- 1Department of General Surgery, Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, Jiangsu, China
- 2Department of Gynecology, Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, Jiangsu, China
Background: Duplication of the transverse colon is a rare gastrointestinal malformation. Its pathogenesis is still unclear, and it is extremely rare in adults. Patients often present with symptoms of tumor compression such as abdominal mass, abdominal pain, and constipation as the first manifestation.
Methods and result: A patient with a duplication of the transverse colon was admitted to the Department of General Surgery of our hospital. Laparoscopic exploration found a mass at the rear of the transverse colon near the splenic flexure, and the root was connected to the middle portion of the transverse colon.
Conclusion: Surgery is a radical treatment and reduces the possibility of perforation, bleeding, obstruction, and cancer.
Introduction
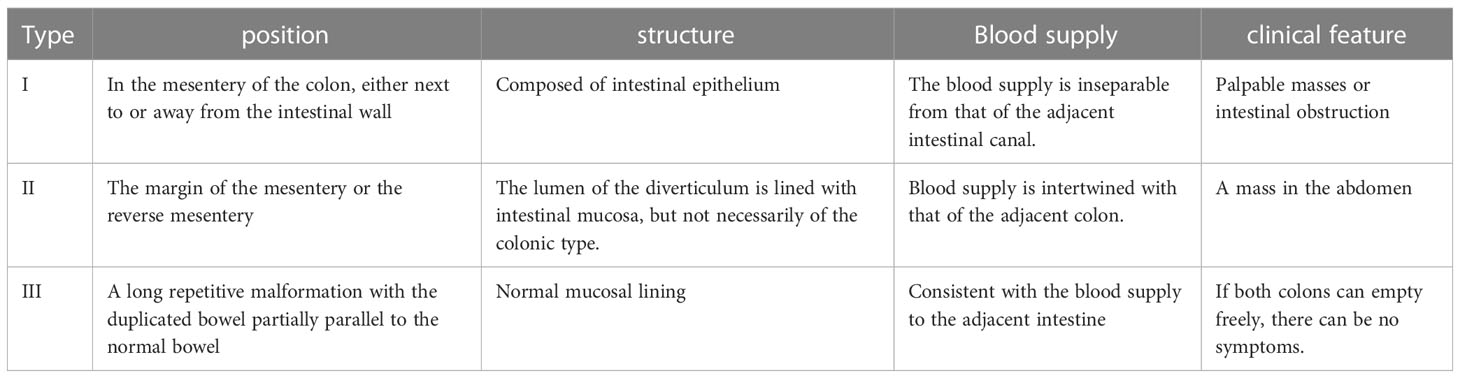
Intestinal duplication malformation is a rare congenital gastrointestinal malformation clinically known as ileal and ileocecal valve malformations. The condition is more common in children under the age of two, with the most common type being ileal and ileocecal valve malformations (approximately 60%), followed by the jejunum (8%), colon (6%) and rectum (5%). Intestinal repeats can generally be divided into four structures (1): tubular structure attached to the mesenteric side separated from the normal intestine (2); double-tube structure communicating with the intestinal lumen (3); cystic structure attached to the mesentery and not communicating with the intestinal lumen; and (4) spherical structure adjacent to the intestine (Figure 1) (1). The cystic structure is the most common, accounting for 90%-95%, while the tubular structure accounts for 5%-10%. The symptoms of this condition are nonspecific and can include abdominal mass, pain, constipation, intussusception, bleeding, and other manifestations. As a result, it can easily be misdiagnosed as an abdominal tumor (2). There have been few reports of repetitive malformations in the transverse colon in China. On January 28, 2023, a patient with a duplication of the transverse colon was admitted to the Department of General Surgery of our hospital in order to improve the understanding of the disease among gastrointestinal surgeons and include it in the differential diagnosis of abdominal pain.
