
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Oncol. , 12 July 2022
Sec. Cancer Imaging and Image-directed Interventions
Volume 12 - 2022 | https://doi.org/10.3389/fonc.2022.925382
This article is part of the Research Topic Women in Cancer Imaging and Image-directed Interventions Vol II: 2022 View all 18 articles
 Jingjing Wang1,2,3
Jingjing Wang1,2,3 Ruolin Wu1,2,3
Ruolin Wu1,2,3 Fang Liu1,2,3
Fang Liu1,2,3 Liu Yang4
Liu Yang4 Fan Hu1,2,3
Fan Hu1,2,3 Zhijian Wu1,2,3
Zhijian Wu1,2,3 Zairong Gao1,2,3*
Zairong Gao1,2,3* Xiaotian Xia1,5*
Xiaotian Xia1,5*Cutaneous and subcutaneous soft tissue metastases are rare in lung adenocarcinoma and suggest poor prognosis. We report a patient with lung adenocarcinoma who initially presented with cutaneous and subcutaneous metastases to the abdomen that were initially presumed to be herpes zoster and an occult subcutaneous soft tissue mass. Because the lesions progressed over 3 weeks despite routine herpes zoster treatment, magnetic resonance imaging was performed and showed a presumed sarcoma; however, 18F-fluourodeoxyglucose positron emission tomography/computed tomography demonstrated pulmonary lesions. Biopsy of the abdominal lesion confirmed poorly differentiated lung adenocarcinoma. Early diagnosis of soft tissue metastasis can be difficult. Clinicians should suspect internal organ malignancy when a progressive cutaneous or subcutaneous soft tissue lesion is encountered.
Lung cancer is a frequently encountered malignancy that can metastasize to almost all organs and is associated with high mortality (1, 2). Lung adenocarcinoma commonly metastasizes to the liver, adrenal glands, brain, and bone (3). Soft tissue metastases from lung adenocarcinoma are rare and occur predominantly in men (4). They may be apparent before the primary tumor and typically herald a poor prognosis. Reported mean survival in patients with skin metastases is 2.9 months (5), so early diagnosis and treatment are important. However, the diagnosis of skin metastases may be delayed or missed. A high index of suspicion is required.
A 52-year-old woman presented with a 3-week history of painful rash and subcutaneous soft tissue mass overlying the right abdomen at the waistline. She denied constitutional symptoms such as fever, chills, night sweats, and unintentional weight loss. There was no history of major trauma, surgery, smoking, alcohol use, or drug or food allergy. Notably, the patient was exposed to secondhand smoke from nicotine cigarettes due to her husband’s smoking. In addition, her father died of esophageal cancer. Herpes zoster was initially suspected but appropriate treatment did not result in clinical improvement. In fact, progression had occurred. Therefore, she was hospitalized for further investigation and treatment. Physical examination showed a raised skin mass surrounded by swelling and erythema on the right abdomen (Figure 1A). Serum erythrocyte sedimentation rate, C-reactive protein, white blood cell count, and multiple tumor markers were elevated. Ultrasonography revealed a solid mass underneath the rash. On magnetic resonance imaging (MRI), the mass was 10 cm in diameter and inhomogeneous on T2-weighted sequences (Figures 1B, C) and exhibited markedly restricted diffusion on diffusion-weighted sequences (Figure 1D). The mass was suspected to be a sarcoma. To investigate potential distant metastases, 18F-fluourodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) was performed, which showed the previously demonstrated large abdominal mass was hypermetabolic in the periphery and hypometabolic in the center (Figure 2A); other hypermetabolic lesions were shown in the right lung and the posterior pleural wall (Figure 2B–E). Lung cancer with metastases was suspected and the patient underwent ultrasound-guided biopsy of the subcutaneous soft tissue mass. Examination of hematoxylin and eosin-stained specimen (Figure 3A) revealed abundant oval and plump cells with enlarged nuclei and red, broad cytoplasm. Immunohistochemical examination showed staining was positive for CK7 (Figure 3B), TTF-1 (Figure 3C), and PCK but negative for P63, CK20, Villin, ER, CDX2, HER2, P16, GATA-3, and VT-1. This suggested a diagnosis of primary pulmonary adenocarcinoma with metastasis. Because PDL-1 was expressed (Figure 3D) and EGFR mutation was not detected, the patient was placed on bevacizumab plus pemetrexed–platinum doublet chemotherapy. After six cycles, the primary pulmonary lesions shrunk but the cutaneous lesions did not. Molecular testing revealed mutation in the BRAF 15 exon and targeted therapy was proposed, but the patient refused for financial reasons. For relieving the patient’s pain, palliative radiotherapy was initiated.
