
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Oncol., 26 October 2022
Sec. Gynecological Oncology
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.979799
This article is part of the Research TopicCervical Cancer Control in Latin America and the CaribbeanView all 10 articles
Introduction: Self-efficacy has been related to different health preventive behaviors, included adherence to the Papanicolaou test—also called Pap smear or Pap test. The aim of this study is to test construct and criterion validity and reliability of a questionnaire on self-efficacy and the Pap test in Chilean women.
Method: This study was carried out on a sample of 969 women of ages from 25 to 64, who are users of the public health care system in Santiago, Chile. The validity of the Self-Efficacy Scale for the Pap Smear Screening Participation (SES-PSSP) questionnaire was done by confirmatory factor analysis, external criteria by t-test, and reliability by Cronbach’s alpha.
Results: Three models were tested, obtaining a questionnaire with 20 items and 2 dimensions. The criteria validity was confirmed by adherence to the Pap test. The final questionnaire has a reliability of 0.95, measured by Cronbach´s alpha.
Conclusion: A valid and reliable questionnaire to measure self-efficacy in relation to the Pap test is a relevant contribution in cervical cancer prevention, especially related to interventions focused on increasing adherence.
The need to explain behavior has been the motivation of many health theorists. Bandura’s Social Cognitive Theory (1) establishes self-efficacy among its main components, defined as the perception of control that can be exercised over a certain health behavior. The level of self-efficacy affects the choices people make, how much effort they invest, and how long they will persist in carrying out a certain behavior (2). The higher the level of self-efficacy, the greater the commitment to comply with a certain health behavior and the lower the perception of obstacles to carrying it out (1).
Self-efficacy has been related to different preventive health behaviors, such as screening for breast cancer (3–8), colon cancer (7, 9–11) and certain preventive practices in skin cancer (12). Regarding cervical cancer (CC), its relationship with adherence to the human papillomavirus vaccine (13, 14), adherence to the Papanicolaou (Pap) test—also called Pap smear or Pap—and to colposcopy (15), to educational interventions (16–21) and to depressive symptoms in women with the disease (22) has been studied.
The relationship between self-efficacy and adherence to Pap tests has also been studied (23–32) and found to establish that high levels of self-efficacy predict both the behavior of adhering to screening (33–41), as well as the intention (35, 42, 43). The participants’ CC and Pap test screening knowledge levels increased as their self-efficacy levels increased (44).
Given the importance of CC prevention and the relationship with self-efficacy, it is relevant to have a valid and reliable instrument in a commonly spoken and understood language that allows measurement of the self-efficacy of women in relation to adherence to CC screening. The aim of this work is to validate an instrument on self-efficacy related to Pap tests in Chilean women, written in Spanish.
The study is part of the FONDECYT #11130626 grant, “Social determinants for adherence to CC screening.” The universe of study corresponds to women from ages 25 to 64 years, belonging to the Chilean public health system—National Health Fund (FONASA)—and registered in one of the four primary health care centers of the Puente Alto commune in Santiago, Chile. The sample was selected and stratified by health centers and Pap test coverage levels. According to Pap test coverage data, four primary health care centers were randomly selected, with probabilities proportional to their size, one from each group: with the highest coverage, medium-high coverage, medium-low coverage, and low coverage. The sample size was calculated for a broader study using structural equation models, in which several instruments are related, such as beliefs, knowledge, activity planning, and self-efficacy. Using an online calculator and the methodology described by Soper (2003) (45), for a small effect size of 0.1 (relationship between the instruments), a power of 80%, a number of 15 latent and 40 observed variables, and a level of reliability of 95%, it was estimated that at least 850 women needed to be interviewed. The sample size corresponding to 969 women also meets the requirement regarding instrument validation (46). The inclusion criteria were the characteristics of the universe previously. The exclusion criteria were the presence of CC and/or total hysterectomy. Recruitment was carried out by telephone or by home visit. The interviews were conducted by previously trained personnel.
