
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 17 November 2023
Sec. Surgical Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1288044
This article is part of the Research Topic Advances in Bronchoscopic Techniques for the Diagnosis of Lung Cancer View all 7 articles
 Zilin Wang1,2
Zilin Wang1,2 Gang Hou1*
Gang Hou1*Endobronchial leiomyomas are uncommon benign tracheobronchial tumors. Bronchoscopic intervention is a safe and effective strategy for patients with contraindications for surgery or refusal to undergo surgery. Endoscopic submucosal dissection (ESD) is widely used to treat early gastrointestinal tumors. The novel hybrid knife is useful during ESD owing to functions of submucosal injections, lesion dissection and hemostasis, and makes ESD more convenient. Here, we report a case of a benign leiomyoma at the orifice of RB7 in an adolescent boy. The diagnosis was confirmed based on bronchoscopic and pathological findings. The patient was successfully treated with combined electrocautery snare and cryoresection, ESD using a hybrid knife and the wound was managed with argon plasma coagulation. The postoperative course was satisfactory, with a good general condition and no severe respiratory symptoms. This is, to our knowledge, the first reported case of ESD using a hybrid knife to treat an endobronchial leiomyoma in an adolescent patient.
Endobronchial leiomyomas are rare benign tumors derived from the smooth muscle layer of the bronchi, bronchioles, or blood vessels (1) that account for 3% of all benign endobronchial tumors (2). Considering their rarity, systematic studies on the sex and age distribution, tumor location within the airway, growth patterns, and pathological classifications are lacking. Surgical resection, including sleeve lobectomy, segmentectomy, and pneumonectomy (3), is recommended for endobronchial leiomyomas. Although it often results in favorable long-term outcomes without recurrence, perioperative complications can arise (4). With the development of bronchoscopic techniques, endobronchial interventions have become increasingly viable (5–7). These methods are favored owing to their minimally invasive nature and ease of operation, particularly for benign tumors. Nonetheless, incomplete resection and recurrence after endoscopic approaches, particularly for tumors with a wide base, can occur (4, 8). This underscores the requirement of an endoscopic technique that can completely excise tumors.
Endoscopic submucosal dissection (ESD) is performed for submucosal tumors within the gastrointestinal tract, often achieving curative results (9–13). The hybrid knife, with multifunctional capabilities, such as circumferential dissection, submucosal injections, dissection, and hemostasis (14, 15), has expedited ESD procedures (14). It can also be used to treat recurrent benign tracheal tumors (16). It may represent a novel approach for completely removing benign endobronchial tumors, thereby decreasing recurrence.
Here, we report a case of endobronchial leiomyoma in an adolescent patient treated with ESD using a water-jet hybrid knife.
A 16-year-old boy presented to our hospital with a 2-month history of right chest pain and no other respiratory symptoms. Computed tomography conducted at another hospital revealed a high-density nodule-like shadow measuring appropriately 0.6 cm in the bronchial lumen of the right lower lobe. Morphological and immunohistochemical analyses of the biopsied tissue confirmed endobronchial leiomyoma. Although surgical intervention remains the recommended treatment, considering the patient’s age, both the patient and his parents refused a surgical resection. ESD was performed using a water-jet hybrid knife to thoroughly expose the tumor base for comprehensive resection. Under general anesthesia, the bronchoscopy (BF-1T290; Olympus, Tokyo, Japan) conducted using a rigid bronchoscope revealed an irregular, protuberant mass at the orifice of RB7, which obstructed the lumen (Figure 1A). Switching to the narrow-spectrum mode highlighted a few blood vessels on the lesion surface. A significant portion of the tumor was excised and collected using an electrocautery snare and cryoprobe. Subsequently, a hybrid knife (HybridKnife® ERBE JET2 Elektromedizin, Tübingen, Germany) was employed to dissect the tumor stump, as described previously (Figure 1B) (16). A water jet was used to administer a 2% lidocaine solution into the submucosal layer of the tumor base under a 30-bar pressure. The hybrid knife then entered the submucosal space via the injection site, making a circumferential incision (VIO mode ENDOCUT Q, effect 3-width 1-interval of incision 4, Coagulation effect 2 and 30 W). After the tumor base resection, argon plasma coagulation (APC) was applied to treat the wound surface (Figure 1C). Postoperatively, the patient’s general condition was stable, with no signs of chest tightness, chest pain, or hemoptysis. Physical examination revealed no abnormalities. The 3-month and 5-month follow-up showed no signs of recurrence (Figure 1D). Long-term surveillance is necessary for further assessment of recurrence.