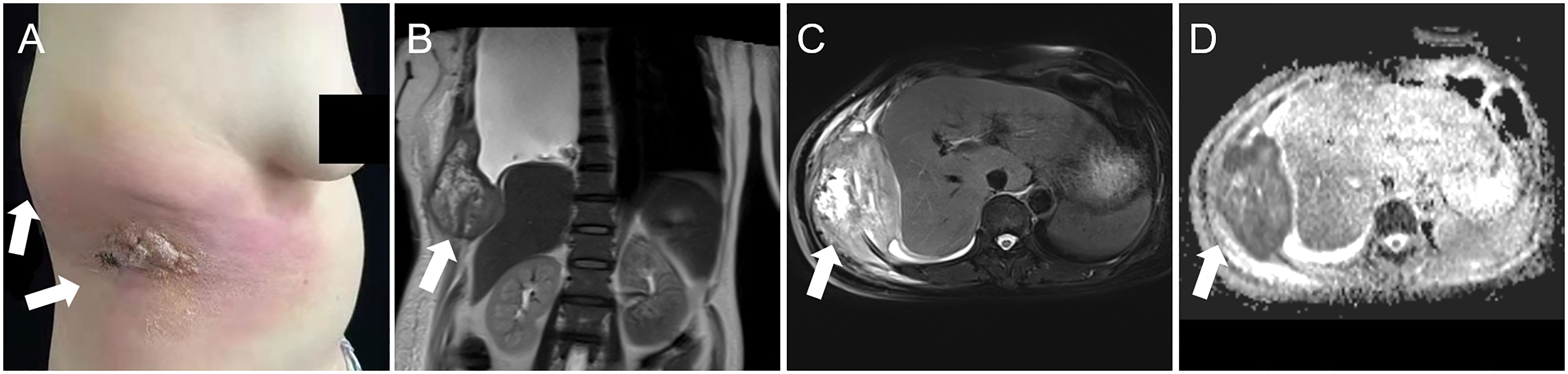
Figure 1 Physical examination showed an erythematous rash and swelling surrounding a skin mass on the right abdomen (A, arrows). Magnetic resonance imaging shoed an inhomogeneous soft tissue mass approximately 10 cm in diameter (B, coronal T2-weighted image; C, axial fat saturation T2-weighted image). The lesion also showed markedly restricted diffusion on diffusion-weighted sequences (D, arrow).
