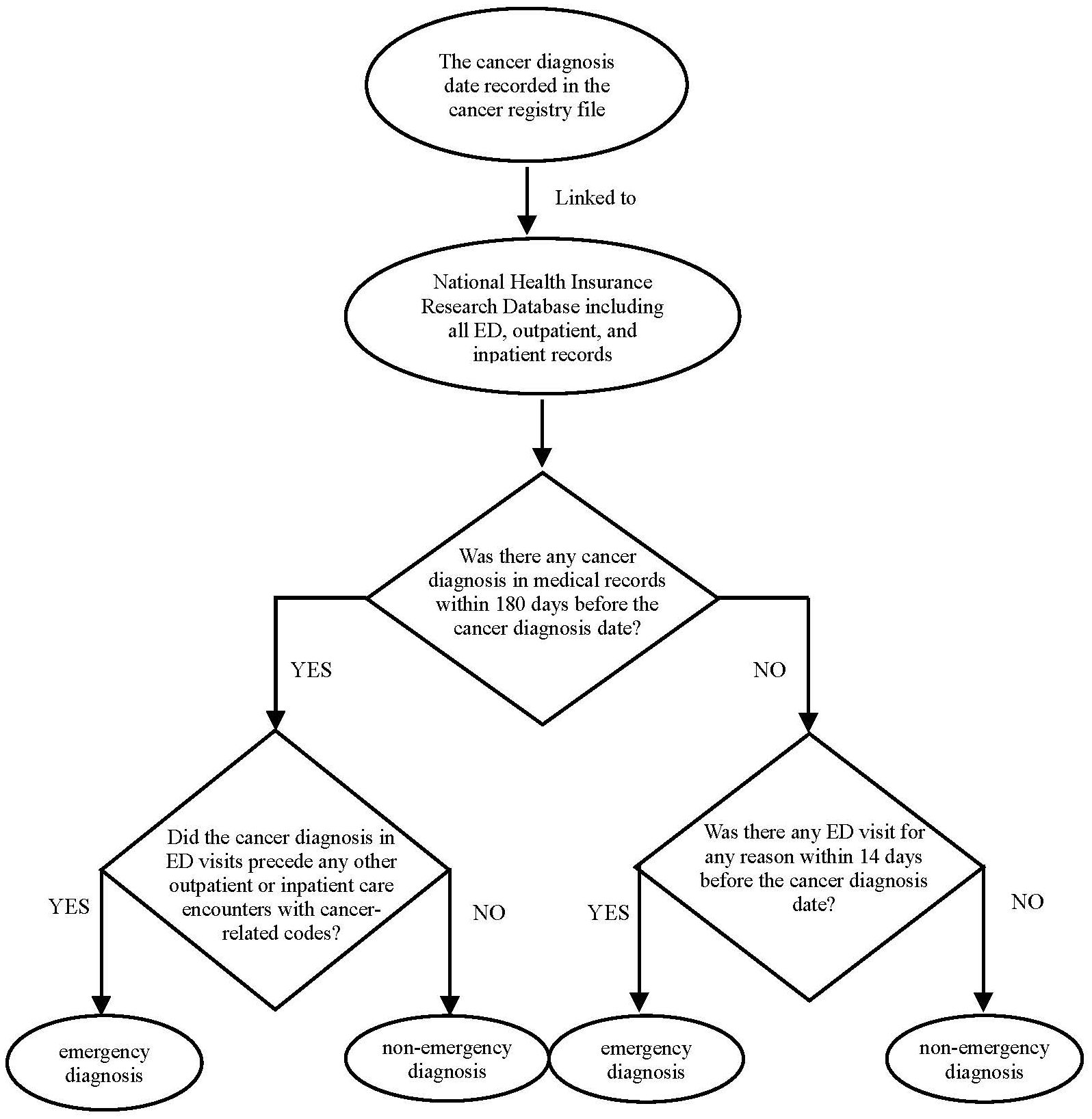
Route to diagnosis, stage at diagnosis, and survival were used as dependent variables. We obtained information on cancer diagnosis and date of diagnosis (and stage at diagnosis) from the Taiwan cancer registry, and in subsequent steps, we have classified each cancer case either as emergency department-diagnosed or non-emergency department-diagnosed. We have chiefly used two criteria, as follows:
First, we have examined the linked National Health Insurance Research Database (NHIRD) records of each cancer patient up to 180 days pre-diagnosis, searching for healthcare encounters with cancer-related diagnostic codes. Among cancer patients with a cancer-related diagnostic code in their NHIRD record up to 180 days pre-diagnosis, if the chronologically first occurrence of such code(s) related to an emergency department encounter (which preceded any other outpatient or elective inpatient care encounters with cancer-related codes), we classified such a case as an emergency department-diagnosed. Second, among cancer cases who did not have an NHIRD cancer-relevant code in the 180-day pre-diagnosis, we have additionally examined NHIRD for the occurrence of an emergency department encounter up to -14 days from the cancer registry diagnosis date, and if there has been such an encounter, the patient was classified as emergency department diagnosed. Notably, unlike our first criterion, this second criterion was not restricted to cancer-relevant diagnosis codes, i.e., the mere fact of an emergency department encounter up to -14 days from a cancer diagnosis sufficed for the second criterion to be met (the flow chart of the cancer diagnosis route shown in Figure 2).
The tumor, node, and metastasis cancer staging methods of the American Joint Committee on Cancer were applied to the data in the cancer registry to confirm cancer stages of 1, 2, 3, or 4 among the five cancers. The participants were then divided into two groups: one comprising patients with early-stage (stages 1 and 2) disease and the other comprising patients with advanced stage (stages 3 and 4) disease. For survival status, the cause of death data was connected to track whether a participant died after diagnosis. Cause of death was tracked until the end of 2018. Death was defined as an event. Conversely, survival at the end of 2018 or participants withdrawn from the National Health Insurance was defined as censored data.
Other variables included the type of cancer (female breast, colorectal, lung, prostate, and oral), as well as personal characteristics, including sex, age at diagnosis, education level, marital status, monthly salary (≤NT$17,280, NT$17,281–22,800, NT$22,801–28,800, NT$28,801–36,300, NT$36,301–45,800, NT$45,801–57,800, NT$57,801–72,800, or ≥NT$72,801), degree of urbanization of the place of residence (divided into seven grades, with grade 1 being areas with the highest degree of urbanization and grade 7 being areas with the lowest degree of urbanization (14), type of main medical institution attended (medical center, regional hospital, district hospital, or clinic), institutional ownership type (public hospital or nonpublic hospital), and year of diagnosis. Regarding health status, based on the Charlson Comorbidity Index modified by Deyo et al., the primary and secondary diagnosis codes of the patients as per ICD-9-CM were converted into numerical weighted scores to represent the severity of comorbidities. These scores were divided into 0, 1, 2, and ≥3 points, with a higher score indicating more a serious comorbidity (15).
Statistical analysis
This study used descriptive and inferential statistical analyses. Descriptive statistics such as numbers and percentages were used to demonstrate the annual proportions and trends of the patients with the five major cancers diagnosed through outpatient clinics or emergency departments. The chi squared test was performed to examine differences in cancer types, personal characteristics, economic status, environmental factors, health status, type of main medical institution, and year of diagnosis between patients diagnosed with cancer through the two routes. Differences in diagnostic pathway and distribution of related variables were explored among the patients in the cohort who were diagnosed at early and advanced stages. The log-rank test was then performed to examine the differences in survival among patients with the five major cancers by route to diagnosis, personal characteristics, economic status, environmental factor, cancer stage, health status, cancer treatment, and type of main medical institution, respectively.
Inferential statistical analyses included the use of logistic regression to compare the risk of diagnosis through the emergency department for patients with the five major cancers. Moreover, logistic regression analysis was performed to explore the risk of diagnosis at advanced stages among patients with the five cancers. The Cox proportional hazard model was used to explore the differences in mortality risk between patients with the five cancers who were diagnosed through outpatient and emergency departments. This study was approved by the research ethics committee of China Medical University and Hospital (Institutional Review Board No. CRREC-109-156).
Results
The trend in the proportion of patients with cancer diagnosed through the emergency department was first analyzed. A total of 389,043 patients who were newly diagnosed with one of the five major cancers (including breast, colorectal, lung, prostate, and oral cancers) from 2008 to 2017 were enrolled. Among the newly diagnosed patients, the highest proportion of diagnoses through the emergency department was observed for lung cancer (25.1%), followed by colorectal cancer (23.6%). The lowest proportion of diagnoses was observed for breast cancer (2.8%) (Table 1). The highest proportion of patients newly diagnosed with stage 4 cancer through the emergency department was observed for colorectal cancer (32.2%), followed by lung cancer (31.2%); the lowest was observed for breast cancer. Of note, is that the proportion of cancer diagnoses through emergency department visits was stable from 2008 to 2017. However, a slight upward trend for breast and colorectal cancer was observed (Figure 3).
