- 1Department of Thoracic Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences, and Peking Union Medical College, Beijing, China
- 2Department of Medical Oncology, Yancheng No. 1 People’s Hospital, Yancheng, Jiangsu, China
- 3Department of Medical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences, and Peking Union Medical College, Beijing, China
- 4Department of Pathology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences, and Peking Union Medical College, Beijing, China
In recent decades, multiple primary lung cancer (MPLC) has been increasingly prevalent in clinical practice. However, many details about MPLC have not been completely settled, such as understanding the driving force, clinical management, pathological mechanisms, and genomic architectures of this disease. From the perspective of diagnosis and treatment, distinguishing MPLC from lung cancer intrapulmonary metastasis (IPM) has been a clinical hotpot for years. Besides, compared to patients with single lung lesion, the treatment for MPLC patients is more individualized, and non-operative therapies, such as ablation and stereotactic ablative radiotherapy (SABR), are prevailing. The emergence of next-generation sequencing has fueled a wave of research about the molecular features of MPLC and advanced the NCCN guidelines. In this review, we generalized the latest updates on MPLC from definition, etiology and epidemiology, clinical management, and genomic updates. We summarized the different perspectives and aimed to offer novel insights into the management of MPLC.
Introduction
Lung cancer is the most fatal malignancy globally, significantly burdening the public health system (1). In recent decades, lung cancer risk has increased along with the prolonged lifespan of people (2). Meanwhile, the prevalence of low-dose computed tomography (LDCT) lung cancer screening programs boosted lung cancer diagnosis (3).
Multiple primary lung cancer (MPLC), indicating patients with multiple tumor sites of independent origins in the lung, which can be synchronous or metachronous (4), is becoming a common phenomenon in clinical practice. In 1975, Martini and Melamed outlined the first clinical and pathological criteria for MPLC (M-M criteria) based on 108 cases (5). Based on the M-M criterion, many researchers have put much effort into this kind of disease.
The definite etiology and epidemiology of this disease remain unclear, although previous studies have reported that smoking (6), field cancerization (7–9), and familial heredity (10) were factors tightly associated with the initiation of MPLC. Moreover, choosing the best therapy, studying genomic mutations and architectures (11), distinguishing intrapulmonary metastasis (IPM) from MPLC (12), and understanding the tumor microenvironment of MPLC (13) are still research hotspots.
What we know about the MPLC is far from enough. From the perspective of diagnosis and clinical management, distinguishing MPLC from IPM is vital and may seriously affect the treatment strategy. Nowadays, preoperative imaging evidence can no longer accurately distinguish these two diseases. Therefore, distinguishing MPLC from IPM always expects genomic technology (14–16). Besides, surgical resection is still the mainstream treatment choice for MPLC patients. Researchers spent years searching for the best surgical time and resection strategy for patients (17). However, for patients who are not suitable for surgery, non-operative therapy such as image-guided thermal ablation (IGAB) and stereotactic ablative radiotherapy (SABR) were considered (18–20). And in recent years, immunotherapy for multiple GGOs (ground glass opacities) attracted much attention, while the curative effect is not ideal (21, 22). From the perspective of genomic profiling, several previous researchers have reported the enormous genetic heterogeneity among the multiple lesions of MPLC using next-generation sequencing (11, 15, 23). Moreover, exploring the origin and initiation mechanisms of MPLC will also need the help of genomic profiling or other technologies such as RNA sequencing and single-cell sequencing (24).
In this review, we will give a comprehensive scenario of MPLC. We tried to generalize the latest updates on MPLC from definition, etiology and epidemiology, clinical management, and genomic updates. And we hope our work can open novel avenues for the major concerns of MPLC and advance the management of this unsolved disease.
Definition of MPLC
The definition and staging process of MPLC started with Martini and Melamed. They outlined the first clinical and pathological criteria for MPLC (M-M criteria) (5). In the M-M criteria, for synchronous MPLC, tumors should be physically separate, histologically identical, or different. If the tumors were the same histologically, they should originate from carcinoma in situ or without metastases. For metachronous MPLC, the tumors could be histologically heterogeneous or the same. If they were of the same histology, the intervals should be at least two years, or the tumors were physically distinct and without metastases, or they should originate from carcinoma in situ. The M-M criteria were used for 20 years until the revised definition of MPLC was brought up by Antakli et al. (25) in 1995. The underlying logic of the M-M criteria and Antakli’s standard were similar, while Antakli was more concise. In 2016, the International Association for the Study of Lung Cancer (IASLC) classified multifocal lung nodules into four types based on histology judgment, clinical information (including lesion location and radiologic features), and prognosis (26): Type I-Second primary lung cancers, Type II-Separate tumor nodules (intrapulmonary metastasis), Type III-Multifocal lung adenocarcinoma with ground glass/lepidic features, and Type IV-Pneumonic-type lung adenocarcinoma. Most clinicians classified second primary lung cancers (Type I) and Multifocal lung adenocarcinoma with ground glass/lepidic feature (Type III) into MPLC. In second primary lung cancers (Type I), each tumor is of independent biological origin. Thus, in clinical practice, separate T, N, and M stage should be determined for each lesion, like individual tumors. For multifocal lung adenocarcinoma with ground glass/lepidic feature (Type III), which belongs to ground-glass opacity (GGO), IASLC suggested assigning the T stage according to the highest T lesions and the N and M stages for all lesions collectively, and we summarized the criteria identifying them in Table 1. So far, the current classification of MPLC from IASLC has been widely accepted, offering much support for establishing the diagnosis criteria for MPLC. In 2022, the NCCN guidelines (NSCLC Version 3.2022) emphasized that the MPLC diagnosis requires a multidisciplinary setting involving surgeons, pathologists, radiation oncologists, and medical oncologists. In addition, they suggested some approaches to distinguish MPLC and IPM, which will be discussed later in this review.
