
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Oncol., 30 January 2024
Sec. Surgical Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1215284
This article is part of the Research TopicOncoplastic Surgery for Breast CancerView all 13 articles
Breast surgery has evolved from mastectomy to breast-conserving surgery (BCS). Breast oncoplastic surgery later emerged with the inclusion and development of techniques used in plastic surgery for breast neoplasms. Recently, a new paradigm has been considered for mastectomy candidates with large multifocal and multicentric tumours, designated extreme oncoplasty (EO), which has allowed new techniques to be applied to tumours that would have been ineligible for BCS before. There are few publications and no uniform descriptions grouping all the technical possibilities and new indications together. We performed this a review with the objective of evaluating the indications and surgeries performed in the EO context, representing a new perspective for BCS. We observed new indications as extensive microcalcifications, locally advanced breast carcinoma with partial response to chemotherapy, small to moderate-sized non-ptotic central tumours and extreme ptosis. Small breasts are able for EO since the presence of ptosis. New surgeries are reported as disguised geometric compensation, perforators flaps, local/regional flaps, latissimus dorsi miniflap and partial breast amputation. It is important to decrease barriers to oncoplastic surgery if we want to increase the use of EO and BCS rates.
Oncoplastic surgery (OS) allows for higher levels of care in breast-conserving surgery (BCS). BCS was initially advised for the treatment of tumours up to 3–5 cm with a favourable breast/tumour ratio, being deemed safe and having an acceptable recurrence rate (1, 2). OS associated with BCS evolved from breast remodelling (3, 4), causing a loss of 20–50% of the breast parenchyma, to the mammoplasty and mastopexy techniques, which was classified as a type II procedure for the above tumours (5, 6). OS was later used for tumours up to 5 cm or multicentric/multifocal tumours, in which case it was designated extreme oncoplasty (EO) (7).
EO is a group of new BCS techniques for patients who are initial candidates for mastectomy. This new paradigm for BCS includes diverse techniques. Recently, a systematic review article described geometric compensation (GC)/split reduction based on Wise pattern (WP) mammoplasty, but it only reviewed one technique that fell under EO (8), noting the improvement of the initial indications. We aimed to review the EO concepts in more detail to summarize the state of the art and propose future directions.
A review was conducted to evaluate the indications and surgeries performed in the context of EO. We used the PICO system for article evaluation: Problem = breast neoplasm; Intervention =EO; Comparison = all; Outcome = indication and type of surgery. We also considered OS and reconstructive surgical procedures to find associated surgeries related to EO.
Based on the concept of EO with resection for tumours larger than 5 cm or multicentric/multifocal tumours, and referring to previous publications, we based our search strategy on the following search terms: extreme oncoplasty, geometric compensation, regional flaps and mammaplasty. A review was performed by screening two databases (PubMed and LILACS). To evaluate articles in PubMed, we used the following terms: (((“breast neoplasms”[Mesh]) AND (“surgery, plastic”[Mesh] OR “plastic surgery procedures”[Mesh] OR “mammaplasty”[Mesh] OR “mastectomy, segmental”[Mesh])) AND (“oncoplastic surgery” OR “oncoplasty” OR “oncoplastic” OR “extreme oncoplasty” OR “extreme oncoplastic” OR “regional flaps” OR “geometric compensation”)). The terms used in LILACS were “neoplasias da mama” and “ procedimentos cirúrgicos reconstrutivos”; “neoplasias da mama” and “ cirurgia oncoplastica ou oncoplastia.” The deadline for article publication was 12/31/2022. There was no language restriction. Two authors (RACV, I-OJr) performed the revision and jointly evaluated the full articles selected. Each article selected was evaluated based on the type of study, its main endpoints (Table 1; Supplementary Table 1) and indications related to EO (Table 2). Based on main endpoints we group variables to be considered in future studies (Supplementary Table 2). The quality of the studies was evaluated using the MINORS instrument (24) (Supplementary Table 3) and NOS (Newcastle-Ottawa Scale) instrument (25) (Supplementary Table 4).
Initially, 806 articles were identified from the PubMed database and 2 articles from LILACS. All articles identified and selected were in English. The titles and abstracts were evaluated, and 140 articles were selected for reading. After content evaluation, 46 articles were selected for this study. For EO specifically, 23 original articles and four comments were evaluated. Supplementary Figure 1 shows the PRISMA flowchart.
Silverstein suggested the term “EO” and the articles selected here (7, 10, 11). Paulinelli considered the term “GC using WP resection” (9, 16), and similar articles were selected based on modified techniques (22), case descriptions (26–28), and one institutional casuistic with systematic reviews (8). We found articles related to preoperative care (15, 20, 29–31), traditional indications (13, 17), multicentric/multifocal tumours (14, 23), increased indications (8, 13, 19, 21), casuistic (14, 17), and case reports (27, 32, 33). Quality of life (12, 14) was also evaluated. In addition, four replies were found (29–31, 34).
