
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Oncol. , 09 February 2023
Sec. Surgical Oncology
Volume 13 - 2023 | https://doi.org/10.3389/fonc.2023.1049294
 Wu Wangjian1†
Wu Wangjian1† Lu Tianyi2†
Lu Tianyi2† Ma Xiaoqian3†
Ma Xiaoqian3† Zhang Di2
Zhang Di2 Zhou Chuan1
Zhou Chuan1 Wang Chao1
Wang Chao1 Da Zijian1
Da Zijian1 Jin Tongtong1
Jin Tongtong1 Zhou Fenghai1,2,4*
Zhou Fenghai1,2,4*Objectives: In recent years, enhanced recovery after surgery (ERAS) has been widely used in the field of urology, especially in radical cystectomy and radical prostatectomy, and has demonstrated its advantages. Although studies on the application of ERAS in partial nephrectomy for renal tumors are increasing, the conclusions are mixed, especially in terms of postoperative complications, etc, and its safety and efficacy are questionable. We conducted a systematic review and meta-analysis to assess the safety and efficacy of ERAS in the application of partial nephrectomy for renal tumors.
Methods: Pubmed, Embase, Cohrance library, Web of science and Chinese databases (CNKI, VIP, Wangfang and CBM) were systematically searched for all published literature related to the application of enhanced recovery after surgery in partial nephrectomy for renal tumors from the date of establishment to July 15, 2022, and the literature was screened by inclusion/exclusion criteria. The quality of the literature was evaluated for each of the included literature. This Meta-analysis was registered on PROSPERO (CRD42022351038) and data were processed using Review Manager 5.4 and Stata 16.0SE. The results were presented and analyzed by weighted mean difference (WMD), Standard Mean Difference (SMD) and risk ratio (RR) at their 95% confidence interval (CI). Finally, the limitations of this study are analyzed in order to provide a more objective view of the results of this study.
Results: This meta-analysis included 35 literature, including 19 retrospective cohort studies and 16 randomized controlled studies with a total of 3171 patients. The ERAS group was found to exhibit advantages in the following outcome indicators: postoperative hospital stay (WMD=-2.88, 95% CI: -3.71 to -2.05, p<0.001), total hospital stay (WMD=-3.35, 95% CI: -3.73 to -2.97, p<0.001), time to first postoperative bed activity (SMD=-3.80, 95% CI: -4.61 to -2.98, p < 0.001), time to first postoperative anal exhaust (SMD=-1.55, 95% CI: -1.92 to -1.18, p < 0.001), time to first postoperative bowel movement (SMD=-1.52, 95% CI: -2.08 to -0.96, p < 0.001), time to first postoperative food intake (SMD=-3.65, 95% CI: -4.59 to -2.71, p<0.001), time to catheter removal (SMD=-3.69, 95% CI: -4.61 to -2.77, p<0.001), time to drainage tube removal (SMD=-2.77, 95% CI: -3.41 to -2.13, p<0.001), total postoperative complication incidence (RR=0.41, 95% CI: 0.35 to 0.49, p<0.001), postoperative hemorrhage incidence (RR=0.41, 95% CI: 0.26 to 0.66, p<0.001), postoperative urinary leakage incidence (RR=0.27, 95% CI: 0.11 to 0.65, p=0.004), deep vein thrombosis incidence (RR=0.14, 95% CI: 0.06 to 0.36, p<0.001), and hospitalization costs (WMD=-0.82, 95% CI: -1.20 to -0.43, p<0.001).
Conclusion: ERAS is safe and effective in partial nephrectomy of renal tumors. In addition, ERAS can improve the turnover rate of hospital beds, reduce medical costs and improve the utilization rate of medical resources.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO, identifier CRD42022351038.
Renal tumors are relatively common neoplastic diseases of the urinary system, approximately 85% of which are renal cell carcinomas, and the incidence of the latter is increasing by an average of 0.6% per year (1). It is estimated that 77,410 Chinese will be diagnosed with kidney cancer in China in 2022, and 46,345 of them will die from the disease (2). For renal tumors, the earlier they are detected and treated, the better the prognosis of patients. The traditional treatment for localized renal cell carcinoma is radical nephrectomy, but with the continuous development of medical technology and the improvement of people’s demand for quality of life, the treatment for localized renal cell carcinoma is gradually shifted from radical nephrectomy to partial nephrectomy. Furthermore, the study (3) has shown that compared with radical nephrectomy, partial nephrectomy is more advantageous in terms of postoperative renal function, incidence of chronic kidney disease, tumor recurrence rate, cancer-specific mortality and all-cause mortality, but the complexity of the partial nephrectomy procedure makes it have a higher rate of postoperative complications.
Enhanced recovery after surgery (ERAS) was originally proposed by Danish physicians Wilmore and Kehlet (4) to minimize perioperative physiological dysfunction and surgical stress to promote faster return to normal function, shorter hospital stays and fewer postoperative complications (5). Currently, ERAS has been used in urological procedures such as radical prostatectomy and radical cystectomy, and has shown its advantages (6, 7). Important components of ERAS include detailed preoperative communication, 6-hour preoperative fasting and 2-hour preoperative water fasting, no preoperative enema treatment, preoperative oral carbohydrate, preoperative antibiotic use, intraoperative maintenance of body temperature, intraoperative goal-directed fluid therapy(GDT), reduction of opioid use, early postoperative feeding, early postoperative bed mobility, and early postoperative extubation. One of the more distinctive features of ERAS, GDT, is an optimized intraoperative individualized fluid therapy strategy that uses advanced dynamic detection methods and effective standard treatment procedures to obtain ideal preload and oxygen delivery to improve patient circulation and tissue support, reduce complications, and ultimately achieve a better prognosis. In addition, early bed mobility in ERAS is a way to perform simple activities in bed with the help of a physiotherapist on the day after surgery, and to walk slowly afterwards, which can reduce the complications of prolonged bed rest after surgery and promote rapid postoperative recovery. In recent years, studies on the application of ERAS in partial nephrectomy for renal tumors have been increasing, but the effectiveness of its application in partial nephrectomy for renal tumors is still controversial, especially the findings on postoperative complications are not consistent, so this study was conducted to evaluate the safety and efficacy of ERAS in partial nephrectomy for renal tumors.
The systematic review and meta-analysis strictly followed the preferred reporting items (PRISMA) list for systematic reviews and meta-analyses (8). The systematic evaluation and meta-analysis has been registered on PROSPERO (CRD42022351038).
This search was conducted using subject terms plus free words for all literature related to enhanced recovery after surgery in partial nephrectomy from Pubmed, Embase, Cohrance library, Web of science, CNKI, VIP, Wangfang, and CBM from the date of library construction to July 15, 2022. There are no publication language and time restrictions in the search process. In addition, references to the literature were retroactively included to supplement access to relevant literature. Search terms include: “enhanced recovery after surgery”, “fast track surgery”, “ERAS”, “FTS”, “renal Cell Carcinomas”, “Kidney Neoplasms”, “partial nephrectomy”, “nephron sparing surgery”, etc. Take Pubmed search strategy as an example, see Table 1.
