- 1Department of Urology, The No. 1 People’s Hospital of Pinghu, Pinghu, China
- 2Department of Urology, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, China
Rationale: Primary renal parenchymal squamous cell carcinoma (SCC) is an extremely rare tumor that is difficult to diagnose by hematology and imaging studies and is often diagnosed later than other primary renal cancers.
Diagnosis: A 52-year-old male patient was found to have cysts in both kidneys for 1 week. No urgency and frequency of urination, no dysuria, no gross hematuria, and no significant changes in recent body weight were reported.
Interventions: The upper pole of the right kidney is a cystic and solid mass (8.3 cm * 8.2 cm * 8.1 cm), the cystic part has long T1 and long T2 signals, the solid part has mixed signals, and some parts have limited diffusion. There were nodular long T1 and short T2 calcification signals. An enhanced scan of the solid part showed uneven enhancement and continuous enhancement of the mass capsule. Cystic renal cancer was considered because of the multiple cysts in both kidneys. Surgical treatment was performed. Postoperative pathology revealed well-differentiated squamous cell carcinoma of the right kidney with cystic degeneration, 8.5 cm * 6 cm in size, infiltrating the renal parenchyma, and the cutting edge was negative. The pathological stage was pT2bN0M0.
Outcome: At the follow-up 5 months after the operation, no metastasis was found.
Conclusion: Renal SCC is rare and easily misdiagnosed and missed. Pathological diagnosis is still the gold standard for its diagnosis. However, with active surgical treatment, the short-term prognosis of the patient is good.
1 Introduction
Primary renal parenchymal squamous cell carcinoma (SCC) is an extremely rare tumor that is difficult to diagnose by hematology and imaging studies and is often diagnosed later than other primary renal cancers. This article reports a case of squamous cell carcinoma originating in the renal parenchyma. After active surgical treatment, the postoperative recovery was good, but the prognosis still needs long-term follow-up.
2 Case presentation
This human study was approved by The Second Affiliated Hospital of Zhejiang University School of Medicine Institutional Review Board, and the patient provided informed consent for the publication of the case.
A 52-year-old male patient was admitted to the hospital on 4 January 2022 for “one week of renal cyst found in physical examination”. One week prior, the patient went to the hospital for a physical examination. Abdominal B-ultrasound showed that there were multiple cysts in both kidneys, including a larger right kidney with calcification of the cyst wall and multiple calcifications. Further enhanced CT scan of the kidney revealed cystic solid lesions of the right kidney with multiple calcifications. There was no acute urination, no dysuria, and no gross hematuria. There had been no recent significant change in body weight. Upon physical examination, no obvious mass was found in the waist and abdomen, and there was no percussion pain in the renal region. There was no abnormality in routine hematuria and renal function. The tumor markers were as follows: squamous cell carcinoma antigen (SCCA) 4.1 μg/ml, alpha-fetoprotein (AFP) 3.6 ng/ml, carcinoembryonic antigen (CEA) 3.3 ng/ml, renal contrast-enhanced MR revealing a cystic solid mass in the right upper pole (8.3 cm * 8.2 cm * 8.1 cm), the signal of the solid part was mixed, the solid part was inhomogeneously enhanced, and the capsule of mass was continuously enhanced. Cystic renal carcinoma and multiple renal cysts were considered. Emission computed tomography (Ect) examination: mild-to-moderate reduction of left renal function and a right renal cyst. Right upper pole renal cell carcinoma was considered. On 6 January 2022, a robot-assisted partial nephrectomy was performed under general anesthesia. The patient was placed in the left lateral position, a channel was established in the posterior peritoneum, and the extraperitoneal fat and perirenal fascia were cleaned. It was found that the tumor was located in the upper pole of the kidney, protruding from the surface of the kidney, approximately 8 cm * 8 cm in size, was cystic solid, and had no obvious adhesion to the surrounding area. The tumor was completely resected with scissors along the surface of the tumor, 0.5 cm away from the edge of the tumor. The gross specimen revealed well-differentiated squamous cell carcinoma of the right kidney with cystic change, 8.5 cm * 6 cm in size, infiltrating the renal parenchyma, with the negative cutting edge of the broken end. Pathological diagnosis was pT2bN0M0. Immunohistochemistry showed Pax-8 (+), CK5/6 (+), P40 (+), p63 (+), and GATA-3 (partial +). Gene detection revealed that there was no first-order variation with clear clinical significance and nine secondary variants with potential clinical significance (ARID1A p.P1207fs, FAT1 p.Q961X, FBXW7 p.S92X, FGFR3 p.S249C, KMT2D p.L4152fs, KMT2D p.P4324fs, NFE2L2 p.L30F, PIK3CA p.E545K, and TERT c.-124G>A). Five months after the operation, a CT examination showed no local or retroperitoneal metastasis. Tumor markers were as follows: SCCA 0.8 μg/ml, AFP 2.0 ng/ml, and CEA 1.2 ng/ml.