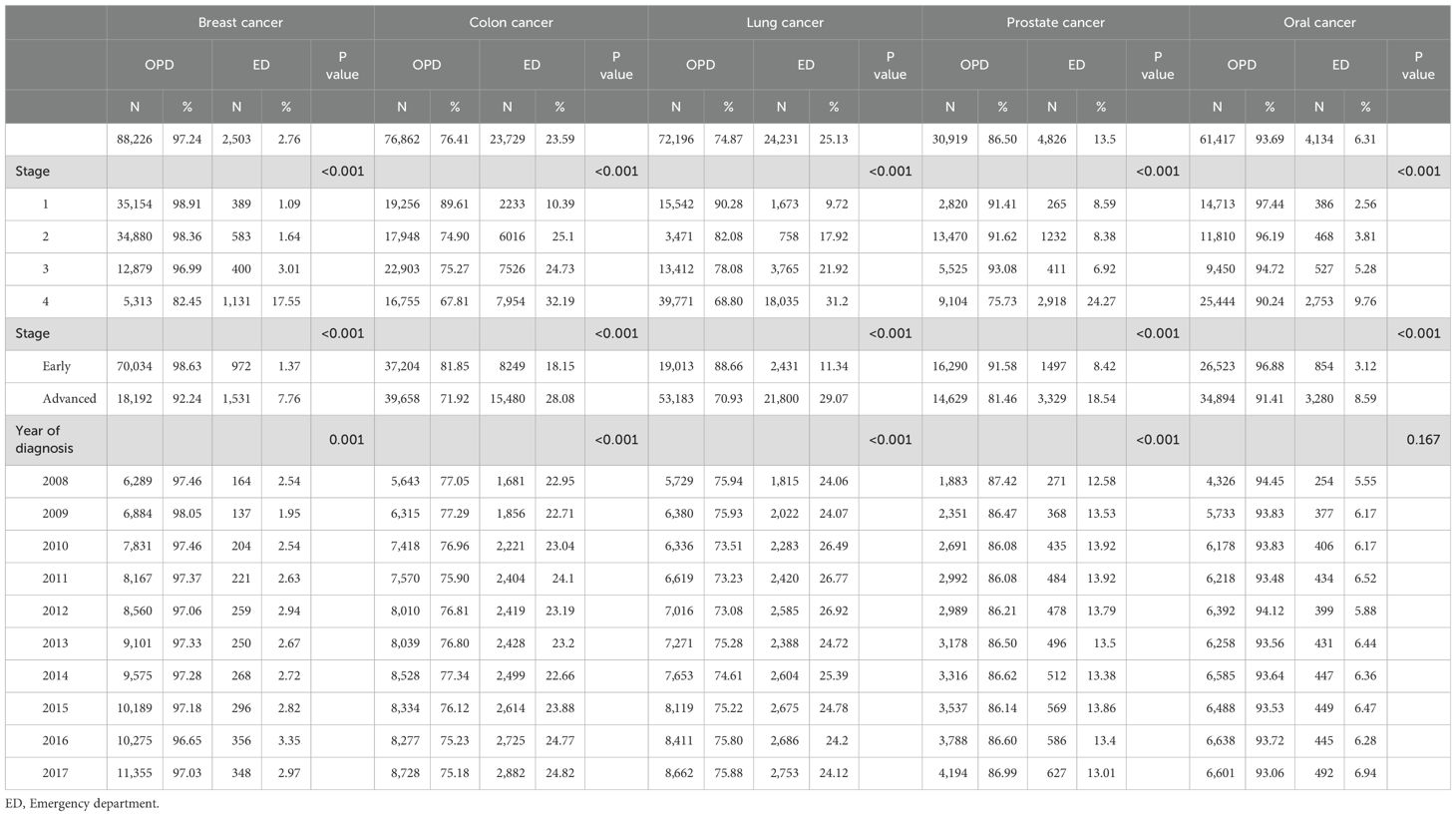
Table 1. The number and staging of cancer diagnoses made through emergency and non-emergency departments from 2008 to 2017.
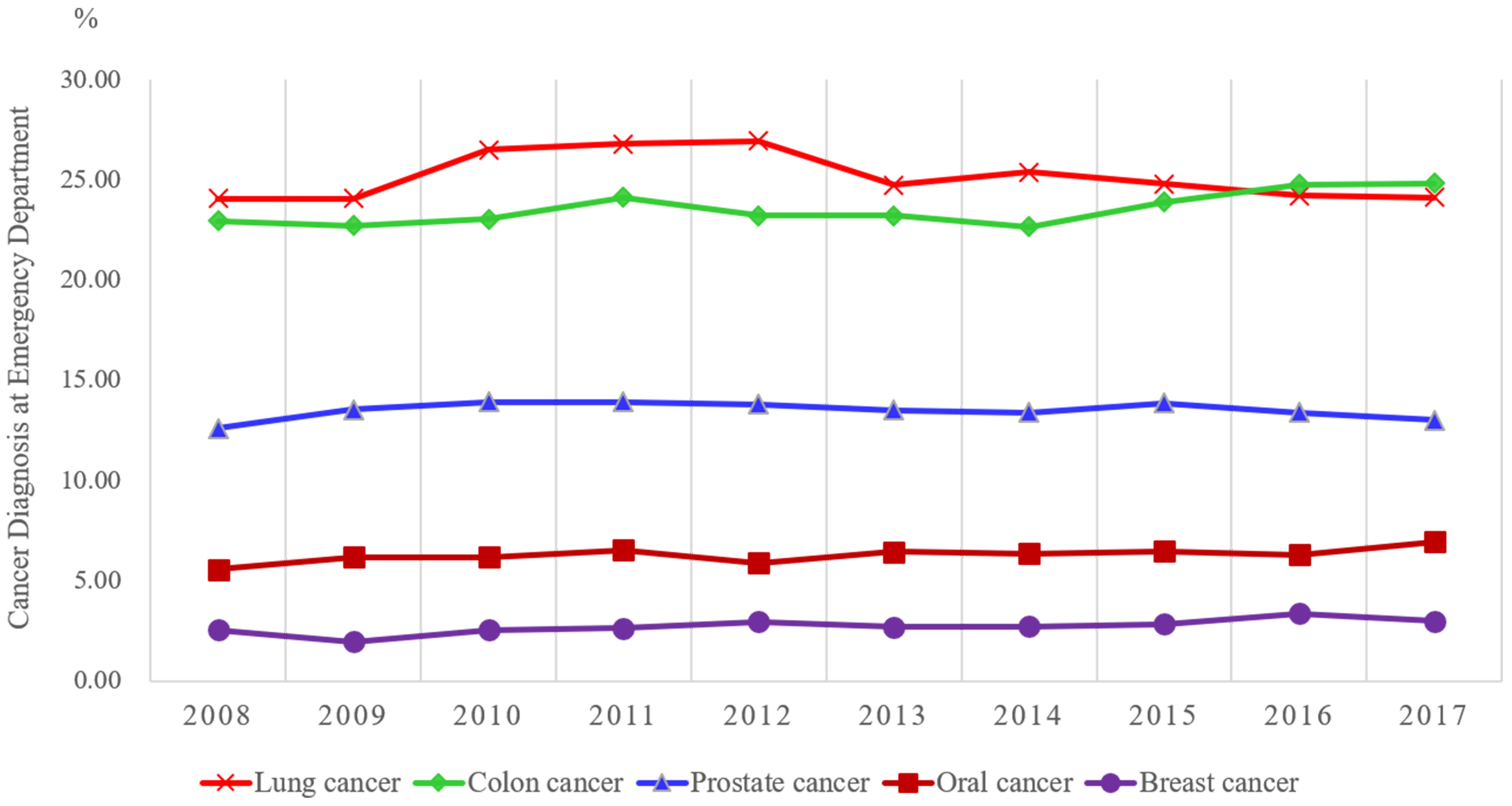
Figure 3. Trend in the proportion of cancer cases diagnosed through the emergency department by year.