Evaluating the quality of the studies MINORS (Supplementary Table 3) score range of 12 to 19 points, and NOS (Newcastle-Ottawa Scale) evaluation (Supplementary Table 4) range of 3 to 7 stars. Most studies are retrospective. The best methodological study was a matched case-control study comparing EO with mastectomy (23). Four case−control studies, evaluated level II oncoplastic procedures (10, 12, 23), the indications and surgeries were different and one study performed matched evaluation (23) and one compare volume replacement with latissimus dorsi flaps (15). Of the case-control studies, the comparisons patients who underwent OE or not (10, 12, 23). Two studies present a retrospective component and prospective collection of information such as cosmesis assessment photos (8) and quality of life questionnaires (14). Two studies are prospective, showing the geometric compensation technique and its variation (9, 22). In most studies, follow-up time was short, limiting the assessment of local recurrence. Follow-up is stated in a generic way, without description related to patients’ loss of follow-up, being considered positive in studies with cosmesis and with quality outcomes.
EO was associated with higher tumour size, higher specimen weight, narrower margins, and possible conversion to mastectomy, without increasing the recurrence rate. Of the seven observational studies (8, 9, 13, 14, 16, 17, 22), four used the geometric compensation technique or its modification (8, 9, 16, 22). The main endpoint was related to indications, postoperative complications and cosmesis. Table 1 summarizes the main published results related to EO. Supplementary Table 1 shows the main results related to the studies.
Retrospective cohort studies maintained the indications for EO (13, 14, 17), showing that it is a safe procedure for large tumours (> 5 cm), multicentric tumours, and multifocal tumours with acceptable complication rates (7.7% to 28%) (8, 9, 13, 14, 17) and low recurrence rates at a follow-up of > 5 years (6% to 9%) (12, 17). Some studies mentioned breast sized/tumour size ratio or resection size to breast size ratio (35, 36), which can be used for small- and medium-sized breasts, using regional tissue transfer with local/regional flaps (18, 35–37). We also observed new options, such as regional flaps (38–47), partial breast amputation (48–51), and flap guides for central tumours (52). It is important to accept and include these new indications in the spectrum of EO. With this in mind, Table 2 summarizes all possible indications, and Figures 1 and 2 show the indication flowchart.
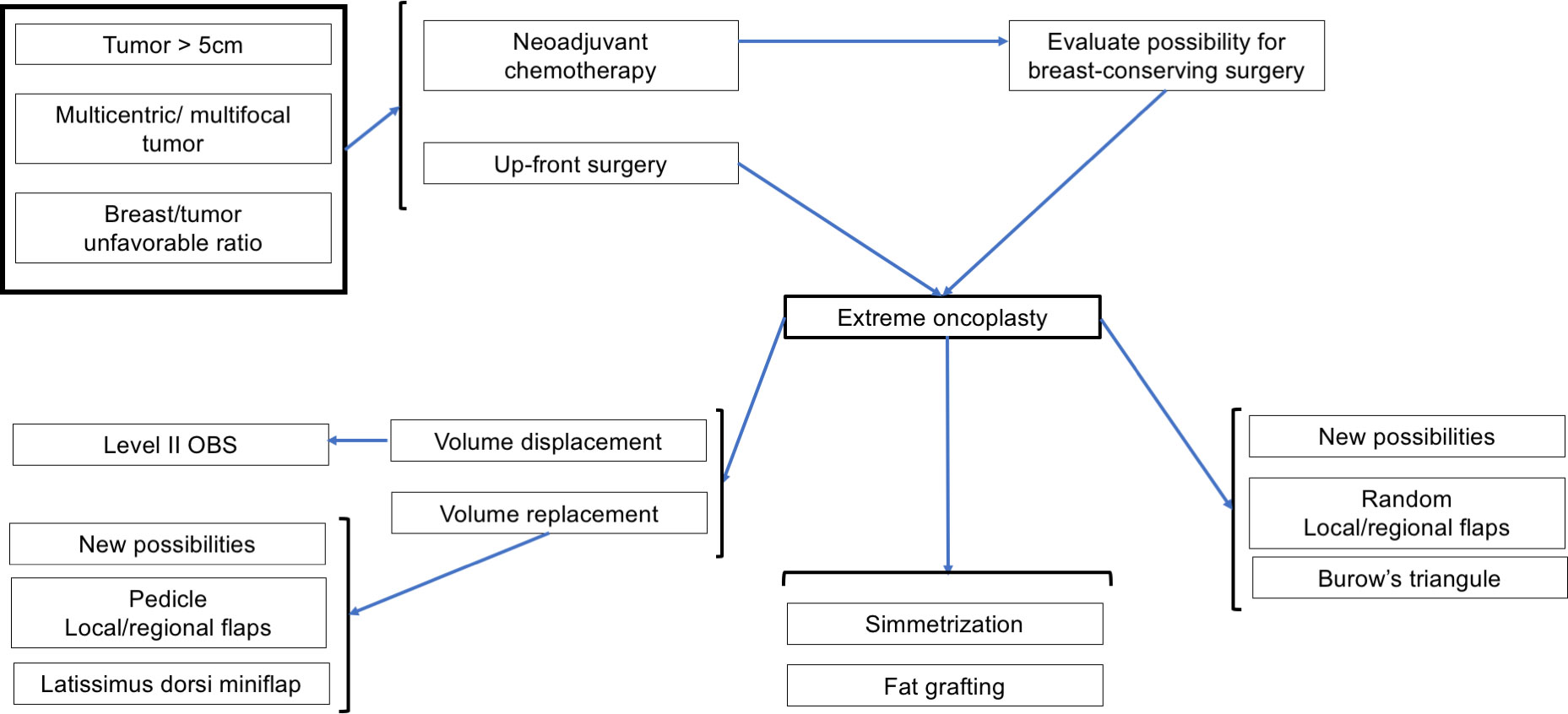
Figure 1 Indications flow associated with Extreme Oncoplasty and associated surgeries. NCT, neoadjuvant chemotherapy.
