
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Oncol. , 27 March 2023
Sec. Cancer Imaging and Image-directed Interventions
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1098594
Introduction: Extracorporeal membrane oxygenation (ECMO) is widely used during refractory cardiac or respiratory failure, and some case reports described ECMO utilization in critical airway interventional therapy.
Methods: Eligible reports about patients receiving airway interventional therapy under ECMO were retrieved from Web of Science, Embase, Medline, and Cochrane databases up to 1 August 2022.
Results: Forty-eight publications including 107 patients who underwent ECMO for critical airway problems met the inclusion criteria. The critical airway problem that was reported the most was tumor-associated airway obstruction (n = 66, 61.7%). The second most reported etiology was postoperative airway collapse or stenosis (n = 19, 17.8%). The main interventional therapies applied were airway stent placement or removal (n = 61, 57.0%), mass removal (n = 22, 20.6%), and endotracheal intubation (n = 12, 11.2%) by bronchoscopy. The median ECMO duration was 39.5 hours. Eleven patients had ECMO-associated complications, including seven cases of airway hemorrhage, one case of arteriovenous fistula, one case of vein rupture and hematoma, one case of foot ischemia, and one case of neuropraxia of the cannulation site. In total, 91.6% of the patients survived and were discharged from the hospital.
Conclusion: ECMO appears to be a viable form of life support for patients undergoing interventional therapy for critical airway problems.
Critical airway problems include airway obstruction, massive airway hemorrhage, and acute tracheal or bronchial lesions, which may lead to severe hypoxia or death. Airway obstruction is the leading cause of critical airway problems. Respiratory interventional therapies, including airway stent placement and mass removal by bronchoscopy, are effective in treating airway problems (1, 2). Most of these procedures can be safely and successfully performed using various ventilation techniques (3). However, interventional therapy can be particularly dangerous and cause hypoxemia in patients with critical airway problems such as near-total airway obstruction.
Extracorporeal membrane oxygenation (ECMO) has become an important intervention for patients with severe cardiac or pulmonary dysfunction for whom conventional therapies fail (4). The expanded utilization of ECMO in non-traditional indications, such as upper airway surgery and malignant airway obstruction, has been reported in some studies. Critical airway problems indicate that ECMO prevents or overcomes deadly hypoxemia and hypercapnia. This review summarizes the reports on the combination of ECMO and airway interventional therapy for critical airway problems.
We searched the Cochrane, Web of Science, Medline, and Embase databases for studies using the terms “{[extracorporeal membrane oxygenation (Title/Abstract)] OR [extracorporeal life support (Title/Abstract)]} AND {[airway (Title/Abstract)] OR [trachea (Title/Abstract)] OR [bronchial (Title/Abstract)]}”. We searched for reports from database inception until 1 August 2022. We also retrieved the references and keywords of all included studies to reduce bias. The results were according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. This study was registered with PROSPERO (No. CRD42022367887).
The inclusion criteria were as follows: 1) randomized controlled trials, single-arm cohort studies, or case reports; 2) trials conducted in patients with critical airway problems; and 3) trials reporting data on ECMO and interventional therapy. Patients were excluded if they were admitted for other medical problems or if they had been diagnosed with brain death.
Two investigators performed study selection and recorded the reasons for exclusion. A third reviewer was consulted if no consensus was reached.
Two investigators independently extracted and recorded the study’s demographic characteristics and outcomes in a standard form, as recommended by Cochrane. A third investigator resolved any disagreements.
Outcome measures were the underlying etiology of critical airway problems, ECMO-associated complications, anticoagulation therapy, interventional therapy, and in-hospital survival rate.
Data are presented as the median and interquartile range (IQR) or absolute numbers and percentages. Data were analyzed using SPSS version 25.0 (IBM, Armonk, NY, USA).
Forty-eight publications (5–52) including 107 patients who underwent ECMO for critical airway problems met the inclusion criteria. One patient underwent ECMO twice. Details of the study selection process are presented in Figure 1. All reports were case reports or case series. The median age was 57 (IQR 40, 67) years, and men accounted for 61.7% (n = 66) of the patients. Emergent ECMO accounted for 53.3% (n = 57) of the cases. Details of the included studies are presented in Supplementary Tables 1, 2.