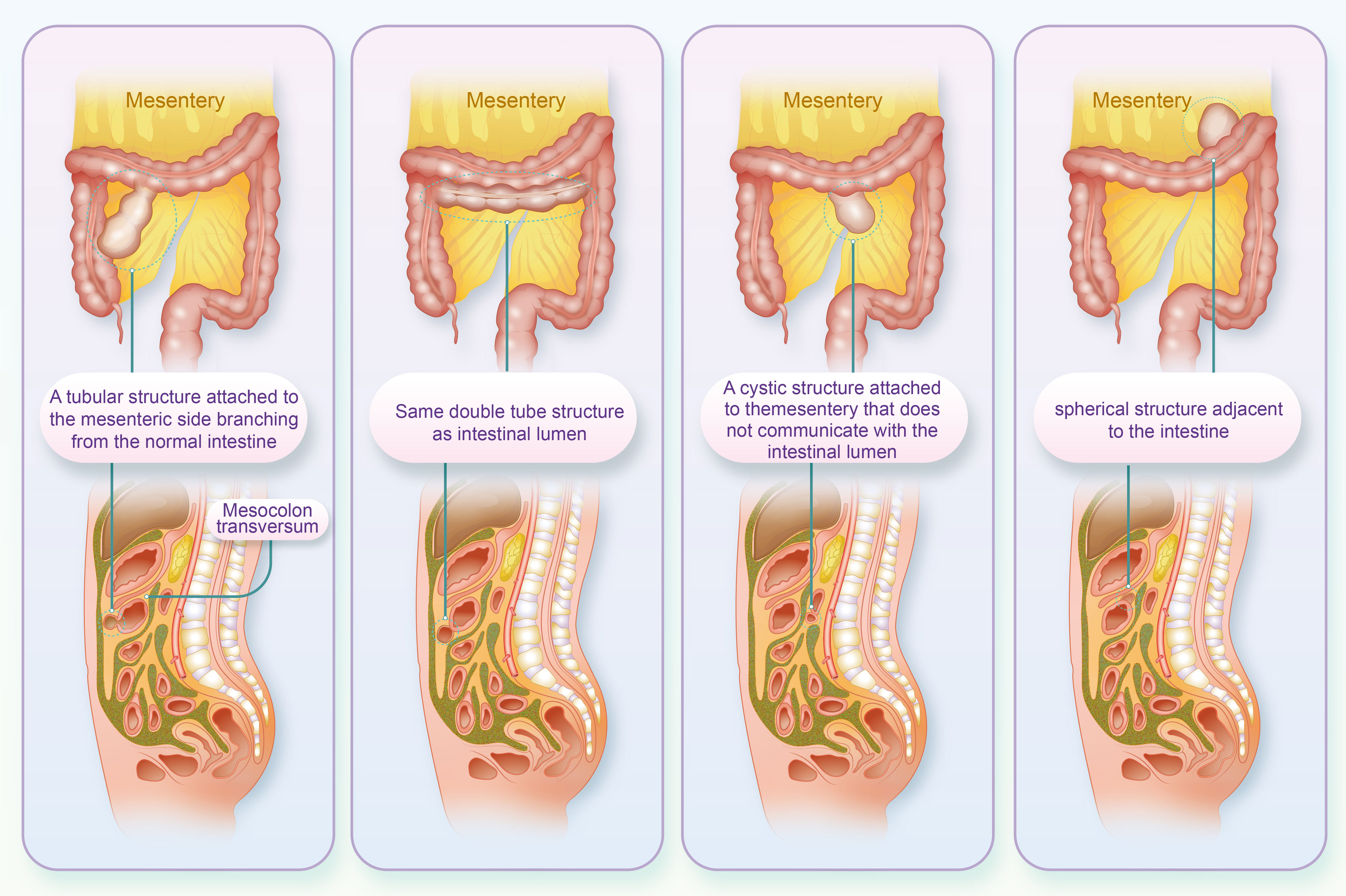
Figure 1 The four structures of the intestinal repeat (Above is the coronal position, below is the sagittal position).
Case presentation
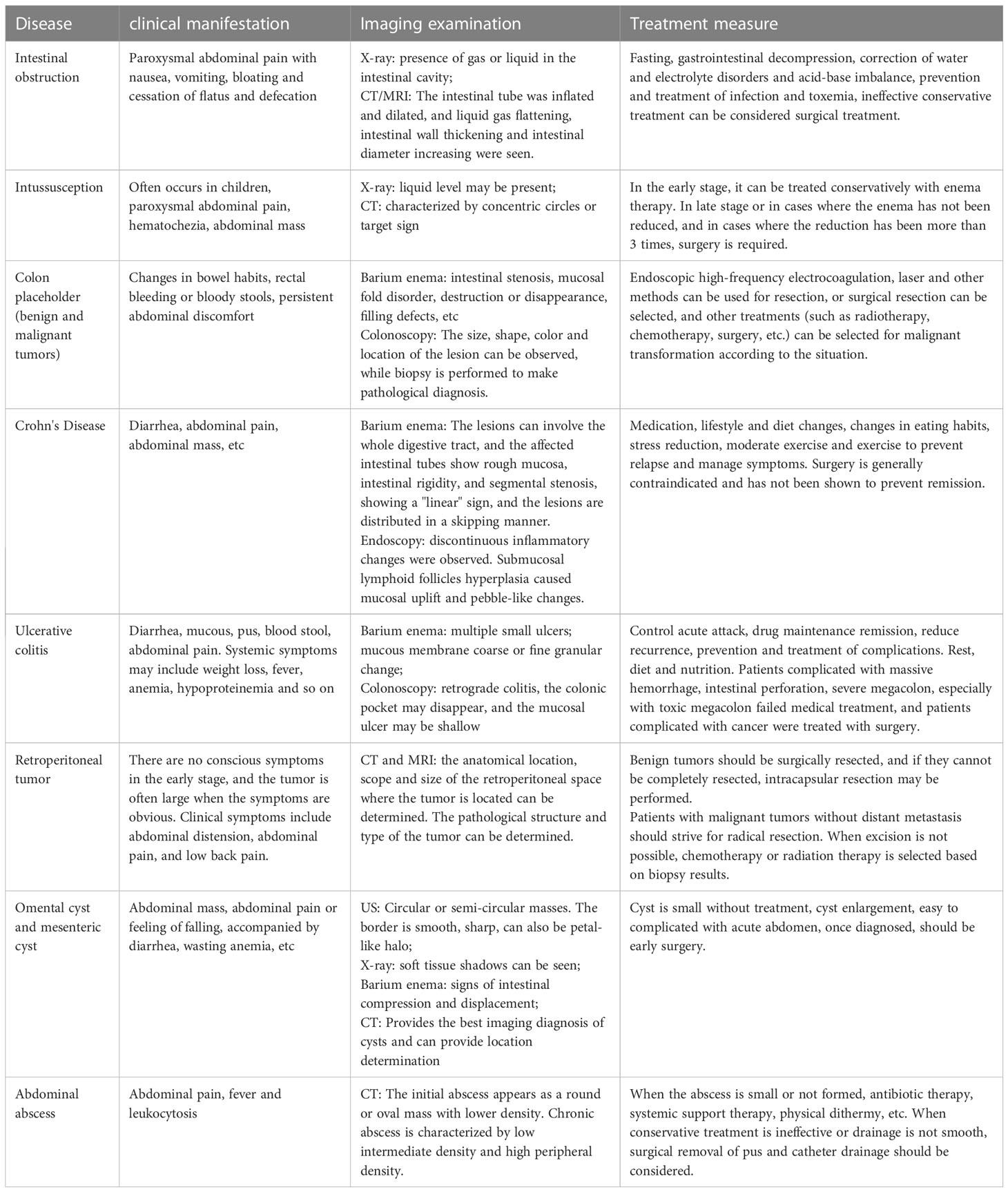
On January 2, 2023, an unmarried 30-year-old male patient presented with intercropping epigastric distension and pain that had persisted for over a month and worsened over the past week. One month prior, the patient experienced epigastric tenderness without being predisposed to referred pain, nausea, vomiting, acid belching, or hiccups. 2023 January 26 to another hospital to check the abdominal computed tomography (CT) suggests: “The left middle abdominal soft tissue mass is occupied, considering the malignant tumor lesion, there is pipeline communication between the lesion and the transverse colon, and the gas accumulation is seen in it, the other end is the blind end, and the periphery of the lesion exudes, and multiple enlarged lymph nodes can be seen”. After rehydration, pain relief were administered. However, there was no significant improvement, and the patient was transferred to our hospital to enroll in the “abdominal pain” department. Upon admission, the patient complained of obvious swelling pain and occasional colic with cold sweats, but there was no cough or eating obstruction. The patient reported poor sleep, normal urine adjustment, and 2-3 bowel movements per day, with no black or bloody stool. There was no previous family history of intestinal congenital diseases. There was no previous history of abdominal surgery. Physical examination revealed a flat abdomen with no gastrointestinal type, peristaltic