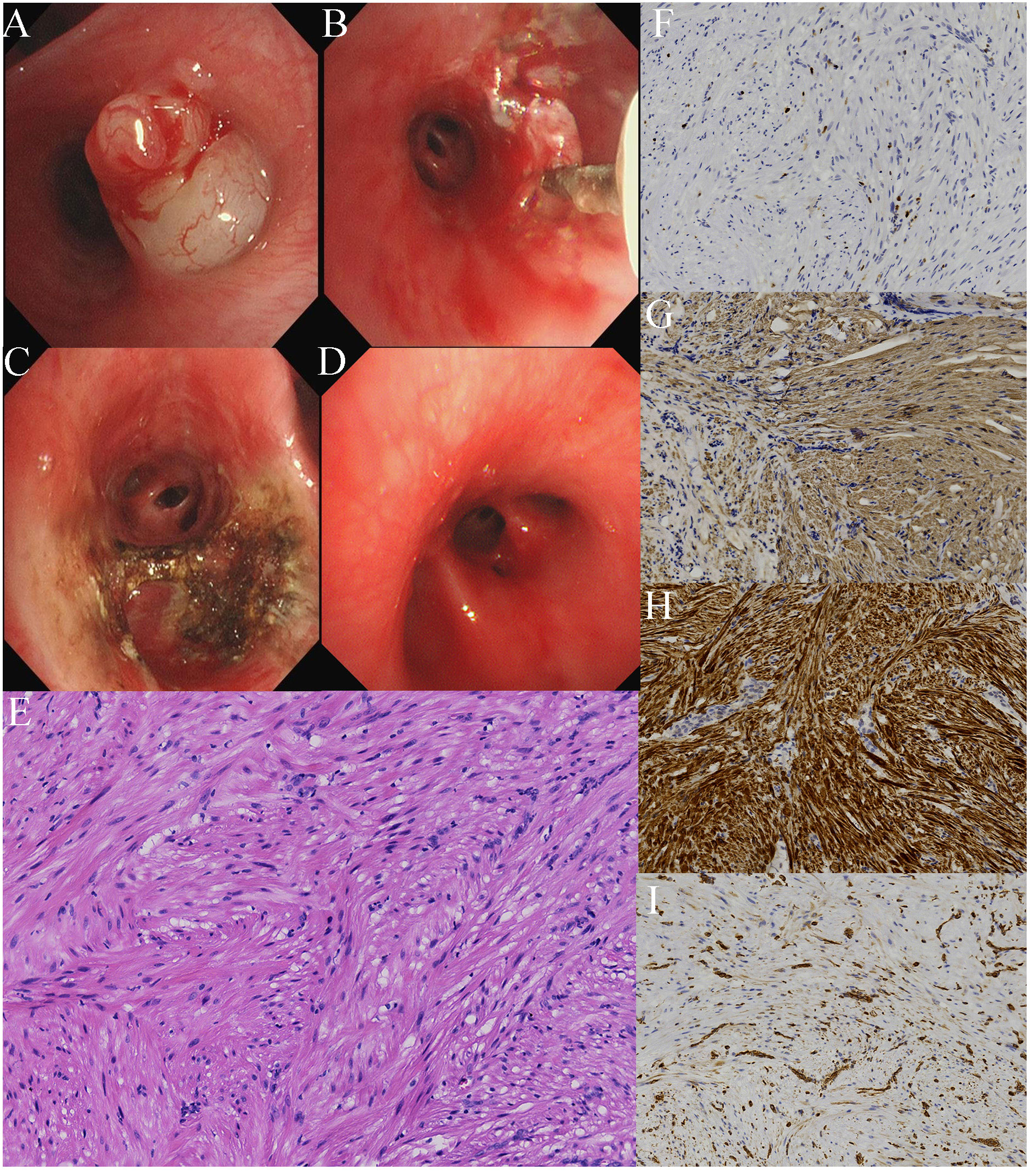
Figure 1 Bronchoscopic examination shows (A) an irregular, protuberant mass at the orifice of RB7 on bronchoscopy, (B) a hybrid knife used to remove the tumor stump, (C) the appearance of the orifice of RB7, after a combined treatment of electrocautery snare, cryoresection, ESD using a hybrid knife, and APC for wound management, and (D) the appearance of the orifice of RB7 3-month post-treatment. (E) Hematoxylin and eosin staining shows the mass composed of spindle cells. Immunohistochemical staining reveals a (F) Ki-67 index of 3%+; the mass is positive for (G) alpha-smooth muscle actin, (H) desmin, and (I) vimentin.
Hematoxylin and eosin staining indicated that the mass was composed of spindle cells (Figure 1E). Immunohistochemical staining revealed a relatively low Ki-67 proliferation index of 3%+ (Figure 1F), positive for alpha-smooth muscle actin, desmin, and vimentin (Figures 1G–I) and negative for HMB45 and S-100. These pathological results confirmed the diagnosis of an endobronchial leiomyoma.
