- 1Department of Urology, the First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, China
- 2Department of Pathology, the First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, China
- 3Department of Urology, Ganzhou People’s Hospital, Ganzhou, Jiangxi, China
Objectives: To compare the efficacy and safety of retroperitoneal laparoscopic adrenalectomy (RLA) and transperitoneal laparoscopic adrenalectomy (TLA) in the treatment of large (≥6cm) adrenal pheochromocytomas.
Methods: We retrospectively collected the clinical data of 130 patients with large pheochromocytoma who underwent RLA or TLA in our hospital from 2012 to 2022. The perioperative parameters and follow-up outcomes of the two groups were compared, and univariate and multivariate analyses were used to evaluate the risk factors of hemodynamic instability (HI).
Results: A total of 57 patients underwent TLA and 73 underwent RLA. There was no difference in demographic characteristics such as age, sex and tumor size between the two groups. Compared with the TLA group, patients in the RLA group had shorter operation time (P<0.001) and less estimated blood loss (EBL) (P<0.001). The time to ambulation, time to oral food and time to removal of drainage of RLA group were earlier than those of TLA group. In addition, the hospital stay was shorter in the RLA group than in the TLA group. There were no differences in HI, complications, or blood pressure (BP) improvement between the two groups. The mean follow-up time was 61.4 and 65.5 months, respectively, during which no tumors recurred or metastasized. Multivariate analysis showed that elevated hormone levels and larger tumor size were independent risk factors for HI.
Conclusions: Both RLA and TLA are effective treatment methods for large pheochromocytomas, but the perioperative outcomes of RLA are better than that of TLA. Our study demonstrates the superiority of RLA for the treatment of large pheochromocytomas.
Introduction
Pheochromocytoma is a neuroendocrine tumor, most of which arise from the adrenal medulla (1). The etiology of pheochromocytoma is not known, but studies have shown that about 10% of pheochromocytomas are genetically related (2). Pheochromocytoma patients often present with hypertension, headache, arrhythmia and other clinical manifestations, which are related to the large amount of catecholamines secreted by the tumor (3). Surgical removal of the tumor is considered to be the best treatment for pheochromocytoma because it not only removes the tumor but also improves the patient’s symptoms. However, the adrenal gland is located in the posterior abdominal cavity, which makes the operation more difficult. In addition, the removal of pheochromocytoma is a very difficult task because of the abundance of blood vessels and the increased secretion of catecholamines caused by surgical procedures (4).
Laparoscopic adrenalectomy has been the standard surgical procedure for small pheochromocytomas since it was first reported in 1992 (5). Because laparoscopic surgery is less traumatic and more elaborate, this makes it have an incomparable advantage of open surgery. Studies have shown that laparoscopic adrenalectomy has a shorter operative time, lower complication rate, and faster postoperative recovery than open adrenalectomy (6, 7). Laparoscopic adrenalectomy involves transperitoneal and retroperitoneal approaches, both of which have good results. Several studies have shown that retroperitoneal laparoscopic adrenalectomy (RLA) is superior to transperitoneal laparoscopic adrenalectomy (TLA) in a number of surgical indicators (8, 9). However, these studies involved small tumors, and the difference between TLA and RLA for large pheochromocytomas (≥6cm) is unclear. The purpose of this study was to compare the perioperative and follow-up outcomes of TLA and RLA in the treatment of large pheochromocytoma, so as to provide reference for the surgical treatment of large pheochromocytoma.
Methods
Patients
We retrospectively collected the clinical data of pheochromocytoma patients who underwent TLA or RLA in our hospital from January 2012 to July 2022. The inclusion criteria were as follows: maximum tumor diameter ≥6cm; the postoperative specimen was pathologically confirmed as pheochromocytoma. Exclusion criteria were as follows: bilateral lesions; patients who underwent an open surgery; patients who are unable to undergo laparoscopic approach due to anesthesiologic contraindications; pheochromocytoma originating from outside the adrenal gland; clinical data were incomplete. All the patients signed an informed consent form. Our study was approved by the Ethics Committee of the First Affiliated Hospital of Nanchang University.