Most of the critical airway problems were tumor-associated airway obstructions (n = 66, 61.7%), among which malignant tumor invasion or metastasis and benign tumor occlusion or oppression accounted for 57.0% (n = 61) and 4.7% (n = 5), respectively. The second most reported etiology was postoperative airway collapse or stenosis (n = 19, 17.8%). Congenital or idiopathic airway stenosis (n = 8, 7.5%), foreign body aspiration (n = 7, 6.5%), airway hemorrhage (n = 4, 3.7%), inflammatory disease (n = 4, 3.7%), migration or fracture of airway stent (n = 3, 3.7%), nearly tissue or organ oppression (n = 2, 1.9%), and airway lesions or fistulas (n = 2, 1.9%) were the other indications. Lung cancer (n = 27, 25.2%) was the most common indication of airway obstruction in our review. The details are presented in Table 1.
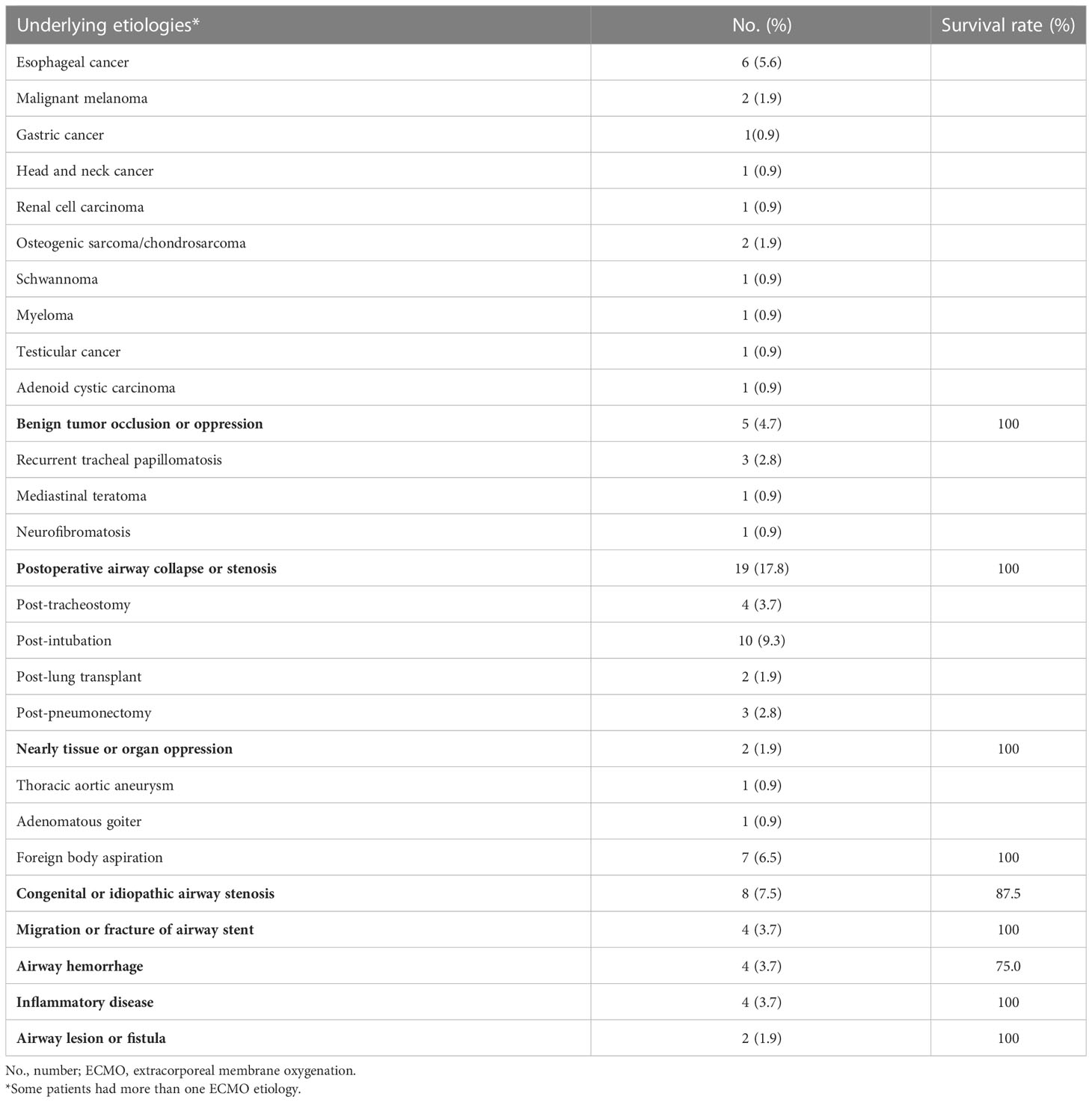
Table 1 Underlying etiologies and survival rate of patients with critical airway problems receiving ECMO.