3 Discussion
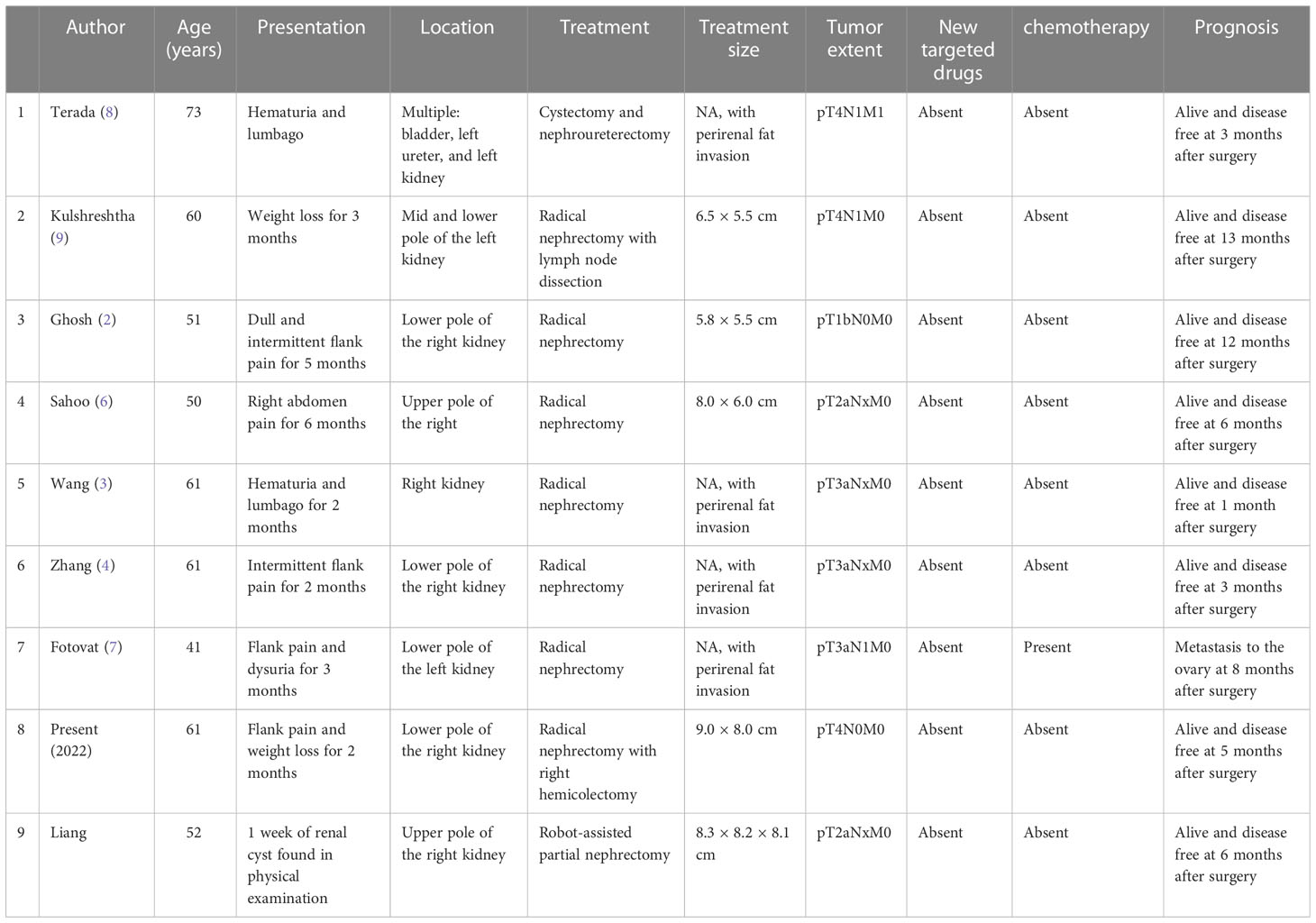
Primary squamous cell carcinoma of the kidney is a rare urological tumor, accounting for 0.5%–0.8% of renal malignancies (1), including renal pelvis SCC and renal SCC. There are more and more reports on renal pelvis SCC in clinical practice. Most experts believe that long-term renal pelvic stones, chronic pelvic inflammatory reaction, and hydronephrosis are the main reasons for inducing SCC (2–4). There are also reports that chemical substances (including drug abuse), hormone imbalance in the body, vitamin A deficiency, and chronic inflammatory reactions of renal transplantation are all potential causes (5). With the deepening of research, renal pelvis SCC is considered to be caused by urothelial metaplasia (6). Primary renal parenchyma SCC is extremely rare. So far, only nine cases including this case have been reported (2–4, 6–10) Table 1. The mechanism of the disease is not clear.