The re-excision rate of EO is acceptable (0–12.5%) (7, 8, 12, 14, 15, 17). It was high (37.8%) in a study in which 73.9% of patients had multifocal/multicentric disease (13). The rate of conversion to mastectomy ranges from 0% to 13.5% (8, 13, 14, 34). One study reported 21% and 3% of mastectomy when EO was associated with traditional mammoplasty or latissimus dorsi, respectively (34).
The studies reported different follow-up, which were generally short and approximately 12 (14, 22), 24 (9, 10), and 36 months (8, 13, 16). Four studies had a follow-up higher than 60 months (12, 15, 17, 23).The recurrences were described as locoregional or local recurrences. Although limited follow up, local recurrence reported is lower than 3.5% (14/413 patients). The rate of breast symmetrisation is variable (48–100%) (10, 13, 17), and although it is not part of EO, it allows us to evaluate symmetry and cosmesis. All studies have shown that EO is a safe procedure (7, 12) with acceptable cosmetic results (8, 9, 16).
OS is associated with high satisfaction with the breasts (78%–83.5%) (8, 9, 12, 16, 22) and seems to improve the quality of life (12, 14, 22). Three studies evaluated quality of life using the Breast-Q questionnaire. One, a case series (n=39), reported high (>75%) satisfaction with the breast, outcomes, psychosocial well-being, and sexual well-being (14). The second study reported high scores associated with satisfaction with outcome and satisfaction with breasts (22). The third was a case−control study, which evaluated BCS (n=171) versus OE (n=33) and observed superior scores for OE in the outcome, satisfaction with the nipple complex, and psychological well-being (12).
In 2014, Silverstein et al. (7) presented a new paradigm for OS, putting forth the concept of EO (10). Sixty-six potential candidates for a mastectomy with an unfavourable breast/tumour ratio due to the presence of tumours larger than 5 cm and/or multicentric/multifocal tumours (10) were subjected to standard WP reduction or split reduction procedures and immediate contralateral surgery to achieve symmetry (10). In the same year (2014), another publication showed, through mammaplasty techniques, the achievement of BCS in 17 cases of advanced tumours using the modified WP, called GC (9). This technique emphasizes breast preservation in situations when a breast-versus-tumour relationship is unfavourable for BCS. The skin is resected over the tumour, but using a modification of the standard WP and constituting an EO, which shows satisfactory cosmetic results (9, 28). The procedure is also performed for unicentric tumours < 5 cm with resection of the skin over the tumour, valuing other indications for EO (9), which was also evidenced in a larger series that used split reduction (16). A recent case series with systematic review refined the indications, considering the breast-size ratio, and it showed results associated with small and medium breasts (8). Since the objective of this study was to evaluate the indications, techniques and main results associated with EO, we opted to separately discuss all aspects related to EO, performing an integrative review.
EO is not for beginners (31). For OS, it is necessary to plan, perform clinical and imaging evaluations, and have surgical training (30, 34). Clinical evaluation, preoperative radiological evaluation, intraoperative frozen section margins, intraoperative specimen radiography, and clipped cavity margins are helpful for patient selection and operative evaluation (29, 31). Only one publication has considered the importance of breast nuclear magnetic resonance for surgical planning in the presence of multifocal/multicentric lesions (20).
The EO definition is extended to candidates for mastectomy who underwent BCS (14, 30), including patients with extensive ductal in situ, previously irradiated breast, locally advanced breast carcinoma with limited or partial imaging response to neoadjuvant chemotherapy, past excision biopsy with inappropriate scarring (14), extensive microcalcifications, and an unfavourable tumour/breast volume ratio (8, 21).