Benign airway tumors are uncommon, accounting for only 2% of all pulmonary tumors. Endobronchial leiomyomas are extremely rare, accounting for approximately 0.66% of all benign pulmonary tumors (17). These tumors originate from the mesenchymal layer and are composed of bronchial and vascular smooth muscle cells (2). Advanced endoscopic technologies have enabled bronchoscopic interventions as potential alternatives to the endoscopic removal of leiomyomas within the airway. This can be achieved through various methods, such as electrocautery, laser, APC, and cryotherapy (5). Pedunculated benign tumors are often effectively treated using these resection methods, although wide-based tumor recurrence has been reported in a single-institution review (18). Episodes of recurrence have also been reported in tracheobronchial leiomyomas after tumor removal, whether with laser ablation or APC (8, 16, 19). Limited cases and comparative studies may not conclusively prove this, but these instances highlight potential limitations in the width and depth of the current endoscopic approaches (20).
ESD is used to resect superficial gastrointestinal lesions (21). The hybrid knife is a novel tool that integrates a high-pressure water jet with an electrocautery knife. This combination renders ESD more convenient because the same device can be used for submucosal injections, lesion dissection, and hemostasis (14). ESD can effectively expose the tumor base for a more comprehensive resection. Additionally, the submucosal water cushion formed by the hybrid knife acts as a protective barrier for the surrounding tissue and reduces the perforation risk. Previous use of the hybrid knife has shown promising outcomes after the resection of recurrent lesions of benign tracheal tumors in two patients (16, 22). This procedure involves the creation of a submucosal tunnel using a water jet, followed by circumferential dissection of the lesion. The water jet pressure differed between the present case (30-bar pressure) and Gu et al.’s case (40-bar pressure). The choice of a lower pressure in the present case was necessary because of the location of the leiomyoma in the segmental bronchus, which possesses a thinner wall amplifying the perforation risk.
ESD with the hybrid knife is a viable treatment option for endobronchial leiomyoma in adolescents, with no recurrence observed at the 5-month follow-up. However, some limitations should be acknowledged. The evidence was primarily derived from a single case with a 5-month follow-up period. Comprehensive long-term follow-up studies are essential to determine the safety and efficacy of ESD using a hybrid knife in the management of endobronchial leiomyomas. Furthermore, the cost of the hybrid knife and the requirement of specialized equipment may render it inaccessible to some medical facilities.
In summary, ESD using a hybrid knife is a novel and effective method for treating endobronchial leiomyomas without complications. This approach may emerge as a potential treatment method for benign tracheobronchial tumors. However, considering the relatively short follow-up period and its nascent adoption, a comprehensive evaluation of the safety and efficacy of ESD with a hybrid knife to manage endobronchial leiomyomas requires further clinical research and case studies for validation.
The data presented in this study are available on request from the corresponding author.
Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
GH: Conceptualization, Resources, Supervision, Validation, Writing – review & editing. ZW: Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by National High Level Hospital Clinical Research Funding (2022-NHLHCRF-LX-01), the Elite Medical Professionals Project of China-Japan Friendship Hospital (No. ZRJY2021- BJ08), and the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (No. 2020-PT320-001).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Yellin A, Rosenman Y, Lieberman Y. Review of smooth muscle tumours of the lower respiratory tract. Br J Dis Chest (1984) 78(4):337–51. doi: 10.1016/0007-0971(84)90166-9
2. Insler JE, Seder CW, Furlan K, Mir F, Reddy VB, Gattuso P. Benign endobronchial tumors: A clinicopathologic review. Front Surg (2021) 8:644656. doi: 10.3389/fsurg.2021.644656
3. Kajiwara N, Kakihana M, Usuda J, Ohira T, Kawate N, Ikeda N. Interventional management for benign airway tumors in relation to location, size, character and morphology. J Thorac Dis (2011) 3(4):221–30. doi: 10.3978/j.issn.2072-1439.2011.04.06
