
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol. , 09 January 2024
Sec. Cancer Epidemiology and Prevention
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1248921
This article is part of the Research Topic Improving Clinical Practice in Cancer Patients: Pain and Symptom Management View all 4 articles
Background: Breakthrough cancer pain (BTCP) is a transient exacerbation of pain that affects the length of hospitalization and quality of life of patients. The objective of this study was to determine the prevalence and factors associated with BTCP among cancer patients at oncology units in Northern Ethiopia in 2022.
Methods: A multi-center cross-sectional study was conducted from April to June 2022. After obtaining ethical approval, data were collected prospectively from 424 adult cancer patients admitted to oncology units. Breakthrough cancer pain was assessed by the numeric rating scale. Descriptive and binary logistic regression analyses were performed to determine the factors associated with BTCP. The strength of association was described in adjusted odds ratio (AOR) with 95% confidence intervals and variables with a P-value < 0.05 were considered to have a statistically significant association with BTCP.
Result: The prevalence of BTCP among cancer patients was 41.5%. The factors that were found to be associated with BTCP were colorectal cancer (AOR: 7.7, 95% CI: 1.8, 32.3), lung cancer (AOR: 6.9, 95% CI: 1.9, 26.0), metastasis (AOR: 9.3, 95% CI: 3.0, 29.1), mild background pain (AOR: 7.5, 95% CI: 2.5, 22.6), moderate background pain (AOR: 7.0, 95% CI: 2.2, 23.1), severe background pain (AOR: 7.1, 95% CI: 2.2, 22.8), no analgesics taken for background pain (AOR: 5.1, 95% CI: 2.8, 9.3) and uncontrolled background pain (AOR: 3.3, 95% CI: 1.8, 6.1).
Conclusion: The prevalence of BTCP was high. Colorectal cancer, lung cancer, the presence of metastasis, the presence of background pain, not taking analgesics for background pain, and uncontrolled background pain were significantly associated with BTCP.
Cancer is a multi-symptomatic disease associated with physical, social, and emotional sequelae, and it is one of the leading causes of death worldwide (1). Overall, nearly 10 million deaths were reported in 2020. Data from the World Health Organization’s Global Cancer Observatory (GLOBOCAN) showed that breast (2.26 million), lung (2.21 million), and colorectal (1.93 million) cancers were the most frequent new cases in 2020 (2). In sub-Saharan Africa in 2020, breast and cervical cancer were the most common, and prostate cancer was the leading incidence of cancer in men (3).
Cancer pain is one of the most complex symptoms due to its cognitive, behavioral, sensory, and emotional components. It is the most frightening symptom with a prevalence of 50% to 70%. The highest prevalence of pain is commonly observed among pancreatic and head/neck cancer (4–7).
Breakthrough cancer pain (BTCP) is defined as a transient exacerbation of pain that occurs either spontaneously or in relation to a specific, predictable, or unpredictable trigger, despite having relatively stable and adequately controlled background pain (8). It is a common clinical condition in cancer patients characterized by rapid onset, short duration, and severe intensity. It has a significant impact on a patient’s quality of life (9–11). Breakthrough cancer pain is categorized as spontaneous pain and incidental pain. Spontaneous pain is unpredictable and its precipitants are not clearly identifiable, whereas incidental pain is somewhat predictable (12–14). The consequences of poor breakthrough cancer pain management include poor functional ability, poor sleep patterns, increased anxiety and depression, poor compliance with cancer treatments, increased costs of care, and patient dissatisfaction (9, 15–17). A variety of factors such as sociodemographic factors, the type and site of cancer, stage, metastasis, physical activity, background pain, and pain medications have been found associated with BTCP (4, 18–29).
Breakthrough cancer pain is commonly overlooked by healthcare providers. Despite its deleterious consequences, the management of BTCP is still sub-optimal (5). Limited research-based evidence is available regarding BTCP in low- and middle-income countries, particularly in sub-Saharan Africa. The general objective of this study was to assess the prevalence and factors associated with BTCP at oncologic units in Northern Ethiopia.
A multi-center cross-sectional study was conducted from 1 April to 28 June 2022. Three oncology units are based in Northern Ethiopia, including the University of Gondar Comprehensive Specialized Hospital (UoGCSH), Felege Hiwot Comprehensive Specialized Hospital (FHCSH), and Dessie Comprehensive Specialized Hospital (DCSH).
All adult (18+) cancer patients admitted to oncology units in the aforementioned hospitals in the Amhara National Regional State during the study period were included. Patients who were unable to communicate and volunteer to participate in the study were excluded.
The dependent variable was breakthrough cancer pain and the independent variables were socio-demographic characteristics (age, sex), cancer characteristics (type, site, stage, and metastases), treatment-related factors, and background pain intensity.
Breakthrough pain: a transitory increase in pain to a score greater than NRS ≥ 7/10, which occurred alongside or further to a background pain (30).
Background pain: a mild to moderate intensity of the pain with a value of 1 to 6 on NRS (31).
Controlled background pain: background pain that is managed with scheduled opioids and non-opioid analgesics and has an NRS of < 3/10 (32).