waves, mid-upper abdominal tenderness, rebound tenderness, and no palpable mass. After a complete 3.0 T full abdominal magnetic resonance (MRI) plain scan and enhancement, the patient was diagnosed with a soft tissue mass in the left middle abdominal tube with a size of approximately 6.4*4.7 cm. The mass showed a long T1 and long T2 signal, and multiple gas signals were seen inside the lesion. The sac-like long T1 long T2 signal shadow was seen behind the left peritoneum, the size was approximately 2.1*1.3 cm, and the enhanced scan did not show strengthening. The results suggest the presence of left mid-quadrant lesions, which could be inflammatory lesions or lymphoma that need to be drained. Moreover, there was a left retroperitoneal cystic mass, which could be a benign lesion, but lymphangioma was possible, and regular review was recommended. In the case of barium enema colitis, the upper right edge of the transverse colon is seen to the right to left, with a walking curved thin bowel tube-like shadow. The base is approximately 42 mm wider, and in the supine position, it is inflated, the prone position is full, the liquid level is visible in the distal section of the vertical position, the total length is approximately 190 mm, the blind end is seen, and a titanium clip can be seen in the proximal section. The results suggest an abnormal open bowel lesion in the transverse colon. A painless colonoscopy revealed a dilated lumen and an open-like structure in the reverse scope. Pathological diagnosis showed chronic inflammation of mucosal tissue covered with squamous epithelium and gastric columnar epithelium (Figures 2A–F).