The sociodemographic variables, adherence to the Pap test, and self-efficacy in relation to screening were measured during the interview. The self-efficacy variable was measured with the SES-PSSP questionnaire (Self-Efficacy Scale for Pap Smear Screening Participation) (47). This questionnaire, validated in the North American population, has 20 items distributed in two dimensions: the first, on personal costs, includes aspects such as time, money, transportation and interruptions of life; and the second, on relationships, which includes the opinion of family members and peers. According to the original recommendation of the author of the instrument, 2 items can be added in case the interviewed woman has children and can leave them alone; given that these items are not applicable to all women, the author of the instrument does not include them in the dimensions described above and therefore they were not included in this research either. The answers are measured on a 5-point Likert scale (1 corresponding to “I would definitely do the Pap test” and 5 corresponding to “I would definitely not do the Pap test”).
For the validation of the instrument, the translation and back-translation of the questionnaire was carried out by two professionals in their respective native languages (English and Spanish); it was later submitted for determination of validity of cultural content to five thematic experts. First, the original questionnaire was translated into Spanish by a bilingual (Spanish/English) and native Spanish professional and researcher, and the “Spanish version” was obtained. Second, a bilingual native English professional researcher translated the “Spanish version” into English. Third, another bilingual researcher compared the original and translated versions of the instrument to ensure that the meaning of each item was not altered. In this case, both versions matched; thus, no changes to the translated version were needed. In relation to content validity, the reviews by the five researchers—who analyzed the characteristics of each of the items in terms of their understanding and applicability to the context in which the instrument would be used—were considered. There were no suggested changes. Subsequently, the questionnaire was applied to 10 women from the population that would be studied, to find out if the questions were understandable and/or if there were any terms that prevented a fluid response; there were no suggested changes.
The continuous variables were described using means and standard deviations, and categorical variables using absolute frequencies and percentages. Construct validity was performed using confirmatory factor analysis (CFA), criterion validity using Student’s t-test, and reliability using Cronbach’s alpha. Adherence to the Pap test was used as an external criterion of validity, for which the scores for each of the factors and the total score were calculated using the regression method. The scores of those who adhered to the Pap test were then compared with the scores of those who did not, using the t-Student test for independent samples. The regression method using a multiple ordinary least squares regression to predict each individual’s factor score based on their observed variables was used (48). The models were estimated using diagonally weighted least squares. The fit of the models was measured using the chi square statistic and two fit indices: the Comparative Fit Index (CFI) and the Tucker-Lewis index (TLI). The Root Mean Square Error of Approximation (RMSEA) was used as the parsimonious fit index. CFI and TLI values greater than 0.95, with RMSEA less than 0.05 are good; CFI and TLI values between 0.90 and 0.95, and RMSEA between 0.05 and 0.08 acceptable; and CFI and TLI values less than 0.90, or RMSEA greater than 0.08 unacceptable. The data were analyzed with the lavaan and psych packages of the R program. A p value <0.05 was considered significant.
The study was approved by the Ethics Committee of the Southeast Metropolitan Health Service, Santiago, Chile. Their signature of the informed consent document was requested from each of the women in the study.
The average age of the study group is 43.37 ± 10.77 years, and educational level is 10.97 ± 3.4 years. 63.7% of the women work for pay; 79.2% have a partner; 74.5% maintain sexual activity, with 2.69 ± 2.73 (range 1 to 40) being the number of sexual partners; 93.3% have children; and 58.9% use some method of family planning.
76.5% of the women (n = 741) reported having adhered to the Pap test in the last three years. Of the group of women who did not have a Pap test in that period (n = 228), 14% had never had a Pap test, and the remaining 86% reported having it for more than 3 years.
The items with their respective means and standard deviations are presented in Table 1.