The main interventional therapies were airway stent placement, replacement, or removal by bronchoscopy (n = 61, 57.0%), mass removal (n = 22, 20.6%), and endotracheal intubation (n = 12, 11.2%) by bronchoscopy. Other therapies included biopsy (n = 6, 5.6%), tracheostomy (n = 5, 4.7%), foreign body extraction (n = 7, 6.5%), laser (n = 4, 3.7%), suction and removal of blood clots (n = 3, 2.8%), balloon dilatation (n = 3, 2.8%), bronchoalveolar lavage (n = 2, 1.9%), endobronchial balloon occlusion and hemostatic therapy (n = 1, 0.9%), cryotherapy (n = 1, 0.9%), and photodynamic therapy (n = 1, 0.9%). Some patients received several adjunctive therapies. The details are presented in Table 2.
In this review, 89 patients who received venovenous-ECMO (VV-ECMO) for refractory hypoxia or hypercapnia were included. In comparison, 18 patients received venoarterial-ECMO (VA-ECMO) for hemodynamic instability or cardiopulmonary resuscitation. The ECMO cannulation sites were as follows: both femoral veins (n = 39), femoral and internal jugular veins (n = 30), femoral vein and artery (n = 12), single cannulation with a double lumen in the internal jugular vein (n = 4), internal jugular vein and artery (n = 1), and not mentioned (n = 21). The median total ECMO duration was 39.5 (IQR 17.4, 100.8) hours. Unfractionated heparin (n = 59) was the most commonly used anticoagulant. In 13 patients, continuous infusion of nafamostat mesylate and heparin was administered to maintain the targeted activated clotting time (ACT). Two patients did not receive anticoagulation therapy because of the high risk of bleeding. ACT was used as a monitor for anticoagulation therapy in most studies. The range of ACT was 130–250 seconds in most studies. Some reports did not record the exact anticoagulation therapy used. Only one patient was not successfully weaned off ECMO for the underlying disease. Eleven patients reported ECMO-associated complications, including seven cases of airway hemorrhage, one case of arteriovenous fistula, one case of vein rupture and hematoma, one case of foot ischemia, and one case of neuropraxia at the cannulation site. One patient died of massive airway bleeding after being weaned off ECMO. The details are presented in Table 3 and Supplementary Table 2.
In total, 91.6% (n = 98) of the patients survived and were discharged from the hospital. Among the nine patients who died, eight died of the underlying disease, and only one died of ECMO-associated massive airway hemorrhage. During the follow-up period of 60 days in 53 patients, seven died due to the progression of the underlying disease. The details are presented in Table 4 and Supplementary Table 1.
In our review, airway obstruction caused by malignant tumors was found to be the primary cause of critical airway problems. Surgical resection and reconstruction may provide the highest probability of definitively managing malignant tumors. However, most patients with malignant airway obstruction cannot undergo surgery for metastatic disease or are in poor physical condition (53). Respiratory interventional therapy in patients with acute severe airway problems provides adequate emergency ventilation, palliation, and airway stabilization, allowing for additional treatments. Bronchoscopy plays a beneficial role in treating patients with malignant airway obstruction (54, 55). However, bleeding may be the most common complication of interventional therapy.
In critically ill patients, interventional airway therapy can be hazardous and cause life-threatening hypoxemia. Additionally, endotracheal intubation for mechanical ventilation may be impossible or even fatal. VV-ECMO is used for treating critical respiratory failure, and VA-ECMO provides both respiratory and cardiac support (56). To date, a series of studies have reported a combination of ECMO and interventional therapy for critical airway problems. However, the available evidence is only based on case reports and case series studies.
