
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol., 14 June 2023
Sec. Head and Neck Cancer
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.920889
Objective: To investigate the incidence of complications and types of chemoradiotherepy induces symptom clusters in patients with nasopharyngeal carcinoma (NPC) who were first diagnosed after treatment and discharged from hospital.
Methods: After their discharge home, 130 NPC patients who had been treated with chemoradiotherapy were asked to complete a modified Chinese version of the Quality of Life Questionnaire–Head and Neck Module developed by the European Organization for the Research and Treatment of Cancer in the Head and Neck. Symptom clusters in patients were identified through exploratory factor analysis.
Results: The most serious symptoms for discharged NPC patients who had received chemoradiotherapy were dental problems, a sense of obstruction while swallowing, embarrassment in physical contact with family members and friends, difficulty in speaking with others, and embarrassment in public. The six symptom clusters identified through exploratory factor analysis were (1) painful eating, (2) social difficulties, (3) psychological disorders, (4) symptomatic shame, (5) teeth/throat injuries, and (6) sensory abnormalities. The total contribution rate of variance was 65.73%.
Conclusion: NPC patients who are treated with chemoradiotherapy can experience adverse symptom clusters that continue after discharge. Nurses should evaluate the patients’ symptoms before discharge and provide targeted health education services which would reduce the patients’ complications and improve the quality of life at home. Besides, medical staff should evaluate the complications in a timely and comprehensive manner and provide individualized health education for the affected patients to help them manage chemoradiotherapy side effects.
Nasopharyngeal carcinoma (NPC) is the primary malignant tumor of the head, neck, and the epithelium that covers the nasopharyngeal mucosa. It is reported that the incidence of NPC is 1 in 100,000 (1). In China, 80% of NPC occurs in Guangdong, Guangxi, and other locations in South China; 92% of the newly-diagnosed cases are also located in these areas (2). Radiotherapy combined with adjuvant chemotherapy is the primary therapeutic method for NPC. The side effects of chemoradiotherapy for NPC are including early and long-term effects (3). Early side effects present during the process of therapy and during the immediate post therapy period, mucositis is the most common early side-effect to the oral mucosa with severe pain, impaired swallowing and malnutrition (4, 5). Late effects can occur from weeks to several years after its completion including xerostomia and dysgeusia, hearing loss, consistent xerostomia, mandibular osteoradionecrosis and dysphagia (6, 7). Serious complications may interrupt the treatment, affect the therapeutic results, shorten the interval of tumor recurrence, and affect the patients’ quality of life.
The complications caused by chemotherapy occur in the form of symptom clusters that severely affect the quality of life of NPC patients. Liao et al. (8) found that patients discharged after NPC chemoradiotherapy asked for further health education. The patient’s discharge might be delayed for days or even weeks due to serious complications such as myelosuppression and gastrointestinal reactions. The medical staff should be aware of the patients’ complications before the end of treatment so that the patients may undertake effective self-care as they return to their homes, families, and social roles. This study will provide a theoretical basis for the clinical management of cluster symptoms resulting from chemoradiotherapy side effects in NPC patients.
Using a convenience sampling method, 130 patients with NPC were enrolled in the study. They had been treated in The People's Hospital of Guangxi Zhuang Autonomous Region, Guangxi Academy of Medical Sciences from April to November 2017. The authors interviewed NPC patients 48 hours after hospital discharge to assess their symptom clusters. The patients had received the same therapeutic protocols:
Radiotherapy: A linear accelerator was used for intensity-modulated radiotherapy with an average dose of 72Gy/7~8W.
Chemotherapy: Two cycles of chemotherapy with platinum + 5-fluorouracil were administered. A micropump continuously injected 5-fluorouracil for 120 hours and once every 28 days. The regime of chemotherapy was cisplatin (30 mg/m2 per day for 3 days)with 5-fluorouracil (2000 mg/m2 for 5 days) in this cohort.
Patients were selected for the study using the following criteria:
Inclusion criteria: (1) first-time NPC patients diagnosed by histopathology who underwent chemoradiotherapy, (2) no additional malignant tumors, (3) conscious and able to communicate normally. (4) The Karnofsky Performance Status (KPS) of all patients recruited were more than 80.
Exclusion criteria: (1) age less than 18 years old, (2) hearing impairments, and (3) deceased or unable to complete the study for other reasons.