For construct validity, the first model tested considered the distribution of the 20 items in the two factors of the original instrument. Given that the fit indices were not good, and the modification indices suggest transferring item 1.3 to the personal costs dimension, a second model was tested. The change of the item is welcome since the meaning of this corresponds to a personal cost. The second model showed acceptable adjustment indices; however, a correlation of 0.857 between both factors was presented, which suggested testing a second-order model. The third model tested was second-order; the results indicated acceptable adjustment indices, so it was decided to retain it. The fit indices of the three models tested are presented in Table 2. The standardized parameters of the final model and the significant correlations between the items are presented in Figure 1. Cronbach’s alpha for the total instrument is 0.95, 0.94 for the personal costs dimension, and 0.91 for the relationships dimension. The results of criterion validity are presented in Table 3.
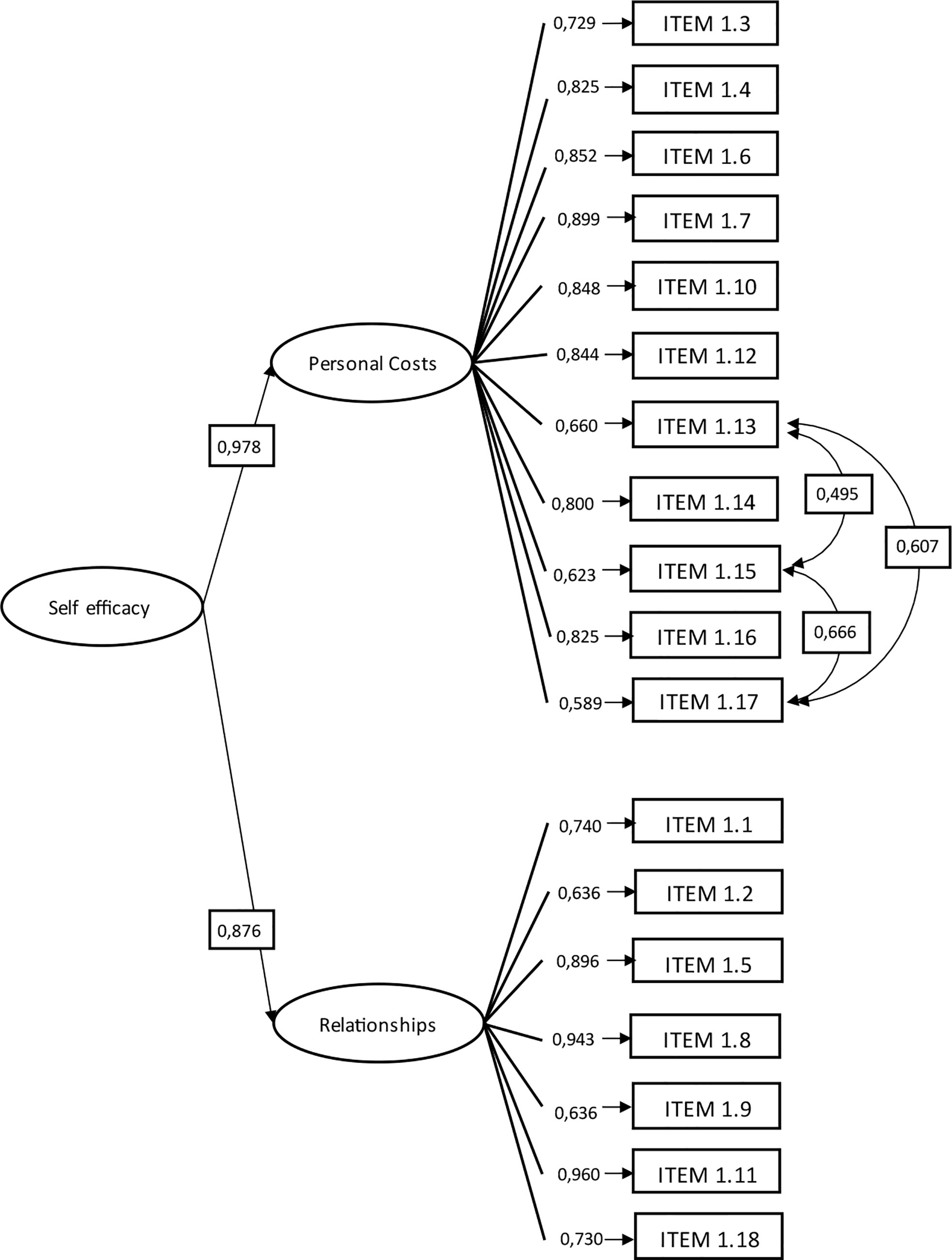
Figure 1 Factor loadings of first and second-order and correlations between items of the final model (n = 969).