Preoperative preparation
All patients underwent CT scan and ultrasound before operation. Baseline hormone levels were assessed in all patients before surgery. The evaluation content included cortisol, dopamine, norepinephrine, epinephrine, adrenocorticotropic hormone, and serum potassium. The levels of 24-h urinary dopamine, norepinephrine, epinephrine and vanillylmandelic acid were also evaluated. All patients were treated with oral α-receptor blockers for at least 2 weeks before surgery. Patients with tachycardia should also be treated with β-receptor blockers. All patients received intravenous fluids to expand their blood volume 3-5 days before surgery. Patients can undergo surgery when they meet the following criteria: blood pressure (BP) <140/90 mmHg, heart rate <100/min, haematocrit <45%, and warm fingertips.
Baseline data and outcome indicators
Data to be evaluated include patient demographics and perioperative outcomes. Demographic characteristics included gender, age, body mass index (BMI), hypertension, diabetes, arrhythmia, ASA score, hormone levels, tumor side, tumor size and CT findings. Perioperative indicators included operation Time, pneumoperitoneum time, estimated blood loss (EBL), hemodynamic instability (HI), time to ambulation, time to oral food, time to removal of drainage, postoperative hospital stay, complications, and BP improvement rate.
The ASA score was used to evaluate the patient’s tolerance to anesthesia. Complications were classified according to the Clavien-Dindo classification (10). HI was defined as intraoperative BP >180 mmHg or mean arterial pressure <60 mmHg (11). BP improvement was defined as a decrease in BP after surgery or a decrease in the dose or type of antihypertensive medication taken (12).
Surgical technique