The authors interviewed NPC patients 48 hours within hospital discharge to assess their symptom clusters. After unified training, questionnaires were distributed by two research nurses with master’s degree. The questionnaires were completed face-to-face with the patients, 48 hours before discharge, and collected. At the beginning of the survey, the purpose of the study was explained, and each item was clarified to ensure full understanding by the respondent. If the patient had a vision impairment or physical limitations, the investigators read the questions. A total of 130 questionnaires were issued and 130 valid questionnaires were returned. The effective recovery was 100%.
The questionnaire included demographic data (gender, age, nationality, occupation, educational background, and marital status) and disease-related information (body mass index, smoking and drinking history, therapeutic protocols, and pathological staging).
The researchers used a modified Chinese version of the Quality of Life Questionnaire–Head and Neck Module, developed by the European Organization for the Research and Treatment of Cancer in the Head and Neck (EORTC QLQ-H&N35).
The 35 questions include seven symptomatic domains (head and neck pain, swallowing function, sense, speech, social eating, social contact, and sexuality) and eleven single-symptom items (dental effects, mouth movements, dry mouth, sticky saliva, coughing, ill-feeling, use of pain killer, nutritional supplements, feeding tube, weight gain, and weight loss). Items 1 to 30 are scored from 1 to 4 according to four Likert’s grades: “no,” “a little,” “equivalent,” and “unusual.” Items 31 to 35 are scored “yes” or “no.” A higher score equals more severity in the symptom area and a diminished quality of life. The Cronbach’s coefficient α of the scale was 0.623~0.970, indicating good reliability and validity (9). This study used the first 30 symptoms of the QLQ-H&N35 to extract the symptom clusters.