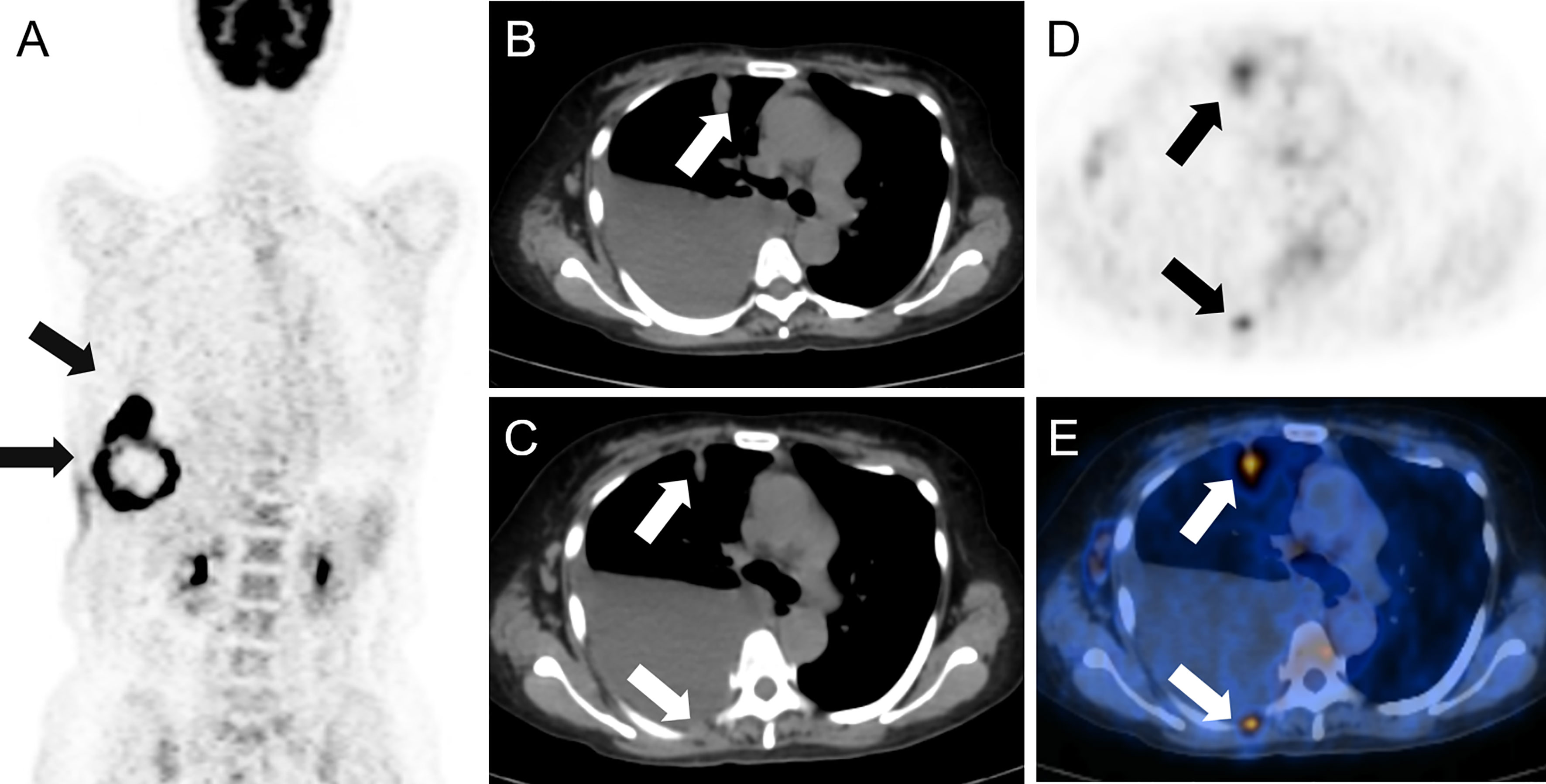
Figure 2 A large mass showing hypermetabolism peripherally and hypometabolism centrally was found on 18F-fluorodeoxyglucose positron emission tomography/computed tomography (A), arrows. Hypermetabolic lesions were imaged in the right lung and the posterior pleural wall (arrows) on axial computed tomography (B, C), positron emission tomography (D) and fusion imaging (E).
