
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Oncol., 22 August 2022
Sec. Cancer Epidemiology and Prevention
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.959852
This article is part of the Research TopicRacial Health Disparity in Cancer: Assessments of NeedView all 12 articles
Liver cancer incidence has tripled since the early 1980s, making this disease one of the fastest rising types of cancer and the third leading cause of cancer-related deaths worldwide. In the US, incidence varies by geographic location and race, with the highest incidence in the southwestern and southeastern states and among racial minorities such as Hispanic and Black individuals. Prognosis is also poorer among these populations. The observed ethnic disparities do not fully reflect differences in the prevalence of risk factors, e.g., for cirrhosis that may progress to liver cancer or from genetic predisposition. Likely substantial contributors to risk are environmental factors, including chemical and non-chemical stressors; yet, the paucity of mechanistic insights impedes prevention efforts. Here, we review the current literature and evaluate challenges to reducing liver cancer disparities. We also discuss the hypothesis that epigenetic mediators may provide biomarkers for early detection to support interventions that reduce disparities.
Primary liver cancer incidence has tripled since the early 1980s, with most cases (~75%) classified as hepatocellular carcinoma (HCC). Liver cancer is among the fastest increasing cancers, and is the third leading cause of cancer-related deaths worldwide and in the US (1). While the incidence increased until 2015, it appears to have plateaued among Asians/Pacific Islanders. Among non-Hispanic Blacks and American Indians/Alaska Natives, the incidence of HCC continues to increase (2).
In the US, over 40,000 primary liver cancer cases are diagnosed annually, but the incidence not only varies by race/ethnicity, but also by geographic location. The highest liver cancer incidence is in the Western and Southern US and among ethnic minorities. Data from 2005 to 2014 suggest that the US age-adjusted incidence rate was 6–7.7/100,000 overall; yet, in Non-Hispanic Black individuals the rate was 10–13/100,000 and in Hispanics was 13–17/100,000 during the same period (3–6). Moreover, two-year survival is approximately 50%, and prognosis is poorer in minority populations (7–10). While deaths related to other malignancies such as lung, breast, and colorectal cancer declined over 40% from 1990–2016, liver cancer mortality is rising among both men and women (11). Consequently, liver cancer is projected to surpass breast and colorectal cancer by 2030 to become the leading cause of cancer-related death in the US (12). The underlying causes of this rapid increase that disproportionately affects racial minorities are poorly understood.
The majority of HCC (over 90%) occurs in the background of chronic liver disease with cirrhosis of any etiology being the strongest risk factor (13). HCC has traditionally been driven by chronic liver disease from viral infections such as chronic hepatitis B virus (HBV) and hepatitis C virus (HCV). Increased vaccine rates and successful treatments have been associated with major declines in the incidence of HCC from these etiologies. However, the prevalence of these risk factors cannot fully explain the ethnic disparities observed. More recent data support a shifting of the underlying etiologies of HCC primarily due to the high prevalence of metabolic conditions that include obesity and diabetes, which increase the risk of non-alcoholic fatty liver disease (NAFLD) and its progression to NASH and cirrhosis. (14, 15). NAFLD represents a spectrum of chronic liver disease associated with obesity and insulin resistance that includes simple accumulation of fat in the liver (i.e., simple steatosis), to more severe non-alcoholic steatohepatitis (NASH) in which steatosis is complicated by necroinflammation and fibrosis, to cirrhosis, the end stage of fibrosis and scarring of the liver (16, 17). Although the potential for NAFLD to progress to fibrosis, cirrhosis and HCC is well established, progression, and thus HCC risk varies substantially by age and obesity status (Figure 1).
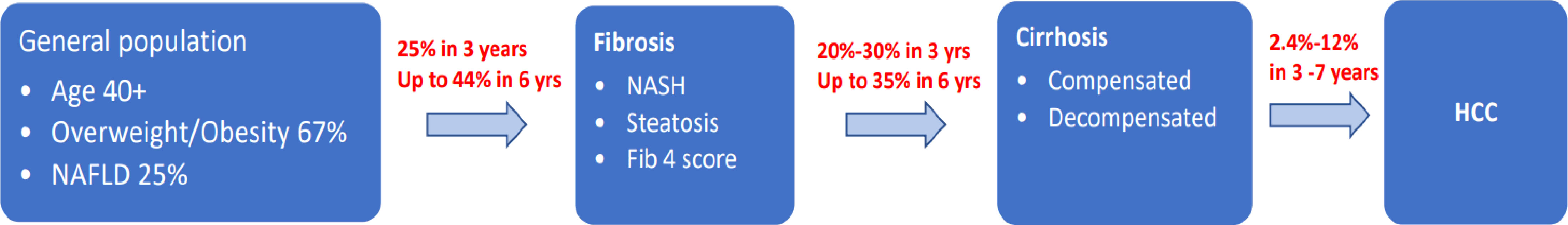
Figure 1 Conceptual model for progression from metabolic dysfunction, NAFLD, NASH, Cirrhosis and HCC.
The prevalence of metabolic conditions such as obesity and type II diabetes (but not NAFLD) is also higher in Non-Hispanic Black, Hispanic, and Native American individuals. In the US, 31% of adults are overweight and approximately 10% are severely obese (18). National Health and Nutrition Examination Survey (NHANES) data from 2017–18 suggest that the age-adjusted prevalence of overweight/obesity varies by race among adults, with the highest incidence among Non-Hispanic Black (50%), followed by Hispanic (45%), Non-Hispanic white (42%), and Asian (17%) individuals. Similar race/ethnic prevalence patterns were reported for type II diabetes mellitus: among Non-Hispanic Black and Hispanic individuals, the prevalence is 13.2% and 12.8% respectively, whereas in Asian individuals it is 7.6% and in non-Hispanic white individuals it is 9% (19). Addressing disparities in liver cancer incidence and mortality requires rigorous investigation of upstream factors that give rise to metabolic derangement and progression to NAFLD, fibrosis, and cirrhosis that eventually leads to liver decompensation, liver cancer, and death. Advances in (epi)genomic sequencing technologies may help identify molecular mechanisms and events that promote liver deterioration. Molecular markers of liver cancer, that include genetic variants in genes such as PNPLA3, and epigenetic shifts largely identified from array data, are being developed into early detection tools aimed at reducing HCC risk and inherent ethnic disparities. Here, we review clinical and lifestyle risk factors for liver disease, the potential role of environmental exposures in liver cancer development, and the emerging role of epigenetics as a marker of past exposure to environmental contaminants, and contributor to liver cancer risk.