SPSS20.0 software was used for statistical analysis. The general characteristics of the patients were labeled by the descriptive statistics, and the counting data were described by frequency, ratio, or percentage. Measurement data subject to a normal distribution used means ± standard deviation. For measurement data not subject to normal distribution, M(P25, P75) was adopted in the statistical description. Exploratory factor analysis was used for the symptom clusters.
The general characteristics of the NPC patients are presented in Table 1.
At the end of treatment, patients had the highest incidence in eight of the 30 QLQ-H&N35 symptoms: dry mouth (98.5%), difficulty in swallowing (96.9%), sticky saliva (96.9%), aversion to eating (96.9%), abnormal taste (96.2%), sore throat (93.1%), ill-feeling (92.3%), and difficulty in eating (86.9%). The symptoms with the highest severity and their M(P25,P75) scores were dental problems: 94.5 (32.0, 94.5); a feeling of obstruction while swallowing: 92.0 (44.5, 92.0); embarrassment during physical contact with family and friends: 89.0 (30.0, 89.0); difficulty in speaking: 87.5 (31.5, 87.5); and embarrassment in public: 87.5 (27.0, 87.5) (Table 2).
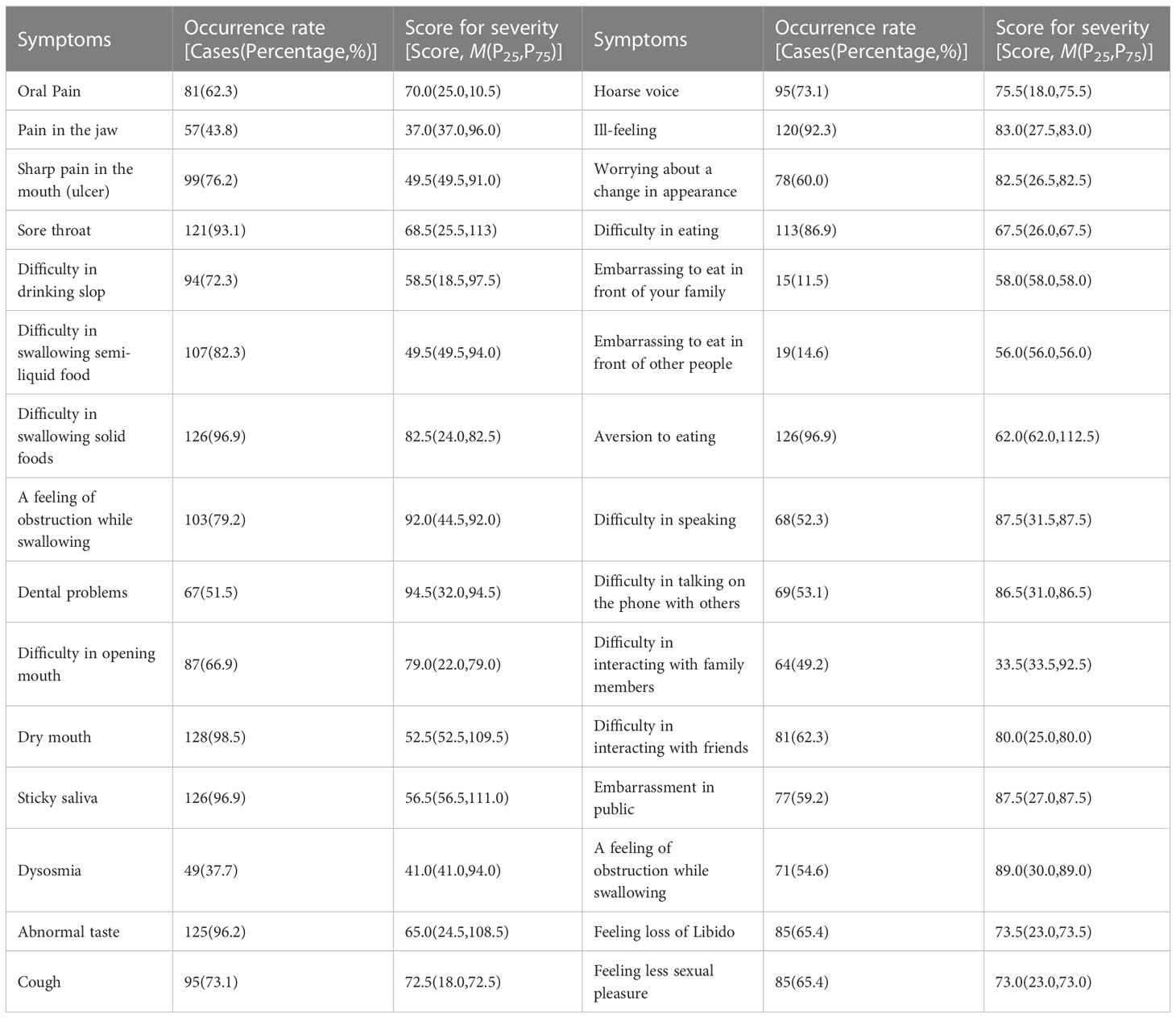
Table 2 The incidence of complications and the severity after the completion of treatment in patients with NPC (n=130).
The calculation of the exploratory factor analysis was performed using the principal component analysis and maximum variance rotation. In the Kaiser-Meyer-Olkin test, KMO = 0.829. The Bartlett sphericity test of P < 0.001 suggested that the data in the present study were suitable for factor analysis. Six factors with an eigenvalue > 1.3 were extracted for analysis. The total contribution rate of variance was 65.73%. The symptoms with a factor load > 0.6 were included in the symptom clusters. The six symptom clusters had high internal reliability, and the Cronbach’s α coefficients were 0.903, 0.937, 0.881, 0.969, 0.609, and 0.497, respectively. The load component matrix of the symptom cluster factors after rotation is shown in Table 3.
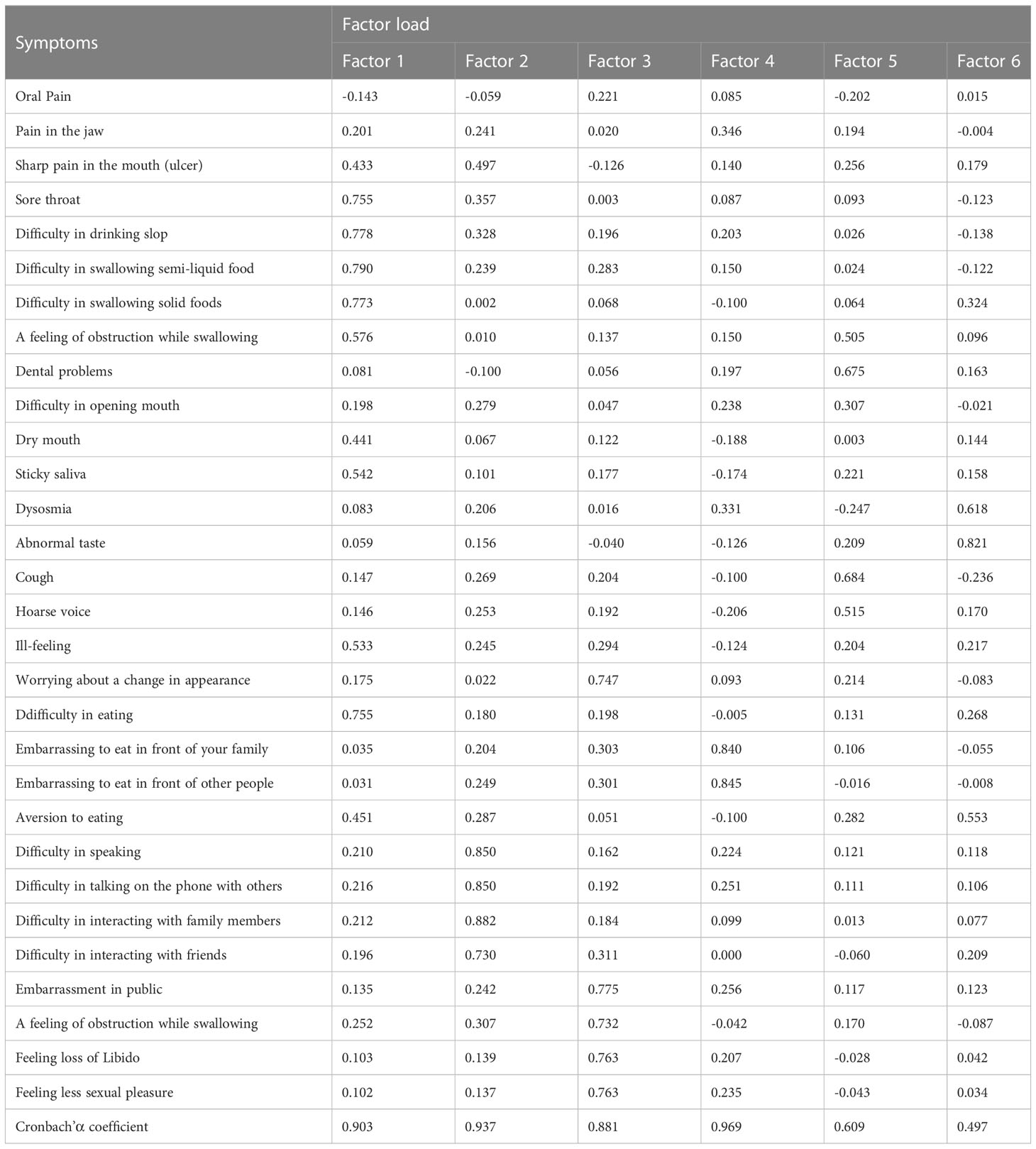
Table 3 Analysis of symptom clusters in admitted patients with NPC after the completion of treatment (n=130).