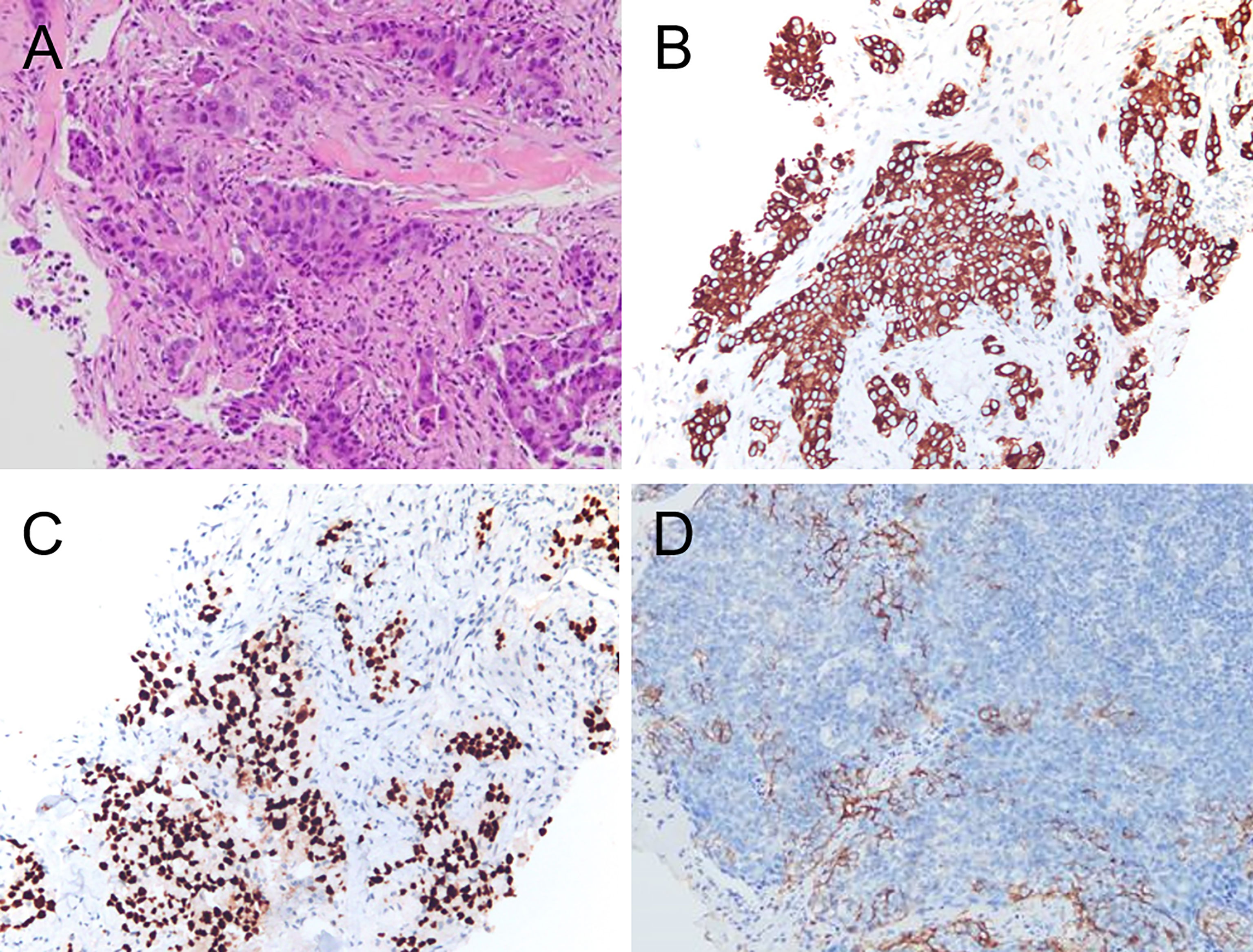
Figure 3 Hematoxylin and eosin staining revealed the tumor was composed of abundant oval and plump cells with enlarged nuclei and red, broad cytoplasm (A). Immunohistochemical staining for CK 7 (B) showed a strong and diffuse brown cytoplasmic reaction. TTF-1 staining (C) Showed strong nuclear staining of tumor cells. Immunohistochemical analysis showed PDL-1 expression (D).
Lung cancer morbidity and mortality is highest of all cancers (1, 2) and lung adenocarcinoma accounts for approximately 40% of all lung cancers (6). Although lung carcinoma can metastasize to all organs, the liver, adrenal glands, bone, kidney, and brain are the most common sites (3). Metastasis to cutaneous and subcutaneous soft tissues is rare, with reported incidence rates ranging between 1% and 12% (5, 7–9). Soft tissue metastasis can be challenging to diagnose when it is the initial cancer manifestation, as in our patient, who presented with a painful rash in the absence of typical lung adenocarcinoma symptoms (10). Soft tissue metastases may rapidly progress when the initial diagnosis is missed.
To evaluate soft tissue metastases, MRI is the most sensitive and specific imaging modality and enables assessment of tissue characteristics, tumor extent, and areas of reactivity (11, 12). In our patient, MRI was highly suspicious for sarcoma but 18F-FDG PET/CT suggested a lung primary, which was confirmed by biopsy. Although MRI can distinguish between benign and malignant tumors, it cannot further distinguish malignancy. Compared with sarcoma, soft tissue metastases from organ malignancies are rare. They are easily missed, especially when symptoms of the primary are absent or atypical. Therefore, 18F-FDG PET/CT before biopsy is essential to improve diagnostic accuracy and distinguish soft tissue masses.