The reduction of mortality and morbidity due to CC requires, among other things, the identification of factors that allow predicting adherence to Pap test; self-efficacy is a construct that had been related to CC screening. The main contribution of this study is the validation of an instrument to measure self-efficacy for taking Pap test, which can be very useful in both health care and research. Although there is another instrument validated in the Latino population that measures self-efficacy on this same topic (49), the SES-PSSP is important since it measures different situations that women could hypothetically face when deciding whether to adhere to screening. The possibility of posing different situations is a necessary condition to efficiently measure self-efficacy (2).
CC is an important public health problem in Latin America and the Caribbean. Therefore, having a questionnaire in Spanish will be very useful in measuring the self-efficacy of women and developing interventions to increase it because enhancement programs result in increased screening rates (50–52). Findings suggest that the inclusion of self-efficacy information in entertainment programming may lead to beneficial health outcomes (35).
Although the questionnaire was validated in the Chilean population, its usefulness transcends borders, since the Latino population shares cultural values that explain many health behaviors, including barriers to adherence to CC screening (53). Latina women in the United States have greater CC mortality rates than non-Latina women because of their low rates of screening (54). Receiving provider advice both directly and indirectly predicted Pap test adherence through greater self-efficacy (55). A systematic review found that self-efficacy is also a facilitator to CC screening in young people (56).
Related to the construct validation, in general, the factor loadings of the CFA are higher than in the PCA. This is a consequence of having a second-order factorial analysis, with different loads for each one of the dimensions, and therefore, the role of the items in each of the dimensions appears a little more precise.
The CFA carried out using a second-order model supports the two original dimensions proposed by the author of the SES-PSSP, and therefore provides sufficient evidence to consider the instrument valid and reliable. The confirmatory analysis in the Chilean population provides new evidence that both factors, validated in the original instrument, are explained by a second-order factor, self-efficacy. Although there is a difference between the characteristics of the women in the validation of the original instrument (47) and the Chilean sample, the instrument was maintained with the same items with high factor loads.
The change in item 1.3 from the relationship dimension to the personal cost dimension may be explained by the differences that exist between the women in both studies. The North American sample is an institutionalized population (inpatient), while the Chilean sample was drawn from the population belonging to primary health centers. Therefore, the fact of “being busy during office hours” is a personal cost for the Chilean woman, while for the North American, she is dependent on others. It has been previously described in the Chilean population that both office hours and waiting time are a difficulty for women when deciding to adhere to screening (57). The context in which each woman finds herself determines this difference.
When analyzing the moderate correlations between the items that are not explained by belonging to the personal costs factor, these could be explained by the three items referring to the use of alcohol or drugs. Since none of the correlations presented values above 0.8, all the items were kept in the instrument.
Finally, the results of the criterion validity provide additional strength to the instrument since higher scores in the total and in both dimensions of the instrument are significantly associated with adherence to the Pap test.
The World Health Organization’s efforts to eliminate CC by 2030 with a target of 70% screening coverage using a high-performance test necessitate that women increase participation in screening (58). Self-efficacy is a construct that has proven to be very useful in explaining health behaviors, and specifically to be included in interventions aimed at increasing women’s adherence to CC screening. Therefore, having a validated and reliable instrument in the Spanish language is very useful, both for professionals in the clinical field and those who carry out research in the area.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of the Southeast Metropolitan Health Service, Santiago-Chile. The patients/participants provided their written informed consent to participate in this study.
MT-U and OP contributed to conception and design of the study. MT-U and OP organized the database. OP performed the statistical analysis. MT-U wrote the first draft of the manuscript. Both authors contributed to manuscript revision, read, and approved the submitted version.
