
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 10 May 2024
Sec. Surgical Oncology
Volume 14 - 2024 | https://doi.org/10.3389/fonc.2024.1344662
 Weibi Che1†
Weibi Che1† Jian Zhong1†
Jian Zhong1† Jiawei Huang1†
Jiawei Huang1† Huilong Chen1
Huilong Chen1 Caihou Feng1
Caihou Feng1 Yujie Xie1
Yujie Xie1 Haiquan He1
Haiquan He1 Ying Chen1
Ying Chen1 Cui Li1
Cui Li1 Bomeng Wu1
Bomeng Wu1 Wei Ding2*
Wei Ding2* Wanli Lin1*
Wanli Lin1*Minimally invasive esophagectomy for cancer surgery remains associated with significant morbidity and surgical complications across the globe. Non-intubation video-assisted thoracic surgery (NIVATS) has been successfully employed in lung resection in recent years, but there are few reported cases with regard to the safety and feasibility of this approach in radical esophagectomy for patients with esophageal cancers. We present 4 consecutive cases with esophageal squamous cell carcinoma (ESCC) who received minimally invasive McKeown’s esophagectomy under non-intubation general anesthesia from November 2022 to April 2023. All these patients were aged from 55 to 75 years old and were pathologically diagnosed with ESCC. All procedures of McKeown’s esophagectomy in these patients were completed with non-invasive ventilation by laryngeal mask-assisted anesthesia. Operation duration ranged from 185 to 395 minutes and the estimated blood loss ranged from 25 to 60 ml in these 4 cases. No severe hypoxia was observed and transient hypercapnia was resolved intraoperatively. None of them was converted to endotracheal intubation with mechanical ventilation or to thoracotomy. The number of retrieved lymph nodes in mediastinum were 21-27 and all patients received R0 surgery with pathological stage as T1bN0M0 to T3N2M0. There was no serious complication (Clavien-Dindo grade III-IV) observed perioperatively and they were all discharged 11-14 days after the surgery with resumption of oral feeding. They are all alive without tumor recurrence at the date of data collection. The safety and efficacy of minimally invasive esophagectomy with non-invasive ventilation by laryngeal mask-assisted anesthesia for patients with ESCC are warranted for explored in a larger cohort study.
Although esophagectomy is the cornerstone of treatment for patients with esophageal cancers, it is notorious for its high invasiveness and high mortality rate (1). Esophagectomy with double-lumen endotracheal intubation and one lung mechanical ventilation is the preferred approach in esophageal surgery at most cancer center (2). Great efforts have been made, for instance, total minimally invasive esophagectomy and robotic-assisted esophagectomy, to minimize the influence of radical esophagectomy on the physical function in patients with esophageal cancers in recent years (3). But the complication rate remains 41%-48%, with major complication (Clavien-Dindo classification ≥ III) ranged from 10%-12% (4), revealing that to shorten the recovery time after esophagectomy and reduce the incidence of postoperative complication still challenge the anesthetist and surgeons. Nonintubated video-assisted thoracoscopic surgery recently has been demonstrated to be a safe and feasible approach for various thoracic diseases (5, 6), but the application of this procedure in esophageal surgery has not been well depicted.
We report a case series who received radical esophagectomy with non-intubation general anesthesia and discontinuous spontaneous ventilation. These four patients were admitted with progressive dysphagia. After histopathological diagnosis with esophageal squamous cell carcinoma (ESCC) by gastroscopy, these patients routinely received preoperative examinations including enhanced contrast CT, cardiovascular ultrasound, pulmonary function and so on to rule out contraindication for radical esophagectomy. These patients were diagnosed with locally advanced ESCC (cT1b-3N1-2M0) and refused neoadjuvant therapy. Minimally invasive esophagectomy and two field lymphadenectomy under non-incubated anesthesia with discontinuous spontaneous ventilation was performed after acquisition of informed consents. This anesthesia procedure was approved by the Institutional Review Board of our hospital.