Optimal management requires accurate diagnosis, which requires biopsy in most cases (13, 14). In our patient, histopathological and immunohistochemical examinations resulted in a diagnosis of poorly differentiated pulmonary adenocarcinoma (15, 16). In this disease, the appearance of metastatic soft tissue masses indicates an advanced stage and poor prognosis. Chemotherapy, immunotherapy, targeted therapy, and radiotherapy are the mainstay treatments for soft tissue metastasis; surgery is not typically recommended (17–19). Unfortunately, six cycles of bevacizumab plus pemetrexed–platinum doublet chemotherapy were not as effective as we had hoped. The targeted therapy has been shown to decrease tumor burden, decrease symptoms, and dramatically improve survival outcomes in advanced lung cancers (19, 20). However, our patient refused the targeted therapy for financial reasons. Then palliative radiotherapy was initiated and proved effective for pain relief. To date, the patient’s general condition has remained stable.
Early diagnosis of soft tissue metastasis can be difficult. Clinicians should suspect internal organ malignancy when a progressive cutaneous or subcutaneous soft tissue lesion is encountered. A thorough examination should be performed and 18F-FDG PET/CT should be considered for further evaluation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethical Committee of Union Hospital, Tongji Medical College. The patients/participants provided their written informed consent to participate in this study.
JW, RW, LY, ZW and XX obtained and analyzed the clinical data. JW and XX wrote the manuscript. FL and FH designed and constructed the figures. XX and ZG designed the study. All authors contributed to patient care and writing and revising the manuscript and figures. All authors contributed to the article and approved the submitted version.
This research was supported by the National Natural Science Foundation of China (Grant Numbers 81801737, 81771866).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank Dr. Ranran Ding for providing and analyzing the immunohistochemical data of CK7 and TTF-1. We thank Liwen Bianji (Edanz) (https://www.liwenbianji.cn) for editing the language of a draft of this manuscript.
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin (2021) 71(1):7–33. doi: 10.3322/caac.21654
2. Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global Surveillance of Trends in Cancer Survival 2000–14 (Concord-3): Analysis of Individual Records for 37 513 025 Patients Diagnosed With One of 18 Cancers From 322 Population-Based Registries in 71 Countries. Lancet (2018) 391(10125):1023–75. doi: 10.1016/s0140-6736(17)33326-3
3. Tamura T, Kurishima K, Nakazawa K, Kagohashi K, Ishikawa H, Satoh H, et al. Specific Organ Metastases and Survival in Metastatic Non-Small-Cell Lung Cancer. Mol Clin Oncol (2015) 3(1):217–21. doi: 10.3892/mco.2014.410
4. Alcaraz I, Cerroni L, Rütten A, Kutzner H, Requena L. Cutaneous Metastases From Internal Malignancies: A Clinicopathologic and Immunohistochemical Review. Am J Dermatopathol (2012) 34(4):347–93. doi: 10.1097/DAD.0b013e31823069cf
5. Song Z, Lin B, Shao L, Zhang Y. Cutaneous Metastasis as a Initial Presentation in Advanced Non-Small Cell Lung Cancer and Its Poor Survival Prognosis. J Cancer Res Clin Oncol (2012) 138(10):1613–7. doi: 10.1007/s00432-012-1239-6
6. Tvedten E, Deak Z, Schwartz B, Rice A. An Atypical Presentation of Soft Tissue Metastasis in a Patient With Lung Cancer. Cureus (2021) 13(7):e16294. doi: 10.7759/cureus.16294