FONDECYT #11130626 “Determinantes Sociales para la Adherencia al Tamizaje de Cáncer Cervicouterino”/Social determinants for adherence to Cervical Cancer screening”
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bandura A. Health promotion by social cognitive means. Health Educ Behav (2004) 31(2):143–64. doi: 10.1177/1090198104263660
2. Bandura A, Adams A. Analysis of self-efficacy theory of behavioral change. Cognit Ter Res (1977) 1(4):287–310. doi: 10.1007/BF01663995
3. Lee EE, Nandy K, Szalacha L, Park H, Oh KM, Lee J, et al. Korean American Women and mammogram uptake. J Immigr Minor Health (2016) 18(1):179–86. doi: 10.1007/s10903-015-0164-6
4. Ahmadian M, Carmack S, Samah AA, Kreps G, Saidu MB. Psychosocial predictors of breast self-examination among female students in Malaysia: A study to assess the roles of body image, self-efficacy and perceived barriers. Asian Pac J Cancer Prev (2016) 17(3):1277–84. doi: 10.7314/APJCP.2016.17.3.1277
5. Lee CH, Kim YI. Effects of attitude, social influence, and self-efficacy model factors on regular mammography performance in life-transition aged women in Korea. Asian Pac J Cancer Prev (2015) 16(8):3429–34. doi: 10.7314/APJCP.2015.16.8.3429
6. Jerome-D'Emilia B, Suplee PD. Mammogram use and self-efficacy in an urban minority population. Public Health Nurs (2015) 32(4):287–97. doi: 10.1111/phn.12162
7. Sohler NL, Jerant A, Franks P. Socio-psychological factors in the expanded health belief model and subsequent colorectal cancer screening. Patient Educ Couns (2015) 98(7):901–7. doi: 10.1016/j.pec.2015.03.023
8. Farzaneh E, Heydari H, Shekarchi AA, Kamran A. Breast and cervical cancer-screening uptake among females in ardabil, northwest Iran: a community-based study. Onco Targets Ther (2017) 10:985–92. doi: 10.2147/OTT.S125344
9. Miller SJ, Iztkowitz SH, Redd WH, Thompson HS, Valdimarsdottir HB, Jandorf L. Colonoscopy-specific fears in African americans and hispanics. Behav Med (2015) 41(2):41–8. doi: 10.1080/08964289.2014.897930
10. Fernandez ME, Savas LS, Wilson KM, Byrd TL, Atkinson J, Torres-Vigil I, et al. Colorectal cancer screening among latinos in three communities on the Texas-Mexico border. Health Educ Behav (2015) 42(1):16–25. doi: 10.1177/1090198114529592
11. Wang HL, Christy SM, Skinner CS, Champion VL, Springston JK, Perkins SM, et al. Predictors of stage of adoption for colorectal cancer screening among African American primary care patients. Cancer Nurs (2014) 37(4):241–51. doi: 10.1097/NCC.0b013e3182a40d8d
12. Dehbari SR, Dehdari T, Dehdari L, Mahmoudi M. Predictors of sun-protective practices among Iranian female college students: Application of protection motivation theory. Asian Pac J Cancer Prev (2015) 16(15):6477–80. doi: 10.7314/APJCP.2015.16.15.6477
13. Kuo PF, Yeh YT, Sheu SJ, Wang TF. Factors associated with future commitment and past history of human papilloma virus vaccination among female college students in northern Taiwan. J Gynecol Oncol (2014) 25(3):188–97. doi: 10.3802/jgo.2014.25.3.188
14. Khodadadi AB, Hansen B, Kim YI, Scarinci IC. Latinx immigrant mothers' perceived self-efficacy and intentions regarding human papillomavirus vaccination of their daughters. Womens Health Issues (2022) 32(3):293–300. doi: 10.1016/j.whi.2021.10.009
15. Miller SM, Tagai EK, Wen KY, Lee M, Hui SA, Kurtz D, et al. Predictors of adherence to follow-up recommendations after an abnormal pap smear among underserved inner-city women. Patient Educ Couns (2017) 100(7):1353–9. doi: 10.1016/j.pec.2017.01.020