The Centers for Disease Control and the National Academy of Sciences estimates that environmental exposures account for at least 70% of variation in many chronic diseases risk, including liver diseases. Exposure to aflatoxin B1–lysine, cigarette smoking, mycotoxins, HBV and HCV infection, and poor access to treatment modalities increase liver disease risk including liver cancer. These findings now inform clinical practice to prevent these exposures and/or reduce the risk of progression. Conversely, habitual coffee intake and long-term statin and metformin use have protective effects on the liver. Indeed, much of this information is included in public health education. Association between comorbidities and drugs used to treat them, lifestyle factors such as diet, physical activity, and non-chemical stressors/social stressors and liver cancer are poorly characterized. Analgesics, such as acetaminophen, may also be linked to liver cancer. Together, data accumulated over the last two decades indicate that the prevalence of these risk factors disproportionately affects ethnic minorities, though data regarding risk factors among these populations remain sparse. Nonetheless, the prevalence of viral hepatitis infections, NAFLD, alcohol use, and exposure to mycotoxins, do not fully explain the continued HCC increase, especially the ethnic or geographic variation in liver disease.
Co-morbidities and the drugs used to treat them may also alter HCC risk. Prenatal acetaminophen exposure in mice results in loss of fetal liver stem cells, altering immune function (20, 21) and in adults, acetaminophen is the leading cause of acute liver injury/failure. Acetaminophen targets the liver and may interact with environmental contaminants such as cadmium that naturally target the liver, to increase risk of liver damage. Acetaminophen is used routinely by ~56% of the US population (22). Conversely, metformin and statins reduce HCC risk (23, 24). Accurate retrospective assessment of pharmaceuticals taken routinely for common ailments e.g., colds, or pain, is challenging. Another challenge is the lag in statistical methods development to investigate the effects of exposure to multiple drugs (i.e., drug mixtures).
Mounting evidence including high-quality randomized trials link anti-inflammatory diets, such a Mediterranean-style diet, to improvement in chronic diseases including cardiovascular diseases (25), reduced breast cancer incidence (26), and reduced metabolic diseases (27, 28). Coffee consumption is associated with lowered HCC risk while processed meat high in nitrates increases liver cancer risk and may also support liver cancer progression and mortality due to carcinogens released from nitrates that accelerate tumor growth. Diets rich in fruits, vegetables, and antioxidants reduce liver cancer risk, severity, and mortality (29–34). Certain dietary patterns (e.g., Mediterranean, glycemic index/load, or dietary inflammation index) decrease other biliary cancer risk (35–37), but little is known about the effects of diet on HCC prognosis. Moreover, non-pregnant minority adults report less adherence to these diets (38, 39). Mechanistically, anti-inflammatory diets reduce systemic free radicals and oxidative stress, leading to decreased circulating pro-inflammatory cytokines and chemokines (40–43).
Physical activity may reduce liver cancer risk and severity and improve outcomes in human studies and animal models. Inconsistent evidence supports the association between light, moderate, or vigorous physical activity and low liver cancer risk (44–47). Lack of consistency in findings is likely because physical activity tends to benefit subsets of populations, likely with other risk factors, such as smokers or obese individuals. However, a recent meta-analysis found that physical activity helped reduce liver cancer risk and mortality in a dose-dependent manner. At a minimum, two hours/week of physical activity was associated with reduced risk of liver cancer mortality (48).
Cigarette smoking is a source of non-occupational exposure to multiple exogenous chemicals, including cadmium, a chemical with oncogenic potential, and alcohol is associated with alcoholic cirrhosis such that these lifestyle factors may either modify or directly interact to increase HCC risk. Conversely, meta-analyses using data accumulated over the last two decades suggest that coffee intake reduces HCC and other liver cancer risk (49–54). However, the mechanisms underlying these connections are unclear.
Social stressors captured at the neighborhood level are persistent risk factors for disparities in a range of cancer outcomes (55). In the US, neighborhood ethnic composition is a strong predictor of hazardous toxicant exposure (56–58). Early data suggests that the racial distribution of the geographic cluster with the highest cadmium exposure is 2% white, 78% Black, and 14% Hispanic (59). Neighborhood disadvantage scores revealed that disadvantage is associated with elevated exposure to environmental contaminants such as cadmium, a probable carcinogen, in adults (59).
HCC risk is higher in males and mortality varies by sex, as do competing risk factors, e.g., moderate/heavy alcohol intake while overweight status is more common in men and obesity is more common in women. Conversely, women have higher concentrations of contaminants in their bodies, such as cadmium, compared to men who experience similar exposure levels. This may result from higher gastrointestinal absorption of cadmium (60) in women or from competitive binding of cadmium to transporters that are typically bound by nutritive elements such as iron and selenium and may be depleted (60). Moreover, poor cadmium excretion leads to bioaccumulation and increased urinary cadmium with age.
Chronic environmental contaminant exposure is understudied yet may contribute substantially to metabolic dysfunction, fatty liver, fibrosis, and HCC. Increased industrial applications of toxic metals such as cadmium, arsenic, and lead as well as per- and poly-fluoroalkyl substances (PFAS) (e.g., perfluoro-octanoic acid; PFOA, or perfluoro-octane sulfonic acid; PFOS) coupled with their slow degradation has increased these environmental pollutants in atmospheric, terrestrial, and aquatic systems. Their persistence in the environment provides a stable exogenous source for human exposure. Once in the body, slow excretion leads to bioaccumulation in primary organs of metabolism, including the liver (61), with a half-life in the body of 30–45 years for cadmium (59, 62) and up to 5 years for PFOA (63–65). Toxic metals such as cadmium and arsenic are classified as probable human carcinogens by the International Agency for Research on Cancer (66) and ranked in the top ten environmental chemicals of concern by the Agency for Toxic Substances and Disease Registry (ATSDR) (67), while PFOA is classified as a possible carcinogen. Whereas hepato-toxic effects of contaminants such as cadmium at high levels characteristic of occupational settings are well-documented (reviewed in 66), data are limited regarding exposure at levels experienced by the general population.
PFAS are widely used in food packaging, flame-retardants, scratch-resistant coating, fire-fighting foam, and metal plating. Notably, PFAS were identified as drinking water contaminants throughout the US, with roughly 6 million Americans drinking water that exceeds EPA guidelines for safe levels of PFOA and PFOS (64). When all PFAS are considered or more stringent guidelines are used, the estimate is much higher. Additionally, metal exposure is also widespread; arsenic is naturally present in some water supplies and cadmium is a constituent of tobacco smoke and is present in some commercial fertilizers (68–71) such that ingestion of dietary staples contributes to exposure. In the US, dietary cadmium intake is estimated at ~1 µg/day (72, 73). In pregnant women in Durham, NC, cadmium and PFOA were found to co-contaminate house dust that can be ingested or inhaled (59). Serum PFAS levels are also higher in non-Hispanic white and Hispanic than in non-Hispanic Black pregnant women (74, 75). Further, among all adults, rural African Americans have higher concentrations (76). In contrast, cadmium body burden is highest in African American and Hispanic individuals (62, 77, 78)—populations with a higher HCC incidence. The US National Toxicology Program has called for further research on the effects of these environmental chemicals on organ dysfunction, including liver cancers (79). Multiethnic cohort investigations are needed to determine the impact of toxic metals and PFAS exposure on liver fibrosis and HCC.