This review analyzed published reports on ECMO-assisted respiratory interventional therapy in patients with critical airway problems. VV-ECMO provides adequate oxygenation during surgical or bronchoscopic interventions, and VA-ECMO should be used in high-risk patients with hemodynamic instability (16). Serino et al. reported that lung cancer accounted for 57.1% of patients with malignant airway obstruction (n = 56) and many other cancers through metastasis (57). ECMO for critical airway problems has been initially reported in pediatric populations and has been successfully used in interventional therapy in children for foreign body aspiration (11, 12, 25), congenital tracheal stenosis (6), and endotracheal masses (14). In adults, the first use of ECMO in a patient with sawdust aspiration undergoing foreign body extraction by bronchoscopy was published by Higashi in 1989 (5). For malignant central airway occlusions, airway stenting is an optional therapy (58, 59). As a palliative therapy, stenting can relieve symptoms immediately and improve quality of life (60). Extrinsic or endobronchial obstruction and tracheoesophageal fistula are indications for stenting in malignant tumors (61). In our review, airway stent placement via bronchoscopy was the most commonly used interventional therapy. However, complications associated with stent placement have also been reported. Serino et al. (57) reported that 37.5% of patients with stent placement were associated with ≥1 complication, including mucositis, migration, tumor in-growth, and granulation tissue. However, no case of airway hemorrhage during interventional therapy has been reported.
Various complications associated with ECMO have been reported in critically ill patients (4). These complications may affect patient outcomes and mortality rates. The most common complications associated with VV-ECMO are bleeding and venous thrombosis (62). In our review, airway bleeding was found to be the most common complication. No post-cannulation venous thrombosis was reported because of the relatively short duration of ECMO. Limb ischemia is a common complication of VA-ECMO. However, distal limb reperfusion with an antegrade catheter markedly reduces its incidence (63).
Most patients included in this review experienced immediate relief from symptoms and survived, suggesting that ECMO is practical and safe during interventional therapy in patients at high risk of airway blockade. This study is the first comprehensive analysis of the efficacy of ECMO in critical airway interventional therapy in a large number of patients. Nevertheless, the following limitations should be considered. First, all included studies were case or case series, and the application of ECMO for critical airway therapy is relatively rare. However, avoiding ECMO therapy in patients with a high risk of airway obstruction or refractory cardiac or pulmonary failure does not conform to ethical standards. Second, the patients had different underlying diseases that influenced their survival rates. Third, anticoagulation therapy and targeted ACT differed between studies, which may have affected the incidence of bleeding. Nevertheless, the results of this study have specific value and significance, and further research is warranted.
In conclusion, ECMO is viable for providing adequate cardiac or respiratory support, with an acceptable risk of complications. ECMO accompanied by airway interventional therapy can be successfully performed in patients with critical airway problems. However, further studies are needed to validate these standardized procedures.
HW initiated and coordinated the study. KZ and HW were responsible for the data collection and data analysis. Studies were reviewed by DC. HW wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Thanks to all the participants and investigators of the included studies.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1098594/full#supplementary-material
ECMO, extracorporeal membrane oxygenation; VV, venovenous; VA, venoarterial; ACT, activated clotting time; UFH, unfractionated heparin.
1. Ratwani AP, Davis A, Maldonado F. Current practices in the management of central airway obstruction. Curr Opin Pulm Med (2022) 28(1):45–51. doi: 10.1097/MCP.0000000000000838
2. Jeon K, Kim H, Yu CM, Koh WJ, Suh GY, Chung MP, et al. Rigid bronchoscopic intervention in patients with respiratory failure caused by malignant central airway obstruction. J Thorac Oncol (2006) 1(4):319–23. doi: 10.1097/01243894-200605000-00009
3. Pearson KL, McGuire BE. Anaesthesia for laryngo-tracheal surgery, including tubeless field techniques. BJA Educ (2017) 17(7):242–8. doi: 10.1093/bjaed/mkx004
4. Gajkowski EF, Herrera G, Hatton L, Velia Antonini M, Vercaemst L, Cooley E. ELSO guidelines for adult and pediatric extracorporeal membrane oxygenation circuits. ASAIO J (2022) 68(2):133–52. doi: 10.1097/MAT.0000000000001630
5. Higashi K, Takeshita J, Terasaki H, Tanoue T, Esaki K, Sakamoto M, et al. A case of acute airway obstruction with sharp sawdust particles, successfully treated by extracorporeal lung assist. Kokyu To Junkan (1989) 37(3):329–33.