The non-intubated anesthesia with discontinuous spontaneous ventilation was accomplished by laryngeal mask (Figure 1). During the thoracic phrase, as shown in Figure 1, manipulation holes for the operator were placed in the seventh intercostal space at the right middle axillary line (10mm) and the fourth intercostal space at right posterior axillary line (5mm). The manipulation hole for the assistant was placed in the fourth intercostal space at right anterior axillary line by enlarging the trocar incision (4cm). The observational hole was placed in the sixth intercostal space at the right middle axillary line (10mm). 2% Lidocaine was sprayed on the lung surface and visceral pleura (Figure 2) and intrathoracic vagal nerve blockade was performed by injection of 2% lidocaine into the right intrathoracic vagal nerve trunk at the beginning of surgery (Figure 3). During the thoracic phase, on the basis of keeping oxygen saturation above 90%, spontaneous respiration frequency was controlled to 10-15 times/min and the tidal volume 200-300 mL in order to reduce the mediastinal oscillation and produce a greater surgical field. In addition, the integrity of contralateral mediastinal pleura was ensured during the whole process of esophagus dissociation for preventing contralateral pneumothorax. Abdominal surgery was successfully completed with CO2 pneumoperitoneum pressure controlled < 13 mmHg and mechanical anastomosis between tubular stomach and cervical esophagus was achieved in all these patients.

Figure 1 Non-intubation general anesthesia with spontaneous ventilation was performed by laryngeal mask.
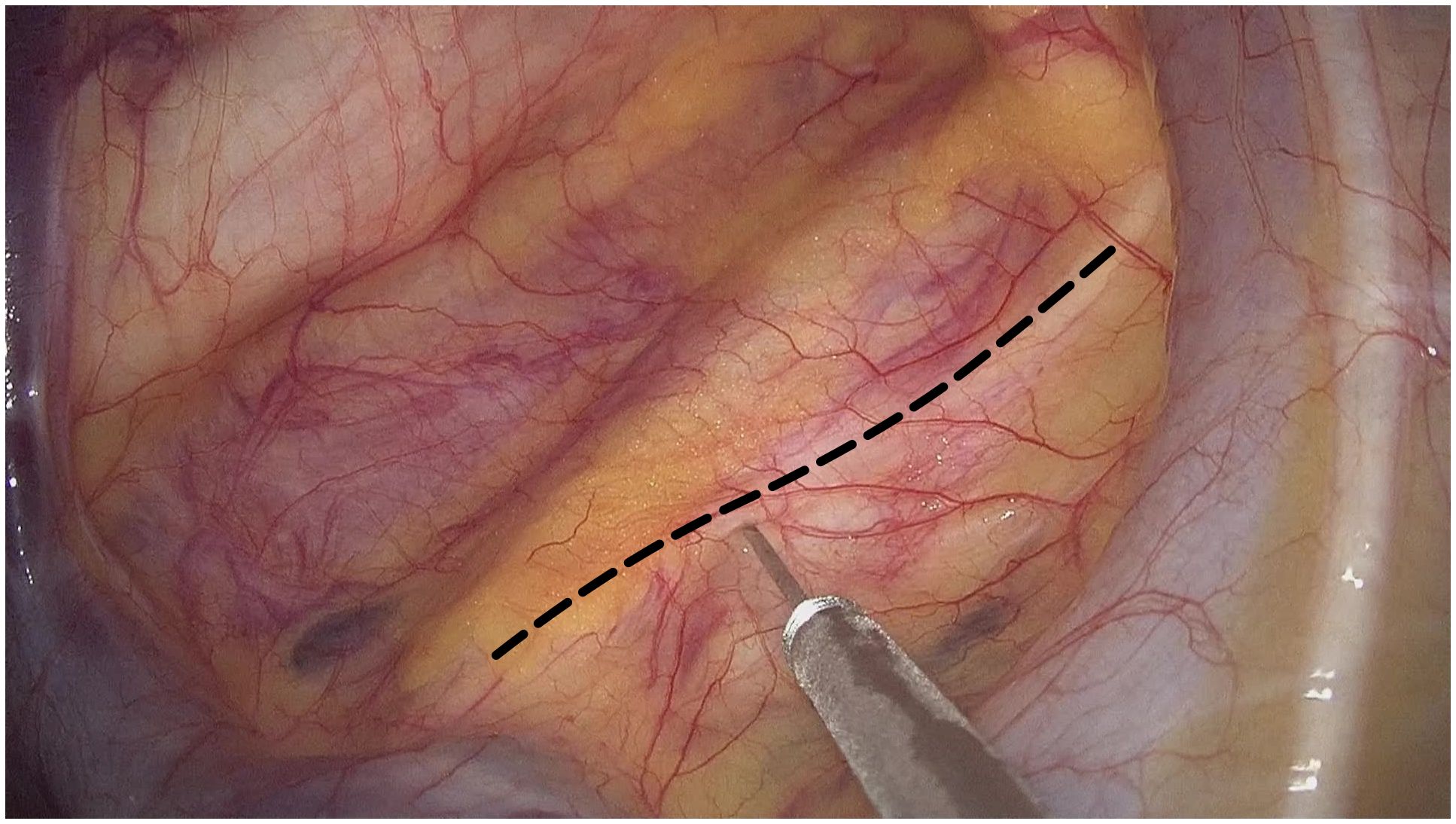
Figure 3 2% lidocaine was injected into the right intrathoracic vagal nerve trunk (black dotted line) at the beginning of thoracic phrase in the operation.
In our cancer center, the adjustment of pulmonary ventilation parameters during the operation mainly follows the principle: to maintain a relative shallow and fast breathing is conducive to the manipulation of the surgeon. If tidal volume of the patient is too large, which affects the manipulation of surgeon, a small dose of cisatracurium (1mg) will be administered intravenously to reduce the tidal volume, and manual assisted ventilation will be used if necessary. The reference for adjusting pulmonary ventilation parameters is to keep carbon dioxide partial pressure (PaCO2) less than 80mmHg. Tracheal intubation with a single-lumen endotracheal tube was always prepared for emergency situations during all the surgical procedure, however, all surgical processes were accomplished without conversion to endotracheal intubation.