Numerical Rating Scale: A pain assessment tool in which a number is assigned from 0 – 10 to represent the severity of the pain; 0 = no pain; 1 – 3 = mild pain 4 – 6 = moderate pain 7 – 10 = severe pain (33).
Somatic pain: Pain arising from the skin, subcutaneous tissue, and musculoskeletal system characterized by being intense, constant, and localized to a particular area (34).
Visceral pain: Pain originating from internal organs characterized by a diffuse, dull, and poorly localized type of pain (35).
Neuropathic pain: Pain resulting from damage to the nervous system characterized by burning, electrical shocks, shooting, and needle-type pain (36, 37).
The sample size was determined by using a single population proportion formula with the assumptions of 50% prevalence rate and 5% margin of error at 95% confidence level. The final sample size was 424 with the addition of 10% non-response rates. All consecutive cancer patients who were admitted to those oncology units were included in this study center until the calculated sample size was attained. There were 2,736 cancer patients receiving cancer treatment follow-up in the three oncology units (864 at UoGCSH, 720 at FHCSH, and 1,152 at DCSH). The sample taken from each unit was calculated by using a proportion formula (134 UoGCSH, 112 FHCSH, and 178 from DCSH) (Figure 1).
Ethical approval was obtained from the Ethical Review Committee of the School of Medicine, University of Gondar (Reference number: SOM/1404/2022), and permission to conduct data collection was obtained from each hospital. Written informed consent was obtained from each study participant after a detailed explanation of the study. All methods were performed in accordance with the relevant research guidelines and regulations.
The data were collected by three trained nurses by interviewing the participants and chart review, using a structured questionnaire. The questionnaire was adapted from the Alberta Breakthrough Pain Assessment. It was found valid and reliable to assess BTCP (Cronbach’s alpha = 0.83) (19, 32, 38, 39). To ensure the quality of the data, a pretest was conducted on 22 patients (5% of the sample). The accuracy, completeness, and consistency of the collected data were checked; and data collectors were closely supervised by the investigators.
The collected data were cleaned, coded, entered, and analyzed by SPSS version 26 (IBM Corporate). The normality of the data were tested using the Shapiro-Wilk normality test. Variables with variance inflation factors of less than 10 were considered to have no collinearity. The fitness of the model was checked using the Hosmer-Lemeshow goodness-of-fittest. Descriptive, Chi-square, and binary logistic regression analyses were