With the wide knowledge and dissemination of EO, it is necessary to review potential techniques and group them to facilitate decision-making regarding the indications, surgical possibilities, technical training, and associated complications (8, 18). GC (9) is a technical modification of the initially described procedure (22). An exceptional example of such a literature review was recently published that evaluated patients undergoing GC and WP and examined 243 patients previously described to have undergone this procedure (8). In that review (8), 36 patients were included. The indication for GC was extended to single tumours of smaller size and medium-to-small breasts, provided that they presented with ptosis and that EO was possible in tumours with an unfavourable breast/tumour ratio, valuing the indication for EO in tumours smaller than 5 cm.
When evaluation studies about EO, we have to review the level of oncoplastic surgery. Urban (53) considered three levels of Oncoplasty and EO would be considered for Level II procedures. Clough et al. (3) considered two levels and EO would be considered for Level II: extensive resections, requiring mammoplasty techniques, representing 20-50% of the breast/volume ratio. In 2019, the American Society of Breast Surgeons (6) began to use the term volume displacement and volume replacement. Volume displacement techniques are Level I (< 20%) and Level II techniques (20-50%), and volume replacement (>50%) are local/regional flap reconstruction, miocutaneous flaps and implants. Among the procedures performed for EO, most used WP reduction mastoplasty (8, 9, 17), followed by mastopexy and racquet mammoplasty (13), which is associated with Level II OS procedures associated with volume displacement (6). We have to add volume replacement techniques to arsenal of options related to EO (Figures 1, 2). After reviewing the concept of extensive resection associated with BCS, we found that other techniques could be included, such as pedicled flaps (17) and flaps with lateral thoracic perforators (19). One study compared traditional EO with latissimus dorsi (LD) miniflap (15), with lower complications and higher revision related to LD but no impact on local recurrence.
The EO concept extends the original technique to the use of locoregional flaps (37) and other techniques where extensive resections would lead to loss of cosmetic results (54), while OS allows safe resection with acceptable results. New possibilities for EO are random flaps (55), pedicled flaps (38), latissimus dorsi miniflaps (12, 39), and partial breast amputation (48–51). The techniques are associated with volume replacement (37) for small-to-moderate-sized breasts. For example, of random flaps, we have thoraco-epigastric flap, thoracic-lateral flap, bilobed flap and Burow’s triangle (55), but they can be used in lower resections. Older techniques used before the emergence of OS should not be forgotten. They are usually performed in a nonstandard way for patients in whom preservation of the breast is desired and cosmesis is not the primary endpoint. These techniques are locoregional flaps (37, 38, 40–47, 52, 55) and nonpedicled flaps, such as thoracoepigastric, thoracic-lateral, and bilobed flaps (55). It is necessary to accept and group these new techniques, allowing other reviews in the future.
Articles have shown images of voluminous breasts (7–10, 16, 19, 32) and medium-sized breasts (7, 8) subjected to EO. Hence, we must use techniques such as mammoplasty WP, GC (8, 9, 16, 22), and other mammoplasty techniques (13, 17). Some techniques are associated with volume replacement for small- to moderate-sized breasts (37). The presence of a small-to-moderate-sized nonptotic breast presenting centrally located breast cancer was initially considered a limitation, but perforator flaps are useful in this condition (19).
All patients who are candidates for EO should be aware of the possibility of conversion to mastectomy (8), and skin-preserving mastectomy may eventually be an option. This requires prior reservation of a breast prosthesis if BCS with OS is not safe during surgery based on the tumour margins of breast cosmesis.
Symmetrisation has an unknown impact on quality of life (56) since patients evaluate their cosmesis better than health professionals (57). Another option that can be used after extensive resection associated with BCS is immediate autologous fat grafting (58), which can improve patient selection for EO.
We try to evaluate the quality of the studies, but there was no randomized study and RoB 2.0 assess risk of bias was not performed, and for observational studies we used MINORS (Supplementary Table 3) and NOS scores (Supplementary Table 4). The major problem observed was too little description of the control group and short follow up in some studies. Although scores are low these studies are important to show the importance of EO. As it is an innovation, the follow up is low and we need more time to evaluate local recurrence. There is a lack of a paired matched case-control study, and new studies need to be performed, comparing EO, oncoplastic surgery and simple breast-conserving surgery. Locorregional recurrence would not be an endpoint but local recurrence. The future authors must take care reporting adequate follow up, loss of patient and local disease-free recurrence.
EO arose due to the need for breast preservation in cases that were difficult to resolve. This fact makes it impossible to carry out prospective randomized studies. It is unethical to perform a mastectomy when breast-conserving treatment can be performed. It limits the quality of the studies (Supplementary Table 3). Therefore, we must improve the literature (59), seeking to report the main metrics reported in previous studies (Supplementary Table 2), aiming to standardize information. Future studies determine the complexity of performing different procedures, reporting the experience of training centres in oncoplasty, and evaluating the learning curve, mastectomy conversion rate, complications, re-excision rate, local recurrence, patient satisfaction, and cosmetic results of different techniques. Also, it is necessary to perform matched case-control studies, with a long follow-up period.
