- Department of Gastroenterology, The 909th Hospital, School of Medicine, Xiamen University, Fujian, China
Background: No previous studies have reported on the use of minimally invasive endoscopic therapy for colon cancer in older patients.
Case presentation: An 80-year-old man was admitted to our hospital with haematochezia and diagnosed with advanced colon cancer in 2018. Traditional surgical care was rejected by his family. We successfully treated the patient with multiple minimally invasive endoscopic therapies, such as argon plasma coagulation, from 2018 to 2021.
Conclusion: Invasive endoscopic therapy is a feasible way to treat colon cancer in older patients.
Introduction
Colorectal cancer (CRC) is the third most common cause of cancer mortality worldwide and the third leading cause of death in men aged over 80 years (1, 2). Older patients with CRC are often in an advanced stage at the time of diagnosis, losing the opportunity to undergo surgical treatment and substantially limiting their life expectancy. Moreover, many older patients have major comorbidities that may minimize or even negate the benefits of adjuvant chemotherapy or radiotherapy (3, 4). Choosing an appropriate method for treating CRC in older patients is a current challenge in clinical practice. This case report describes the successful treatment of an 80-year-old patient with advanced colon cancer using multi-stage endoscopic minimally invasive therapy with the intention of providing new ideas for the treatment of colon cancer in older patients.
Case presentation
An 80-year-old Asian man with haematochezia for 10 days was admitted to our hospital in Nov. 2018 and diagnosed with advanced colon cancer, protruded type, clinical stage T2N0M0 (Figure 1). Colonoscopy revealed a mass in the descending colon that blocked the lumen, and blocked passage of the endoscope (Figure 1A). The biopsy specimen was friable and bled easily. Histopathological examination (H&E staining) showed deeply stained irregular nuclei with necrotizing tumour cells and revealed adenocarcinoma (Figure 1B). Contrast-enhanced abdominal computed tomography showed a thickening confined to the descending colon wall and no metastasis to the lymph nodes or abdominal organs (Figures 1C, D). The man had hypertension and coronary artery disease for more than ten years, type 2 diabetes mellitus for more than six years, and had been on long-term medication (unspecified) for years. He did not have a history of surgery or radiation exposure, and his family history was unremarkable. Considering the age and health status of the patient, his family rejected traditional surgery and neoadjuvant therapy because of potential complications like wound infection and kidney injuries, leading to the shortage of lifespan. Therefore, we aimed to prevent luminal obstruction and maintain the patient’s quality of life by using a disposable polyp snare, endoscopic resection, and argon plasma coagulation (APC) to remove part of the tumour (Figures 2A, B) and then placing a stent using the colonoscope (Figure 2C). From April 2019 to February 2021, the patient underwent a colonoscopy six times for the tumour in our hospital, including polyp resection, electro-coagulation and electro-section, and APC (Supplementary Figure 1). The tumour size in the colon gradually decreased and no other complications developed (Figure 3). During the entire process, the patient did not receive any other therapy, including chemotherapy, radiotherapy, or traditional Chinese medicine. Surprisingly, a regular examination with colonoscopy in July 2021 showed that only postoperative scars were seen at the original tumour site, and no tumour proliferation was found (Figure 4A). One year later, in May 2022, the patient underwent colonoscopy and still showed no colon cancer recurrence (Figure 4B). And the follow-up examination by abdominal ultrasounds and chest X-ray also showed no metastases or other diseases from 2019 to 2022. However, we did not conduct the follow-up examination in 2023 because the patient could not tolerate the long car rides. Therefore, we phoned his family and were told the activity of daily living (ADL) in this patient was still well, and no warning symptoms of colon cancer had recurred until now.