In our hospital, preoperative preparation involves educating patients on mastering the correct and effective coughing techniques in order to ensure the efficient clearance of respiratory secretions postoperatively. The postoperative recuperation measures encompass respiratory tract management (sputum aspiration by fibrobronchoscopy if necessary) and individually tailored early enteral and parenteral nutritional support, which is primarily overseen by the Department of Nutrition.
The characteristics and perioperative parameters of the four patients were show in Table 1. All these patients received R0 esophagectomy and developed no distinct postoperative complications (Clavien-Dindo grade III-IV (7)) including anastomosis leakage and hoarseness. Without evidence of anastomosis leakage in barium meal examination 7-8 days after surgery, oral intake was resumed in all patients and they were discharged 11 to 14 days after surgery (Table 1). The number of resected lymph nodes in mediastinum were 21-27, while the number of resected lymph nodes in total were 31-37. The highest and lowest intraoperative oxygen saturation and the peak end-tidal carbon dioxide (EtCO2) and PaCO2 were reported in Table 1, this result revealed that safety of the NIVATS depended on pulmonary ventilation (PaCO2) but rather than oxygen saturation.
With regard to the adjuvant therapy, Case 4 received concurrent radiochemotherapy 2 months postoperatively. According to the schedule, these patients are recommended for follow up in the outpatient clinic every 3 months for the first 2 years after the surgery, every 6 months for the next 3 years, and annually thereafter. Until the date of data collection (10 October 2023), there has no neoplasm been detected by computed tomography (CT) in the thoracic cavity and upper abdomen, and enlarged supraclavicular lymph nodes have not been detected in the neck. There was a minimal amount of pleural effusion discovered in one patient’s CT scan (Case 2), however, as the patient did not exhibit any symptoms such as dyspnea or other related discomfort, no immediate corrective measures were deemed necessary.