To further explore each variable, logistic regression was performed to analyze differences in the risk of diagnosis through the emergency department for different types of cancer and its related factors (Table 2). Breast cancer was used as the reference. Compared with the risk of diagnosis through the emergency department for patients with breast cancer, the risk of diagnosis through that department was 8.4 times (95% confidence interval [95% CI, 7.99-8.78) higher for patients with lung cancer, 7.9 times (95% CI, 7.58-8.31) higher for those with colorectal cancer, 3.6 times (95% CI, 3.37-3.78) higher for those with prostate cancer, and 1.8 times (95% CI, 1.74-1.95) higher for those with oral cancer. The differences all reached statistical significance (P < 0.05). The probability of being diagnosed through the emergency department was significantly higher (P < 0.05) for male (odds ratio [OR], 1.18) patients older than 75 years old (OR, 1.22), those with a low level of education (OR, 1.30~1.75), those who were single (including unmarried, divorced, or widowed; OR, 1.25~1.51), those who earned a lower salary (OR, 1.12~1.52), and those with diabetes mellitus (OR, 1.37), chronic kidney disease (OR, 1.92), stroke (OR, 1.67), hypertension (OR, 1.35), or chronic mental illness (OR, 1.82).
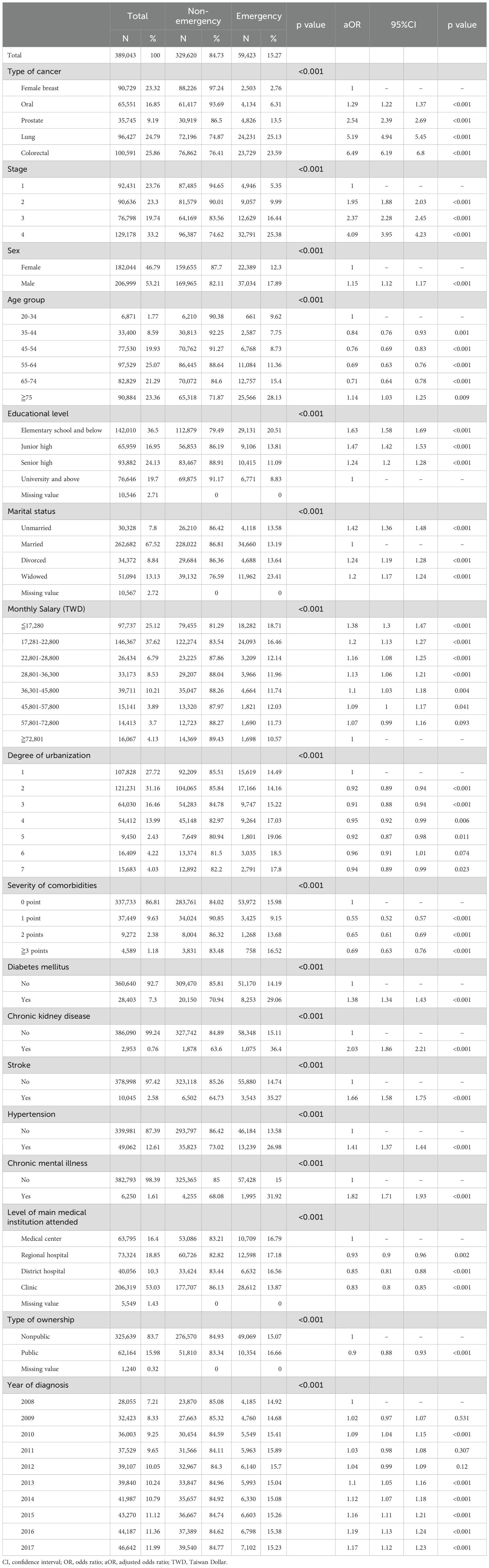
Table 2. Bivariate analysis and multivariable logistic regression analysis of diagnoses made through the emergency and non-emergency departments and related factors for five cancers.
Overall, approximately 47.1% of participants had early-stage cancer and 52.9% had advanced-stage cancer (Table 3). Among those diagnosed through emergency departments, approximately 76.4% had advanced cancer. The proportion of diagnosis of early-stage cancer was the highest for female breast cancer at 78.3%, while the proportion of diagnosis of advanced cancer was the highest for lung cancer at 77.8%. Patients with cancer who were male, older, and had lower education levels were more likely to be diagnosed with advanced cancer. In the health status analysis, the proportion of diagnosis with advanced cancer was the highest for newly diagnosed patients with a comorbidity severity (CCI) of 3 points or more (57.7%), followed by patients with 2 points (53.7%). The proportion of patients diagnosed with advanced cancer was also high for patients with diabetes mellitus, stroke, hypertension, or chronic mental illness, and the difference was statistically significant (P < 0.05).
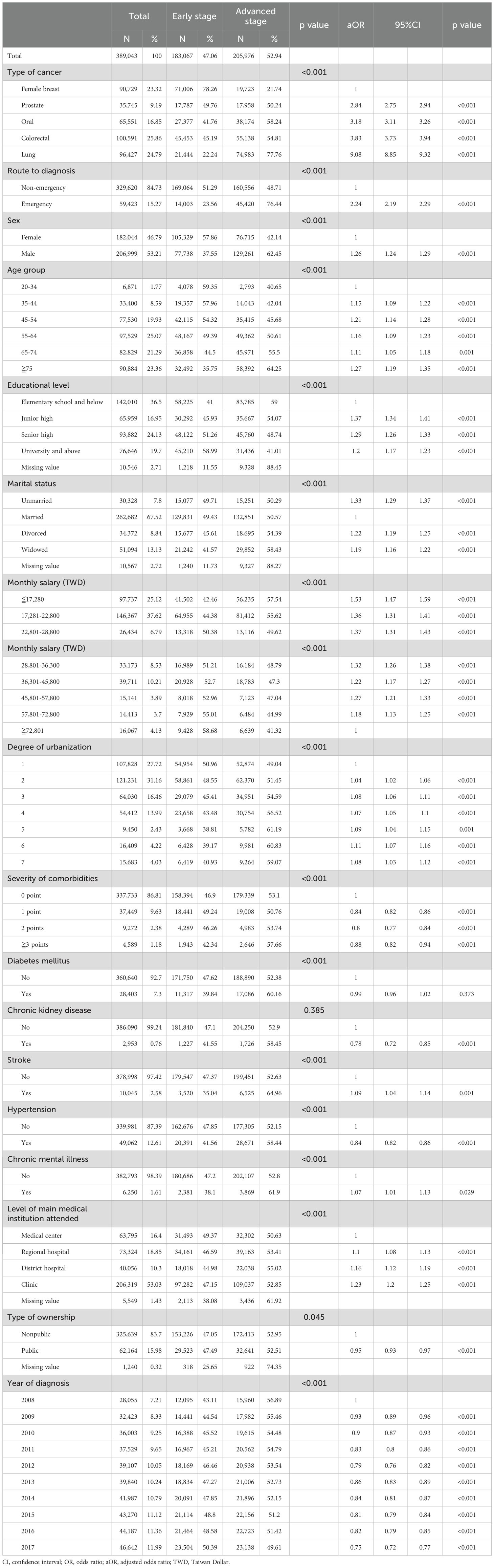
Table 3. Bivariate analysis and multivariable logistic regression analysis of the correlation between cancer stage at diagnosis and route to diagnosis for patients with one of the five cancers.
The impact of the route to diagnosis on the diagnosis of advanced cancer was explored (Table 3) through logistic regression analysis. After controlling for relevant variables, the results showed that patients with cancer diagnosed through an emergency department were more likely to be diagnosed with advanced cancer than those diagnosed through a nonemergency setting (OR, 2.24; 95%CI, 2.19–2.29). After controlling for the effect of the route to diagnosis, the probability of patients with any of the other four cancers being diagnosed with advanced cancer was 3.2 to 9.1 times higher than that of patients with breast cancer, with the highest probability observed for patients with lung cancer (OR, 9.1). All differences were statistically significant (P < 0.05).
In total, 389,043 patients were newly diagnosed with cancer from 2008 to 2017. By the end of 2018, 164,949 patients had died (Table 4). Among them, the highest number of deaths was observed for patients with lung cancer (71,171 [73.8%]), while the lowest mortality rate was observed for patients with breast cancer (14.2%). Of the patients with cancer diagnosed through the emergency department, 42,165 (71.0%) patients died. Until 2018, the mortality rate was highest for patients diagnosed with stage 4 cancer (approximately 77.7%).