According to the factor load after rotation, the following six symptom clusters were evident in the present study: Factor 1: painful eating and swallowing (sore throat, difficulty in drinking liquid, difficulty in swallowing semiliquid food, and difficulty in swallowing solid food); Factor 2: social anxiety difficulties (speaking with others, speaking on the phone, and socializing with friends and family members); Factor 3: psychological disorders (worried about changes in appearance, embarrassed to appear in public, embarrassed to have physical contact with family members and friends, decreased sexual desire, and decreased pleasure in sexuality); Factor 4: symptomatic shame (embarrassment while eating in front of other people and shame from being a cancer patient); Factor 5: teeth/throat injuries (dental problems and cough); and Factor 6: sensory abnormality (abnormal taste and smell).
At present, chemoradiotherapy is still the primary therapeutic protocol for patients with NPC. The side effects of chemoradiotherapy are present throughout the entire treatment process. Serious complications may interrupt the treatment, prolong the length of hospital stay, and reduce the quality of life. After completion of the therapy, the side effects of chemoradiotherapy continue after the patients return home. The medical staff should evaluate the complications before discharge and provide an individualized education plan for each patient.
The quality of life of the NPC patients was measured using the EORTC QLQ-H&N35, and 25 of the 30 symptoms had an incidence of more than 50%, meaning that the patients suffered from a variety of symptoms. Among these symptoms, the most serious were dental problems (M[P25,P75] = 94.5 [32.0, 94.5]), followed by a feeling of obstructed swallowing (M[P25,P75] = 92.0 [44.5, 92.0]). In previous studies, Sroussi et al. found that the most serious complications of head and neck radiotherapy were oral mucositis, dry mouth, and malnutrition (10). Myelosuppression is one of the most common complications of chemoradiotherapy, which indicates that the immune function of the body is damaged and has decreased immunity (11).