Data linking environmental contaminants to NAFLD or HCC are limited. Data from in vitro and in vivo models accumulated over the last decade support the hypothesis that exposure to PFAS or toxic metals such as cadmium and arsenic induces NAFLD/NASH and liver carcinogenesis (66). However, doses used to induce liver diseases in experimental settings were orders of magnitude higher than those experienced by the general population. The hypothesis that exposure to chemicals such as cadmium increases fatty liver risk and progression to fibrosis, cirrhosis, and HCC is supported by weak evidence in humans. These data include autopsy data that demonstrate that concentrations of both toxic metals such as cadmium, and PFAS such as PFOS and PFOA, are higher in the liver than other organs sites with increasing cancer incidence (e.g., pancreas, ovary) (80–82), indicating that the liver is a main repository for these organic and inorganic chemicals. These autopsy data are supported by murine models data that have demonstrated significantly higher liver fat fractions consistent with fatty liver disease and hepatic neoplastic lesions, found in mice exposed to cadmium at concentrations equivalent to non-occupational exposure (83). In human populations, consistent with geographic information systems (GIS) data (59), findings based on a representative sample of Americans (NHANES) (84) suggest that urinary cadmium—an established dosimeter for long-term exposure, is higher in African American and Hispanic than in white individuals, and is associated with overall liver cancer risk, mortality, and the HCC precursors, NAFLD and NASH. However, there was a limited number of African Americans in the study and the data are cross-sectional.
Although these findings support higher body burdens of at least one toxic metal individually contributing to HCC and precursors such as NAFLD, NASH, and cirrhosis, multiple challenges to defining the link between environmental exposures and liver cancer remain. First, HCC incidence requires a population-based case–control design, relying on cancer registries for case identification. However, cancer registry-based rapid case ascertainment systems for case identification are ill-suited for studying HCC, since most (80%) cases are diagnosed solely based on radiographic imaging. Thus, case-control studies that rely on rapid case ascertainment systems may be biased toward the ~20% of cases whose identification relies on biopsy tissue from transplant patients. Consequently, ethnic minorities at higher risk of liver diseases are likely under-represented. Further, advances in mass spectrometry (MS) (e.g., liquid or gas chromatography (LC/GC) for PFAS and inductively coupled plasma mass spectrometry (ICP-MS) for metals, human data from NHANES, and from our group support environmental co-occurrence of PFAS, such as PFOA and PFOS, and toxic metals, such cadmium, arsenic, and lead (85). These toxins also co-occur in the blood or urine of Americans (86–89). Interaction profiles from in vitro models of the ATSDR (67) also support that at least for toxic metals, the effects of toxic metals such as cadmium, lead, and arsenic are synergistic. Yet, statistical methods to identify chemical mixtures contributing to health outcomes are limited and may require large sample sizes. Studies that focus on surmounting these challenges will greatly benefit the field.
Perhaps one of the biggest challenges in investigating the role of environmental contaminants in liver disease and cancer risk, in general, is the need for retrospective exposure assessment and comparing exposure odds in individuals with and without cancer. Indeed, case–control design is most efficient and is sufficient to investigate exposures such as urinary cadmium, an established dosimeter estimating the cumulative body burden over the life course, to investigate liver cancer etiology. However, the body burden of contaminants such as lead, arsenic, PFOA, and PFOS measured at cancer diagnosis are unlikely to reflect the body before diagnosis. This temporal ambiguity between environmental contaminant assessment and HCC is one of the main complications for causal inference. One way of circumventing this challenge requires molecular profiling that mediates exposure and outcomes.
While twin and familial studies estimate cancer heritability and its precursors such as obesity from 40 to 70%, cancer etiology is complex. Genetic loci contribute to less than 10% of obesity variation. Rather, heritable environmentally induced-epigenetic adaptation, including dysregulation of growth regulating genes, drives heritability, although the regions of the epigenome that contribute to liver diseases are undefined. Epigenetic marks act as exposure archives that approximate past exposure (90, 91). This is in part because epigenetic regulation, a means by which gene expression is altered in response to environmental exposures, can cause long-term changes in expression in mechanistic pathways contributing to liver injury, dysmetabolism, nutrient acquisition, fat deposition, appetite, and satiety. Both covalent DNA methylation at cytosines of CpG dinucleotides and histone modifications regulate chromatin structure and gene expression. The value of DNA methylation as an assay target is its stability. This enables its measurement from nearly any sample type, regardless of handling, by utilizing both targeted and high-throughput bisulfite sequencing methods.
Human epigenetic data linking liver cancer and its precursors to epigenetic dysregulation has three main challenges that hamper identification of epigenomic regions mechanistically involved in cancer development. First, clinically accessible peripheral cells (e.g., blood or buccal cells) may not be appropriate surrogates for tissue types of etiologic significance to liver cancer. Second, epigenetic marks respond to environmental cues throughout the life course such that without serial samples, inference of cause-and-effect between obesity and any epigenetic alterations is difficult. Additionally, epigenetic marks associated with obesity are often identified from known regions or genes, targeted by function. Moreover, agnostic approaches use array technology (e.g., Golden Gate, 14K, 27K, 450K, or EPIC), but there are physical limitations such as the limited number of CpGs per array, and these approaches are selected based on predetermined criteria of likely significance. For example, while target regions have been selected to cover gene promoters and bodies, as well as CpG islands, with >28 million CpG sites in the genome, less than 5% are covered. Thus, the scope of affected regions is unknown. Another genome-wide tool, meDIP, covers ~40% of the genome, but is dependent on antibody precipitation of methylcytosine, and is thus more effective in CG-rich regions. Also, because meDIP captures only methylated sites, accurate quantitation of methylation percentage is not feasible. Reduced representation bisulfite sequencing is genome-wide but covers ~10% of CpG sites due to technological dependence on endonuclease recognition of specific sites. While these methods are all highly informative for measurable regions, many epigenetic regions occur at long (>10-20kb) distances from gene bodies, and in areas of low CG content. Thus, the coverage has selection/sequence bias.
Addressing these challenges in epidemiologic settings requires multiple approaches to identify epigenomic regions of functional relevance that link environmental exposures and liver dysfunction. These include using agnostic genome scale approaches such as whole-genome bisulfite sequencing or agnostic arrays (e.g., EPIC850 methylation array) and case and control specimens to identify genomic regions that differ between cases and controls in a cell type accessible for both cases and controls, e.g., blood. This step is followed by determination of the relevance of the marker, in affected cancer tissues. Among regions with a high likelihood of being functionally important, follow-up investigation determining if the epigenetic marks with case–control differences that are also found in relevant tissues are stable over time, and thus unlikely to be caused by disease, is performed to establish cause-and-effect. Finally, the biological significance in cancer is determined. Because these approaches have limitations to identifying epigenetic markers for liver cancer risk overtime, circumventing these challenges requires inclusion of molecular profiling that mediates exposures and outcomes in large cohorts with long-term follow up, such us the All of Us study (https://allofus.nih.gov/news-events-and-media/announcements/all-us-research-program-initial-protocol).