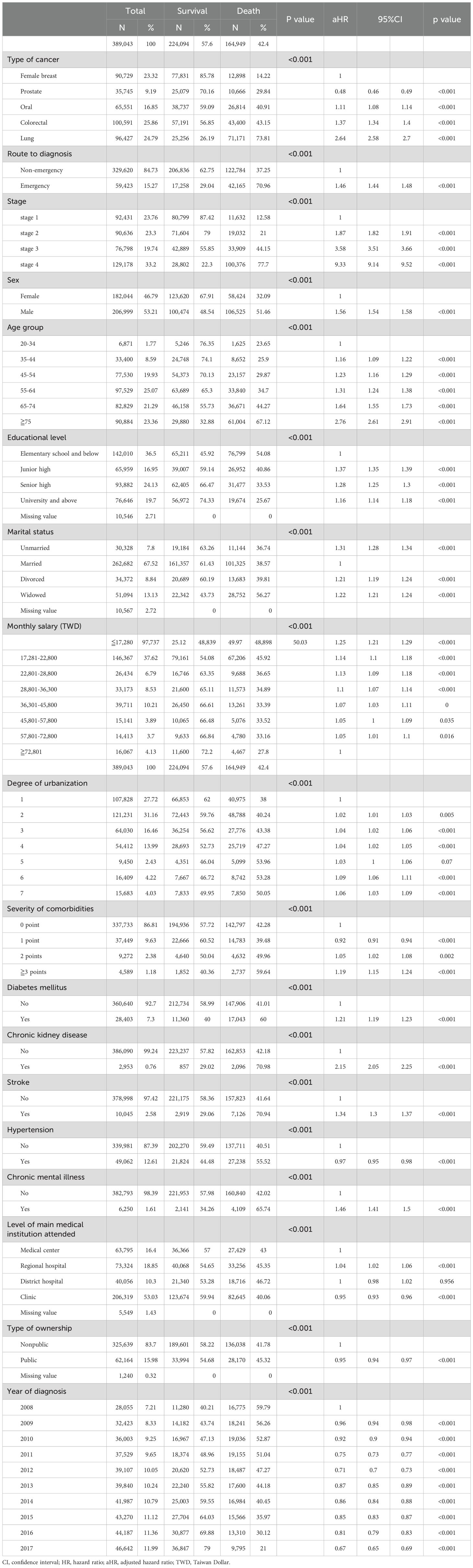
Table 4. Long rank tests and Cox proportional hazards models of factors associated with survival among patients with one of the five cancers.
The Cox proportional hazard model was adopted in the current study, and patients with cancer were tracked from the time of diagnosis until death or the end of 2018 (Table 4). Patients diagnosed with cancer through emergency departments had a significantly higher risk of death (aHR, 1.46; 95% CI, 1.44-1.48) (Figure 4). Compared with breast cancer, prostate cancer had a significantly lower risk of mortality (aHR, 0.48; 95% CI, 0.46-0.49), while the risk of mortality for oral (aHR, 1.11; 95% CI, 1.08-1.14), colorectal (aHR, 1.37; 95% CI, 1.34-1.40), and lung (aHR, 2.64; 95% CI, 2.58-2.70) cancers were all significantly higher (P < 0.05). Cancer stage, baseline personal characteristics, environment, economic factors, health status, type of main medical institution, and the year of diagnosis all were significantly associated with the survival of patients with cancer.
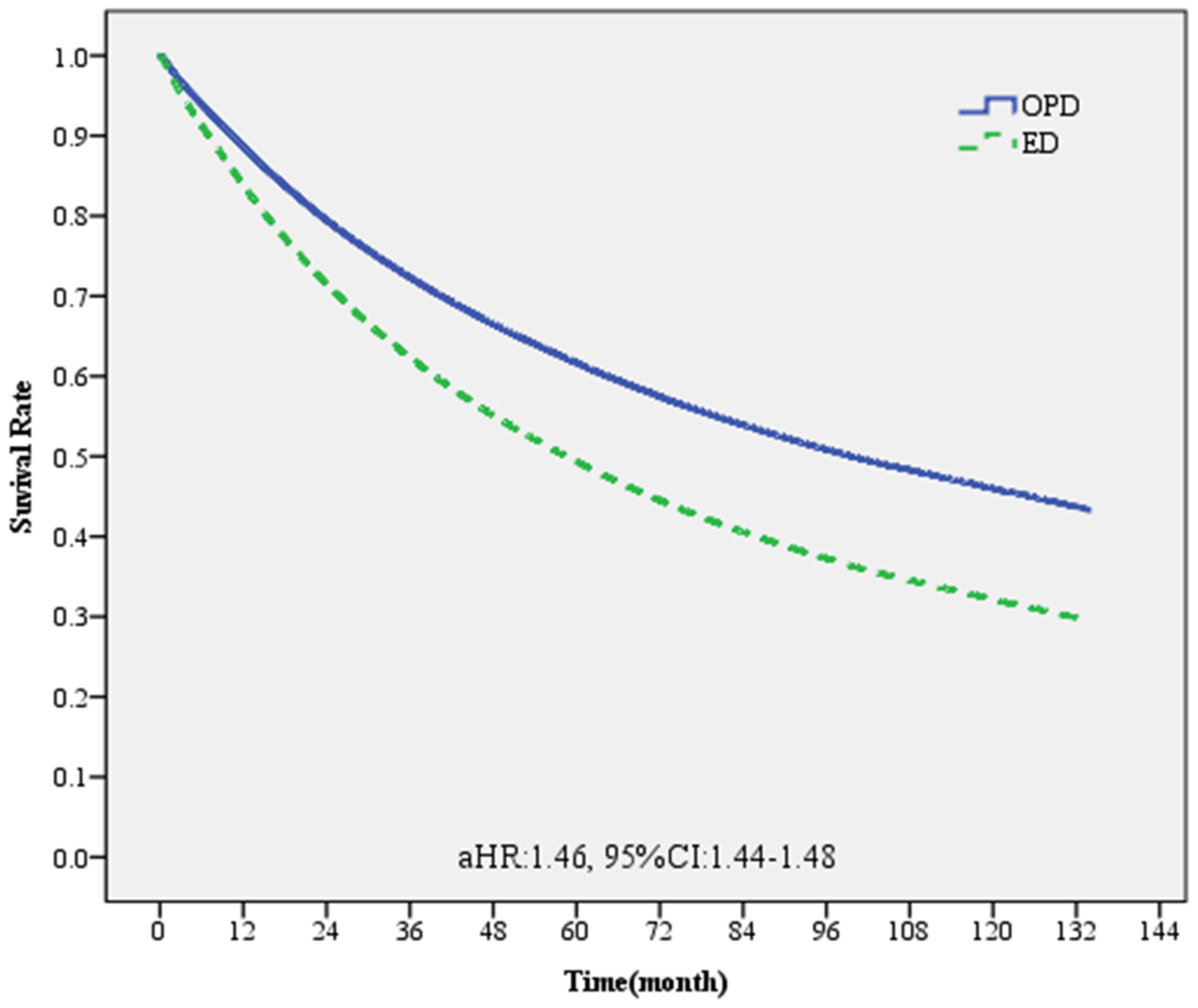
Figure 4. Survival curve of patients with one of the five major cancers diagnosed through emergency and non-emergency departments.
We further conducted stratified analyses for each cancer type. The results showed that patients with prostate cancer diagnosed at the emergency department had the highest death risk compared to those diagnosed at the non-emergency department (aHR, 1.76; 95%CI, 1.68–1.84), followed by patients with breast cancer (aHR, 1.62; 95%CI, 1.52-1.73) (Table 5).
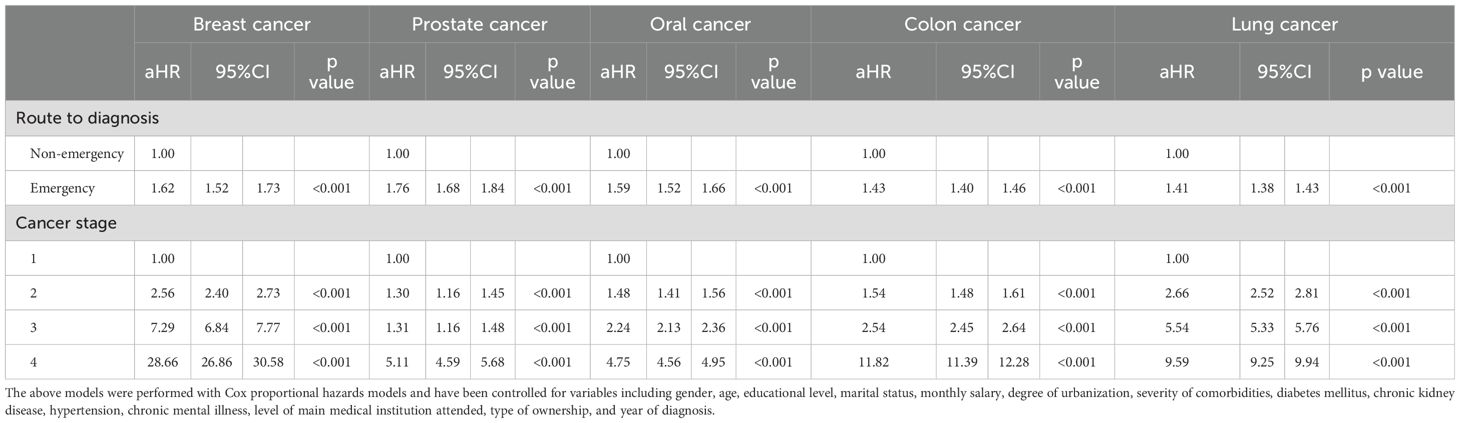
Table 5. Relative mortality risks associated with the route to diagnosis and cancer staging for each cancer.