The choice of surgical method is based on the wishes of the patient and the preferences of the surgeon. All the operations were performed by six senior surgeons from our department. The specific steps of TLA and RLA have been explained in detail in previous studies (9).
Follow-up
Follow-up was performed every 3 months during the first year after surgery and every 6 months thereafter. Follow-up included routine physical examination, hematology, hormone levels, and abdominal and chest imaging. For patients who could not come to our hospital for review, we all evaluated their health status by telephone.
Statistical analysis
All data in this study were statistically analyzed using IBM SPSS26.0. Continuous variables conforming to normal distribution were expressed as mean and standard deviation (SD), and comparisons between groups were performed using independent sample t-test. Continuous variables that did not conform to normal distribution were expressed as median and interquartile range (IQR), and comparison between groups was performed using the Mann-Whitney U test. Categorical variables were expressed as percentages, and comparisons between groups were performed using Pearson’s chi-square test. Univariate and multivariate logistic regression models were used to evaluate the risk factors for HI. A P value of <0.05 was considered statistically significant.
Results
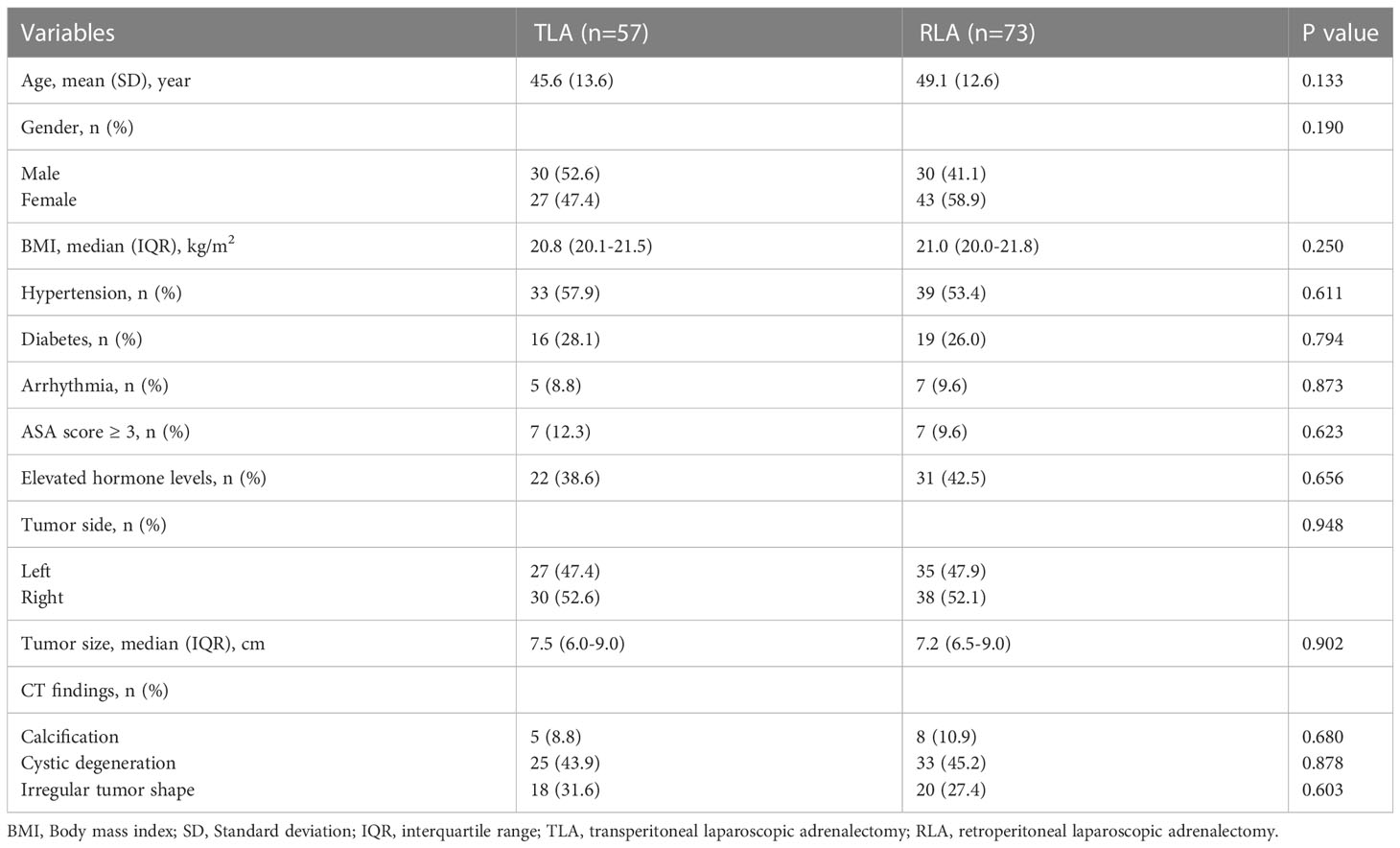
The preoperative characteristics of patients are summarized in Table 1. Fifty-seven patients underwent TLA and 73 underwent RLA. Overall, there were no differences in gender, age, BMI, Hypertension, Diabetes, Arrhythmia, ASA score ≥3, hormone levels, tumor side, tumor size and CT findings between the two groups.
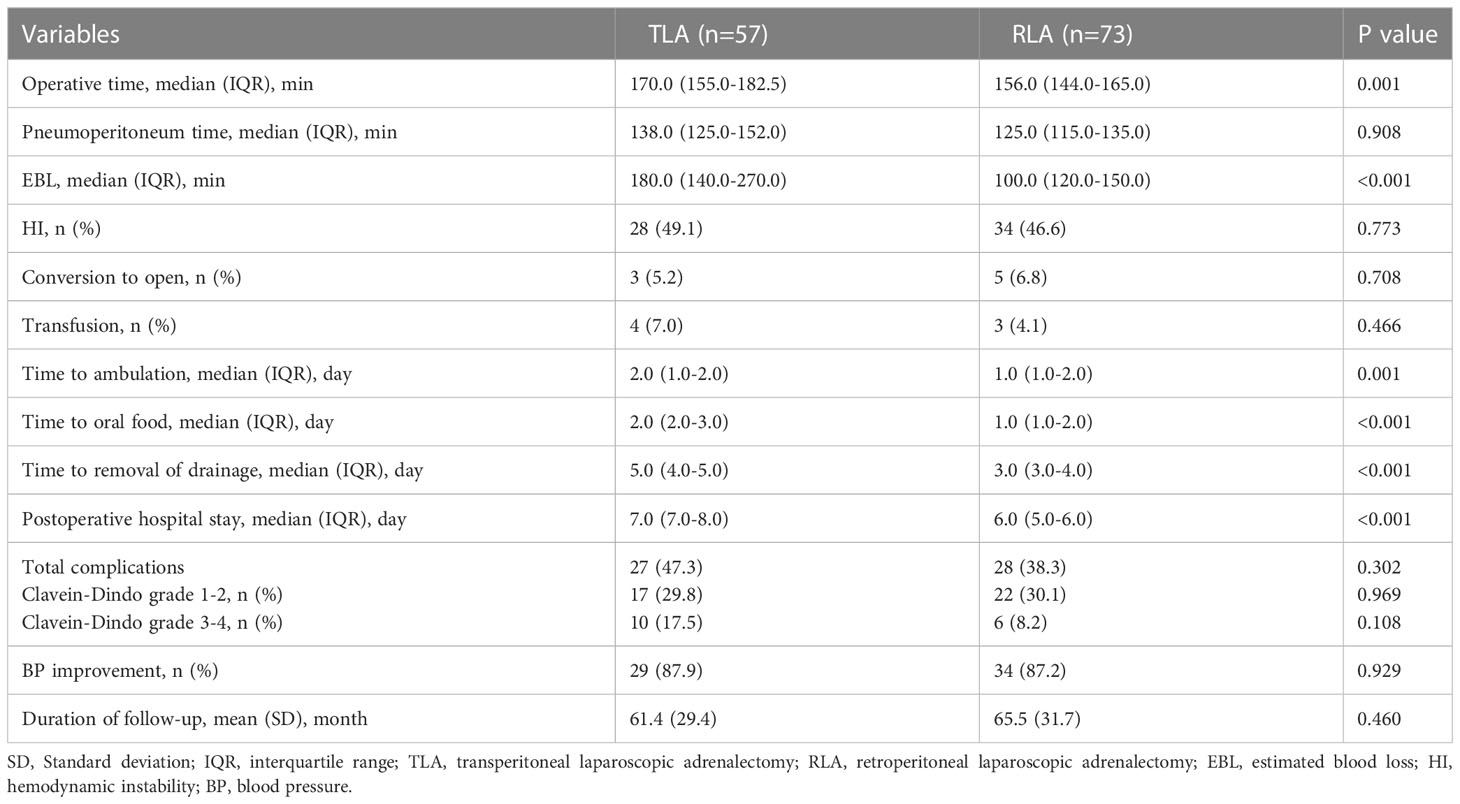