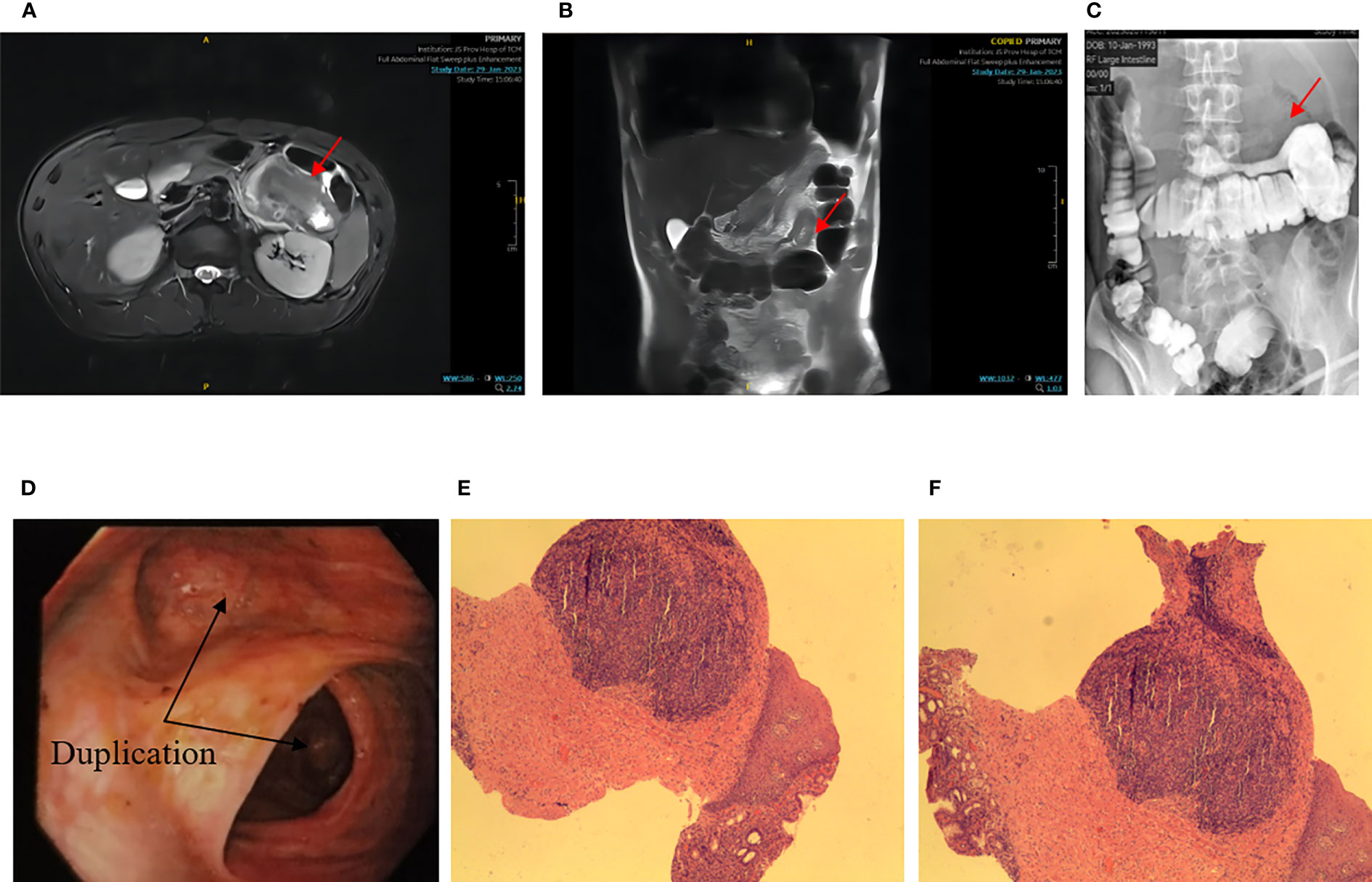
Figure 2 (A) NMR transverse axial view: the red arrow indicates a soft tissue mass located in the left mid-abdomen, closely related to the bowel, approximately 6.4*4.7cm, with multiple internal gas signals; (B) Coronal view of MRI; (C) Barium enema X – ray: the red arrow points to a right-to-left image of a smaller intestinal tube about 190mm long; (D) Endoscopy: the black arrow points to an open-like structure, and the distal segment’s stenosis was obvious; (E, F) Pathology: chronic inflammation of mucosal tissue covered with squamous epithelium and gastric columnar epithelium). Coloration HE, magnification ×100.
To confirm the diagnosis, laparoscopic surgery was performed under general anesthesia at 1:40 on February 7, 2023. Intraoperative exploration revealed a palpable mass near the splenic flexure at the back of the transverse colon, measuring approximately 8.0 cm by 9.0 cm, with an intact capsule, inflammatory edema of surrounding tissues, and adhesions. The mass did not invade adjacent organs, and the root was connected to the middle section of the transverse colon, confirming the preoperative diagnosis of repetitive deformity of the transverse colon. The root of the mass was exposed, revealing nourishing blood vessels emanating from the ligament of Treitz, and a dissected specimen showed the presence of intestinal mucosal tissue in the mass (Figures 3A–C). we removed the duplicate colon and extended it 2cm into the original transverse colon, and performed a colon-colon anastomosis with a stapler. After surgery, the patient underwent an accelerated rehabilitation program and recovered well, leading to their discharge from the hospital on February 13.

Figure 3 Specimens seen and resected during surgery [(A, B) proximal splenic flexural mass at the back of the transverse colon, approximately 8.0 cm by 9.0 cm, inflammatory edema of the surrounding tissues, the root of the mass is connected to the middle section of the transverse colon, and the root of the mass is exposed with nourishing blood vessels emanating from the ligament of Treitz; (C) The specimen showed intestinal mucosal tissue in the mass. The black arrow indicates a duplicate deformity that separates from the normal transverse colon and communicates with the intestinal lumen)].