EO implies developing clinical training to select cases, technical knowledge to evaluate different oncoplastic solutions, a fact that denotes a long learning curve. It is important to decrease barriers to OS (60) if we want to increase the use of EO. When performing OS, it is important to report the indications, type of surgeries (61, 62), postoperative endpoints and long term results (Supplementary Table 2). The EO qualifies the service and should be one of the parameters to be used in the quality assessment of breast centres.
Reflections and discussions of published articles (29, 30, 34) are important, but systematic reviews (8) are essential. Since the definition of EO (7, 11), the literature has evolved in indications, and this review considers the new technical possibilities (Table 2). Future systematic reviews evaluating the different techniques will facilitate a better understanding of the multiple technical availabilities and results, helping surgical oncologists choose the right procedure for BCS from the multiple techniques of EO.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
RV: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. IdO-J: Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. RP: Methodology, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was receive fot the publication of this article. The “Barretos Cancer Hospital” provided funding for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1215284/full#supplementary-material
1. Carrara GF, Scapulatempo-Neto C, Abrahao-MaChado LF, Brentani MM, Nunes JS, Folgueira MA, et al. Breast-conserving surgery in locally advanced breast cancer submitted to neoadjuvant chemotherapy. Safety and effectiveness based on ipsilateral breast tumor recurrence and long-term follow-up. Clinics (Sao Paulo) (2017) 72(3):134–42. doi: 10.6061/clinics/2017(03)02
2. Santos G, Urban C, Edelweiss MI, Zucca-Matthes G, de Oliveira VM, Arana GH, et al. Long-term comparison of aesthetical outcomes after oncoplastic surgery and lumpectomy in breast cancer patients. Ann Surg Oncol (2015) 22(8):2500–8. doi: 10.1245/s10434-014-4301-6
3. Clough KB, Ihrai T, Oden S, Kaufman G, Massey E, Nos C. Oncoplastic surgery for breast cancer based on tumour location and a quadrant-per-quadrant atlas. Br J Surg (2012) 99(10):1389–95. doi: 10.1002/bjs.8877
4. Gainer SM, Lucci A. Oncoplastics: techniques for reconstruction of partial breast defects based on tumor location. J Surg Oncol (2011) 103(4):341–7. doi: 10.1002/jso.21672
5. Clough KB, Kaufman GJ, Nos C, Buccimazza I, Sarfati IM. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol (2010) 17(5):1375–91. doi: 10.1245/s10434-009-0792-y
6. Chatterjee A, Gass J, Patel K, Holmes D, Kopkash K, Peiris L, et al. A consensus definition and classification system of oncoplastic surgery developed by the american society of breast surgeons. Ann Surg Oncol (2019) 26(11):3436–44. doi: 10.1245/s10434-019-07345-4
7. Silverstein MJ, Mai T, Savalia N, Vaince F, Guerra L. Oncoplastic breast conservation surgery: the new paradigm. J Surg Oncol (2014) 110(1):82–9. doi: 10.1002/jso.23641
8. Franca FC, de Oliveira-Junior I, Morgan AM, Haikel RL, da Costa Vieira RA. Breast-conserving surgery with the geometric compensation/split reduction technique. Indications, oncologic safety and cosmesis. A cohort series and systematic review of the literature. Surg Oncol (2022) 44:101839. doi: 10.1016/j.suronc.2022.101839
9. Paulinelli RR, de Oliveira VM, Bagnoli F, Chade MC, Alves KL, Freitas-Junior R. Oncoplastic mammaplasty with geometric compensation–a technique for breast conservation. J Surg Oncol (2014) 110(8):912–8. doi: 10.1002/jso.23751
10. Silverstein MJ, Savalia N, Khan S, Ryan J. Extreme oncoplasty: breast conservation for patients who need mastectomy. Breast J (2015) 21(1):52–9. doi: 10.1111/tbj.12356
11. Silverstein MJ. Radical mastectomy to radical conservation (Extreme oncoplasty): A revolutionary change. J Am Coll Surg (2016) 222(1):1–9. doi: 10.1016/j.jamcollsurg.2015.10.007