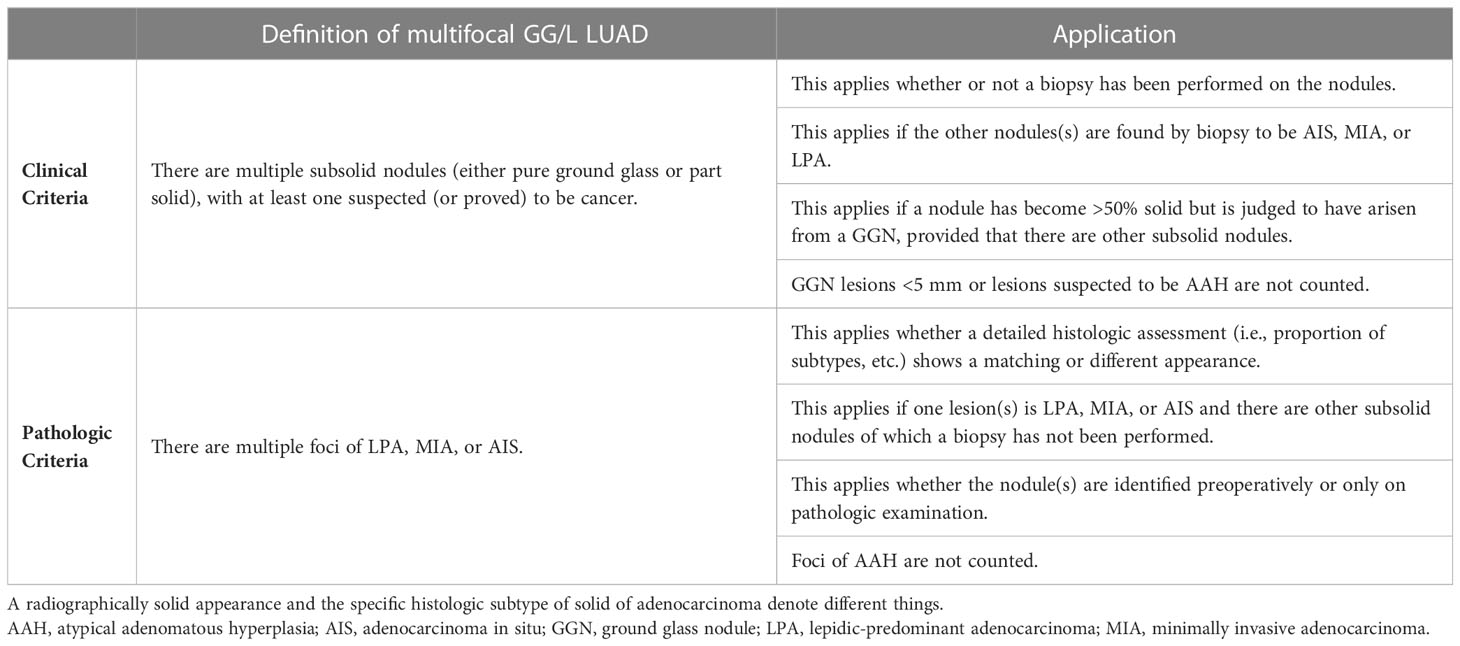
Table 1 Multifocal ground glass/lepidic lung adenocarcinoma diagnosis criteria according to the 8th edition of TNM classification.
Distinguishing MPLC from IPM
In the process of defining MPLC, IPM diagnosis is often accompanied. Although the M-M criteria involve pathological diagnosis, it is still important to distinguish between MPLC and IPM before treatment. If MPLC is wrongly diagnosed as IPM, the patient may lose the opportunity for surgery or receive chemical and radiation damage caused by unnecessary doses (27). Conversely, if IPM is diagnosed as MPLC, the patient’s survival will be affected (11). Previously, the differential diagnosis of MPLC and IPM was mainly based on histopathological evidence. However, the accuracy of pathological diagnosis is limited, and the accuracy of the M-M standard has been proven to be relatively low (28). The pathological diagnosis standard proposed by Girard et al. in 2009 is considered as accurate as 91% and received wide acceptance (28, 29). Since the diffusion of next-generation sequencing, the diagnosis at the gene level is indispensable to distinguishing the two diseases. We will elaborate these topics more specifically in the following article.
Etiology and epidemiology
The hypotheses of MPLC etiology are various. Tobacco use (including passive smoking by never-smokers) (6) and familial inheritance (9, 10) are the two main points. Field cancerization was also reported to be a likely mechanism of multifocal lung cancer (30, 31). In addition, a previous study reported that lung cancer survivors were more vulnerable to subsequent pulmonary malignancies (32). In 2021, Chen et al. first demonstrated that microplastic exposure was associated with the etiology of multiple pulmonary GGOs (ground-glass nodules) (33), linking MPLC pathogenesis to environmental factors. Genetic variants, such as EGFR germline mutations, were also reported to be the driving force of MPLC (15, 34). A SEER (Surveillance Epidemiology and End Results) analysis suggested that younger age, female gender, earlier stage, and white race are risk factors for MPLC (35). Previous studies reported that the incidence of multi-focal lung cancer ranges from 0.2% to 20% (36–38). We believe that the incidence of MPLC in the real world is far more than what has been reported. Since the COVID-19 (Corona Virus Disease-19) pandemic in 2019, the number of patients undergoing pulmonary CT (computerized tomography) increased, resulting in a wave of the rapid growth of MPLC (39). So far, the associations between COVID-19 and MPLC have not been illustrated.
Clinical management and prognosis
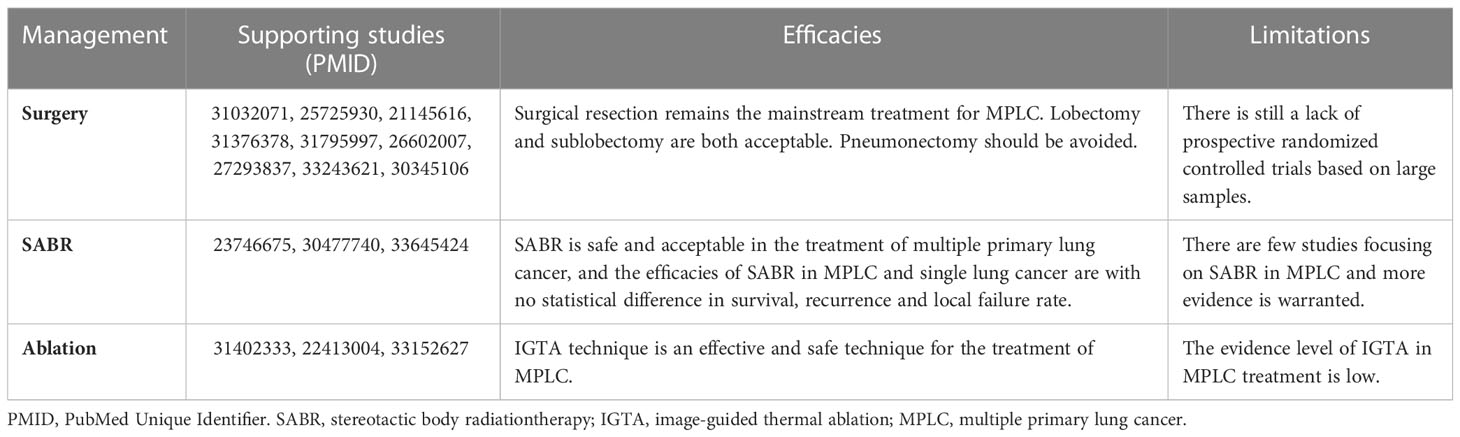
Nowadays, there are multiple treatments for MPLC, including surgery, stereotactic ablative radiation (SABR), immunotherapy, and ablation. If the multiple lung tumors were diagnosed as IPM, the treatment strategy should obey the principle of treating T3/T4 NSCLC. In this part, we collected the relevant studies on MPLC and compared the efficacies and limitations of different treatments, which are summarized in Table 2.