Postoperative pathology (Figures 4A, B) (transverse colon) revealed a microscopic organ-like structure visible to the intrinsic muscle wall, which was covered with squamous epithelium, gastric mucosa, and large intestine mucosa. The propria muscle wall and extramuscular fibrous tissue showed hyperplasia with focal inflammatory granulation tissue hyperplasia, foreign body giant cell reaction, and abscess formation. Combined with clinical findings, this is consistent with repetitive digestive tract malformations with chronic active inflammatory changes. Immunohistochemical results indicated that hyperplastic fibrous tissue expressed SMA (+), Desmin (focal+), S-100 (-), cald esmon (-), B-catenin (pulp+), and CD34 (vascular +).
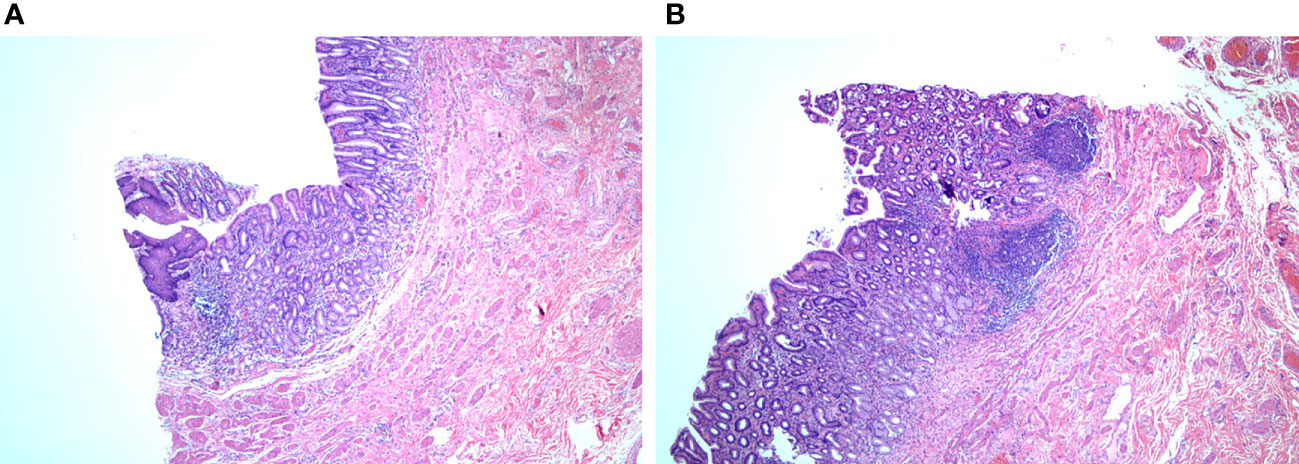
Figure 4 Pathology report (A) and (B) can be seen in the intrinsic muscular wall, covered with squamous epithelium, gastric mucosa, and large intestine mucosa). coloration HE, magnification ×200.
Discussion
Gastrointestinal repetitive malformations are rare congenital malformations and usually present as cystic or tubular structures on one side of the mesangium in neonates (3, 4). The incidence of the disease is 1/10000~1/4500, and it can occur in the entire digestive tract from the oropharynx to the anus (5). Colonic duplication is a type of repetitive gastrointestinal malformation reported in fewer than 50 cases in the literature since 1950, with 80% of cases occurring before age 2 (6). Adult onset of the disease is rare (7). The disease was first reported in 1876 and is known as “alimentary tract duplications” (8). The disease has three major features: (1) it is similar to normal intestinal structure; (2) the lining mucosa is similar to the intestine; and (3) it is attached to the normal intestinal tract and shares blood supply (9). The disease does not have specific symptoms, but it may cause an abdominal mass, chronic pain, and constipation. Volvulus, intussusception, bleeding, or perforation are rare and generally occur in the sigmoid colon, similar to diverticulitis. Colonic repetitive malformations can occur anywhere in the colon, mostly with normal digestive tract structure. Most malformations fuse with the attached main bowel to form a common muscular wall, sharing a common serosus, intestinal membrane, and blood supply, but with independent, separate, or communicating mucosal cavities. For repetitive colonic malformations, McPherson AG (10) proposed another classification, namely, type I (simple cyst), type II (diverticulus), and type III (tubular colon malformation) (Table 1), which in turn can be Y-type and double-cast (11). In this case, the root of the mass is connected to the middle section of the transverse colon, the proximal blind closure. A large amount of mucosal secretion accumulates in the intestinal lumen, which belongs to type III. Y type.
Based on the literature at home and abroad to clear diagnosis of adult transverse repeat deformity in 16 cases and 1 case analysis, this paper in order to improve the understanding of the disease (Table 2) (12–26). Two main theories explain the pathogenesis of repetitive malformations in the transverse colon. The first theory, abnormal lumen recanalization, suggests that during embryonic development, the internal embryonic vacuole enlarges and fuses to form the intestinal lumen. However, a range of factors can cause the vacuole to remain separated, resulting in one or more primitive intestinal repeats. The second theory, the diverticular theory, proposes that embryonic diverticula cause repetitive malformations. However, this theory cannot fully explain complete pancolonic repetitive malformations with a round or longitudinal muscular layer (27, 28). In addition, environmental factors such as trauma or hypoxia can contribute to the condition (29). Over time, the compressive effects due to secretion and accumulation of intestinal mucus may be the underlying pathogenesis.