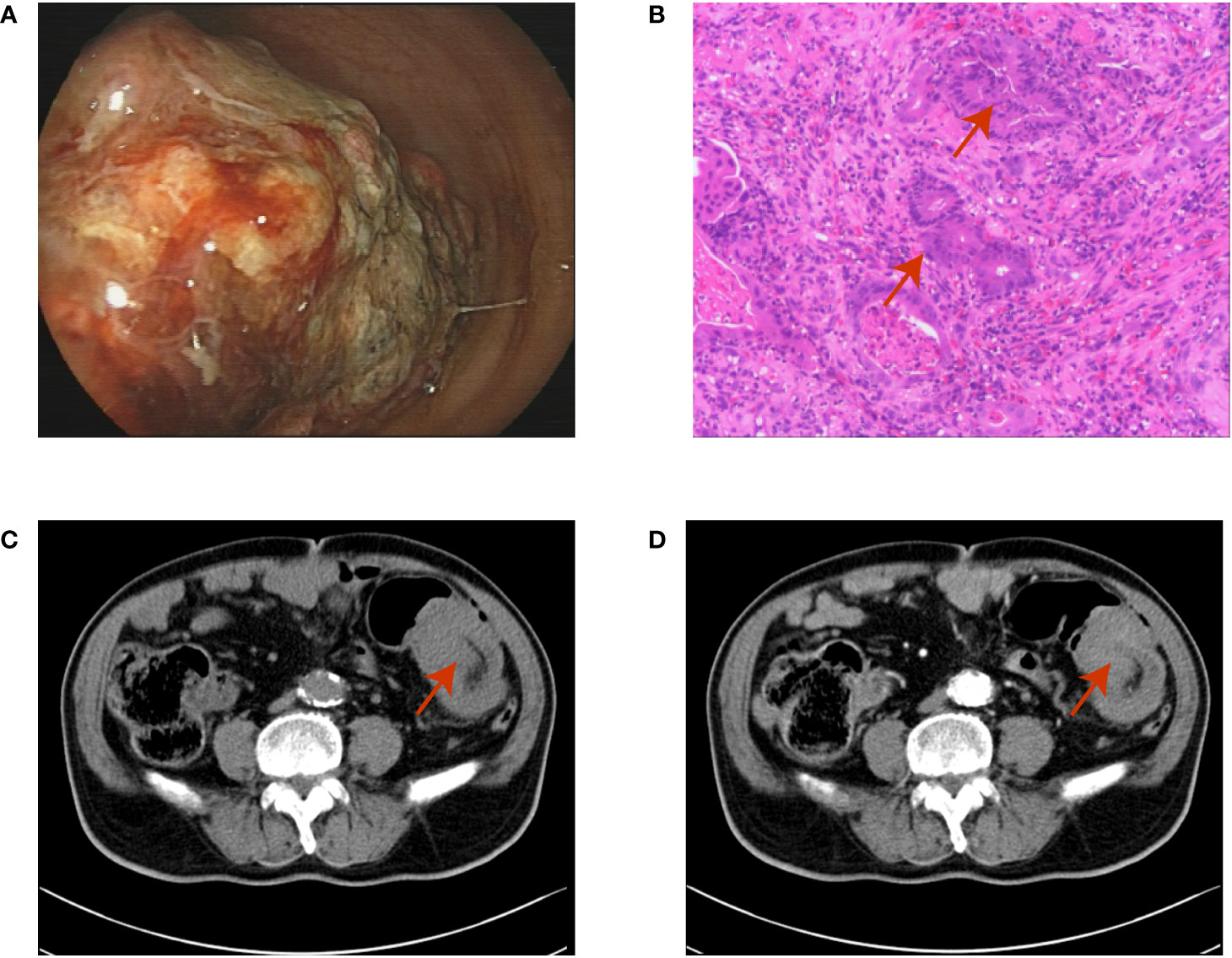
Figure 1 (A) The colonoscopy shows a mass blocked the lumen of the descending colon and the endoscope could not pass; (B) The haematoxylin-eosin staining of the biopsy shows adenocarcinoma (red arrow); (C, D) The contrast-enhanced abdominal computed tomography shows the colon wall thickening and the maximum cross-section of the mass is 4.4×7.0 mm (red arrow).