16. Ramaswamy M, Kelly PJ. "The vagina is a very tricky little thing down there": Cervical health literacy among incarcerated women. J Health Care Poor Underserved (2015) 26(4):1265–85. doi: 10.1353/hpu.2015.0130
17. Ghahremani L, Harami ZK, Kaveh MH, Keshavarzi S. Investigation of the role of training health volunteers in promoting pap smear test use among Iranian women based on the protection motivation theory. Asian Pac J Cancer Prev (2016) 17(3):1157–62. doi: 10.7314/APJCP.2016.17.3.1157
18. Nguyen AB, Clark TT, Belgrave FZ. Gender roles and acculturation: relationships with cancer screening among Vietnamese American women. Cultur Divers Ethnic Minor Psychol (2014) 20(1):87–97. doi: 10.1037/a0033474
19. Nguyen AB, Clark TT. The role of acculturation and collectivism in cancer screening for Vietnamese American women. Health Care Women Int (2014) 35(10):1162–80. doi: 10.1080/07399332.2013.863317
20. Dehdari T, Hassani L, Hajizadeh E, Shojaeizadeh D, Nedjat S, Abedini M. Effects of an educational intervention based on the protection motivation theory and implementation intentions on first and second pap test practice in Iran. Asian Pac J Cancer Prev (2014) 15(17):7257–61. doi: 10.7314/APJCP.2014.15.17.7257
21. Kessler TA. Increasing mammography and cervical cancer knowledge and screening behaviors with an educational program. Oncol Nurs Forum (2012) 39(1):61–8. doi: 10.1188/12.ONF.61-68
22. Yang YL, Liu L, Wang XX, Wang Y, Wang L. Prevalence and associated positive psychological variables of depression and anxiety among Chinese cervical cancer patients: a cross-sectional study. PloS One (2014) 9(4):e94804. doi: 10.1371/journal.pone.0094804
23. Ghalavandi S, Heidarnia A, Zarei F, Beiranvand R. Knowledge, attitude, practice, and self-efficacy of women regarding cervical cancer screening. Obstet Gynecol Sci (2021) 64(2):216–25. doi: 10.5468/ogs.20236
24. Bunkarn O, Kusol K. The relationship between perceived self-efficacy and cervical cancer screening among village health volunteers in suratthani province, Thailand. Asian Pac J Cancer Prev (2021) 22(1):179–83. doi: 10.31557/APJCP.2021.22.1.179
25. Juwitasari, Harini R, Rosyad AA. Husband support mediates the association between self-efficacy and cervical cancer screening among women in the rural area of Indonesia. Asia Pac J Oncol Nurs (2021) 8(5):560–4. doi: 10.4103/apjon.apjon-2085
26. Ngune I, Kalembo F, Loessl B, Kivuti-Bitok LW. Biopsychosocial risk factors and knowledge of cervical cancer among young women: A case study from Kenya to inform HPV prevention in Sub-Saharan Africa. PloS One (2020) 15(8):e0237745. doi: 10.1371/journal.pone.0237745
27. Salehiniya H, Momenimovahed Z, Allahqoli L, Momenimovahed S, Alkatout I. Factors related to cervical cancer screening among Asian women. Eur Rev Med Pharmacol Sci (2021) 25(19):6109–22. doi: 10.26355/eurrev_202110_26889
28. Lee YH, Huang LH, Chen SH, Shao JH, Lai CH, Yang NP. Effects of mobile application program (App)-assisted health education on preventive behaviors and cancer literacy among women with cervical intraepithelial neoplasia. Int J Environ Res Public Health (2021) 18(21):11603. doi: 10.3390/ijerph182111603
29. Calderón-Mora J, Alomari A, Byrd TL, Shokar NK. Evaluation of a narrative video to promote prevention and early detection of cervical cancer among latinas. Health Promot Pract (2021) 23(5):884–91. doi: 10.1177/15248399211038943