Another limitation of epigenetics studies is that environmental exposures affecting the epigenome may cause temporary changes in methylation that could be reverted after the exposure is no longer present. Thus, it is important to focus on CpG methylation marks that are stochastically established before specifications that control metastable epiallele expression (92) and imprinting control regions (ICR) that regulate imprinted gene monoallelic expression (93, 94). Methylation marker stability with age also makes them long-term ‘records’ of early exposures that are difficult to obtain through questionnaires or other exposure assessment assays (93). CpG methylation of metastable epialleles and ICRs is established before gastrulation and are mitotically heritable. Thus, epigenetic marks are similar across tissues and cell types throughout the individual’s life. Unlike metastable epialleles, however, ICRs are defined by parent-of-origin specific methylation marks that are important gene dosage regulators based on the allele’s parental origin. Consequently, in contrast to epigenetic marks controlling metastable epiallele expression, methylation marks regulating imprinted genes are similar across individuals (95, 96). Importantly, changes in ICR methylation patterns are implicated in adult-onset diseases suspected to have fetal origins, including neurological disorders, cancers, and metabolic diseases stemming from abnormal growth and nutrient acquisition disorders (97, 98). With the recent publication mapping the complete repertoire of human ICRs (99), examining the effects ICR dysregulation on liver diseases, including cancer, should yield new insights.
Chronic exposure to environmental contaminants characteristic of non-occupational settings results in subtle molecular adaptive responses detectable as methylation marks at epigenetically labile CG dinucleotides (100–102). Targeted methylation sequencing approaches demonstrated that cadmium alone or in a mixture with arsenic is associated with hypermethylation of the DLK1/MEG3 imprinted domain in leukocyte-derived DNA (103). Conversely, untargeted whole genome bisulfite sequencing revealed that cadmium exposure was associated with differential methylation, at ~2,000 loci (104). Recent studies using Illumina Beadchip arrays also support that DNA methylation of two CG dinucleotides, measured in cell-free DNA, can distinguish HCC from cirrhosis with both sensitivity and specificity in excess of 90% (105). Intriguingly, these CG dinucleotides map to two genes that are key components of the extracellular matrix, epithelial to mesenchymal transition, and signaling (106). This is consistent with dying hepatocytes contributing to the pool of circulating DNA in plasma (107) and the observation that up to 70% of cell free DNA in HCC cases is contributed by the liver (107–109). While these data suggest methods for etiologic investigations and early detection using accessible cells of relevance circulating in plasma, the role of environmental contaminants in methylation alterations has not been examined. Further, racial minorities have not been included in case–control design, hampering causal inference.
Similarly, circulating cell-free RNA is comprised of different classes of RNA, including messenger, micro, circular, long-coding, transfer, ribosomal, and mitochondrial RNAs. RNA pools reflect physiological and pathophysiological insight into human health and have the potential for diagnostic and prognostic markers of disease and monitoring (110, 111). The most studied group of cell free RNAs are miRNAs that can target and regulate genomic output through multiple mechanisms (112) and are an emerging class of effector molecules regulated by diet (113). These miRNAs circulate throughout the body and due to their size and stability are found in most bodily fluids including blood, urine, saliva, breast milk, and tears (114, 115). The epigenome regulates miRNAs and in turn, miRNAs reciprocally regulate DNA methylation by inhibiting DNA-modifying enzymes (116). However, inclusion of racial minorities under-represented in epidemiological research studies remains low, which challenges the interpretation of existing data. Better representation of these groups is needed to understand disparities in liver cancer and in the development of early detection methods.
Racial/ethnic disparities in the incidence of cancers such as HCC is paralleled by increased prevalence of environmental contaminants. The inflammatory effects of environmental exposures may be modulated by disparities in lifestyle factors, comorbidities, and higher body burden of environmental contaminants. Resilience factors such as anti-inflammatory diets may mitigate exposure effects and are linked with a lower liver cancer prevalence among ethnic minorities. However, establishing the effects of risk factors in epidemiologic studies is complicated by retrospective exposure assessment. These shortcomings may be circumvented by a more detailed knowledge of epigenetic responses linking environmental exposures to cancer outcomes.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funded by NIH R01HD098857, R01ES093351, and R01MD011746-S1.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kim D, Li AA, Perumpail BJ, Gadiparthi C, Kim W, Cholankeril G, et al. Changing trends in etiology-based and ethnicity-based annual mortality rates of cirrhosis and hepatocellular carcinoma in the united states. Hepatology (2019) 69(3):1064–74. doi: 10.1002/hep.30161
2. McGlynn KA, Petrick JL, El-Serag HB. Epidemiology of Hepatocellular Carcinoma. Hepatology (2021) 73(Suppl 1):4–13. doi: 10.1002/hep.31288.
3. Islami F, Miller KD, Siegel RL, Fedewa SA, Ward EM, Jemal A. Disparities in liver cancer occurrence in the united states by race/ethnicity and state. CA Cancer J Clin (2017) 67(4):273–89. doi: 10.3322/caac.21402
4. White DL, Thrift AP, Kanwal F, Davila J, El-Serag HB. Incidence of hepatocellular carcinoma in all 50 United States, from 2000 through 2012. Gastroenterology (2017) 152(4):812–820 e815. doi: 10.1053/j.gastro.2016.11.020
5. Endeshaw M, Hallowell BD, Razzaghi H, Senkomago V, McKenna MT, Saraiya M. Trends in liver cancer mortality in the united states: Dual burden among foreign- and US-born persons. Cancer (2019) 125(5):726–34. doi: 10.1002/cncr.31869
6. Hallowell BD, Endeshaw M, McKenna MT, Senkomago V, Razzaghi H, Saraiya M. Cancer mortality rates among US and foreign-born individuals: United States 2005-2014. Prev Med (2019) 126:105755. doi: 10.1016/j.ypmed.2019.105755