employed to determine the factors associated with BTCP. Variables with a P value < 0.2 on bivariate logistic regression were entered into multivariate logistic regression analysis. In the multivariable logistic regression analysis, variables with a p-value of < 0.05 were considered to have a statistically significant association with BTCP. The strength of association was described in adjusted odds ratio (AOR) at a 95% confidence interval (CI).
A total of 424 patients were incorporated into this study (100% response rate), with 265 (62.5%) female patients. The median age was 50.0 years (interquartile range = 39 – 62 years). Background pain was present among 380 (89.6%) patients, out of whom 121 (28.5%) were experiencing severe pain. Of the total, 259 (61.1%) patients took analgesics for background cancer pain (Table 1).
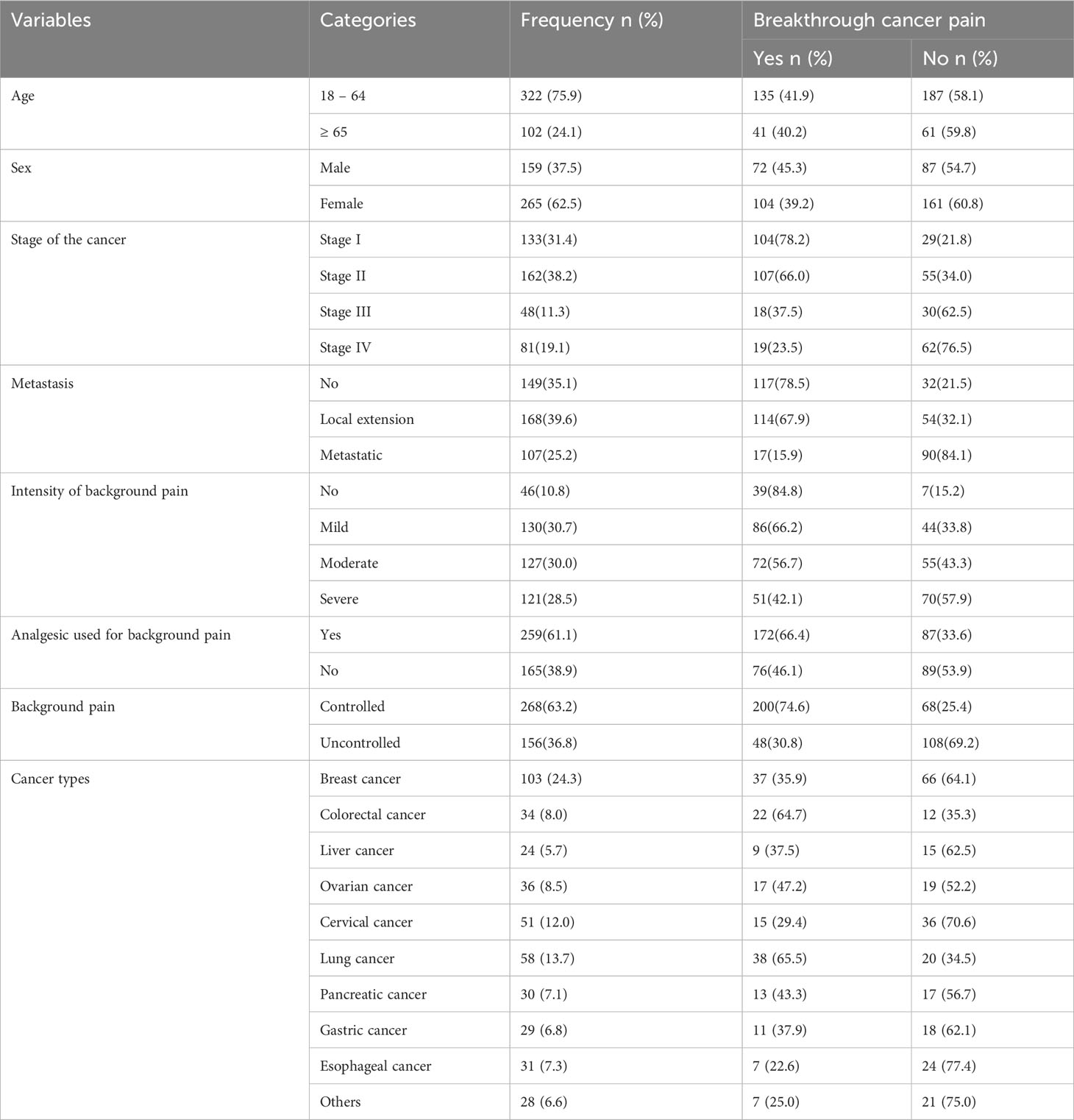
Table 1 Socio-demographic and clinical characteristics, and cross-tabulations with breakthrough cancer pain, N = 424.
We found that 176 patients had BTCP (41.5%, 95% CI = 36.8 – 46.2). The prevalence of BTCP among female patients was 59.1%, whereas it was 40.9% among male patients. Among those 176 patients who had BTCP, 136 (77.3%) used medication to relieve BTCP, while the remaining 40 (22.7%) subjects did not use any medication to relieve their pain. The 56 (41.2%) patients were taking Morphine to relieve BTCP, while the remaining 42 (30.9%) and 38 (27.9%) took NSAID and NSAID with other combinations respectively (Table 2). The prevalence of BTCP was relatively high in the oncology unit at FHCSH (Table 3).
In the bivariate logistic regression analysis, cancer types, stage of cancer, metastasis, the intensity of background pain, the analgesic used for background pain, and uncontrolled background pain were found to be significantly associated with BTCP (P < 0.02) and fitted for the final analysis model. The multivariate logistic regression analysis showed that cancer types (colorectal and lung cancer), metastasis, intensity of background pain, the analgesic drugs used for background pain, and uncontrolled background pain were statistically associated with BTCP (P < 0.05) (Table 4).
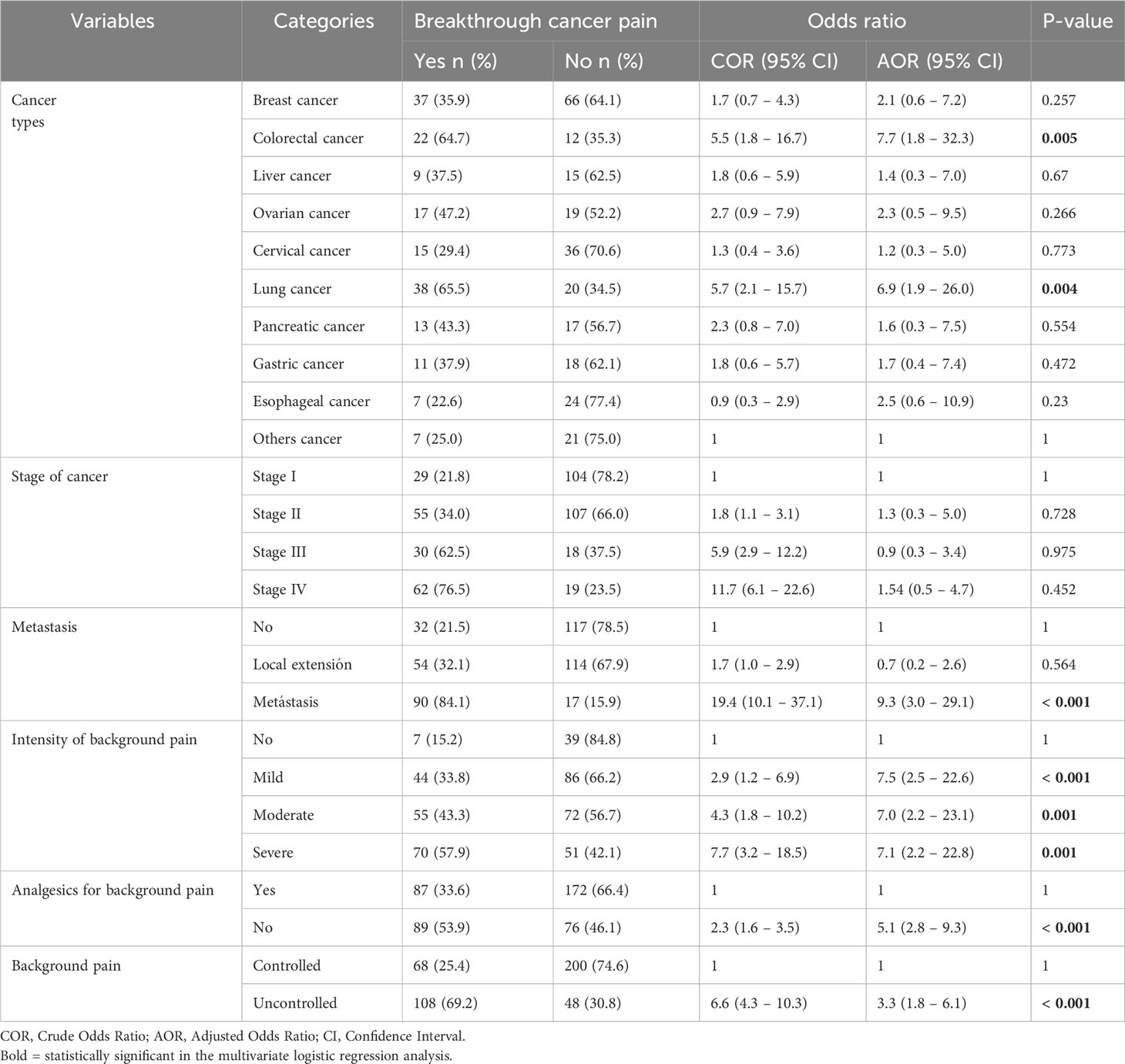
Table 4 Bivariable and multivariable logistic regression analysis: factors associated with breakthrough cancer pain, N = 424.
Patients with colorectal and lung cancer had seven times higher odds of having BTCP [AOR = 7.7, 95% CI = 1.8 – 32.3, P = 0.005] and [AOR = 6.9, 95% CI = 1.9 – 26.0, P = 0.004] respectively. The presence of metastasis increased the odds of having BTCP by nine times [AOR = 9.3, 95% CI = 3.0 – 29.1, P < 0.001]. Patients who were not taking analgesics for background pain were found to have BTCP in fivefold more cases [AOR = 5.1, 95% CI = 2.8 – 9.3, P < 0.001]. Having background pain of any intensity increased the odds of having BTCP by over seven times [P ≤ 0.001]. Similarly, having uncontrolled pain was found to predispose patients to BTCP by triple fold [AOR = 3.3, 95% CI = 1.8 – 6.1, P < 0.004] (Table 4).