6. Isaacson G. Acute airway obstruction in the hospitalized infant: Four hard lessons in the distal trachea. Ann Otol Rhinol Laryngol (1996) 105(7):532–5. doi: 10.1177/000348949610500707
7. Morneault L, Johnston A, Perreault T. Management of acute airway obstruction using extracorporeal membrane oxygenation. ASAIO J (1996) 42(4):321–3. doi: 10.1097/00002480-199642040-00017
8. Rosa P Jr, Johnson EA, Barcia PJ. The impossible airway: A plan. Chest (1996) 109(6):1649–50. doi: 10.1378/chest.109.6.1649
9. Belmont MJ, Wax MK, DeSouza FN. The difficult airway: Cardiopulmonary bypass–the ultimate solution. Head Neck (1998) 20(3):266–9. doi: 10.1002/(SICI)1097-0347(199805)20:3<266::AID-HED12>3.0.CO;2-I
10. Stewart AS, Smythe WR, Aukburg S, Kaiser LR, Fox KR, Bavaria JE. Severe acute extrinsic airway compression by mediastinal tumor successfully managed with extracorporeal membrane oxygenation. ASAIO J (1998) 44(3):219–21. doi: 10.1097/00002480-199805000-00018
11. Brown KL, Shefler A, Cohen G, DeMunter C, Pigott N, Goldman AP. Near-fatal grape aspiration with complicating acute lung injury successfully treated with extracorporeal membrane oxygenation. Pediatr Crit Care Med (2003) 4(2):243–5. doi: 10.1097/01.PCC.0000059332.48377.7A
12. Ignacio RC Jr, Falcone RA Jr, Brown RL. A case report of severe tracheal obstruction requiring extracorporeal membrane oxygenation. J Pediatr Surg (2006) 41(10):E1–4. doi: 10.1016/j.jpedsurg.2006.06.021
13. Smith IJ, Sidebotham DA, McGeorge AD, Dorman EB, Wilsher ML, Kolbe J. Use of extracorporeal membrane oxygenation during resection of tracheal papillomatosis. Anesthesiology (2009) 110(2):427–9. doi: 10.1097/ALN.0b013e3181943288
14. Chen A. ECMO-assisted rigid bronchoscopy for tracheal obstruction. J Bronchol Interv Pulmonol (2009) 16(4):296–7. doi: 10.1097/LBR.0b013e3181b767ff
15. Collar RM, Taylor JC, Hogikyan ND, Tutuo N, Ohye RG, Green GE. Awake extracorporeal membrane oxygenation for management of critical distal tracheal obstruction. Otolaryngol Head Neck Surg (2010) 142(4):618–20. doi: 10.1016/j.otohns.2009.10.031
16. Willms DC, Mendez R, Norman V, Chammas JH. Emergency bedside extracorporeal membrane oxygenation for rescue of acute tracheal obstruction. Respir Care (2012) 57(4):646–9. doi: 10.4187/respcare.01417
17. Thung AK, Hayes D Jr, Preston TJ, Tobias JD. Respiratory support including emergent extracorporeal membrane oxygenation as a bridge to airway dilatation following perioperative bronchial occlusion. Middle East J Anaesthesiol (2012) 21(6):879–88.