12. Acea Nebril B, Garcia Novoa A, Polidorio N, Cereijo Garea C, Bouzon Alejandro A, Mosquera Oses J. Extreme oncoplasty: The last opportunity for breast conservation-Analysis of its impact on survival and quality of life. Breast J (2019) 25(3):535–6. doi: 10.1111/tbj.13267
13. Crown A, Laskin R, Rocha FG, Grumley J. Extreme oncoplasty: Expanding indications for breast conservation. Am J Surg (2019) 217(5):851–6. doi: 10.1016/j.amjsurg.2019.01.004
14. Koppiker CB, Noor AU, Dixit S, Busheri L, Sharan G, Dhar U, et al. Extreme oncoplastic surgery for multifocal/multicentric and locally advanced breast cancer. Int J Breast Cancer (2019) 2019:4262589. doi: 10.1155/2019/4262589
15. Pearce BCS, Fiddes RN, Paramanathan N, Chand N, Laws SAM, Rainsbury RM. Extreme oncoplastic conservation is a safe new alternative to mastectomy. Eur J Surg Oncol (2020) 46(1):71–6. doi: 10.1016/j.ejso.2019.09.004
16. Paulinelli RR, de Oliveira VM, Bagnoli F, Letzkus Berrios J, Cezar Chade M, Bragatto Picoli L, et al. Oncoplastic mammaplasty with geometric compensation: Evolution of the technique, outcomes and follow-up in a multicentre retrospective cohort. J Surg Oncol (2020) 121(6):967–74. doi: 10.1002/jso.25860
17. Savioli F, Seth S, Morrow E, Doughty J, Stallard S, Malyon A, et al. Extreme oncoplasty: breast conservation in patients with large, multifocal, and multicentric breast cancer. Breast Cancer (Dove Med Press) (2021) 13:353–9. doi: 10.2147/BCTT.S296242
18. Alder L, Zaidi M, Zeidan B, Mazari F. Advanced breast conservation and partial breast reconstruction - a review of current available options for oncoplastic breast surgery. Ann R Coll Surg Engl (2022) 104(5):319–23. doi: 10.1308/rcsann.2021.0169
19. Nigam S, Eichholz A, Bhattacharyya M, Parulekar V, Roy PG. Extreme oncoplasty for centrally located breast cancer in small non-ptotic breasts: extending the indications of chest wall perforator flaps with areolar reconstruction. Ecancermedicalscience (2021) 15:1311. doi: 10.3332/ecancer.2021.1311
20. Joukainen S, Okuma H, Kaarela O, Laaksonen E, Karja V, Vanninen R, et al. Can supine breast magnetic resonance imaging help hit the target in extreme oncoplastic surgery? Eur J Surg Oncol (2021) 47(11):2788–96. doi: 10.1016/j.ejso.2021.07.027
21. Cakmak GK. Innovative standards in oncoplastic breast conserving surgery: from radical mastectomy to extreme oncoplasty. Breast Care (Basel) (2021) 16(6):559–73. doi: 10.1159/000518992
22. Paulinelli RR, Ribeiro LFJ, Santos TD, Caires EMS, Pontes MGM, Faria BM, et al. Oncoplastic Mammoplasty with disguised geometric compensation. Surg Oncol (2021) 39:101660. doi: 10.1016/j.suronc.2021.101660
23. De Lorenzi F, Borelli F, Pagan E, Bagnardi V, Peradze N, Jereczek-Fossa BA, et al. Oncoplastic breast-conserving surgery for synchronous multicentric and multifocal tumors: is it oncologically safe? A retrospective matched-cohort analysis. Ann Surg Oncol (2022) 29(1):427–36. doi: 10.1245/s10434-021-10800-w
24. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg (2003) 73(9):712–6. doi: 10.1046/j.1445-2197.2003.02748.x
25. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses: The Ottawa Hospital Research Institute (2009). Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.htm.
26. Marongiu F, Bertozzi N, Sibilio A, Gasperoni M, Curcio A. "Bifidus pedicle", the use of bilobed superomedial pedicle for breast reshaping following upper outer quadrantectomy: A new oncoplastic breast surgery technique. Aesthetic Plast Surg (2021) 45(3):866–74. doi: 10.1007/s00266-020-01982-x
27. Mele S, Falco G, Borgonovo G, Castagnetti F, Cenini E, Coiro S, et al. Bifurcate inferior pedicle mammoplasty in large ptotic breast for tumor located at the upper outer quadrant with skin involvement-a novel technique allowing good cosmetic outcome: case report. Gland Surg (2020) 9(5):1590–5. doi: 10.21037/gs-20-349
28. Paulinelli RR, Marinho ER. Double independent pedicle oncoplastic mammaplasty: a technique for breast preservation. Rev Bras Mastol (2012) 22(1):25–32.