For surgery, previous researchers have devoted much effort to identifying the most appropriate resection strategy and risk factors of prognosis for MPLC (40). Both synchronous and metachronous MPLC can benefit from surgical resection (41–43). In 2019, Chen et al. suggested that sub-lobar resection can lead to an equivalent prognosis to standard resection (lobectomy) and was beneficial in preserving pulmonary function (44), and for both ipsilateral and bilateral MPLC, surgery resection is as safe as single-nodule lung cancer (43, 45). It is believed that radical pneumonectomy should be avoided, if possible, for it may lead to a poor prognosis (46, 47). It’s worth mentioning that the situation becomes more complicated when GGO/lepidic lesions coexist with solid or subsolid nodules. In clinical practice, removing solid nodules might be the best choice and at the same time, removing the other GGOs on the same side is more helpful for diagnosing and staging (48).
For patients with MPLC, surgery is far from a single treatment. On the one hand, there are many high-risk patients of older age or with underlying cardiopulmonary comorbidities, for whom thoracic operations might lead to severe intraoperative and postoperative complications. On the other hand, some MPLC patients have lung nodules disseminated in more than one lobe, especially for multifocal lung adenocarcinoma with ground glass/lepidic features (Type III), which are inert in nature compared to solid and subsolid nodules. Removing all nodules seems impossible for these people or will lead to much lung function loss. Besides, the selection logic of resection strategy is different among different surgeons, for removing tumors to the maximum extent is as essential as guaranteeing patients’ post-treatment life quality.
For MPLC patients who are not suitable for surgery, stereotactic ablative radiation (SABR), and image-guided thermal ablation (IGTA) (18–20, 49) are recommended. The ESMO guidelines for early and locally advanced NSCLC recommended that MPLC should be mainly assessed with curative intent (complete resection), while SABR was also an effective choice (50). Previous research showed that stereotactic ablative body radiotherapy achieved an 84% lesion control rate after two years in MPLC (19). And Nikittas et al. compared the effectiveness and safety between MPLC patients and single nodule patients. They suggested improved disease and survival outcomes in patients receiving both surgery and SBRT and multiple courses of SBRT alone for MPLC, though this could be due to selection bias (18). Image-guided thermal ablation is a method that has been proven to be applicable to the treatment of pulmonary nodules in recent years (20, 51). And it contains radiofrequency ablation (RFA), microwave ablation (MWA), and cryoablation (CA) (51). Aufranc et al. (52) studied 115 patients with a total of 160 lung tumors to compare microwave (MWA) and radiofrequency (RFA) ablation in the percutaneous treatment of primary and secondary lung tumors. They found that MWA and RFA are effective and safe IGTA techniques for the treatment of lung cancer. Besides, there are other retrospective studies that improved the safety and efficiency of IGTA (53–55), but they are small-sized cohort studies.
Many factors are associated with better survival in MPLC, including small tumor size (size of the largest tumor and sum of tumor sizes, also presenting as SUVmax value in radiologic images) (56, 57), similar histology of multiple lesions, N0 stage (better prognosis) (58), T1 stage (42), female gender (59), young age, non-smoker and FEV1/FVC ≥70% (42). Evidence showed that male gender, symptomatic disease, and lymph node involvement were independent factors for adverse prognosis (60). The prognosis of stage I synchronous multiple primary non-small cell lung cancer is similar to that of solitary primary NSCLC (61). To take precautions against metachronous primary lung cancers, regular CT examination after surgical resection is recommended for heavy smokers (62). Long-term follow-up for both synchronous and metachronous MPLC is necessary by which potentially curable secondary lung cancers can be identified when they are still under control (63).
Taken together, although people spent years finding the best treatment for MPLC, surgical resection remains the mainstream, while the non-surgical treatment approaches for MPLC are also indispensable.
Clinical trials about MPLC
To the best of our knowledge, nine registered clinical trials about MPLC have been launched so far (Table 3), half of which are interventional, and the other half are observational. Most clinical trials are still recruiting patients, and no trial has been completed. The combination of immunotherapy and ablation-related methods are under the spotlight. The newest trial was launched on 22nd December 2022, by Li et al. from Ruijin Hospital, Affiliated to Shanghai Jiao Tong University School of Medicine. They aim to compare ablation plus surgery with surgery alone in treating bilateral MPLC. Jie et al. from the First Affiliated Hospital of Xiamen University, China, launched clinical trials of inoperable synchronous MPLC, applying stereotactic ablation radiotherapy and Sintilimab. At the same time as Jie et al., Chen et al. from Shanghai Pulmonary Hospital, China, started a phase II clinical trial of MPLC using microwave ablation plus Camrelizumab. To evaluate the diagnostic value of 18F-FDG PET/CT dynamic imaging of distinguishing MPLC from IPM, Jin et al. from Fifth Affiliated Hospital, Sun Yat-Sen University, started a clinical trial including 120 participants in 2018, which is estimated to be completed in 2024.
There was also a trial focused on the targeted therapy of multiple GGOs. Li et al. from Ruijin Hospital, affiliated to Shanghai Jiao Tong University School of Medicine, started a phase II clinical trial applying Furmonertinib (EGFR-TKI) to multiple synchronous ground-glass opacities in October 2021. Immunotherapy was also in GGOs clinical trials. He et al. from the First Affiliated Hospital of Guangzhou Medical University are recruiting GGOs MPLC patients for Sintilimab (anti-PD-1therapy).
Notably, all nine clinical trials are launched by Chinese researchers. Chinese researchers have paid much attention to MPLC in the past five years, and the results of the most established trials will come out within the next five years. We hope their findings can offer constructive suggestions to the management of MPLC, though, among the current trials, the maximal number of recruiting patients is 172, which might not be enough for a comprehensive illustration of this disease in our recognition.
Overall, the attention MPLC received from clinical trials does not match the significance of this disease in lung cancer, considering its high incidence. We are especially looking forward to more trials exploring the efficacy of immunotherapy in MPLC since the introduction of checkpoint inhibitors opens new avenues for cancer therapy. In addition, we look forward to the trials conducted on Caucasians, which might provide a valuable understanding of MPLC.