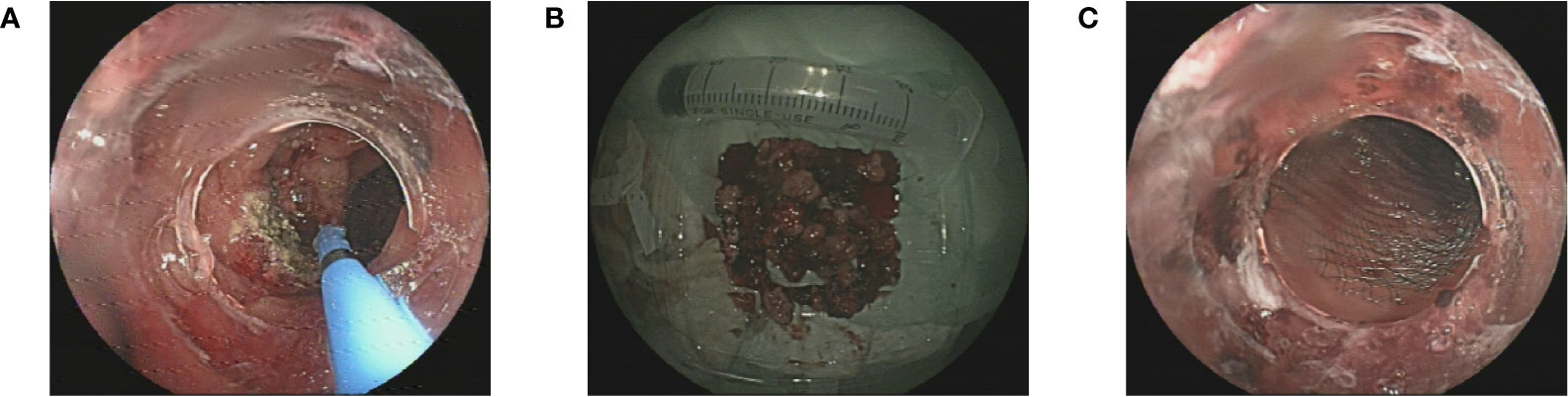
Figure 2 (A) The endoscopic resection and argon plasma coagulation of the tumour; (B) The excised tumour tissue; (C) The stent placed in the lumen.
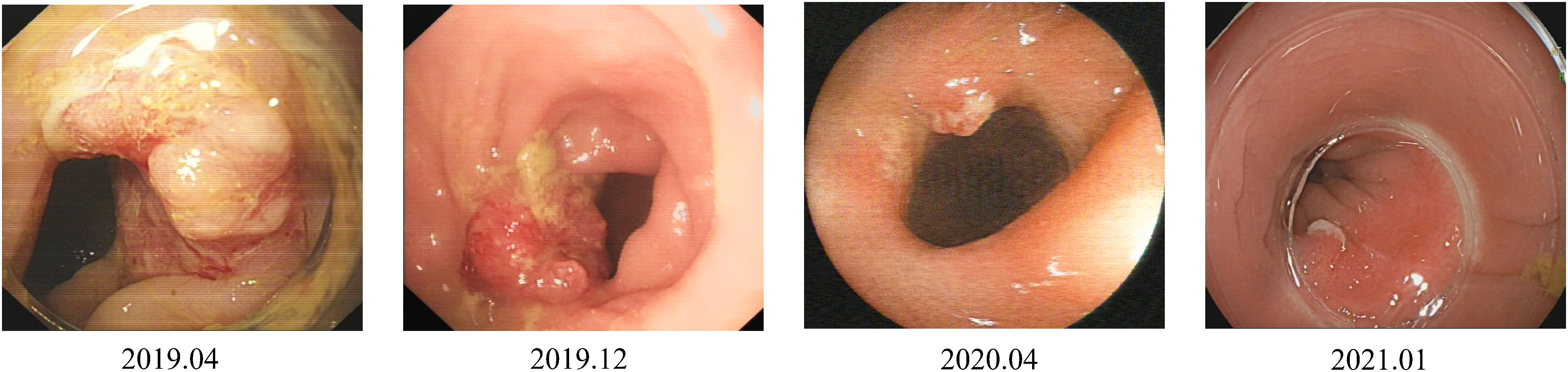
Figure 3 The size of the tumour in the colon has gradually shrunk over three years from 2019 to 2021 after endoscopic therapy.