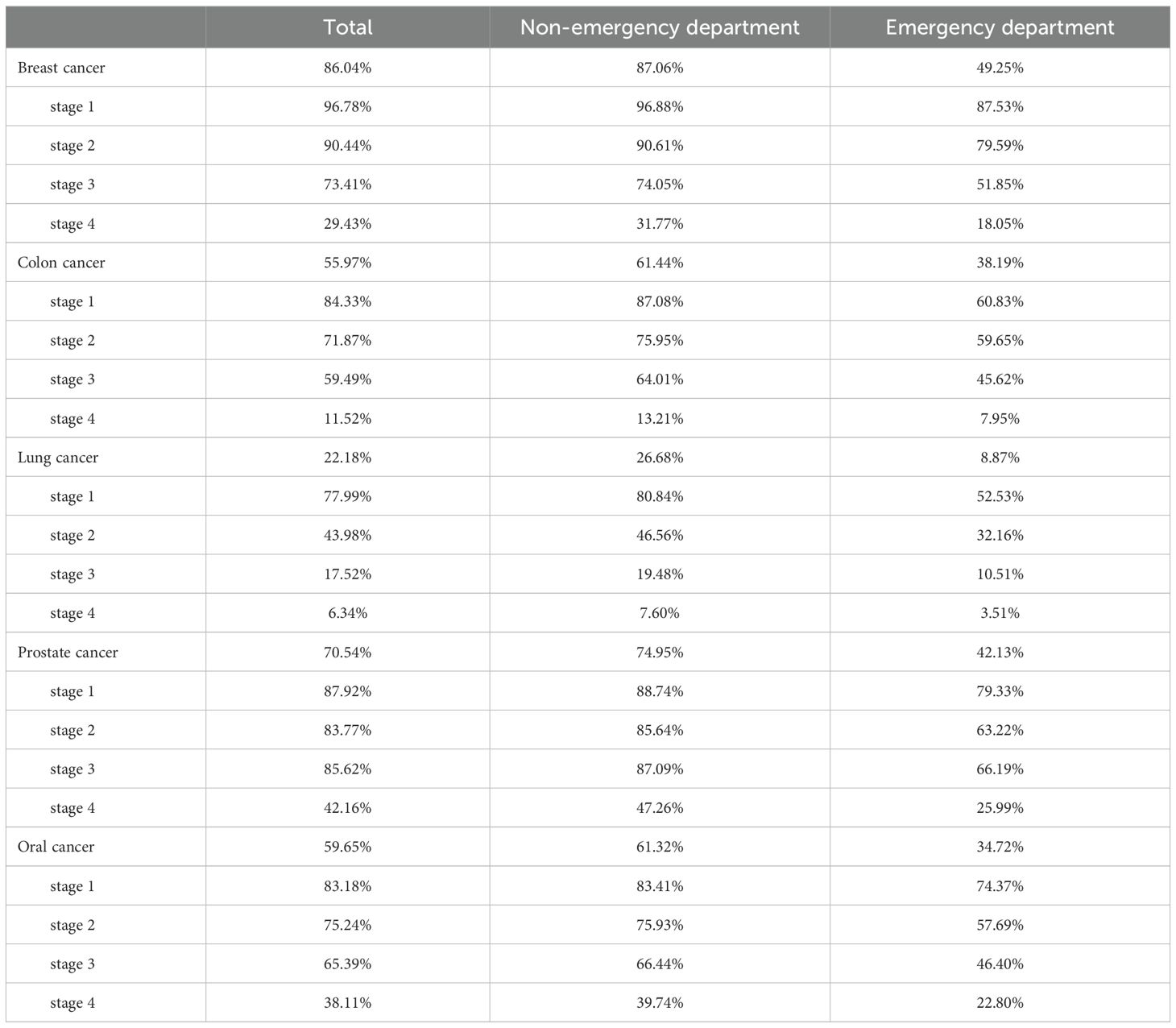
Finally, whether the 5-year cancer survival rate was different between patients diagnosed through the emergency and non-emergency departments was explored (Table 6; Figure 5). The overall 5-year survival rate of patients with any of the five cancers included in this study was approximately 56.7%. Among them, the 5-year survival rate of patients diagnosed with cancer through the emergency department was only 26.9%. The survival rate of patients with stage 1 cancer was the highest (88.0%), while the survival rate of those with stage 4 cancer was the lowest (18.9%). In terms of cancer type, the 5-year survival rate of patients with breast cancer was the highest at 86.0%, while that of patients with breast cancer diagnosed through the emergency department was 49.3%. The 5-year survival rate of patients with lung cancer was the lowest (22.2%), while that of patients with lung cancer diagnosed through the emergency department was 8.87%. For patients diagnosed with stage 4 lung cancer through the emergency department, the 5-year survival rate was even lower (3.51%).

Figure 5. Survival curve of patients with different cancers diagnosed through emergency and non-emergency departments.
Discussion
The routes to diagnose cancer can be divided into three categories: cancer screening, outpatient clinics, and the emergency department (16–18). In the present study, the proportion of initial diagnoses made through the emergency department was the lowest for patients with breast cancer. This may be because noting abnormalities in the appearance of the breasts is easy, resulting in early stages being found at initial diagnosis and fewer diagnoses being made through the emergency department. The proportion of diagnoses made through the emergency department was highest for patients with lung cancer (25.1%), followed by that for patients with colorectal cancer (23.6%). This finding aligns with a SEER-Medicare study that showed EDs play a crucial role in diagnosing cancer in older US adults. ED visits accounted for 23% of cancer diagnoses among 614,748 patients, with the highest rates in colorectal and lung cancers (19). Despite variations in diagnostic standards, both lung cancer and rectal cancer impact patients’ lives in a significant manner. The former manifests as dyspnea or cough, while the latter leads to intestinal obstruction or bleeding, prompting patients to seek emergency treatment. Nonetheless, both cancers have room for tumor growth, making detection challenging. Hence, the onset of symptoms may necessitate emergency treatment, thereby increasing opportunities for cancer diagnosis under such circumstances.
However, a study by McPhail et al., which looked at eight types of cancer across six countries, contradicts our findings. The study includes data from 857,068 patients across 14 regions. The results showed that emergency diagnosis occurred in 24% to 42.5% of cases. The highest rate of emergency diagnosis was recorded in relation to pancreatic cancer, ranging from 34.1% to 60.4%. Conversely, the lowest rate was observed in rectal cancer cases, which ranged from 9.1% to 19.8% (20). There are various factors that could impact the percentage of emergency diagnoses, such as public perceptions and awareness regarding potential cancer symptoms, healthcare system organization, presence and participation in population-based cancer screening programs, and the type of definition used, whether broad or narrow. Furthermore, there may be other unmeasured variables that impact these findings (20).
In this study, the date of cancer diagnosis of the study participants was obtained through the cancer registry files. The use of cancer registration files to identify cancer is rarely used in other studies as a diagnosis of cancer. In addition, in the absence of any medical records for target cancer within 180 days before the diagnosis date, we determine whether there is any emergency department care record within two weeks (14 days) before the cancer diagnosis date to classify it as an emergency diagnosis. If no such records existed, they fall under the non-emergency diagnosis category. A patient’s cancer diagnosis occurred within 14 days after the emergence visit, and it was still considered an emergency-diagnosed cancer since the cancer-related diagnosis codes might be reported late due to the cancer-related examination process. Some studies defined an emergency diagnosis of cancer based on an emergency visit within 30 days before the diagnosis (19–21), for that definition is too imprecise and too much interference. Our definition is more precise, making it less prone to errors.