7. Ha J, Yan M, Aguilar M, Bhuket T, Tana MM, Liu B, et al. Race/ethnicity-specific disparities in cancer incidence, burden of disease, and overall survival among patients with hepatocellular carcinoma in the United States. Cancer (2016) 122(16):2512–23. doi: 10.1002/cncr.30103
8. Ha J, Yan M, Aguilar M, Tana M, Liu B, Frenette CT, et al. Race/Ethnicity-specific disparities in hepatocellular carcinoma stage at diagnosis and its impact on receipt of curative therapies. J Clin Gastroenterol (2016) 50(5):423–30. doi: 10.1097/MCG.0000000000000448
9. Wang S, Sun H, Xie Z, Li J, Hong G, Li D, et al. Improved survival of patients with hepatocellular carcinoma and disparities by age, race, and socioeconomic status by decade 1983-2012. Oncotarget (2016) 7(37):59820–33. doi: 10.1002/cncr.30103
10. Davila JA, El-Serag HB. Racial differences in survival of hepatocellular carcinoma in the united states: a population-based study. Clin Gastroenterol Hepatol (2006) 4(1):104–110; quiz 104-105. doi: 10.1038/srep33711
11. Ryerson AB, Eheman CR, Altekruse SF, Ward JW, Jemal A, Sherman RL, et al. Annual report to the nation on the status of cancer 1975-2012, featuring the increasing incidence of liver cancer. Cancer (2016) 122(9):1312–37. doi: 10.1016/S1542-3565(05)00745-7
12. Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the united states. Cancer Res (2014) 74(11):2913–21. doi: 10.1002/cncr.29936
13. Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocelllar carcinoma. Nat Rev Res Primers (2021) 7(1):6. doi: 10.1158/0008-5472.CAN-14-0155
14. Younossi Z, Stepanova M, Ong JP, Jacobson IM, Bugianesi E, Duseja A, et al. Nonalcoholic steatohepatitis is the fastest growing cause of hepatocellular carcinoma in liver transplant candidates. Clin Gastroenterol Hepatol (2019) 17(4):748–755 e743. doi: 10.1038/s41572-020-00240-3
15. Ioannou GN. Epidemiology and risk-stratification of NAFLD-associated HCC. J Hepatol (2021) 75(6):1476–84. doi: 10.1016/j.cgh.2018.05.057
16. Rinella ME. Nonalcoholic fatty liver disease: a systematic review. Jama (2015) 313(22):2263–73. doi: 10.1016/j.jhep.2021.08.012
17. Diehl AM, Day C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis. N Engl J Med (2017) 377(21):2063–72. doi: 10.1001/jama.2015.5370
18. Ogden CL, Fryar CD, Martin CB, Freedman DS, Carroll MD, Gu Q, et al. Trends in obesity prevalence by race and Hispanic origin-1999-2000 to 2017-2018. Jama (2020) 324(12):1208–10. doi: 10.1056/NEJMra1503519
19. Rodríguez JE, Campbell KM. Racial and ethnic disparities in prevalence and care of patients with type 2 diabetes. Clin Diabetes (2017) 35(1):66–70. doi: 10.1001/jama.2020.14590
20. Karimi K, Keßler T, Thiele K, Ramisch K, Erhardt A, Huebener P, et al. Prenatal acetaminophen induces liver toxicity in dams, reduces fetal liver stem cells, and increases airway inflammation in adult offspring. J Hepatol (2015) 62(5):1085–91. doi: 10.2337/cd15-0048
21. Thiele K, Solano ME, Huber S, Flavell RA, Kessler T, Barikbin R, et al. Prenatal acetaminophen affects maternal immune and endocrine adaptation to pregnancy, induces placental damage, and impairs fetal development in mice. Am J Pathol (2015) 185(10):2805–18. doi: 10.1016/j.jhep.2014.12.020
22. Blieden M, Paramore LC, Shah D, Ben-Joseph R. A perspective on the epidemiology of acetaminophen exposure and toxicity in the united states. Expert Rev Clin Pharmacol (2014) 7(3):341–8. doi: 10.1016/j.ajpath.2015.06.019
23. Singh S, Singh PP, Singh AG, Murad MH, Sanchez W. Statins are associated with a reduced risk of hepatocellular cancer: a systematic review and meta-analysis. Gastroenterology (2013) 144(2):323–32. doi: 10.1586/17512433.2014.904744
24. Facciorusso A, Abd El Aziz MA, Singh S, Pusceddu S, Milione M, Giacomelli L, et al. Statin use decreases the incidence of hepatocellular carcinoma: An updated meta-analysis. Cancers (Basel) (2020) 12(4):874. doi: 10.1053/j.gastro.2012.10.005
25. Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med (2018) 378(25):e34. doi: 10.3390/cancers12040874
26. Toledo E, Salas-Salvadó J, Donat-Vargas C, Buil-Cosiales P, Estruch R, Ros E, et al. Mediterranean Diet and invasive breast cancer risk among women at high cardiovascular risk in the PREDIMED trial: A randomized clinical trial. JAMA Intern Med (2015) 175(11):1752–60. doi: 10.1056/NEJMoa1800389
27. Salas-Salvadó J, Bulló M, Babio N, Martínez-González MA, Ibarrola-Jurado N, Basora J, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-reus nutrition intervention randomized trial. Diabetes Care (2011) 34(1):14–9. doi: 10.1001/jamainternmed.2015.4838
28. Salas-Salvadó J, Bulló M, Estruch R, Ros E, Covas MI, Ibarrola-Jurado N, et al. Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann Intern Med (2014) 160(1):1–10. doi: 10.2337/dc10-1288
29. Ji BT, Chow WH, Gridley G, Mclaughlin JK, Dai Q, Wacholder S, et al. Dietary factors and the risk of pancreatic cancer: A case-control study in shanghai China. Cancer Epidemiol Biomarkers Prev (1995) 4(8):885–93. doi: 10.7326/M13-1725
30. Gong Z, Holly EA, Wang F, Chan JM, Bracci PM. Intake of fatty acids and antioxidants and pancreatic cancer in a large population-based case-control study in the San Francisco bay area. Int J Cancer (2010) 127(8):1893–904. doi: 10.1002/ijc.25208
31. Jansen RJ, Robinson DP, Stolzenberg-Solomon RZ, Bamlet WR, de Andrade M, Oberg AL, et al. Fruit and vegetable consumption is inversely associated with having pancreatic cancer. Cancer Causes Control (2011) 22(12):1613–25. doi: 10.1002/ijc.25208
32. Heinen MM, Verhage BAJ, Goldbohm RA, van den Brandt PA. Intake of vegetables, fruits, carotenoids and vitamins c and e and pancreatic cancer risk in the Netherlands cohort study. Int J Cancer (2012) 130(1):147–58. doi: 10.1007/s10552-011-9838-0
33. Chan JM, Gong Z, Holly EA, Bracci PM. Dietary patterns and risk of pancreatic cancer in a large population-based case-control study in the San Francisco bay area. Nutr Cancer (2013) 65(1):157–64. doi: 10.1002/ijc.25989
34. Jansen RJ, Robinson DP, Stolzenberg-Solomon RZ, Bamlet WR, de Andrade M, Oberg AL, et al. Nutrients from fruit and vegetable consumption reduce the risk of pancreatic cancer. J Gastrointest Cancer (2013) 44(2):152–61. doi: 10.1080/01635581.2012.725502
35. Rothwell PM, Fowkes FGR, Belch JFF, Ogawa H, Warlow CP, TMeade TW. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet (2011) 377(9759):31–41. doi: 10.1007/s12029-012-9441-y
36. Hu J, La Vecchia C, Augustin LS, Negir E, de Groh M, Morrison H, et al. Glycemic index, glycemic load and cancer risk. Ann Oncol (2013) 24(1):245–51. doi: 10.1016/S0140-6736(10)62110-1