Inclusion criteria: (1) Patients with renal tumors who underwent partial nephrectomy; (2) A comparative study between ERAS and conventional nursing; (3) At least one primary or secondary outcome must be included: length of postoperative hospital stay(from the end of surgery to the time of discharge), total hospital stay(time from admission to discharge), time to first postoperative bed activity, time to first postoperative anal exhaust, time to first postoperative bowel movement, time to first postoperative food intake, time to removal of catheter, time to removal of drainage tube, incidence of total postoperative complications, and hospitalization cost.
Exclusion criteria: (1) Literature with completely duplicated or mostly duplicated data sources; (2) Literature that is not available in full text; (3) Literature that does not identify the type of surgery or non-partial nephrectomy; (4) Literature with ERAS of less than 2 factors; (5) Types of articles such as overviews, case reports, reviews, etc; (6) NOS < 6.
The literature searched from each database was imported into EndNote X7 and screened independently by two authors (WWJ and LTY) according to the inclusion exclusion criteria, with the assistance of a third author (MXQ) to judge if disagreement arose. For literature screening, duplicates were first screened out and excluded, then apparently irrelevant studies were excluded by reading the titles and abstracts of the literature, and finally the full text was read to determine the final literature to be included in this study. The content to be extracted included: first author, year of publication, study type, country, age, gender, sample size, composition of ERAS, surgical modality (robot-assisted laparoscopic surgery, laparoscopic surgery, or open surgery), surgical access (transabdominal or extra-abdominal), and outcome indicators (primary outcome: postoperative length of stay and total length of stay; secondary outcomes: postoperative time to first bed activity, postoperative time to first anal exhaust, postoperative time to first bowel movement, postoperative time to first food intake, catheter removal time, drainage tube removal time, total postoperative complication rate, and hospitalization cost).
Two authors jointly conducted quality assessment of randomized controlled studies (RCTs) according to the Cochrane Risk of Bias tool (9) and case-control studies or cohort studies according to the Newcastle-Ottawa (NOS) scale (10). The Cochrane Risk of Bias Tool assessment focused on whether the random allocation method was correct, whether the allocation scheme was well concealed, whether blinding was implemented, whether the data results were complete, whether there was selective reporting, and whether there were other biases in the study. The NOS scale was evaluated for appropriateness of cohort selection (0-4 points), comparability between groups (0-2 points), and method of determining outcomes of interest (0-3 points), for a total of 9 points.
This Meta-analysis was performed using Review Manager 5.4 and Stata 16.0SE. For dichotomous variables, the relative risk ratio (RR) is used as an effect indicator; for continuous variables, the weighted mean difference (WMD) or standardized mean difference (SMD) is used as an effect indicator, and estimates and 95% confidence intervals (95% CI) are provided. The chi-square test and I2 test were used to assess heterogeneity between studies. If there was no statistical heterogeneity between studies (p≥0.10 and I²≤50%), the fixed-effects model was used; conversely, the random-effects model was used. Subgroup analysis was used to analyze the source of heterogeneity. Sensitivity analysis was used to test the stability of the meta-analysis results. The presence of publication bias was assessed using funnel plots and Egger’s test.
A total of 1263 associated articles were searched, and 35 articles were finally obtained through screening (11–45), of which 19 were retrospective cohort studies and 16 were RCTs. A total of 3171 patients were involved in the 35 literature, with 1632 patients in the ERAS group and 1539 patients in the usual care group. The literature screening process is shown in Figure 1. The basic characteristics of the included literature are shown in Table 2. The ERAS elements included in the studies are shown in Table 3.
The quality of the included retrospective cohort studies was assessed using the NOS scale, which showed six with a score of 6, six with a score of 7, one with a score of 8, and six with a score of 9. The detailed scoring results are shown in Table 4. Quality assessment of randomized controlled studies using the Cochrane Risk of Bias tool identified three different studies (30, 36, 38) that were at high risk of selection bias. See Figure 2.
A total of 29 studies reported on postoperative length of stay, involving a total of 2471 patients (1243 patients in the ERAS group and 1228 patients in the routine care group). A random-effects model summary showed that the postoperative hospital stay was significantly shorter by 2.88 days in the ERAS group compared with the routine care group (WMD=-2.88, 95% CI: -3.71 to -2.05, p<0.001, I2 = 99.0%) (Figure 3A). Subgroup analysis by surgical approach showed that the postoperative hospital stay was reduced by 2.09 days (WMD=-2.09, 95% CI: -3.37 to -0.80, p<0.001, I2 = 97.7%) in the subgroup of robot-assisted laparoscopic surgery (Figure 1 in Supplementary Data Sheet 1); the postoperative hospital stay was reduced by 3.00 days in the subgroup of laparoscopic surgery (WMD=-3.00, 95% CI: -4.03 to -1.98, p < 0.001, I2 = 99.0%) (Figure 1 in Supplementary Data Sheet 1).
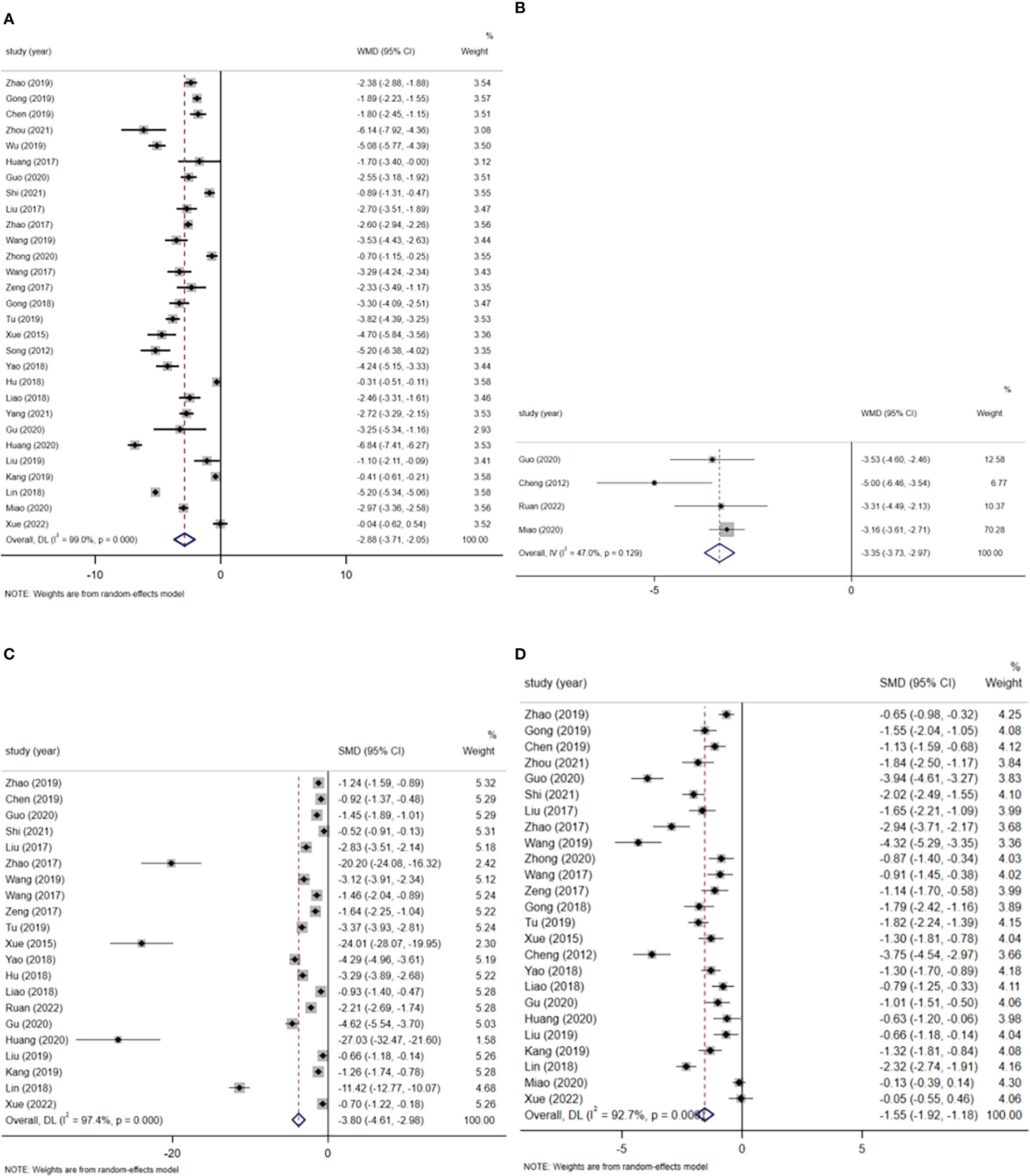
Figure 3 (A) Postoperative hospital stay. (B) Total hospital time. (C) First time out of bed after surgery. (D) Time of first postoperative anal exhaust.