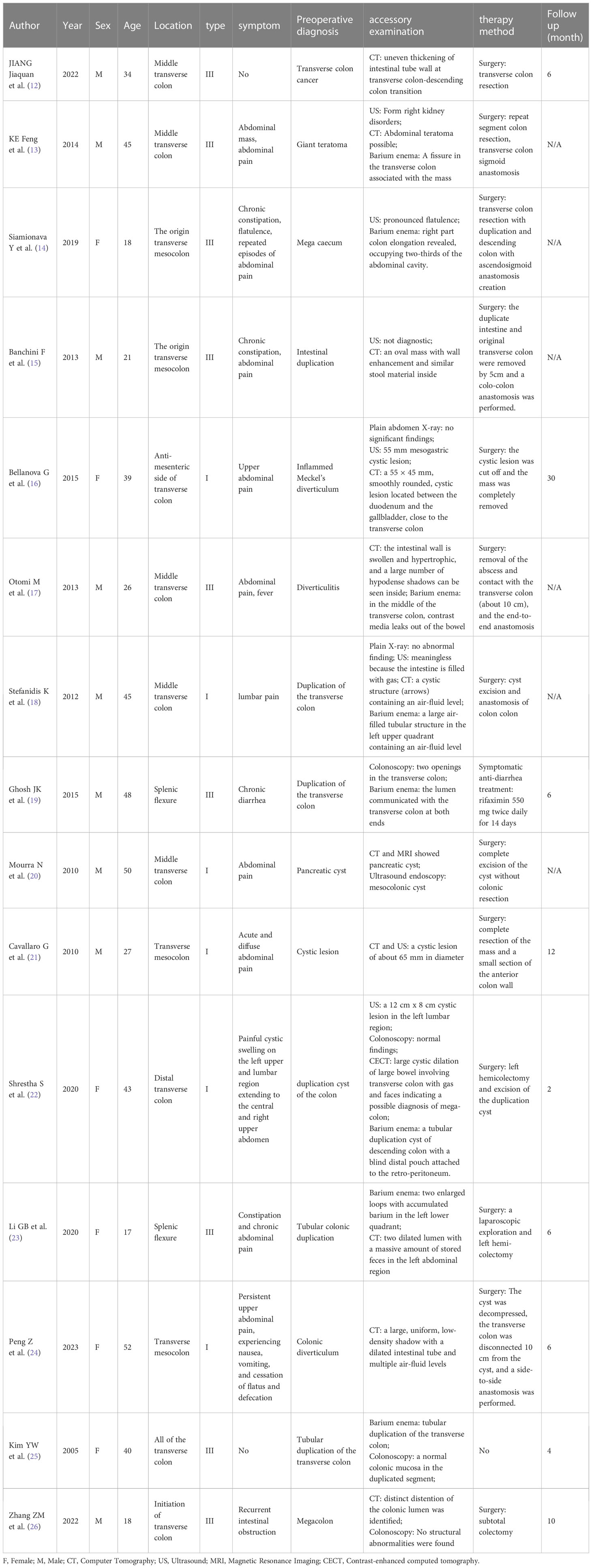
Table 2 Demographic and clinical profiles of transverse colon duplication have been reported previously.
There is a lack of unified diagnostic and treatment criteria for transverse colonic repetitive malformations. 12 cases were diagnosed using abdominal multirow CT (12, 13, 15–18, 20–24, 26), 8 cases using digitized barium enema colography (13, 14, 17–19, 22, 23, 25), and colonoscopy in 4 cases (19, 20, 25, 26), 8 cases using US (13–16, 18, 20–22) and 2 cases using plain X-ray (16, 18). Because the symptoms of repeat transverse colon malformations in adults are mostly nonspecific, clinical diagnosis is difficult. All diseases with abdominal pain and abdominal mass as the main complaints should be included in the differential diagnosis of this disease. The differential diagnosis of transverse colon duplication is shown in Table 3. Abdominal CT, barium enema, and colonoscopy remain the best diagnostic tools. US is often the first choice for screening because it has no radiation and is simple to operate. CT shows a comprehensive anatomical structure, and 99TCM-pertechnetate scintigraphy is helpful for the diagnosis of highly suspected intestinal duplication in clinical practice, especially for those with no clear positive performance on CT and ultrasound (30). Type I (simple cysts) are easier to observe on US than CT due to their liquid contents attached to the mesentery. Barium enema may show an open-mouth lesion that communicates with a normal bowel. Colonoscopy can also be used when repetitive malformations and the opening between the normal lumen are evident.
Surgical resection is a radical treatment for repetitive deformities of the colon. Only one patient in previous studies had been treated with drugs (19), with one case complicated by transverse colon carcinogenesis (12) and one case of mild dysplasia (20). Resection of repetitive malformations and additional resection of 2 cm to the normal bowel may disengage the fibrotic bowel and reduce the risk of perforation, bleeding, obstruction, and carcinogenesis (31). For type I, simple cystectomy and cyst mucosal decortication may be used, but if there is communication with the normal bowel tube, the adjacent bowel needs to be removed to ensure complete cyst resection. With the development of endoscopic technology, endoscopic submucosal dissection for the treatment of intestinal duplication has gradually become one of the new treatment methods that can partially replace surgical operations, which has the characteristics of less trauma and low cost. In recent years, ESD resection has also been reported (32).