18. Hong SH, Moon YE, Lee SR, Cho SJ, Kwon OK. Anesthetic management for the insertion of a self-expandable metallic tracheal stent under venovenous extracorporeal membrane oxygenation. Korean J Anesthesiol (2012) 63(6):569–70. doi: 10.4097/kjae.2012.63.6.569
19. Gourdin M, Dransart C, Delaunois L, Louagie YA, Gruslin A, Dubois P. Use of venovenous extracorporeal membrane oxygenation under regional anesthesia for a high-risk rigid bronchoscopy. J Cardiothorac Vasc Anesth (2012) 26(3):465–7. doi: 10.1053/j.jvca.2011.02.013
20. George TJ, Knudsen KP, Sodha NR, Beaty CA, Feller-Kopman D, Shah AS, et al. Respiratory support with venovenous extracorporeal membrane oxygenation during stenting of tracheobronchomalacia. Ann Thorac Surg (2012) 94(5):1736–7. doi: 10.1016/j.athoracsur.2012.03.016
21. Hong Y, Jo KW, Lyu J, Huh JW, Hong SB, Jung SH, et al. Use of venovenous extracorporeal membrane oxygenation in central airway obstruction to facilitate interventions leading to definitive airway security. J Crit Care (2013) 28(5):669–74. doi: 10.1016/j.jcrc.2013.05.020
22. Chang YC, Lee JM, Ko WJ, Lee YC. Airway obstruction following bronchoscopic photodynamic therapy in early centrally located lung cancer requiring extracorporeal membrane oxygenation. J Formos Med Assoc (2013) 112(1):54–6. doi: 10.1016/j.jfma.2012.07.013
23. Metcalf KB, Michaels AJ, Edlich RF, Long WB. Extracorporeal membrane oxygenation can provide cardiopulmonary support during bronchoscopic clearance of airways after sand aspiration. J Emerg Med (2013) 45(3):380–3. doi: 10.1016/j.jemermed.2013.03.017
24. Wang L, Xu XP, Zhan H, Zhang SM. Application of ECMO to the treatment of benign double tracheoesophageal fistula: Report of a case. Ann Thorac Cardiovasc Surg (2014) 20 Suppl:423–6. doi: 10.5761/atcs.cr.13-00313
25. Kim JJ, Moon SW, Kim YH, Choi SY, Jeong SC. Flexible bronchoscopic excision of a tracheal mass under extracorporeal membrane oxygenation. J Thorac Dis (2015) 7(3):E54–7. doi: 10.3978/j.issn.2072-1439.2015.01.26
26. Park JM, Kim CW, Cho HM, Son BS, Kim DH. Induced airway obstruction under extracorporeal membrane oxygenation during treatment of life-threatening massive hemoptysis due to severe blunt chest trauma. J Thorac Dis (2014) 6(12):E255–8. doi: 10.3978/j.issn.2072-1439.2014.10.22
27. Park AH, Tunkel DE, Park E, Barnhart D, Liu E, Lee J, et al. Management of complicated airway foreign body aspiration using extracorporeal membrane oxygenation (ECMO). Int J Pediatr Otorhinolaryngol (2014) 78(12):2319–21. doi: 10.1016/j.ijporl.2014.10.021
28. Ko M, dos Santos PR, Machuca TN, Marseu K, Waddell TK, Keshavjee S, et al. Use of single-cannula venous-venous extracorporeal life support in the management of life-threatening airway obstruction. Ann Thorac Surg (2015) 99(3):e63–5. doi: 10.1016/j.athoracsur.2014.12.033
29. McLenon M, Bittle GJ, Jones K, Menaker J, Pham SM, Iacono AT, et al. Extracorporeal lung support as a bridge to airway stenting and radiotherapy for airway-obstructing pancoast tumor. Ann Thorac Surg (2016) 102(1):e7–9. doi: 10.1016/j.athoracsur.2015.10.109
30. Natt B, Knepler J Jr, Kazui T, Mosier JM. The use of extracorporeal membrane oxygenation in the bronchoscopic management of critical upper airway obstruction. J Bronchol Interv Pulmonol (2017) 24(1):e12–4. doi: 10.1097/LBR.0000000000000347
31. Park JH, Shin JH, Kim KY, Lim JY, Kim PH, Tsauo J, et al. Respiratory support with venovenous extracorporeal membrane oxygenation during stent placement for the palliation of critical airway obstruction: Case series analysis. J Thorac Dis (2017) 9(8):2599–607. doi: 10.21037/jtd.2017.06.88
32. Fung R, Stellios J, Bannon PG, Ananda A, Forrest P. Elective use of veno-venous extracorporeal membrane oxygenation and high-flow nasal oxygen for resection of subtotal malignant distal airway obstruction. Anaesth Intensive Care (2017) 45(1):88–91. doi: 10.1177/0310057X1704500113