Four studies reported total length of stay, involving a total of 495 patients (253 patients in the ERAS group and 242 patients in the routine care group). A fixed-effects model summary showed that the total length of stay was 3.35 days shorter in the ERAS group compared with the routine care group (WMD=-3.35, 95% CI: -3.73 to -2.97, p<0.001, I2 = 47.0%) (Figure 3B).
A total of 21 studies reported time to first postoperative bed activity. A total of 1794 patients were involved, including 900 patients in the ERAS group. A random-effects model summary showed that the ERAS group significantly moved patients out of bed earlier after surgery compared to the routine care group (SMD=-3.80, 95% CI: -4.61 to -2.98, p<0.001, I2 = 97.4%) (Figure 3C). Subgroup analysis by surgical approach showed that ERAS significantly earlier postoperative bed mobility in both robot-assisted laparoscopic surgery and laparoscopic surgery (robot-assisted laparoscopic surgery: SMD=-3.91, 95% CI: -5.21 to -2.61, p<0.001, I2 = 82.2%; laparoscopic surgery: SMD=-4.33, 95% CI. -5.33 to -3.33, p<0.001, I2 = 97.7%) (Figure 2 in Supplementary Data Sheet 1).
A total of 25 studies reported the time of first postoperative anal exhaust and included a total of 2114 patients (1062 patients in the ERAS group and 1052 patients in the usual care group). The Meta-analysis showed that the ERAS group had an earlier time to first postoperative anal exhaust compared to the usual care group (SMD=-1.55, 95% CI: -1.92 to -1.18, p<0.001, I2 = 92.7%) (Figure 3D). Subgroup analysis by surgical approach showed that ERAS resulted in earlier postoperative anal exhaust in patients who underwent robotic-assisted laparoscopic surgery and laparoscopic surgery (robotic-assisted laparoscopic surgery: SMD=-1.15, 95% CI: -1.56 to -0.74, p<0.001, I2 = 48.7%; laparoscopic surgery: SMD=-1.70, 95% CI: - 2.18 to -1.23, p<0.001, I2 = 94.1%) (Figure 3 in Supplementary Data Sheet 1).
A total of 7 studies reported the time to first postoperative bowel movement. A total of 775 patients were included, including 394 patients in the ERAS group and 381 patients in the usual care group. A random-effects model summary showed that ERAS significantly earlier the time to first postoperative bowel movement in patients compared to routine care (SMD=-1.52, 95% CI: -2.08 to -0.96, p<0.001, I2 = 91.2%) (Figure 4A). Subgroup analysis by surgical approach showed that ERAS was associated with earlier postoperative defecation in both robot-assisted laparoscopic surgery and laparoscopic surgery (robot-assisted laparoscopic surgery: SMD=-1.26, 95% CI: -1.58 to -0.94, p<0.001, I2 = 0.0%; laparoscopic surgery: SMD=-1.56, 95% CI: - 2.89 to -0.23, p=0.021, I2 = 96.7%) (Figure 4 in Supplementary Data Sheet 1).
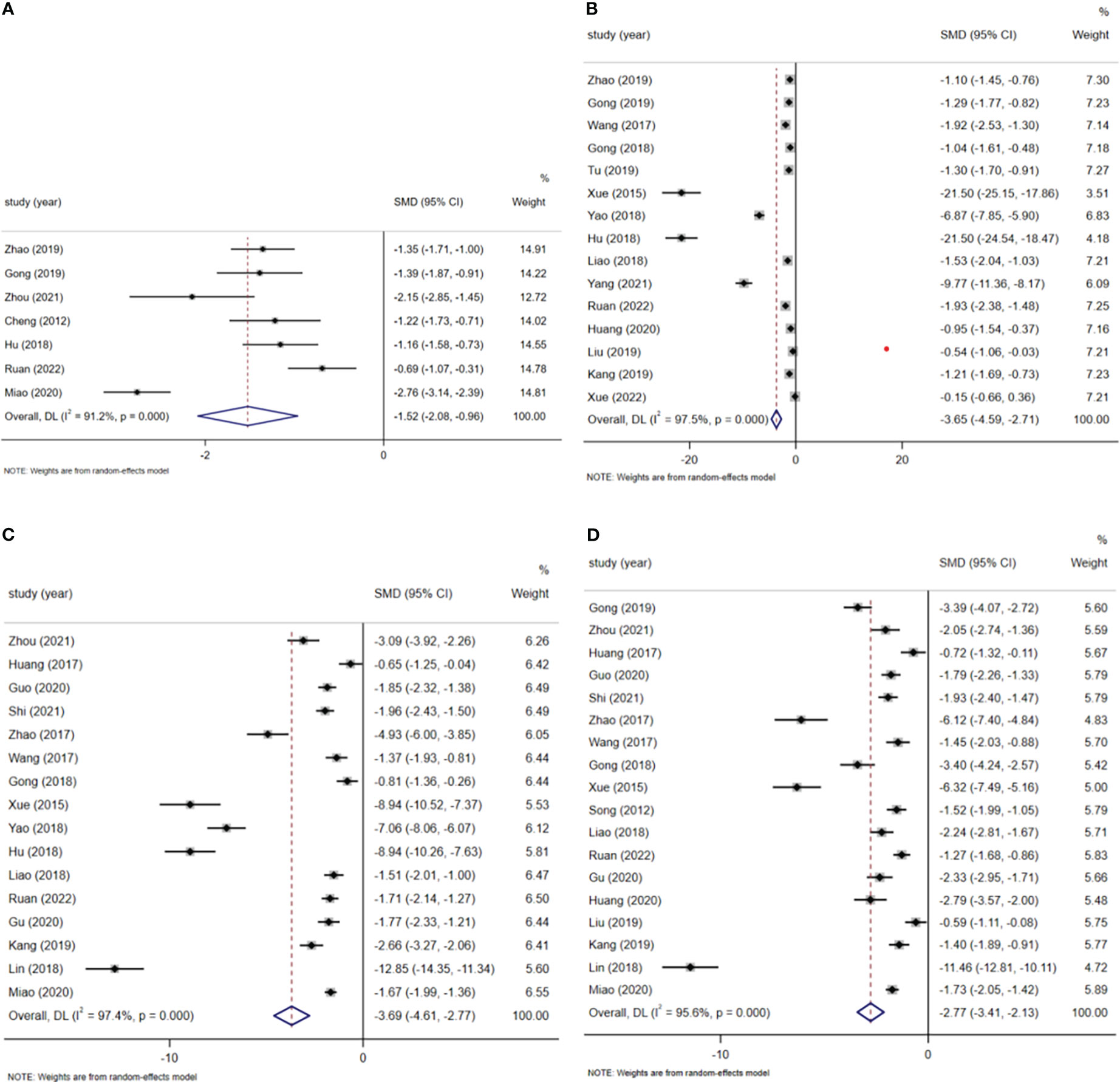
Figure 4 (A) Time of first bowel movement after surgery. (B) Time of first postoperative food intake. (C) Removal time of catheter. (D) Removal time of drainage tube.