Radiation can destroy the periodontal connective tissue, causing injury to the periodontal mucosa defense system and resulting in gum swelling and pain, oral ulcers, oral microflora, other oral microenvironment disorders, and oral infection (11), especially Candida albicans infection (12, 13). Schuurhuis et al. (14) found that patients who received intensity-modulated radiotherapy and concurrent chemoradiotherapy had an increase in oral Escherichia coli, Staphylococcus, Candida, and other opportunistic pathogens. Radiation has a direct effect on teeth, and the atrophy of gingiva and interdental papilla results in the exposure of tooth roots, food impaction and bacterial retention, a decrease in saliva secretion, a decrease in oral self-cleaning ability, and radiation caries (15). Although the patients had teeth cleanings and periodontal disease prevention before the chemoradiotherapy treatment, they were not examined during the treatment period, and dental problems developed.
After discharge, NPC patients returned to a wider social network and often experienced social anxiety symptoms. Li et al. found that patients with NPC generally had emotional problems and psychological pain, often brought on by their physical challenges (16).
More than 95% of the patients in our study experienced dry mouth, sticky saliva, abnormal taste, difficulty in swallowing solid food, and reduced enjoyment from food. Although these difficulties are less consequential than dental disease, swallowing obstruction, or social disorder, they seriously affected the quality of life at home and should be brought to the attention of medical staff during follow-up.
As described above, the six symptom clusters were (1) painful eating and swallowing, (2) social anxiety, (3) psychological disorders, (4) symptomatic shame, (5) teeth/throat injuries, and (6) sensory abnormalities.
In the present study, the symptom cluster of painful eating and swallowing included sore throat, difficulty in drinking liquid, difficulty in swallowing semiliquid food, difficulty in swallowing solid food, and difficulty in eating. Shen et al. reported that patients in the late stage of radiotherapy treatment suffered from sticky saliva, dysphagia, taste abnormality, dry mouth, and oral/throat pain (17).
These previously reported symptoms were not entirely consistent with the findings of the present study, which might be due to different symptom evaluation scales and statistical methods. Almost all patients with NPC who are undergoing chemoradiotherapy will have radiation stomatitis and laryngopharyngitis (18); as the doses increase, patients are often unable to swallow at will because of the severe pain.
At the same time, radiotherapy may cause fibrosis of the muscles involved with swallowing through extracellular matrix deposits and fibroblast proliferation. Radiotherapy damages up to 30 pairs of muscles and six pairs of cranial nerves (19), leading to a loss of muscular strength, coordination, swallowing function, and eventually dysphagia. Because the salivary glands might be injured by the radiation, the secretion of saliva is reduced, which also impairs the swallowing process. Patients also suffer from dysphagia due to acute oropharyngeal cavity pain, which should be managed in clinical practice to ensure that they eat sufficiently and receive adequate daily nutrition.
The social anxiety symptom cluster included difficulties in speaking with others, speaking on the phone, and socializing with friends and family members. The negative emotions of patients often come from a lack of awareness and understanding of radiation therapy, as well as the heavy economic burden. In addition, the deeper the treatment, the more obvious the toxic and side effects brought by radiotherapy and chemotherapy. Patients who are unable to bear the toxic and side effects are prone to develop anxiety, panic, suspicion, and even give up treatment, ultimately affecting the effectiveness of treatment and rehabilitation.
It is reported that 60.62% of patients with head and neck cancer have depressive symptoms (20). The majority of patients with NPC are young and middle-aged males, who are often the breadwinners for their families and are in the prime of their careers and personal lives. The occurrence of tumors and the side effects of chemoradiotherapy may cause different degrees of physical and mental distress to the patients and make them reluctant to communicate with their loved ones. The patients also fear letting others know about their illness because it may negatively affect their future opportunities.
These negative physical and mental problems will seriously harm the quality of life of the NPC patients and may even cause a recurrence of the cancer. In addition, the incidence of cancer-related fatigue in patients with NPC is as high as 82.5%, which is inversely proportional to the amount of social support the patient does receive. Providing good social support can effectively improve the patients’ anxiety, depression, and quality of life (21). Noh et al. (22) reported that ratios of anxiety, substance abuse, and soma to form/conversion disorders fell after the start of radiotherapy compared to before radiotherapy.
The psychological disorder symptom cluster consisted of worry about changes in appearance, embarrassment at appearing in public, embarrassment during physical contact with friends and family members, a decreased sex drive, and decreased pleasure in sexual activities. Radiotherapy to the head and face causes increased pigmentation, hair loss, nasal hemorrhage, and necrosis of the nasal tissue; these undesirable changes in appearance are a source of negative emotions. Decreased libido is a common complaint in cancer patients. However, another study (23) suggests that there is no significant difference in the sexual function in NPC patients between three months to one year after treatment, suggesting that sexual function might be correlated with adverse emotions such as anxiety and depression during the treatment.