Since 1995, Taiwan has successively implemented services to screen for the four major cancers. Currently, free screening services are provided to the public for cervical, oral, breast, and colorectal cancers. According to the statistical analyses of the Health Promotion Administration of the Ministry of Health and Welfare of Taiwan, having a fecal occult blood test every 2 years may reduce the mortality rate of colorectal cancer by 23% and having a mammography examination every 2 years may reduce the mortality rate of breast cancer by 41%; regular examination of the oral mucosa may reduce the risk of death by 26% in men who chew betel nut or smoke (22). In the current study, stage 4 cancer was most common among patients diagnosed with cancer through the emergency department. Among all types of cancer, the highest proportion of stage 4 cancer was observed for patients with colorectal cancer (32.2%), followed by patients with lung cancer (31.2%). The lowest proportion of stage 4 cancer was observed among patients with breast cancer (17.6%). An analysis of cases by year showed that the number of diagnoses of various types of cancer through the emergency department has not decreased, even though the amount of screening data has increased each year. This discrepancy may result from that fact that most of the cases diagnosed through screening were in the early stages of disease. However, in the current study, approximately 76.4% of patients diagnosed with cancer through the emergency department had advanced cancer. Therefore, screening could not have reduced the proportion of diagnoses made through the emergency department.
Gender, age, education level, salary, degree of urbanization of the place of residence, medical insurance, family health history, and personal medical history are factors associated with the cancer stage at diagnosis (23–30). The cancer stage at diagnosis is generally higher for men than for women (23, 24). Similar findings were noted in the present study. Moreover, the cancer stage at diagnosis increases with increasing age (23, 25, 26). A study on prostate cancer showed that patients with advanced cancer at diagnosis were between 70 and 79 years old (27). Recently, a lot of studies reported that older patients with cancer were significantly more likely to be diagnosed with advanced cancer (19, 28). In Denmark, a study examined diagnosis routes for different age groups among 137,876 cancer patients. Most middle-aged patients were identified through cancer patient pathways, but younger and older patients were less likely to be diagnosed this way. Instead, more older patients were diagnosed via unplanned admission, death certificate, or outpatient admission (31). Our study indicated that a high proportion of patients over 75 years old were diagnosed with cancer through the emergency department or with advanced cancer. The relative lack of knowledge on cancer among older people, as well as their inability to obtain timely medical care, may cause a delay in their receiving care, thus resulting in the advanced cancer stage at diagnosis (29).
Cancer stage at diagnosis is more advanced for people with lower education levels than for those with higher education levels (7, 19, 20, 30), with lower income levels than for those with higher income levels (7, 22, 23, 27, 30), and for residents of rural areas than for residents of urban centers (7, 23, 30). Similarly, the findings of the current study revealed that patients were significantly more likely to be diagnosed with advanced cancer or die if they had low education levels, low salaries, or lived in suburban areas.
The literature suggests that unmarried individuals may be more likely to have their cancer diagnosed through emergency presentation, which can lead to poorer prognoses (19, 21). This could be due to a range of factors, including social support mechanisms and access to healthcare resources, which are often more limited for unmarried individuals (32, 33). Further research is needed to elucidate the pathways through which marital status influences the likelihood of ED involvement in cancer diagnosis and to develop targeted interventions to improve outcomes for unmarried patients (34, 35). We also found that unmarried patients were more likely to be diagnosed through the emergency department or diagnosed with advanced cancer than married patients. This finding has rarely been mentioned in the literature. Married people may receive social support from their spouses and have low cortisol levels, or perhaps high levels of natural killer cells, which may slow tumor progression. Spouses may also encourage patients to undergo early testing and treatment (36).
Personal medical history or family history of cancer may also affect cancer stage at the time of diagnosis (7, 24, 25). Patients with a history of hypertension or hyperlipidemia are more likely to be diagnosed with early-stage liver cancer (25) and patients with a history of polyp are more likely to be diagnosed with early-stage colorectal cancer (24). According to the literature, patients with more comorbidities are more likely to be diagnosed with tumors through the emergency department (37). Similar findings were noted in the present study: the proportion of patients newly diagnosed with advanced cancer was high (57.7%) for patients with a comorbidity severity score of 3 or more, followed by patients with a score of 2 (53.7%). The proportion of advanced cancers diagnosed was also high for patients with diabetes mellitus, stroke, hypertension, or chronic mental illness.
Prostate cancer had a significantly lower mortality risk than breast cancer; however, the risk was highest for lung cancer. Compared with other cancers, the probability of having advanced lung cancer at diagnosis is high (28). The same finding was noted in the present study. Compared with other cancer types, patients with lung cancer had an increased chance of being diagnosed with advanced cancer. Factors that lead to a delayed diagnosis of lung cancer should be prioritized when formulating policies and public health measures. Reasons for lung cancer being diagnosed at an advanced stage often include a combination of factors such as ignorance of initial symptoms and delays in seeking medical care, having diagnostic biopsies, and even getting referrals. All these factors could lead to having advanced cancer at diagnosis (38).
The current study showed that, regardless of cancer type, patients diagnosed with cancer through emergency departments had a significantly higher risk of death (2.24 times higher). A recent retrospective study found that, compared with patients diagnosed with cancer in non-emergency settings, patients diagnosed through emergency departments were at higher risk of being diagnosed with advanced cancer (relative risk, RR, 1.30; 95% CI, 1.39–1.58), and their survival rate was lower (RR, 0.61; 95% CI, 0.49–0.75) (37). In New Zealand, it was discovered that being diagnosed with cancer through emergency departments led to significantly lower survival rates among all ethnic groups (adj. OR 2.40, 95% CI 2.10–2.74) (39). The same condition could be found in Denmark, where the mortality rate within a year varied from 1.4% among patients who underwent screening to 53.0% among those who received a diagnosis following an unscheduled hospital admission. Individuals with an unscheduled admission had a higher likelihood of dying in the first year following diagnosis [OR = 3.38 (95% CI: 3.24–3.52)] compared to patients who were diagnosed through the cancer patient pathway from primary care (40). Similarly, the current study showed that approximately 76.4% of patients diagnosed with cancer via emergency departments had advanced cancer, and the risk of death was significantly high (HR, 1.46; 95% CI, 1.44–1.48). Another US study shows visiting emergency departments (ED) six months before a cancer diagnosis results in a higher mortality risk (OR = 1.73, 95% CI 1.38–2.18). Having Medicaid insurance leads to a higher rate (OR = 4.16, 95% CI 2.45–7.07). Over a third of cancer patients visit EDs before diagnosis (41). Also, a study illustrated that emergency presenters also had a greater risk of 12-month mortality than non-emergency presenters. Furthermore, a 10% increase in emergency presentations was associated with a decrease in one-year net survival of between 2.5% and 7% (20).
The survival curves of patients diagnosed through non-emergency and emergency departments revealed that the 5-year survival rate of patients diagnosed through the emergency department was lower than that of patients diagnosed through non-emergency departments. In terms of cancer types, compared with breast cancer, the mortality risk of prostate cancer was significantly lower, while those of oral, colorectal, and lung cancers were all significantly higher (P < 0.05). This finding was consistent with those of previous studies that found that patients diagnosed through the emergency department tended to have advanced disease and were at high risk of death (37, 42). Therefore, the emergency department plays a crucial role in the initial diagnosis of cancer and must be regarded as an important part of cancer care (43).
The current research’s findings, which are consistent with those of McPhail et al., show that patients over 75 years old, those with low incomes and education levels, those living in rural areas, and those with more comorbidities are more likely to receive a cancer diagnosis from the emergency department (20). For such patients, the initial diagnosis was often at advanced cancer stage. Therefore, patients over 75 years old, with a low education level, with low income, living in rural areas, or having more comorbidities may be classified as being at high risk for delayed cancer diagnosis. As Elliss-Brookes et al. emphasized, connecting patients with cancer with oncology care networks is a complex process, even for communities with complex cancer care systems (44). Another study found that certain sociodemographic and clinical factors, such as older age, non-Hispanic Black and Native Hawaiian/Other Pacific Islander race being unmarried, recent diagnosis year, later-stage disease, comorbidities, and poverty, were associated with an increased likelihood of ED involvement in cancer diagnosis (19). Cancer diagnoses often occur as emergencies across the globe, particularly among the elderly and those with advanced cancer, leading to negative impacts on survival rates. Enhancing cancer control on a global scale requires effective monitoring of emergencies, determining behavioral and healthcare factors, and prioritizing suitable interventions (20).
Patients in the abovementioned high-risk groups may not be able to attend cancer screenings and may ignore early symptoms, or they may not be able to get timely check-ups as they are busy earning a living. Hence, they are only connected to the medical care system through the emergency department. Therefore, it follows that these patients are mostly diagnosed with cancer through the emergency department, and they may not even undergo complete treatment. Recent literature suggests the need for a standardized referral process from emergency departments to cancer care systems, which may strengthen the connection between oncology and emergency teams and establish a multi-specialty medical cooperation system to improve the quality and efficiency of care (45). In the United States of America, the Comprehensive Oncologic Emergencies Research Network—established with support from the National Cancer Institute—promotes collaboration between the oncology and emergency medical departments to expand knowledge on the treatment of cancer in emergency medicine settings (46). On the other hand, there is a literature that has developed a digital quality measure (DQM) to help identify missed opportunities for diagnosis (MODs) and mortality due to diagnostic errors, such as overlooked test results, missed referrals, or miscommunication. Many patients with EP experience MODs, indicating that EP is linked to increased mortality and is responsible for preventable diagnostic delays. Nationwide implementation could result in strategies developed to address preventable cancer diagnostic delays (47).