Genomic updates about MPLC
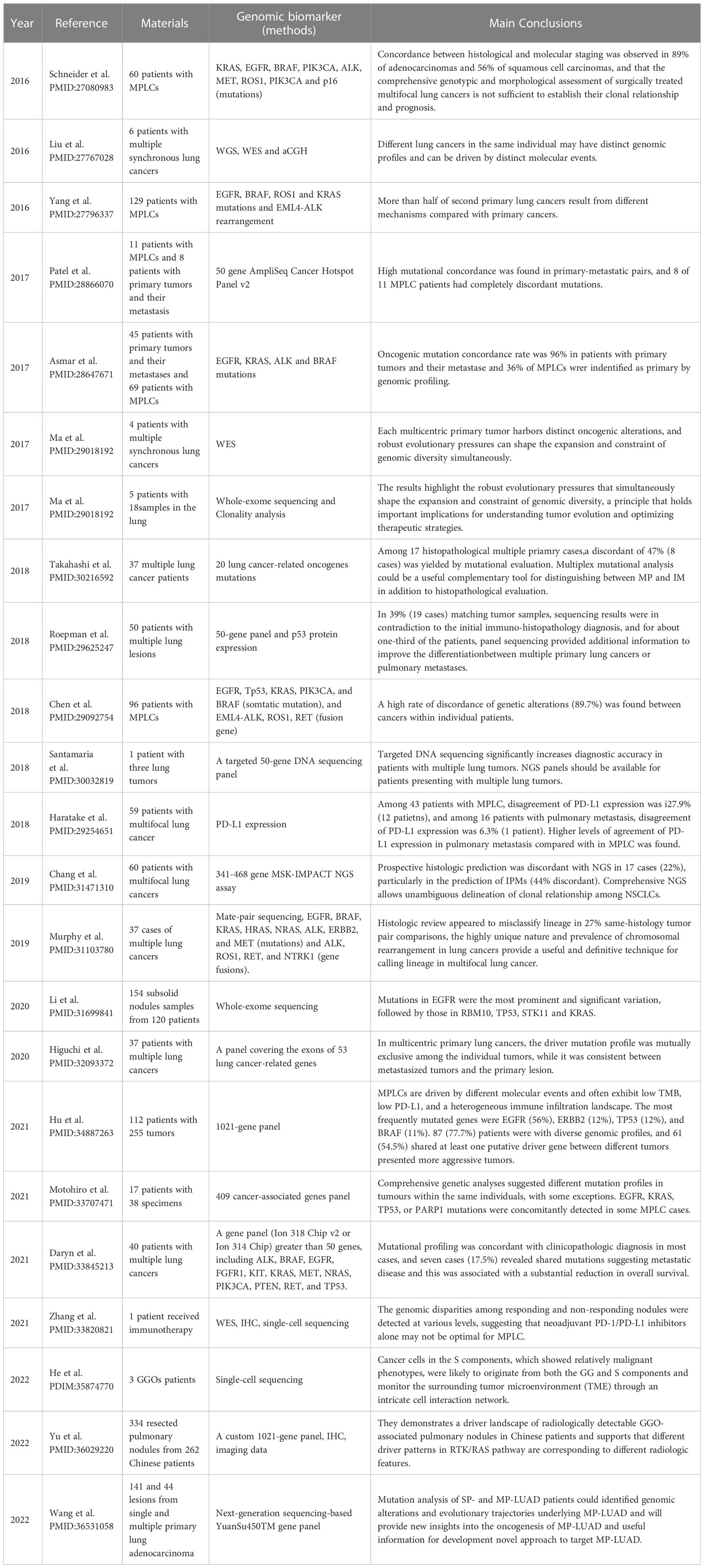
Genomic characteristics of multifocal lung cancer started over 25 years ago (64). With the development of science and technology and the progress of gene research methods, several molecular methods such as DNA microsatellite analysis, array comparative genomic hybridization (aCGH), targeted sequencing, next-generation sequencing (NGS), and single-cell sequencing have been applied to profiling the characteristics of MPLC. We summarized the representative research on MPLC’s genomic profiling in recent years, as shown in Table 4.
Before the widespread of NGS, gene panels containing a few oncogenic/tumor-suppressor genes (usually 1 to 5 genes) and chromosome alterations in MPLC were the focus, which was far from enough for profiling the MPLC genome. Using target sequencing, many researchers tested genes such as EGFR, KRAS, and p53 in MPLC (65–67). Chromosome alterations such as copy number analysis (27, 68), microsatellite instability (MSI) (69), loss of heterozygosity (LOH) analysis (69, 70), and X chromosome inactivation (37) were also detected in MPLC by genomic hybridization (aCGH). Those previous researchers tried to find out the difference and similarities of lesions of MPLC (37, 40), but inefficient technology hinders our in-depth understanding of the MPLC genome.
In the era of NGS, various sequencing approaches and analysis methods have emerged, fueling a wave of genomic research on MPLC.
1. The distinction between MPLC and IPM
The precise differentiation between MPLC and IPM is one of the driving forces of the genomic exploration of MPLC. Genomic profiling information challenged the traditional clinicopathologic criteria of MPLC. In the era of next-generation sequencing (NGS), the application of large gene sequencing panels, whole-genome sequencing (WGS), and chromosome rearrangements helped us distinguish MPLC from IPM
In 2018, Santamaria et al. (71) conducted a targeted 50-gene DNA sequencing panel on a lung cancer patient with three lesions. Their results supported that all three lesions were independent in mutation background, indicating they were MPLC rather than advanced lung cancer. In 2019, similar research was conducted by Chang et al. using an NGS assay covering up to 468 cancer-related genes in 60 patients, showing that the histologic classification was contrary to the judgment based on NGS in 22% of all cases, especially in the prediction of IPMs, in which the misdiagnosis rate was up to 44% (72).
Whole-genome sequencing (WGS) and whole-exome sequencing (WES) are more comprehensive in profiling genomic features than targeted sequencing. In 2016, Liu et al. (73) were the first to portray the genomic architecture of MPLC using WGS and WES. They collected 16 tumor samples from six patients. One patient was identified as having metastasis under histopathological standards and was classified as primary based on genomic sequencing results. In 2018, Li et al. (74) performed exome sequencing on two non-smoker patients with multiple GGOs (patient 1 had seven subsolid nodules and one pure GGO, and all the six nodules of patient 2 were pure GGOs). Results showed that two subsolid nodules in patient one and two pure GGOs in patient 2 were clonally-related, respectively, indicating that intrapulmonary metastasis could occur among GGOs, even in pure GGOs, which reshaped people’s impression of multiple GGOs.
Recently, chromosome rearrangements were reported to be an effective tool for this discrimination (29, 38). In 2014 and 2019, Murphy et al. applied mate-pair sequencing (MPS) to 11 and 37 patients with multifocal lung cancer with known metastasis lesions, respectively. In 2019, a lung cancer NGS panel was applied to 17 of 37 patients. Both the two studies of Murphy et al. showed that DNA rearrangements generated by MPS performed well in the lineage calling of MPLC.
2. Multi-omics analysis of MPLC
Nowadays, multi-omics analysis of MPLC is used to confirm the heterogeneity and discuss the tumor immune microenvironment of multiple nodules in MPLC. Clonal evolution is a method to portray the evolution of MPLC. PyClone is a statistical model introduced by Roth et al. (75) for inference of clonal population structures in cancers. In 2017, Ma et al. (76) sequenced four patients with multiple synchronous lesions by WES and performed phylogenetic analysis showing clonal architectures. Despite the identical genetic background and environmental exposure, they found significant genomic heterogeneity in individual patients’ inter-focal and intra-focal levels. Currently, this method has not been well performed in MPLC.