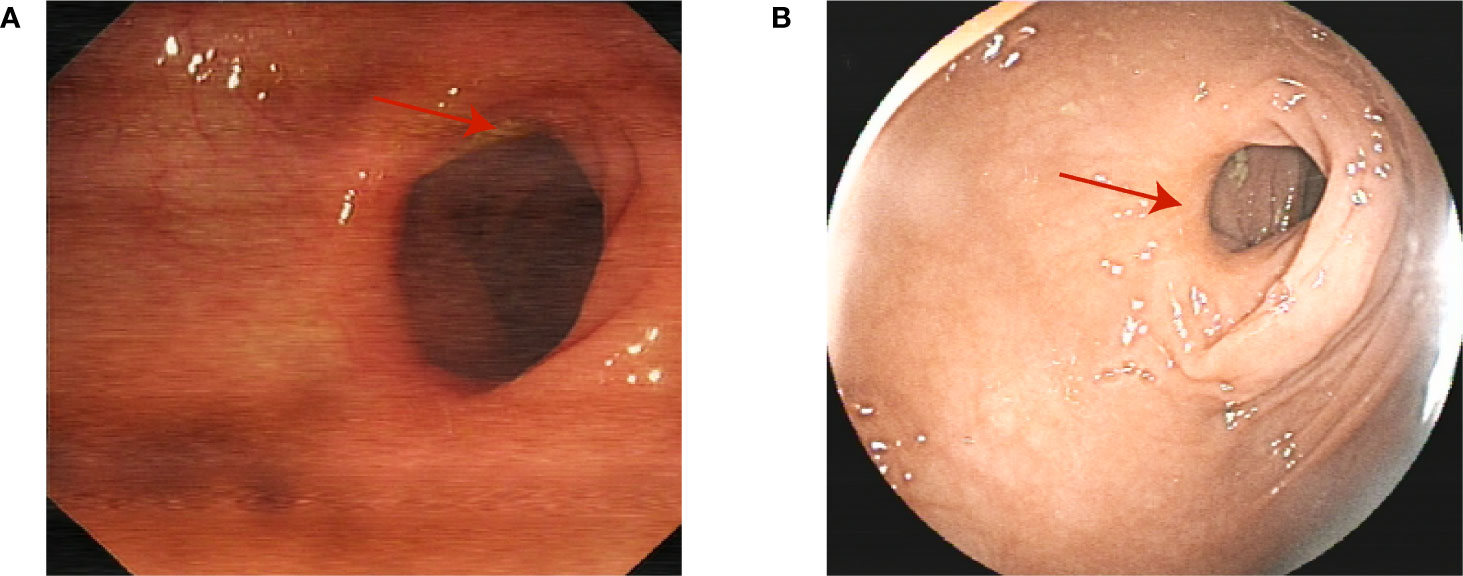
Figure 4 Scars are seen at the original tumour site in three (A) and four (B) years after the original diagnosis in 2018. (red arrow).
Discussion
To our knowledge, this is the first report of the successful treatment of colon cancer in an older man using multifrequency endoscopic minimally invasive therapy. Older patients diagnosed with advanced CRC are less likely to receive standard antitumour therapies, such as cytotoxic chemotherapy and biological therapy, and the proportion of patients receiving treatment declines with advanced age (5, 6). In this case, we originally aimed to prevent colonic obstruction by the tumour and to maintain the basic quality of life of the patient through endoscopic palliative care. However, the final successful treatment of cancer by multifrequency endoscopic resection provided an easily acceptable and low-risk protocol for the treatment of CRC in older patients.
Relevant literature was reviewed to explore potential reasons. Biller et al. reported that the 5-year survival rate of patients with metastatic CRC is less than 20% (7). The colon cancer in this patient was localised in the lumen when diagnosed and did not metastasise to the lymph nodes or distant sites. The recognition of warning symptoms and accurate diagnosis of colorectal cancer are important, and there were no signs of metastasis during the 4-year follow-up treatment and re-examination, providing an opportunity for long-term endoscopic invasive therapy. Endoscopic invasive therapy is less harmful and safer for older patients than traditional surgical care because of postoperative pain and the risk of complications such as wound infection and poor healing caused by the surgery (8). Older patients also are more liable to postoperative surgical site infections and poor recovery after colorectal surgery than young patients because of their poor nutritional absorption and weak resistance to pathogens (9–11). And the complications are reported to be associated with many adverse outcomes like increasing patient costs and length of hospital stay, promoting the incidence of sepsis, or even causing death (12, 13). Recently, minimally invasive endoscopic therapy has been considered for gastrointestinal tumours treatment (14–18). APC has been reported to be effective in treating superficial oesophageal squamous cell carcinoma in patients with severe concomitant disease (15). Endoscopic submucosal dissection (ESD) and endoscopic full-thickness resection (EFTR) have been found as available ways for early colorectal cancer confined to the mucosa or submucosa (16–18). The appropriate frequency of endoscopic therapy for this patient may also be one of the reasons for successful treatment. Moreover, the tumour location of this patient was in the descending colon, and Zhang et al. reported that the prognosis of patients with left-sided colon cancers was better than that of patients with right-sided colon cancers, regardless of stage (19), which may also have contributed to the successful treatment of the patient. Therefore, the primary location of the colon cancer, its staging, the accurate diagnosis and the appropriate choice of therapy were combined to account for the favourable outcome in this patient.