30. Luque JS, Tarasenko YN, Reyes-Garcia C, Alfonso ML, Suazo N, Rebing L, et al. Salud es Vida: a cervical cancer screening intervention for rural latina immigrant women. J Cancer Educ (2017) 32(4):690–9. doi: 10.1007/s13187-015-0978-x
31. Mohammad Z, Ahmad N, Baharom A. The effects of theory-based educational intervention and WhatsApp follow-up on papanicolaou smear uptake among postnatal women in Malaysia: Randomized controlled trial. JMIR Mhealth Uhealth (2022) 10(6):e32089. doi: 10.2196/32089
32. Ghalavandi S, Zarei F, Heidarnia A, Beiranvand R. A blended educational intervention program on pap-test related behavior among Iranian women. Reprod Health (2021) 18(1):228. doi: 10.1186/s12978-021-01281-x
33. Babazadeh T, Nadrian H, Rezakhani Moghaddam H, Ezzati E, Sarkhosh R, Aghemiri S. Cognitive determinants of cervical cancer screening behavior among housewife women in Iran: An application of health belief model. Health Care Women Int (2018) 39(5):555–70. doi: 10.1080/07399332.2018.1425873
34. Majdfar Z, Khodadost M, Majlesi F, Rahimi A, Shams M, Mohammadi G. Relationships between self-efficacy and pap smear screening in Iranian women. Asian Pac J Cancer Prev (2016) 17(S3):263–8. doi: 10.7314/APJCP.2016.17.S3.263
35. Kim S, Hmielowski JD. The influence of self-efficacy in medical drama television programming on behaviors and emotions that promote cervical cancer prevention. Am J Health Behav (2017) 41(6):719–27. doi: 10.5993/AJHB.41.6.6
36. Hajek A, Bock JO, Konig HH. The role of general psychosocial factors for the use of cancer screening-findings of a population-based observational study among older adults in Germany. Cancer Med (2017) 6(12):3025–39. doi: 10.1002/cam4.1226
37. Moore de Peralta A, Holaday B, McDonell JR. Factors affecting Hispanic women's participation in screening for cervical cancer. J Immigr Minor Health (2015) 17(3):684–95. doi: 10.1007/s10903-014-9997-7
38. Luszczynska A, Durawa AB, Scholz U, Knoll N. Empowerment beliefs and intention to uptake cervical cancer screening: three psychosocial mediating mechanisms. Women Health (2012) 52(2):162–81. doi: 10.1080/03630242.2012.656187
39. Gemeda EY, Kare BB, Negera DG, Bona LG, Derese BD, Akale NB, et al. Prevalence and predictor of cervical cancer screening service uptake among women aged 25 years and above in sidama zone, southern Ethiopia, using health belief model. Cancer Control (2020) 27(1):1073274820954460. doi: 10.1177/1073274820954460
40. Solomon K, Tamire M, Kaba M. Predictors of cervical cancer screening practice among HIV positive women attending adult anti-retroviral treatment clinics in bishoftu town, Ethiopia: the application of a health belief model. BMC Cancer (2019) 19(1):989. doi: 10.1186/s12885-019-6171-6
41. Nair UN, Madhivanan P, Saad ER, Adsul P. Multi-level factors are associated with uptake of cervical cancer screening in sexual and gender diverse adults residing in Arizona. Cancer Epidemiol Biomarkers Prev (2022) 31(7):1510. doi: 10.1158/1055-9965.EPI-22-0473
42. Higgins LM, Dirksing KN, Ding L, Morrow CD, Widdice LA, Kahn JA. Adolescents' intention and self-efficacy to follow pap testing recommendations after receiving the HPV vaccine. Hum Vaccin Immunother (2016) 12(6):1498–503. doi: 10.1080/21645515.2016.1150395
43. Tung WC, Smith-Gagen J, Lu M, Warfield M. Application of the transtheoretical model to cervical cancer screening in latina women. J Immigr Minor Health (2016) 18(5):1168–74. doi: 10.1007/s10903-015-0183-3