Conclusion
In conclusion, transverse colonic repetitive malformation is a rare gastrointestinal malformation with unclear pathogenesis. Children often have acute abdomen as the first symptom, while adults experience atypical onset and tumor compression symptoms such as abdominal mass, abdominal pain, and constipation. Full abdominal CT, contrast enema, and colonoscopy were usually used to make the diagnosis. Surgery is a radical treatment and reduces the possibility of perforation, bleeding, obstruction, and cancer.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the [individual(s) AND/OR minor(s)’ legal guardian/next of kin] for the publication of any potentially identifiable images or data included in this article.
Author contributions
XZ and GD conceptualized the report. GG supervised the data collection. XZ and GD drafted the report. All authors contributed to the article and approved the submitted version.
Acknowledgments
We are grateful to the patient for giving consent for the case report.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. SMITH JR. Accessory enteric formations: a classification and nomenclature. Arch Dis Child (1960) 35(179):87–9. doi: 10.1136/adc.35.179.87
2. Kekez T, Augustin G, Hrstic I, Smud D, Majerovic M, Jelincic Z, et al. Colonic duplication in an adult who presented with chronic constipation attributed to hypothyroidism. World J Gastroentero (2008) 14(4):644–6. doi: 10.3748/wjg.14.644
3. Cheng KC, SF Ko, Lee KC. Colonic duplication presenting as a huge abdominal mass in an adult female. Int J Colorectal Dis (2019) 34(11):1995–8. doi: 10.1007/s00384-019-03409-9
4. Fotiadis C, Genetzakis M, Papandreou I, Misiakos EP, Agapitos E, Zografos GC. Colonic duplication in adults: report of two cases presenting with rectal bleeding. World J Gastroentero (2005) 11(32):5072–4. doi: 10.3748/wjg.v11.i32.5072
5. Bakir B, Gokce S, Dursun M, Guven K, Salmaslioglu A. An unusual cause of diffuse ascites in an infant: colonic duplication associated with bladder duplication. Diagn Interv Radiol (2009) 15(3):210–1.
6. Cherchi V, Intini S, Velkoski J, Calandra S, Ventin M, MM D, et al. A rare case of duplication of the descending colon in a pregnant woman: case report and literature review. Acta BioMed (2023) 94(S1):e2023042. doi: 10.23750/abm.v94iS1.12169
7. Vargas-de LLR, Garcia-Huerta G, Gutierrez-Mata F, Noriega-Maldonado O, Dorantes-Gonzalez HJ, Lopez-GiacOman C. [Sigmoid colon duplication: an adult case report.]. Rev Gastroenterol Me (2009) 74(3):259–62.
8. Med LW. Duplications of the alimentary tract. South Med J (1937) 30(1937):363–71. doi: 10.1097/00007611-193704000-00002
9. Kumar A, Kumar J, Gadodia A, Chumber S, Aggarwal L. Multiple short-segment colonic duplications. Pediatr Radiol (2008) 38(5):567–70. doi: 10.1007/s00247-007-0730-8
10. McPherson AG, Trapnell JE, Airth GR. Duplication of the colon. Brit J Surg (1969) 56(2):138–42. doi: 10.1002/bjs.1800560214
11. Kyo K, Azuma M, Okamoto K, Nishiyama M, Shimamura T, Maema A, et al. Laparoscopic resection of adult colon duplication causing intussusception. World J Gastroentero (2016) 22(7):2398–402. doi: 10.3748/wjg.v22.i7.2398
12. JIANG J, LIU W, YAN X. Two cases of adult intestinal duplication report and literature review. Clin Res Pract (2022) 7(20):39–41. doi: 10.19347/j.cnki.2096-1413.202220010
13. KE F, CHENG Y, YIN D. A case report of repetitive malformation in the transverse colon descending colon. Chin J Pract Surg (2014) 34(02):195. doi: CNKI:SUN:ZGWK.0.2014-02-038
14. Siamionava Y, Varabei A, Makhmudov A. Transverse colon duplication with chronic constipation in adult. BMJ Case Rep (2019) 12(4):e226450. doi: 10.1136/bcr-2018-226450
15. Banchini F, Delfanti R, Begnini E, Tripodi MC, Capelli P. Duplication of the transverse colon in an adult: case report and review. World J Gastroentero (2013) 19(4):586–9. doi: 10.3748/wjg.v19.i4.586
16. Bellanova G, Valduga P, Costa A, Barbareschi M, De Carli N, Giannelli G, et al. Double intestinal duplication and incidental neuroendocrine tumor of appendix, a rare case of acute abdomen. Int J Surg Case Rep (2015) 13:116–8. doi: 10.1016/j.ijscr.2015.06.021
17. Otomi M, Yano M, Takai S, Takahashi K, Nakamoto J, Omoya T, et al. [A case of duplication of the transverse colon in adult, lined with ciliated columnar and squamous epithelium]. Nihon Shokakibyo Gakkai Zasshi (2013) 110(12):2089–99. doi: 10.5334/jbr-btr.92
18. Stefanidis K, Lappas I, Kolofousi C, Kalogeropoulos I. A rare presentation of colonic duplication cyst: report of a case and review of literature. Jbr-Btr (2012) 95(2):71–3. doi: 10.5334/jbr-btr.92
19. Ghosh JK, Goyal SK, Behera MK, Abhilash VB, Dixit VK, Jain AK. Duplication of transverse colon in an adult presenting as chronic diarrhea. Trop Gastroenterol (2015) 36(1):62–3. doi: 10.7869/tg.253
20. Mourra N, Chafai N, Bessoud B, Reveri V, Werbrouck A, Tiret E. Colorectal duplication in adults: report of seven cases and review of the literature. J Clin Pathol (2010) 63(12):1080–3. doi: 10.1136/jcp.2010.083238
21. Cavallaro G, Arena R, D'Ermo G, Basile U, Polistena A, Scorsi A, et al. Cystic duplication of transverse colon: an unusual case of abdominal pain and bowel obstruction. G Chir (2010) 31(5):236–8.