A total of 15 studies reported the time to first postoperative food intake, involving a total of 1269 patients (639 patients in the ERAS group and 630 patients in the routine care group). A random-effects model summary showed patients in the ERAS group had their first postoperative meal earlier compared to the usual care group (SMD=-3.65, 95% CI: -4.59 to -2.71, p<0.001, I2 = 97.5%) (Figure 4B). Subgroup analysis by surgical approach showed no significant difference in time to first postoperative food intake with ERAS in robotic-assisted laparoscopic surgery (SMD=-11.34, 95% CI: -31.15 to 8.47, p=0.262, I2 = 99.4%), but limited studies were included and the results need to be treated with caution; ERAS in laparoscopic surgery was able to advance patients’ postoperative time to first meal (SMD=-3.37, 95% CI: -4.50 to -2.24, p<0.001, I2 = 97.4%) (Figure 5 in Supplementary Data Sheet 1).
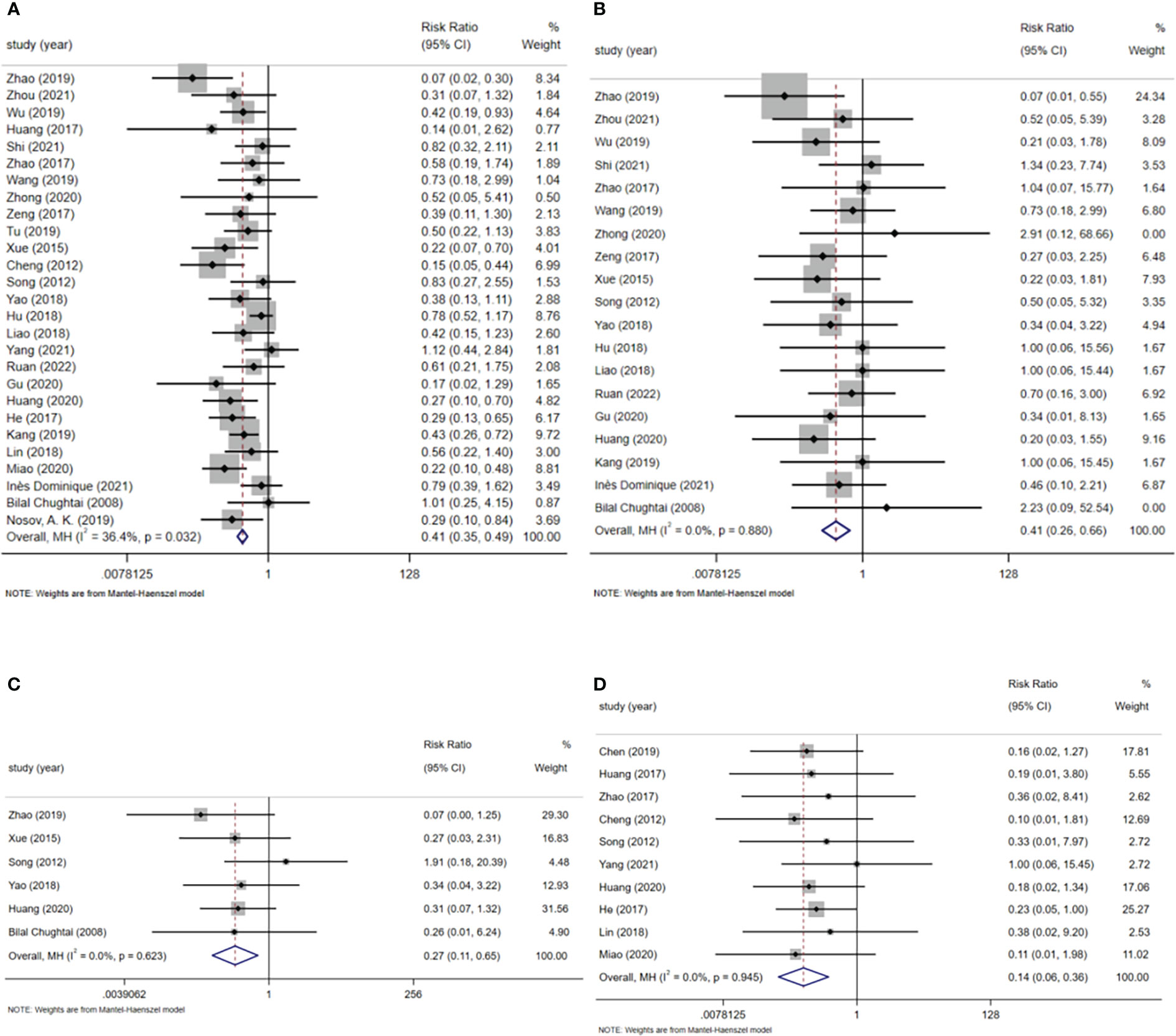
Figure 5 (A) Postoperative complications. (B) Postoperative bleeding. (C) Postoperative urine leakage. (D) Deep vein thrombosis.