In 2020, Wang and his team (77) first integrated the radiological image data of mGGOs into their genomic analysis to investigate the intratumoral heterogeneity and clonal relationship of multifocal GGOs. They found that the differences between subsolid nodules (SSNs) and advanced-stage LUADs at a genomic level were unraveled. Although multicentric origin was predominant, they also detected early metastatic events among multifocal SSNs. Similarly, Yu et al. (78) performed a custom 1021-gene panel sequencing of 334 resected pulmonary nodules presenting as GGO from 262 Chinese patients. They compared gene pathways enriched in different GGOs (pure GGOs and mixed GGOs) through genomic profiling. They demonstrate a driver landscape of radiologically detectable GGO-associated pulmonary nodules in Chinese patients and support that different driver patterns in RTK/RAS pathway correspond to different radiologic features.
Single-cell sequencing technology has been a brilliant new technology for tumor analysis in recent years. It studied the changes in the multicellular microenvironment of the tumor by studying the cell composition in tumor tissue. In 2021, Zhang et al. (21) performed WES, Immunohistochemistry (IHC), single-cell RNA seq, TCR (T cell receptor repertoire)-seq in the multiple nodules of one MPLC case undergoing neoadjuvant pembrolizumab treatment. The genomic disparities among responding and non-responding nodules were detected at various levels, suggesting that neoadjuvant PD-1/PD-L1 inhibitors alone may not be optimal for MPLC.
In 2022, 10x Genomics single-cell RNA-seq was used in GGOs by Li et al. (79), and they identified transcriptomic differences in the vital signaling pathways of tumor and immune cells within GGOs, implying the transcriptomic heterogeneity of this disease. Similarly, He et al. (80) macro-dissected the solid (S) components and ground-glass (GG) components of mGGO and performed single-cell sequencing analyses of six paired components from three mGGO patients. They found that cancer cells and macrophages were the dominant cell types in the S and GG components, respectively. Cancer cells in the S components, which showed relatively malignant phenotypes, were likely to originate from both the GG and S components and monitor the surrounding tumor microenvironment (TME) through an intricate cell interaction network.
In summary, with the progress of science and technology, our perceptions about MPLC are growing. Thanks to the initial exploration of the heterogeneity of MPLC, to the later identification of MPLC and IPM, and finally to the use of advanced sequencing technology to clarify the development mechanisms/tumor immune microenvironment, our understanding of MPLC is now deeper and it is expected to increase in the future.
Summary
From clinical management to genomic profiling, this review gives a comprehensive description of MPLC, which is a highly focused malignancy by clinicians. We hope our work can enlighten more profound reflections about MPLC from the public.
Author contributions
JH, SG, and CL designed this study and provided funding support. HT, GB, and ZY drafted the manuscript and completed the tables. PC, JX, TL, TF, BW, and CX collected the references and completed the tables. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Special Research Fund for Central Universities, Peking Union Medical College (3332022132), the National Key R&D Program of China (2018YFC1312100), the National Natural Science Foundation of China (81972196), The CAMS Innovation Fund for Medical Sciences (CIFMS) (2017-I2M-1-005, 2019-I2M-2-002), The Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2018PT32033), The Innovation team development project of Ministry of Education (IRT_17R10).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin (2022) 72(1):7–33. doi: 10.3322/caac.21708
2. Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ Jr., Wu YL, et al. Lung cancer: current therapies and new targeted treatments. Lancet (2017) 389(10066):299–311. doi: 10.1016/S0140-6736(16)30958-8
3. Sands J, Tammemägi MC, Couraud S, Baldwin DR, Borondy-Kitts A, Yankelevitz D, et al. Lung screening benefits and challenges: A review of the data and outline for implementation. J Thorac Oncol (2021) 16(1):37–53. doi: 10.1016/j.jtho.2020.10.127
4. Loukeri AA, Kampolis CF, Ntokou A, Tsoukalas G, Syrigos K. Metachronous and synchronous primary lung cancers: Diagnostic aspects, surgical treatment, and prognosis. Clin Lung Cancer (2015) 16(1):15–23. doi: 10.1016/j.cllc.2014.07.001
5. Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg (1975) 70(4):606–12. doi: 10.1016/S0022-5223(19)40289-4
6. Tucker MA, Murray N, Shaw EG, Ettinger DS, Mabry M, Huber MH, et al. Second primary cancers related to smoking and treatment of small-cell lung cancer. lung cancer working cadre. J Natl Cancer Inst (1997) 89(23):1782–8. doi: 10.1093/jnci/89.23.1782
7. Braakhuis BJ, Tabor MP, Kummer JA, Leemans CR, Brakenhoff RH. A genetic explanation of slaughter's concept of field cancerization: Evidence and clinical implications. Cancer Res (2003) 63(8):1727–30. Available at: https://aacrjournals.org/cancerres/article/63/8/1727/511142/A-Genetic-Explanation-of-Slaughter-s-Concept-of.