Breakthrough pain is frequent in cancer patients and is often characterized by a rapid onset, short duration, and severe intensity (5, 40). In this study, the prevalence of breakthrough cancer pain was 41.5% and it was consistent with previous studies that reported 39.3% (41), 41% (42), and 40.3% (43). However, it was considerably higher compared to other studies that reported 21% (44) and 29% (45). This discrepancy could be explained by the differences in the study settings. Access to quality cancer pain treatment and palliative care can be restricted in low-income countries (46). Furthermore, conflict affected areas are expected to suffer from disrupted cancer care due to damaged infrastructures, shattered supply chains, financial burdens, and evacuation of the health workforce. Similar to Northern Ethiopia, this finding is evidenced by recent studies in Ukraine and the Middle East (47, 48). In contrast, the prevalence of BTCP in the current study was relatively lower than that of other studies at 64.8% (49), 69.8% (22), 73%, and 79% (50).
Among cancer types, colorectal and lung cancer were found to be significantly associated with BTCP. This finding was supported by previous studies and justified by worsening pain and discomfort during coughing, laughing, deep breathing, straining, and defecation (28, 51, 52).
Patients who had metastasis were highly likely to have BTCP and previous studies have supported this finding (10, 49). This condition might be explained by metastatic cancer affecting multiple organs and systems. The size and rate of growth are two important factors that determine pain due to metastatic cancer. Patients could be affected by BTCP and its negative consequences, such as reduced daily activity, worsened quality of life, and dissatisfaction. Patients with metastasis are more likely to receive chemotherapy and radiation therapy, which can result in pain flare-ups (23).
Background pain of any intensity (mild, moderate, or severe) was associated with BTCP. It increased the likelihood of having BTCP by seven times. The association between background pain and BTCP has been reported in multiple previous studies (23, 27, 53, 54). Cancer patients frequently experience pain, which has a favorable correlation with breakthrough pain. Untreated background pain causes a release of an excitatory neurotransmitter such as glutamate, which facilitates the development of BTCP (55).