37. Shivappa N, Bosetti C, Zucchetto A, Serraino D, La Vecchia C, Hébert JR. Dietary inflammatory index and risk of pancreatic cancer in an Italian case-control study. Br J Nutr (2015) 113(2):292–8. doi: 10.1093/annonc/mds235
38. Gonzalez-Nahm S, Mendez M, Robinson W, Murphy SK, Hoyo C, Hogan V, et al. Low maternal adherence to a Mediterranean diet is associated with increase in methylation at the MEG3-IG differentially methylated region in female infants. Environ Epigenet (2017) 3(2):dvx007. doi: 10.1017/S0007114514003626
39. McCullough LE, Miller EE, Calderwood LE, Shivappa N, Steck SE, Forman MR, et al. Maternal inflammatory diet and adverse pregnancy outcomes: Circulating cytokines and genomic imprinting as potential regulators? Epigenetics (2017) 12(8):688–697. doi: 10.1080/15592294.2017.1347241
40. Devaraj S, Mathur S, Basu A, Aung HH, Vasu VT, Meyers S, et al. A dose-response study on the effects of purified lycopene supplementation on biomarkers of oxidative stress. J Am Coll Nutr (2008) 27(2):267–73. doi: 10.1080/15592294.2017.1347241
41. Meyer KA, Sijtsma FPC, Nettleton JA, Steffen LM, Van Horn L, Shikany JM, et al. Dietary patterns are associated with plasma F2-isoprostanes in an observational cohort study of adults. Free Radic Biol Med (2013) 57:201–9. doi: 10.1080/07315724.2008.10719699
42. Tamashiro KL, Moran TH. Perinatal environment and its influences on metabolic programming of offspring. Physiol Behav (2010) 100(5):560–6. doi: 10.1016/j.physbeh.2010.1004.1008
43. Dancause KN, Laplante DP, Hart KJ, O'Hara MW, Elgbeili G, Brunet A, et al. Prenatal stress due to a natural disaster predicts adiposity in childhood: The Iowa flood study. J Obes (2015) 2015:570541. doi: 10.1155/2015/570541
44. Fock KM, Khoo J. Diet and exercise in management of obesity and overweight. J Gastroenterol Hepatol (2013) 28 Suppl 4:59–63. doi: 10.1155/2015/570541
45. Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med (2016) 176(6):816–25. doi: 10.1111/jgh.12407
46. Yang H, Shi L, Wang Y, Duan G, Wang Y. RE: Physical activity and the risk of liver cancer: a systematic review and meta-analysis of prospective studies and a bias analysis. J Natl Cancer Inst (2019) 112(6):651–652. doi: 10.1001/jamainternmed.2016.1548
47. Zhang YB, Pan XF, Chen J, Cao A, Zhang YG, Xia L, et al. Combined lifestyle factors, incident cancer, and cancer mortality: a systematic review and meta-analysis of prospective cohort studies. Br J Cancer (2020) 122(7):1085–93. doi: 10.1093/jnci/djz187
48. Junga L. Associations between physical activity and liver cancer risks and mortality: A systematic review and meta-analysis. Int J Environ Res Public Health (2020) 17(23):8943. doi: 10.1038/s41416-020-0741-x
49. Wang A, Wang S, Zhu C, Huang H, Wu L, Wan X, et al. Coffee and cancer risk: A meta-analysis of prospective observational studies. Sci Rep (2016) 6:33711. doi: 10.1038/srep33711
50. Alicandro G, Tavani A, La Vecchia C. Coffee and cancer risk: A summary overview. Eur J Cancer Prev (2017) 26(5):424–32. doi: 10.1097/CEJ.0000000000000341
51. Godos J, Micek A, Marranzano M, Salomone F, Rio DD, Ray S. Coffee consumption and risk of biliary tract cancers and liver cancer: A dose-response meta-analysis of prospective cohort studies. Nutrients (2017) 9(9):950. doi: 10.3390/nu9090950
52. Kennedy OJ, Roderick P, Buchanan R, Fallowfield JA, Hayes PC, Parkes J. Coffee, including caffeinated and decaffeinated coffee, and the risk of hepatocellular carcinoma: A systematic review and dose-response meta-analysis. BMJ Open (2017) 7(5):e013739. doi: 10.1136/bmjopen-2016-013739
53. Tamura T, Hishida A, Wakai K. Coffee consumption and liver cancer risk in Japan: a meta-analysis of six prospective cohort studies. Nagoya J Med Sci (2019) 81(1):143–50. doi: 10.18999/nagjms.81.1.143
54. Tanaka K, Tamakoshi A, Sugawara Y, Mizoue T, Inoue M, Sawada N, et al. Coffee, green tea and liver cancer risk: An evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol (2019) 49(10):972–84. doi: 10.1093/jjco/hyz097
55. Olden K, Olden HA, Lin YS. The role of the epigenome in translating neighborhood disadvantage into health disparities. Curr Environ Health Rep (2015) 2(2):163–70. doi: 10.1007/s40572-015-0048-x
56. Boberg E, Lessner L, Carpenter DO. The role of residence near hazardous waste sites containing benzene in the development of hematologic cancers in upstate new York. Int J Occup Med Environ Health (2011) 24(4):327–38. doi: 10.2478/s13382-011-0037-8
57. Singer M. Down cancer alley: the lived experience of health and environmental suffering in louisiana's chemical corridor. Med Anthropol Q (2011) 25(2):141–63. doi: 10.1111/j.1548-1387.2011.01154.x
58. Lu X, Lessner L, Carpenter DO. Association between hospital discharge rate for female breast cancer and residence in a zip code containing hazardous waste sites. Environ Res (2014) 134:375–81. doi: 10.1016/j.envres.2014.07.005
59. King KE, Darrah TH, Money E, Meentemeyer R, Maguire RL, Nye MD, et al. Geographic clustering of elevated blood heavy metal levels in pregnant women. BMC Public Health (2015) 15(1):1035. doi: 10.1186/s12889-015-2379-9
60. Vahter M, Marafante E. Effects of low dietary intake of methionine, choline or proteins on the biotransformation of arsenite in the rabbit. Toxicol Lett (1987) 37(1):41–6. doi: 10.1016/0378-4274(87)90165-2
61. Nawrot T, Plusquin M, Hogervorst J, Roels HA, Celis H, Thijs L, et al. Environmental exposure to cadmium and risk of cancer: a prospective population-based study. Lancet Oncol (2006) 7(2):119–26. doi: 10.1016/S1470-2045(06)70545-9
62. McKelvey W, Gwynn RC, Jeffery N, Kass D, Thorpe LE, Garg RK, et al. A biomonitoring study of lead, cadmium, and mercury in the blood of New York city adults. Environ Health Perspect (2007) 115(10):1435–41. doi: 10.1289/ehp.10056
63. Russell MH, Waterland RL, Wong F. Calculation of chemical elimination half-life from blood with an ongoing exposure source: The example of perfluorooctanoic acid (PFOA). Chemosphere (2015) 129:210–6. doi: 10.1016/j.chemosphere.2014.07.061
64. Li Y, Fletcher T, Mucs D, Scott K, Lindh CH, Tallving P, et al. Half-lives of PFOS, PFHxS and PFOA after end of exposure to contaminated drinking water. Occup Environ Med (2018) 75(1):46–51. doi: 10.1136/oemed-2017-104651
65. Pizzurro DM, Seeley M, Kerper LE, Beck BD. Interspecies differences in perfluoroalkyl substances (PFAS) toxicokinetics and application to health-based criteria. Regul Toxicol Pharmacol (2019) 106:239–50. doi: 10.1016/j.yrtph.2019.05.008
66. Boffetta P. Carcinogenicity of trace elements with reference to evaluations made by the international agency for research on cancer. Scand J Work Environ Health (1993) 19 Suppl 1:67–70.