A total of 16 studies reported validated data on catheter removal time, containing 1453 patients (731 patients in the ERAS group and 722 patients in the routine care group). The meta-analysis showed that the ERAS group had a shorter catheter removal time compared to the usual care group (SMD=-3.69, 95% CI: -4.61 to -2.77, p<0.001, I2 = 97.4%) (Figure 4C). Subgroup analysis by surgical approach showed ERAS reduced catheter removal time in both robot-assisted laparoscopic and laparoscopic procedures (robot-assisted laparoscopic surgery: SMD=-3.72, 95% CI: -7.10 to -0.33, p=0.031, I2 = 98.4%; laparoscopic surgery: SMD=-3.98, 95% CI: - 5.12 to -2.84, p<0.001, I2 = 97.7%) (Figure 6 in Supplementary Data Sheet 1).
A total of 18 studies containing valid data on drain removal time involved a total of 1521 patients (766 patients in the ERAS group and 755 patients in the routine care group). In a random effects model pooled analysis, patients in the ERAS group had a shorter drain removal time compared to those in the usual care group (SMD=-2.77, 95% CI: -3.41 to -2.13, p<0.001, I2 = 95.6%) (Figure 4D). In a subgroup analysis by surgical method, ERAS was able to reduce the removal time of drains in patients both in robot-assisted laparoscopic surgery and in laparoscopic surgery (robot-assisted laparoscopic surgery: SMD=-2.14, 95% CI: -3.66 to -0.62, p=0.006, I2 = 94.2%; laparoscopic surgery: SMD=-3.05, 95% CI: -3.88 to -2.22, p<0.001, I2 = 96.6%) (Figure 7 in Supplementary Data Sheet 1).
A total of 27 studies reported total postoperative complications, mainly including fever, nausea and vomiting, abdominal distention, postoperative hemorrhage, postoperative urinary leakage, and deep vein thrombosis, involving a total of 2599 patients, (1343 patients in the ERAS group and 1256 patients in the usual care group). In a fixed-effects model pooled analysis, ERAS reduced the rate of total postoperative complications after partial nephrectomy compared to usual care (RR=0.41, 95% CI: 0.35-0.49, p<0.001, I2 = 36.4%) (Figure 5A). In a subgroup analysis by surgical approach, ERAS was demonstrated to reduce total postoperative complication rates in both robot-assisted laparoscopic surgery, laparoscopic surgery and open surgery (robot-assisted laparoscopic surgery: RR=0.61, 95% CI: 0.45-0.84, p=0.002, I2 = 6.0%; laparoscopic surgery: RR=0.40, 95% CI: 0.32~ 0.49, p<0.001, I2 = 20.8%; open surgery: RR=0.42, 95% CI: 0.22-0.82, p=0.010, I2 = 0.0%) (Figure 8 in Supplementary Data Sheet 1).
A total of 20 studies reported postoperative hemorrhage involving a total of 1670 patients (878 patients in the ERAS group and 792 patients in the routine care group) and a total of 87 patients (26 patients in the ERAS group and 61 patients in the routine care group) with postoperative hemorrhage. A fixed-effects model summary showed ERAS was more able to reduce the incidence of postoperative hemorrhage in patients compared to usual care (RR=0.41, 95% CI: 0.26 to 0.66, p<0.001, I2 = 0.0%) (Figure 5B).
A total of 6 studies reported postoperative urinary leakage involving 529 patients (269 patients in the ERAS group and 260 patients in the routine care group), of which a total of 30 patients had postoperative leakage (6 patients in the ERAS group and 24 patients in the routine care group). In a fixed-effects model pooled analysis, ERAS reduced the incidence of postoperative urinary leakage in patients compared to routine care (RR=0.27, 95% CI: 0.11 to 0.65, p=0.004, I2 = 0.0%) (Figure 5C).
A total of 11 studies reported the incidence of deep vein thrombosis in a total of 993 patients (498 patients in the ERAS group and 495 patients in the routine care group), of which 44 patients developed deep limb venous thrombosis (5 patients in the ERAS group and 39 patients in the routine care group). A fixed-effects model summary showed ERAS was more able to reduce the formation of DVT in patients compared to usual care (RR=0.14, 95% CI: 0.06-0.36, p<0.001, I2 = 0.0%) (Figure 5D).
A total of 14 studies reported patient hospital costs for a total of 1247 patients (626 patients in the ERAS group and 621 patients in the routine care group). A random-effects model pooled analysis showed that ERAS reduced patients’ hospital costs compared to usual care (WMD=-0.82, 95% CI: -1.20 to -0.43, p<0.001, I2 = 99.0%) (Figure 6). A subgroup analysis by surgical approach found that ERAS reduced patient hospitalization costs in both robot-assisted laparoscopic and laparoscopic procedures (robot-assisted laparoscopic surgery: WMD=-2.44, 95% CI: -2.90 to -1.98, p=0.006, I2 = 86.2%; laparoscopic surgery: WMD=-0.56, 95% CI: - 0.90 to -0.22, p=0.001, I2 = 98.6%) (Figure 9 in Supplementary Data Sheet 1).
Sensitivity analysis was performed on the outcome indicators of postoperative hospital stay, total hospital stay, first time out of bed after surgery, time of first postoperative anal exhaust, time of first bowel movement after surgery, time of first postoperative food intake, removal time of catheter, removal time of drainage tube, incidence of total postoperative complications, incidence of postoperative hemorrhage, incidence of postoperative urine leakage, incidence of deep vein thrombosis, and hospitalization costs by excluding one study at a time and observing the combined effect size. The results of the sensitivity analysis showed that the pooled results of these outcome indicators were stable. See Supplementary Data Sheet 2.
Publication bias for each outcome indicator was assessed using funnel plots with Egger’s test. The funnel diagram of each outcome indicator is shown in Supplementary Data Sheet 3. Egger’s test showed significant publication bias for first time out of bed after surgery (P<0.001), time of first postoperative anal exhaust (P<0.001), time of first postoperative food intake (P<0.001), removal time of catheter (P<0.001), and removal time of drainage tube (P<0.001), and significant publication bias for postoperative hospital stay (P=0.881), total hospital time (P=0.233), time to first postoperative bowel movement (P=0.907), total postoperative complication rate (P=0.049), postoperative hemorrhage rate (P=0.554), postoperative urine leakage rate (P=0.853), deep vein thrombosis rate (P=0.614) and hospitalization cost (P=0.940) were not publication biased.
ERAS is a new model of care based on evidence-based medicine, consisting of surgery, nursing, anesthesia, rehabilitation, nutrition, and other disciplines, which aims to reduce the length of hospital stay and postoperative complications by reducing the stress response caused by surgical trauma, thereby facilitating rapid patient recovery (46). The effectiveness of ERAS was initially demonstrated in colorectal surgery and then widely used in urology for radical cystectomy and radical prostatectomy with favorable results. Although ERAS has been well studied in partial nephrectomy for renal tumors, the conclusions are mixed, especially in terms of postoperative complications and other aspects, and its safety and efficacy are debatable. This study was the first to compare the recent efficacy of ERAS and routine care application in the perioperative period of partial nephrectomy for renal tumors by Meta-analysis method to confirm that ERAS application is safe and effective in partial nephrectomy for renal tumors.