The onset of primary renal SCC is insidious, with no obvious symptoms, typical signs, and imaging manifestations in the early stage. It is often covered by hydronephrosis, calculus, or inflammation, which is easy to be misdiagnosed and missed. Compared with other types of tumors, it is often diagnosed later (11). According to the reported primary renal SCC, 88.89% (8/9) patients had lumbar and abdominal pain, and 22.22% (2/9) had hematuria. There was no significant difference in the incidence rate between sexes (5 men and 4 women). The most common tumors were on the right side (6/9 cases) and the inferior pole (5/9 cases). Although two cases were associated with renal calculi, the histology of the renal pelvis system was normal in all cases. More than half of the cases (5/9) were in the advanced stage (higher than pT3), and two cases had lymph node metastasis, which led to a worse prognosis. The patient was diagnosed with a renal cyst upon physical examination, and the tumor did not invade the collection system. FDG-PET/CT result was improved, and the possibility of metastatic renal SCC was excluded. However, FDG-PET/CT was not effective in distinguishing renal inflammatory diseases from various types of tumors (3). SCCA is a tumor-associated antigen extracted from cervical squamous cell carcinoma. It has certain clinical value in the diagnosis and monitoring of tumor recurrence of squamous cell carcinoma (12). With textual research considering the non-specific characteristics of the case, it is difficult to make a definite diagnosis before the operation. For imaging findings of renal tumors, a biopsy can be performed to confirm the diagnosis. Ureteroscopy and urine cytology are helpful in the diagnosis of renal pelvis SCC or invasive lesions.
For primary renal SCC, a pathological examination is still the gold standard for diagnosis. As it is not sensitive to chemoradiotherapy, radical nephrectomy is recommended for treatment, and surgery is also the most effective way for patients with local metastasis. All reported cases were followed up for an average of 4.22 months, and all patients survived. Only one pT3aN1 patient had ovarian metastasis (7). The patient was followed up for 0.5 years. There were no signs of recurrence and metastasis, indicating that early diagnosis and early treatment of renal SCC can achieve a better curative effect, but it is still lacking long-term follow-up verification. If the tumor relapses, there are still many targeted drugs to choose from according to the results of gene detection. Examples include bevacizumab combined with everolimus (T3A), sunitinib (T3A), temsirolimus (T3B), and mTOR inhibitors (sirolimus, everolimus, and T4) (based on the patient’s gene detection).
4 Conclusion
Primary renal parenchymal SCC is a very rare tumor, and at hematological and imaging examinations, diagnosis is difficult, compared with other primary renal cell carcinomas, and its diagnosis is often late. There is still no unified treatment plan, surgery is still the main choice, and new targeted drugs also provide individualized schemes, but their efficacy still lacks clinical follow-up verification.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Materials. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the First People’s Hospital of Pinghu City. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Conceptualization: KL. Investigation: KL. Supervision: YY. Writing—original draft: KL. Formal analysis: BL. Funding support: ZK. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer XH declared a shared affiliation with the authors YY and BL to the handling editor at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1037156/full#supplementary-material
Abbreviations
SCC, squamous cell carcinoma.