8. Johnson BE. Second lung cancers in patients after treatment for an initial lung cancer. J Natl Cancer Inst (1998) 90(18):1335–45. doi: 10.1093/jnci/90.18.1335
9. Li X, Hemminki K. Familial and second lung cancers: A nation-wide epidemiologic study from Sweden. Lung Cancer (2003) 39(3):255–63. doi: 10.1016/S0169-5002(02)00535-4
10. Li X, Hemminki K. Familial multiple primary lung cancers: A population-based analysis from Sweden. Lung Cancer (2005) 47(3):301–7. doi: 10.1016/j.lungcan.2004.07.048
11. Goodwin D, Rathi V, Conron M, Wright GM. Genomic and clinical significance of multiple primary lung cancers as determined by next-generation sequencing. J Thorac Oncol (2021) 16(7):1166–75. doi: 10.1016/j.jtho.2021.03.018
12. Tian S, Li F, Pu J, Zheng Y, Shi H, Dong Y, et al. Differential diagnostic value of histology in MPLC and IPM: A systematic review and meta-analysis. Front Oncol (2022) 12:871827. doi: 10.3389/fonc.2022.871827
13. Izumi M, Sawa K, Oyanagi J, Noura I, Fukui M, Ogawa K, et al. : Tumor microenvironment disparity in multiple primary lung cancers: Impact of non-intrinsic factors, histological subtypes, and genetic aberrations. Transl Oncol (2021) 14(7):101102. doi: 10.1016/j.tranon.2021.101102
14. Wright GM, Goodwin D. Response to letter: Beyond "Personalized" to "Tumoralized" therapy. J Thorac Oncol (2022) 17(6):e54. doi: 10.1016/j.jtho.2022.03.013
15. Izumi M, Oyanagi J, Sawa K, Fukui M, Ogawa K, Matsumoto Y, et al. Mutational landscape of multiple primary lung cancers and its correlation with non-intrinsic risk factors. Sci Rep (2021) 11(1):5680. doi: 10.1038/s41598-021-83609-y
16. Suh YJ, Lee H-J, Sung P, Yoen H, Kim S, Han S, et al. A novel algorithm to differentiate between multiple primary lung cancers and intrapulmonary metastasis in multiple lung cancers with multiple pulmonary sites of involvement. J Thorac Oncol (2020) 15(2):203–15. doi: 10.1016/j.jtho.2019.09.221
17. Tie H, Luo J, Shi R, Li Z, Chen D, Wu Q. Characteristics and prognosis of synchronous multiple primary lung cancer after surgical treatment: A systematic review and meta-analysis of current evidence. Cancer Med (2021) 10(2):507–20. doi: 10.1002/cam4.3614
18. Nikitas J, DeWees T, Rehman S, Abraham C, Bradley J, Robinson C, et al. Stereotactic body radiotherapy for early-stage multiple primary lung cancers. Clin Lung Cancer (2019) 20(2):107–16. doi: 10.1016/j.cllc.2018.10.010
19. Griffioen GH, Lagerwaard FJ, Haasbeek CJ, Smit EF, Slotman BJ, Senan S. Treatment of multiple primary lung cancers using stereotactic radiotherapy, either with or without surgery. Radiother Oncol (2013) 107(3):403–8. doi: 10.1016/j.radonc.2013.04.026
20. Lin M, Eiken P, Blackmon S. Image guided thermal ablation in lung cancer treatment. J Thorac Dis (2020) 12(11):7039–47. doi: 10.21037/jtd-2019-cptn-08
21. Zhang C, Yin K, Liu SY, Yan LX, Su J, Wu YL, et al. Multiomics analysis reveals a distinct response mechanism in multiple primary lung adenocarcinoma after neoadjuvant immunotherapy. J Immunother Cancer (2021) 9(4):1–4. doi: 10.1136/jitc-2020-002312
22. Xu L, Shi M, Wang S, Li M, Yin W, Zhang J, et al. Immunotherapy for bilateral multiple ground glass opacities: An exploratory study for synchronous multiple primary lung cancer. Front Immunol (2022) 13:1009621. doi: 10.3389/fimmu.2022.1009621
23. Wang Y, Wang G, Zheng H, Liu J, Ma G, Huang G, et al. Distinct gene mutation profiles among multiple and single primary lung adenocarcinoma. Front In Oncol (2022) 12:1014997. doi: 10.3389/fonc.2022.1014997
24. Xing X, Yang F, Huang Q, Guo H, Li J, Qiu M, et al. Decoding the multicellular ecosystem of lung adenocarcinoma manifested as pulmonary subsolid nodules by single-cell RNA sequencing. Sci Adv (2021) 7(5):1–5. doi: 10.1126/sciadv.abd9738
25. Antakli T, Schaefer RF, Rutherford JE, Read RC. Second primary lung cancer. Ann Thorac Surg (1995) 59(4):863–6. discussion 867. doi: 10.1016/0003-4975(95)00067-u
26. Detterbeck FC, Nicholson AG, Franklin WA, Marom EM, Travis WD, Girard N, et al. The IASLC lung cancer staging project: Summary of proposals for revisions of the classification of lung cancers with multiple pulmonary sites of involvement in the forthcoming eighth edition of the TNM classification. J Thorac Oncol (2016) 11(5):639–50. doi: 10.1016/j.jtho.2016.01.024
27. Girard N, Ostrovnaya I, Lau C, Park B, Ladanyi M, Finley D, et al. Genomic and mutational profiling to assess clonal relationships between multiple non-small cell lung cancers. Clin Cancer Res (2009) 15(16):5184–90. doi: 10.1158/1078-0432.CCR-09-0594
28. Girard N, Deshpande C, Lau C, Finley D, Rusch V, Pao W, et al. Comprehensive histologic assessment helps to differentiate multiple lung primary nonsmall cell carcinomas from metastases. Am J Surg Pathol (2009) 33(12):1752–64. doi: 10.1097/PAS.0b013e3181b8cf03
29. Murphy SJ, Harris FR, Kosari F, Barreto Siqueira Parrilha Terra S, Nasir A, Johnson SH, et al. Using genomics to differentiate multiple primaries from metastatic lung cancer. J Thorac Oncol (2019) 14(9):1567–82. doi: 10.1016/j.jtho.2019.05.008
30. Gazdar AF, Minna JD. Multifocal lung cancers–clonality vs field cancerization and does it matter? J Natl Cancer Inst (2009) 101(8):541–3. doi: 10.1093/jnci/djp059
31. Dotto GP. Multifocal epithelial tumors and field cancerization: Stroma as a primary determinant. J Clin Invest (2014) 124(4):1446–53. doi: 10.1172/JCI72589
32. Barclay ME, Lyratzopoulos G, Walter FM, Jefferies S, Peake MD, Rintoul RC. Incidence of second and higher order smoking-related primary cancers following lung cancer: a population-based cohort study. Thorax (2019) 74(5):466–72. doi: 10.1136/thoraxjnl-2018-212456
33. Chen Q, Gao J, Yu H, Su H, Liu H. An emerging role of microplastics in the etiology of lung ground glass nodules. Cold Spring Harbor Lab Press (2021) 16:1–5. doi: 10.1101/2021.04.22.21255586