67. ATSDR. Agency for toxic substances and disease registry. In: The ATSDR 2011 substance priority list (2011). U.S. Department of Health and Human Services, CDC. Available at: http://www.atsdr.cdc.gov/.
68. Webb S, Bartos J, Boles R, Hasty E, Thuotte E, Thiex NJ. Simultaneous determination of arsenic, cadmium, calcium, chromium, cobalt, copper, iron, lead, magnesium, manganese, molybdenum, nickel, selenium, and zinc in fertilizers by microwave acid digestion and inductively coupled plasma-optical emission spectrometry detection: single-laboratory validation of a modification and extension of AOAC 2006.03. J AOAC Int (2014) 97(3):700–11. doi: 10.5740/jaoacint.13-408
69. Dharma-Wardana MWC. Fertilizer usage and cadmium in soils, crops and food. Environ Geochem Health (2018) 40(6):2739–2759. doi: 10.1007/s10653-018-0140-x
70. Rao ZX, Huang DY, Wu JS, Zhu QH, Zhu HH, Xu C, et al. Distribution and availability of cadmium in profile and aggregates of a paddy soil with 30-year fertilization and its impact on cd accumulation in rice plant. Environ pollut (2018) 239:198–204. doi: 10.1016/j.envpol.2018.04.024
71. Xu Y, Tang H, Liu T, Li Y, Huang X, Pi J. Effects of long-term fertilization practices on heavy metal cadmium accumulation in the surface soil and rice plants of double-cropping rice system in southern China. Environ Sci pollut Res Int (2018) 25(20):19836–19844. doi: 10.1007/s11356-018-2175-z
72. Organization, W. H, International Programme on Chemical Safety Environmental Health Criteria (INCHEM), International Programme on Chemical Safety Environmental Health Criteria (INCHEM). Cadmium. Environ Health Criteria (1992) 134:1–201.
74. Craig JA, Hoffman K, Stapleton HM, Calafat A, Ye X, Hoyo C, et al. Toxicological sciences under review (2020).
75. Hall SM, Patton S, Petreas M, Zhang S, Phillips AL, Hoffman K, et al. Per- and polyfluoroalkyl substances in dust collected from residential homes and fire stations in north America. Environ Sci Technol (2020) 54(22):14558–67. doi: 10.1021/acs.est.0c04869
76. Kotlarz N, McCord J, Collier D, Lea CS, Strynar M, Lindstrom AB, et al. Measurement of novel, drinking water-associated PFAS in blood from adults and children in Wilmington, north Carolina. Environ Health Perspect (2020) 128(7):77005. doi: 10.1289/EHP6837
77. Mijal RS, Holzman CB. Blood cadmium levels in women of childbearing age vary by race/ethnicity. Environ Res (2010) 110(5):505–12. doi: 10.1016/j.envres.2010.02.007
78. Aoki Y, Yee J, Mortensen ME. Blood cadmium by race/hispanic origin: The role of smoking. Environ Res (2017) 155:193–8. doi: 10.1016/j.envres.2017.02.016
79. Program NT. Report on carcinogens, fourteenth edition: Cadmium and cadmium compounds (2016). Available at: https://ntp.niehs.nih.gov/ntp/roc/content/profiles/cadmium.pdf.
80. Aalbers TG, Houtman JP, Makkink B. Trace-element concentrations in human autopsy tissue. Clin Chem (1987) 33(11):2057–64. doi: 10.1093/clinchem/33.11.2057
81. Yeung LWY, Guruge KS, Taniyasu S, Yamashita N, Angus PW, Herath CB. Profiles of perfluoroalkyl substances in the liver and serum of patients with liver cancer and cirrhosis in Australia. Ecotoxicol Environ Saf (2013) 96:139–46. doi: 10.1016/j.ecoenv.2013.06.006
82. Buha A, Wallace D, Matovic V, Schweitzer A, Oluic B, Micic D. Cadmium exposure as a putative risk factor for the development of pancreatic cancer: Three different lines of evidence. Biomed Res Int. (2017) 2017:1981837. doi: 10.1155/2017/1981837
83. Jackson TW, Ryherd GL, Scheibly CM, Sasser AL, Guillette TC, Belcher SM. Gestational cd exposure in the CD-1 mouse induces sex-specific hepatic insulin insensitivity, obesity, and metabolic syndrome in adult female offspring. Toxicol Sci (2020) 78(2):264–280. doi: 10.1093/toxsci/kfaa154
84. Hyder O, Chung M, Cosgrove D, Herman JM, Li Z, Firoozmand A, et al. Cadmium exposure and liver disease among US adults. J Gastrointest Surg (2013) 17(7):1265–73. doi: 10.1007/s11605-013-2210-9
85. Adebambo OA, Ray PD, Shea D, Fry RC. Toxicological responses of environmental mixtures: Environmental metal mixtures display synergistic induction of metal-responsive and oxidative stress genes in placental cells. Toxicol Appl Pharmacol (2015) 289(3):534–41. doi: 10.1016/j.taap.2015.10.005
86. Agarwal S, Zaman T, Tuzcu EM, Kapadia SR. Heavy metals and cardiovascular disease: results from the national health and nutrition examination survey (NHANES) 1999-2006. Angiology (2011) 62(5):422–9. doi: 10.1177/0003319710395562
87. Satarug S. Long-term exposure to cadmium in food and cigarette smoke, liver effects and hepatocellular carcinoma. Curr Drug Metab (2012) 13(3):257–71. doi: 10.2174/138920012799320446
88. Cousins IT, DeWitt JC, Glüge J, Goldenman G, Herzke D, Lohmann R, et al. Strategies for grouping per- and polyfluoroalkyl substances (PFAS) to protect human and environmental health. Environ Sci Process Impacts (2020) 22(7):1444–60. doi: 10.1039/D0EM00147C
89. Fenton SE, Ducatman A, Boobis A, DeWitt JC, Lau C, Ng C, et al. Per- and polyfluoroalkyl substance toxicity and human health review: Current state of knowledge and strategies for informing future research. Environ Toxicol Chem (2020) 40(3):606–30. doi: 10.1002/etc.4890
90. Hoyo C, Murtha AP, Schildkraut JM, Jirtle R, Demark-Wahnefried W, Forman MR, et al. Methylation variation at IGF2 differentially methylated regions and maternal folic acid use before and during pregnancy. Epigenetics (2011) 6(5):928–36.
91. Dolinoy DC, Weinhouse C, Jones TR, Rozek LS, Jirtle RL. Variable histone modifications at the Avy metastable epiallele. Epigenetics (2011) 5(7):637–44.