Study limitations
To the best of our knowledge, this is the first study conducted in Taiwan to compare the five major cancers diagnosed through outpatient clinics and emergency departments. The advantages of our study include that it was population-based and conducted over an extended period of time, and that it had a large sample size. However, certain limitations must be acknowledged.
Since the National Health Insurance Research Database was used to obtain data for analysis in the current study, only submitted data were presented, and we do not know whether patients underwent self-paid health examinations. Such patients were eventually diagnosed through outpatient clinics; however, it may have affected the proportion of diagnoses made through the emergency department. Furthermore, patients may have received interim treatment in an emergency department but were subsequently referred to an outpatient clinic for further confirmatory testing; this procedure may have resulted in an underestimation of the number of cancer cases diagnosed through emergency departments and an overestimation of the number of cancer cases diagnosed through outpatient clinics. Similar studies conducted in the United States of America determined that only 55% of the population was enrolled in the government’s medical insurance programs. The literature indicates that enrollment in a medical insurance plan has a significant impact on the cancer stage at diagnosis. People without medical insurance are more likely to be diagnosed with advanced cancer (48, 49). National Health Insurance in Taiwan has achieved full coverage, with an enrollment rate of 99.7% (50). For this reason, the findings of the current study cannot be extrapolated to other countries.
Conclusions
The treatment outcome of patients with cancer is closely related to the cancer stage determined at the initial diagnosis. In the present study, patients with one of the top five cancers who were diagnosed through an emergency department often had a more advanced stage than those diagnosed through an outpatient clinic. Since the National Health Insurance Program has been implemented in Taiwan, almost 99.7% of people have been covered by health insurance. However, some people are still diagnosed with advanced cancer. Therefore, promoting regular health check-ups is important to reduce the risk of advanced cancer developing and only being identified at diagnosis. In addition, despite screening programs being implemented for four cancers, the proportion of cancer diagnoses made through the emergency department remains high. The government should consider further strengthening cancer screening for high-risk groups and people with low socioeconomic status to detect and treat cancer early. Patients diagnosed with one of the five major cancers through the emergency department mostly have advanced cancer and are at high risk of death. The trend of the proportion of cancer diagnoses through the emergency department may be used as an indicator for the effectiveness of cancer screening programs. Methods for strengthening the integration of the emergency department and cancer teams to reduce patients’ mortality risks must also be included as an important topic in cancer care.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the research ethics committee of China Medical University and Hospital (Institutional Review Board No. CRREC-109-156). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
Y-CL: Conceptualization, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. W-YK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft. P-TK: Conceptualization, Funding acquisition, Methodology, Resources, Software, Supervision, Validation, Writing – review & editing. W-CT: Conceptualization, Funding acquisition, Methodology, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by China Medical University (CMU110-S-19). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
We are grateful for using the National Health Insurance Research Databases provided by the Ministry of Health and Welfare, Taiwan. We also thank Health Data Science Center, China Medical University Hospital, for providing administrative, technical, and funding support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1399326/full#supplementary-material
References
1. Taiwan Ministry of Health and Welfare. >2021 Cancer Registry Annual Report. Taipei, Taiwan: Health Promotion Administration. (2023).
2. Mehrkhani F, Nasiri S, Donboli K, Meysamie A, Hedayat A. Prognostic factors in survival of colorectal cancer patients after surgery. Colorectal Dis. (2009) 11:157–61. doi: 10.1111/j.1463-1318.2008.01556.x
3. Chen PC, Lee JC, Wang JD. Estimation of life-year loss and lifetime costs for different stages of colon adenocarcinoma in Taiwan. PloS One. (2015) 10:e0133755. doi: 10.1371/journal.pone.0133755
4. Wang JH, Changchien CS, Hu TH, Lee CM, Kee KM, Lin CY, et al. The efficacy of treatment schedules according to Barcelona Clinic Liver Cancer staging for hepatocellular carcinoma - Survival analysis of 3892 patients. Eur J Cancer. (2008) 44:1000–6. doi: 10.1016/j.ejca.2008.02.018
5. Yuen MF, Cheng CC, Lauder IJ, Lam SK, Ooi CG, Lai CL. Early detection of hepatocellular carcinoma increases the chance of treatment: Hong Kong experience. Hepatology. (2000) 31:330–5. doi: 10.1002/hep.510310211
6. Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol. (2004) 130:417–22. doi: 10.1007/s00432-004-0552-0
7. Shen CT, Chen FM, Hsieh HM. Effect of a national population-based breast cancer screening policy on participation in mammography and stage at breast cancer diagnosis in Taiwan. Health Policy. (2020) 124:478–85. doi: 10.1016/j.healthpol.2020.02.006
8. Ho PS, Wang WC, Huang YT, Yang YH. Finding an oral potentially Malignant disorder in screening program is related to early diagnosis of oral cavity cancer - Experience from real world evidence. Oral Oncol. (2019) 89:107–14. doi: 10.1016/j.oraloncology.2018.12.007
9. Chuang SL, Su WWY, Chen SLS, Yen AMF, Wang CP, Fann JCY, et al. Population-based screening program for reducing oral cancer mortality in 2,334,299 Taiwanese cigarette smokers and/or betel quid chewers. Cancer. (2017) 123:1597–609. doi: 10.1002/cncr.30517
10. Kronenfeld JP, Ryon EL, Goldberg D, Lee RM, Yopp A, Wang A, et al. Survival inequity in vulnerable populations with early-stage hepatocellular carcinoma: a United States safety-net collaborative analysis. HPB. (2021) 23:868–76. doi: 10.1016/j.hpb.2020.11.1150
11. Abel GA, Mendonca SC, Mcphail S, Zhou Y, Elliss-Brookes L, Lyratzopoulos G. Emergency diagnosis of cancer and previous general practice consultations: insights from linked patient survey data. Br J Gen Practice. (2017) 67:e377–87. doi: 10.3399/bjgp17x690869
12. Frey RS, Boldanova T, Heim M. Ultrasound surveillance for hepatocellular carcinoma: real-life performance in a hepatology outpatient clinic. Swiss Med Wkly. (2015) 145:w14200. doi: 10.4414/smw.2015.14200
13. Zhou Y, Abel GA, Hamilton W, Pritchard-Jones K, Gross CP, Walter FM, et al. Diagnosis of cancer as an emergency: a critical review of current evidence. Nat Rev Clin Oncol. (2017) 14:45–56. doi: 10.1038/nrclinonc.2016.155
14. Liu CY, Hung YT, Chuang YL, Chen YJ, Weng WS, Liu JS. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manage. (2006) 4:1–22. doi: 10.29805/JHM.200606.0001
15. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. (1992) 45:613–9. doi: 10.1016/0895-4356(92)90133-8
16. Taiwan Ministry of Health and Welfare. Procedures for the follow-up diagnosis and treatment for cases with positive fecal occult blood test. Taipei, Taiwan: Health Promotion Administration. (2012).
17. Taiwan Ministry of Health and Welfare. Procedures for the follow-up diagnosis and treatment for cases with positive oral mucosal examination results. Taipei, Taiwan: Health Promotion Administration. (2014).
18. Taiwan Ministry of Health and Welfare. Procedures for the follow-up diagnosis and treatment for cases with positive mammography results. Taipei, Taiwan: Health Promotion Administration. (2018).
19. Thompson CA, Sheridan P, Metwally E, Peacock Hinton S, Mullins MA, Dillon EC, et al. Emergency department involvement in the diagnosis of cancer among older adults: a SEER-Medicare study. JNCI Cancer Spectr. (2024) 8(3):pkae039. doi: 10.1093/jncics/pkae039
20. McPhail S, Swann R, Johnson SA. Risk factors and prognostic implications of diagnosis of cancer within 30 days after an emergency hospital admission (emergency presentation): an International Cancer Benchmarking Partnership (ICBP) population-based study. Lancet Oncol. (2022) 23:587–600. doi: 10.1016/s1470-2045(22)00127-9
21. Sheridan P, Lyratzopoulos G, Murphy JD, Thompson CA. Emergency department-mediated cancer diagnosis among older adults in the United States. J Clin Oncol. (2019) 37:139–9. doi: 10.1200/JCO.2019.37.27_suppl.139
22. Taiwan Ministry of Health and Welfare. The effectiveness of cancer prevention and treatment. Taipei, Taiwan: Health Promotion Administration. (2022).