Non-intubated video-assisted thoracic surgery (NIVATS) has been successfully performed in lobectomy and segmentectomy in recent years (8). Moreover, NIVATS is favor to conventional intubation surgery for less invasiveness and shorter recovery time postoperatively (9), but the safety and efficacy of NIVATS in esophagectomy for esophageal cancers remains unclear. Exploration of this report contributed to provide a deep insight into the practice of NIVATS with discontinuous spontaneous ventilation in patients with esophageal cancers. Theoretically, this approach with non-invasive ventilation by laryngeal mask-assisted anesthesia may benefit from diminished residual effects of muscle relaxants on systemic autonomic nerves and facilitating postoperative recovery.
None of the four patients converted to endotracheal intubation with one lung mechanical ventilation in this study, albeit with conversion rate of 1-2% reported by Zhihua Guo and colleagues (10). Although the peak EtCO2/PaCO2 during operation was 51-63 mmHg in these four cases, this transitory hypercapnia resolved by increasing ventilation manually was permissive, given that moderate hypercapnia with EtCO2 50-60 mmHg is helpful to improve lung oxygenation without compromise with hemodynamics and surgical maneuvers (11). Laryngeal mask has been proved to be safe in esophagectomy, but the successful airway management require the careful observation of anesthetist to prevent aspiration and air leakage (12). So there is no doubt that an experienced team of surgeons, anesthetists and nurses is the key point of a successful NIVATS (13). There is no consensus about the indication for the standard tracheal intubation in esophagectomy with NIVATS. In addition, NIVATS was performed in selected patients in our cancer center, we haven’t encountered any situation that requires conversion to tracheal intubation during NIVATS so far. Therefore, the indications for conversion to tracheal intubation mentioned below are based on our surgical experience but not the surgical accidence we have faced during the operation. The potential indications for conversion to tracheal intubation are: 1) esophagus cannot be effectively mobilized due to the violent mediastinal oscillation during thoracic phrase; 2) persistent hyoxemia or carbon dioxide retention due to the limited pulmonary ventilation is observed.
The number of retrieved lymph nodes in mediastinum was 21-27, suggesting that thorough lymphadenectomy was capable in minimally invasive esophagectomy under NIVATS, as described in lobectomy and segmentectomy by Jun Liu et al. (7). We carefully selected these four patients with BMI < 25kg/m2 given that obesity patients with BMI > 30kg/m2 have the anatomical disadvantage of smaller thoracic cavity causing by higher mediastinum-to-chest ratio and a higher position of the diaphragm (14). The extent of lymph node resection in esophagectomy under NIVATS for obesity patients remains to be further explored.
Intriguingly, it is reported that NIVATS with spontaneous ventilation is associated with a higher proportion of natural-killer cells and total lymphocyte count postoperatively than those with endotracheal intubation anesthesia and mechanical one lung ventilation (15). One possible explanation is that mechanical one lung ventilation increases the alveolar concentrations of proinflammatory mediators, e.g. interleukin-6 and tumor necrosis factor-α, which may spillover into systemic circulation and play a vital role on the postoperative lymphocyte response and natural-killer activity (16). At the date of data collection in this report, there is no recurrence detected in these four patients, but whether or NIVATS with spontaneous ventilation has an impact on the immune cells and the clinical outcomes in esophagectomy is an interesting investigation in the future.
Given that the utilization of robotic assisted esophagectomy offers distinct advantages, including higher lymph nodes harvest number but rather than length of hospital stay and other perioperative outcomes (17, 18). As such, the potential synergy between NIVATS and robotic esophagectomy in further accelerating recovery warrants exploration.
The minimally invasive esophagectomy with NIVATS may avoid the potential complications that intubation may result in, and may be helpful to judge the reason of postoperative hoarseness. On the other hand, patients may benefit from the reduced residual effects of muscle relaxants which may contribute to promote the postoperatively effective and self-directed expectoration and then reduce the pulmonary complications. This approach was alignment with the core idea of enhanced recovery pathways. According to our limited data, the short-term oncology outcomes were comparable to the standard techniques with tracheal intubation, but there is no doubt that the safety and feasibility of this NIVATS is warranted to be determined.