Postoperative length of stay and total length of stay are important indicators to assess the effectiveness of ERAS. The results of this study showed that both the subgroup analysis and the pooled analysis of the robot-assisted laparoscopic surgery group and the laparoscopic surgery group showed that the postoperative hospital stay was significantly shorter in the ERAS group than in the usual care group (WMD=-2.88, 95% CI: -3.71 to -2.05, p<0.001), which is consistent with the study of Domenic Di Rollo et al (47). Similarly, ERAS reduced the total length of stay (WMD=-3.35, 95% CI: -3.73 to -2.97, p<0.001), but given the limited number of included studies, no subgroup analysis was performed. The reduction of postoperative hospital stay may be closely related to preoperative oral carbohydrates, preoperative prehabilitation, effective postoperative analgesia, early feeding, and early bed mobility treatment. The absence of preoperative enema treatment reduces intestinal flora and water and electrolyte disturbances, which in turn accelerates the recovery of intestinal function (48). With regard to postoperative feeding time in the robot-assisted laparoscopic subgroup, however, there was no statistical difference between the ERAS group and the usual care group (P=0.262). Nevertheless, considering the small number of included studies and the fact that ERAS was able to shorten the feeding time after robotic-assisted partial nephrectomy in all included studies (12, 31), it cannot be completely stated that ERAS cannot shorten the feeding time after robotic-assisted partial nephrectomy, and further clinical validation is required for follow-up. This study showed that ERAS can shorten the removal time of catheter and drainage tube (P < 0.001), which can indirectly reduce the occurrence of catheter-related urinary tract infections (49, 50) and also facilitate early patient mobility. However, there was publication bias in the results of catheter and drainage tube removal times, which was considered to be caused by the small sample size of some included literature and unreported outcome indicators (14, 16, 20, 25, 36), so further validation in future clinical studies with large samples should be performed.
The incidence of total postoperative complications is an important indicator to assess the safety of ERAS. The main postoperative complications of partial nephrectomy include fever, nausea and vomiting, abdominal distention, postoperative hemorrhage, postoperative urinary leakage, and deep vein thrombosis, among other complications. The results of this study showed that the implementation of ERAS in either the robotic-assisted laparoscopic group or the laparoscopic group did not increase the postoperative complication rate, but rather led to a decrease (RR=0.41, 95% CI: 0.35 to 0.49, p<0.001). This may be related to ERAS elements such as oral intake of liquid carbohydrates and goal-directed fluid management 2 hours prior to surgery. Perioperative application of goal-directed fluid management significantly reduces postoperative complications, shortens the length of hospital stay, and accelerates patient recovery (51, 52). Hemorrhage and urinary leakage are the two main procedure-related renal complications of partial nephrectomy (53), and studies have shown that ERAS reduces the incidence of both complications, which is associated with detailed preoperative counseling and preoperative oral carbohydrates (54). Deep vein thrombosis is a serious life-threatening complication, and with its development associated with tumors, stress reactions due to surgical trauma, prolonged postoperative bed rest, and other risk factors. In the case of ERAS, it was able to reduce the stress response caused by the procedure and enable patients to get out of bed earlier, which in turn reduced the formation of deep vein thrombosis. In terms of medical costs of partial nephrectomy, both in China and in other countries they mainly include: medical care, nursing care, medication, blood, laboratory, radiology, inspection, pathology, housing, disposable material, anesthesia and operating room use. Compared to other countries, medical care and nursing care costs are lower in China, while disposable material and medication costs are higher, probably because disposable supplies and medications are mainly imported into China. A study from China showed that disposable consumables and drugs accounted for the largest share of hospitalization costs (55). ERAS can further reduce the use of drugs and disposable supplies by facilitating rapid postoperative recovery and reducing surgical complications, thereby reducing the cost of hospitalization for patients. This study likewise showed that ERAS did not increase patients’ hospital costs, but instead reduced them by 0.82 million RMB (WMD = -0.82, 95% CI: -1.20 to -0.43, p < 0.001), which, in addition to the previously stated reasons, was closely associated with a shorter hospital stay (56). Therefore, ERAS is very helpful for patients with renal tumors requiring partial nephrectomy worldwide, especially those coming from low- and middle-income countries.
The strengths of this study are the search of eight major databases to ensure that no relevant articles were missed, the inclusion of a relatively large number of randomized controlled trials and a large sample size, and the fact that the pooled results were shown to be stable after sensitivity analysis, which provides reliable evidence for the results of this study. Nevertheless, there are some limitations in this study. In the first place, most of the included studies were from China, and the findings could not be well generalized to other regions, probably because the implementation of care for partial nephrectomy in China was performed in the hospital, whereas in other regions, care continued in the community with early discharge (57). Therefore, more high-quality randomized controlled studies are still needed worldwide. As the second, because the outcome indicators such as time to first postoperative bed activity, time to first postoperative anal exhaust, time to first postoperative bowel movement, time to first postoperative meal, time to drainage tube removal, and time to catheter removal in the included literature were not in consistent units, the standardized mean difference (SMD) was used as the effect indicator, making the data results only provide qualitative clinical significance. The third one is that the heterogeneity of the outcome indicators, except for total postoperative complications, postoperative hemorrhage, postoperative leakage, and deep vein thrombosis, was too high and remained high after subgroup analysis, which was considered to be caused by various factors such as study type, surgical approach, and surgical access. Finally, publication bias in time to first postoperative bed activity, time to first postoperative anal exhaust, time to first postoperative feeding, time to catheter removal, and time to drainage tube removal may be due to a combination of small sample sizes in some studies, unavailability of data from some studies, failure of some studies to report the above outcome indicators, duplication of publication in national and international journals by some authors, and the fact that negative results are not easily published.