In terms of perioperative outcomes, the operative time was significantly shorter in the RLA group than in the TLA group (P=0.001). There was no difference in pneumoperitoneum time between the two groups. The RLA group had significantly less EBL than the TLA group (P <0.001). In addition, the time to ambulation, time to oral food and time to removal of drainage of the RLA group were shorter than those of the TLA group (all P <0.001). Compared with the TLA group, the postoperative hospital stay was significantly shorter in the RLA group (P<0.001). There were no significant differences in the incidence of complications or the rate of BP improvement between the two groups. The mean follow-up time was 61.4 (29.4) months in the TLA group and 65.5 (31.7) months in the RLA group. There was no tumor recurrence or metastasis in the two groups during the follow-up (Table 2).
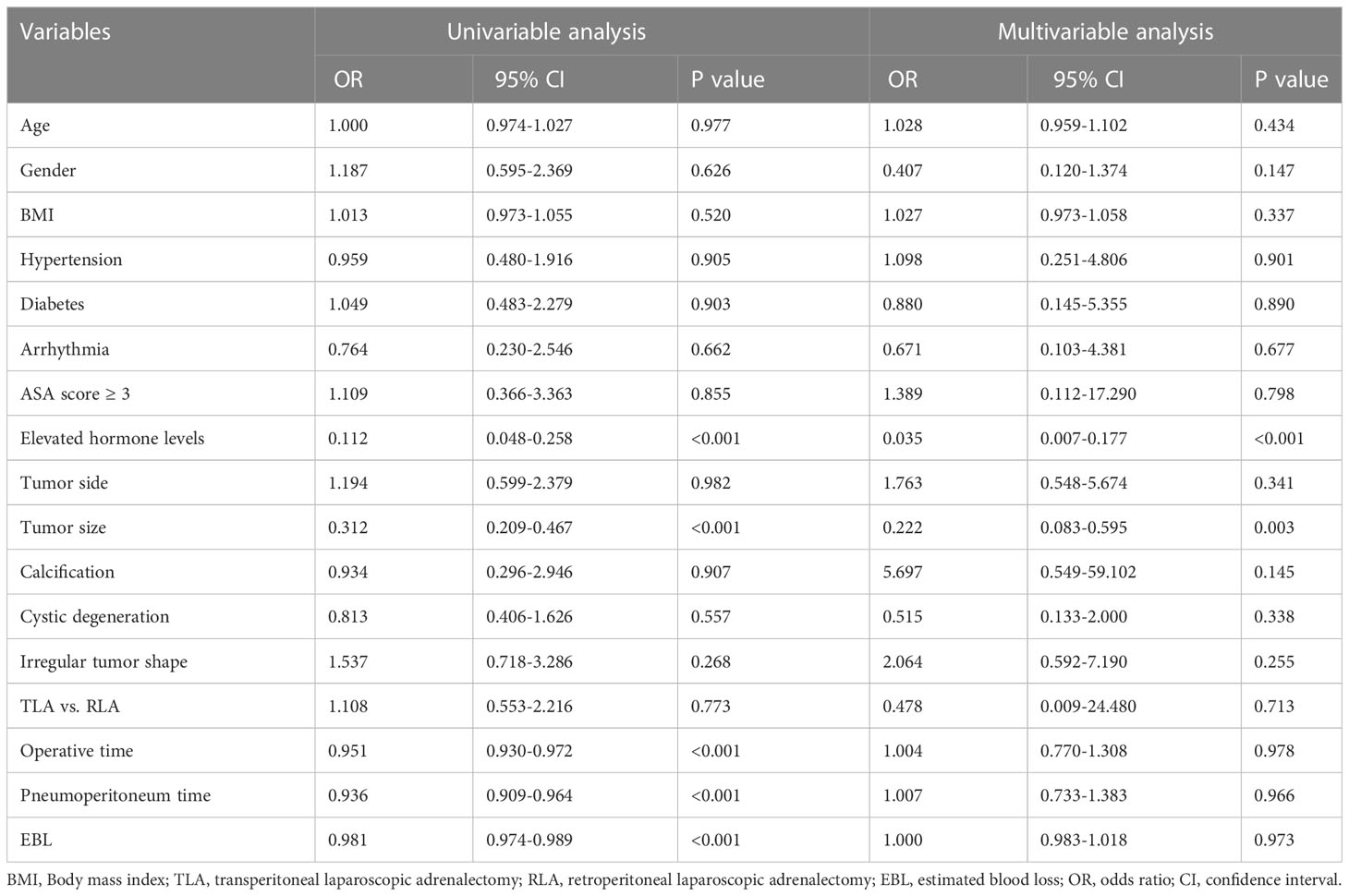
To assess the risk factors for intraoperative HI, logistic regression analysis was performed (Table 3). Univariate analysis showed that elevated hormone levels, larger tumor size, longer operation time and pneumoperitoneum time, and more EBL were risk factors for HI (all P <0.001). Multivariate analysis showed that elevated hormone levels and larger tumor size were independent risk factors for HI (P <0.001, P=0.003 respectively).
Discussion
The surgical treatment of adrenal pheochromocytoma is a very challenging task because of the special anatomical location of the adrenal gland, which makes it difficult for the surgeon to operate. In the past, removing the adrenal gland often required a large incision, even for small adrenal tumors. In addition, pheochromocytomas are very rich in blood vessels, often leading to severe bleeding during surgery. Moreover, because