If patients did not take analgesics to treat background pain, they were highly likely to develop BTCP. A large international survey in twenty-four countries showed that BTCP predominantly occurred among patients who did not take analgesics to treat background pain compared to those who did (49). Multiple previous studies also supported this finding (22, 56–58). Tumor compression against bones, nerves, and other tissues causes the release of chemicals that initiate and mediate pain. The administration of analgesics for cancer patients helps to heal the damaged tissue and prevents the release of those chemicals (5, 23). Patients who had uncontrolled background pain were more likely to complain of BTCP (59–61).
This multi-center study was conducted in a research-scarce part of the world on breakthrough cancer pain. However, it did not establish temporal and causal relationships between factors and breakthrough cancer pain due to the cross-sectional nature of the study design. Statistical analysis was performed with logistic regression which could overestimate the odds ratio as the prevalence of BTCP was higher than 10%. In addition, we measured only spontaneous breakthrough pain but not incident pain during certain triggering activities such as motion. Furthermore, the inclusion of heterogeneous patients with different typologies of cancer might have limited the generalizability of the findings.
There is a high prevalence of breakthrough cancer pain in oncology units in Northern Ethiopia. Colorectal and lung cancer, metastasis, intensity of background pain, not using analgesics for background pain, and uncontrolled background pain were found to be significantly associated with breakthrough cancer pain. It is advised to regularly assess cancer patients for breakthrough cancer pain and provide adequate pain management.
Data and materials used in this study are available and can be presented by the corresponding author upon reasonable request.
Ethical approval was obtained from the Ethical Review Committee of the School of Medicine, University of Gondar (Reference number: SOM/1404/2022). Permission to conduct data collection was obtained from each hospital. Written informed consent was obtained from each study participant after a detailed explanation of the study. All methods were performed in accordance with the relevant research guidelines and regulations.
YT conceptualized the study and objectives and developed the proposal. YB, YN, and WM criticized the proposal. All authors participated in data management and statistical analyses. YB and YT led the manuscript preparation. All authors contributed to the article and approved the submitted version.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Aksum University, Aksum, Ethiopia, and the University of Gondar, Ethiopia.
Aksum University, University of Gondar Comprehensive Specialized Hospital, Felege-Hiwot Comprehensive Specialized Hospital, Dessie Comprehensive Specialized Hospital, study participants and the data collectors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ovayolu Ö, Ovayolu N, Aytaç S, Serçe S, Sevinc A. Pain in cancer patients: pain assessment by patients and family caregivers and problems experienced by caregivers. Supportive Care Cancer. (2015) 23(7):1857–64. doi: 10.1007/s00520-014-2540-5
2. Ferlay J, Colombet M, Soerjomataram I, Parkin DM, Piñeros M, Znaor A, et al. Cancer statistics for the year 2020: An overview. Int J cancer. (2021) 149(4):778–89. doi: 10.1002/ijc.33588
3. Bray F, Parkin DM, Gnangnon F, Tshisimogo G, Peko J-F, Adoubi I, et al. Cancer in sub-Saharan Africa in 2020: a review of current estimates of the national burden, data gaps, and future needs. Lancet Oncol (2022), 719–28. doi: 10.1016/S1470-2045(22)00270-4
4. Davies A, Buchanan A, Zeppetella G, Porta-Sales J, Likar R, Weismayr W, et al. Breakthrough cancer pain: an observational study of 1000 European oncology patients. J Pain symptom management. (2013) 46(5):619–28. doi: 10.1016/j.jpainsymman.2012.12.009
5. Marinangeli F, Saetta A, Lugini A. Current management of cancer pain in Italy: Expert opinion paper. Open Med (2022) 17(1):34–45.
6. Van den Beuken-van Everdingen M, De Rijke J, Kessels A, Schouten H, Van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol (2007) 18(9):1437–49. doi: 10.1093/annonc/mdm056
7. Payne RJPM. Recognition and diagnosis of breakthrough pain. Pain Med (2007) 8(suppl_1):S3–7. doi: 10.1111/j.1526-4637.2006.00269.x
8. Davies AN, Dickman A, Reid C, Stevens A-M, Zeppetella G. The management of cancer-related breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. Eur J Pain. (2009) 13(4):331–8. doi: 10.1016/j.ejpain.2008.06.014
9. Vellucci R, Mediati RD, Gasperoni S, Mammucari M, Marinangeli F, Romualdi P. Assessment and treatment of breakthrough cancer pain: from theory to clinical practice. J Pain Res (2017) 10:2147. doi: 10.2147/JPR.S135807
10. Deandrea S, Corli O, Consonni D, Villani W, Greco MT, Apolone G. Prevalence of breakthrough cancer pain: a systematic review and a pooled analysis of published literature. J Pain symptom management. (2014) 47(1):57–76. doi: 10.1016/j.jpainsymman.2013.02.015
11. Davies AN, Vriens J, Kennett A, McTaggart M. An observational study of oncology patients’ utilization of breakthrough pain medication. J Pain symptom management. (2008) 35(4):406–11. doi: 10.1016/j.jpainsymman.2007.05.010