34. Li C, Wang Y, Su K, Liu Y, Wang L, Zheng B, et al. Presentation of EGFR mutations in 162 family probands with multiple primary lung cancer. Transl Lung Cancer Res (2021) 10(4):1734–46. doi: 10.21037/tlcr-20-1001
35. Bhaskarla A, Tang PC, Mashtare T, Nwogu CE, Demmy TL, Adjei AA, et al. Analysis of second primary lung cancers in the SEER database. J Surg Res (2010) 162(1):1–6. doi: 10.1016/j.jss.2009.12.030
36. Nakata M, Sawada S, Yamashita M, Saeki H, Kurita A, Takashima S, et al. Surgical treatments for multiple primary adenocarcinoma of the lung. Ann Thorac Surg (2004) 78(4):1194–9. doi: 10.1016/j.athoracsur.2004.03.102
37. Wang X, Wang M, MacLennan GT, Abdul-Karim FW, Eble JN, Jones TD, et al. Evidence for common clonal origin of multifocal lung cancers. J Natl Cancer Inst (2009) 101(8):560–70. doi: 10.1093/jnci/djp054
38. Murphy SJ, Aubry MC, Harris FR, Halling GC, Johnson SH, Terra S, et al. Identification of independent primary tumors and intrapulmonary metastases using DNA rearrangements in non-small-cell lung cancer. J Clin Oncol (2014) 32(36):4050–8. doi: 10.1200/JCO.2014.56.7644
39. Liao Z, Rivin Del Campo E, Salem A, Pang Q, Liu H, Lopez Guerra JL. Optimizing lung cancer radiation treatment worldwide in COVID-19 outbreak. Lung Cancer (2020) 146:230–5. doi: 10.1016/j.lungcan.2020.05.029
40. Chen C, Huang X, Peng M, Liu W, Yu F, Wang X. Multiple primary lung cancer: a rising challenge. J Thorac Dis (2019) 11(Suppl 4):S523–s536. doi: 10.21037/jtd.2019.01.56
41. Hamaji M, Ali SO, Burt BM. A meta-analysis of resected metachronous second non-small cell lung cancer. Ann Thorac Surg (2015) 99(4):1470–8. doi: 10.1016/j.athoracsur.2014.11.033
42. Jung EJ, Lee JH, Jeon K, Koh WJ, Suh GY, Chung MP, et al. Treatment outcomes for patients with synchronous multiple primary non-small cell lung cancer. Lung Cancer (2011) 73(2):237–42. doi: 10.1016/j.lungcan.2010.11.008
43. Lee D-S, LaChapelle C, Taioli E, Kaufman A, Wolf A, Nicastri D, et al. Second primary lung cancers demonstrate similar survival with wedge resection and lobectomy. Ann Thorac Surg (2019) 108(6):1724–8. doi: 10.1016/j.athoracsur.2019.06.023
44. Chen TF, Xie CY, Rao BY, Shan SC, Zhang X, Zeng B, et al. Surgical treatment to multiple primary lung cancer patients: a systematic review and meta-analysis. BMC Surg (2019) 19(1):185. doi: 10.1186/s12893-019-0643-0
45. Yang H, Sun Y, Yao F, Yu K, Gu H, Han B, et al. Surgical therapy for bilateral multiple primary lung cancer. Ann Thorac Surg (2016) 101(3):1145–52. doi: 10.1016/j.athoracsur.2015.09.028
46. Liu M, He W, Yang J, Jiang G. Surgical treatment of synchronous multiple primary lung cancers: a retrospective analysis of 122 patients. J Thorac Dis (2016) 8(6):1197–204. doi: 10.21037/jtd.2016.04.46
47. Nie Y, Wang X, Yang F, Zhou Z, Wang J, Chen K. Surgical prognosis of synchronous multiple primary lung cancer: Systematic review and meta-analysis. Clin Lung Cancer (2021) 22(4):1–3. doi: 10.1016/j.cllc.2020.10.022
48. Waller DA. Surgical management of lung cancer with multiple lesions: Implication of the new recommendations of the 8(th) edition of the TNM classification for lung cancer. J Thorac Dis (2018) 10(Suppl 22):S2686–s2691. doi: 10.21037/jtd.2018.04.159
49. Steber CR, Hughes RT, Soike MH, Helis CA, Nieto K, Jacobson T, et al. Stereotactic body radiotherapy for synchronous early stage non-small cell lung cancer. Acta Oncol (Stockholm Sweden) (2021) 60(5):605–12. doi: 10.1080/0284186X.2021.1892182
50. Postmus PE, Kerr KM, Oudkerk M, Senan S, Waller DA, Vansteenkiste J, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol (2017) 28(suppl_4):iv1–iv21. doi: 10.1093/annonc/mdx222
51. Paez-Carpio A, Gomez FM, Isus Olive G, Paredes P, Baetens T, Carrero E, et al. Image-guided percutaneous ablation for the treatment of lung malignancies: Current state of the art. Insights Imaging (2021) 12(1):57. doi: 10.1186/s13244-021-00997-5
52. Aufranc V, Farouil G, Abdel-Rehim M, Smadja P, Tardieu M, Aptel S, et al. Percutaneous thermal ablation of primary and secondary lung tumors: Comparison between microwave and radiofrequency ablation. Diagn Interv Imaging (2019) 100(12):781–91. doi: 10.1016/j.diii.2019.07.008
53. Nomori H, Yamazaki I, Shiraishi A, Adachi T, Kanno M. Cryoablation for T1N0M0 non-small cell lung cancer using liquid nitrogen. Eur J Radiol (2020) 133:109334. doi: 10.1016/j.ejrad.2020.109334
54. Moore W, Talati R, Bhattacharji P, Bilfinger T. Five-year survival after cryoablation of stage I non-small cell lung cancer in medically inoperable patients. J Vasc Interv Radiol (2015) 26(3):312–9. doi: 10.1016/j.jvir.2014.12.006
55. Yamauchi Y, Izumi Y, Hashimoto K, Yashiro H, Inoue M, Nakatsuka S, et al. Percutaneous cryoablation for the treatment of medically inoperable stage I non-small cell lung cancer. PloS One (2012) 7(3):e33223. doi: 10.1371/journal.pone.0033223
56. Hsu HH, Ko KH, Chou YC, Lin LF, Tsai WC, Lee SC, et al. SUVmax and tumor size predict surgical outcome of synchronous multiple primary lung cancers. Med (Baltimore) (2016) 95(6):e2351. doi: 10.1097/MD.0000000000002351
57. Tanvetyanon T, Robinson L, Sommers KE, Haura E, Kim J, Altiok S, et al. Relationship between tumor size and survival among patients with resection of multiple synchronous lung cancers. J Thorac Oncol (2010) 5(7):1018–24. doi: 10.1097/JTO.0b013e3181dd0fb0
58. Zhang Y, Hu H, Wang R, Ye T, Pan Y, Wang L, et al. Synchronous non-small cell lung cancers: Diagnostic yield can be improved by histologic and genetic methods. Ann Surg Oncol (2014) 21(13):4369–74. doi: 10.1245/s10434-014-3840-1
59. Finley DJ, Yoshizawa A, Travis W, Zhou Q, Seshan VE, Bains MS, et al. Predictors of outcomes after surgical treatment of synchronous primary lung cancers. J Thorac Oncol (2010) 5(2):197–205. doi: 10.1097/JTO.0b013e3181c814c5
60. Zhang Z, Gao S, Mao Y, Mu J, Xue Q, Feng X, et al. Surgical outcomes of synchronous multiple primary non-small cell lung cancers. Sci Rep (2016) 6:23252. doi: 10.1038/srep23252