pheochromocytomas are neuroendocrine tumors that secrete large amounts of catecholamines, the surgeon’s compression of the tumor during surgical resection can cause severe HI (13, 14). The use of laparoscopy has solved all of these problems. First, the surgeon can remove the tumor without having to make a large incision. Secondly, the magnification function of laparoscopy enables the surgeon to better identify the blood vessels of the tumor, thus better hemostasis. In addition, compared with open surgery, laparoscopic resection of pheochromocytoma is performed more gently, thus avoiding the occurrence of HI (15). Robotic surgical systems overcome the limitations of laparoscopic surgery, such as two-dimensional imaging and surgeon discomfort. Robot-assisted laparoscopic adrenalectomy involves less EBL and faster postoperative recovery than laparoscopic adrenalectomy (16, 17). For large adrenal pheochromocytomas, many scholars believe that open surgery should be used, because they believe that these tumors tend to be malignant and that open surgery can facilitate a more complete resection of the tumor. In addition, the limited surgical space in the posterior abdominal cavity is not conducive to laparoscopic resection of large pheochromocytomas. However, several studies have shown that laparoscopic adrenalectomy is more effective and safer than open adrenalectomy for large adrenal pheochromocytoma (18, 19). The above findings provide a good basis for laparoscopic adrenalectomy in the treatment of large pheochromocytoma. Therefore, this study compared two approaches of laparoscopic adrenalectomy, namely TLA and RLA, in order to clarify the advantages and disadvantages of the two approaches, so as to provide reference for the surgical treatment of large pheochromocytoma.