22. Shrestha S, Adhikari SK. Colonic duplication cyst in an adult woman: A case report. Jnma J Nepal Med Assoc (2020) 58:948–50. doi: 10.31729/jnma.5114
23. Li GB, Han JG, Wang ZJ, Zhai ZW, Tao Y. Successful management of tubular colonic duplication using a laparoscopic approach: A case report and review of the literature. World J Clin cases (2020) 8:3291–98. doi: 10.12998/wjcc.v8.i15.3291
24. Peng Z, Zhang M, Wang R, Huang H, Sun Z, Li Y. Giant duplication of the transverse colon in an adult: A case report and literature review. Open Life Sci (2023) 18:20220626. doi: 10.1515/biol-2022-0626
25. Kim YW, Kim J, Lee KY, Kim NK, Cho CH. Asymptomatic tubular duplication of the transverse colon in an adult. Yonsei Med J (2005) 46:189–91. doi: 10.3349/ymj.2005.46.1.189
26. Zhang ZM, Kong S, Gao XX, Jia XH, Zheng CN. Colonic tubular duplication combined with congenital megacolon: A case report. World J Clin cases (2022) 10:12768–74. doi: 10.12998/wjcc.v10.i34.12768
27. Bakir B. Colonic duplications: clinical presentation and radiologic features of five cases. Eur J Radiol (2007) 61(3):490. doi: 10.1016/j.ejrad.2006.11.013
28. Zouari M, Bouthour H, Abdallah RB, Hlel Y, Malek RB, Gharbi Y, et al. Alimentary tract duplications in children: report of 16 years' experience. Afr J Paediatr Surg (2014) 11(4):330–3. doi: 10.4103/0189-6725.143146
29. Yang J, Kim KH, Lee JY, Wang KC. Caudal duplication syndrome: a literature review and reappraisal of its pathoembryogenesis. Child Nerv Syst (2021) 37(8):2577–87. doi: 10.1007/s00381-021-05166-z
30. WANG W, DONG H, ZHU X, ZHAO F, YU Y. Multiple intestinal duplication with ectopic pancreas in adult: a case report. J Laparoscopic Surg (2022) 27:879–80. doi: 10.13499/j.cnki.fqjwkzz.2022.11.879
31. Reiser-Erkan C, Erkan M, Ulbrich E, Nahrig J, Kleeff J. Cystic colon duplication causing intussusception in a 25-year-old man: report of a case and review of the literature. BMC Surg (2010) 10:19. doi: 10.1186/1471-2482-10-19
Keywords: transverse colon, duplication of deformity, abdominal pain, adult, space-occupying lesion, surgical resection
Citation: Zhang X, Di G, Cheng W, Wang C, Gong G and Jiang Z (2023) Duplication of the transverse colon in adults: a case report and literature review. Front. Oncol. 13:1230860. doi: 10.3389/fonc.2023.1230860
Received: 29 May 2023; Accepted: 31 July 2023;
Published: 04 September 2023.
Edited by:
Audrius Dulskas, National Cancer Institute, LithuaniaReviewed by:
Roy Hajjar, Montreal University, CanadaZhanxue Zhao, Qinghai Provincial People’s Hospital, China
Copyright © 2023 Zhang, Di, Cheng, Wang, Gong and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guanwen Gong, bG92ZV9nZ3cyQDE2My5jb20=; Zhiwei Jiang, c3VyZ2VyeTM0QDE2My5jb20=
†These authors have contributed equally to this work
‡ORCID: Xiaochun Zhang, orcid.org/0009-0000-3644-5333
 Xiaochun Zhang
Xiaochun Zhang Guangci Di
Guangci Di Wei Cheng
Wei Cheng Cuizhong Wang
Cuizhong Wang Zhiwei Jiang1*
Zhiwei Jiang1*