92. Kessler NJ, Waterland RA, Prentice AM, Silver MJ. Establishment of environmentally sensitive DNA methylation states in the very early human embryo. Sci Adv (2018) 4(7):eaat2624. doi: 10.1126/sciadv.aat2624
93. Hoyo C, Murphy SK, Jirtle RL. Imprint regulatory elements as epigenetic biosensors of exposure in epidemiological studies. J Epidemiol Community Health (2009) 63(9):683–4. doi: 10.1136/jech.2009.090803
94. Skaar DA, Li Y, Bernal AJ, Hoyo C, Murphy SK, Jirtle RL. The human imprintome: regulatory mechanisms, methods of ascertainment, and roles in disease susceptibility. ILAR J (2012) 53(3-4):341–58. doi: 10.1093/ilar.53.3-4.341
95. Murphy SK. Targeting the epigenome in ovarian cancer. Future Oncol (2012) 8(2):151–64. doi: 10.2217/fon.11.152
96. Murphy SK, Adigun A, Huang Z, Overcash F, Wang F, Jirtle RL, et al. Gender-specific methylation differences in relation to prenatal exposure to cigarette smoke. Gene (2012) 494(1):36–43. doi: 10.1016/j.gene.2011.11.062
97. Kitsiou-Tzeli S, Tzetis M. Maternal epigenetics and fetal and neonatal growth. Curr Opin Endocrinol Diabetes Obes (2017) 24(1):43–6. doi: 10.1097/MED.0000000000000305
98. Cassidy FC, Charalambous M. Genomic imprinting, growth and maternal-fetal interactions. J Exp Biol (2018) 221:1). doi: 10.1242/jeb.164517
99. Jima DD, Skaar DA, Planchart A, Motsinger-Reif A, Cevik SE, Park SS, et al. Genomic map of candidate human imprint control regions: The imprintome. Epigenetics (2022) 4: 1–24. oi: 10.1080/15592294.2022.2091815.
100. Hou L, Zhang X, Wang D, Baccarelli A. Environmental chemical exposures and human epigenetics. Int J Epidemiol (2012) 41(1):79–105. doi: 10.1093/ije/dyr154
101. Liu X, Zheng Y, Zhang W, Zhang X, Lioyd-Jones DM, Baccarelli AA, et al. Blood methylomics in response to arsenic exposure in a low-exposed US population. J Expo Sci Environ Epidemiol (2014) 24(2):145–9. doi: 10.1038/jes.2013.89
102. Vidal AC, Semenova V, Darrah T, Vengosh A, Huang Z, King K. Maternal cadmium, iron and zinc levels, DNA methylation and birth weight. BMC Pharmacol Toxicol (2015) 16(1):20. doi: 10.1186/s40360-015-0020-2
103. House JS, Hall J, Park SS, Planchart A, Money E, Maguire RL, et al. Cadmium exposure and MEG3 methylation differences between whites and African americans in the NEST cohort. Environ Epigenet (2019) 5(3):dvz014. doi: 10.1093/eep/dvz014
104. Cowley M, Skaar DA, Jima DD, Maguire RL, Hudson KM, Park SS, et al. Effects of cadmium exposure on DNA methylation at imprinting control regions and genome-wide in mothers and newborn children. Environ Health Perspect (2018) 126(3):037003. doi: 10.1289/EHP2085
105. Zhang C, Ge S, Wang J, Jing X, Li H, Mei S, et al. Epigenomic profiling of DNA methylation for hepatocellular carcinoma diagnosis and prognosis prediction. J Gastroenterol Hepatol (2019) 34(10):1869–77. doi: 10.1111/jgh.14694
106. Holmila R, Sklias A, Muller DC, Degli Esposti D, Guilloreau P, Mckay J, et al. Targeted deep sequencing of plasma circulating cell-free DNA reveals vimentin and fibulin 1 as potential epigenetic biomarkers for hepatocellular carcinoma. PloS One (2017) 12(3):e0174265. doi: 10.1371/journal.pone.0174265
107. Sun K, Jiang P, Chan KC, Wong J, Cheng YK, Liang RH, et al. Plasma DNA tissue mapping by genome-wide methylation sequencing for noninvasive prenatal, cancer, and transplantation assessments. Proc Natl Acad Sci U.S.A. (2015) 112(40):E5503–5512. doi: 10.1073/pnas.1508736112
108. Lo YM, Tein MS, Pang CC, Yeung CK, Tong KL, Hjelm NM. Presence of donor-specific DNA in plasma of kidney and liver-transplant recipients. Lancet (1998) 351(9112):1329–30. doi: 10.1016/S0140-6736(05)79055-3
109. Zheng YW, Chan KC, Sun H, Jiang P, Su X, Chen EZ, et al. Nonhematopoietically derived DNA is shorter than hematopoietically derived DNA in plasma: A transplantation model. Clin Chem (2012) 58(3):549–58. doi: 10.1373/clinchem.2011.169318
110. Drag MH, Kilpelainen TO. Cell-free DNA and RNA-measurement and applications in clinical diagnostics with focus on metabolic disorders. Physiol Genomics (2021) 53(1):33–46. doi: 10.1152/physiolgenomics.00086.2020
111. Larson MH, Pan W, Kim HJ, Mauntz RE, Stuart SM, Pimentel M, et al. A comprehensive characterization of the cell-free transcriptome reveals tissue- and subtype-specific biomarkers for cancer detection. Nat Commun (2021) 12(1):2357. doi: 10.1038/s41467-021-22444-1
112. Vanderburg C, Beheshti A. MicroRNAs (miRNAs), the final frontier: The hidden master regulators impacting biological response in all organisms due to spaceflight (2020). Available at: https://three.jsc.nasa.gov/articles/miRNA_Beheshti.pdf.
113. Ramos-Lopez O, Milagro FI, Riezu-Boj JI, Martinez JA. Epigenetic signatures underlying inflammation: An interplay of nutrition, physical activity, metabolic diseases, and environmental factors for personalized nutrition. Inflammation Res (2021) 70(1):29–49. doi: 10.1007/s00011-020-01425-y
114. Weber JA, Baxter DH, Zhang S, Huang DY, Huang KH, Lee MJ, et al. The microRNA spectrum in 12 body fluids. Clin Chem (2010) 56(11):1733–41. doi: 10.1373/clinchem.2010.147405
115. Carr LE, Virmani MD, Rosa F, Munblit D, Matazel KS, Elolimy AA, et al. Role of human milk bioactives on infants' gut and immune health. Front Immunol (2021) 12:604080. doi: 10.3389/fimmu.2021.604080
Keywords: liver cancer, race, epigenetic, contaminants, epigenome
Citation: Vidal AC, Moylan CA, Wilder J, Grant DJ, Murphy SK and Hoyo C (2022) Racial disparities in liver cancer: Evidence for a role of environmental contaminants and the epigenome. Front. Oncol. 12:959852. doi: 10.3389/fonc.2022.959852
Received: 02 June 2022; Accepted: 21 July 2022;
Published: 22 August 2022.
Edited by:
Jennie L. Williams, Stony Brook University, United StatesReviewed by:
Benjamin Zhan, Texas State University, United StatesCopyright © 2022 Vidal, Moylan, Wilder, Grant, Murphy and Hoyo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adriana C. Vidal, YXZpZGFsQG5jc3UuZWR1; Cathrine Hoyo, Y2hveW9AbmNzdS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.