4. Dmello D, Javed A, Espiritu J, Matuschak GM. Endobronchial leiomyoma: case report and literature review. J Bronchology Interv Pulmonol (2009) 16(1):49–51. doi: 10.1097/LBR.0b013e318193bc71
5. Bilaçeroğlu S. Endobronchial ablative therapies. Clin Chest Med (2018) 39(1):139–48. doi: 10.1016/j.ccm.2017.11.008
6. Hou G. Bronchoscopic lung volume reduction in chronic obstructive pulmonary disease: History and progress. J Trans Internal Med (2015) 3(4):147–50. doi: 10.1515/jtim-2015-0023
7. Itoi S, Ohara G, Kagohashi K, Kawaguchi M, Kurishima K, Satoh H. Tracheobronchial mucoid pseudotumor. Open Med (2012) 7(3):385–7. doi: 10.2478/s11536-011-0149-3
8. Kwon YS, Kim H, Koh WJ, Suh GY, Chung MP, Kwon OJ, et al. Clinical characteristics and efficacy of bronchoscopic intervention for tracheobronchial leiomyoma. Respirology (2008) 13(6):908–12. doi: 10.1111/j.1440-1843.2008.01366.x
9. Zhou JQ, Tang XW, Ren YT, Wei ZJ, Huang SL, Gao QP, et al. Endoscopic submucosal tunnel dissection of upper gastrointestinal submucosal tumors: A comparative study of hook knife vs hybrid knife. World J Gastroenterol (2017) 23(10):1843–50. doi: 10.3748/wjg.v23.i10.1843
10. Zhao Z, Jiao Y, Yang S, Zhou A, Zhao G, Guo S, et al. Endoscopic diagnosis and treatment of superficial non-ampullary duodenal epithelial tumors: A review. J Trans Internal Med (2023) 11(3):206–15. doi: 10.2478/jtim-2023-0102
11. Dong X, Zhao J, Sun Z. Endoscopic resection of gastric glomus tumor: a case report and literature review. Oncologie (2023) 25(5):565–9. doi: 10.1515/oncologie-2022-1013
12. Zhang Y, Zhang B, Wang Y, Zhang J, Wu Y, Xiao T, et al. Advances in the prevention and treatment of esophageal stricture after endoscopic submucosal dissection of early esophageal cancer. J Trans Internal Med (2020) 8(3):135–45. doi: 10.2478/jtim-2020-0022
13. Hu J, Ge N, Wang S, Liu X, Guo J, Wang G, et al. The role of endoscopic ultrasound and endoscopic resection for gastric glomus: A case series and literature review. J Trans Internal Med (2019) 7(4):149–54. doi: 10.2478/jtim-2019-0030
14. De-la-Peña J, Calderón Á, Esteban JM, López-Rosés L, Martínez-Ares D, Nogales Ó, et al. Experimental study of hybrid-knife endoscopic submucosal dissection (ESD) versus standard ESD in a Western country. Rev Esp Enferm Dig
15. Neuhaus H, Wirths K, Schenk M, Enderle MD, Schumacher B. Randomized controlled study of EMR versus endoscopic submucosal dissection with a water-jet hybrid-knife of esophageal lesions in a porcine model. Gastrointest Endosc (2009) 70(1):112–20. doi: 10.1016/j.gie.2008.10.042
16. Ma JW, Miao Y, Lin XY, Wang QY, Wang W, Kang J, et al. Endoscopic submucosal dissection of tracheal deep benign fibrous histiocytoma using hybrid knife. Onco Targets Ther (2019) 12:5609–13. doi: 10.2147/OTT.S213747
17. Stevic R, Milenkovic B. Tracheobronchial tumors. J Thorac Dis (2016) 8(11):3401–13. doi: 10.21037/jtd.2016.11.24
18. Park JS, Lee M, Kim HK, Choi YS, Kim K, Kim J, et al. Primary leiomyoma of the trachea, bronchus, and pulmonary parenchyma–a single-institutional experience. Eur J Cardiothorac Surg (2012) 41(1):41–5. doi: 10.1016/j.ejcts.2011.03.051
19. Miller SM, Bellinger CR, Chatterjee A. Argon plasma coagulation and electrosurgery for benign endobronchial tumors. J Bronchology Interv Pulmonol (2013) 20(1):38–40. doi: 10.1097/LBR.0b013e318282d3ca
20. Bawaadam H, Ivanick N, AlShelli I, Krishna G. Endobronchial Leiomyoma: A case report with cryoprobe extraction and review of literature. Respir Med Case Rep (2021) 33:101467. doi: 10.1016/j.rmcr.2021.101467
21. Yamamoto H, Yube T, Isoda N, Sato Y, Sekine Y, Higashizawa T, et al. A novel method of endoscopic mucosal resection using sodium hyaluronate. Gastrointestinal Endoscopy (1999) 50(2):251–6. doi: 10.1016/S0016-5107(99)70234-8
Keywords: endobronchial leiomyomas, hybrid knife, endoscopic submucosal dissection, case report, adolescent
Citation: Wang Z and Hou G (2023) Endoscopic submucosal dissection of endobronchial leiomyoma with a hybrid knife in an adolescent patient: a case report. Front. Oncol. 13:1288044. doi: 10.3389/fonc.2023.1288044
Received: 25 September 2023; Accepted: 23 October 2023;
Published: 17 November 2023.
Edited by:
Martina Ferioli, IRCCS Azienda Ospedaliero-Universitaria di Bologna, ItalyReviewed by:
Panaiotis Finamore, Campus Bio-Medico University Hospital, ItalyCopyright © 2023 Wang and Hou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gang Hou, aG91Z2FuZ2NtdUAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.