23. Wong RJ, Kim D, Ahmed A, Singal AK. Patients with hepatocellular carcinoma from more rural and lower-income households have more advanced tumor stage at diagnosis and significantly higher mortality. Cancer. (2021) 127:45–55. doi: 10.1002/cncr.33211
24. Akada K, Koyama N, Taniguchi S, Miura Y, Aoshima K. Database analysis of patients with hepatocellular carcinoma and treatment flow in early and advanced stages. Pharmacol Res Perspectives. (2019) 7:e00486. doi: 10.1002/prp2.486
25. Andrew AS, Parker S, Anderson JC, Rees JR, Robinson C, Riddle B, et al. Risk factors for diagnosis of colorectal cancer at a late stage: a population-based study. J Gen Internal Med. (2018) 33:2100–5. doi: 10.1007/s11606-018-4648-7
26. Klassen AC, Curriero FC, Hong JH, Williams C, Kulldorff M, Meissner HI, et al. The role of area-level influences on prostate cancer grade and stage at diagnosis. Prev Med. (2004) 39:441–8. doi: 10.1016/j.ypmed.2004.04.031
27. Wu C-C, Lin C-H, Chiang H-S, Tang M-J. A population-based study of the influence of socioeconomic status on prostate cancer diagnosis in Taiwan. Int J Equity Health. (2018) 17:79. doi: 10.1186/s12939-018-0792-2
28. Mills S, Donnan P, Buchanan D, Smith BH. Age and cancer type: associations with increased odds of receiving a late diagnosis in people with advanced cancer. BMC Cancer. (2023) 23:1174. doi: 10.1186/s12885-023-11652-1
29. Robb K, Stubbings S, Ramirez A, Macleod U, Austoker J, Waller J, et al. Public awareness of cancer in Britain: a population-based survey of adults. Br J Cancer. (2009) 101:S18–23. doi: 10.1038/sj.bjc.6605386
30. Shen Y, Guo H, Wu T, Lu Q, Nan K-J, Lv Y, et al. Lower education and household income contribute to advanced disease, less treatment received and poorer prognosis in patients with hepatocellular carcinoma. J Cancer. (2017) 8:3070–7. doi: 10.7150/jca.19922
31. Danckert B, Christensen NL, Falborg AZ, Frederiksen H, Lyratzopoulos G, McPhail S, et al. Assessing how routes to diagnosis vary by the age of patients with cancer: a nationwide register-based cohort study in Denmark. BMC Cancer. (2022) 22:906. doi: 10.1186/s12885-022-09937-y
32. Yang CC, Cheng LC, Lin YW, Wang SC, Ke TM, Huang CI, et al. The impact of marital status on survival in patients with surgically treated colon cancer. Med (Baltimore). (2019) 98:e14856. doi: 10.1097/md.0000000000014856
33. Yang KB, Zhang YZ, Chen ZH, Wu CF, Zheng WH, Kou J, et al. Contribution of insurance status to the association between marital status and cancer-specific survival: a mediation analysis. BMJ Open. (2022) 12:e060149. doi: 10.1136/bmjopen-2021-060149
34. Martínez ME, Unkart JT, Tao L, Kroenke CH, Schwab R, Komenaka I, et al. Prognostic significance of marital status in breast cancer survival: A population-based study. PloS One. (2017) 12:e0175515. doi: 10.1371/journal.pone.0175515
35. Pruthi RS, Lentz AC, Sand M, Kouba E, Wallen EM. Impact of marital status in patients undergoing radical cystectomy for bladder cancer. World J Urol. (2009) 27:573–6. doi: 10.1007/s00345-009-0380-6
36. Aizer AA, Chen M-H, Mccarthy EP, Mendu ML, Koo S, Wilhite TJ, et al. Marital status and survival in patients with cancer. J Clin Oncol. (2013) 31:3869–76. doi: 10.1200/jco.2013.49.6489
37. Kang S, McLeod SL, Walsh C, Grewal K. Patient outcomes associated with cancer diagnosis through the emergency department: A systematic review. Acad Emerg Med. (2023) 30:955–62. doi: 10.1111/acem.14671
38. Ellis PM, Vandermeer R. Delays in the diagnosis of lung cancer. J Thorac Dis. (2011) 3:183–8. doi: 10.3978/j.issn.2072-1439.2011.01.01
39. Gurney J, Davies A, Stanley J, Signal V, Costello S, Dawkins P, et al. Emergency presentation prior to lung cancer diagnosis: A national-level examination of disparities and survival outcomes. Lung Cancer. (2023) 179:107174. doi: 10.1016/j.lungcan.2023.03.010
40. Danckert B, Falborg AZ, Christensen NL, Frederiksen H, Lyratzopoulos G, McPhail S, et al. Routes to diagnosis and the association with the prognosis in patients with cancer - A nationwide register-based cohort study in Denmark. Cancer Epidemiol. (2021) 74:101983. doi: 10.1016/j.canep.2021.101983
41. Pettit NR, Li X, Stewart L, Kline J. Worsened outcomes of newly diagnosed cancer in patients with recent emergency care visits: A retrospective cohort study of 3699 adults in a safety net health system. Cancer Med. (2023) 12:4832–41. doi: 10.1002/cam4.5303
42. Tsang C, Bottle A, Majeed A, Aylin P. Cancer diagnosed by emergency admission in England: an observational study using the general practice research database. BMC Health Serv Res. (2013) 13:308. doi: 10.1186/1472-6963-13-308
43. Fauvel D, Alix, Bischof JJ, Reinbolt RE, Weihing VK, Boyer EW, Caterino JM, et al. Diagnosis of cancer in the Emergency Department: A scoping review. Cancer Med. (2023) 12:8710–28. doi: 10.1002/cam4.5600
44. Elliss-Brookes L, Mcphail S, Ives A, Greenslade M, Shelton J, Hiom S, et al. Routes to diagnosis for cancer – determining the patient journey using multiple routine data sets. Br J Cancer. (2012) 107:1220–6. doi: 10.1038/bjc.2012.408
45. Faiella A, Onofrio L, Liccardi F, Paladino F, Chiurazzi M, Riccardi F, et al. Oncological assistance in the emergency room setting: the role of a dedicated oncology unit. Int J Cancer Manage. (2021) 14:e110512. doi: 10.5812/ijcm.110512
46. Greene J. CONCERN for cancer. Ann Emergency Med. (2015) 66:A13–5. doi: 10.1016/j.annemergmed.2015.05.015
47. Kapadia P, Zimolzak AJ, Upadhyay DK, Korukonda S, Rekha RM, Mushtaq U, et al. Development and implementation of a digital quality measure of emergency cancer diagnosis. J Clin Oncol. (2024) 42(21):2506–15. doi: 10.1200/jco.23.01523
48. Farkas DT, Greenbaum A, Singhal V, Cosgrove JM. Effect of insurance status on the stage of breast and colorectal cancers in a safety-net hospital. Am J Manag Care. (2012) 18:Sp65–70. doi: 10.1200/JOP.2012.000542
49. Franzoi MA, Schwartsmann G, de Azevedo SJ, Geib G, Zaffaroni F, Liedke PER. Differences in breast cancer stage at diagnosis by ethnicity, insurance status, and family income in young women in the USA. J Racial Ethn Health Disparities. (2019) 6:909–16. doi: 10.1007/s40615-019-00591-y
Keywords: breast cancer, lung cancer, oral cancer, colorectal cancer, prostate cancer, emergency department, survival, cancer stage
Citation: Lin Y-C, Kuo W-Y, Kung P-T and Tsai W-C (2024) Proportion trends, cancer stage, and survival of patients with cancer diagnosed through emergency and nonemergency departments: a nationwide cohort study. Front. Oncol. 14:1399326. doi: 10.3389/fonc.2024.1399326
Received: 08 May 2024; Accepted: 05 August 2024;
Published: 26 August 2024.
Edited by:
Wen-Wei Sung, Chung Shan Medical University Hospital, TaiwanReviewed by:
Georgios Lyratzopoulos, University College London, United KingdomJanaki Deepak, University of Maryland, United States
Copyright © 2024 Lin, Kuo, Kung and Tsai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-Chen Tsai, d2N0c2FpMjAxMUBnbWFpbC5jb20=
†These authors have contributed equally to this work
 Ying-Chao Lin
Ying-Chao Lin Wei-Yin Kuo
Wei-Yin Kuo Pei-Tseng Kung
Pei-Tseng Kung Wen-Chen Tsai
Wen-Chen Tsai