ERAS is safe and effective in partial nephrectomy of renal tumors. In addition, ERAS can improve the turnover rate of hospital beds, reduce medical costs and improve the utilization rate of medical resources.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
WW, LT, and MX contributed to conception and design of the study. ZD organized the database. WW, LT, and MX performed the statistical analysis. WW wrote the first draft of the manuscript. ZC, WC, DZ, JT, and ZF wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1049294/full#supplementary-material
1. Motzer RJ, Jonasch E, Agarwal N, Alva A, Baine M, Beckermann K, et al. Kidney cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw (2022) 20(1):71–90. doi: 10.6004/jnccn.2022.0001
2. Xia C, Dong X, Li H, Cao M, Sun D, He S, et al. Cancer statistics in China and united states, 2022: profiles, trends, and determinants. Chin Med J (Engl) (2022) 135(5):584–90. doi: 10.1097/CM9.0000000000002108
3. Mir MC, Derweesh I, Porpiglia F, Zargar H, Mottrie A. Autorino r. partial nephrectomy versus radical nephrectomy for clinical T1b and T2 renal tumors: A systematic review and meta-analysis of comparative studies. Eur Urol (2017) 71(4):606–17. doi: 10.1016/j.eururo.2016.08.060
4. Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg (2002) 183(6):630–41. doi: 10.1016/s0002-9610(02)00866-8
5. Prionas A, Craddock C, Papalois V. Enhanced recovery after renal transplantation decreases recipients’ urological complications and hospital stay: A systematic review and meta-analysis. J Clin Med (2021) 10(11):2286. doi: 10.3390/jcm10112286
6. Zhao Y, Zhang S, Liu B, Li J, Hong H. Clinical efficacy of enhanced recovery after surgery (ERAS) program in patients undergoing radical prostatectomy: a systematic review and meta-analysis. World J Surg Oncol (2020) 18(1):131. doi: 10.1186/s12957-020-01897-6
7. Williams SB, Cumberbatch MGK, Kamat AM, Jubber I, Kerr PS, McGrath JS, et al. Reporting radical cystectomy outcomes following implementation of enhanced recovery after surgery protocols: A systematic review and individual patient data meta-analysis. Eur Urol (2020) 78(5):719–30. doi: 10.1016/j.eururo.2020.06.039
8. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg (2010) 8(5):336–41. doi: 10.1016/j.ijsu.2010.02.007
9. Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev (2019) 10:ED000142. doi: 10.1002/14651858.ED000142
10. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol (2010) 25(9):603–5. doi: 10.1007/s10654-010-9491-z
11. Zhao LJ, Li P, Zhuang JL. The influence of ERAS concept on perioperative period of partial nephrectomy with nephron sparing. J Xuzhou Med Univ (2019) 39(3):212–6. doi: 10.3969/j.issn.2096-3882.2019.03.013
12. Gong T, Cao Y, Tang LP, Xiong ZF. Evaluation of the effectiveness of ERAS in patients undergoing robotic-assisted laparoscopic partial nephrectomy. Chin Gen Pract Nurs (2019) 17(6):723–6. doi: 10.12104/j.issn.1674-4748.2019.06.032
13. Chen QF, Jin L. The preventive effect of FTS on lower extremity venous thrombosis in patients after laparoscopic partial nephrectomy for renal tumors. Today Nurse (2019) 26(11):53–5.
14. Zhou QL. A study on the effectiveness of rapid rehabilitation care for patients undergoing partial nephrectomy. Contemp Med Forum (2021) 19(2):195–6. doi: 10.3969/j.issn.2095-7629.2021.02.142
15. Wu HL. Rapid perioperative rehabilitation care for robot-assisted posterior laparoscopic partial nephrectomy. China Pharm (2019) 28(S02):201–2. doi: 10.3969/j.issn.1006-4931.2019.Z2.146
16. Huang P, Huang L. Rapid rehabilitation care after robotic-assisted partial nephrectomy. For all Health (2017) 11(9):196.
17. Guo JM, Zhao K, Xing NZ, Wang ZL, Zhang ZL, Zhao HW, et al. Clinical study of retroperitoneal laparoscopic partial nephrectomy under accelerated rehabilitation surgery. J Urol Clin Electron Vers (2020) 12(01):32–8. doi: 10.3969/j.issn.1674-7410.2020.01.006
18. Shi Q, Deng ZX, Peng XX, Gu X, Wu YX, Guo BY, et al. Application of enhanced recovery after surgery in laparoscopic partial nephrectomy. J Clin Med Pract (2021) 25(06):34–37+41. doi: 10.7619/jcmp.20201522
19. Liu XF, Li FZ, Zhang QF, Jiang AH. The application of enhanced recovery after surgery in laparoscopic partial nephrectomy. Chin J Front Med Sci (2017) 9(07):20–3. doi: 10.12037/YXQY.2017.07-05
20. Zhao HW, Zhang QQ, Xie M, Wang K. Application of enhanced recovery after surgery in retroperitoneal laparoscopic partial nephrectomy. Chin J Front Med Sci (2017) 9(07):16–9. doi: 10.12037/YXQY.2017.07-04
21. Wang L, Li J, Yan SJ, Fu RR, Chai YY, Wang R. Accelerated rehabilitation surgery in the perioperative care of patients undergoing partial nephrectomy. Today Nurse (2019) 26(11):52–3.
22. Zhong LF, Peng LJ. Rapid rehabilitation concept in patients undergoing robotic-assisted partial nephrectomy. Electron J Pract Clin Nurs Sci (2020) 5(43):132,136.
23. Wang YH, Li Y. Rapid rehabilitation surgical care in the perioperative period of renal tumor resection with preserved renal units. China Med Eng (2017) 25(7):93–5. doi: 10.19338/j.issn.1672-2019.2017.07.029
24. Zeng XY, Zhong WY, Tan CM. Effectiveness of rapid rehabilitation surgical care in laparoscopic nephrectomy for renal tumors. Int J Nurs (2017) 36(21):2941–4. doi: 10.3760/cma.j.issn.1673-4351.2017.21.019
25. Gong J, Lu T. Rapid rehabilitation surgical care in posterior laparoscopic partial nephrectomy with preserved renal unit. J Contemp Urol Reprod Oncol (2018) 10(2):123–4. doi: 10.3870/j.issn.1674-4624.2018.02.015
26. Tu FZ. Effect of rapid rehabilitation surgical concept on early activity after laparoscopic partial nephrectomy. Our Health (2019) 16):9.
27. Xue MP, Wang CY, Hu WT. The effect of fast track surgery intervention in perioperative period of retroperitoneal laparoscopic partial nephrectomy. Modern Med J (2015) 43(12):1575–7. doi: 10.3969/j.issn.1671-7562.2015.12.032
28. Cheng C, Zhang LL, Zhang WT, Liu HN, Qi Y, Li JT, et al. The application study of concept of fast track surgery in nephron sparing surgery of perioperative period. J Shandong First Med Univ (2012) 33(09):641–6.
29. Song Z, Ding P, Cen T. Rapid recovery surgical concept in the perioperative period of laparoscopic preservation of renal units. J Clin Nurs (2012) 11(3):16–7. doi: 10.3969/j.issn.1671-8933.2012.03.006
30. Yao HQ. Application of rapid rehabilitation surgical concept in the care of patients undergoing posterior laparoscopic partial nephrectomy. Med Equip (2018) 31(8):152–3. doi: 10.3969/j.issn.1002-2376.2018.08.114
31. Hu YN. Application of rapid rehabilitation surgical concepts in the perioperative care of patients undergoing robotic-assisted post-laparoscopic partial nephrectomy. Shanghai Nurs (2018) 18(6):54–6. doi: 10.3969/j.issn.1009-8399.2018.06.016
32. Liao YQ, Liu QD. Application effect of rapid rehabilitation surgical nursing mode in patients with open renal tumor operation. China Mod Med (2018) 25(36):181–3. doi: 10.3969/j.issn.1674-4721.2018.36.057
33. Yang JC, Guo FF. Study on the application of enhanced recovery after surgery in laparoscopic partial nephrectomy in urology. World Latest Med Inform (2021) 21(18):37–9. doi: 10.3969/j.issn.1671-3141.2021.18.013
34. Ruan XG, Ran LX, Ji W, Li MJ, Liu Y. Effect of rapid rehabilitation surgery concept in patients with renal tumor who underwent laparoscopic partial nephrectomy. J Qilu Nurs (2022) 28(02):4–6. doi: 10.3969/j.issn.1006-7256.2022.02.002