29. Franceschini G, Di Leone A, Masetti R. Comment on "Extreme oncoplastic surgery for multifocal/multicentric and locally advanced breast cancer". Int J Breast Cancer (2019) 2019:4693794. doi: 10.1155/2019/4693794
30. Franceschini G, Masetti R. Extreme oncoplastic breast conserving surgery: Is surgical dexterity all that is need? Am J Surg (2020) 219(1):211–2. doi: 10.1016/j.amjsurg.2019.04.008
31. Franceschini G, Masetti R. Evidence-based surgery to realize a successful extreme oncoplastic breast conservation. Eur J Surg Oncol (2020) 46(5):924–5. doi: 10.1016/j.ejso.2020.02.003
32. Bordoni D, Cadenelli P, Falco G, Rocco N, Manna P, Tessone A, et al. Extreme oncoplastic breast surgery: A case report. Int J Surg Case Rep (2016) 28:182–7. doi: 10.1016/j.ijscr.2016.09.037
33. Giacaman N, Abu Al-Halawa D, Tos SM, Ibdah MG, Sharaf K. Extreme Oncoplastic Breast Surgery: A case series of three patients from a lower-middle income country. Ann Med Surg (Lond) (2022) 84:104899. doi: 10.1016/j.amsu.2022.104899
34. Pearce BCS, Fiddes RN, Paramanathan N, Chand N, Laws SAM, Rainsbury RM. Reply to: Evidence-based surgery to realize a successful extreme oncoplastic breast conservation. Eur J Surg Oncol (2020) 46(5):926–7. doi: 10.1016/j.ejso.2020.02.004
35. Losken A, Chatterjee A. Improving results in oncoplastic surgery. Plast Reconstr Surg (2021) 147(1):123e–34e. doi: 10.1097/PRS.0000000000007478
36. Salibian AA, Olson B, Shauly O, Patel KM. Oncoplastic breast reconstruction: Principles, current techniques, and future directions. J Surg Oncol (2022) 126(3):450–9. doi: 10.1002/jso.26897
37. Yang JD, Lee JW, Cho YK, Kim WW, Hwang SO, Jung JH, et al. Surgical techniques for personalized oncoplastic surgery in breast cancer patients with small- to moderate-sized breasts (part 2): volume replacement. J Breast Cancer (2012) 15(1):7–14. doi: 10.4048/jbc.2012.15.1.7
38. Schaverien MV, Kuerer HM, Caudle AS, Smith BD, Hwang RF, Robb GL. Outcomes of volume replacement oncoplastic breast-conserving surgery using chest wall perforator flaps: comparison with volume displacement oncoplastic surgery and total breast reconstruction. Plast Reconstr Surg (2020) 146(1):14–27. doi: 10.1097/PRS.0000000000006911
39. Abdelrahman EM, Nawar AM, Balbaa MA, Shoulah AA, Shora AA, Kharoub MS. Oncoplastic volume replacement for breast cancer: latissimus dorsi flap versus thoracodorsal artery perforator flap. Plast Reconstr Surg Glob Open (2019) 7(10):e2476. doi: 10.1097/GOX.0000000000002476
40. Lee J, Bae Y, Audretsch W. Combination of two local flaps for large defects after breast conserving surgery. Breast (2012) 21(2):194–8. doi: 10.1016/j.breast.2011.09.011
41. Schoeller T, Bauer T, Haug M, Otto A, Wechselberger G, Piza-Katzer H. A new contralateral split-breast flap for breast reconstruction and its salvage after complication: an alternative for select patients. Ann Plast Surg (2001) 47(4):442–5. doi: 10.1097/00000637-200110000-00015
42. Kijima Y, Yoshinaka H, Hirata M, Nakajo A, Arima H, Okumura H, et al. Oncoplastic breast surgery combining partial mastectomy with immediate breast reshaping using a keyhole-shaped skin glandular flap for Paget's disease. Surg Today (2014) 44(9):1783–8. doi: 10.1007/s00595-013-0687-1
43. Joshi S, Jaiswal D, Chougle Q, Wadasadawala T, Badwe RA. Transposition flap for the oncoplastic reconstruction of outer quadrant breast defects. J Plast Reconstr Aesthet Surg (2021) 74(9):2176–83. doi: 10.1016/j.bjps.2020.12.037
44. Hirata M, Toda H, Higo N, Shinden Y, Ohtsuka T, Kijima Y. Modification of oncoplastic breast surgery with immediate volume replacement using a thoracodorsal adipofascial flap. Breast Cancer (2022) 29(3):531–40. doi: 10.1007/s12282-022-01331-7
45. Kijima Y, Hirata M, Higo N, Toda H, Shinden Y. Oncoplastic breast surgery combining partial mastectomy with resection of double equilateral triangular skin flaps. Surg Today (2022) 52(3):514–8. doi: 10.1007/s00595-021-02355-w
46. Hong S, Wang S, Liu J, Qiang Z, Zheng X, Chen G. Usefulness of lateral thoracic adipofascial flaps after breast-conserving surgery in small-to moderate-sized breasts. Clin Breast Cancer (2019) 19(5):370–6. doi: 10.1016/j.clbc.2019.04.009
47. Kollias V, Kollias J. Safety and efficacy of anterior intercostal artery perforator flaps in oncoplastic breast reconstruction. ANZ J Surg (2022) 92(5):1184–9. doi: 10.1111/ans.17496