Our study has several limitations. Firstly, it is a retrospective report with a relative small sample size. Therefore, our results need further validation in larger samples with direct comparison to standard tracheal intubation approach. All included patients did not receive lung function test postoperatively which prevent us from analyzing the characteristic of NIVATS in protecting lung function. Moreover, the short follow-up duration precludes recurrence and survival analysis of this study. But the major objective of this report was to explore the primary feasibility of this approach, the recurrent data and survival analysis will be reported in the future.
Minimally invasive esophagectomy with non-invasive ventilation by laryngeal mask-assisted anesthesia is probably a promising alternative approach for selected patients with ESCC. The exploration of safety and effectiveness for this approach in a larger scale study is warranted.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by the Ethics Committee of Gaozhou People’s Hospital (GYLLPJ-2023092). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
WC: Writing – original draft, Investigation, Data curation, Conceptualization. JZ: Writing – original draft, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation. JH: Writing – original draft, Software, Methodology, Formal analysis, Data curation. HC: Writing – original draft, Methodology, Data curation. CF: Writing – original draft, Resources, Methodology, Data curation. YX: Writing – original draft, Resources, Formal analysis. HH: Writing – original draft. YC: Writing – original draft, Resources, Formal analysis. CL: Writing – original draft, Resources, Methodology. BW: Writing – original draft, Resources. WD: Writing – review & editing. WL: Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Grant M202225 from the Science and Technology program of Guangdong Institute of Esophageal Cancer and Grant Q202307 from the Science and Technology program of Guangdong Institute of Esophageal Cancer.
We appreciate all participating patients and contributing staff members in our hospital.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ESCC, esophageal squamous cell carcinoma; EtCO2, end-tidal carbon dioxide; NIVATS, Non-intubated video-assisted thoracic surgery; SPO2, oxyhemoglobin saturation by pulse oximetry.
1. Yoshida N, Yamamoto H, Baba H, Miyata H, Watanabe M, Toh Y, et al. Can minimally invasive esophagectomy replace open esophagectomy for esophageal cancer? Latest analysis of 24,233 esophagectomies from the Japanese national clinical database. Ann Surg. (2020) 272:118–24. doi: 10.1097/SLA.0000000000003222
2. Bonavina L, Asti E, Sironi A, Bernardi D, Aiolfi A. Hybrid and total minimally invasive esophagectomy: How I do it. J Thorac Dis. (2017) 9:S761–72. doi: 10.21037/jtd
3. Hoelzen JP, Sander KJ, Sesia M, Roy D, Rijcken E, Schnabel A, et al. Robotic-assisted esophagectomy leads to significant reduction in postoperative acute pain: A retrospective clinical trial. Ann Surg Oncol. (2022) 29:7498–509. doi: 10.1245/s10434-022-12200-0
4. Yang Y, Li B, Yi J, Hua R, Chen H, Tan L, et al. Robot-assisted versus conventional minimally invasive esophagectomy for resectable esophageal squamous cell carcinoma: early results of a multicenter randomized controlled trial: the RAMIE trial. Ann Surg. (2022) 275:646–53. doi: 10.1097/SLA.0000000000005023
5. Noda M, Okada Y, Maeda S, Kondo T. Successful thoracoscopic surgery for intractable pneumothorax after pneumonectomy under local and epidural anesthesia. J Thorac Cardiovasc Surg. (2011) 141:1545–7. doi: 10.1016/j.jtcvs.2010.10.021
6. Zhu Y, Wang G, Gao W, Lin M, Li Y, Wang J, et al. Phrenic nerve block during nonintubated video-assisted thoracoscopic surgery: A single-centre, double-blind, randomized controlled trial. Sci Rep. (2021) 11:13056. doi: 10.1038/s41598-021-92003-7
7. Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. (2004) 240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae
8. Liu J, Cui F, Pompeo E, Gonzalez-Rivas D, Chen H, Yin W, et al. The impact of non-intubated versus intubated anaesthesia on early outcomes of video-assisted thoracoscopic anatomical resection in non-small-cell lung cancer: A propensity score matching analysis. Eur J Cardiothorac Surg. (2016) 50:920–5. doi: 10.1093/ejcts/ezw160
9. Wen Y, Liang H, Qiu G, Liu Z, Liu J, Ying W, et al. Non-intubated spontaneous ventilation in video-assisted thoracoscopic surgery: A meta-analysis. Eur J Cardiothorac Surg. (2020) 57:428–37. doi: 10.1093/ejcts/ezz279
10. Guo Z, Yin W, Wang W, Zhang J, Zhang X, Peng G, et al. Spontaneous ventilation anaesthesia: Total intravenous anaesthesia with local anaesthesia or thoracic epidural anaesthesia for thoracoscopic bullectomy. Eur J Cardiothorac Surg. (2016) 50:927–32. doi: 10.1093/ejcts/ezw209
11. Joe Y-E, Lee CY, Kim N, Lee K, Kang SJ, Oh YJ. Effect of permissive hypercarbia on lung oxygenation during one-lung ventilation and postoperative pulmonary complications in patients undergoing thoracic surgery: A prospective randomised controlled trial. Eur J Anaesthesiol. (2023) 40:691–8. doi: 10.1097/EJA.0000000000001873
12. Zhang R-X, Li Y, Liu X-B, Lu X-H, Sun H-B, Wang Z-F, et al. Is laryngeal mask airway general anesthesia feasible for minimally invasive esophagectomy? J Thorac Dis. (2018) 10:E210–3. doi: 10.21037/jtd
13. Metelmann I, Broschewitz J, Pietsch U-C, Huschak G, Eichfeld U, Bercker S, et al. Procedural times in early non-intubated VATS program - a propensity score analysis. BMC Anesthesiol. (2021) 21:44. doi: 10.1186/s12871-021-01270-4
14. Wang M-L, Galvez C, Chen J-S, Navarro-Martinez J, Bolufer S, Hung M-H, et al. Non-intubated single-incision video-assisted thoracic surgery: A two-center cohort of 188 patients. J Thorac Dis. (2017) 9:2587–98. doi: 10.21037/jtd
15. Vanni G, Tacconi F, Sellitri F, Ambrogi V, Mineo TC, Pompeo E. Impact of awake videothoracoscopic surgery on postoperative lymphocyte responses. Ann Thorac Surg. (2010) 90:973–8. doi: 10.1016/j.athoracsur.2010.04.070
16. Schilling T, Kozian A, Senturk M, Huth C, Reinhold A, Hedenstierna G, et al. Effects of volatile and intravenous anesthesia on the alveolar and systemic inflammatory response in thoracic surgical patients. Anesthesiology. (2011) 115:65–74. doi: 10.1097/ALN.0b013e318214b9de
17. Ekeke CN, Kuiper GM, Luketich JD, Ruppert KM, Copelli SJ, Baker N, et al. Comparison of robotic-assisted minimally invasive esophagectomy versus minimally invasive esophagectomy: A propensity-matched study from a single high-volume institution. J Thorac Cardiovasc Surg. (2023) 166:374–382.e1. doi: 10.1016/j.jtcvs.2022.11.027
Keywords: esophageal squamous cell carcinoma, non-intubation, spontaneous ventilation, minimally invasive esophagectomy, case report
Citation: Che W, Zhong J, Huang J, Chen H, Feng C, Xie Y, He H, Chen Y, Li C, Wu B, Ding W and Lin W (2024) Minimally invasive esophagectomy with non-invasive ventilation by laryngeal mask-assisted anesthesia for esophageal squamous cell carcinoma: case report. Front. Oncol. 14:1344662. doi: 10.3389/fonc.2024.1344662
Received: 26 November 2023; Accepted: 08 April 2024;
Published: 10 May 2024.
Edited by:
Mingzhou Guo, People’s Liberation Army General Hospital, ChinaReviewed by:
Savvas Lampridis, Imperial College London, United KingdomCopyright © 2024 Che, Zhong, Huang, Chen, Feng, Xie, He, Chen, Li, Wu, Ding and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Ding, NjE0MjEzODQ3QHFxLmNvbQ==; Wanli Lin, d2FubGlsaW4yMDIwQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.