44. Tiraki Z, Yılmaz M. Cervical cancer knowledge, self-efficacy, and health literacy levels of married women. J Cancer Educ (2018) 33(6):1270–8. doi: 10.1007/s13187-017-1242-3
45. Soper DS. A-priori sample size calculator for structural equation models [Software]. (2003). Available at: https://www.danielsoper.com/statcalc
47. Hogenmiller JR, Atwood JR, Lindsey AM, Johnson DR, Hertzog M, Scott JC Jr. Self-efficacy scale for pap smear screening participation in sheltered women. Nurs Res (2007) 56(6):369–77. doi: 10.1097/01.NNR.0000299848.21935.8d
48. Logan JAR, Jiang H, Helsabeck N, Yeomans-Maldonado G, et al. Should I allow my confirmatory factors to correlate during factor score extraction? implications for the applied researcher. Qual Quant (2022) 56(4):2107–31. doi: 10.1007/s11135-021-01202-x
49. Fernandez ME, Diamond PM, Rakowski W, Gonzales A, Tortolero-Luna G, Williams J, et al. Development and validation of a cervical cancer screening self-efficacy scale for low-income Mexican American women. Cancer Epidemiol Biomarkers Prev (2009) 18(3):866–75. doi: 10.1158/1055-9965.EPI-07-2950
50. Bunkarn O, Kusol K, Eksirinimit T. The outcome of a self-efficacy enhancement program for cervical cancer screening among women in phrasaeng district, suratthani province, Thailand. Asian Pac J Cancer Prev (2020) 21(7):2075–81. doi: 10.31557/APJCP.2020.21.7.2075
51. Ebu NI, Amissah-Essel S, Asiedu C, Akaba S, Pereko KA. Impact of health education intervention on knowledge and perception of cervical cancer and screening for women in Ghana. BMC Public Health (2019) 19(1):1505. doi: 10.1186/s12889-019-7867-x
52. Figueroa-Muñoz Ledo AA, Márquez-Serrano M, Idrovo AJ, Allen-Leigh B. Individual and community effectiveness of a cervical cancer screening program for semi-urban Mexican women. J Community Health (2014) 39(3):423–31. doi: 10.1007/s10900-013-9802-x
53. Chong N. The Latino patient. In: A cultural guide for health care providers, 1st ed. London: Intercultural Press (2002).
54. Tung WC, Lu M, Smith-Gagen J, Yao Y. Latina women and cervical cancer screening: Decisional balance and self-efficacy. Clin J Oncol Nurs (2016) 20(3):E71–6. doi: 10.1188/16.CJON.E71-E76
55. Kim K, Xue QL, Walton-Moss B, Nolan MT, Han HR. Decisional balance and self-efficacy mediate the association among provider advice, health literacy and cervical cancer screening. Eur J Oncol Nurs (2018) 32:55–62. doi: 10.1016/j.ejon.2017.12.001
56. Kirubarajan A, Leung S, Li X, Yau M, Sobel M. Barriers and facilitators for cervical cancer screening among adolescents and young people: a systematic review. BMC Womens Health (2021) 21(1):122. doi: 10.1186/s12905-021-01264-x
57. Urrutia MT, Araya A, Jaque MF. Why do Chilean women choose to have or not have pap tests? J Obstet Gynecol Neonatal Nurs (2017) 46(1):e3–e12. doi: 10.1016/j.jogn.2016.09.002
Keywords: uterine cervical neoplasms, Papanicolaou test, self-efficacy, reproducibility of results, surveys and questionnaires. 2
Citation: Urrutia M-T and Padilla O (2022) Validity of a questionnaire on self-efficacy for Pap test adherence screening. Front. Oncol. 12:979799. doi: 10.3389/fonc.2022.979799
Received: 28 June 2022; Accepted: 13 October 2022;
Published: 26 October 2022.
Edited by:
Lucely Cetina-Pérez, National Institute of Cancerology (INCAN), MexicoReviewed by:
Leila Allahqoli, Iran University of Medical Sciences, IranCopyright © 2022 Urrutia and Padilla. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: María-Teresa Urrutia, bWFyaWEudXJydXRpYUB1bmFiLmNs
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.