7. Gül U, Kiliç A, Gönül M, Külcü Cakmak S, Erinçkan C. Spectrum of Cutaneous Metastases in 1287 Cases of Internal Malignancies: A Study From Turkey. Acta dermato-venereol (2007) 87(2):160–2. doi: 10.2340/00015555-0199
8. Dhambri S, Zendah I, Ayadi-Kaddour A, Adouni O, El Mezni F. Cutaneous Metastasis of Lung Carcinoma: A Retrospective Study of 12 Cases. J Eur Acad Dermatol Venereol JEADV (2011) 25(6):722–6. doi: 10.1111/j.1468-3083.2010.03818.x
9. Hidaka T, Ishii Y, Kitamura S. Clinical Features of Skin Metastasis From Lung Cancer. Internal Med (1996) 35(6):459–62. doi: 10.2169/internalmedicine.35.459
10. Kocher F, Hilbe W, Seeber A, Pircher A, Schmid T, Greil R, et al. Longitudinal Analysis of 2293 Nsclc Patients: A Comprehensive Study From the Tyrol Registry. Lung Cancer (2015) 87(2):193–200. doi: 10.1016/j.lungcan.2014.12.006
11. Mayerson JL, Scharschmidt TJ, Lewis VO, Morris CD. Diagnosis and Management of Soft-Tissue Masses. J Am Acad Orthop Surg (2014) 22(11):742–50. doi: 10.5435/jaaos-22-11-742
12. Miwa S, Otsuka T. Practical Use of Imaging Technique for Management of Bone and Soft Tissue Tumors. J Orthopaedic Sci (2017) 22(3):391–400. doi: 10.1016/j.jos.2017.01.006
13. Khoo M, Pressney I, Hargunani R, Saifuddin A. Small, Superficial, Indeterminate Soft-Tissue Lesions as Suspected Sarcomas: Is Primary Excision Biopsy Suitable? Skeletal Radiol (2017) 46(7):919–24. doi: 10.1007/s00256-017-2635-4
14. Fenzl L, Bubel K, Mehrmann M, Schneider G. Bildgebung Und Biopsie Von Weichteiltumoren. Der Radiologe (2018) 58(1):79–92. doi: 10.1007/s00117-017-0331-y
15. Kummar S, Fogarasi M, Canova A, Mota A, Ciesielski T. Cytokeratin 7 and 20 Staining for the Diagnosis of Lung and Colorectal Adenocarcinoma. Br J Cancer (2002) 86(12):1884–7. doi: 10.1038/sj.bjc.6600326
16. Ordóñez NG. Value of Thyroid Transcription Factor-1, E-Cadherin, Bg8, Wt1, and Cd44s Immunostaining in Distinguishing Epithelial Pleural Mesothelioma From Pulmonary and Nonpulmonary Adenocarcinoma. Am J Surg Pathol (2000) 24(4):598–606. doi: 10.1097/00000478-200004000-00016
17. Damron TA, Heiner J. Distant Soft Tissue Metastases: A Series of 30 New Patients and 91 Cases From the Literature. Ann Surg Oncol (2000) 7(7):526–34. doi: 10.1007/s10434-000-0526-7
18. Hashimoto K, Nishimura S, Akagi M. Lung Adenocarcinoma Presenting as a Soft Tissue Metastasis to the Shoulder: A Case Report. Medicina (Kaunas Lithuania) (2021) 57(2):181. doi: 10.3390/medicina57020181
19. Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman J, Chirieac LR, et al. Non-Small Cell Lung Cancer, Version 5.2017, Nccn Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Network JNCCN (2017) 15(4):504–35. doi: 10.6004/jnccn.2017.0050
Keywords: lung adenocarcinoma, soft tissue, skin rashes, metastasis, 18F-FDG, PET/CT
Citation: Wang J, Wu R, Liu F, Yang L, Hu F, Wu Z, Gao Z and Xia X (2022) Case Report: Lung Adenocarcinoma Initially Presenting With Cutaneous and Subcutaneous Metastases. Front. Oncol. 12:925382. doi: 10.3389/fonc.2022.925382
Received: 21 April 2022; Accepted: 23 June 2022;
Published: 12 July 2022.
Edited by:
Pilar López-Larrubia, Spanish National Research Council (CSIC), SpainReviewed by:
Murat Fani BOZKURT, Hacettepe University, TurkeyCopyright © 2022 Wang, Wu, Liu, Yang, Hu, Wu, Gao and Xia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zairong Gao, Z2FvYm9ubkBodXN0LmVkdS5jbg==; Xiaotian Xia, WGlheGlhb3RpYW5feGlhQGh1c3QuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.