The transperitoneal approach was the first approach to be used, and it was once the most popular approach. The transperitoneal approach offers more space for manoeuvre, a better vision, and a more defined anatomical structure, allowing the adrenal gland to be easily located. However, this approach inevitably affects the intestine and may result in intestinal adhesions. In addition, vital organs such as the liver and pancreas are also vulnerable to damage, which can lead to serious complications (20). The advantage of the retroperitoneal approach is that it avoids affecting organs such as the intestine, so patients recover more quickly after surgery. In addition, because this approach goes directly into the posterior abdominal cavity, where the adrenal gland is located, surgical time is saved. However, due to the limited space of the posterior abdominal cavity, the surgeon’s manipulation may be limited during the removal of large adrenal tumors (21). A retrospective study by Li et al. was the first to compare the perioperative outcomes of RLA and TLA for pheochromocytoma (8). Their study showed that the RLA group was superior to the TLA group in terms of operation time, EBL, postoperative hospital stay, and complications. However, their study only included patients with tumors smaller than 6cm, making it difficult to uncover the drawbacks of RLA. Shiraishi et al. compared the perioperative results of RLA and TLA in the treatment of pheochromocytoma larger than 5cm, and their findings also confirmed the superiority of RLA in terms of operation time, pneumoperitoneum time, and EBL (22). However, their study included only 22 patients, so the reliability of their findings may be limited. In the present study, the RLA group outperformed the TLA group on a number of perioperative indicators, such as shorter postoperative hospital stays in the RLA group than in the TLA group, which is similar to what has been reported. These advantages of RLA are related to the small impact on the intestine and other organs in the abdominal cavity, which makes patients less traumatic and recover faster after surgery. Although the limited space in the posterior abdominal cavity may prolong the operation time when removing large tumors, this did not occur in our study. This is because our center has been using this technology for a long time, so it has developed a skilled operation process. It can be seen that for experienced surgeons, the operation time will not be significantly prolonged even if the operating space is limited.
HI is one of the biggest challenges that surgeons face when removing pheochromocytoma because it can be life-threatening. Studies have shown that the incidence of HI during adrenalectomy ranges from 17 to 83%, which is generally consistent with our results (23). The occurrence of HI is related in tumor traction, therefore, gentle manipulation is the key to avoid HI. In addition, preoperative administration of α-receptor blockers and early adrenal central vein ligation prevented adverse cardiovascular and cerebrovascular events, although they did not reduce the frequency of HI (24). Once HI occurs, it is very important to use medicine promptly to keep the patient’s vital signs stable. Therefore, an experienced anesthesiologist is one of the keys to a successful pheochromocytoma resection (25). Our findings suggest that elevated hormone levels and larger tumor size were independent risk factors for HI during pheochromocytoma resection. According to previous studies, the development of HI is related to the size of the tumor, because the larger the tumor, the higher the level of catecholamines (26, 27). In addition, other studies have shown that the preoperative hormone level of patients is also one of the key factors affecting the occurrence of intraoperative HI, which is consistent with our findings (28, 29). Therefore, for large adrenal pheochromocytoma, surgeons should prevent the occurrence of HI to ensure patient safety.
Our study has several limitations. First, this study is a retrospective study. Secondly, the choice of surgical methods is based on the surgeon’s preference, which may lead to selection bias. Finally, although this is the largest study involving large pheochromocytoma patients to date, the number of cases is still limited, so we look forward to large randomized controlled trials in the future.
Conclusion
Both RLA and TLA are effective treatment methods for large pheochromocytoma, but the perioperative outcome of RLA is better than that of TLA. Larger tumor size and elevated hormone levels are independent risk factors for HI. Perfect preoperative preparation and gentle intraoperative operation are the key to prevent HI. Our study demonstrates the feasibility and superiority of RLA in the treatment of large adrenal pheochromocytoma.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
All the patients signed an informed consent form. Our study was approved by the Ethics Committee of the First Affiliated Hospital of Nanchang University.