33. Ramírez-Romero M, Hernández-Alonso B, García-Polo C, Abraldes-Bechiarelli AJ, Garrino-Fernández A, Gordillo-Brenes A. Central airway obstruction due to inflammatory bowel disease and rescue with extracorporeal membrane oxygenation. Med Intensiva (2018) 42(5):317–9. doi: 10.1016/j.medine.2018.04.006
34. Nokes BT, Vaszar L, Jahanyar J, Swanson KL. VV-ECMO-Assisted high-risk endobronchial stenting as rescue for asphyxiating mediastinal mass. J Bronchol Interv Pulmonol (2018) 25(2):144–7. doi: 10.1097/LBR.0000000000000435
35. Vobruba V, Votruba J, Bělohlávek J, Grus T, Leden P, Zaoral T, et al. Endobronchial stenting on VV-ECMO in a 6-month-old girl with right lung agenesis and severe stenosis of the left main bronchus. Perfusion (2018) 33(7):599–601. doi: 10.1177/0267659118768153
36. Yamada Y, Ohata T, Kitahara M, Kohata H, Kumasawa J, Kohno M. Venovenous extracorporeal membrane oxygenation for the management of critical airway stenosis. J Artif Organs (2018) 21(4):479–81. doi: 10.1007/s10047-018-1070-1
37. Yunoki K, Miyawaki I, Yamazaki K, Mima H. Extracorporeal membrane oxygenation-assisted airway management for difficult airways. J Cardiothorac Vasc Anesth (2018) 32(6):2721–5. doi: 10.1053/j.jvca.2018.01.006
38. Munakata H, Higashi M, Tamura T, Adachi YU. Fatal airway obstruction due to a ball-valve clot with identical signs of tension pneumothorax. Acute Crit Care (2020) 35(4):298–301. doi: 10.4266/acc.2019.00570
39. Pu H, Huang X, Allingstrup MJ, Doig GS, Liang Z. Airway reconstruction supported by venovenous extracorporeal membrane oxygenation for patients with malignant critical central airway obstructions: A case series. J Clin Anesth (2020) 61:109690. doi: 10.1016/j.jclinane.2019.109690
40. Yu W, Zhou P, Chen K, Tang W, Xia Q, Ma J. Bronchoscopy-guided intervention therapy with extracorporeal membrane oxygenation support for advanced cancer metastasis to the central airway: A case report. Medicine (2020) 99(11):e19488. doi: 10.1097/MD.0000000000019488
41. Ni Fhlatharta M, Khan A, Carton E, Redmond KC. Pre-emptive extracorporeal membrane oxygenation to support endobronchial stenting for severe airway obstruction. Eur J Cardiothorac Surg (2021) 59(6):1345–6. doi: 10.1093/ejcts/ezaa425
42. Kitazawa S, Kobayashi N, Ueda S, Enomoto Y, Inoue Y, Shiozawa T, et al. Successful use of extracorporeal membrane oxygenation for airway-obstructing lung adenocarcinoma. Thorac Cancer (2020) 11(10):3024–8. doi: 10.1111/1759-7714.13623
43. Kuroda Y, Uchida T, Hamasaki A, Yamashita A, Mizumoto M, Ishizawa A, et al. Treatment strategy for severe airway stenosis due to a thoracic aortic aneurysm. Ann Thorac Surg (2020) 110(3):e195–7. doi: 10.1016/j.athoracsur.2020.01.024
44. Odigwe C, Krieg J, Owens W, Lopez C, Arya RR. Usefulness of extracorporeal membrane oxygenation in status asthmaticus with severe tracheal stenosis. Proc (2020) 33(3):404–6. doi: 10.1080/08998280.2020.1759333
45. Zimmermann M, Vallier S, Sanchez BG, Agossou M, Venissac N. Tracheal obstruction due to tumour: Use of veno-venous extracorporeal membrane oxygenation during rigid bronchoscopy. Anaesth Rep (2020) 8(2):120–2. doi: 10.1002/anr3.12064
46. Meyer S, Dincq AS, Pirard L, Ocak S, D'Odémont JP, Eucher P, et al. Bronchotracheal stenting management by rigid bronchoscopy under extracorporeal membrane oxygenation (ECMO) support: 10 years of experience in a tertiary center. Can Respir J (2021) 2021:8822591. doi: 10.1155/2021/8822591
47. Shirasaki K, Hifumi T, Kato T, Ishimatsu S. Central airway obstruction treated with initial support by venovenous extracorporeal membrane oxygenation. BMJ Case Rep (2021) 14(3):e237282. doi: 10.1136/bcr-2020-237282