In conclusion, this case implies that invasive endoscopic therapy may be feasible to treat colon cancer in older populations. However, there are also limitations, such as how frequently and to what extent endoscopic resection should be performed and which older patients would benefit. Moreover, the early and accurate diagnosis of colon cancer is also vital to provide the chance for minimally invasive therapy, and some studies have reported deep learning algorithms have the potential to improve the accuracy and efficacy of CRC detection (20, 21). Therefore, further clinical practice and investigations are needed to apply deep learning algorithms to the classification and diagnosis of CRC and invasive endoscopic therapy for the therapy of CRC.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The Ethical Committee of the 909th hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
NZ: Conceptualization, Methodology, Software, Writing – original draft. LZ: Conceptualization, Methodology, Writing – original draft. YL: Conceptualization, Methodology, Writing – review & editing. XC: Writing – review & editing. BZ: Writing – review & editing. CW: Supervision, Writing – review & editing. HZ: Writing – review & editing. QT: Writing – review & editing. MZ: Methodology, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We thank the patient for his support of this case report, and thank Jiangbin Huang and Junyi Wang for the guidance to the pathologic diagnosis and clinically staging.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2024.1367173/full#supplementary-material
References
1. Wang Z, Dan W, Zhang N, Fang J, Yang Y. Colorectal cancer and gut microbiota studies in China. Gut Microbes (2023) 15(1):2236364. doi: 10.1080/19490976.2023.2236364
2. Hathout L, Maloney-Patel N, Malhotra U, Wang SJ, Chokhavatia S, Dalal I, et al. Management of locally advanced rectal cancer in the elderly: a critical review and algorithm. J Gastrointest Oncol (2018) 9(2):363–76. doi: 10.21037/jgo.2017.10.10
3. Muss HB, Biganzoli L, Sargent DJ, Aapro M. Adjuvant therapy in the elderly: making the right decision. J Clin Oncol (2007) 25(14):1870–5. doi: 10.1200/JCO.2006.10.3457
4. De Marco MF, Janssen-Heijnen ML, van der Heijden LH, Coebergh JW. Comorbidity and colorectal cancer according to subsite and stage: a population-based study. Eur J Cancer (2000) 36(1):95–9. doi: 10.1016/s0959-8049(99)00221-x
5. Luo R, Giordano SH, Freeman JL, Zhang D, Goodwin JS. Referral to medical oncology: a crucial step in the treatment of older patients with stage III colon cancer. Oncologist (2006) 11(9):1025–33. doi: 10.1634/theoncologist.11-9-1025
6. Schrag D, Gelfand SE, Bach PB, Guillem J, Minsky BD, Begg CB. Who gets adjuvant treatment for stage II and III rectal cancer? Insight from surveillance, epidemiology, and end results–Medicare. J Clin Oncol (2001) 19(17):3712–8. doi: 10.1200/JCO.2001.19.17.3712
7. Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal cancer: A review. JAMA (2021) 325(7):669–85. doi: 10.1001/jama.2021.0106
8. Teitelbaum EN, Swanstrom LL. Submucosal surgery: novel interventions in the third space. Lancet Gastroenterol Hepatol (2018) 3(2):134–40. doi: 10.1016/S2468-1253(17)30286-8
9. Panos G, Mulita F, Akinosoglou K, Liolis E, Kaplanis C, Tchabashvili L, et al. Risk of surgical site infections after colorectal surgery and the most frequent pathogens isolated: a prospective single-centre observational study. Med Glas (Zenica) (2021) 18(2):438–43. doi: 10.17392/1348-21
10. Tian Y, Li R, Wang G, Xu K, Li H, He L. Prediction of postoperative infectious complications in elderly patients with colorectal cancer: a study based on improved machine learning. BMC Med Inform Decis Mak (2024) 24(1):11. doi: 10.1186/s12911-023-02411-0