35. Gu XY. Rapid rehabilitation care experience of robot-assisted partial nephrectomy. Orient Med Diet (2020) 16):135.
36. Huang JY, Zhang LH. Accelerated rehabilitation surgical concept in the perioperative period of posterior laparoscopic nephrectomy with preserved renal units. Today Nurse (2020) 27(11):84–6. doi: 10.19791/j.cnki.1006-6411.2020.31.033
37. He YQ, Yan SJ. Application of rapid rehabilitation surgical concept in perioperative care of laparoscopic partial nephrectomy. Chin Gen Pract Nurs (2017) 15(30):3763–4. doi: 10.3969/j.issn.1674-4748.2017.30.019
38. Liu Z, Wang Y. Study on the application of rapid rehabilitation concept to the recovery of gastrointestinal function in patients after laparoscopic partial nephrectomy. J Contemp Urol Reprod Oncol (2019) 11(2):114–6. doi: 10.3870/j.issn.1674-4624.2019.02.014
39. Kang C, Qiao X, Sun M. Application of fast-track surgery in the perioperative period of laparoscopic partial nephrectomy for renal tumors. J Int Med Res (2019) 47(6):2580–90. doi: 10.1177/0300060519847853
40. Lin C-H, Lin X-N, Lu Y-Y, Liu Q-Z, Men C-P, Gao Z-L, et al. Application value of enhanced recovery after surgery (ERAS) in laparoscopic nephron sparing surgery. Int J Clin Exp Med (2018) 11(7):7448–53.
41. Miao C, Yu A, Yuan H, Gu M, Wang Z. Effect of enhanced recovery after surgery on postoperative recovery and quality of life in patients undergoing laparoscopic partial nephrectomy. Front Oncol (2020) 10:513874. doi: 10.3389/fonc.2020.513874
42. Dominique I, Palamara C, Seizilles De Mazancourt E, Ecochard R, Hacquard H, Tremblais B, et al. Enhanced recovery after robot-assisted partial nephrectomy for cancer: Is it better for patients to have a quick discharge? Urol Int (2021) 105(5-6):499–506. doi: 10.1159/000505757
43. Xue X, Wang D, Ji Z, Xie Y. Enhanced recovery after surgery in patients undergoing laparoscopic partial nephrectomy. results from a real-world randomized controlled trial. Wideochir Inne Tech Maloinwazyjne (2022) 17(1):116–26. doi: 10.5114/wiitm.2021.108216
44. Chughtai B, Abraham C, Finn D, Rosenberg S, Yarlagadda B, Perrotti M. Fast track open partial nephrectomy: reduced postoperative length of stay with a goal-directed pathway does not compromise outcome. Adv Urol (2008) 2008:507543. doi: 10.1155/2008/507543
45. Nosov AK, Petrov SB, Lushina PA, Berkut MV, Semenov AV, Saad AE. Fast track for partial nephrectomy. Onkourologiya (2019) 15(3):47–55. doi: 10.17650/1726-9776-2019-15-3-47-55
46. Ripollés-Melchor J, Abad-Motos A, Zorrilla-Vaca A. Enhanced recovery after surgery (ERAS) in surgical oncology. Curr Oncol Rep (2022) 24(9):1177–87. doi: 10.1007/s11912-022-01282-4
47. Di Rollo D, Mohammed A, Rawlinson A, Douglas-Moore J, Beatty J. Enhanced recovery protocols in urological surgery: a systematic review. Can J Urol (2015) 22(3):7817–23.
48. Chen S, He Z, Yao S, Xiong K, Shi J, Wang G, et al. Enhanced recovery after surgery protocol optimizes results and cost of laparoscopic radical nephrectomy. Front Oncol (2022) 12:840363. doi: 10.3389/fonc.2022.840363
49. Letica-Kriegel AS, Salmasian H, Vawdrey DK, Youngerman BE, Green RA, Furuya EY, et al. Identifying the risk factors for catheter-associated urinary tract infections: a large cross-sectional study of six hospitals. BMJ Open (2019) 9(2):e022137. doi: 10.1136/bmjopen-2018-022137
50. Kranz J, Schmidt S, Wagenlehner F, Schneidewind L. Catheter-associated urinary tract infections in adult patients. Dtsch Arztebl Int (2020) 117(6):83–8. doi: 10.3238/arztebl.2020.0083
51. Yuan J, Sun Y, Pan C, Li T. Goal-directed fluid therapy for reducing risk of surgical site infections following abdominal surgery - a systematic review and meta-analysis of randomized controlled trials. Int J Surg (2017) 39:74–87. doi: 10.1016/j.ijsu.2017.01.081
52. Jessen MK, Vallentin MF, Holmberg MJ, Bolther M, Hansen FB, Holst JM, et al. Goal-directed haemodynamic therapy during general anaesthesia for noncardiac surgery: a systematic review and meta-analysis. Br J Anaesth (2022) 128(3):416–33. doi: 10.1016/j.bja.2021.10.046
53. Klatte T, Ficarra V, Gratzke C, Kaouk J, Kutikov A, Macchi V, et al. A literature review of renal surgical anatomy and surgical strategies for partial nephrectomy. Eur Urol (2015) 68(6):980–92. doi: 10.1016/j.eururo.2015.04.010
54. Smith MD, McCall J, Plank L, Herbison GP, Soop M, Nygren J. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Cochrane Database Syst Rev (2014) 8):CD009161. doi: 10.1002/14651858.CD009161
55. Jing X, Zhang B, Xing S, Tian L, Wang X, Zhou M, et al. Cost-benefit analysis of enhanced recovery after hepatectomy in Chinese han population. Med (Baltimore) (2018) 97(34):e11957. doi: 10.1097/MD.0000000000011957
56. Nazzani S, Preisser F, Mazzone E, Tian Z, Mistretta FA, Shariat SF, et al. In-hospital length of stay after major surgical oncological procedures. Eur J Surg Oncol (2018) 44(7):969–74. doi: 10.1016/j.ejso.2018.05.001
Keywords: renal tumors, partial nephrectomy, meta-analysis, enhanced recovery after surgery, systematic review
Citation: Wangjian W, Tianyi L, Xiaoqian M, Di Z, Chuan Z, Chao W, Zijian D, Tongtong J and Fenghai Z (2023) Application of enhanced recovery after surgery in partial nephrectomy for renal tumors: A systematic review and meta-analysis. Front. Oncol. 13:1049294. doi: 10.3389/fonc.2023.1049294
Received: 20 September 2022; Accepted: 19 January 2023;
Published: 09 February 2023.
Edited by:
Michael Poch, Moffitt Cancer Center, United StatesReviewed by:
Wesley Yip, Memorial Sloan Kettering Cancer Center, United StatesCopyright © 2023 Wangjian, Tianyi, Xiaoqian, Di, Chuan, Chao, Zijian, Tongtong and Fenghai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhou Fenghai, WmhvdWZlbmdoQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.