48. Siddiqi MS, Al Kindi AH, Mandisha AF, Al Sukaiti R. Pre-emptive veno-venous ECMO in advanced tracheal malignancy prior to tracheal stenting. BMJ Case Rep (2021) 14(8):e243596. doi: 10.1136/bcr-2021-243596
49. Watanabe K, Oka S, Kai T, Hoshino K, Nakamura J, Abe M, et al. Tracheobronchial obstruction due to blood clots in acute pulmonary embolism with cardiac arrest managed with extracorporeal membrane oxygenation. Intern Med (2021) 60(17):2811–7. doi: 10.2169/internalmedicine.6856-20
50. Zhang J, He X, Hu J, Li T. Application of extracorporeal membrane oxygenation to treatment of serious tracheal stenosis caused by relapsing polychondritis: A case report and literature review. J Int Med Res (2021) 49(4):3000605211009489. doi: 10.1177/03000605211009489
51. Kawakado K, Hotta T, Sakamoto J, Horie M, Kobayashi M, Okuno T, et al. Acute exacerbation of tracheal obstruction and severe respiratory failure after a single dose of 2-gy irradiation for squamous cell lung carcinoma: A case report. Case Rep Oncol (2022) 15(1):356–61. doi: 10.1159/000523941
52. Giani M, Pisa A, Passera E, Avalli L, Rona R, Foti G. Tracheal stenting on venovenous ECMO with a dual lumen right atrium-to-pulmonary artery cannula in a COVID-19 patient with an inferior vena cava filter. Perfusion (2022) 38(3):2676591211066805. doi: 10.1177/02676591211066805
53. Petrou M, Goldstraw P. The management of tracheobronchial obstruction: A review of endoscopic techniques. Eur J Cardiothorac Surg (1994) 8(8):436–41. doi: 10.1016/1010-7940(94)90086-8
54. Wood DE. Management of malignant tracheobronchial obstruction. Surg Clin North Am (2002) 82(3):621–42. doi: 10.1016/S0039-6109(02)00025-7
55. Unger M. Endobronchial therapy of neoplasms. Chest Surg Clin N Am (2003) 13(1):129–47. doi: 10.1016/S1052-3359(02)00041-8
56. Fierro MA, Daneshmand MA, Bartz RR. Perioperative management of the adult patient on venovenous extracorporeal membrane oxygenation requiring noncardiac surgery. Anesthesiology (2018) 128(1):181–201. doi: 10.1097/ALN.0000000000001887
57. Serino M, Freitas C, Saleiro S, Cabrita B, Conde M, Fernandes MGO, et al. Airway stents in malignant central airway obstruction. Pulmonology (2021) 27(5):466–9. doi: 10.1016/j.pulmoe.2021.02.003
58. Mitchell PD, Kennedy MP. Bronchoscopic management of malignant airway obstruction. Adv Ther (2014) 31(5):512–38. doi: 10.1007/s12325-014-0122-z
59. Kniese CM, Musani AI. Bronchoscopic treatment of inoperable nonsmall cell lung cancer. Eur Respir Rev (2020) 29(158):200035. doi: 10.1183/16000617.0035-2020
60. Kim BG, Shin B, Chang B, Kim H, Jeong BH. Prognostic factors for survival after bronchoscopic intervention in patients with airway obstruction due to primary pulmonary malignancy. BMC Pulm Med (2020) 20(1):54. doi: 10.1186/s12890-020-1095-0
61. Oberg C, Folch E, Fernando Santacruz J. Management of malignant airway obstruction. AME Med J (2018) 3:115. doi: 10.21037/amj.2018.11.06
62. Marasco SF, Lukas G, McDonald M, McMillan J, Ihle B. Review of ECMO (extra corporeal membrane oxygenation) support in critically ill adult patients. Heart Lung Circ (2008) 17(Suppl 4):S41–7. doi: 10.1016/j.hlc.2008.08.009
Keywords: extracorporeal membrane oxygenation, interventional therapy, bronchoscopy, malignant tumor, airway stenosis, airway obstruction
Citation: Wu H, Zhuo K and Cheng D (2023) Extracorporeal membrane oxygenation in critical airway interventional therapy: A review. Front. Oncol. 13:1098594. doi: 10.3389/fonc.2023.1098594
Received: 15 November 2022; Accepted: 13 March 2023;
Published: 27 March 2023.
Edited by:
Venkatesan Renugopalakrishnan, Harvard University, United StatesReviewed by:
Suresh Keshavamurthy, University of Kentucky, United StatesCopyright © 2023 Wu, Zhuo and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Deyun Cheng, emh1b2txMjAxNEAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.