61. Li J, Yang X, Xia T, Guan Y, Zhong N. Stage I synchronous multiple primary non-small cell lung cancer: CT findings and the effect of TNM staging with the 7th and 8th editions on prognosis. J Thorac Dis (2017) 9(12):5335–44. doi: 10.21037/jtd.2017.12.101
62. Usuda J, Ichinose S, Ishizumi T, Hayashi H, Ohtani K, Maehara S, et al. Management of multiple primary lung cancer in patients with centrally located early cancer lesions. J Thorac Oncol (2010) 5(1):62–8. doi: 10.1097/JTO.0b013e3181c42287
63. Wang Y, Yeung JC, Hanna WC, Allison F, Paul NS, Waddell TK, et al. Metachronous or synchronous primary lung cancer in the era of computed tomography surveillance. J Thorac Cardiovasc Surg (2018) 157:1–6. doi: 10.1016/j.jtcvs.2018.09.052
64. Mitsudomi T, Yatabe Y, Koshikawa T, Hatooka S, Shinoda M, Suyama M, et al. Mutations of the P53 tumor suppressor gene as clonal marker for multiple primary lung cancers. J Thorac Cardiovasc Surg (1997) 114(3):354–60. doi: 10.1016/S0022-5223(97)70180-6
65. Chang YL, Wu CT, Lin SC, Hsiao CF, Jou YS, Lee YC. Clonality and prognostic implications of p53 and epidermal growth factor receptor somatic aberrations in multiple primary lung cancers. Clin Cancer Res (2007) 13(1):52–8. doi: 10.1158/1078-0432.CCR-06-1743
66. Girard N, Deshpande C, Azzoli CG, Rusch VW, Travis WD, Ladanyi M, et al. Use of epidermal growth factor receptor/Kirsten rat sarcoma 2 viral oncogene homolog mutation testing to define clonal relationships among multiple lung adenocarcinomas: Comparison with clinical guidelines. Chest (2010) 137(1):46–52. doi: 10.1378/chest.09-0325
67. Warth A, Macher-Goeppinger S, Muley T, Thomas M, Hoffmann H, Schnabel PA, et al. Clonality of multifocal nonsmall cell lung cancer: implications for staging and therapy. Eur Respir J (2012) 39(6):1437–42. doi: 10.1183/09031936.00105911
68. Gallegos Ruiz MI, van Cruijsen H, Smit EF, Grünberg K, Meijer GA, Rodriguez JA, et al. Genetic heterogeneity in patients with multiple neoplastic lung lesions: A report of three cases. J Thorac Oncol (2007) 2(1):12–21. doi: 10.1016/S1556-0864(15)30012-5
69. Wu C, Zhao C, Yang Y, He Y, Hou L, Li X, et al. High discrepancy of driver mutations in patients with NSCLC and synchronous multiple lung ground-glass nodules. J Thorac Oncol (2015) 10(5):778–83. doi: 10.1097/JTO.0000000000000487
70. Dacic S, Ionescu DN, Finkelstein S, Yousem SA. Patterns of allelic loss of synchronous adenocarcinomas of the lung. Am J Surg Pathol (2005) 29(7):897–902. doi: 10.1097/01.pas.0000164367.96379.66
71. Eguren-Santamaria I, Sanchez-Bayona R, Patiño-Garcia A, Gil-Bazo I, Lopez-Picazo JM. Targeted DNA sequencing for assessing clonality in multiple lung tumors: A new approach to an old dilemma. Lung Cancer (2018) 122:120–3. doi: 10.1016/j.lungcan.2018.05.029
72. Chang JC, Alex D, Bott M, Tan KS, Seshan V, Golden A, et al. Comprehensive next-generation sequencing unambiguously distinguishes separate primary lung carcinomas from intrapulmonary metastases: Comparison with standard histopathologic approach. Clin Cancer Res (2019) 25(23):7113–25. doi: 10.1158/1078-0432.CCR-19-1700
73. Liu Y, Zhang J, Li L, Yin G, Zhang J, Zheng S, et al. Genomic heterogeneity of multiple synchronous lung cancer. Nat Commun (2016) 7:13200. doi: 10.1038/ncomms13200
74. Li R, Li X, Xue R, Yang F, Wang S, Li Y, et al. Early metastasis detected in patients with multifocal pulmonary ground-glass opacities (GGOs). Thorax (2018) 73(3):290–2. doi: 10.1136/thoraxjnl-2017-210169
75. Roth A, Khattra J, Yap D, Wan A, Laks E, Biele J, et al. PyClone: statistical inference of clonal population structure in cancer. Nat Methods (2014) 11(4):396–8. doi: 10.1038/nmeth.2883
76. Ma P, Fu Y, Cai MC, Yan Y, Jing Y, Zhang S, et al. Simultaneous evolutionary expansion and constraint of genomic heterogeneity in multifocal lung cancer. Nat Commun (2017) 8(1):823. doi: 10.1038/s41467-017-00963-0
77. Li Y, Li X, Li H, Zhao Y, Liu Z, Sun K, et al. Genomic characterisation of pulmonary subsolid nodules: mutational landscape and radiological features. Eur Respir J (2020) 55(2):1–4. doi: 10.1183/13993003.01409-2019
78. Yu F, Peng M, Bai J, Zhu X, Zhang B, Tang J, et al. Comprehensive characterization of genomic and radiologic features reveals distinct driver patterns of RTK/RAS pathway in ground-glass opacity pulmonary nodules. Int J Cancer (2022) 151(11):2020–30. doi: 10.1002/ijc.34238
79. Li Y, Li X, Chen H, Sun K, Li H, Zhou Y, et al. Single-cell RNA sequencing reveals the multi-cellular ecosystem in different radiological components of pulmonary part-solid nodules. Clin Transl Med (2022) 12(2):e723. doi: 10.1002/ctm2.723
Keywords: multiple primary lung cancer (MPLC), clinical management, genomic, heterogeneity, intrapulmonary metastasis (IPM)
Citation: Tian H, Bai G, Yang Z, Chen P, Xu J, Liu T, Fan T, Wang B, Xiao C, Li C, Gao S and He J (2023) Multiple primary lung cancer: Updates of clinical management and genomic features. Front. Oncol. 13:1034752. doi: 10.3389/fonc.2023.1034752
Received: 02 September 2022; Accepted: 13 February 2023;
Published: 22 February 2023.
Edited by:
Mirella Marino, Hospital Physiotherapy Institutes (IRCCS), ItalyReviewed by:
Huiyu Li, University of Texas Southwestern Medical Center, United StatesQiongwen Zhang, Sichuan University, China
Sabahattin Cömertpay, Kahramanmaras Sütçü Imam University, Türkiye
Copyright © 2023 Tian, Bai, Yang, Chen, Xu, Liu, Fan, Wang, Xiao, Li, Gao and He. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunxiang Li, bGljaHVueGlhbmdAY2ljYW1zLmFjLmNu; Shugeng Gao, Z2Fvc2h1Z2VuZ0BjaWNhbXMuYWMuY24=; Jie He, aGVqaWVAY2ljYW1zLmFjLmNu
†These authors have contributed equally to this work
 He Tian
He Tian Guangyu Bai
Guangyu Bai Zhenlin Yang
Zhenlin Yang Ping Chen2
Ping Chen2 Jiachen Xu
Jiachen Xu Tao Fan
Tao Fan Chu Xiao
Chu Xiao Chunxiang Li
Chunxiang Li Shugeng Gao
Shugeng Gao