Author contributions
KL and XW conceived the study. YL collected the data. WX, TS and ZY re-examined the data. KL and XW analyzed the data. KL, XW and ZY wrote the manuscript. MM and ZY reviewed the manuscript. ZY revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Science and Technology Plan of Jiangxi Provincial Health Commission (202210397).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lenders J, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet (London England) (2005) 366(9486):665–75. doi: 10.1016/s0140-6736(05)67139-5
2. Tanabe A, Naruse M. Recent advances in the management of pheochromocytoma and paraganglioma. Hypertension Res Off J Japanese Soc Hypertension (2020) 43(11):1141–51. doi: 10.1038/s41440-020-0531-0
3. Lenders J, Duh Q, Eisenhofer G, Gimenez-Roqueplo A, Grebe S, Murad M, et al. Pheochromocytoma and paraganglioma: An endocrine society clinical practice guideline. J Clin Endocrinol Metab (2014) 99(6):1915–42. doi: 10.1210/jc.2014-1498
4. Inabnet W, Pitre J, Bernard D, Chapuis Y. Comparison of the hemodynamic parameters of open and laparoscopic adrenalectomy for pheochromocytoma. World J Surg (2000) 24(5):574–8. doi: 10.1007/s002689910094
5. Gagner M, Lacroix A, Bolté E. Laparoscopic adrenalectomy in cushing's syndrome and pheochromocytoma. New Engl J Med (1992) 327(14):1033. doi: 10.1056/nejm199210013271417
6. Boylu U, Oommen M, Lee B, Thomas R. Laparoscopic adrenalectomy for Large adrenal masses: Pushing the envelope. J Endourol (2009) 23(6):971–5. doi: 10.1089/end.2008.0555
7. Heger P, Probst P, Hüttner F, Gooßen K, Proctor T, Müller-Stich B, et al. Evaluation of open and minimally invasive adrenalectomy: A systematic review and network meta-analysis. World J Surg (2017) 41(11):2746–57. doi: 10.1007/s00268-017-4095-3
8. Li Q, Li F. Laparoscopic adrenalectomy in pheochromocytoma: Retroperitoneal approach versus transperitoneal approach. J Endourol (2010) 24(9):1441–5. doi: 10.1089/end.2010.0065
9. Dickson P, Alex G, Grubbs E, Ayala-Ramirez M, Jimenez C, Evans D, et al. Posterior retroperitoneoscopic adrenalectomy is a safe and effective alternative to transabdominal laparoscopic adrenalectomy for pheochromocytoma. Surgery (2011) 150(3):452–8. doi: 10.1016/j.surg.2011.07.004
10. Dindo D, Demartines N, Clavien P. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg (2004) 240(2):205–13. doi: 10.1097/01.sla.0000133083.54934.ae
11. Vorselaars W, Postma E, Mirallie E, Thiery J, Lustgarten M, Pasternak J, et al. Hemodynamic instability during surgery for pheochromocytoma: Comparing the transperitoneal and retroperitoneal approach in a multicenter analysis of 341 patients. Surgery (2018) 163(1):176–82. doi: 10.1016/j.surg.2017.05.029
12. Fu S, Zhuang C, Yang X, Xie W, Gong B, Liu Y, et al. Comparison of robot-assisted retroperitoneal laparoscopic adrenalectomy versus retroperitoneal laparoscopic adrenalectomy for Large pheochromocytoma: A single-centre retrospective study. BMC Surg (2020) 20(1):227. doi: 10.1186/s12893-020-00895-5
13. Edwin B, Kazaryan A, Mala T, Pfeffer P, Tønnessen T, Fosse E. Laparoscopic and open surgery for pheochromocytoma. BMC Surg (2001) 1:2. doi: 10.1186/1471-2482-1-2
14. Lang B, Fu B, OuYang J, Wang B, Zhang G, Xu K, et al. Retrospective comparison of retroperitoneoscopic versus open adrenalectomy for pheochromocytoma. J Urol (2008) 179(1):57–60. doi: 10.1016/j.juro.2007.08.147
15. Eichhorn-Wharry L, Talpos G, Rubinfeld I. Laparoscopic versus open adrenalectomy: Another look at outcome using the clavien classification system. Surgery (2012) 152(6):1090–5. doi: 10.1016/j.surg.2012.08.020
16. Isiktas G, Nazli Avci S, Ergun O, Krishnamurthy V, Jin J, Siperstein A, et al. Laparoscopic versus robotic adrenalectomy in pheochromocytoma patients. J Surg Oncol (2022) 126(3):460–4. doi: 10.1002/jso.26918