References
1. Li MK, Cheung WL. Squamous cell carcinoma of the renal pelvis. J Urol (1987) 138(2):269–71. doi: 10.1016/S0022-5347(17)43116-8
2. Ghosh P, Saha K. Primary intraparenchymal squamous cell carcinoma of the kidney: a rareand unique entity. Case Rep Pathol (2014) 2014:1–3. doi: 10.1155/2014/256813
3. Wang Z, Yan B, Wei YB, Hu NA, Shen Q, Li D, et al. Primary kidney parenchyma squamous cell carcinoma mimicking xanthogranulomatous pyelonephritis: a case report. OncolLett (2016) 11(3):2179–81. doi: 10.3892/ol.2016.4200
4. Zhang X, Zhang Y, Ge C, Zhang J, Liang P. Squamous cell carcinoma of the renal parenchyma presentingas hydronephrosis: A case report and review of the recent literature. BMC Urol (2020) 20(1):107. doi: 10.1186/s12894-020-00676-5
5. Bandyopadhyay R, Biswas S, Nag D, Ghosh AK. Squamous cell carcinoma of the renal pelvis presenting as hydronephrosis. J Cancer Res Ther (2010) 6(4):537–539. doi: 10.4103/0973-1482.77060
6. Sahoo TK, Das SK, Mishra C, Dhal I, Nayak R, Ali I, et al. Squamous cell carcinoma of kidney and its prognosis: A case report and review of the literature. Case Rep Urol (2015) 2015:469327. doi: 10.1155/2015/469327
7. Fotovat A, Gheitasvand M, Amini E, Ayati M, Nowroozi MR, Sharifi L. Primary squamous cell carcinoma of renal parenchyma: case report and review of literature. Urol. Case Rep (2021) 37:101627. doi: 10.1016/j.eucr.2021.101627
8. Terada T. Synchronous squamous cell carcinoma of the kidney, squamous cell carcinoma of the ureter, and sarcomatoid carcinoma of the urinary bladder: a case report. Pathol Res.Pract. (2010) 206(6):379–383. doi: 10.1016/j.prp.2009.07.021
9. Kulshreshtha P, Kannan N, Bhardwaj R, Batra S. Primary squamous cell carcinoma of the renal parenchyma. Indian J Pathol Microbiol (2012) 55(3):370–1. doi: 4103/0377-4929.101747
10. Cko A, Jyk B. Primary squamous cell carcinoma of the kidney parenchyma with ascending colon invasion: A case report and literature review - ScienceDirect. Int J Surg Case Rep (2022) 91:106762. doi: 10.1016/j.ijscr.2022.106762
11. Mizusawa H, Komiyama I, Ueno Y, Maejima T, Kato T. Squamous cell carcinoma in the renal pelvis of a horseshoe kidney. Int.J.Urol (2004) 11(9):782–84. doi: 10.1111/j.1442-2042.2004.00873.x
12. Qi C, He S, Cai L, Zhang L, Ding H, Chen Y, et al. A study on the clinical value of (18)F-fluorodeoxyglucose positron emission tomography/computed tomography combined with serum squamous cell carcinoma antigen in diagnosing recurrence/metastases in patients with early metaphase cervical cancer. Oncol Lett (2021) 22:746. doi: 10.3892/ol.2021.13007
Keywords: carcinoma, squamous cell carcinoma, renal parenchyma, pathology, prognosis
Citation: Liang K, Yuan Y, Lv B and Ke Z (2023) Primary squamous cell carcinoma of renal parenchyma: A case report and literature review. Front. Oncol. 13:1037156. doi: 10.3389/fonc.2023.1037156
Received: 05 September 2022; Accepted: 20 March 2023;
Published: 30 March 2023.
Edited by:
Maribel Acién, Miguel Hernández University of Elche, SpainReviewed by:
Wen Jie Huang, Zhejiang Chinese Medical University, ChinaXiaojun Huang, Zhejiang University, China
Bannakij Lojanapiwat, Chiang Mai University, Thailand
Copyright © 2023 Liang, Yuan, Lv and Ke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zunjin Ke, a2V6dW5qaW4xOTcyQDEyNi5jb20=
 Ke Liang
Ke Liang Yichu Yuan2
Yichu Yuan2