11. Martínez-Escribano C, Arteaga Moreno F, Pérez-López M, Cunha-Pérez C, Belenguer-Varea Á, Cuesta Peredo D, et al. Malnutrition and increased risk of adverse outcomes in elderly patients undergoing elective colorectal cancer surgery: A case-control study nested in a cohort. Nutrients (2022) 14(1):207. doi: 10.3390/nu14010207
12. Mulita F, Liolis E, Akinosoglou K, Tchabashvili L, Maroulis I, Kaplanis C, et al. Postoperative sepsis after colorectal surgery: a prospective single-center observational study and review of the literature. Prz Gastroenterol (2022) 17(1):47–51. doi: 10.5114/pg.2021.106083
13. Ramanathan ML, MacKay G, Platt J, Horgan PG, McMillan DC. The impact of open versus laparoscopic resection for colon cancer on C-reactive protein concentrations as a predictor of postoperative infective complications. Ann Surg Oncol (2015) 22(3):938–43. doi: 10.1245/s10434-014-4065-z
14. Park SU, Min YW, Shin JU, Choi JH, Kim YH, Kim JJ, et al. Endoscopic submucosal dissection or transanal endoscopic microsurgery for nonpolypoid rectal high grade dysplasia and submucosa-invading rectal cancer. Endoscopy (2012) 44(11):1031–6. doi: 10.1055/s-0032-1310015
15. Tahara K, Tanabe S, Ishido K, Higuchi K, Sasaki T, Katada C, et al. Argon plasma coagulation for superficial esophageal squamous-cell carcinoma in high-risk patients. World J Gastroenterol (2012) 18(38):5412–7. doi: 10.3748/wjg.v18.i38.5412
16. Ebigbo A, Probst A, Messmann H. Endoscopic treatment of early colorectal cancer - just a competition with surgery? Innov Surg Sci (2017) 3(1):39–46. doi: 10.1515/iss-2017-0037
17. Hong SW, Byeon JS. Endoscopic diagnosis and treatment of early colorectal cancer. Intest Res (2022) 20(3):281–90. doi: 10.5217/ir.2021.00169
18. Silva GL, de Moura EG, Bernardo WM, Leite de Castro V, Morais C, Baba ER, et al. Endoscopic versus surgical resection for early colorectal cancer-a systematic review and meta-analysis. J Gastrointest Oncol (2016) 7(3):326–35. doi: 10.21037/jgo.2015.10.02
19. Zheng C, Jiang F, Lin H, Li S. Clinical characteristics and prognosis of different primary tumor location in colorectal cancer: a population-based cohort study. Clin Transl Oncol (2019) 21(11):1524–31. doi: 10.1007/s12094-019-02083-1
20. Bousis D, Verras GI, Bouchagier K, Antzoulas A, Panagiotopoulos I, Katinioti A, et al. The role of deep learning in diagnosing colorectal cancer. Prz Gastroenterol (2023) 18(3):266–73. doi: 10.5114/pg.2023.129494
21. Chlorogiannis DD, Verras G, Tzelepi V, Chlorogiannis A, Apostolos A, Kotis A, et al. Tissue classification and diagnosis of colorectal cancer histopathology images using deep learning algorithms. Is the time ripe for clinical practice implementation. Prz Gastroenterol (2023) 18(4):353–67. doi: 10.5114/pg.2023.130337
Keywords: colonic neoplasms, aged, endoscopy, argon plasma coagulation, surgery
Citation: Zhang N, Zhu L, Liu Y, Chen X, Zhang B, Wen C, Zhang H, Tang Q and Zhang M (2024) Case report: Successful treatment of advanced colon cancer in an eighty-year-old man with long-term and multi-stage endoscopic minimally invasive therapy. Front. Oncol. 14:1367173. doi: 10.3389/fonc.2024.1367173
Received: 12 January 2024; Accepted: 18 January 2024;
Published: 20 February 2024.
Edited by:
Francesk Mulita, General University Hospital of Patras, GreeceReviewed by:
Spyros Papadoulas, General University Hospital of Patras, GreeceDimitrios Bousis, General University Hospital of Patras, Greece
Christos Pitros, General University Hospital of Patras, Greece
Copyright © 2024 Zhang, Zhu, Liu, Chen, Zhang, Wen, Zhang, Tang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingqing Zhang, em1xaW5nODA4NEBzaW5hLmNvbQ==
†These authors share first authorship
 Nana Zhang
Nana Zhang Lulu Zhu
Lulu Zhu Yan Liu
Yan Liu