17. Sforza S, Minervini A, Tellini R, Ji C, Bergamini C, Giordano A, et al. Perioperative outcomes of robotic and laparoscopic adrenalectomy: A Large international multicenter experience. Surg Endoscopy (2021) 35(4):1801–7. doi: 10.1007/s00464-020-07578-5
18. Zhu W, Wang S, Du G, Liu H, Lu J, Yang W. Comparison of retroperitoneal laparoscopic versus open adrenalectomy for Large pheochromocytoma: A single-center retrospective study. World J Surg Oncol (2019) 17(1):111. doi: 10.1186/s12957-019-1649-x
19. Shen W, Sturgeon C, Clark O, Duh Q, Kebebew E. Should pheochromocytoma size influence surgical approach? a comparison of 90 malignant and 60 benign pheochromocytomas. Surgery (2004) 136(6):1129–37. doi: 10.1016/j.surg.2004.05.058
20. Mohammadi-Fallah M, Mehdizadeh A, Badalzadeh A, Izadseresht B, Dadkhah N, Barbod A, et al. Comparison of transperitoneal versus retroperitoneal laparoscopic adrenalectomy in a prospective randomized study. J Laparoendoscopic Adv Surg Techniques Part A (2013) 23(4):362–6. doi: 10.1089/lap.2012.0301
21. Rubinstein M, Gill I, Aron M, Kilciler M, Meraney A, Finelli A, et al. Prospective, randomized comparison of transperitoneal versus retroperitoneal laparoscopic adrenalectomy. J Urol (2005) 174(2):442–5. doi: 10.1097/01.ju.0000165336.44836.2d
22. Shiraishi K, Kitahara S, Ito H, Oba K, Ohmi C, Matsuyama H. Transperitoneal versus retroperitoneal laparoscopic adrenalectomy for Large pheochromocytoma: Comparative outcomes. Int J Urol Off J Japanese Urol Assoc (2019) 26(2):212–6. doi: 10.1111/iju.13838
23. Scholten A, Vriens M, Cromheecke G, Borel Rinkes I, Valk G. Hemodynamic instability during resection of pheochromocytoma in men versus non-men patients. Eur J Endocrinol (2011) 165(1):91–6. doi: 10.1530/eje-11-0148
24. Wang W, Li P, Wang Y, Wang Y, Ma Z, Wang G, et al. Effectiveness and safety of laparoscopic adrenalectomy of Large pheochromocytoma: A prospective, nonrandomized, controlled study. Am J Surg (2015) 210(2):230–5. doi: 10.1016/j.amjsurg.2014.11.012
25. Conzo G, Musella M, Corcione F, De Palma M, Ferraro F, Palazzo A, et al. Laparoscopic adrenalectomy, a safe procedure for pheochromocytoma. a retrospective review of clinical series. Int J Surg (London England) (2013) 11(2):152–6. doi: 10.1016/j.ijsu.2012.12.007
26. Namekawa T, Utsumi T, Kawamura K, Kamiya N, Imamoto T, Takiguchi T, et al. Clinical predictors of prolonged postresection hypotension after laparoscopic adrenalectomy for pheochromocytoma. Surgery (2016) 159(3):763–70. doi: 10.1016/j.surg.2015.09.016
27. Pisarska M, Pędziwiatr M, Budzyński A. Perioperative hemodynamic instability in patients undergoing laparoscopic adrenalectomy for pheochromocytoma. Gland Surg (2016) 5(5):506–11. doi: 10.21037/gs.2016.09.05
28. Kramer C, Leitão C, Azevedo M, Canani L, Maia A, Czepielewski M, et al. Degree of catecholamine hypersecretion is the most important determinant of intra-operative hemodynamic outcomes in pheochromocytoma. J Endocrinol Invest (2009) 32(3):234–7. doi: 10.1007/bf03346458
Keywords: pheochromocytoma, RLA, TLA, hemodynamic instability, preoperative preparation
Citation: Lei K, Wang X, Yang Z, Liu Y, Sun T, Xie W and Ma M (2023) Comparison of the retroperitoneal laparoscopic adrenalectomy versus transperitoneal laparoscopic adrenalectomy for large (≥6cm) pheochromocytomas: A single-centre retrospective study. Front. Oncol. 13:1043753. doi: 10.3389/fonc.2023.1043753
Received: 14 September 2022; Accepted: 09 February 2023;
Published: 22 February 2023.
Edited by:
Marta Araujo-Castro, Ramón y Cajal University Hospital, SpainReviewed by:
Simone Sforza, University of Florence, ItalyKenichiro Ikeda, Hiroshima University, Japan
Copyright © 2023 Lei, Wang, Yang, Liu, Sun, Xie and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhongsheng Yang, ndyangzhongsheng@163.com
†These authors have contributed equally to this work
 Kunyang Lei
Kunyang Lei Xu Wang
Xu Wang Zhongsheng Yang3*†
Zhongsheng Yang3*†