12. Wengström Y, Geerling J, Rustøen T. European Oncology Nursing Society breakthrough cancer pain guidelines. Eur J Oncol Nursing. (2014) 18(2):127–31. doi: 10.1016/j.ejon.2013.11.009
13. Mercadante S, Portenoy RK. Understanding the chameleonic breakthrough cancer pain. Drugs (2021) 81(4):411–8. doi: 10.1007/s40265-021-01466-5
14. Camps Herrero C, Batista N, Díaz Fernández N, Escobar Álvarez Y, Gonzalo Gómez A, Isla Casado D, et al. Breakthrough cancer pain: review and calls to action to improve its management. Clin Trans Oncol (2020) 22(8):1216–26. doi: 10.1007/s12094-019-02268-8
15. Burton B, Zeppetella G. Assessing the impact of breakthrough cancer pain. Br J nursing. (2011) 20(Sup5):S14–S9. doi: 10.12968/bjon.2011.20.Sup5.S14
16. Camps Herrero C, Reina Zoilo J, Monge Martín D, Caballero Martínez F, Guillem Porta V, Aranda Aguilar E, et al. Active study: undetected prevalence and clinical inertia in the treatment of breakthrough cancer pain (BTcP). Clin Trans Oncol (2019) 21(3):380–90. doi: 10.1007/s12094-018-1925-1
17. Vellucci R, Fanelli G, Pannuti R, Peruselli C, Adamo S, Alongi G, et al. What to do, and what not to do, when diagnosing and treating breakthrough cancer pain (BTcP): expert opinion. Drugs (2016) 76(3):315–30. doi: 10.1007/s40265-015-0519-2
18. Guitart J, Vargas MI, De Sanctis V, Folch J, Salazar R, Fuentes J, et al. Effects of age among elderly cancer patients on breakthrough pain management with sublingual fentanyl tablets. Drugs (2019) 19(3):247–54. doi: 10.1007/s40268-019-0276-x
19. Haugen DF, Hjermstad MJ, Hagen N, Caraceni A, Kaasa S. Assessment and classification of cancer breakthrough pain: a systematic literature review. Eur Palliative Care Res Collaborative. (2010) 149(3):476–82. doi: 10.1016/j.pain.2010.02.035
20. Lennernäs B, Frank-Lissbrant I, Lennernäs H, Kälkner KM, Derrick R, Howell J. Sublingual administration of fentanyl to cancer patients is an effective treatment for breakthrough pain: results from a randomized phase II study. Palliative Med (2010) 24(3):286–93. doi: 10.1177/0269216309356138
21. Liu Q, Gao L-L, Dai Y-L, Wang Y, Wang H-X, Luo X-J, et al. Breakthrough pain: a qualitative study of patients with advanced cancer in Northwest China. Pain Manage Nursing. (2018) 19(5):506–15. doi: 10.1016/j.pmn.2017.11.006
22. Mercadante S, Maltoni M, Russo D, Adile C, Ferrera P, Rossi R, et al. The prevalence and characteristics of breakthrough cancer pain in patients receiving low doses of opioids for background pain. Cancers (2021) 13(5):1058. doi: 10.3390/cancers13051058
23. Mercadante S, Marchetti P, Cuomo A, Caraceni A, Mediati RD, Vellucci R, et al. Factors influencing the clinical presentation of breakthrough pain in cancer patients. Cancers (2018) 10(6):175. doi: 10.3390/cancers10060175
24. Montague L, Green CR. Cancer and breakthrough pain’s impact on a diverse population. Pain Med (2009) 10(3):549–61. doi: 10.1111/j.1526-4637.2009.00564.x
25. Pérez-Hernández C, Blasco A, Gándara Á, Mañas A, Rodríguez-López MJ, Martínez V, et al. Prevalence and characterization of breakthrough pain in patients with cancer in Spain: the CARPE-DIO study. Sci Rep (2019) 9(1):1–10.
26. Qadire MA, Tubaishat A, Aljezawi M. Cancer pain in Jordan: prevalence and adequacy of treatment. Int J palliative nursing. (2013) 19(3):125–30. doi: 10.12968/ijpn.2013.19.3.125
27. Shi L, Liu Y, He H, Wang C, Li H, Wang N. Characteristics and prognostic factors for pain management in 152 patients with lung cancer. Patient preference adherence. (2016) 10:571. doi: 10.2147/PPA.S103276
28. Wang N, Dong Y, Zhao L, Zhao H, Li W, Cui J. Factors associated with optimal pain management in advanced cancer patients. Curr Problems Cancer. (2019) 43(1):77–85. doi: 10.1016/j.currproblcancer.2018.05.002
29. Zeppetella G, O’Doherty CA, Collins S. Prevalence and characteristics of breakthrough pain in cancer patients admitted to a hospice. J Pain symptom management. (2000) 20(2):87–92. doi: 10.1016/S0885-3924(00)00161-5
30. Mercadante S, Adile C, Torta R, Varetto A, Fulfaro F, Giarratano A, et al. Meaningful cut-off pain intensity for breakthrough pain changes in advanced cancer patients. Curr Med Res opinion. (2013) 29(1):93–7. doi: 10.1185/03007995.2012.755120
31. Mercadante S, Valle A, Porzio G, Aielli F, Adile C, Ficorella C, et al. Relationship between background cancer pain, breakthrough pain, and analgesic treatment: a preliminary study for a better interpretation of epidemiological and clinical studies. Curr Med Res opinion. (2013) 29(6):667–71. doi: 10.1185/03007995.2013.792247
32. Hagen NA, Stiles C, Nekolaichuk C, Biondo P, Carlson LE, Fisher K, et al. The Alberta Breakthrough Pain Assessment Tool for cancer patients: a validation study using a delphi process and patient think-aloud interviews. J Pain symptom management. (2008) 35(2):136–52. doi: 10.1016/j.jpainsymman.2007.03.016
33. Oldenmenger WH, Pleun J, de Klerk C, van der Rijt CC. Cut points on 0–10 numeric rating scales for symptoms included in the Edmonton Symptom Assessment Scale in cancer patients: a systematic review. J Pain symptom management. (2013) 45(6):1083–93. doi: 10.1016/j.jpainsymman.2012.06.007
34. Schmidt S. OTC pain management: The importance of understanding pain. South Afr Pharmacist’s Assistant. (2021) 21(4):5–8.