48. Kijima Y, Yoshinaka H, Hirata M, Mizoguchi T, Ishigami S, Arima H, et al. Oncoplastic surgery combining partial mastectomy with breast reconstruction using a free nipple-areola graft for ductal carcinoma in situ in a ptotic breast: report of a case. Surg Today (2011) 41(3):390–5. doi: 10.1007/s00595-010-4294-0
49. Kijima Y, Yoshinaka H, Hirata M, Shinden Y, Nakajo A, Arima H, et al. Therapeutic mammoplasty combining partial mastectomy with nipple-areola grafting for patients with early breast cancer: a case series. Surg Today (2016) 46(10):1187–95. doi: 10.1007/s00595-015-1294-0
50. Manie TM, Youssef M, Taha SN, Rabea A, Farahat AM. Batwing mammoplasty: a safe oncoplastic technique for breast conservation in breast cancer patients with gigantomastia. Ann R Coll Surg Engl (2020) 102(2):115–9. doi: 10.1308/rcsann.2019.0129
51. Mattioli WM, Penazzi-Júnior SA, de Melo DSF. Use of the back-folded dermaglandular inferior pedicle in mammary amputation: improving results. Rev Bras Cir Plast (2017) 32(3):340–5. doi: 10.5935/2177-1235.2017RBCP0057
52. Carstensen L, Bigaard J. Management of central breast tumours with immediate reconstruction of the nipple-areola complex; a suggested guide. Breast (2015) 24(1):38–45. doi: 10.1016/j.breast.2014.11.002
53. Urban C, Gazoto-Junior O, Pires DM, Garcia GN, Paulinelli RR, Amoroso V, et al. Trends and attitues toward oncoplastics training in Mastology in Brazil. Mastology (2017) 27(3):182–6. doi: 10.5327/Z2594539420170000221
54. Winters ZE, Bernaudo L. Evaluating the current evidence to support therapeutic mammoplasty or breast-conserving surgery as an alternative to mastectomy in the treatment of multifocal and multicentric breast cancers. Gland Surg (2018) 7(6):525–35. doi: 10.21037/gs.2018.07.01
55. Paulinelli RR, Luz MV, Faria BM, Ribeiro FJR. Oncoplastia e cirurgia conservadora: Retalhos locorregionais. In: Boff RA, Brenelli FP, Almeida NR, editors. Compêndio de mastologia abordagem multidisciplinar, 2nd ed. São Paulo: Lemar & Goi (2022). p. 1061–70.
56. de Oliveira-Junior I, da Silva IA, da Silva FCB, da Silva JJ, Sarri AJ, Paiva CE, et al. Oncoplastic surgery in breast-conserving treatment: patient profile and impact on quality of life. Breast Care (Basel) (2021) 16(3):243–53. doi: 10.1159/000507240
57. de Oliveira-Junior I, Brandini da Silva FC, Nazima F, Ribeiro JC Jr., Castellani L, Zucca-Matthes G, et al. Oncoplastic surgery: does patient and medical specialty influences the evaluation of cosmetic results? Clin Breast Cancer (2021) 21(3):247–55 e3. doi: 10.1016/j.clbc.2020.09.012
58. Biazus JV, Stumpf CC, Melo MP, Zucatto AE, Cericatto R, Cavalheiro JA, et al. Breast-conserving surgery with immediate autologous fat grafting reconstruction: oncologic outcomes. Aesthetic Plast Surg (2018) 42(5):1195–201. doi: 10.1007/s00266-018-1155-5
59. de Oliveira-Junior I, Haikel RL, Vieira RAC. Breast-conserving treatment in oncoplastic times: indications, cosmesis, and quality of life. Mastology (2021) 31:e20200040. doi: 10.29289/2594539420200040
60. Chatterjee A, Gass J, Burke MB, Kopkash K, El-Tamer MB, Holmes DR, et al. Results from the American society of breast surgeons oncoplastic surgery committee 2017 survey: current practice and future directions. Ann Surg Oncol (2018) 25(10):2790–4. doi: 10.1245/s10434-018-6586-3
61. Emiroglu M, Sert I, Karaali C, Aksoy SO, Ugurlu L, Aydin C. The effectiveness of simultaneous oncoplastic breast surgery in patients with locally advanced breast cancer. Breast Cancer (2016) 23(3):463–70. doi: 10.1007/s12282-015-0585-z
62. Araujo Pereira Lisboa FC, Paulinelli RR, Campos Veras LP, Jube Ribeiro LF, Padua Oliveira LF, Sousa Rahal RM, et al. Aesthetic results were more satisfactory after oncoplastic surgery than after total breast reconstruction according to patients and surgeons. Breast (2023) 71:47–53. doi: 10.1016/j.breast.2023.07.006
Keywords: breast neoplasms, oncoplastic surgery, extreme oncoplasty, breast conserving therapy, surgical procedures, surgical flaps
Citation: Vieira RAdC, Paulinelli RR and de Oliveira-Junior I (2024) Extreme oncoplasty: past, present and future. Front. Oncol. 13:1215284. doi: 10.3389/fonc.2023.1215284
Received: 01 May 2023; Accepted: 08 November 2023;
Published: 30 January 2024.
Edited by:
Mangesh A. Thorat, Guy’s and St Thomas’ NHS Foundation Trust, United KingdomReviewed by:
Nidhi Garg, Guy’s and St Thomas’ NHS Foundation Trust, United KingdomCopyright © 2024 Vieira, Paulinelli and de Oliveira-Junior. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: René Aloisio da Costa Vieira, cmVuZWFjdkBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.