The symptoms in the shame cluster range from common feelings such as embarrassment at eating in front of other people to more profound feelings of shame caused by being a cancer patient, which is manifested as guilt, shame, self-reproach, and fear of being discriminated against (24). At present, the majority of the research on symptomatic shame has focused on patients with lung and breast cancers (25), with less attention given to head and neck carcinomas. Chemoradiotherapy for NPC injures the head and face and can also lead to more serious complications such as deafness and blurred vision. Patients may suffer from dysphagia and radiation oropharyngeal mucositis, which can cause severe pain and slow the speed of eating. Most of the food taken by the patients is liquid or semiliquid, and their eating habits are different from those of healthy individuals. When patients return to their families, they may suffer from different degrees of symptomatic shame.
The teeth/throat injury symptom cluster included dental problems and cough, which might be primarily caused by radiation injury. Radiation damages teeth through the destruction of the enamel surface layer, the formation of craters under the surface layer, the exposure of dentin under the surface layer, the formation of a wide range of porous structures, and the development of radioactive caries (26). Most of the NPC patients were affected by subjective discomforts such as tooth or gingival tenderness and tooth sensitivity. In addition, radiotherapy can cause dry mouth, sore throat, thick throat sputum, frequent coughing, and a decreased self-cleaning ability of the mouth, all of which might aggravate the symptoms of tooth-throat injury.
The sensory abnormality symptom cluster included abnormal taste and smell. In the present study, most of the patients with NPC received one cycle of induction chemotherapy followed by radiotherapy, and the abnormal taste and smell often occurred in the radiotherapy stage. Most patients complained that the changes of taste resulted in a loss of appetite, a decrease in food intake, and changes in eating habits. This led to anxiety and depression and affected their quality of life (27, 28).
Shen et al. (17) extracted four symptom clusters from 133 NPC cases in the late radiotherapy stages of concurrent chemoradiotherapy: emotion-pain, diseased feeling, and digestive tract symptom clusters. Xiao et al. (29) extracted four symptom clusters: general, gastrointestinal, nutritional, and social. The findings of our study are consistent with the symptom clusters found in previous studies, except for the digestive tract symptom cluster. The difference might be caused by different symptom evaluation forms and different evaluation time points.
This study was a single-center study, and the number of study population was relatively small. Thus, the results of this study need to be further confirmed by a larger study population in a multicenter. Besides, this study did not consider the physical performance of the patients before starting the chemoradiation, which might have an influence to the results of this study. In the management of the discharged NPCs, it should be careful about eating, social, psychological, symptomatic, and sensory condition, which is helpful to manage cluster symptoms resulting from chemoradiotherapy side effects in NPC patients. Finally, due to small sample size and incomplete information, this study did not analyze and compare the symptoms after chemoradiation in NPC patients between two criterias, for example, between man and woman, between early stage and advance stage, or between young and old patients. In the future, multi-center studies with large samples and at least 6 months of follow-up data should be carried out.
NPC patients are troubled by many symptom clusters, especially dental disease, social challenges, and a sense of obstruction while swallowing. Patients suffer a diminished quality of life and difficulty in returning to their homes because of a number of disorder symptom clusters: painful eating, social anxieties, psychological disorders, symptomatic shame, teeth/throat injuries, and sensory abnormalities. Nurses should evaluate the patients’ symptoms before discharge and provide targeted health education services. This will help to reduce the patients’ complications and improve the quality of life at home.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethics Committee of The People’s Hospital of Guangxi Zhuang Autonomous Region. The patients/participants provided their written informed consent to participate in this study.
G-FF and XL conceived the idea and conceptualised the study. Y-YH and Q-YJ collected the data. X-YH and J-TZ analysed the data. XL and G-FF drafted the manuscript, then S-HQ reviewed the manuscript. All authors read and approved the final draft. All authors contributed to the article and approved the submitted version.
Guangxi Key Research and Development Plan (Contract No.: Guike AB16450009, Guike AB1850010). Fund project of Guangxi Health Commission (Contract No.: Z20180753, Z20180752, Z2015686, Z2014218). National Natural Science Foundation of China (Contract No.: 81960186, 81460097). Guangxi Natural Science Foundation (Contract No.: 2017GXNSFAA198013). Guangxi Science and Technology Base and Talent Project (GuiKe-AD20297069).