36. Yang W, Chen T, Zhang W-W, Tian J-H, Yang Y-C, Wang Y-Q. Neurobiological mechanism of acupuncture analgesia in chronic somatic pain. In: Advanced acupuncture research: from bench to bedside. Springer (2022). p. 471–90.
37. Bennett MI, Attal N, Backonja MM, Baron R, Bouhassira D, Freynhagen R, et al. Using screening tools to identify neuropathic pain. Pain (2007) 127(3):199–203. doi: 10.1016/j.pain.2006.10.034
38. Webber K, Davies AN, Zeppetella G, Cowie MRJ. Development and validation of the breakthrough pain assessment tool (BAT) in cancer patients. J Pain symptom management. (2014) 48(4):619–31. doi: 10.1016/j.jpainsymman.2013.10.026
39. Sperlinga R, Campagna S, Berruti A, Laciura P, Ginosa I, Paoletti S, et al. Alberta Breakthrough Pain Assessment Tool: A validation multicentre study in cancer patients with breakthrough pain. Eur J Pain. (2015) 19(7):881–8. doi: 10.1002/ejp.612
40. Notartomaso S, Antenucci N, Liberatore F, Mascio G, Boccadamo Pompili SV, Font J, et al. Light-induced activation of a specific type-5 metabotropic glutamate receptor antagonist in the ventrobasal thalamus causes analgesia in a mouse model of breakthrough cancer pain. Int J Mol Sci (2022) 23(14):8018. doi: 10.3390/ijms23148018
41. Canal-Sotelo J, Trujillano-Cabello J, Larkin P, Arraràs-Torrelles N, González-Rubió R, Rocaspana-Garcia M, et al. Prevalence and characteristics of breakthrough cancer pain in an outpatient clinic in a Catalan teaching hospital: incorporation of the Edmonton Classification System for Cancer pain into the diagnostic algorithm. BMC palliative Care (2018) 17(1):1–8. doi: 10.1186/s12904-018-0336-y
42. Gómez-Batiste X, Madrid F, Moreno F, Gracia A, Trelis J, Nabal M, et al. Breakthrough cancer pain: prevalence and characteristics in patients in Catalonia, Spain. J Pain symptom management. (2002) 24(1):45–52. doi: 10.1016/S0885-3924(02)00421-9
43. Greco MT, Corli O, Montanari M, Deandrea S, Zagonel V, Apolone G. Epidemiology and pattern of care of breakthrough cancer pain in a longitudinal sample of cancer patients: results from the Cancer Pain Outcome Research Study Group. Clin J pain. (2011) 27(1):9–18. doi: 10.1097/AJP.0b013e3181edc250
44. Raj SX, Thronaes M, Brunelli C, Hjermstad MJ, Klepstad P, Kaasa S. A cross-sectional study on prevalence of pain and breakthrough pain among an unselected group of outpatients in a tertiary cancer clinic. Supportive Care Cancer. (2014) 22(7):1965–71. doi: 10.1007/s00520-014-2178-3
45. Baek SK, Kang SY, Sym SJ, Kim YS, Lee JY. A Korean nationwide survey for breakthrough cancer pain in an inpatient setting. Cancer Res Treatment: Off J Korean Cancer Assoc (2016) 48(2):768–74. doi: 10.4143/crt.2015.087
46. Li Z, Aninditha T, Griene B, Francis J, Renato P, Serrie A, et al. Burden of cancer pain in developing countries: a narrative literature review. Clinico-economics outcomes research: CEOR. (2018) 10:675. doi: 10.2147/CEOR.S181192
47. Al-Ibraheem A, Abdlkadir AS, Mohamedkhair A, Mikhail-Lette M, Al-Qudah M, Paez D, et al. Cancer diagnosis in areas of conflict. Front Oncol (2022) 12. doi: 10.3389/fonc.2022.1087476
48. Caglevic C, Rolfo C, Gil-Bazo I, Cardona A, Sapunar J, Hirsch FR, et al. The armed conflict and the impact on patients with cancer in Ukraine: urgent considerations. JCO Global Oncol (2022) 8):e2200123. doi: 10.1200/GO.22.00123
49. Caraceni A, Martini C, Zecca E, Portenoy RK. Breakthrough pain characteristics and syndromes in patients with cancer pain. An international survey. Palliative Med (2004) 18(3):177–83. doi: 10.1191/0269216304pm890oa
50. Caraceni A, Bertetto O, Labianca R, Maltoni M, Mercadante S, Varrassi G, et al. Episodic (breakthrough) pain prevalence in a population of cancer pain patients. Comparison of clinical diagnoses with the QUDEI—Italian questionnaire for intense episodic pain. J Pain symptom management (2012) 43(5):833–41. doi: 10.1016/j.jpainsymman.2011.05.018
51. Simmons CP, MacLeod N, Laird BJ. Clinical management of pain in advanced lung cancer. Clin Med Insights: Oncol (2012) 6:331–46. doi: 10.4137/CMO.S8360
52. Walling AM, Weeks JC, Kahn KL, Tisnado D, Keating NL, Dy SM, et al. Symptom prevalence in lung and colorectal cancer patients. J Pain symptom management. (2015) 49(2):192–202. doi: 10.1016/j.jpainsymman.2014.06.003
53. Mercadante S, Adile C, Masedu F, Marchetti P, Costanzi A, Aielli F. Factors influencing the use of opioids for breakthrough cancer pain: A secondary analysis of the IOPS-MS study. Eur J Pain. (2019) 23(4):719–26. doi: 10.1002/ejp.1339
54. Koh S-J, Keam B, Hyun MK, Ju Seo J, Uk Park K, Oh SY, et al. Cancer pain management education rectifies patients’ misconceptions of cancer pain, reduces pain, and improves quality of life. Pain Med (2018) 19(12):2546–55. doi: 10.1093/pm/pny039
55. Wang H, Li X, Xie X, Zhao H, Gao Y, Li Y, et al. Promotion of bone cancer pain development by decorin is accompanied by modification of excitatory synaptic molecules in the spinal cord. Mol pain. (2019) 15:1744806919864253. doi: 10.1177/1744806919864253
56. Hjermstad MJ, Kaasa S, Caraceni A, Loge JH, Pedersen T, Haugen DF, et al. Characteristics of breakthrough cancer pain and its influence on quality of life in an international cohort of patients with cancer. BMJ Supportive Palliative Care (2016) 6(3):344–52. doi: 10.1136/bmjspcare-2015-000887
57. Mercadante S, Marchetti P, Cuomo A, Caraceni A, Mediati RD, Mammucari M, et al. Breakthrough cancer pain: preliminary data of the italian oncologic pain multisetting multicentric survey (IOPS-MS). Adv Ther (2017) 34(1):120–35. doi: 10.1007/s12325-016-0440-4
58. Fan R, Li X, Yang S, Bu X, Chen Y, Wang Y, et al. Retrospective observational study on the characteristics of pain and associated factors of breakthrough pain in advanced cancer patients. Pain Res Manage (2022) 2022:1–11. doi: 10.1155/2022/8943292
59. Mercadante S, Adile C, Giarratano A, Casuccio A. Breakthrough pain in patients with abdominal cancer pain. Clin J Pain. (2014) 30(6):510–4. doi: 10.1097/AJP.0000000000000004
60. Baek S, Kim D, Lee J. 491P_PR Background pain vs breakthrough pain? Which is the priority of cancer pain treatment. Ann Oncol (2016) 27:ix159. doi: 10.1016/S0923-7534(21)00649-9
61. Løhre ET, Klepstad P, Bennett MI, Brunelli C, Caraceni A, Fainsinger RL, et al. From “breakthrough” to “episodic” cancer pain? A European Association for Palliative Care Research Network Expert Delphi Survey toward a common terminology and classification of transient cancer pain exacerbations. J Pain symptom management. (2016) 51(6):1013–9. doi: 10.1016/j.jpainsymman.2015.12.329
Keywords: breakthrough pain, cancer pain, cancer, pain, breakthrough cancer pain (BTCP)
Citation: Tekie Y, Nigatu YA, Mekonnen W and Berhe YW (2024) Breakthrough pain among cancer patients at oncology units in Northern Ethiopia; a multi-center study. Front. Oncol. 13:1248921. doi: 10.3389/fonc.2023.1248921
Received: 03 July 2023; Accepted: 18 December 2023;
Published: 09 January 2024.
Edited by:
Karina Meira, School of Health at the Federal University of Rio Grande do Norte, BrazilReviewed by:
Akram Al-ibraheem, King Hussein Cancer Center, JordanCopyright © 2024 Tekie, Nigatu, Mekonnen and Berhe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yophtahe Woldegerima Berhe, eW9waHRpaUBnbWFpbC5jb20=
†Present address: Yophtahe Woldegerima Berhe, Department of Global Public Health, IKarolinska Institutet, Stockholm, Sweden
†ORCID: Yohanes Tekie, orcid.org/0000-0002-0988-7723
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.