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Shah AB, Zulfiqar H, Nagalli S. Nasopharyngeal carcinoma. In: StatPearls. Treasure Island (FL: StatPearls Publishing (2022).
2. Ji MF, Sheng W, Cheng WM, Ng MH, Wu BH, Yu X, et al. Incidence and mortality of nasopharyngeal carcinoma: interim analysis of a cluster randomized controlled screening trial (PRO-NPC-001) in southern China. Ann Oncol (2019) 30(10):1630–7. doi: 10.1093/annonc/mdz231
3. Liu F, Jin T, Liu L, Xiang Z, Yan R, Yang H. The role of concurrent chemotherapy for stage II nasopharyngeal carcinoma in the intensity-modulated radiotherapy era: a systematic review and meta-analysis. PloS One (2018) 13(3):e0194733. doi: 10.1371/journal.pone.0194733
4. De Felice F, Musio D, Tombolini V. Immune check-point inhibitors and standard chemoradiotherapy in definitive head and neck cancer treatment. J Pers Med (2021) 11(5):393. doi: 10.3390/jpm11050393
5. Sagaonkar PS, Pattanshetty R. Effect of medical qigong therapy on distress, fatigue, and quality of life in head and neck cancer patients undergoing intensity-modulated radiation therapy: a single arm clinical trial. World J Tradit Chin Med (2021) 7:427–35. doi: 10.4103/wjtcm.wjtcm_15_21
6. Loewen I, Jeffery CC, Rieger J, Constantinescu G. Prehabilitation in head and neck cancer patients: a literature review. J Otolaryngol Head Neck Surg (2021) 50(1):2. doi: 10.1186/s40463-020-00486-7
7. Xiao W, Chan CWH, Xiao J, Wong CL, Chow KM. Development of a nurse-led educational intervention program in managing the nutrition impact symptom cluster in patients with nasopharyngeal carcinoma following the medical research council framework. Asia Pac J Oncol Nurs (2021) 8(6):653–61. doi: 10.4103/apjon.apjon-2141
8. Liao T, Yang L, Qiu L, Guo M, Ji Lu, Huang X, et al. The need of nursing care and influencing factors in patients with nasopharyngeal carcinoma. Chin Nurs Manage (2019) 19(7):985–91. doi: 10.3969/j.issn.1672-1756.2019.07.007
9. Zhang X, Zheng Q, Hao Y, Zhang C. Assessment of EORTC QLQ C30/H&N35 in nasopharyngeal carcinoma patients quality of life. New Med (2013) 44(7):467–71. doi: 10.3969/g.issn.0253-9802.2013.07.008
10. Sroussi HY, Epstein JB, Bensadoun RJ, Saunders DP, Lalla RV, Migliorati CA, et al. Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med (2017) 6(12):2918–31. doi: 10.1002/cam4.1221
11. Yan F, Li Q, Han Y, Peng J. Effect of PRECEDE on oral infections in patients with head and neck radiotherapy. Chin J Nosocomiol (2018) 28(2):243–6. doi: 10.11816/cn.ni.2018-171283
12. Zhu XX, Yang XJ, Chao YL, Zheng HM, Sheng HF, Liu HY, et al. The potential effect of oral microbiota in the prediction of mucositis during radiotherapy for nasopharyngeal carcinoma. EBioMedicine (2017) 18:23–31. doi: 10.1016/j.ebiom.2017.02.002
13. Liu YP, Lv X, Zou X, Hua YJ, You R, Yang Q, et al. Minimally invasive surgery alone compared with intensity-modulated radiotherapy for primary stage I nasopharyngeal carcinoma. Cancer Commun (Lond) (2019) 39(1):75. doi: 10.1186/s40880-019-0415-3
14. Schuurhuis JM, Stokman MA, Witjes MJH, Reintsema H, Langendijk JA, Vissink A, et al. Patients with advanced periodontal disease before intensity-modulated radiation therapy are prone to develop bone healing problems: a 2-year prospective follow-up study. Support Care Cancer (2018) 26(4):1133–42. doi: 10.1007/s00520-017-3934-y
15. Budure AN, Winquist E, Palma D, Correa RJM. Successful treatment of nasopharyngeal cancer using radiotherapy with concurrent cetuximab in a patient with charcot-Marie-Tooth disease. BMJ Case Rep (2019) 12(7):e228956. doi: 10.1136/bcr-2018-228956
16. Li Z. Analysis of psychological distress status and influencing factors in patients with nasopharyngeal carcinoma treated with radiotherapy. J Prev Med Chin PLA (2019) 37(7):156–7. doi: 10.13704/j.cnki.jyyx.2019.07.074
17. Shen Y, Qiang W, Li Z, Liu G, Shen A. Analysis of symptoms and influencing factors in patients with nasopharyngeal carcinoma undergoing concurrent chemoradiotherapy. J Nurs Educ (2019) 32(14):1279–84. doi: 10.16821/j.cnki.hsjx.2017.14.008
18. Ingrosso G, Saldi S, Marani S, Wong AYW, Bertelli M, Aristei C, et al. Breakdown of symbiosis in radiation-induced oral mucositis. J Fungi (Basel) (2021) 7(4):290. doi: 10.3390/jof7040290
19. Guillen-Sola A, Soler NB, Marco E, Pera-Cegarra O, Foro P. Effects of prophylactic swallowing exercises on dysphagia and quality of life in patients with head and neck cancer receiving (chemo) radiotherapy: the redyor study, a protocol for a randomized clinical trial. Trials (2019) 20(1):503. doi: 10.1186/s13063-019-3587-x
20. Yan X, Chen X, Li M, Zhang P. Prevalence and risk factors of anxiety and depression in Chinese patients with lung cancer:a cross-sectional study. Cancer Manag Res (2019) 11:4347–56. doi: 10.2147/CMAR.S202119
21. Peng Y, Tang H, Zhang S, Wei Y, Zhang Y, Chen C. Correlation study of cancer induced fatigue, social support and quality of life in nasopharyngeal cancer radiotherapy patients. Nurs Res (2019) 33(14):2514–7. doi: 10.12102/j.issn.1009-6493.2019.14.036
22. Noh OK, Heo J. Mental disorders in nasopharyngeal carcinoma patients receiving radiation therapy: a nationwide population-based study. In Vivo (2021) 35(5):2901–8. doi: 10.21873/invivo.12580
23. Gan Y, Lin Z, Chen S, Shi Y, Peng X, Zhan Y, et al. Effect of cognitive intervention on sexual function after treatment of nasopharyngeal carcinoma. Chin Cancer (2008) 7(17):609–11. doi: 10.3969/j.issn.1004-0242.2008.07.019
24. Rose S, Boyes A, Kelly B, Cox M, Palazzi K, Paul C. Help-seeking behaviour in newly diagnosed lung cancer patients: assessing the role of perceived stigma. Psychooncology (2018) 27(9):2141–7. doi: 10.1002/pon.4779
25. Gao L, Cao X, Zhang Y, Liu T, Zhang A. Bibliometric analysis about stigma of cancer research based on web of science database. Chin Ment Health J (2018) 06:484–9. doi: 10.3969/j.issn.1000-6729.2018.06.007
26. Wu LL, Gao QP, Fu QY, Geng K. Analysis of the risk factors of radiation-induced caries in patients with head and neck cancer. Hua Xi Kou Qiang Yi Xue Za Zhi (2019) 37(1):87–91. doi: 10.7518/hxkq.2019.01.017
27. Postma EM, Kok DE, de Graaf C, Kampman E, Boesveldt S. Chemosensory perception and food preferences in colorectal cancer patients undergoing adjuvant chemotherapy. Clin Nutr ESPEN (2020) 40:242–51. doi: 10.1016/j.clnesp.2020.09.012
28. Kaizu M, Komatsu H, Yamauchi H, Yamauchi T, Sumitani M, Doorenbos AZ. Characteristics of taste alterations in people receiving taxane-based chemotherapy and their association with appetite, weight, and quality of life. Support Care Cancer (2021) 29(9):5103–14. doi: 10.1007/s00520-021-06066-3
Keywords: nasopharyngeal carcinoma, chemoradiotherapy, symptom clusters, nursing, otorhinolaryngology
Citation: Li X, Fu G-F, Huang Y-Y, Jiang Q-Y, Huang X-Y, Zhang J-T and Qu S-H (2023) Symptom clusters after chemoradiotherapy in discharged nasopharyngeal carcinoma patients. Front. Oncol. 13:920889. doi: 10.3389/fonc.2023.920889
Received: 20 May 2022; Accepted: 16 May 2023;
Published: 14 June 2023.
Edited by:
Moran Amit, University of Texas MD Anderson Cancer Center, United StatesReviewed by:
Hamsu Kadriyan, University of Mataram, IndonesiaCopyright © 2023 Li, Fu, Huang, Jiang, Huang, Zhang and Qu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shen-Hong Qu, cXVfc2hob25nODc1QDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.